User login
Not All Stool Discussions Are Unproductive
On August 22, 2014, a baby girl was born healthy and at full term. She was discharged on August 24 after a routine hospital stay. A day later, the infant’s mother called the pediatrician’s emergency after-hours hotline, in distress. She was concerned because the infant had not had a bowel movement since August 23. She was also concerned that each feeding was lasting an hour. A nurse told the mother that her concerns would be discussed in a routine follow-up appointment scheduled for the next morning.
At the appointment, the pediatrician noted the infant was having feeding problems and had lost 11% of her at-birth weight. The pediatrician also noted a high respiratory rate and abnormal skin coloring. However, the pediatrician concluded that the infant’s feeding problems had resolved, reassured the parents she was healthy, and discharged her, telling her parents to return in 2 weeks.
On August 29, the mother again called the pediatrician’s office, this time with concerns over a decrease in the infant’s feeding. A nurse told her to bring the infant to the emergency department (ED). At the ED, the infant was found to have lost 12% of her weight since birth and to be severely dehydrated. Due to hypovolemia, health care providers could not complete lab tests on the infant until aggressive resuscitation had been performed for 4 hours. The infant’s lab values showed she had hypernatremia, which put her at risk for brain injury through a decrease in cellular hydration, increased vascular permeability, or elevated intracranial pressure.
The infant did sustain a permanent brain injury from the condition: right-side paralysis. Her multi-organ failure from dehydration also caused significant damage to her left kidney, which stopped functioning altogether in 2017.
The infant sued her pediatrician and his office. Plaintiff’s counsel stated that the infant’s early weight loss was a red flag and that the standard of care required the pediatrician to order in-office follow-up within 24 hours to confirm if the loss had been corrected. Plaintiff’s counsel also alleged the baby’s respiratory rate and poor coloring were also red flags for dehydration. He further alleged that if the infant had returned to the office, her weight loss would have prompted supplementation before the dehydration caused her brain injury.
VERDICT
The case was settled for $1,375,000.
COMMENTARY
This case merits discussion because it involves a type of patient many clinicians see in practice. Complaints of newborn and infant feeding problems are common. Most cases require reassurance and troubleshooting about common feeding problems—but the clinician must be on the lookout for serious issues. Thus, it is helpful to revisit expected newborn feeding, stooling, and weight status.
Continue to: With regard to feeding...
With regard to feeding, breastfed infants should receive between 8-12 feeds per day during the newborn hospitalization.1 Bottlefed infants should be fed 20 kcal per 30 mL of iron-containing formula. Infants are fed on demand, and the duration of the feeding should not exceed 4 hours. The volume of the feed for the first few days of life should be 15-30 mL per feed.
For breastfed infants, clinicians should be attentive to issues that can impact nutrition, including latching difficulties, pain, mastitis, blocked duct, and engorgement. These can limit nutrition and be extremely upsetting to the mother.
Stooling frequency for newborns varies and depends on whether the infant is bottle fed or breast fed. During the first week of life, infants pass a mean of 4 stools per day.2 Breastfed infants may have as few as one stool per day, increasing as mother’s milk production increases.2
With regard to weight loss, term infants may lose up to 10% of their birth weight in the first few days of life, which is typically regained in 10 to 14 days.1 Infants born via cesarean section lose more weight, with 25% of these babies losing more than 10% by 72 hours. Of them, 76% return to birth weight by 14 days and 92% by 21 days. By contrast, vaginally born infants regain weight faster, with 86% returning to their birth weight by 14 days and 95% by the 21st day.1
Here, the infant was term and healthy, but we are not told some important details. Was she breast fed or bottle fed? Was she born by cesarean section or vaginally? We do know she was discharged on August 24th, her mother called the hotline on the 25th, and she was seen by the pediatrician on the 26th—at which point the infant had not stooled in 3 days. The mother called the physician’s office again on August 29th and was sent to the ED. We are told only that each feeding lasted an hour and the infant hadn’t stooled.
Continue to: Regarding stool...
Regarding stool—we have all had discussions with patients regarding hypervigilant concerns about stool color. We know there are some big things to look for with stool color (eg, black tarry reveals upper GI bleeding, while clay-colored or pale may reveal the absence of bile). Yet, patients’ expectations of the color-coded diagnostic abilities of their stool knows no bounds. Patients are convinced that we have some color wheel in our jacket pocket corresponding to stool color—and that the nuances between shades have important medical implications. If you ask, “Would you say it is more marigold, butterscotch yellow, or Tuscan sun?” … your patient will have an answer.
Patients reveal stool color hesitantly, reservedly, with nervous expectation. They wait for your response in quivering anticipation that the coming reply will include words to the effect that a boysenberry-purple stool is equivalent to a Death tarot card. A subconjunctival hemorrhage is the only thing that approaches the anxiety level of the oddly hued stool (Oddly Hued Stool Anxiety). Woe be the patient with both. For a patient bearing a subconjunctival hemorrhage who has also passed a jungle-green stool in the past 24 hours fully expects to explode within the next 60 minutes.
I’ve been rather facetious for a reason. My purpose is to acknowledge and to help you recognize that most discussions regarding stooling will not be (forgive me) productive. They are not productive because most stool coloration issues are nonentities—yet they produce patient anxiety that takes some time to address, leaving a busy clinician prone to curtly dismiss such discussions out of hand. Because many patient-initiated stool discussions aren’t productive, there is the risk for stool tune-out. As gross and unproductive as they can be, don’t tune out all stool discussions.
In this case, the appropriate frequency of stooling should have been at least once per day. For newborns, a stool color question is helpful; stool should not be white, pale, or clay-colored, which is suggestive of acholic stools from biliary atresia. Here, despite the absence of stool over a 3-day period, the defendant concluded the feeding problem was resolved and set a return visit for 2 weeks later. The plaintiff’s expert contended that the weight loss and absence of stooling was evidence of inadequate intake and warranted a return check the next day. Rather than risk the case going to trial, the defendant settled for $1,375,000.
IN SUM
Newborn nutrition is important. Understand that parents will be anxious about newborn feeding, although often there is no major medical concern. However, do not be dismissive of feeding concerns because of this expected anxiety. Listen to the parents fully, paying particular attention to quantifying feeding difficulty and stooling frequency matters. Don’t let patients’ rainbow parade of needless stool concerns blind you to considering important information. In other words, don’t be a stool fool.
1. McKee-Garrett TM. Overview of the routine management of the healthy newborn infant. UpToDate. Updated July 12, 2019. www.uptodate.com/contents/overview-of-the-routine-management-of-the-healthy-newborn-infant. Accessed November 18, 2019.
2. Sood MR. Constipation in infants and children: evaluation. UpToDate. Updated August 1, 2019. www.uptodate.com/contents/constipation-in-infants-and-children-evaluation. Accessed November 18, 2019.
On August 22, 2014, a baby girl was born healthy and at full term. She was discharged on August 24 after a routine hospital stay. A day later, the infant’s mother called the pediatrician’s emergency after-hours hotline, in distress. She was concerned because the infant had not had a bowel movement since August 23. She was also concerned that each feeding was lasting an hour. A nurse told the mother that her concerns would be discussed in a routine follow-up appointment scheduled for the next morning.
At the appointment, the pediatrician noted the infant was having feeding problems and had lost 11% of her at-birth weight. The pediatrician also noted a high respiratory rate and abnormal skin coloring. However, the pediatrician concluded that the infant’s feeding problems had resolved, reassured the parents she was healthy, and discharged her, telling her parents to return in 2 weeks.
On August 29, the mother again called the pediatrician’s office, this time with concerns over a decrease in the infant’s feeding. A nurse told her to bring the infant to the emergency department (ED). At the ED, the infant was found to have lost 12% of her weight since birth and to be severely dehydrated. Due to hypovolemia, health care providers could not complete lab tests on the infant until aggressive resuscitation had been performed for 4 hours. The infant’s lab values showed she had hypernatremia, which put her at risk for brain injury through a decrease in cellular hydration, increased vascular permeability, or elevated intracranial pressure.
The infant did sustain a permanent brain injury from the condition: right-side paralysis. Her multi-organ failure from dehydration also caused significant damage to her left kidney, which stopped functioning altogether in 2017.
The infant sued her pediatrician and his office. Plaintiff’s counsel stated that the infant’s early weight loss was a red flag and that the standard of care required the pediatrician to order in-office follow-up within 24 hours to confirm if the loss had been corrected. Plaintiff’s counsel also alleged the baby’s respiratory rate and poor coloring were also red flags for dehydration. He further alleged that if the infant had returned to the office, her weight loss would have prompted supplementation before the dehydration caused her brain injury.
VERDICT
The case was settled for $1,375,000.
COMMENTARY
This case merits discussion because it involves a type of patient many clinicians see in practice. Complaints of newborn and infant feeding problems are common. Most cases require reassurance and troubleshooting about common feeding problems—but the clinician must be on the lookout for serious issues. Thus, it is helpful to revisit expected newborn feeding, stooling, and weight status.
Continue to: With regard to feeding...
With regard to feeding, breastfed infants should receive between 8-12 feeds per day during the newborn hospitalization.1 Bottlefed infants should be fed 20 kcal per 30 mL of iron-containing formula. Infants are fed on demand, and the duration of the feeding should not exceed 4 hours. The volume of the feed for the first few days of life should be 15-30 mL per feed.
For breastfed infants, clinicians should be attentive to issues that can impact nutrition, including latching difficulties, pain, mastitis, blocked duct, and engorgement. These can limit nutrition and be extremely upsetting to the mother.
Stooling frequency for newborns varies and depends on whether the infant is bottle fed or breast fed. During the first week of life, infants pass a mean of 4 stools per day.2 Breastfed infants may have as few as one stool per day, increasing as mother’s milk production increases.2
With regard to weight loss, term infants may lose up to 10% of their birth weight in the first few days of life, which is typically regained in 10 to 14 days.1 Infants born via cesarean section lose more weight, with 25% of these babies losing more than 10% by 72 hours. Of them, 76% return to birth weight by 14 days and 92% by 21 days. By contrast, vaginally born infants regain weight faster, with 86% returning to their birth weight by 14 days and 95% by the 21st day.1
Here, the infant was term and healthy, but we are not told some important details. Was she breast fed or bottle fed? Was she born by cesarean section or vaginally? We do know she was discharged on August 24th, her mother called the hotline on the 25th, and she was seen by the pediatrician on the 26th—at which point the infant had not stooled in 3 days. The mother called the physician’s office again on August 29th and was sent to the ED. We are told only that each feeding lasted an hour and the infant hadn’t stooled.
Continue to: Regarding stool...
Regarding stool—we have all had discussions with patients regarding hypervigilant concerns about stool color. We know there are some big things to look for with stool color (eg, black tarry reveals upper GI bleeding, while clay-colored or pale may reveal the absence of bile). Yet, patients’ expectations of the color-coded diagnostic abilities of their stool knows no bounds. Patients are convinced that we have some color wheel in our jacket pocket corresponding to stool color—and that the nuances between shades have important medical implications. If you ask, “Would you say it is more marigold, butterscotch yellow, or Tuscan sun?” … your patient will have an answer.
Patients reveal stool color hesitantly, reservedly, with nervous expectation. They wait for your response in quivering anticipation that the coming reply will include words to the effect that a boysenberry-purple stool is equivalent to a Death tarot card. A subconjunctival hemorrhage is the only thing that approaches the anxiety level of the oddly hued stool (Oddly Hued Stool Anxiety). Woe be the patient with both. For a patient bearing a subconjunctival hemorrhage who has also passed a jungle-green stool in the past 24 hours fully expects to explode within the next 60 minutes.
I’ve been rather facetious for a reason. My purpose is to acknowledge and to help you recognize that most discussions regarding stooling will not be (forgive me) productive. They are not productive because most stool coloration issues are nonentities—yet they produce patient anxiety that takes some time to address, leaving a busy clinician prone to curtly dismiss such discussions out of hand. Because many patient-initiated stool discussions aren’t productive, there is the risk for stool tune-out. As gross and unproductive as they can be, don’t tune out all stool discussions.
In this case, the appropriate frequency of stooling should have been at least once per day. For newborns, a stool color question is helpful; stool should not be white, pale, or clay-colored, which is suggestive of acholic stools from biliary atresia. Here, despite the absence of stool over a 3-day period, the defendant concluded the feeding problem was resolved and set a return visit for 2 weeks later. The plaintiff’s expert contended that the weight loss and absence of stooling was evidence of inadequate intake and warranted a return check the next day. Rather than risk the case going to trial, the defendant settled for $1,375,000.
IN SUM
Newborn nutrition is important. Understand that parents will be anxious about newborn feeding, although often there is no major medical concern. However, do not be dismissive of feeding concerns because of this expected anxiety. Listen to the parents fully, paying particular attention to quantifying feeding difficulty and stooling frequency matters. Don’t let patients’ rainbow parade of needless stool concerns blind you to considering important information. In other words, don’t be a stool fool.
On August 22, 2014, a baby girl was born healthy and at full term. She was discharged on August 24 after a routine hospital stay. A day later, the infant’s mother called the pediatrician’s emergency after-hours hotline, in distress. She was concerned because the infant had not had a bowel movement since August 23. She was also concerned that each feeding was lasting an hour. A nurse told the mother that her concerns would be discussed in a routine follow-up appointment scheduled for the next morning.
At the appointment, the pediatrician noted the infant was having feeding problems and had lost 11% of her at-birth weight. The pediatrician also noted a high respiratory rate and abnormal skin coloring. However, the pediatrician concluded that the infant’s feeding problems had resolved, reassured the parents she was healthy, and discharged her, telling her parents to return in 2 weeks.
On August 29, the mother again called the pediatrician’s office, this time with concerns over a decrease in the infant’s feeding. A nurse told her to bring the infant to the emergency department (ED). At the ED, the infant was found to have lost 12% of her weight since birth and to be severely dehydrated. Due to hypovolemia, health care providers could not complete lab tests on the infant until aggressive resuscitation had been performed for 4 hours. The infant’s lab values showed she had hypernatremia, which put her at risk for brain injury through a decrease in cellular hydration, increased vascular permeability, or elevated intracranial pressure.
The infant did sustain a permanent brain injury from the condition: right-side paralysis. Her multi-organ failure from dehydration also caused significant damage to her left kidney, which stopped functioning altogether in 2017.
The infant sued her pediatrician and his office. Plaintiff’s counsel stated that the infant’s early weight loss was a red flag and that the standard of care required the pediatrician to order in-office follow-up within 24 hours to confirm if the loss had been corrected. Plaintiff’s counsel also alleged the baby’s respiratory rate and poor coloring were also red flags for dehydration. He further alleged that if the infant had returned to the office, her weight loss would have prompted supplementation before the dehydration caused her brain injury.
VERDICT
The case was settled for $1,375,000.
COMMENTARY
This case merits discussion because it involves a type of patient many clinicians see in practice. Complaints of newborn and infant feeding problems are common. Most cases require reassurance and troubleshooting about common feeding problems—but the clinician must be on the lookout for serious issues. Thus, it is helpful to revisit expected newborn feeding, stooling, and weight status.
Continue to: With regard to feeding...
With regard to feeding, breastfed infants should receive between 8-12 feeds per day during the newborn hospitalization.1 Bottlefed infants should be fed 20 kcal per 30 mL of iron-containing formula. Infants are fed on demand, and the duration of the feeding should not exceed 4 hours. The volume of the feed for the first few days of life should be 15-30 mL per feed.
For breastfed infants, clinicians should be attentive to issues that can impact nutrition, including latching difficulties, pain, mastitis, blocked duct, and engorgement. These can limit nutrition and be extremely upsetting to the mother.
Stooling frequency for newborns varies and depends on whether the infant is bottle fed or breast fed. During the first week of life, infants pass a mean of 4 stools per day.2 Breastfed infants may have as few as one stool per day, increasing as mother’s milk production increases.2
With regard to weight loss, term infants may lose up to 10% of their birth weight in the first few days of life, which is typically regained in 10 to 14 days.1 Infants born via cesarean section lose more weight, with 25% of these babies losing more than 10% by 72 hours. Of them, 76% return to birth weight by 14 days and 92% by 21 days. By contrast, vaginally born infants regain weight faster, with 86% returning to their birth weight by 14 days and 95% by the 21st day.1
Here, the infant was term and healthy, but we are not told some important details. Was she breast fed or bottle fed? Was she born by cesarean section or vaginally? We do know she was discharged on August 24th, her mother called the hotline on the 25th, and she was seen by the pediatrician on the 26th—at which point the infant had not stooled in 3 days. The mother called the physician’s office again on August 29th and was sent to the ED. We are told only that each feeding lasted an hour and the infant hadn’t stooled.
Continue to: Regarding stool...
Regarding stool—we have all had discussions with patients regarding hypervigilant concerns about stool color. We know there are some big things to look for with stool color (eg, black tarry reveals upper GI bleeding, while clay-colored or pale may reveal the absence of bile). Yet, patients’ expectations of the color-coded diagnostic abilities of their stool knows no bounds. Patients are convinced that we have some color wheel in our jacket pocket corresponding to stool color—and that the nuances between shades have important medical implications. If you ask, “Would you say it is more marigold, butterscotch yellow, or Tuscan sun?” … your patient will have an answer.
Patients reveal stool color hesitantly, reservedly, with nervous expectation. They wait for your response in quivering anticipation that the coming reply will include words to the effect that a boysenberry-purple stool is equivalent to a Death tarot card. A subconjunctival hemorrhage is the only thing that approaches the anxiety level of the oddly hued stool (Oddly Hued Stool Anxiety). Woe be the patient with both. For a patient bearing a subconjunctival hemorrhage who has also passed a jungle-green stool in the past 24 hours fully expects to explode within the next 60 minutes.
I’ve been rather facetious for a reason. My purpose is to acknowledge and to help you recognize that most discussions regarding stooling will not be (forgive me) productive. They are not productive because most stool coloration issues are nonentities—yet they produce patient anxiety that takes some time to address, leaving a busy clinician prone to curtly dismiss such discussions out of hand. Because many patient-initiated stool discussions aren’t productive, there is the risk for stool tune-out. As gross and unproductive as they can be, don’t tune out all stool discussions.
In this case, the appropriate frequency of stooling should have been at least once per day. For newborns, a stool color question is helpful; stool should not be white, pale, or clay-colored, which is suggestive of acholic stools from biliary atresia. Here, despite the absence of stool over a 3-day period, the defendant concluded the feeding problem was resolved and set a return visit for 2 weeks later. The plaintiff’s expert contended that the weight loss and absence of stooling was evidence of inadequate intake and warranted a return check the next day. Rather than risk the case going to trial, the defendant settled for $1,375,000.
IN SUM
Newborn nutrition is important. Understand that parents will be anxious about newborn feeding, although often there is no major medical concern. However, do not be dismissive of feeding concerns because of this expected anxiety. Listen to the parents fully, paying particular attention to quantifying feeding difficulty and stooling frequency matters. Don’t let patients’ rainbow parade of needless stool concerns blind you to considering important information. In other words, don’t be a stool fool.
1. McKee-Garrett TM. Overview of the routine management of the healthy newborn infant. UpToDate. Updated July 12, 2019. www.uptodate.com/contents/overview-of-the-routine-management-of-the-healthy-newborn-infant. Accessed November 18, 2019.
2. Sood MR. Constipation in infants and children: evaluation. UpToDate. Updated August 1, 2019. www.uptodate.com/contents/constipation-in-infants-and-children-evaluation. Accessed November 18, 2019.
1. McKee-Garrett TM. Overview of the routine management of the healthy newborn infant. UpToDate. Updated July 12, 2019. www.uptodate.com/contents/overview-of-the-routine-management-of-the-healthy-newborn-infant. Accessed November 18, 2019.
2. Sood MR. Constipation in infants and children: evaluation. UpToDate. Updated August 1, 2019. www.uptodate.com/contents/constipation-in-infants-and-children-evaluation. Accessed November 18, 2019.
Stay Informed About Informed Consent
On May 24, 2011, a 53-year-old woman presented to a Wisconsin hospital emergency department (ED) with complaints of severe abdominal pain, a rapid heartbeat, and a fever of 101.3°F. During her 9-hour visit, she was treated by a PA and his supervising physician. She was seen by the physician for a total of 6 minutes; the rest of her care was provided by the PA. The patient was discharged around midnight with instructions to contact her gynecologist in the morning for management of uterine fibroids. At the time of discharge, her temperature was 102.9°F.
The following day, May 25, the patient collapsed in her home and was transported to another hospital. She was treated for septic shock from a group A streptococcus infection. Although the infection was halted, the patient sustained ischemic damage to her extremities and a month later required amputation of her 4 limbs.The plaintiff claimed that the supervising physician was negligent in failing to diagnose the strep A infection, which, left undetected, led to septic shock. She also alleged that the PA should have recognized the potential for her condition’s severity to quickly escalate. She maintained that the supervising physician should have been more involved in her case because of its complexity.
Plaintiff’s counsel also argued that the PA should have provided “alternative medical diagnoses,” which would have prompted consideration of other treatment options. The plaintiff contended that under Wisconsin’s informed consent law, both the PA and the physician failed to disclose enough information about her condition and failed to inform her of any choices for treatment.
The defense argued that the plaintiff received proper treatment based on the information available to the providers at the time.
VERDICT
The jury found for the plaintiff and apportioned 65% liability to the physician and 35% liability to the PA. A total of $25,342,096 was awarded to the plaintiff.
COMMENTARY
This is a huge verdict. Cases involving group A strep or necrotizing fasciitis frequently give rise to large medical malpractice verdicts, because everything about them is difficult to defend: Although there is typically trivial to no trauma involved, the wounds from these infections provide explicit images of damage, intraoperatively and postoperatively. Vasopressors required for hemodynamic support or sepsis itself frequently result in limb ischemia, gangrene, and amputation. In this case, the plaintiff, as a quadruple amputee, was a sympathetic and impressive courtroom presence—the personal toll was evident to anyone in the room.
Two providers—a PA and a physician—saw the patient. We are told only that she complained of severe abdominal pain, rapid heartbeat, and fever, which increased at some point during her ED stay. We aren’t given specifics on the rest of the patient’s vital signs or examination details. However, we can infer that the exam and lab findings were not impressive, because they weren’t mentioned in the case report. But as a result of the failure to catch the group A strep infection, the plaintiff suffered what one judge hearing the case described as a harrowing and unimaginable ordeal: the life-changing amputation of 4 limbs.1 While the jury did not find the PA or physician negligent, they still found the clinicians liable and awarded a staggering verdict.
Continue to: How could this happen?
How could this happen? The answer is the theory of recovery: The jury found that the physician and the PA failed to provide the patient with informed consent in the form of “alternative medical diagnoses.”2 The plaintiff’s attorney argued that the patient was never told a life-threatening bacterial infection was one possible diagnosis and claimed that if she had known, the patient would have pursued other treatment.
As in many malpractice cases, the plaintiff alleged failure to diagnose and failure to provide informed consent. Depending on state law, there are 3 standards for informed consent: subjective patient, reasonable patient, and reasonable physician.3 About half of the states have a physician-focused standard, while the other half have a patient-focused standard.3
Under the subjective patient standard, we would ask, “What would this patient need to know and understand to make an informed decision?”4 The subjective standard requires the clinician to essentially “get in the head” of a specific patient to determine what he or she would want to know when making a medical decision. This standard is problematic because it requires the clinician to have an intimate familiarity with the patient’s belief system and medical decision-making process—a daunting requirement for many clinicians, particularly in the absence of a longstanding clinician-patient relationship, as is the case in most emergency settings. Thankfully, the subjective patient standard is not followed by most states that have a patient-focused standard.
Under the objective reasonable patient standard, we would ask “What would the average patient need to know to be an informed participant in the decision?”4 One could argue that this standard more adequately allows the patient to be an active participant in shared decision-making. However, the drawback is that what is “reasonable” often falls on a spectrum, which would require the clinician to gauge the volume and type of information a patient cohort would want to have when making a medical decision. Under this standard, the plaintiff must prove that the clinician omitted information that a reasonable patient would want to know. Therefore, these standards are more friendly to the plaintiff, whereas the reasonable physician standard is more defendant friendly.
To meet the standard of care under a reasonable physician standard, information must be provided to the patient that a “reasonably prudent practitioner in the same field of practice or specialty” would provide to a patient.5 For a plaintiff to successfully sue under this standard, the plaintiff’s expert must testify that a reasonably prudent physician would have disclosed the omitted information.6 The reasonable physician standard is obviously better for malpractice defendants.
Continue to: While reasonable clinicians...
While reasonable clinicians can disagree (as can reasonable patients), clinicians are more likely to be closer in opinion. Clinicians are a smaller group whose opinions are underpinned by similar education, training, and experience. By contrast, among the general population, beliefs held by one hypothetical “reasonable person” are much less settled, and in some cases, wildly divergent from another’s. For example, vaccine skepticism would probably be considered unreasonable in the majority of jury pools but absolutely reasonable in some. The large size of the general population, coupled with opinions untethered to any definable discipline, make the reasonable patient standard hard to predict.
Additionally, the reasonable physician standard forces the plaintiff to prove his or her case by producing an expert witness (clinician) to specifically testify that the standard of care required the defendant clinician to disclose certain specific information, and that disclosure was lacking. That is an important requirement. Under patient-focused standards, the plaintiff doesn’t need a medical expert on this point and can simply argue to the jury that a reasonable patient would require an exhaustive discussion of each possibility in the differential diagnosis. Therefore, I would argue that the reasonable physician standard is more predictable and workable and should be followed.
At the time of this case, Wisconsin’s informed consent law was based on the reasonable patient standard. As a result of this case, Wisconsin lawmakers changed the law to a “reasonable physician standard,” which states “any physician who treats a patient shall inform the patient about the availability of reasonable alternate medical modes of treatment and about the benefits and risks of these treatments.”7 However, the law stipulates that this duty to inform does not require disclosure of (among others):
- Detailed technical information that in all probability a patient would not understand
- Risks apparent or known to the patient
- Extremely remote possibilities that might falsely or detrimentally alarm the patient
- Information about alternate medical modes of treatment for any condition the physician has not included in his or her diagnosis at the time the physician informs the patient.7
Finally, this case involved an extremely high verdict of more than $25 million. It may surprise you to learn that many states have caps for medical malpractice awards for noneconomic damages, such as pain and suffering. If you’re having a holiday dinner with friends or family members who are plaintiff’s attorneys and you’re itching for a good argument, skip current politics and go all-in: How about liability caps, Uncle Jim? Get ready for a lively debate.
Of the $25 million verdict, $16.5 million was awarded for pain and suffering—the jury was obviously shocked by the extent of the life-changing nature of the plaintiff’s injuries. At the time of this case, Wisconsin had a cap of $750,000 for noneconomic damages.8 However, plaintiffs may challenge state constitutionality of these caps when they feel they have the right case, which the plaintiff and her attorney felt they did. Two lower courts found the state cap unconstitutional and gave the plaintiff the full award. But the state Supreme Court later reversed that decision, upholding the cap.1 The court decided that the legislature had a rational basis for making the law and changes to it should occur through the legislature, not the courts. The dissenting justices argued that there was no rational basis for the $750,000 cap, because there was no evidence that clinicians would flee the state fearing malpractice liability, or practice more defensive medicine, or suffer runaway malpractice insurance premiums without the cap. As a result of this case, the cap was upheld, and there was a “lively debate” on this issue at the highest levels of government.
Continue to: IN SUM
IN SUM
Become familiar with your state’s informed consent laws. Involve patients in decision-making, and convey information related to reasonable treatment options and risks. Document all of these discussions. Lastly, state-level political discussions on issues of tort reform, caps, and malpractice matters are ongoing—so take n
1. Mayo v Wisconsin Injured Patients & Families Compensation Fund. WI 78 (2018).
2. Spivak C. Jury awards Milwaukee woman $25.3 million in medical malpractice case. Milwaukee Journal Sentinel. July 7, 2014.
3. Moore GP, Matlock AG, Kiley JL, et al. Emergency physicians: beware of the consent standard of care. Clin Pract Cases Emerg Med. 2018; 2(2):109-111.
4. Gossman W, Thornton I, Hipskind JE. Informed Consent. StatPearls. www.ncbi.nlm.nih.gov/books/NBK430827/. Updated July 10, 2019. Accessed October 25, 2019.
5. King JS, Moulton BW. Rethinking informed consent: the case for shared medical decision-making. Am J Law Med. 2006;32:429-501.
6. Tashman v Gibbs, 556 SE 2d 772 (263 Va 2002).
7. Wis Stat subchapter 2, §448.30.
8. Wis Stat §893.55.
On May 24, 2011, a 53-year-old woman presented to a Wisconsin hospital emergency department (ED) with complaints of severe abdominal pain, a rapid heartbeat, and a fever of 101.3°F. During her 9-hour visit, she was treated by a PA and his supervising physician. She was seen by the physician for a total of 6 minutes; the rest of her care was provided by the PA. The patient was discharged around midnight with instructions to contact her gynecologist in the morning for management of uterine fibroids. At the time of discharge, her temperature was 102.9°F.
The following day, May 25, the patient collapsed in her home and was transported to another hospital. She was treated for septic shock from a group A streptococcus infection. Although the infection was halted, the patient sustained ischemic damage to her extremities and a month later required amputation of her 4 limbs.The plaintiff claimed that the supervising physician was negligent in failing to diagnose the strep A infection, which, left undetected, led to septic shock. She also alleged that the PA should have recognized the potential for her condition’s severity to quickly escalate. She maintained that the supervising physician should have been more involved in her case because of its complexity.
Plaintiff’s counsel also argued that the PA should have provided “alternative medical diagnoses,” which would have prompted consideration of other treatment options. The plaintiff contended that under Wisconsin’s informed consent law, both the PA and the physician failed to disclose enough information about her condition and failed to inform her of any choices for treatment.
The defense argued that the plaintiff received proper treatment based on the information available to the providers at the time.
VERDICT
The jury found for the plaintiff and apportioned 65% liability to the physician and 35% liability to the PA. A total of $25,342,096 was awarded to the plaintiff.
COMMENTARY
This is a huge verdict. Cases involving group A strep or necrotizing fasciitis frequently give rise to large medical malpractice verdicts, because everything about them is difficult to defend: Although there is typically trivial to no trauma involved, the wounds from these infections provide explicit images of damage, intraoperatively and postoperatively. Vasopressors required for hemodynamic support or sepsis itself frequently result in limb ischemia, gangrene, and amputation. In this case, the plaintiff, as a quadruple amputee, was a sympathetic and impressive courtroom presence—the personal toll was evident to anyone in the room.
Two providers—a PA and a physician—saw the patient. We are told only that she complained of severe abdominal pain, rapid heartbeat, and fever, which increased at some point during her ED stay. We aren’t given specifics on the rest of the patient’s vital signs or examination details. However, we can infer that the exam and lab findings were not impressive, because they weren’t mentioned in the case report. But as a result of the failure to catch the group A strep infection, the plaintiff suffered what one judge hearing the case described as a harrowing and unimaginable ordeal: the life-changing amputation of 4 limbs.1 While the jury did not find the PA or physician negligent, they still found the clinicians liable and awarded a staggering verdict.
Continue to: How could this happen?
How could this happen? The answer is the theory of recovery: The jury found that the physician and the PA failed to provide the patient with informed consent in the form of “alternative medical diagnoses.”2 The plaintiff’s attorney argued that the patient was never told a life-threatening bacterial infection was one possible diagnosis and claimed that if she had known, the patient would have pursued other treatment.
As in many malpractice cases, the plaintiff alleged failure to diagnose and failure to provide informed consent. Depending on state law, there are 3 standards for informed consent: subjective patient, reasonable patient, and reasonable physician.3 About half of the states have a physician-focused standard, while the other half have a patient-focused standard.3
Under the subjective patient standard, we would ask, “What would this patient need to know and understand to make an informed decision?”4 The subjective standard requires the clinician to essentially “get in the head” of a specific patient to determine what he or she would want to know when making a medical decision. This standard is problematic because it requires the clinician to have an intimate familiarity with the patient’s belief system and medical decision-making process—a daunting requirement for many clinicians, particularly in the absence of a longstanding clinician-patient relationship, as is the case in most emergency settings. Thankfully, the subjective patient standard is not followed by most states that have a patient-focused standard.
Under the objective reasonable patient standard, we would ask “What would the average patient need to know to be an informed participant in the decision?”4 One could argue that this standard more adequately allows the patient to be an active participant in shared decision-making. However, the drawback is that what is “reasonable” often falls on a spectrum, which would require the clinician to gauge the volume and type of information a patient cohort would want to have when making a medical decision. Under this standard, the plaintiff must prove that the clinician omitted information that a reasonable patient would want to know. Therefore, these standards are more friendly to the plaintiff, whereas the reasonable physician standard is more defendant friendly.
To meet the standard of care under a reasonable physician standard, information must be provided to the patient that a “reasonably prudent practitioner in the same field of practice or specialty” would provide to a patient.5 For a plaintiff to successfully sue under this standard, the plaintiff’s expert must testify that a reasonably prudent physician would have disclosed the omitted information.6 The reasonable physician standard is obviously better for malpractice defendants.
Continue to: While reasonable clinicians...
While reasonable clinicians can disagree (as can reasonable patients), clinicians are more likely to be closer in opinion. Clinicians are a smaller group whose opinions are underpinned by similar education, training, and experience. By contrast, among the general population, beliefs held by one hypothetical “reasonable person” are much less settled, and in some cases, wildly divergent from another’s. For example, vaccine skepticism would probably be considered unreasonable in the majority of jury pools but absolutely reasonable in some. The large size of the general population, coupled with opinions untethered to any definable discipline, make the reasonable patient standard hard to predict.
Additionally, the reasonable physician standard forces the plaintiff to prove his or her case by producing an expert witness (clinician) to specifically testify that the standard of care required the defendant clinician to disclose certain specific information, and that disclosure was lacking. That is an important requirement. Under patient-focused standards, the plaintiff doesn’t need a medical expert on this point and can simply argue to the jury that a reasonable patient would require an exhaustive discussion of each possibility in the differential diagnosis. Therefore, I would argue that the reasonable physician standard is more predictable and workable and should be followed.
At the time of this case, Wisconsin’s informed consent law was based on the reasonable patient standard. As a result of this case, Wisconsin lawmakers changed the law to a “reasonable physician standard,” which states “any physician who treats a patient shall inform the patient about the availability of reasonable alternate medical modes of treatment and about the benefits and risks of these treatments.”7 However, the law stipulates that this duty to inform does not require disclosure of (among others):
- Detailed technical information that in all probability a patient would not understand
- Risks apparent or known to the patient
- Extremely remote possibilities that might falsely or detrimentally alarm the patient
- Information about alternate medical modes of treatment for any condition the physician has not included in his or her diagnosis at the time the physician informs the patient.7
Finally, this case involved an extremely high verdict of more than $25 million. It may surprise you to learn that many states have caps for medical malpractice awards for noneconomic damages, such as pain and suffering. If you’re having a holiday dinner with friends or family members who are plaintiff’s attorneys and you’re itching for a good argument, skip current politics and go all-in: How about liability caps, Uncle Jim? Get ready for a lively debate.
Of the $25 million verdict, $16.5 million was awarded for pain and suffering—the jury was obviously shocked by the extent of the life-changing nature of the plaintiff’s injuries. At the time of this case, Wisconsin had a cap of $750,000 for noneconomic damages.8 However, plaintiffs may challenge state constitutionality of these caps when they feel they have the right case, which the plaintiff and her attorney felt they did. Two lower courts found the state cap unconstitutional and gave the plaintiff the full award. But the state Supreme Court later reversed that decision, upholding the cap.1 The court decided that the legislature had a rational basis for making the law and changes to it should occur through the legislature, not the courts. The dissenting justices argued that there was no rational basis for the $750,000 cap, because there was no evidence that clinicians would flee the state fearing malpractice liability, or practice more defensive medicine, or suffer runaway malpractice insurance premiums without the cap. As a result of this case, the cap was upheld, and there was a “lively debate” on this issue at the highest levels of government.
Continue to: IN SUM
IN SUM
Become familiar with your state’s informed consent laws. Involve patients in decision-making, and convey information related to reasonable treatment options and risks. Document all of these discussions. Lastly, state-level political discussions on issues of tort reform, caps, and malpractice matters are ongoing—so take n
On May 24, 2011, a 53-year-old woman presented to a Wisconsin hospital emergency department (ED) with complaints of severe abdominal pain, a rapid heartbeat, and a fever of 101.3°F. During her 9-hour visit, she was treated by a PA and his supervising physician. She was seen by the physician for a total of 6 minutes; the rest of her care was provided by the PA. The patient was discharged around midnight with instructions to contact her gynecologist in the morning for management of uterine fibroids. At the time of discharge, her temperature was 102.9°F.
The following day, May 25, the patient collapsed in her home and was transported to another hospital. She was treated for septic shock from a group A streptococcus infection. Although the infection was halted, the patient sustained ischemic damage to her extremities and a month later required amputation of her 4 limbs.The plaintiff claimed that the supervising physician was negligent in failing to diagnose the strep A infection, which, left undetected, led to septic shock. She also alleged that the PA should have recognized the potential for her condition’s severity to quickly escalate. She maintained that the supervising physician should have been more involved in her case because of its complexity.
Plaintiff’s counsel also argued that the PA should have provided “alternative medical diagnoses,” which would have prompted consideration of other treatment options. The plaintiff contended that under Wisconsin’s informed consent law, both the PA and the physician failed to disclose enough information about her condition and failed to inform her of any choices for treatment.
The defense argued that the plaintiff received proper treatment based on the information available to the providers at the time.
VERDICT
The jury found for the plaintiff and apportioned 65% liability to the physician and 35% liability to the PA. A total of $25,342,096 was awarded to the plaintiff.
COMMENTARY
This is a huge verdict. Cases involving group A strep or necrotizing fasciitis frequently give rise to large medical malpractice verdicts, because everything about them is difficult to defend: Although there is typically trivial to no trauma involved, the wounds from these infections provide explicit images of damage, intraoperatively and postoperatively. Vasopressors required for hemodynamic support or sepsis itself frequently result in limb ischemia, gangrene, and amputation. In this case, the plaintiff, as a quadruple amputee, was a sympathetic and impressive courtroom presence—the personal toll was evident to anyone in the room.
Two providers—a PA and a physician—saw the patient. We are told only that she complained of severe abdominal pain, rapid heartbeat, and fever, which increased at some point during her ED stay. We aren’t given specifics on the rest of the patient’s vital signs or examination details. However, we can infer that the exam and lab findings were not impressive, because they weren’t mentioned in the case report. But as a result of the failure to catch the group A strep infection, the plaintiff suffered what one judge hearing the case described as a harrowing and unimaginable ordeal: the life-changing amputation of 4 limbs.1 While the jury did not find the PA or physician negligent, they still found the clinicians liable and awarded a staggering verdict.
Continue to: How could this happen?
How could this happen? The answer is the theory of recovery: The jury found that the physician and the PA failed to provide the patient with informed consent in the form of “alternative medical diagnoses.”2 The plaintiff’s attorney argued that the patient was never told a life-threatening bacterial infection was one possible diagnosis and claimed that if she had known, the patient would have pursued other treatment.
As in many malpractice cases, the plaintiff alleged failure to diagnose and failure to provide informed consent. Depending on state law, there are 3 standards for informed consent: subjective patient, reasonable patient, and reasonable physician.3 About half of the states have a physician-focused standard, while the other half have a patient-focused standard.3
Under the subjective patient standard, we would ask, “What would this patient need to know and understand to make an informed decision?”4 The subjective standard requires the clinician to essentially “get in the head” of a specific patient to determine what he or she would want to know when making a medical decision. This standard is problematic because it requires the clinician to have an intimate familiarity with the patient’s belief system and medical decision-making process—a daunting requirement for many clinicians, particularly in the absence of a longstanding clinician-patient relationship, as is the case in most emergency settings. Thankfully, the subjective patient standard is not followed by most states that have a patient-focused standard.
Under the objective reasonable patient standard, we would ask “What would the average patient need to know to be an informed participant in the decision?”4 One could argue that this standard more adequately allows the patient to be an active participant in shared decision-making. However, the drawback is that what is “reasonable” often falls on a spectrum, which would require the clinician to gauge the volume and type of information a patient cohort would want to have when making a medical decision. Under this standard, the plaintiff must prove that the clinician omitted information that a reasonable patient would want to know. Therefore, these standards are more friendly to the plaintiff, whereas the reasonable physician standard is more defendant friendly.
To meet the standard of care under a reasonable physician standard, information must be provided to the patient that a “reasonably prudent practitioner in the same field of practice or specialty” would provide to a patient.5 For a plaintiff to successfully sue under this standard, the plaintiff’s expert must testify that a reasonably prudent physician would have disclosed the omitted information.6 The reasonable physician standard is obviously better for malpractice defendants.
Continue to: While reasonable clinicians...
While reasonable clinicians can disagree (as can reasonable patients), clinicians are more likely to be closer in opinion. Clinicians are a smaller group whose opinions are underpinned by similar education, training, and experience. By contrast, among the general population, beliefs held by one hypothetical “reasonable person” are much less settled, and in some cases, wildly divergent from another’s. For example, vaccine skepticism would probably be considered unreasonable in the majority of jury pools but absolutely reasonable in some. The large size of the general population, coupled with opinions untethered to any definable discipline, make the reasonable patient standard hard to predict.
Additionally, the reasonable physician standard forces the plaintiff to prove his or her case by producing an expert witness (clinician) to specifically testify that the standard of care required the defendant clinician to disclose certain specific information, and that disclosure was lacking. That is an important requirement. Under patient-focused standards, the plaintiff doesn’t need a medical expert on this point and can simply argue to the jury that a reasonable patient would require an exhaustive discussion of each possibility in the differential diagnosis. Therefore, I would argue that the reasonable physician standard is more predictable and workable and should be followed.
At the time of this case, Wisconsin’s informed consent law was based on the reasonable patient standard. As a result of this case, Wisconsin lawmakers changed the law to a “reasonable physician standard,” which states “any physician who treats a patient shall inform the patient about the availability of reasonable alternate medical modes of treatment and about the benefits and risks of these treatments.”7 However, the law stipulates that this duty to inform does not require disclosure of (among others):
- Detailed technical information that in all probability a patient would not understand
- Risks apparent or known to the patient
- Extremely remote possibilities that might falsely or detrimentally alarm the patient
- Information about alternate medical modes of treatment for any condition the physician has not included in his or her diagnosis at the time the physician informs the patient.7
Finally, this case involved an extremely high verdict of more than $25 million. It may surprise you to learn that many states have caps for medical malpractice awards for noneconomic damages, such as pain and suffering. If you’re having a holiday dinner with friends or family members who are plaintiff’s attorneys and you’re itching for a good argument, skip current politics and go all-in: How about liability caps, Uncle Jim? Get ready for a lively debate.
Of the $25 million verdict, $16.5 million was awarded for pain and suffering—the jury was obviously shocked by the extent of the life-changing nature of the plaintiff’s injuries. At the time of this case, Wisconsin had a cap of $750,000 for noneconomic damages.8 However, plaintiffs may challenge state constitutionality of these caps when they feel they have the right case, which the plaintiff and her attorney felt they did. Two lower courts found the state cap unconstitutional and gave the plaintiff the full award. But the state Supreme Court later reversed that decision, upholding the cap.1 The court decided that the legislature had a rational basis for making the law and changes to it should occur through the legislature, not the courts. The dissenting justices argued that there was no rational basis for the $750,000 cap, because there was no evidence that clinicians would flee the state fearing malpractice liability, or practice more defensive medicine, or suffer runaway malpractice insurance premiums without the cap. As a result of this case, the cap was upheld, and there was a “lively debate” on this issue at the highest levels of government.
Continue to: IN SUM
IN SUM
Become familiar with your state’s informed consent laws. Involve patients in decision-making, and convey information related to reasonable treatment options and risks. Document all of these discussions. Lastly, state-level political discussions on issues of tort reform, caps, and malpractice matters are ongoing—so take n
1. Mayo v Wisconsin Injured Patients & Families Compensation Fund. WI 78 (2018).
2. Spivak C. Jury awards Milwaukee woman $25.3 million in medical malpractice case. Milwaukee Journal Sentinel. July 7, 2014.
3. Moore GP, Matlock AG, Kiley JL, et al. Emergency physicians: beware of the consent standard of care. Clin Pract Cases Emerg Med. 2018; 2(2):109-111.
4. Gossman W, Thornton I, Hipskind JE. Informed Consent. StatPearls. www.ncbi.nlm.nih.gov/books/NBK430827/. Updated July 10, 2019. Accessed October 25, 2019.
5. King JS, Moulton BW. Rethinking informed consent: the case for shared medical decision-making. Am J Law Med. 2006;32:429-501.
6. Tashman v Gibbs, 556 SE 2d 772 (263 Va 2002).
7. Wis Stat subchapter 2, §448.30.
8. Wis Stat §893.55.
1. Mayo v Wisconsin Injured Patients & Families Compensation Fund. WI 78 (2018).
2. Spivak C. Jury awards Milwaukee woman $25.3 million in medical malpractice case. Milwaukee Journal Sentinel. July 7, 2014.
3. Moore GP, Matlock AG, Kiley JL, et al. Emergency physicians: beware of the consent standard of care. Clin Pract Cases Emerg Med. 2018; 2(2):109-111.
4. Gossman W, Thornton I, Hipskind JE. Informed Consent. StatPearls. www.ncbi.nlm.nih.gov/books/NBK430827/. Updated July 10, 2019. Accessed October 25, 2019.
5. King JS, Moulton BW. Rethinking informed consent: the case for shared medical decision-making. Am J Law Med. 2006;32:429-501.
6. Tashman v Gibbs, 556 SE 2d 772 (263 Va 2002).
7. Wis Stat subchapter 2, §448.30.
8. Wis Stat §893.55.
Don’t Take the Fall With Head Injuries
In the early morning hours of June 10, 2009, a 77-year-old man who had been undergoing chemotherapy for multiple myeloma took sleep medication. He then fell down a flight of stairs in his split-level home.
The patient sustained a laceration to his scalp but returned to bed and waited until later that morning to call his internist for an appointment. Later that day, the physician placed 11 sutures for the scalp laceration and performed a neurologic examination; he did not note any abnormalities. The patient complained of back pain, so the physician ordered a back x-ray, which revealed a TI2 fracture that had occurred from the fall. No further treatment was provided for the scalp injury, except removal of the stitches about a week later.
Six days after the fall and doctor visit, the patient’s condition began to deteriorate rapidly, with noted slurred speech and loss of consciousness. He was transported to an emergency department, where CT revealed a massive subdural hematoma. An immediate craniotomy was performed. However, on June 27, 2009, the patient died as a result of the brain bleed.
His estate filed suit against the physician and his practice, alleging medical malpractice and violations in the standard of care. The estate alleged that the standard of care required the physician to obtain a CT scan and that, had one been performed, it would have revealed a small subdural hematoma in time for it to have been successfully treated (ie, before the massive second related bleed). The estate’s theory of the case did not rest on the presentation of clinical symptoms. A medical expert who testified for the estate stated that the subdural hematoma began at the time of the fall.
The defense denied any violations in the standard of care. The physician contended that the patient had presented with no symptoms other than a head laceration, and there were no criteria for ordering CT. Further, the defense asserted that the patient was symptom free for 6 days post-fall. According to the defense, the patient experienced a sudden arterial bleed that was not caused by the fall and would not have been revealed on CT ordered at the time of initial presentation, because it did not occur until 6 days later.
VERDICT
After a 10-day trial and 25 minutes’ deliberation, the jury returned a defense verdict.
COMMENTARY
The 25-minute deliberation suggests that terms such as “bridging veins” and “shearing injury” were unlikely bandied about in the jury room. The jury was likely dismissive of the plaintiff’s claim owing to his cancer diagnosis, and perhaps rightly so. But if we eliminate the multiple myeloma diagnosis, the jury might have decided differently.
Continue to: The defendant physician...
The defendant physician did a good job of documenting a negative neurologic exam, which helped him convince the jury that the patient did not have any signs or symptoms when first evaluated. But in this patient, was imaging to rule out intracranial bleeding indicated?
As an oversimplification, we tend to think of intracranial hemorrhage in 2 varieties: the insidious and the bold. Subdural hematomas are stealthy, they are sneaky, and they prey on the old. They step out of the shadows to cause symptoms. They are the ninjas of intracranial hemorrhage. Beware.
Epidural hematomas and subarachnoid hemorrhage (SAH) are the opposite. They classically present with a sudden and severe symptom complex: with epidural hematoma, the loss of consciousness, lucid interval, and final loss of consciousness; with SAH, the “worst in your life” thunder-clap headache, which may be heralded by a sentinel headache.1 When manifesting this way, they are brash, direct, and unsubtle to the point of being obnoxious—the Steven Stifler of intracranial bleeding.
This generalization is made to highlight the potentially sneaky nature of subdural hemorrhage. There are circumstances in which the clinical presentation of epidural hematoma and SAH will be more challenging. The question here is whether a negative initial neurologic exam can adequately screen for a potentially stealthy subdural hematoma.
Subdural hemorrhage is caused by rapidly changing velocity that may stretch and tear small bridging veins.2,3 Subdural hematoma is more common in the elderly, those who abuse alcohol, and those with a prior history of head trauma.4 As the brain shrinks with age or atrophy, the subdural space enlarges and traversing veins are stretched to cover a wider distance—rendering them vulnerable to rupture.5 These structures may also weaken as a result of low cerebrospinal fluid (intracranial hypotension); as pressure decreases (eg, from a leak), the brain’s buoyancy is reduced, causing traction on anchoring and supporting structures (eg, bridging veins).5 Injury to bridging veins can even occur as a result of a coup-contrecoup mechanism in the absence of direct physical impact.6,7 Bottom line: the injury itself may be subtle, requiring an index of suspicion to make the diagnosis.
Continue to: The case patient was...
The case patient was elderly. He had a chronic malignancy and sustained a fall down the stairs. He was taking sleeping pills, which may have slowed reflexive protective mechanisms after he started to fall (resulting in greater force imparted to his head). Multiple myeloma can predispose a patient to coagulopathy, and we don’t know in this case if this patient’s multiple myeloma made him more susceptible to bleeding—but it certainly didn’t help.8 The patient’s age, the mechanism of injury, and the history of malignancy made this a setup for hemorrhage.
Interestingly, we are not given details about how the patient looked during his suture removal. We are told the time between the initial fall and deterioration was 6 days. Scalp sutures were removed “about a week later,” which was after the deterioration—so this can’t be correct. Removing scalp sutures after 5 days seems premature, but that is the only possibility if 6 days elapsed between the fall and the deterioration.
In short, these are difficult cases. If intracranial bleeding can be subtle and delayed, how can we be sure a patient is not experiencing a bleed? We can only apply the relevant standard of care using all the clinical information we have. The Canadian CT Head Rule and New Orleans Criteria are clinical tools designed to help providers determine when to image (see Table for details).9
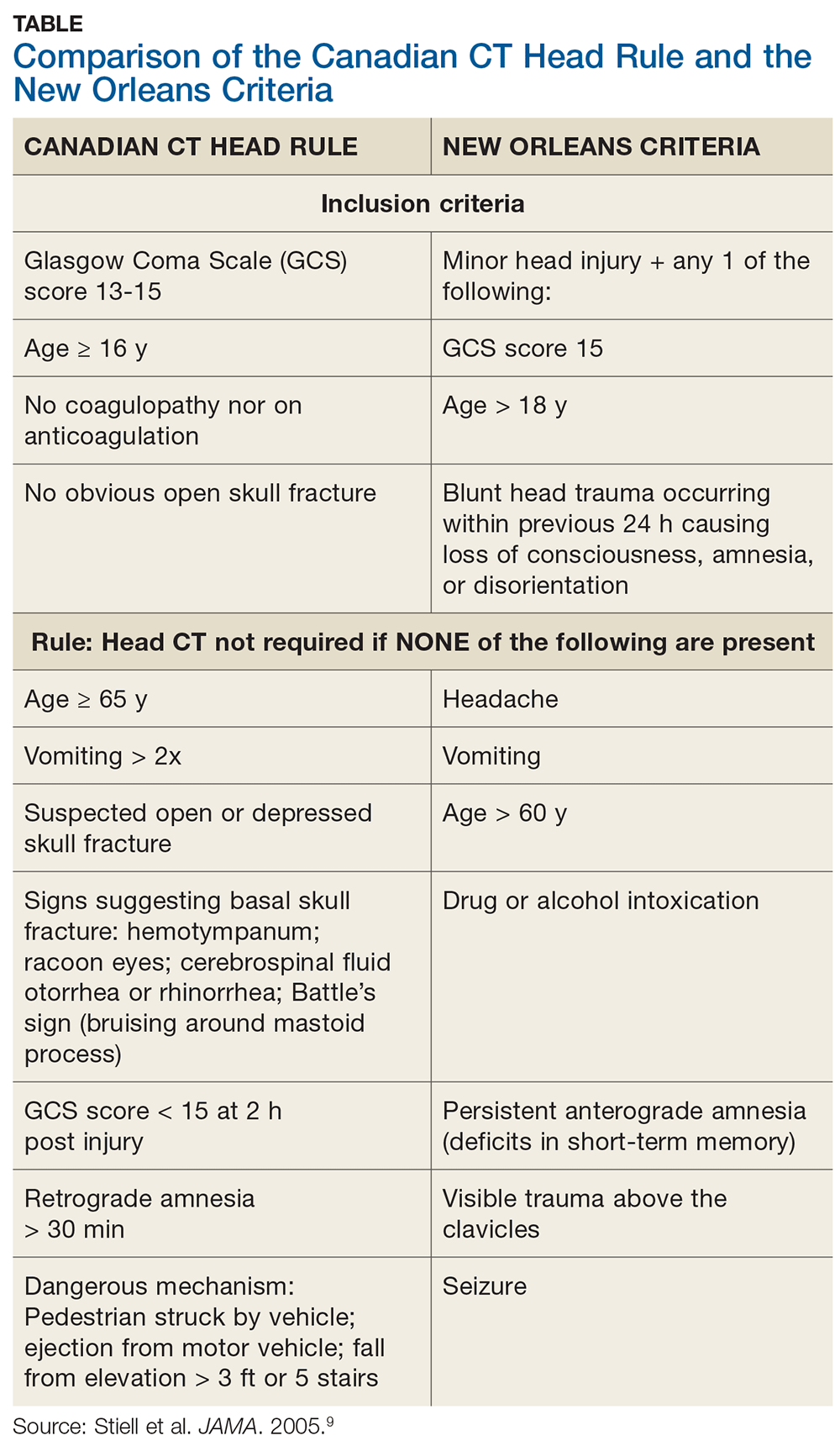
Applying the Canadian CT Head Rule to the facts of this case, we would image the patient because he fell down a “flight” of stairs (which is > 5 stairs) and he is 77 years old (older than 65). The New Orleans Criteria require head CT for minor injury with any positive findings.9 Because the patient is older than 60, he would be scanned according this rule.
In this case, the tools indicate scanning would have been appropriate. The patient’s multiple myeloma might have further impelled a decision to image. However, the jury was persuaded that the defendant’s negative neurologic exam was reasonable under the circumstances. This was likely made possible by the physician’s good recordkeeping and demonstrated genuine concern for the patient’s well-being—as well as a differing viewpoint of the patient’s age and health status.
Continue to: Finally, a word about...
Finally, a word about falls and the elderly: We’ve all heard the 80s advertising catchphrase (which lives on as a present-day meme) “I’ve fallen, and I can’t get up!” The problem is, many don’t. It would be more clinically accurate to say, “I’ve fallen, and I’ll be hospitalized for an extended period of time, then transferred to a skilled nursing facility, but I won’t survive to discharge.” The reality is that falls kill, and the severity is underestimated.10 If it were a “brain-eating amoeba,” the media would be all over it. With falls, not so much. We tend to pay less attention.
Risk factors for a fall include postural hypotension; use of benzodiazepines or other sedative-hypnotic drugs; use of ≥ 4 medications; environmental hazards for tripping; impairment in balance and transfer skills; and gait impairment.11 Home setup also contributes—loose throw rugs, uneven carpet edges, cracked sidewalks, clutter and furniture, cables and wires and cords, oh my.
Do your older patients a favor by reinforcing fall risk. Instruct them to rise slowly from seated or recumbent positions; always consider central nervous system sedation and/or the coordination-hampering properties of medications, particularly in combination. Raise the issue of home safety. A brief 10-second comment from you may plant a seed in a family member’s head to do what you cannot: scan and make safe the patient’s living environment.
1. de Falco FA. Sentinel headache. Neurol Sci. 2004;25(suppl 3):S215-S217.
2. Miller JD, Nader R. Acute subdural hematoma from bridging vein rupture: a potential mechanism for growth. J Neurosurg. 2014;120(6):1378-1384.
3. Victor M, Ropper A. Craniocerebral trauma. In: Victor M, Ropper A, eds. Adams and Victor’s Principles of Neurology. 7th ed. New York, NY: McGraw-Hill; 2001:925.
4. McBridde W. Subdural hematoma in adults: etiology, clinical features, and diagnosis. UpToDate website. www.uptodate.com/contents/subdural-hematoma-in-adults-etiology-clinical-features-and-diagnosis? search=subdural%20hematoma. Published December 10, 2018. Accessed September 23, 2019.
5. US National Library of Medicine. Subdural hematoma. Medline Plus website. https://medlineplus.gov/ency/article/000713.htm. Accessed September 23, 2019.
6. Besenski N. Traumatic injuries: imaging of head injuries. Eur Radiol. 2002;12(6):1237-1252.
7. Mayer S, Rowland L. Head injury. In: Rowland L, ed. Merritt’s Neurology. Philadelphia, PA: Lippincott Williams & Wilkins; 2000:401.
8. Saif MW, Allegra CJ, Greenberg B. Bleeding diathesis in multiple myeloma. J Hematother Stem Cell Res. 2001;10(5):657-660.
9. Stiell IG, Clement CM, Rowe BH, et al. Comparison of the Canadian CT Head Rule and the New Orleans Criteria in patients with minor head injury. JAMA. 2005;294(12):1511-1518.
10. Abdelrahman H, Almadani A, El-Menyar A, et al. Home-related falls: an underestimated mechanism of injury. J Family Community Med. 2018; 25(1):48-51.
11. Fuller GF. Falls in the elderly. Am Fam Physician. 2000;61(7):2159-2168.
In the early morning hours of June 10, 2009, a 77-year-old man who had been undergoing chemotherapy for multiple myeloma took sleep medication. He then fell down a flight of stairs in his split-level home.
The patient sustained a laceration to his scalp but returned to bed and waited until later that morning to call his internist for an appointment. Later that day, the physician placed 11 sutures for the scalp laceration and performed a neurologic examination; he did not note any abnormalities. The patient complained of back pain, so the physician ordered a back x-ray, which revealed a TI2 fracture that had occurred from the fall. No further treatment was provided for the scalp injury, except removal of the stitches about a week later.
Six days after the fall and doctor visit, the patient’s condition began to deteriorate rapidly, with noted slurred speech and loss of consciousness. He was transported to an emergency department, where CT revealed a massive subdural hematoma. An immediate craniotomy was performed. However, on June 27, 2009, the patient died as a result of the brain bleed.
His estate filed suit against the physician and his practice, alleging medical malpractice and violations in the standard of care. The estate alleged that the standard of care required the physician to obtain a CT scan and that, had one been performed, it would have revealed a small subdural hematoma in time for it to have been successfully treated (ie, before the massive second related bleed). The estate’s theory of the case did not rest on the presentation of clinical symptoms. A medical expert who testified for the estate stated that the subdural hematoma began at the time of the fall.
The defense denied any violations in the standard of care. The physician contended that the patient had presented with no symptoms other than a head laceration, and there were no criteria for ordering CT. Further, the defense asserted that the patient was symptom free for 6 days post-fall. According to the defense, the patient experienced a sudden arterial bleed that was not caused by the fall and would not have been revealed on CT ordered at the time of initial presentation, because it did not occur until 6 days later.
VERDICT
After a 10-day trial and 25 minutes’ deliberation, the jury returned a defense verdict.
COMMENTARY
The 25-minute deliberation suggests that terms such as “bridging veins” and “shearing injury” were unlikely bandied about in the jury room. The jury was likely dismissive of the plaintiff’s claim owing to his cancer diagnosis, and perhaps rightly so. But if we eliminate the multiple myeloma diagnosis, the jury might have decided differently.
Continue to: The defendant physician...
The defendant physician did a good job of documenting a negative neurologic exam, which helped him convince the jury that the patient did not have any signs or symptoms when first evaluated. But in this patient, was imaging to rule out intracranial bleeding indicated?
As an oversimplification, we tend to think of intracranial hemorrhage in 2 varieties: the insidious and the bold. Subdural hematomas are stealthy, they are sneaky, and they prey on the old. They step out of the shadows to cause symptoms. They are the ninjas of intracranial hemorrhage. Beware.
Epidural hematomas and subarachnoid hemorrhage (SAH) are the opposite. They classically present with a sudden and severe symptom complex: with epidural hematoma, the loss of consciousness, lucid interval, and final loss of consciousness; with SAH, the “worst in your life” thunder-clap headache, which may be heralded by a sentinel headache.1 When manifesting this way, they are brash, direct, and unsubtle to the point of being obnoxious—the Steven Stifler of intracranial bleeding.
This generalization is made to highlight the potentially sneaky nature of subdural hemorrhage. There are circumstances in which the clinical presentation of epidural hematoma and SAH will be more challenging. The question here is whether a negative initial neurologic exam can adequately screen for a potentially stealthy subdural hematoma.
Subdural hemorrhage is caused by rapidly changing velocity that may stretch and tear small bridging veins.2,3 Subdural hematoma is more common in the elderly, those who abuse alcohol, and those with a prior history of head trauma.4 As the brain shrinks with age or atrophy, the subdural space enlarges and traversing veins are stretched to cover a wider distance—rendering them vulnerable to rupture.5 These structures may also weaken as a result of low cerebrospinal fluid (intracranial hypotension); as pressure decreases (eg, from a leak), the brain’s buoyancy is reduced, causing traction on anchoring and supporting structures (eg, bridging veins).5 Injury to bridging veins can even occur as a result of a coup-contrecoup mechanism in the absence of direct physical impact.6,7 Bottom line: the injury itself may be subtle, requiring an index of suspicion to make the diagnosis.
Continue to: The case patient was...
The case patient was elderly. He had a chronic malignancy and sustained a fall down the stairs. He was taking sleeping pills, which may have slowed reflexive protective mechanisms after he started to fall (resulting in greater force imparted to his head). Multiple myeloma can predispose a patient to coagulopathy, and we don’t know in this case if this patient’s multiple myeloma made him more susceptible to bleeding—but it certainly didn’t help.8 The patient’s age, the mechanism of injury, and the history of malignancy made this a setup for hemorrhage.
Interestingly, we are not given details about how the patient looked during his suture removal. We are told the time between the initial fall and deterioration was 6 days. Scalp sutures were removed “about a week later,” which was after the deterioration—so this can’t be correct. Removing scalp sutures after 5 days seems premature, but that is the only possibility if 6 days elapsed between the fall and the deterioration.
In short, these are difficult cases. If intracranial bleeding can be subtle and delayed, how can we be sure a patient is not experiencing a bleed? We can only apply the relevant standard of care using all the clinical information we have. The Canadian CT Head Rule and New Orleans Criteria are clinical tools designed to help providers determine when to image (see Table for details).9
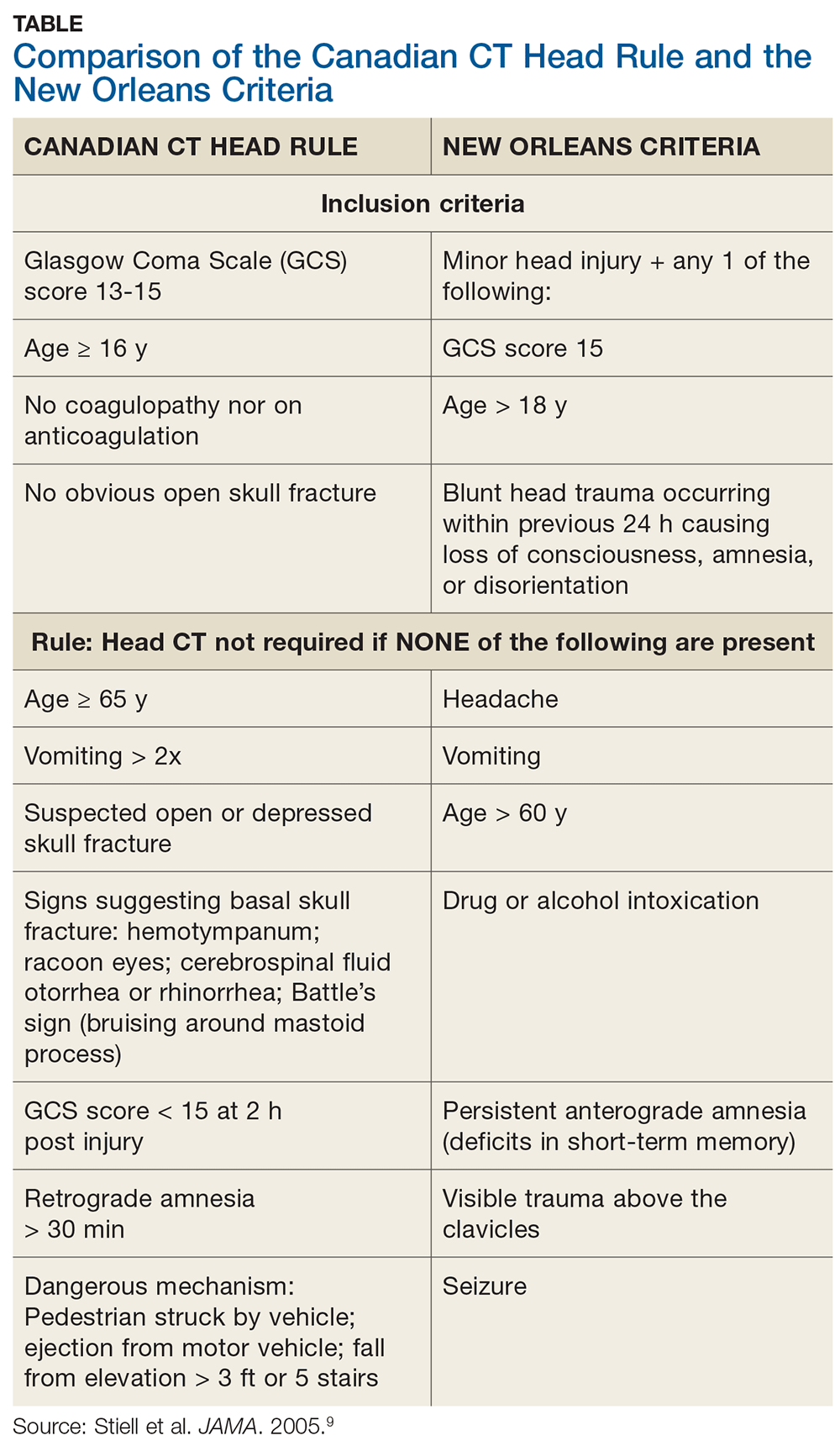
Applying the Canadian CT Head Rule to the facts of this case, we would image the patient because he fell down a “flight” of stairs (which is > 5 stairs) and he is 77 years old (older than 65). The New Orleans Criteria require head CT for minor injury with any positive findings.9 Because the patient is older than 60, he would be scanned according this rule.
In this case, the tools indicate scanning would have been appropriate. The patient’s multiple myeloma might have further impelled a decision to image. However, the jury was persuaded that the defendant’s negative neurologic exam was reasonable under the circumstances. This was likely made possible by the physician’s good recordkeeping and demonstrated genuine concern for the patient’s well-being—as well as a differing viewpoint of the patient’s age and health status.
Continue to: Finally, a word about...
Finally, a word about falls and the elderly: We’ve all heard the 80s advertising catchphrase (which lives on as a present-day meme) “I’ve fallen, and I can’t get up!” The problem is, many don’t. It would be more clinically accurate to say, “I’ve fallen, and I’ll be hospitalized for an extended period of time, then transferred to a skilled nursing facility, but I won’t survive to discharge.” The reality is that falls kill, and the severity is underestimated.10 If it were a “brain-eating amoeba,” the media would be all over it. With falls, not so much. We tend to pay less attention.
Risk factors for a fall include postural hypotension; use of benzodiazepines or other sedative-hypnotic drugs; use of ≥ 4 medications; environmental hazards for tripping; impairment in balance and transfer skills; and gait impairment.11 Home setup also contributes—loose throw rugs, uneven carpet edges, cracked sidewalks, clutter and furniture, cables and wires and cords, oh my.
Do your older patients a favor by reinforcing fall risk. Instruct them to rise slowly from seated or recumbent positions; always consider central nervous system sedation and/or the coordination-hampering properties of medications, particularly in combination. Raise the issue of home safety. A brief 10-second comment from you may plant a seed in a family member’s head to do what you cannot: scan and make safe the patient’s living environment.
In the early morning hours of June 10, 2009, a 77-year-old man who had been undergoing chemotherapy for multiple myeloma took sleep medication. He then fell down a flight of stairs in his split-level home.
The patient sustained a laceration to his scalp but returned to bed and waited until later that morning to call his internist for an appointment. Later that day, the physician placed 11 sutures for the scalp laceration and performed a neurologic examination; he did not note any abnormalities. The patient complained of back pain, so the physician ordered a back x-ray, which revealed a TI2 fracture that had occurred from the fall. No further treatment was provided for the scalp injury, except removal of the stitches about a week later.
Six days after the fall and doctor visit, the patient’s condition began to deteriorate rapidly, with noted slurred speech and loss of consciousness. He was transported to an emergency department, where CT revealed a massive subdural hematoma. An immediate craniotomy was performed. However, on June 27, 2009, the patient died as a result of the brain bleed.
His estate filed suit against the physician and his practice, alleging medical malpractice and violations in the standard of care. The estate alleged that the standard of care required the physician to obtain a CT scan and that, had one been performed, it would have revealed a small subdural hematoma in time for it to have been successfully treated (ie, before the massive second related bleed). The estate’s theory of the case did not rest on the presentation of clinical symptoms. A medical expert who testified for the estate stated that the subdural hematoma began at the time of the fall.
The defense denied any violations in the standard of care. The physician contended that the patient had presented with no symptoms other than a head laceration, and there were no criteria for ordering CT. Further, the defense asserted that the patient was symptom free for 6 days post-fall. According to the defense, the patient experienced a sudden arterial bleed that was not caused by the fall and would not have been revealed on CT ordered at the time of initial presentation, because it did not occur until 6 days later.
VERDICT
After a 10-day trial and 25 minutes’ deliberation, the jury returned a defense verdict.
COMMENTARY
The 25-minute deliberation suggests that terms such as “bridging veins” and “shearing injury” were unlikely bandied about in the jury room. The jury was likely dismissive of the plaintiff’s claim owing to his cancer diagnosis, and perhaps rightly so. But if we eliminate the multiple myeloma diagnosis, the jury might have decided differently.
Continue to: The defendant physician...
The defendant physician did a good job of documenting a negative neurologic exam, which helped him convince the jury that the patient did not have any signs or symptoms when first evaluated. But in this patient, was imaging to rule out intracranial bleeding indicated?
As an oversimplification, we tend to think of intracranial hemorrhage in 2 varieties: the insidious and the bold. Subdural hematomas are stealthy, they are sneaky, and they prey on the old. They step out of the shadows to cause symptoms. They are the ninjas of intracranial hemorrhage. Beware.
Epidural hematomas and subarachnoid hemorrhage (SAH) are the opposite. They classically present with a sudden and severe symptom complex: with epidural hematoma, the loss of consciousness, lucid interval, and final loss of consciousness; with SAH, the “worst in your life” thunder-clap headache, which may be heralded by a sentinel headache.1 When manifesting this way, they are brash, direct, and unsubtle to the point of being obnoxious—the Steven Stifler of intracranial bleeding.
This generalization is made to highlight the potentially sneaky nature of subdural hemorrhage. There are circumstances in which the clinical presentation of epidural hematoma and SAH will be more challenging. The question here is whether a negative initial neurologic exam can adequately screen for a potentially stealthy subdural hematoma.
Subdural hemorrhage is caused by rapidly changing velocity that may stretch and tear small bridging veins.2,3 Subdural hematoma is more common in the elderly, those who abuse alcohol, and those with a prior history of head trauma.4 As the brain shrinks with age or atrophy, the subdural space enlarges and traversing veins are stretched to cover a wider distance—rendering them vulnerable to rupture.5 These structures may also weaken as a result of low cerebrospinal fluid (intracranial hypotension); as pressure decreases (eg, from a leak), the brain’s buoyancy is reduced, causing traction on anchoring and supporting structures (eg, bridging veins).5 Injury to bridging veins can even occur as a result of a coup-contrecoup mechanism in the absence of direct physical impact.6,7 Bottom line: the injury itself may be subtle, requiring an index of suspicion to make the diagnosis.
Continue to: The case patient was...
The case patient was elderly. He had a chronic malignancy and sustained a fall down the stairs. He was taking sleeping pills, which may have slowed reflexive protective mechanisms after he started to fall (resulting in greater force imparted to his head). Multiple myeloma can predispose a patient to coagulopathy, and we don’t know in this case if this patient’s multiple myeloma made him more susceptible to bleeding—but it certainly didn’t help.8 The patient’s age, the mechanism of injury, and the history of malignancy made this a setup for hemorrhage.
Interestingly, we are not given details about how the patient looked during his suture removal. We are told the time between the initial fall and deterioration was 6 days. Scalp sutures were removed “about a week later,” which was after the deterioration—so this can’t be correct. Removing scalp sutures after 5 days seems premature, but that is the only possibility if 6 days elapsed between the fall and the deterioration.
In short, these are difficult cases. If intracranial bleeding can be subtle and delayed, how can we be sure a patient is not experiencing a bleed? We can only apply the relevant standard of care using all the clinical information we have. The Canadian CT Head Rule and New Orleans Criteria are clinical tools designed to help providers determine when to image (see Table for details).9
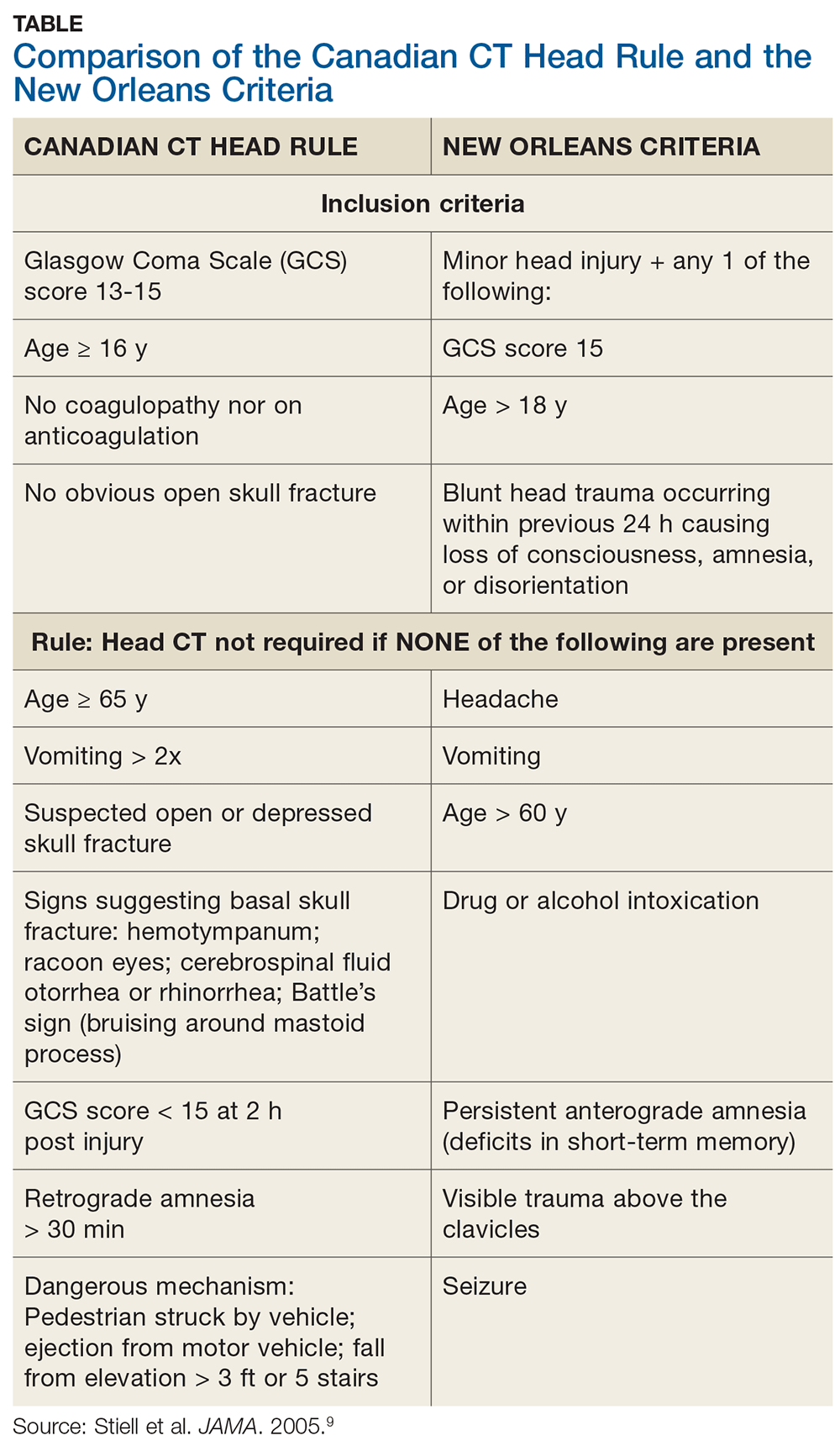
Applying the Canadian CT Head Rule to the facts of this case, we would image the patient because he fell down a “flight” of stairs (which is > 5 stairs) and he is 77 years old (older than 65). The New Orleans Criteria require head CT for minor injury with any positive findings.9 Because the patient is older than 60, he would be scanned according this rule.
In this case, the tools indicate scanning would have been appropriate. The patient’s multiple myeloma might have further impelled a decision to image. However, the jury was persuaded that the defendant’s negative neurologic exam was reasonable under the circumstances. This was likely made possible by the physician’s good recordkeeping and demonstrated genuine concern for the patient’s well-being—as well as a differing viewpoint of the patient’s age and health status.
Continue to: Finally, a word about...
Finally, a word about falls and the elderly: We’ve all heard the 80s advertising catchphrase (which lives on as a present-day meme) “I’ve fallen, and I can’t get up!” The problem is, many don’t. It would be more clinically accurate to say, “I’ve fallen, and I’ll be hospitalized for an extended period of time, then transferred to a skilled nursing facility, but I won’t survive to discharge.” The reality is that falls kill, and the severity is underestimated.10 If it were a “brain-eating amoeba,” the media would be all over it. With falls, not so much. We tend to pay less attention.
Risk factors for a fall include postural hypotension; use of benzodiazepines or other sedative-hypnotic drugs; use of ≥ 4 medications; environmental hazards for tripping; impairment in balance and transfer skills; and gait impairment.11 Home setup also contributes—loose throw rugs, uneven carpet edges, cracked sidewalks, clutter and furniture, cables and wires and cords, oh my.
Do your older patients a favor by reinforcing fall risk. Instruct them to rise slowly from seated or recumbent positions; always consider central nervous system sedation and/or the coordination-hampering properties of medications, particularly in combination. Raise the issue of home safety. A brief 10-second comment from you may plant a seed in a family member’s head to do what you cannot: scan and make safe the patient’s living environment.
1. de Falco FA. Sentinel headache. Neurol Sci. 2004;25(suppl 3):S215-S217.
2. Miller JD, Nader R. Acute subdural hematoma from bridging vein rupture: a potential mechanism for growth. J Neurosurg. 2014;120(6):1378-1384.
3. Victor M, Ropper A. Craniocerebral trauma. In: Victor M, Ropper A, eds. Adams and Victor’s Principles of Neurology. 7th ed. New York, NY: McGraw-Hill; 2001:925.
4. McBridde W. Subdural hematoma in adults: etiology, clinical features, and diagnosis. UpToDate website. www.uptodate.com/contents/subdural-hematoma-in-adults-etiology-clinical-features-and-diagnosis? search=subdural%20hematoma. Published December 10, 2018. Accessed September 23, 2019.
5. US National Library of Medicine. Subdural hematoma. Medline Plus website. https://medlineplus.gov/ency/article/000713.htm. Accessed September 23, 2019.
6. Besenski N. Traumatic injuries: imaging of head injuries. Eur Radiol. 2002;12(6):1237-1252.
7. Mayer S, Rowland L. Head injury. In: Rowland L, ed. Merritt’s Neurology. Philadelphia, PA: Lippincott Williams & Wilkins; 2000:401.
8. Saif MW, Allegra CJ, Greenberg B. Bleeding diathesis in multiple myeloma. J Hematother Stem Cell Res. 2001;10(5):657-660.
9. Stiell IG, Clement CM, Rowe BH, et al. Comparison of the Canadian CT Head Rule and the New Orleans Criteria in patients with minor head injury. JAMA. 2005;294(12):1511-1518.
10. Abdelrahman H, Almadani A, El-Menyar A, et al. Home-related falls: an underestimated mechanism of injury. J Family Community Med. 2018; 25(1):48-51.
11. Fuller GF. Falls in the elderly. Am Fam Physician. 2000;61(7):2159-2168.
1. de Falco FA. Sentinel headache. Neurol Sci. 2004;25(suppl 3):S215-S217.
2. Miller JD, Nader R. Acute subdural hematoma from bridging vein rupture: a potential mechanism for growth. J Neurosurg. 2014;120(6):1378-1384.
3. Victor M, Ropper A. Craniocerebral trauma. In: Victor M, Ropper A, eds. Adams and Victor’s Principles of Neurology. 7th ed. New York, NY: McGraw-Hill; 2001:925.
4. McBridde W. Subdural hematoma in adults: etiology, clinical features, and diagnosis. UpToDate website. www.uptodate.com/contents/subdural-hematoma-in-adults-etiology-clinical-features-and-diagnosis? search=subdural%20hematoma. Published December 10, 2018. Accessed September 23, 2019.
5. US National Library of Medicine. Subdural hematoma. Medline Plus website. https://medlineplus.gov/ency/article/000713.htm. Accessed September 23, 2019.
6. Besenski N. Traumatic injuries: imaging of head injuries. Eur Radiol. 2002;12(6):1237-1252.
7. Mayer S, Rowland L. Head injury. In: Rowland L, ed. Merritt’s Neurology. Philadelphia, PA: Lippincott Williams & Wilkins; 2000:401.
8. Saif MW, Allegra CJ, Greenberg B. Bleeding diathesis in multiple myeloma. J Hematother Stem Cell Res. 2001;10(5):657-660.
9. Stiell IG, Clement CM, Rowe BH, et al. Comparison of the Canadian CT Head Rule and the New Orleans Criteria in patients with minor head injury. JAMA. 2005;294(12):1511-1518.
10. Abdelrahman H, Almadani A, El-Menyar A, et al. Home-related falls: an underestimated mechanism of injury. J Family Community Med. 2018; 25(1):48-51.
11. Fuller GF. Falls in the elderly. Am Fam Physician. 2000;61(7):2159-2168.
Don’t Be a Maverick; Get a Wingman
A 39-year-old woman presented to an Arkansas cardiologist on February 12, 2010, with complaints of chest pain. The physician conducted an ankle-brachial index (ABI) test to measure the blood pressure in her lower extremity and interpreted it as less than 0.9%. He then ordered an echocardiogram to gauge the patient’s ejection fraction and interpreted the reading at 25%. Both measurements were below the normal average, which prompted the cardiologist to diagnose peripheral vascular disease and congestive heart failure.
The patient was eventually prescribed a course of cardiac medication and monitored over the ensuing months. On April 15, the cardiologist conducted a nuclear stress test; the computer-generated measurement of her ejection fraction was 50%, which the physician adjusted to 42%. In May, the patient underwent cardiac catheterization, which showed no lesions or blockages in the vessels. In the following months, the patient’s medication dosages were increased. On September 27, the cardiologist conducted another echocardiogram, which he read as 30%, and reaffirmed his diagnosis of congestive heart failure.
The physician continued to monitor the patient. On November 11, after being diagnosed with congestive heart failure, the patient was admitted to the hospital, where the cardiologist implanted an automated implantable cardioverter defibrillator (AICD).
On May 18, 2011, while running with her 2 daughters and a friend, the patient suddenly collapsed and experienced electrical currents coursing through her body (5 times). She was driven to a hospital, where it was determined that she did not go into cardiac arrest (which she suspected) but rather her defibrillator malfunctioned. The defibrillator was recalibrated to a higher setting, and she experienced no further issues.
In the ensuing years, the patient continued to follow up with her cardiologist. She eventually filed a lawsuit claiming that he had misdiagnosed congestive heart failure and unnecessarily implanted the AICD. Her experts in cardiology and cardiac electrophysiology testified that the defendant’s readings of the February 2010 ABI and echocardiogram results were incorrect; the ABIs were in fact .128 and .138 and the ejection fractions were 50% to 55% percent—in both instances, normal results. Furthermore, the September 2010 echocardiogram and another taken in February 2011, which showed little change from the first echocardiogram, were also normal, according to the experts.
The experts also opined that American College of Cardiology/American Heart Association guidelines state that a patient’s ejection fraction has to be less than 35% before a defibrillator is placed. Both experts concluded that the plaintiff did not have congestive heart failure and was therefore not a candidate for an AICD. The cardiac electrophysiology expert stated that to be a candidate, a patient must have an enlarged left ventricle—which plaintiff did not have. Moreover, none of the plaintiff’s physical findings were ever consistent with congestive heart failure: She did not have fluid in her lungs, as examinations always revealed clear lungs without congestion; there was no distention in her jugular veins; she did not experience sleep apnea; she did not lose consciousness; and she only experienced fatigue with exertion. The cardiology expert further faulted the defendant for failing to adjust the patient’s medication dosages to optimize her cardiac repair.
The defense maintained that the defendant’s treatment of the patient met the standard of care. According to the defense, the defendant’s judgment and interpretation of the patient’s ABI and echocardiogram results were medically sound and the defibrillator was necessary.
Continue to: VERDICT
VERDICT
After a 4-day trial and 3 hours of deliberation, the jury found that the defendant was liable and his actions were a factual cause of injury to plaintiff, who was awarded $1.75 million in damages.
COMMENTARY
In this case, the defendant cardiologist placed an AICD (also known as an implantable cardioverter defibrillator, or ICD). There was no allegation that the placement itself was negligent; rather, the claimed negligence was the decision to place it. But the plaintiff’s damages arise from the device’s malfunction—not the cardiologist’s decision to place it.
This case brings up an interesting issue of causation. As most of us know, medical malpractice plaintiffs must show (1) duty, (2) breach, (3) causation, and (4) harm. In law, there are 2 ways to think of causation: “but for” causation and “proximate” causation.
So-called “but for” causation is based on whether any causal relationship exists between an action and an outcome. For example, a drunk driver veers off the highway, through the breakdown lane, and strikes a tree, catching his car on fire. One minute later, a driver in the high-speed lane is captivated by the flaming vehicle, rubbernecks, fails to pay attention to traffic, and rear-ends the vehicle in front of him—injuring the driver of that car. Using “but for” causation, the drunk driver striking the tree “caused” the accident. If that had never happened, the second driver would never have been distracted, and if the driver wasn’t distracted, the second accident would not have occurred.
By contrast, “proximate” causation entails the immediate cause, which is foreseeable. Black’s Law defines proximate cause as “The result of a direct action and cause of loss to property that sets in motion a chain of events that is unbroken and causes damage, injury and destruction with no other interference” (emphasis added).1 Using a proximate causation analysis, the second driver’s negligent failure to pay attention to the road would be the proximate cause of the second crash.
Continue to: Generally, causation analysis...
Generally, causation analysis is limited to proximate cause on the basis that harm is reasonably foreseeable. A famous example is the case of Palsgraf v. Long Island Railroad.2
Mrs. Palsgraf was standing on a train platform. A man carrying an ordinary-looking package rushed to board a moving train, with help from 2 railroad employees (1 in the car and 1 on the platform). As the employees pushed and pulled the man aboard, the package fell onto the tracks. Unbeknownst to everyone but the package’s owner, it contained fireworks—which exploded when the rear wheels of the train ran over the package. The explosion caused a large standing scale to fall over and land on Mrs. Palsgraf, injuring her. This is what law professors live for.
Mrs. Palsgraf sued the railroad, arguing that if the employees had not negligently pushed and pulled the man, the package would not have fallen and would not have exploded, and the scale never would have fallen on her. Mrs. Palsgraf won her trial and won her first appeal. In a famous decision by a famous judge, the win was overturned on the basis that Mrs. Palsgraf’s injuries “were not a reasonably foreseeable consequence of any possible negligence by the railroad.” This case set a foundation of American law regarding reasonable foreseeability, both in terms of identifiable plaintiffs and expected danger.
What does a railroad accident have to do with medical malpractice? In the case described here, we had an arguably negligent medical decision to place the defibrillator. Then we had a malfunction of the device, which caused the plaintiff injury. Was it reasonably foreseeable that the device would malfunction and cause harm—and should the physician be on the hook for that?
Unlike the unforeseeable risk of knocking a simple package to the ground—which unexpectedly turned out to contain fireworks—the risk of device malfunction would be foreseeable. Why? Beyond the usual surgical risks of bleeding and infection, an ICD’s leads can dislodge, the device can fail, and devices can shock inappropriately (with younger patients at increased risk for inappropriate shocks).3,4 These risks are known, and it is highly likely the defendant cardiologist disclosed them on the consent form he asked the plaintiff to sign. The defense could not credibly argue that device malfunction was an unforeseeable risk. The malpractice here was the decision to place the ICD—and because placement wasn’t warranted in this patient, neither were the risks.
Continue to: This brings us to...
This brings us to the first malpractice trap: If you practice in a setting where a procedure is routinely offered, and that treatment has a billable cost, be cautious. Your decision-making can be made to appear driven by a profit motive. The lay public (including jurors) is suspicious of profit motive in medicine—a concept most clinicians find alien and repugnant.
Back in 2009, while outlining his rationale for the Affordable Care Act, President Obama made several statements that earned him swift rebuke from physician groups; I include them here not to incite political rants but to demonstrate the keen suspicion the public has for profit motives in clinical decision-making. On one occasion, he said, “Right now, doctors a lot of times are forced to make decisions based on the fee payment schedule. ... The doctor may look at the reimbursement system and say to himself, ‘You know what? I make a lot more money if I take this kid’s tonsils out.’”5 In another statement, while acknowledging that primary care providers offering preventive diabetes care make “a pittance,” Obama added, “But if that same [patient] ends up getting their foot amputated, that’s $30,000, $40,000, $50,000 immediately the surgeon is reimbursed.”6
For most clinicians, the idea of deciding on a course of treatment because it will be lucrative is an alien concept. Good clinicians base treatment on the accepted medical standard, and cost factors are a distant consideration if one at all.
However, if your practice involves a procedure or intervention that is a particularly lucrative billable event, do your part to play mental “devil’s advocate” and ensure that patients are genuinely in need of the treatment.
In some rare, bad (and usually highly publicized) cases, a procedure will be overused in a patently fraudulent way, which we all recognize is unethical and illegal. However, in other instances, a procedure may be overused because it is familiar and available. We’ve all heard the adage, “If all you have is a hammer, everything looks like a nail.” This “cute” expression holds some truth about the risk for cognitive bias based on the over-reliance on a familiar remedy.7 This particularly involves specialty practices that perform certain procedures frequently.
Continue to: In this case...
In this case, the plaintiff’s nuclear stress test showed an ejection fraction of 50%, which the defendant decreased to 42%. That is substantially different than the first ejection fraction of 25% and the second of 30% in a 39-year-old patient without any clinical signs of congestive heart failure. Did the defendant’s ability to offer an ICD color his appraisal of the patient’s cardiac function?
In closing arguments to the jury, the plaintiff’s attorney probably argued “this defendant behaved as if every human heart could be improved with a battery and wires.” Examine your practice to be sure you aren’t seeing nails where they don’t exist—because tomorrow, they will be the nails in the coffin of your career.
One thing missing from this case summary—but available via court records—is that the plaintiff claimed she had wanted a second opinion but was told she couldn’t have one: “I wanted a second opinion. And when I called [the defendant’s] office and asked ‘Could I have a second opinion,’ his nurse answered the phone and said that if I did get a second opinion, then I couldn’t come back.”8
There are a few aspects to discuss here, one of which is the second malpractice trap: viewing second opinions as an enemy. Most clinicians realize they are actually your friend. However, some providers are threatened by second opinions. It is as if they roll out of bed in the morning and consult the mirror to ask, “Who is the top cardiologist of them all?” and need the validation of that voice saying, “You, Dr. Smith—why of course, you!”
To that I say, forget the mirror, you egotistical so-and-so. Snow White will help protect you, your career, and most importantly, your patient. Allow the second opinion. In fact, integrate an expectation of the them into your practice style, to disarm any feelings of awkwardness, confrontation, or defensiveness. Think of the benefits: If Snow White validates your opinion, you have much stronger case that a course of treatment was indicated. Conversely, if Snow White arrives at a different opinion, she may have seen something you did not, and/or it may also relieve pressure from the patient to take an action with which you were only borderline comfortable.
Continue to: In cases I've worked on...
In cases I’ve worked on, I’ve seen some excellent surgeons who require a second opinion as a precondition to operating. This is particularly helpful when patient expectations are uncertain or there is a track record of unsuccessful interventions (eg, chronic back pain with multiple failed surgeries). Furthermore, a second opinion shows diligence, humility, and concern for the patient. It also gives you backup. As Top Gun taught us, there is no need to be a “maverick” when you can have a wingman.
As far as the alleged comment by the cardiologist’s nurse: We don’t know for certain if this actually happened—but if it did, it was unwarranted and foolish. Any jury would hear this and conclude the defendant (1) was an ass, (2) had something to hide, or (3) was guarding a profit source. Any way you slice it, this is bad for the patient and ultimately bad for the defendant. Make room in your practice for second opinions.
There was a legal fight regarding the admissibility of what the nurse had said. The defense filed a motion to prevent the plaintiff from telling the jury about the nurse’s statement, on the basis that the nurse’s statement was inadmissible hearsay. The court denied the motion, ruling that the cardiologist’s nurse was his agent and her words could be properly brought before the jury. The court found that the plaintiff relied on that statement in determining whether to have the ICD placed or obtain a second opinion.
This raises an interesting malpractice awareness point: If you are sued for malpractice, anything you had said to a patient, the patient’s family, or your coworkers will be admissible in court as a “party admission,” classified as either nonhearsay or a hearsay exception (assuming the statement was not made as part of a bona fide peer review, in which case it will likely be subject to peer review privilege). As seen in this case, this also applies to people acting as agents on your behalf. Be cautious of what you say and how you say it—and what your practice’s representatives are saying as well.
Interestingly, the jury found for the plaintiff in the amount of $1.75 million, but they declined to award punitive damages, which are designed to punish defendants rather than compensate the plaintiff. In Arkansas, the standard for punitive damages is tough; the plaintiff must “prove by clear and convincing evidence that the defendant knew or ought to have known, that their conduct would naturally and probably result in injury or damage and that they continued the conduct with malice or in reckless disregard of the consequences from which malice may be inferred.”9 A similar standard exists in most states. Because there were no punitive damages, we can infer the jury did not think the defendant implanted the ICD (for profit) knowing it wasn’t indicated.
Continue to: IN SUMMARY
IN SUMMARY
Consider foreseeable risks of practice interventions; be sure your practice is not on “autopilot,” recommending a common procedure or intervention too frequently. Don’t be threatened by second opinions; welcome them. And watch your words—as they say on every police procedural you’ve ever watched, they can be used against you.
1. The Law Dictionary. What is proximate cause? https://thelawdictionary.org/proximate-cause. Accessed August 21, 2019.
2. Palsgraf v Long Island R.R. Co (248 NY 339, 162 NE 99 [1928]).
3. Stanford Health Care. Risks: our approach for ICD. https://stanfordhealthcare.org/medical-treatments/i/icd/risks.html. Accessed August 21, 2019.
4. Hofer D, Steffel J, Hürlimann D, et al. Long-term incidence of inappropriate shocks in patients with implantable cardioverter defibrillators in clinical practice—an underestimated complication? J Interv Card Electrophysiol. 2017;50(3):219-226.
5. Transcript: Obama pleads health care case. CNN.com. July 22, 2009. www.cnn.com/2009/POLITICS/07/22/transcript.obama. Accessed August 21, 2019.
6. The White House Office of the Press Secretary. Remarks by the President at Town Hall on Health Insurance Reform in Portsmouth, New Hampshire [press release]. August 11, 2009. https://obamawhitehouse.archives.gov/the-press-office/remarks-president-town-hall-health-insurance-reform-portsmouth-new-hampshire. Accessed August 21, 2019.
7. Maslow AH. The Psychology of Science: a Reconnaissance. New York, NY: Harper & Row; 1966:15.
8. Thornton Dep. 55:3-55:7, March 16, 2014, AR Cir No. CV-2012-640-2.
9. Arkansas Code Title 16. Practice, procedure, and courts § 16-55-206: standards for award of punitive damages. https://codes.findlaw.com/ar/title-16-practice-procedure-and-courts/ar-code-sect-16-55-206.html. Accessed August 21, 2019.
A 39-year-old woman presented to an Arkansas cardiologist on February 12, 2010, with complaints of chest pain. The physician conducted an ankle-brachial index (ABI) test to measure the blood pressure in her lower extremity and interpreted it as less than 0.9%. He then ordered an echocardiogram to gauge the patient’s ejection fraction and interpreted the reading at 25%. Both measurements were below the normal average, which prompted the cardiologist to diagnose peripheral vascular disease and congestive heart failure.
The patient was eventually prescribed a course of cardiac medication and monitored over the ensuing months. On April 15, the cardiologist conducted a nuclear stress test; the computer-generated measurement of her ejection fraction was 50%, which the physician adjusted to 42%. In May, the patient underwent cardiac catheterization, which showed no lesions or blockages in the vessels. In the following months, the patient’s medication dosages were increased. On September 27, the cardiologist conducted another echocardiogram, which he read as 30%, and reaffirmed his diagnosis of congestive heart failure.
The physician continued to monitor the patient. On November 11, after being diagnosed with congestive heart failure, the patient was admitted to the hospital, where the cardiologist implanted an automated implantable cardioverter defibrillator (AICD).
On May 18, 2011, while running with her 2 daughters and a friend, the patient suddenly collapsed and experienced electrical currents coursing through her body (5 times). She was driven to a hospital, where it was determined that she did not go into cardiac arrest (which she suspected) but rather her defibrillator malfunctioned. The defibrillator was recalibrated to a higher setting, and she experienced no further issues.
In the ensuing years, the patient continued to follow up with her cardiologist. She eventually filed a lawsuit claiming that he had misdiagnosed congestive heart failure and unnecessarily implanted the AICD. Her experts in cardiology and cardiac electrophysiology testified that the defendant’s readings of the February 2010 ABI and echocardiogram results were incorrect; the ABIs were in fact .128 and .138 and the ejection fractions were 50% to 55% percent—in both instances, normal results. Furthermore, the September 2010 echocardiogram and another taken in February 2011, which showed little change from the first echocardiogram, were also normal, according to the experts.
The experts also opined that American College of Cardiology/American Heart Association guidelines state that a patient’s ejection fraction has to be less than 35% before a defibrillator is placed. Both experts concluded that the plaintiff did not have congestive heart failure and was therefore not a candidate for an AICD. The cardiac electrophysiology expert stated that to be a candidate, a patient must have an enlarged left ventricle—which plaintiff did not have. Moreover, none of the plaintiff’s physical findings were ever consistent with congestive heart failure: She did not have fluid in her lungs, as examinations always revealed clear lungs without congestion; there was no distention in her jugular veins; she did not experience sleep apnea; she did not lose consciousness; and she only experienced fatigue with exertion. The cardiology expert further faulted the defendant for failing to adjust the patient’s medication dosages to optimize her cardiac repair.
The defense maintained that the defendant’s treatment of the patient met the standard of care. According to the defense, the defendant’s judgment and interpretation of the patient’s ABI and echocardiogram results were medically sound and the defibrillator was necessary.
Continue to: VERDICT
VERDICT
After a 4-day trial and 3 hours of deliberation, the jury found that the defendant was liable and his actions were a factual cause of injury to plaintiff, who was awarded $1.75 million in damages.
COMMENTARY
In this case, the defendant cardiologist placed an AICD (also known as an implantable cardioverter defibrillator, or ICD). There was no allegation that the placement itself was negligent; rather, the claimed negligence was the decision to place it. But the plaintiff’s damages arise from the device’s malfunction—not the cardiologist’s decision to place it.
This case brings up an interesting issue of causation. As most of us know, medical malpractice plaintiffs must show (1) duty, (2) breach, (3) causation, and (4) harm. In law, there are 2 ways to think of causation: “but for” causation and “proximate” causation.
So-called “but for” causation is based on whether any causal relationship exists between an action and an outcome. For example, a drunk driver veers off the highway, through the breakdown lane, and strikes a tree, catching his car on fire. One minute later, a driver in the high-speed lane is captivated by the flaming vehicle, rubbernecks, fails to pay attention to traffic, and rear-ends the vehicle in front of him—injuring the driver of that car. Using “but for” causation, the drunk driver striking the tree “caused” the accident. If that had never happened, the second driver would never have been distracted, and if the driver wasn’t distracted, the second accident would not have occurred.
By contrast, “proximate” causation entails the immediate cause, which is foreseeable. Black’s Law defines proximate cause as “The result of a direct action and cause of loss to property that sets in motion a chain of events that is unbroken and causes damage, injury and destruction with no other interference” (emphasis added).1 Using a proximate causation analysis, the second driver’s negligent failure to pay attention to the road would be the proximate cause of the second crash.
Continue to: Generally, causation analysis...
Generally, causation analysis is limited to proximate cause on the basis that harm is reasonably foreseeable. A famous example is the case of Palsgraf v. Long Island Railroad.2
Mrs. Palsgraf was standing on a train platform. A man carrying an ordinary-looking package rushed to board a moving train, with help from 2 railroad employees (1 in the car and 1 on the platform). As the employees pushed and pulled the man aboard, the package fell onto the tracks. Unbeknownst to everyone but the package’s owner, it contained fireworks—which exploded when the rear wheels of the train ran over the package. The explosion caused a large standing scale to fall over and land on Mrs. Palsgraf, injuring her. This is what law professors live for.
Mrs. Palsgraf sued the railroad, arguing that if the employees had not negligently pushed and pulled the man, the package would not have fallen and would not have exploded, and the scale never would have fallen on her. Mrs. Palsgraf won her trial and won her first appeal. In a famous decision by a famous judge, the win was overturned on the basis that Mrs. Palsgraf’s injuries “were not a reasonably foreseeable consequence of any possible negligence by the railroad.” This case set a foundation of American law regarding reasonable foreseeability, both in terms of identifiable plaintiffs and expected danger.
What does a railroad accident have to do with medical malpractice? In the case described here, we had an arguably negligent medical decision to place the defibrillator. Then we had a malfunction of the device, which caused the plaintiff injury. Was it reasonably foreseeable that the device would malfunction and cause harm—and should the physician be on the hook for that?
Unlike the unforeseeable risk of knocking a simple package to the ground—which unexpectedly turned out to contain fireworks—the risk of device malfunction would be foreseeable. Why? Beyond the usual surgical risks of bleeding and infection, an ICD’s leads can dislodge, the device can fail, and devices can shock inappropriately (with younger patients at increased risk for inappropriate shocks).3,4 These risks are known, and it is highly likely the defendant cardiologist disclosed them on the consent form he asked the plaintiff to sign. The defense could not credibly argue that device malfunction was an unforeseeable risk. The malpractice here was the decision to place the ICD—and because placement wasn’t warranted in this patient, neither were the risks.
Continue to: This brings us to...
This brings us to the first malpractice trap: If you practice in a setting where a procedure is routinely offered, and that treatment has a billable cost, be cautious. Your decision-making can be made to appear driven by a profit motive. The lay public (including jurors) is suspicious of profit motive in medicine—a concept most clinicians find alien and repugnant.
Back in 2009, while outlining his rationale for the Affordable Care Act, President Obama made several statements that earned him swift rebuke from physician groups; I include them here not to incite political rants but to demonstrate the keen suspicion the public has for profit motives in clinical decision-making. On one occasion, he said, “Right now, doctors a lot of times are forced to make decisions based on the fee payment schedule. ... The doctor may look at the reimbursement system and say to himself, ‘You know what? I make a lot more money if I take this kid’s tonsils out.’”5 In another statement, while acknowledging that primary care providers offering preventive diabetes care make “a pittance,” Obama added, “But if that same [patient] ends up getting their foot amputated, that’s $30,000, $40,000, $50,000 immediately the surgeon is reimbursed.”6
For most clinicians, the idea of deciding on a course of treatment because it will be lucrative is an alien concept. Good clinicians base treatment on the accepted medical standard, and cost factors are a distant consideration if one at all.
However, if your practice involves a procedure or intervention that is a particularly lucrative billable event, do your part to play mental “devil’s advocate” and ensure that patients are genuinely in need of the treatment.
In some rare, bad (and usually highly publicized) cases, a procedure will be overused in a patently fraudulent way, which we all recognize is unethical and illegal. However, in other instances, a procedure may be overused because it is familiar and available. We’ve all heard the adage, “If all you have is a hammer, everything looks like a nail.” This “cute” expression holds some truth about the risk for cognitive bias based on the over-reliance on a familiar remedy.7 This particularly involves specialty practices that perform certain procedures frequently.
Continue to: In this case...
In this case, the plaintiff’s nuclear stress test showed an ejection fraction of 50%, which the defendant decreased to 42%. That is substantially different than the first ejection fraction of 25% and the second of 30% in a 39-year-old patient without any clinical signs of congestive heart failure. Did the defendant’s ability to offer an ICD color his appraisal of the patient’s cardiac function?
In closing arguments to the jury, the plaintiff’s attorney probably argued “this defendant behaved as if every human heart could be improved with a battery and wires.” Examine your practice to be sure you aren’t seeing nails where they don’t exist—because tomorrow, they will be the nails in the coffin of your career.
One thing missing from this case summary—but available via court records—is that the plaintiff claimed she had wanted a second opinion but was told she couldn’t have one: “I wanted a second opinion. And when I called [the defendant’s] office and asked ‘Could I have a second opinion,’ his nurse answered the phone and said that if I did get a second opinion, then I couldn’t come back.”8
There are a few aspects to discuss here, one of which is the second malpractice trap: viewing second opinions as an enemy. Most clinicians realize they are actually your friend. However, some providers are threatened by second opinions. It is as if they roll out of bed in the morning and consult the mirror to ask, “Who is the top cardiologist of them all?” and need the validation of that voice saying, “You, Dr. Smith—why of course, you!”
To that I say, forget the mirror, you egotistical so-and-so. Snow White will help protect you, your career, and most importantly, your patient. Allow the second opinion. In fact, integrate an expectation of the them into your practice style, to disarm any feelings of awkwardness, confrontation, or defensiveness. Think of the benefits: If Snow White validates your opinion, you have much stronger case that a course of treatment was indicated. Conversely, if Snow White arrives at a different opinion, she may have seen something you did not, and/or it may also relieve pressure from the patient to take an action with which you were only borderline comfortable.
Continue to: In cases I've worked on...
In cases I’ve worked on, I’ve seen some excellent surgeons who require a second opinion as a precondition to operating. This is particularly helpful when patient expectations are uncertain or there is a track record of unsuccessful interventions (eg, chronic back pain with multiple failed surgeries). Furthermore, a second opinion shows diligence, humility, and concern for the patient. It also gives you backup. As Top Gun taught us, there is no need to be a “maverick” when you can have a wingman.
As far as the alleged comment by the cardiologist’s nurse: We don’t know for certain if this actually happened—but if it did, it was unwarranted and foolish. Any jury would hear this and conclude the defendant (1) was an ass, (2) had something to hide, or (3) was guarding a profit source. Any way you slice it, this is bad for the patient and ultimately bad for the defendant. Make room in your practice for second opinions.
There was a legal fight regarding the admissibility of what the nurse had said. The defense filed a motion to prevent the plaintiff from telling the jury about the nurse’s statement, on the basis that the nurse’s statement was inadmissible hearsay. The court denied the motion, ruling that the cardiologist’s nurse was his agent and her words could be properly brought before the jury. The court found that the plaintiff relied on that statement in determining whether to have the ICD placed or obtain a second opinion.
This raises an interesting malpractice awareness point: If you are sued for malpractice, anything you had said to a patient, the patient’s family, or your coworkers will be admissible in court as a “party admission,” classified as either nonhearsay or a hearsay exception (assuming the statement was not made as part of a bona fide peer review, in which case it will likely be subject to peer review privilege). As seen in this case, this also applies to people acting as agents on your behalf. Be cautious of what you say and how you say it—and what your practice’s representatives are saying as well.
Interestingly, the jury found for the plaintiff in the amount of $1.75 million, but they declined to award punitive damages, which are designed to punish defendants rather than compensate the plaintiff. In Arkansas, the standard for punitive damages is tough; the plaintiff must “prove by clear and convincing evidence that the defendant knew or ought to have known, that their conduct would naturally and probably result in injury or damage and that they continued the conduct with malice or in reckless disregard of the consequences from which malice may be inferred.”9 A similar standard exists in most states. Because there were no punitive damages, we can infer the jury did not think the defendant implanted the ICD (for profit) knowing it wasn’t indicated.
Continue to: IN SUMMARY
IN SUMMARY
Consider foreseeable risks of practice interventions; be sure your practice is not on “autopilot,” recommending a common procedure or intervention too frequently. Don’t be threatened by second opinions; welcome them. And watch your words—as they say on every police procedural you’ve ever watched, they can be used against you.
A 39-year-old woman presented to an Arkansas cardiologist on February 12, 2010, with complaints of chest pain. The physician conducted an ankle-brachial index (ABI) test to measure the blood pressure in her lower extremity and interpreted it as less than 0.9%. He then ordered an echocardiogram to gauge the patient’s ejection fraction and interpreted the reading at 25%. Both measurements were below the normal average, which prompted the cardiologist to diagnose peripheral vascular disease and congestive heart failure.
The patient was eventually prescribed a course of cardiac medication and monitored over the ensuing months. On April 15, the cardiologist conducted a nuclear stress test; the computer-generated measurement of her ejection fraction was 50%, which the physician adjusted to 42%. In May, the patient underwent cardiac catheterization, which showed no lesions or blockages in the vessels. In the following months, the patient’s medication dosages were increased. On September 27, the cardiologist conducted another echocardiogram, which he read as 30%, and reaffirmed his diagnosis of congestive heart failure.
The physician continued to monitor the patient. On November 11, after being diagnosed with congestive heart failure, the patient was admitted to the hospital, where the cardiologist implanted an automated implantable cardioverter defibrillator (AICD).
On May 18, 2011, while running with her 2 daughters and a friend, the patient suddenly collapsed and experienced electrical currents coursing through her body (5 times). She was driven to a hospital, where it was determined that she did not go into cardiac arrest (which she suspected) but rather her defibrillator malfunctioned. The defibrillator was recalibrated to a higher setting, and she experienced no further issues.
In the ensuing years, the patient continued to follow up with her cardiologist. She eventually filed a lawsuit claiming that he had misdiagnosed congestive heart failure and unnecessarily implanted the AICD. Her experts in cardiology and cardiac electrophysiology testified that the defendant’s readings of the February 2010 ABI and echocardiogram results were incorrect; the ABIs were in fact .128 and .138 and the ejection fractions were 50% to 55% percent—in both instances, normal results. Furthermore, the September 2010 echocardiogram and another taken in February 2011, which showed little change from the first echocardiogram, were also normal, according to the experts.
The experts also opined that American College of Cardiology/American Heart Association guidelines state that a patient’s ejection fraction has to be less than 35% before a defibrillator is placed. Both experts concluded that the plaintiff did not have congestive heart failure and was therefore not a candidate for an AICD. The cardiac electrophysiology expert stated that to be a candidate, a patient must have an enlarged left ventricle—which plaintiff did not have. Moreover, none of the plaintiff’s physical findings were ever consistent with congestive heart failure: She did not have fluid in her lungs, as examinations always revealed clear lungs without congestion; there was no distention in her jugular veins; she did not experience sleep apnea; she did not lose consciousness; and she only experienced fatigue with exertion. The cardiology expert further faulted the defendant for failing to adjust the patient’s medication dosages to optimize her cardiac repair.
The defense maintained that the defendant’s treatment of the patient met the standard of care. According to the defense, the defendant’s judgment and interpretation of the patient’s ABI and echocardiogram results were medically sound and the defibrillator was necessary.
Continue to: VERDICT
VERDICT
After a 4-day trial and 3 hours of deliberation, the jury found that the defendant was liable and his actions were a factual cause of injury to plaintiff, who was awarded $1.75 million in damages.
COMMENTARY
In this case, the defendant cardiologist placed an AICD (also known as an implantable cardioverter defibrillator, or ICD). There was no allegation that the placement itself was negligent; rather, the claimed negligence was the decision to place it. But the plaintiff’s damages arise from the device’s malfunction—not the cardiologist’s decision to place it.
This case brings up an interesting issue of causation. As most of us know, medical malpractice plaintiffs must show (1) duty, (2) breach, (3) causation, and (4) harm. In law, there are 2 ways to think of causation: “but for” causation and “proximate” causation.
So-called “but for” causation is based on whether any causal relationship exists between an action and an outcome. For example, a drunk driver veers off the highway, through the breakdown lane, and strikes a tree, catching his car on fire. One minute later, a driver in the high-speed lane is captivated by the flaming vehicle, rubbernecks, fails to pay attention to traffic, and rear-ends the vehicle in front of him—injuring the driver of that car. Using “but for” causation, the drunk driver striking the tree “caused” the accident. If that had never happened, the second driver would never have been distracted, and if the driver wasn’t distracted, the second accident would not have occurred.
By contrast, “proximate” causation entails the immediate cause, which is foreseeable. Black’s Law defines proximate cause as “The result of a direct action and cause of loss to property that sets in motion a chain of events that is unbroken and causes damage, injury and destruction with no other interference” (emphasis added).1 Using a proximate causation analysis, the second driver’s negligent failure to pay attention to the road would be the proximate cause of the second crash.
Continue to: Generally, causation analysis...
Generally, causation analysis is limited to proximate cause on the basis that harm is reasonably foreseeable. A famous example is the case of Palsgraf v. Long Island Railroad.2
Mrs. Palsgraf was standing on a train platform. A man carrying an ordinary-looking package rushed to board a moving train, with help from 2 railroad employees (1 in the car and 1 on the platform). As the employees pushed and pulled the man aboard, the package fell onto the tracks. Unbeknownst to everyone but the package’s owner, it contained fireworks—which exploded when the rear wheels of the train ran over the package. The explosion caused a large standing scale to fall over and land on Mrs. Palsgraf, injuring her. This is what law professors live for.
Mrs. Palsgraf sued the railroad, arguing that if the employees had not negligently pushed and pulled the man, the package would not have fallen and would not have exploded, and the scale never would have fallen on her. Mrs. Palsgraf won her trial and won her first appeal. In a famous decision by a famous judge, the win was overturned on the basis that Mrs. Palsgraf’s injuries “were not a reasonably foreseeable consequence of any possible negligence by the railroad.” This case set a foundation of American law regarding reasonable foreseeability, both in terms of identifiable plaintiffs and expected danger.
What does a railroad accident have to do with medical malpractice? In the case described here, we had an arguably negligent medical decision to place the defibrillator. Then we had a malfunction of the device, which caused the plaintiff injury. Was it reasonably foreseeable that the device would malfunction and cause harm—and should the physician be on the hook for that?
Unlike the unforeseeable risk of knocking a simple package to the ground—which unexpectedly turned out to contain fireworks—the risk of device malfunction would be foreseeable. Why? Beyond the usual surgical risks of bleeding and infection, an ICD’s leads can dislodge, the device can fail, and devices can shock inappropriately (with younger patients at increased risk for inappropriate shocks).3,4 These risks are known, and it is highly likely the defendant cardiologist disclosed them on the consent form he asked the plaintiff to sign. The defense could not credibly argue that device malfunction was an unforeseeable risk. The malpractice here was the decision to place the ICD—and because placement wasn’t warranted in this patient, neither were the risks.
Continue to: This brings us to...
This brings us to the first malpractice trap: If you practice in a setting where a procedure is routinely offered, and that treatment has a billable cost, be cautious. Your decision-making can be made to appear driven by a profit motive. The lay public (including jurors) is suspicious of profit motive in medicine—a concept most clinicians find alien and repugnant.
Back in 2009, while outlining his rationale for the Affordable Care Act, President Obama made several statements that earned him swift rebuke from physician groups; I include them here not to incite political rants but to demonstrate the keen suspicion the public has for profit motives in clinical decision-making. On one occasion, he said, “Right now, doctors a lot of times are forced to make decisions based on the fee payment schedule. ... The doctor may look at the reimbursement system and say to himself, ‘You know what? I make a lot more money if I take this kid’s tonsils out.’”5 In another statement, while acknowledging that primary care providers offering preventive diabetes care make “a pittance,” Obama added, “But if that same [patient] ends up getting their foot amputated, that’s $30,000, $40,000, $50,000 immediately the surgeon is reimbursed.”6
For most clinicians, the idea of deciding on a course of treatment because it will be lucrative is an alien concept. Good clinicians base treatment on the accepted medical standard, and cost factors are a distant consideration if one at all.
However, if your practice involves a procedure or intervention that is a particularly lucrative billable event, do your part to play mental “devil’s advocate” and ensure that patients are genuinely in need of the treatment.
In some rare, bad (and usually highly publicized) cases, a procedure will be overused in a patently fraudulent way, which we all recognize is unethical and illegal. However, in other instances, a procedure may be overused because it is familiar and available. We’ve all heard the adage, “If all you have is a hammer, everything looks like a nail.” This “cute” expression holds some truth about the risk for cognitive bias based on the over-reliance on a familiar remedy.7 This particularly involves specialty practices that perform certain procedures frequently.
Continue to: In this case...
In this case, the plaintiff’s nuclear stress test showed an ejection fraction of 50%, which the defendant decreased to 42%. That is substantially different than the first ejection fraction of 25% and the second of 30% in a 39-year-old patient without any clinical signs of congestive heart failure. Did the defendant’s ability to offer an ICD color his appraisal of the patient’s cardiac function?
In closing arguments to the jury, the plaintiff’s attorney probably argued “this defendant behaved as if every human heart could be improved with a battery and wires.” Examine your practice to be sure you aren’t seeing nails where they don’t exist—because tomorrow, they will be the nails in the coffin of your career.
One thing missing from this case summary—but available via court records—is that the plaintiff claimed she had wanted a second opinion but was told she couldn’t have one: “I wanted a second opinion. And when I called [the defendant’s] office and asked ‘Could I have a second opinion,’ his nurse answered the phone and said that if I did get a second opinion, then I couldn’t come back.”8
There are a few aspects to discuss here, one of which is the second malpractice trap: viewing second opinions as an enemy. Most clinicians realize they are actually your friend. However, some providers are threatened by second opinions. It is as if they roll out of bed in the morning and consult the mirror to ask, “Who is the top cardiologist of them all?” and need the validation of that voice saying, “You, Dr. Smith—why of course, you!”
To that I say, forget the mirror, you egotistical so-and-so. Snow White will help protect you, your career, and most importantly, your patient. Allow the second opinion. In fact, integrate an expectation of the them into your practice style, to disarm any feelings of awkwardness, confrontation, or defensiveness. Think of the benefits: If Snow White validates your opinion, you have much stronger case that a course of treatment was indicated. Conversely, if Snow White arrives at a different opinion, she may have seen something you did not, and/or it may also relieve pressure from the patient to take an action with which you were only borderline comfortable.
Continue to: In cases I've worked on...
In cases I’ve worked on, I’ve seen some excellent surgeons who require a second opinion as a precondition to operating. This is particularly helpful when patient expectations are uncertain or there is a track record of unsuccessful interventions (eg, chronic back pain with multiple failed surgeries). Furthermore, a second opinion shows diligence, humility, and concern for the patient. It also gives you backup. As Top Gun taught us, there is no need to be a “maverick” when you can have a wingman.
As far as the alleged comment by the cardiologist’s nurse: We don’t know for certain if this actually happened—but if it did, it was unwarranted and foolish. Any jury would hear this and conclude the defendant (1) was an ass, (2) had something to hide, or (3) was guarding a profit source. Any way you slice it, this is bad for the patient and ultimately bad for the defendant. Make room in your practice for second opinions.
There was a legal fight regarding the admissibility of what the nurse had said. The defense filed a motion to prevent the plaintiff from telling the jury about the nurse’s statement, on the basis that the nurse’s statement was inadmissible hearsay. The court denied the motion, ruling that the cardiologist’s nurse was his agent and her words could be properly brought before the jury. The court found that the plaintiff relied on that statement in determining whether to have the ICD placed or obtain a second opinion.
This raises an interesting malpractice awareness point: If you are sued for malpractice, anything you had said to a patient, the patient’s family, or your coworkers will be admissible in court as a “party admission,” classified as either nonhearsay or a hearsay exception (assuming the statement was not made as part of a bona fide peer review, in which case it will likely be subject to peer review privilege). As seen in this case, this also applies to people acting as agents on your behalf. Be cautious of what you say and how you say it—and what your practice’s representatives are saying as well.
Interestingly, the jury found for the plaintiff in the amount of $1.75 million, but they declined to award punitive damages, which are designed to punish defendants rather than compensate the plaintiff. In Arkansas, the standard for punitive damages is tough; the plaintiff must “prove by clear and convincing evidence that the defendant knew or ought to have known, that their conduct would naturally and probably result in injury or damage and that they continued the conduct with malice or in reckless disregard of the consequences from which malice may be inferred.”9 A similar standard exists in most states. Because there were no punitive damages, we can infer the jury did not think the defendant implanted the ICD (for profit) knowing it wasn’t indicated.
Continue to: IN SUMMARY
IN SUMMARY
Consider foreseeable risks of practice interventions; be sure your practice is not on “autopilot,” recommending a common procedure or intervention too frequently. Don’t be threatened by second opinions; welcome them. And watch your words—as they say on every police procedural you’ve ever watched, they can be used against you.
1. The Law Dictionary. What is proximate cause? https://thelawdictionary.org/proximate-cause. Accessed August 21, 2019.
2. Palsgraf v Long Island R.R. Co (248 NY 339, 162 NE 99 [1928]).
3. Stanford Health Care. Risks: our approach for ICD. https://stanfordhealthcare.org/medical-treatments/i/icd/risks.html. Accessed August 21, 2019.
4. Hofer D, Steffel J, Hürlimann D, et al. Long-term incidence of inappropriate shocks in patients with implantable cardioverter defibrillators in clinical practice—an underestimated complication? J Interv Card Electrophysiol. 2017;50(3):219-226.
5. Transcript: Obama pleads health care case. CNN.com. July 22, 2009. www.cnn.com/2009/POLITICS/07/22/transcript.obama. Accessed August 21, 2019.
6. The White House Office of the Press Secretary. Remarks by the President at Town Hall on Health Insurance Reform in Portsmouth, New Hampshire [press release]. August 11, 2009. https://obamawhitehouse.archives.gov/the-press-office/remarks-president-town-hall-health-insurance-reform-portsmouth-new-hampshire. Accessed August 21, 2019.
7. Maslow AH. The Psychology of Science: a Reconnaissance. New York, NY: Harper & Row; 1966:15.
8. Thornton Dep. 55:3-55:7, March 16, 2014, AR Cir No. CV-2012-640-2.
9. Arkansas Code Title 16. Practice, procedure, and courts § 16-55-206: standards for award of punitive damages. https://codes.findlaw.com/ar/title-16-practice-procedure-and-courts/ar-code-sect-16-55-206.html. Accessed August 21, 2019.
1. The Law Dictionary. What is proximate cause? https://thelawdictionary.org/proximate-cause. Accessed August 21, 2019.
2. Palsgraf v Long Island R.R. Co (248 NY 339, 162 NE 99 [1928]).
3. Stanford Health Care. Risks: our approach for ICD. https://stanfordhealthcare.org/medical-treatments/i/icd/risks.html. Accessed August 21, 2019.
4. Hofer D, Steffel J, Hürlimann D, et al. Long-term incidence of inappropriate shocks in patients with implantable cardioverter defibrillators in clinical practice—an underestimated complication? J Interv Card Electrophysiol. 2017;50(3):219-226.
5. Transcript: Obama pleads health care case. CNN.com. July 22, 2009. www.cnn.com/2009/POLITICS/07/22/transcript.obama. Accessed August 21, 2019.
6. The White House Office of the Press Secretary. Remarks by the President at Town Hall on Health Insurance Reform in Portsmouth, New Hampshire [press release]. August 11, 2009. https://obamawhitehouse.archives.gov/the-press-office/remarks-president-town-hall-health-insurance-reform-portsmouth-new-hampshire. Accessed August 21, 2019.
7. Maslow AH. The Psychology of Science: a Reconnaissance. New York, NY: Harper & Row; 1966:15.
8. Thornton Dep. 55:3-55:7, March 16, 2014, AR Cir No. CV-2012-640-2.
9. Arkansas Code Title 16. Practice, procedure, and courts § 16-55-206: standards for award of punitive damages. https://codes.findlaw.com/ar/title-16-practice-procedure-and-courts/ar-code-sect-16-55-206.html. Accessed August 21, 2019.
Don’t Mix Off-label Use With Off-the-rack Pills
A pregnant woman in Wisconsin received prenatal care from a family practitioner. The patient had hypertension, so at about 38 weeks’ gestation, the decision was made to induce labor.
On May 15, 2012, the family practitioner used misoprostol to induce labor. The patient received 100 mcg vaginally at 12:24
At 1:28
Variable late decelerations occurred at 11:36
Although the family practitioner was present at the bedside at 12:40
The on-call physician accomplished a vacuum delivery at 1:30
The child now has severe cerebral palsy, with gross motor involvement in the arms and legs. He can communicate through augmentative communication devices but cannot actually speak. He will require full-time care for the rest of his life.
Continue to: The defense took the position...
The defense took the position that while the dosage of misoprostol was excessive, the drug was no longer active in the mother’s body, based on its half-life, when the fetal distress occurred.
VERDICT
Four days before trial, the case was settled for $9 million.
COMMENTARY
I suspect many of you have made a pot roast—and at least some of you have used the simple, tried-and-true method of putting the meat into the slow cooker with a packet of onion soup mix. It makes a tasty dinner with minimal effort. But onion soup packets are for making onion soup—not seasoning pot roast. Guess what? You just used that soup mix off-label!
As clinicians, we all use medications for clinical indications that haven’t been specifically authorized by the FDA—and we shouldn’t stop. Off-label prescribing is legal, common, and often supported by the standard of care.
But there is a risk: The pill or tablet prepared by the manufacturer is generally aimed at the intended on-label use, not off-label uses. In this case, misoprostol (brand name, Cytotec) is approved by the FDA for prevention and treatment of gastrointestinal ulcers and peptic ulcer disease. The package insert describes dosing as follows:
The recommended adult oral dose of Cytotec for reducing the risk of NSAID-induced gastric ulcers is 200 mcg four times daily with food. If this dose cannot be tolerated, a dose of 100 mcg can be used.1
Continue to: We should not be shocked...
We should not be shocked, then, that Cytotec is supplied as 100- and 200-mcg round white tablets. However, it is frequently used off label for cervical ripening during labor at a dose of “25 mcg inserted into the posterior vaginal fornix.”2
This brings us to the malpractice trap. While off-label use may be appropriate, off-label uses may not neatly “fit” with the substance prepared by the manufacturer. To be properly administered for cervical ripening, the available tablet of misoprostol must be cut with a pill cutter or razor prior to administration.3 Furthermore, dosage is more accurate if the tablet fragments are individually weighed after cutting.3
In this case, the discrepancy between the pill prepared by the manufacturer (100 mcg) and the dosage needed (25 mcg) appears to have caught the defendant family practitioner off guard. So the take-home message is: Use medications as supported by the standard of care—but when using a drug off label, do not assume the product supplied by the manufacturer is appropriate for use as is.
Another interesting aspect of this case is the defense strategy. Most clinicians are aware that the tort of negligence involves (1) duty, (2) breach, (3) causation, and (4) harm. However, it is more logically consistent to think of the elements in this way: (1) duty, (2) breach, (3) harm, and if harm has occurred, (4) examine causation (ie, the logical connection between breach and harm).
In malpractice cases, attorneys frequently focus on one of these specific elements. In this case, the physician’s duty of care and the harm stemming from cerebral palsy are clearly established. Thus, breach and causation take center stage.
Continue to: The defense lawyers...
The defense lawyers acknowledged there was a breach, noting the dosage was “excessive.” However, they argued that this error didn’t matter because the drug was no longer active in the patient’s body. In other words, there was no causal connection between the inappropriately high dose and the resultant uterine tachysystole and fetal distress. This is a difficult road for several reasons.
First, the chief danger of using misoprostol is uterine hyperstimulation and fetal distress. The defense would have to argue the hyperstimulation and fetal distress were coincidental and unrelated to the misoprostol—which carries a black box warning for these very adverse effects. The plaintiff’s attorney is sure to make a big deal out of the black box warning in front of the jury—noting any reasonable clinician practicing obstetrics should be aware of the risks that come with misoprostol’s use. You can almost hear the argument in summation: “It is so important, they drew a warning box around it.”
Furthermore, making the argument that the misoprostol was not in the mother’s system at the time the fetal distress started would entail dueling expert testimony about pharmacokinetics and bioavailability—concepts that are difficult for lay jurors to understand. Misoprostol has a half-life of about 20 to 40 min when administered orally and about 60 min when administered vaginally.4 We know the mother received the overdose of misoprostol at 12:24
The plaintiff’s team might counter with an expert’s explanation that misoprostol’s bioavailability is increased 2- to 3-fold with vaginal versus oral administration. It would also be observed that compared with oral administration, vaginal administration of misoprostol is associated with a slower increase in plasma concentrations but longer elevations (peaking about 1-2 hours after vaginal administration).5
At best, the defense expert would be able to argue that the serum level likely peaked 1 to 2 hours after administration (1:24-2:24
Continue to: Most jurors would...
Most jurors would take a skeptical view of the defendant’s argument that the negative outcome in this case was coincidental. Some might even be angered by it. This realization likely prompted the defense to settle this case for $9 million.
IN SUMMARY
Onion soup mix makes great soup, but it’s an even better seasoning for pot roast. Similarly, there are pharmacologic agents that are effective for conditions for which they are not formally indicated. Do not withhold judicious off-label use of medications when appropriate. However, be aware that off-label uses may require extra attention, and dosing and administration may not be consistent with the product you have on hand. Don’t hesitate to seek guidance from pharmacy colleagues when you have questions—they are an underutilized resource and are generally happy to share their expertise.
1. Cytotec [package insert]. New York, NY: Pfizer Inc; 2009.
2. Misoprostol: dosing considerations. PDR: Prescribers’ Digital Reference. www.pdr.net/drug-summary/Cytotec-misoprostol-1044#8. Accessed July 29, 2019.
3. Williams MC, Tsibris JC, Davis G, et al. Dose variation that is associated with approximated one-quarter tablet doses of misoprostol. Am J Obstet Gynecol. 2002;187(3):615-619.
4. Yount SM, Lassiter N. The pharmacology of prostaglandins for induction of labor. J Midwifery Womens Health. 2013;58(2):133-144; quiz 238-239.
5. Danielsson KG, Marions L, Rodriguez A, et al. Comparison between oral and vaginal administration of misoprostol on uterine contractility. Obstet Gynecol. 1999;93(2):275-280.
A pregnant woman in Wisconsin received prenatal care from a family practitioner. The patient had hypertension, so at about 38 weeks’ gestation, the decision was made to induce labor.
On May 15, 2012, the family practitioner used misoprostol to induce labor. The patient received 100 mcg vaginally at 12:24
At 1:28
Variable late decelerations occurred at 11:36
Although the family practitioner was present at the bedside at 12:40
The on-call physician accomplished a vacuum delivery at 1:30
The child now has severe cerebral palsy, with gross motor involvement in the arms and legs. He can communicate through augmentative communication devices but cannot actually speak. He will require full-time care for the rest of his life.
Continue to: The defense took the position...
The defense took the position that while the dosage of misoprostol was excessive, the drug was no longer active in the mother’s body, based on its half-life, when the fetal distress occurred.
VERDICT
Four days before trial, the case was settled for $9 million.
COMMENTARY
I suspect many of you have made a pot roast—and at least some of you have used the simple, tried-and-true method of putting the meat into the slow cooker with a packet of onion soup mix. It makes a tasty dinner with minimal effort. But onion soup packets are for making onion soup—not seasoning pot roast. Guess what? You just used that soup mix off-label!
As clinicians, we all use medications for clinical indications that haven’t been specifically authorized by the FDA—and we shouldn’t stop. Off-label prescribing is legal, common, and often supported by the standard of care.
But there is a risk: The pill or tablet prepared by the manufacturer is generally aimed at the intended on-label use, not off-label uses. In this case, misoprostol (brand name, Cytotec) is approved by the FDA for prevention and treatment of gastrointestinal ulcers and peptic ulcer disease. The package insert describes dosing as follows:
The recommended adult oral dose of Cytotec for reducing the risk of NSAID-induced gastric ulcers is 200 mcg four times daily with food. If this dose cannot be tolerated, a dose of 100 mcg can be used.1
Continue to: We should not be shocked...
We should not be shocked, then, that Cytotec is supplied as 100- and 200-mcg round white tablets. However, it is frequently used off label for cervical ripening during labor at a dose of “25 mcg inserted into the posterior vaginal fornix.”2
This brings us to the malpractice trap. While off-label use may be appropriate, off-label uses may not neatly “fit” with the substance prepared by the manufacturer. To be properly administered for cervical ripening, the available tablet of misoprostol must be cut with a pill cutter or razor prior to administration.3 Furthermore, dosage is more accurate if the tablet fragments are individually weighed after cutting.3
In this case, the discrepancy between the pill prepared by the manufacturer (100 mcg) and the dosage needed (25 mcg) appears to have caught the defendant family practitioner off guard. So the take-home message is: Use medications as supported by the standard of care—but when using a drug off label, do not assume the product supplied by the manufacturer is appropriate for use as is.
Another interesting aspect of this case is the defense strategy. Most clinicians are aware that the tort of negligence involves (1) duty, (2) breach, (3) causation, and (4) harm. However, it is more logically consistent to think of the elements in this way: (1) duty, (2) breach, (3) harm, and if harm has occurred, (4) examine causation (ie, the logical connection between breach and harm).
In malpractice cases, attorneys frequently focus on one of these specific elements. In this case, the physician’s duty of care and the harm stemming from cerebral palsy are clearly established. Thus, breach and causation take center stage.
Continue to: The defense lawyers...
The defense lawyers acknowledged there was a breach, noting the dosage was “excessive.” However, they argued that this error didn’t matter because the drug was no longer active in the patient’s body. In other words, there was no causal connection between the inappropriately high dose and the resultant uterine tachysystole and fetal distress. This is a difficult road for several reasons.
First, the chief danger of using misoprostol is uterine hyperstimulation and fetal distress. The defense would have to argue the hyperstimulation and fetal distress were coincidental and unrelated to the misoprostol—which carries a black box warning for these very adverse effects. The plaintiff’s attorney is sure to make a big deal out of the black box warning in front of the jury—noting any reasonable clinician practicing obstetrics should be aware of the risks that come with misoprostol’s use. You can almost hear the argument in summation: “It is so important, they drew a warning box around it.”
Furthermore, making the argument that the misoprostol was not in the mother’s system at the time the fetal distress started would entail dueling expert testimony about pharmacokinetics and bioavailability—concepts that are difficult for lay jurors to understand. Misoprostol has a half-life of about 20 to 40 min when administered orally and about 60 min when administered vaginally.4 We know the mother received the overdose of misoprostol at 12:24
The plaintiff’s team might counter with an expert’s explanation that misoprostol’s bioavailability is increased 2- to 3-fold with vaginal versus oral administration. It would also be observed that compared with oral administration, vaginal administration of misoprostol is associated with a slower increase in plasma concentrations but longer elevations (peaking about 1-2 hours after vaginal administration).5
At best, the defense expert would be able to argue that the serum level likely peaked 1 to 2 hours after administration (1:24-2:24
Continue to: Most jurors would...
Most jurors would take a skeptical view of the defendant’s argument that the negative outcome in this case was coincidental. Some might even be angered by it. This realization likely prompted the defense to settle this case for $9 million.
IN SUMMARY
Onion soup mix makes great soup, but it’s an even better seasoning for pot roast. Similarly, there are pharmacologic agents that are effective for conditions for which they are not formally indicated. Do not withhold judicious off-label use of medications when appropriate. However, be aware that off-label uses may require extra attention, and dosing and administration may not be consistent with the product you have on hand. Don’t hesitate to seek guidance from pharmacy colleagues when you have questions—they are an underutilized resource and are generally happy to share their expertise.
A pregnant woman in Wisconsin received prenatal care from a family practitioner. The patient had hypertension, so at about 38 weeks’ gestation, the decision was made to induce labor.
On May 15, 2012, the family practitioner used misoprostol to induce labor. The patient received 100 mcg vaginally at 12:24
At 1:28
Variable late decelerations occurred at 11:36
Although the family practitioner was present at the bedside at 12:40
The on-call physician accomplished a vacuum delivery at 1:30
The child now has severe cerebral palsy, with gross motor involvement in the arms and legs. He can communicate through augmentative communication devices but cannot actually speak. He will require full-time care for the rest of his life.
Continue to: The defense took the position...
The defense took the position that while the dosage of misoprostol was excessive, the drug was no longer active in the mother’s body, based on its half-life, when the fetal distress occurred.
VERDICT
Four days before trial, the case was settled for $9 million.
COMMENTARY
I suspect many of you have made a pot roast—and at least some of you have used the simple, tried-and-true method of putting the meat into the slow cooker with a packet of onion soup mix. It makes a tasty dinner with minimal effort. But onion soup packets are for making onion soup—not seasoning pot roast. Guess what? You just used that soup mix off-label!
As clinicians, we all use medications for clinical indications that haven’t been specifically authorized by the FDA—and we shouldn’t stop. Off-label prescribing is legal, common, and often supported by the standard of care.
But there is a risk: The pill or tablet prepared by the manufacturer is generally aimed at the intended on-label use, not off-label uses. In this case, misoprostol (brand name, Cytotec) is approved by the FDA for prevention and treatment of gastrointestinal ulcers and peptic ulcer disease. The package insert describes dosing as follows:
The recommended adult oral dose of Cytotec for reducing the risk of NSAID-induced gastric ulcers is 200 mcg four times daily with food. If this dose cannot be tolerated, a dose of 100 mcg can be used.1
Continue to: We should not be shocked...
We should not be shocked, then, that Cytotec is supplied as 100- and 200-mcg round white tablets. However, it is frequently used off label for cervical ripening during labor at a dose of “25 mcg inserted into the posterior vaginal fornix.”2
This brings us to the malpractice trap. While off-label use may be appropriate, off-label uses may not neatly “fit” with the substance prepared by the manufacturer. To be properly administered for cervical ripening, the available tablet of misoprostol must be cut with a pill cutter or razor prior to administration.3 Furthermore, dosage is more accurate if the tablet fragments are individually weighed after cutting.3
In this case, the discrepancy between the pill prepared by the manufacturer (100 mcg) and the dosage needed (25 mcg) appears to have caught the defendant family practitioner off guard. So the take-home message is: Use medications as supported by the standard of care—but when using a drug off label, do not assume the product supplied by the manufacturer is appropriate for use as is.
Another interesting aspect of this case is the defense strategy. Most clinicians are aware that the tort of negligence involves (1) duty, (2) breach, (3) causation, and (4) harm. However, it is more logically consistent to think of the elements in this way: (1) duty, (2) breach, (3) harm, and if harm has occurred, (4) examine causation (ie, the logical connection between breach and harm).
In malpractice cases, attorneys frequently focus on one of these specific elements. In this case, the physician’s duty of care and the harm stemming from cerebral palsy are clearly established. Thus, breach and causation take center stage.
Continue to: The defense lawyers...
The defense lawyers acknowledged there was a breach, noting the dosage was “excessive.” However, they argued that this error didn’t matter because the drug was no longer active in the patient’s body. In other words, there was no causal connection between the inappropriately high dose and the resultant uterine tachysystole and fetal distress. This is a difficult road for several reasons.
First, the chief danger of using misoprostol is uterine hyperstimulation and fetal distress. The defense would have to argue the hyperstimulation and fetal distress were coincidental and unrelated to the misoprostol—which carries a black box warning for these very adverse effects. The plaintiff’s attorney is sure to make a big deal out of the black box warning in front of the jury—noting any reasonable clinician practicing obstetrics should be aware of the risks that come with misoprostol’s use. You can almost hear the argument in summation: “It is so important, they drew a warning box around it.”
Furthermore, making the argument that the misoprostol was not in the mother’s system at the time the fetal distress started would entail dueling expert testimony about pharmacokinetics and bioavailability—concepts that are difficult for lay jurors to understand. Misoprostol has a half-life of about 20 to 40 min when administered orally and about 60 min when administered vaginally.4 We know the mother received the overdose of misoprostol at 12:24
The plaintiff’s team might counter with an expert’s explanation that misoprostol’s bioavailability is increased 2- to 3-fold with vaginal versus oral administration. It would also be observed that compared with oral administration, vaginal administration of misoprostol is associated with a slower increase in plasma concentrations but longer elevations (peaking about 1-2 hours after vaginal administration).5
At best, the defense expert would be able to argue that the serum level likely peaked 1 to 2 hours after administration (1:24-2:24
Continue to: Most jurors would...
Most jurors would take a skeptical view of the defendant’s argument that the negative outcome in this case was coincidental. Some might even be angered by it. This realization likely prompted the defense to settle this case for $9 million.
IN SUMMARY
Onion soup mix makes great soup, but it’s an even better seasoning for pot roast. Similarly, there are pharmacologic agents that are effective for conditions for which they are not formally indicated. Do not withhold judicious off-label use of medications when appropriate. However, be aware that off-label uses may require extra attention, and dosing and administration may not be consistent with the product you have on hand. Don’t hesitate to seek guidance from pharmacy colleagues when you have questions—they are an underutilized resource and are generally happy to share their expertise.
1. Cytotec [package insert]. New York, NY: Pfizer Inc; 2009.
2. Misoprostol: dosing considerations. PDR: Prescribers’ Digital Reference. www.pdr.net/drug-summary/Cytotec-misoprostol-1044#8. Accessed July 29, 2019.
3. Williams MC, Tsibris JC, Davis G, et al. Dose variation that is associated with approximated one-quarter tablet doses of misoprostol. Am J Obstet Gynecol. 2002;187(3):615-619.
4. Yount SM, Lassiter N. The pharmacology of prostaglandins for induction of labor. J Midwifery Womens Health. 2013;58(2):133-144; quiz 238-239.
5. Danielsson KG, Marions L, Rodriguez A, et al. Comparison between oral and vaginal administration of misoprostol on uterine contractility. Obstet Gynecol. 1999;93(2):275-280.
1. Cytotec [package insert]. New York, NY: Pfizer Inc; 2009.
2. Misoprostol: dosing considerations. PDR: Prescribers’ Digital Reference. www.pdr.net/drug-summary/Cytotec-misoprostol-1044#8. Accessed July 29, 2019.
3. Williams MC, Tsibris JC, Davis G, et al. Dose variation that is associated with approximated one-quarter tablet doses of misoprostol. Am J Obstet Gynecol. 2002;187(3):615-619.
4. Yount SM, Lassiter N. The pharmacology of prostaglandins for induction of labor. J Midwifery Womens Health. 2013;58(2):133-144; quiz 238-239.
5. Danielsson KG, Marions L, Rodriguez A, et al. Comparison between oral and vaginal administration of misoprostol on uterine contractility. Obstet Gynecol. 1999;93(2):275-280.
Question Marks Lead to Dollar Signs
An employee of a sawmill in Kentucky sustained paralyzing injuries when a large piece of milling equipment struck him in the back. His coworkers took him to the hospital in the back of a pickup truck.
At the time, some of the hospital’s nursing staff were on strike and had been replaced by temporary staff provided by US Nursing Corporation. A female nurse helped load the patient into a wheelchair for transfer into the hospital.
The patient was evaluated for a spinal injury; it was determined that he had sustained an L-3 burst fracture that impinged his spine. He was transferred to another hospital. However, due to the nature of his injuries, he is permanently paralyzed from the waist down.
The plaintiff presented a products liability claim against the machinery manufacturers, which was settled for $3.05 million. He later filed a medical malpractice complaint to include the nursing contractor and 3 individual nurses (1 from the contractor and 2 employed by the hospital). The complaint alleged that the nurses “failed to stabilize and immobilize” the patient when moving him from the pickup truck to the emergency department (ED), which worsened his injuries. A nurse employed by the contractor was identified as the nurse who had transferred him to the wheelchair.
The latter case was litigated for several years. On the eve of trial, the hospital settled for $2 million and the nursing contractor for $1.1 million. However, the hospital brought an indemnification claim against the nursing contractor to recover the $2 million settlement.
At the time of trial, there was a question regarding the identity of the nurse who had transferred the plaintiff from the pickup truck to the wheelchair. The US Nursing Corporation contract nurse contended she did not transfer the plaintiff to the wheelchair. Resolving the uncertainty, the jury concluded that the contract nurse was the nurse who had transferred the plaintiff.
VERDICT
At the conclusion of a 7-day trial, the jury awarded the plaintiff $2,823,522.
Continue to: COMMENTARY
COMMENTARY
Who doesn’t love a good mystery, right? Well, not everyone. Years ago, I was given a gift: a “host your own murder mystery party” game. I recently gave it away when I realized I was statistically more likely to be murdered than ever to host a “murder mystery party.” Love them or hate them, I think you will agree: Mysteries belong in novels or movies or board games. They have no place in your clinical practice.
In litigation, lawyers obsess over trivial details. I’ve attended enough malpractice depositions to see physicians, NPs, PAs, and nurses, with puzzled faces, answering seemingly nonsensical questions that appear to have no bearing on clinical matters. The clinicians respond half amused and half annoyed, through a litany of telephone logs, record access logs, chain-of-custody records, transfer center logs, recorded ambulance communications, time-stamped records, and recollections of who brought a specimen to the lab or what time someone was at the nurses’ station—all peripheral to practice. I understand the quizzical looks and sympathize with providers’ annoyance at having to answer seemingly inane questions. Yet these matters, collateral to practice, can take center stage in a legal case.
These issues form part of the puzzle: the who, what, where, when, why, and how of any case. For example
Who carried a specimen from the operating room (OR)? (Because it was sent from the OR, but the lab has no record of receiving it and knowing the identity of the runner is now key.)
What time did the attending call the hospital to alert the surgical team? (Because precise timing from surgeon’s knowledge to first incision is now at issue.)
Continue to: Where...
Where, specifically, was the culture taken from? (Because there were three wounds, and it turns out later two wounds were from a different source than the third.)
When did scrub tech A clock out of a surgery and scrub tech B clock in? (Because one of the surgical counts was wrong, and a surgical item was retained.)
Why did the patient leave against medical advice? (Because in the ED, he said he “needed to feed his cat.” This wasn’t recorded; the chart only states “patient left AMA.” During litigation, plaintiff claims he left because a nurse told him “it would be better to see your regular doctor.”)
How did a patient get a KFC value meal to eat in his hospital bed when strict oral intake was needed? (Because the hospital’s knowledge of the patient’s dietary intake is now at issue.)
I know—such a list of who, what, etc, can appear cutesy and cloying. Further, some of these trivial details are not recorded by clinicians, so why bring them up? I raise it because in your practice setting, you may be in a position to influence decision-making with regard to recording those minor details, which can become critically important later.
Continue to: In a medical malpractice case...
In a medical malpractice case, every tiny detail is potentially part of the puzzle. If a piece of the puzzle is missing, it becomes a mystery, and a mystery can become a problem. A plaintiff’s lawyer who sees question marks also sees dollar signs.
In this case, the presence of a “mystery nurse” likely kicked up enough dust to confuse the jury. Most clinicians are aware a malpractice plaintiff must prove 4 elements: (1) duty, (2) breach of duty, (3) causation, and (4) harm. The plaintiff must prove all elements by a preponderance of the evidence (ie, greater than 50% likely). Duty and damages are not at issue in this case; there was a clear patient relationship, and the plaintiff is clearly paralyzed. The plaintiff has the burden to prove elements (2) and (3): that there was a breach of the standard of care and that breach caused the plaintiff’s harm.
With respect to element (2), the plaintiff had the burden of showing that the act of putting him into the wheelchair was a breach of the standard of care. I think we’d all agree: The standard of care requires a registered nurse to recognize that a patient struck by a heavy object is at risk for spinal injury and spinal immobilization is required. The patient should have been removed from the vehicle with spinal immobilization techniques.
However, with respect to the causation element, the plaintiff would have been required to prove it was more probable than not (ie, 51% or greater) that the act of putting him into the wheelchair caused the paralysis. This is a stretch. The jury would have to believe it was at least 51% likely that the act of car-to-wheelchair transfer caused the injury—not the heavy mill equipment falling on him in the first place, not the efforts of his coworkers to move him from the scene, not the efforts of his coworkers to load him into the truck, not the bouncy ride in the back of a truck over to the hospital. The plaintiff was able to overcome a big causation hurdle because the identity of the nurse was not known.
The plaintiff would also generally have to show that the coworkers did not mislead the transferring nurse—that is, the statements made at the time of transfer would lead a reasonably skilled nurse to suspect spinal injury, halt transfer attempts, and see to it the patient’s spine was immobilized. Although doubtful, it is possible that in the split seconds when the car arrived at the ED, the initial communications were errant and a reasonable nurse would not have just cause to suspect spinal injury. However, we will never know. We don’t have testimony on what was said during transfer.
Continue to: So we don't know who...
So we don’t know who the nurse was. We don’t know what was said. We don’t know exactly how the plaintiff was transferred out of the vehicle. And those mysteries, to a jury, are suspicious.
IN SUMMARY
Any time a lawyer can draw a giant “?” on a whiteboard during summation, rest assured, someone is in trouble. That someone could be you. I’ve seen lots of question marks in my life; none carry a $1 million/$3 million malpractice policy. The presence of a mystery will transform a case that was defensible into one with unanswered questions. Those unanswered questions open the door to the suggestion or outright accusation of a cover-up. Do your best to document details and work within your system to encourage documentation. In short, don’t let the plaintiff host a mystery party at your expense.
An employee of a sawmill in Kentucky sustained paralyzing injuries when a large piece of milling equipment struck him in the back. His coworkers took him to the hospital in the back of a pickup truck.
At the time, some of the hospital’s nursing staff were on strike and had been replaced by temporary staff provided by US Nursing Corporation. A female nurse helped load the patient into a wheelchair for transfer into the hospital.
The patient was evaluated for a spinal injury; it was determined that he had sustained an L-3 burst fracture that impinged his spine. He was transferred to another hospital. However, due to the nature of his injuries, he is permanently paralyzed from the waist down.
The plaintiff presented a products liability claim against the machinery manufacturers, which was settled for $3.05 million. He later filed a medical malpractice complaint to include the nursing contractor and 3 individual nurses (1 from the contractor and 2 employed by the hospital). The complaint alleged that the nurses “failed to stabilize and immobilize” the patient when moving him from the pickup truck to the emergency department (ED), which worsened his injuries. A nurse employed by the contractor was identified as the nurse who had transferred him to the wheelchair.
The latter case was litigated for several years. On the eve of trial, the hospital settled for $2 million and the nursing contractor for $1.1 million. However, the hospital brought an indemnification claim against the nursing contractor to recover the $2 million settlement.
At the time of trial, there was a question regarding the identity of the nurse who had transferred the plaintiff from the pickup truck to the wheelchair. The US Nursing Corporation contract nurse contended she did not transfer the plaintiff to the wheelchair. Resolving the uncertainty, the jury concluded that the contract nurse was the nurse who had transferred the plaintiff.
VERDICT
At the conclusion of a 7-day trial, the jury awarded the plaintiff $2,823,522.
Continue to: COMMENTARY
COMMENTARY
Who doesn’t love a good mystery, right? Well, not everyone. Years ago, I was given a gift: a “host your own murder mystery party” game. I recently gave it away when I realized I was statistically more likely to be murdered than ever to host a “murder mystery party.” Love them or hate them, I think you will agree: Mysteries belong in novels or movies or board games. They have no place in your clinical practice.
In litigation, lawyers obsess over trivial details. I’ve attended enough malpractice depositions to see physicians, NPs, PAs, and nurses, with puzzled faces, answering seemingly nonsensical questions that appear to have no bearing on clinical matters. The clinicians respond half amused and half annoyed, through a litany of telephone logs, record access logs, chain-of-custody records, transfer center logs, recorded ambulance communications, time-stamped records, and recollections of who brought a specimen to the lab or what time someone was at the nurses’ station—all peripheral to practice. I understand the quizzical looks and sympathize with providers’ annoyance at having to answer seemingly inane questions. Yet these matters, collateral to practice, can take center stage in a legal case.
These issues form part of the puzzle: the who, what, where, when, why, and how of any case. For example
Who carried a specimen from the operating room (OR)? (Because it was sent from the OR, but the lab has no record of receiving it and knowing the identity of the runner is now key.)
What time did the attending call the hospital to alert the surgical team? (Because precise timing from surgeon’s knowledge to first incision is now at issue.)
Continue to: Where...
Where, specifically, was the culture taken from? (Because there were three wounds, and it turns out later two wounds were from a different source than the third.)
When did scrub tech A clock out of a surgery and scrub tech B clock in? (Because one of the surgical counts was wrong, and a surgical item was retained.)
Why did the patient leave against medical advice? (Because in the ED, he said he “needed to feed his cat.” This wasn’t recorded; the chart only states “patient left AMA.” During litigation, plaintiff claims he left because a nurse told him “it would be better to see your regular doctor.”)
How did a patient get a KFC value meal to eat in his hospital bed when strict oral intake was needed? (Because the hospital’s knowledge of the patient’s dietary intake is now at issue.)
I know—such a list of who, what, etc, can appear cutesy and cloying. Further, some of these trivial details are not recorded by clinicians, so why bring them up? I raise it because in your practice setting, you may be in a position to influence decision-making with regard to recording those minor details, which can become critically important later.
Continue to: In a medical malpractice case...
In a medical malpractice case, every tiny detail is potentially part of the puzzle. If a piece of the puzzle is missing, it becomes a mystery, and a mystery can become a problem. A plaintiff’s lawyer who sees question marks also sees dollar signs.
In this case, the presence of a “mystery nurse” likely kicked up enough dust to confuse the jury. Most clinicians are aware a malpractice plaintiff must prove 4 elements: (1) duty, (2) breach of duty, (3) causation, and (4) harm. The plaintiff must prove all elements by a preponderance of the evidence (ie, greater than 50% likely). Duty and damages are not at issue in this case; there was a clear patient relationship, and the plaintiff is clearly paralyzed. The plaintiff has the burden to prove elements (2) and (3): that there was a breach of the standard of care and that breach caused the plaintiff’s harm.
With respect to element (2), the plaintiff had the burden of showing that the act of putting him into the wheelchair was a breach of the standard of care. I think we’d all agree: The standard of care requires a registered nurse to recognize that a patient struck by a heavy object is at risk for spinal injury and spinal immobilization is required. The patient should have been removed from the vehicle with spinal immobilization techniques.
However, with respect to the causation element, the plaintiff would have been required to prove it was more probable than not (ie, 51% or greater) that the act of putting him into the wheelchair caused the paralysis. This is a stretch. The jury would have to believe it was at least 51% likely that the act of car-to-wheelchair transfer caused the injury—not the heavy mill equipment falling on him in the first place, not the efforts of his coworkers to move him from the scene, not the efforts of his coworkers to load him into the truck, not the bouncy ride in the back of a truck over to the hospital. The plaintiff was able to overcome a big causation hurdle because the identity of the nurse was not known.
The plaintiff would also generally have to show that the coworkers did not mislead the transferring nurse—that is, the statements made at the time of transfer would lead a reasonably skilled nurse to suspect spinal injury, halt transfer attempts, and see to it the patient’s spine was immobilized. Although doubtful, it is possible that in the split seconds when the car arrived at the ED, the initial communications were errant and a reasonable nurse would not have just cause to suspect spinal injury. However, we will never know. We don’t have testimony on what was said during transfer.
Continue to: So we don't know who...
So we don’t know who the nurse was. We don’t know what was said. We don’t know exactly how the plaintiff was transferred out of the vehicle. And those mysteries, to a jury, are suspicious.
IN SUMMARY
Any time a lawyer can draw a giant “?” on a whiteboard during summation, rest assured, someone is in trouble. That someone could be you. I’ve seen lots of question marks in my life; none carry a $1 million/$3 million malpractice policy. The presence of a mystery will transform a case that was defensible into one with unanswered questions. Those unanswered questions open the door to the suggestion or outright accusation of a cover-up. Do your best to document details and work within your system to encourage documentation. In short, don’t let the plaintiff host a mystery party at your expense.
An employee of a sawmill in Kentucky sustained paralyzing injuries when a large piece of milling equipment struck him in the back. His coworkers took him to the hospital in the back of a pickup truck.
At the time, some of the hospital’s nursing staff were on strike and had been replaced by temporary staff provided by US Nursing Corporation. A female nurse helped load the patient into a wheelchair for transfer into the hospital.
The patient was evaluated for a spinal injury; it was determined that he had sustained an L-3 burst fracture that impinged his spine. He was transferred to another hospital. However, due to the nature of his injuries, he is permanently paralyzed from the waist down.
The plaintiff presented a products liability claim against the machinery manufacturers, which was settled for $3.05 million. He later filed a medical malpractice complaint to include the nursing contractor and 3 individual nurses (1 from the contractor and 2 employed by the hospital). The complaint alleged that the nurses “failed to stabilize and immobilize” the patient when moving him from the pickup truck to the emergency department (ED), which worsened his injuries. A nurse employed by the contractor was identified as the nurse who had transferred him to the wheelchair.
The latter case was litigated for several years. On the eve of trial, the hospital settled for $2 million and the nursing contractor for $1.1 million. However, the hospital brought an indemnification claim against the nursing contractor to recover the $2 million settlement.
At the time of trial, there was a question regarding the identity of the nurse who had transferred the plaintiff from the pickup truck to the wheelchair. The US Nursing Corporation contract nurse contended she did not transfer the plaintiff to the wheelchair. Resolving the uncertainty, the jury concluded that the contract nurse was the nurse who had transferred the plaintiff.
VERDICT
At the conclusion of a 7-day trial, the jury awarded the plaintiff $2,823,522.
Continue to: COMMENTARY
COMMENTARY
Who doesn’t love a good mystery, right? Well, not everyone. Years ago, I was given a gift: a “host your own murder mystery party” game. I recently gave it away when I realized I was statistically more likely to be murdered than ever to host a “murder mystery party.” Love them or hate them, I think you will agree: Mysteries belong in novels or movies or board games. They have no place in your clinical practice.
In litigation, lawyers obsess over trivial details. I’ve attended enough malpractice depositions to see physicians, NPs, PAs, and nurses, with puzzled faces, answering seemingly nonsensical questions that appear to have no bearing on clinical matters. The clinicians respond half amused and half annoyed, through a litany of telephone logs, record access logs, chain-of-custody records, transfer center logs, recorded ambulance communications, time-stamped records, and recollections of who brought a specimen to the lab or what time someone was at the nurses’ station—all peripheral to practice. I understand the quizzical looks and sympathize with providers’ annoyance at having to answer seemingly inane questions. Yet these matters, collateral to practice, can take center stage in a legal case.
These issues form part of the puzzle: the who, what, where, when, why, and how of any case. For example
Who carried a specimen from the operating room (OR)? (Because it was sent from the OR, but the lab has no record of receiving it and knowing the identity of the runner is now key.)
What time did the attending call the hospital to alert the surgical team? (Because precise timing from surgeon’s knowledge to first incision is now at issue.)
Continue to: Where...
Where, specifically, was the culture taken from? (Because there were three wounds, and it turns out later two wounds were from a different source than the third.)
When did scrub tech A clock out of a surgery and scrub tech B clock in? (Because one of the surgical counts was wrong, and a surgical item was retained.)
Why did the patient leave against medical advice? (Because in the ED, he said he “needed to feed his cat.” This wasn’t recorded; the chart only states “patient left AMA.” During litigation, plaintiff claims he left because a nurse told him “it would be better to see your regular doctor.”)
How did a patient get a KFC value meal to eat in his hospital bed when strict oral intake was needed? (Because the hospital’s knowledge of the patient’s dietary intake is now at issue.)
I know—such a list of who, what, etc, can appear cutesy and cloying. Further, some of these trivial details are not recorded by clinicians, so why bring them up? I raise it because in your practice setting, you may be in a position to influence decision-making with regard to recording those minor details, which can become critically important later.
Continue to: In a medical malpractice case...
In a medical malpractice case, every tiny detail is potentially part of the puzzle. If a piece of the puzzle is missing, it becomes a mystery, and a mystery can become a problem. A plaintiff’s lawyer who sees question marks also sees dollar signs.
In this case, the presence of a “mystery nurse” likely kicked up enough dust to confuse the jury. Most clinicians are aware a malpractice plaintiff must prove 4 elements: (1) duty, (2) breach of duty, (3) causation, and (4) harm. The plaintiff must prove all elements by a preponderance of the evidence (ie, greater than 50% likely). Duty and damages are not at issue in this case; there was a clear patient relationship, and the plaintiff is clearly paralyzed. The plaintiff has the burden to prove elements (2) and (3): that there was a breach of the standard of care and that breach caused the plaintiff’s harm.
With respect to element (2), the plaintiff had the burden of showing that the act of putting him into the wheelchair was a breach of the standard of care. I think we’d all agree: The standard of care requires a registered nurse to recognize that a patient struck by a heavy object is at risk for spinal injury and spinal immobilization is required. The patient should have been removed from the vehicle with spinal immobilization techniques.
However, with respect to the causation element, the plaintiff would have been required to prove it was more probable than not (ie, 51% or greater) that the act of putting him into the wheelchair caused the paralysis. This is a stretch. The jury would have to believe it was at least 51% likely that the act of car-to-wheelchair transfer caused the injury—not the heavy mill equipment falling on him in the first place, not the efforts of his coworkers to move him from the scene, not the efforts of his coworkers to load him into the truck, not the bouncy ride in the back of a truck over to the hospital. The plaintiff was able to overcome a big causation hurdle because the identity of the nurse was not known.
The plaintiff would also generally have to show that the coworkers did not mislead the transferring nurse—that is, the statements made at the time of transfer would lead a reasonably skilled nurse to suspect spinal injury, halt transfer attempts, and see to it the patient’s spine was immobilized. Although doubtful, it is possible that in the split seconds when the car arrived at the ED, the initial communications were errant and a reasonable nurse would not have just cause to suspect spinal injury. However, we will never know. We don’t have testimony on what was said during transfer.
Continue to: So we don't know who...
So we don’t know who the nurse was. We don’t know what was said. We don’t know exactly how the plaintiff was transferred out of the vehicle. And those mysteries, to a jury, are suspicious.
IN SUMMARY
Any time a lawyer can draw a giant “?” on a whiteboard during summation, rest assured, someone is in trouble. That someone could be you. I’ve seen lots of question marks in my life; none carry a $1 million/$3 million malpractice policy. The presence of a mystery will transform a case that was defensible into one with unanswered questions. Those unanswered questions open the door to the suggestion or outright accusation of a cover-up. Do your best to document details and work within your system to encourage documentation. In short, don’t let the plaintiff host a mystery party at your expense.
Sometimes You Should Order Another Test
On August 7, 2012, a 44-year-old electrical engineer sustained a knee injury. He initially sought treatment at an emergency department (ED) in Indiana, where he lived, and was released with a splint on his leg.
On August 9, the patient presented to an Illinois medical clinic. He was seen by a physician who referred the patient to another physician at the clinic for evaluation for surgery. The procedure, to repair ruptured ligaments in the patient’s left knee, was scheduled for August 16.
After returning home, the patient called the first physician with complaints that his splinted left knee, calf, and leg felt hot. The physician sent approval for the patient to undergo Doppler imaging of his left leg at a hospital in Indiana. The Doppler was performed on August 10, and the results were sent to the referring physician. The imaging was negative for any abnormalities.
On the morning of August 13, the patient presented to the Illinois medical clinic for presurgical clearance. The examination was performed by an NP, and then the patient had a presurgical consultation with the surgeon. The patient allegedly reported to the NP and the surgeon that he had continuing pain, swelling, and heat sensation in his left leg. Relying on the Doppler performed a few days earlier, the surgeon told the patient that these symptoms were related to the knee trauma he had sustained. No additional Doppler imaging was ordered.
On August 16, the patient was anesthetized in preparation for surgery and soon thereafter suffered a pulmonary embolism (PE) when a deep vein thrombosis (DVT) in his left leg detached and traveled to his lung. He went into pulmonary arrest, coded, and was declared brain dead within hours of arriving for surgery.
The decedent left behind a wife and 2 daughters, ages 12 and 14. His wife, as the administrator of her husband’s estate, sued the NP and her employer. The 2 orthopedic physicians, a treating cardiologist, and their employer were named as respondents in discovery. The physicians’ employer was ultimately added as a defendant, along with the NP’s employer. Prior to trial, the 3 physicians and the NP were dismissed from the case. The matter proceeded against the 2 employing organizations.
The estate alleged that the NP and operating surgeon/physician, each as agents of their respective employers, failed to order a second Doppler image of the decedent’s left leg during presurgical clearance procedures and in the 4 days leading up to the surgery. The estate alleged that a second Doppler was needed because the decedent had complaints that were consistent with DVT—such as continuing pain, swelling, and heat sensation—in his left leg at the August 13 visit. The estate argued that the failure to order a second Doppler led to a failure to diagnose the DVT from which the decedent was suffering symptoms. The estate alleged that the earlier Doppler was performed too soon after the decedent’s injury to show a DVT, as DVTs do not develop immediately after trauma but grow and spread over time.
Continue to: While pain, swelling, and warmth...
While pain, swelling, and warmth/heat sensation are symptoms that accompany trauma, the estate asserted that these are also symptoms of a DVT and that the surgeon, as a reasonable orthopedic physician, should have tested the decedent for a DVT on August 13, on the morning of the surgery, or any day in between and that he also should have ordered a hematologic consult. The estate’s orthopedic surgery expert testified that the surgeon violated the standard of care by failing to appreciate the symptoms and risk factors the decedent was experiencing. The expert testified that the decedent had 4 of 5 high-risk factors for a DVT: Although there was no family history of DVT, the decedent had sustained leg trauma, he was older than 40, his leg was immobilized, and he was considered obese (BMI > 30).
The same orthopedist further opined that a Doppler performed on August 13 more likely than not would have shown the DVT, and the August 16 knee surgery would have been delayed until it was treated. He added that the failure to perform a second Doppler before surgery constituted negligence that caused the decedent’s death. The estate’s hematology expert testified that the decedent was a candidate for prophylactic anticoagulation on August 13 and, if a Doppler had been performed, the need for such medication would have been discovered.
The defense argued that the decedent’s signs and symptoms did not change following the Doppler on August 10 and, therefore, there was no reason for the surgeon to order a second Doppler prior to performing surgery. The defense further argued that the NP, in the scope of her practice, was not allowed to order a Doppler, knew that the surgeon would be seeing the decedent during the same visit, and could rely on the surgeon to order the necessary presurgical tests. The defense’s orthopedics expert testified that, unless there was an increase in signs and/or symptoms, the standard of care did not require the surgeon to order another Doppler. The expert further testified that the surgeon did not place the decedent on a presurgical anticoagulant because this would have increased his risk for bleeding. The defense’s hematology expert testified that there was no guarantee an anticoagulant would have prevented the PE because of the large size of the clot. He further stated that the decedent was not a candidate for prophylactic anticoagulants prior to surgery because the Doppler was negative for clotting, and there was no increase in his symptoms after the Doppler was performed.
The estate’s NP expert testified that, while performing the presurgical clearance, the defendant NP failed to obtain the Doppler history or a full description of the patient’s symptoms (which resulted from a DVT) and failed to order a Doppler. The defense’s NP expert testified that, based on the defendant NP’s testimony, she was not allowed to order a Doppler, and that, as an NP, she would have had a document in her credentials setting forth what she can and cannot recommend. Since such a document was not produced, this could not be determined, she opined.
VERDICT
After an 11-day trial and 2.5 hours of deliberation, the jury found in favor of the plaintiff estate. The jury found the NP’s employer not liable but the physicians’ employer responsible. Damages totaling $5,511,567 were awarded to the estate.
Continue to: COMMENTARY
COMMENTARY
If the Grim Reaper had an Employee of the Month plaque, DVT would proudly see its name etched thereon about 8 months of the year. Missed bleeding takes second place (muttering under its breath, promising to “up its game” next year). You may think the pathophysiology is boring. DVTs don’t care. They just kill.
While these comments may seem flip, the intention is not to minimize the threat posed by DVTs but rather to underscore it. DVT/PE is one of the most missed clinical entities giving rise to litigation; it is legally problematic because its development is often foreseeable. There is a clear setup (eg, surgery or immobilization) and a disease process that is easily understood by even lay people. Jurors understand the concept of a “clot”—if you aren’t moving much, you are apt to get a “clog” and if the clog is discovered and “dissolved” the threat goes away, but if it “breaks loose” it could kill. Jurors need not understand highbrow concepts such as the renin-angiotensin-aldosterone system or the hypothalamic pituitary adrenal axis; it is a clog. This is common sense; during deliberations, jurors will reason that if they “get it,” why couldn’t you?
To add insult to (endothelial) injury, DVT and PE are generally curable; most patients recover fully with proper treatment. Plaintiff’s counsel can trot out the tried-and-true argument: “If a simple, painless ultrasound test had been done, [the patient] would be having dinner with his family tonight.” Furthermore, affected patients are apt to be on the younger side, with a lengthy employment life ahead of them—potentially giving rise to substantial loss-of-earnings damages.
In the case presented here, we are told that the decedent complained of “continuing pain, swelling, and heat sensation” when he saw both an NP and a surgeon for presurgical clearance. We do not know if his leg was examined, but if it had been, the positive and negative findings likely would have been discussed in the case synopsis. It appears the NP and the surgeon saw the leg in the immobilizer and decided to rely on the previous negative Doppler.
First, let’s address the diagnosis of DVT: We should all realize that Homan’s sign sucks. You have permission to elicit Homan’s sign if you are in a museum for antiquated medicine (where other artifacts include AZT monotherapy, bite-and-swallow nifedipine for hypertensive urgency, and meperidine for sphincter of Oddi spasm). Everywhere else on the planet, Homan’s sign has always been bad and is certainly not the standard of care. If you are still attempting to elicit Homan’s sign—cut it out. It is the 1970s leisure suit in your closet: never was any good, never is going to be. Declutter your clinical test arsenal and KonMari Homan’s sign straight to the junk pile.
Continue to: A diagnostic tool...
A diagnostic tool that works better is the Wells’ Criteria, which operates on a points system (with 3-8 points indicating high probability of DVT, 1-2 points indicating moderate probability, and less than 1 point indicating low probability).1 Patients are assessed according to the following criteria:
- Paralysis, paresis, or recent orthopedic casting of lower extremity (1 pt)
- Recently bedridden (> 3 d) or major surgery within past 4 weeks (1 pt)
- Localized tenderness in deep vein system (1 pt)
- Swelling of entire leg (1 pt)
- Calf swelling 3 cm greater than other leg (measured 10 cm below the tibial tuberosity) (1 pt)
- Pitting edema greater in the symptomatic leg (1 pt)
- Collateral nonvaricose superficial veins (1 pt)
- Active cancer or cancer treated within 6 months (1 pt)
- Alternative diagnosis more likely than DVT (Baker cyst, cellulitis, muscle damage, superficial venous thrombosis, postphlebitic syndrome, inguinal lymphadenopathy, external venous compression) (–2 pts).1
Moving through the Wells’ score system, we don’t have enough clinical data input for this patient. We do know he had leg pain and possibly swelling (1 pt). His knee was immobilized (albeit without plaster) (1 pt). We don’t know how “bedridden” he was. I’ll argue we should not deduct for “an alternative diagnosis more likely” because the decedent injured his knee and we can expect knee pain and knee swelling, not symptoms and findings involving the entire leg. So this patient would score at least 1 point, possibly 2, and thus be stratified as “moderate probability.”
There was an initial suspicion of DVT in this patient, and a Doppler was ordered on August 10. The patient’s symptoms persisted. However, in light of the negative Doppler results, the continued symptoms were attributed to the knee derangement and not a DVT.
Which brings us to the first malpractice trap: reliance on a prior negative study to rule out a dynamic condition. For any condition that can evolve, do not hesitate to order a repeat test when needed. DVT is a dynamic process; given the right clinical setup (in this case, immobility and ongoing/increasing symptoms), a clinician should not be bashful about ordering a follow-up study. As providers, we recognize the static nature of certain studies and have no reservations about ordering serial complete blood counts or a repeat chest film. Yet we are more reluctant to order repeat studies for equally dynamic disease processes—even when they are required by the standard of care. Here, reliance on a 3-day-old Doppler was problematic. Don’t rely on an old study if the disease under suspicion evolves rapidly.
The second trap: Do not allow yourself to be scolded (or engage in self-scolding) if a correctly ordered test is negative. A clinical decision is correct if it is based on science and in the interest of safeguarding the patient. Don’t buy into the trap that your decision needs to be validated by a positive result. Here, the persisting or worsening leg pain with entire leg swelling warranted a new study—even if the result was expected to be negative.
Continue to: When your decision to order...
When your decision to order such a test is challenged, my favorite rhetorical defense is “Those are some pretty big dice to roll.” That is what you are doing if you skip a test that should be ordered. The bounceback kid with a prior negative lumbar puncture, who now appears toxic, needs a repeat tap. Why? Because you cannot afford to miss meningitis—that would be a risky roll of the dice.
One final point about this case: The NP argued “she was not allowed to order a Doppler” and her NP expert made the argument that “she would have had a document in her credentials setting forth what she can and cannot recommend.” The expert testified she could not find such a document and “could not determine” whether the defendant NP could “recommend” that test. I don’t fault the tactical decision to use this argument, in this case, when the surgeon also saw the patient on the same day. However, we should all recognize this will not normally work. A clinician cannot credibly argue she is not “credentialed” to recommend a course of action she can’t presently deliver.
Consider a clinician employed in an urgent care center without direct access to order CT. She evaluates an 80-year-old woman on warfarin who slipped and struck her head on a marble table. The standard of care requires a CT scan (likely several) to rule out an intracranial bleed. The urgent care clinician cannot send the patient away and later claim she was “not credentialed” to recommend CT imaging to rule out an intracranial bleed. As a matter of the standard of care, our hypothetical clinician would be duty bound to advise the patient of the risk for bleeding and then take steps to arrange for that care—even though she is not in a position to personally deliver it.
IN SUMMARY
Protect your patients from evolving cases by ordering updated tests. Do not be afraid of a negative result. Instead, fear the Reaper; keep him away from your patients. Let him get his “more cowbell” somewhere else.
1. Wells PS, Anderson DR, Bormanis J, et al. Value of assessment of pretest probability of deep-vein thrombosis in clinical management. Lancet. 1997;350(9094):1795-1798.
On August 7, 2012, a 44-year-old electrical engineer sustained a knee injury. He initially sought treatment at an emergency department (ED) in Indiana, where he lived, and was released with a splint on his leg.
On August 9, the patient presented to an Illinois medical clinic. He was seen by a physician who referred the patient to another physician at the clinic for evaluation for surgery. The procedure, to repair ruptured ligaments in the patient’s left knee, was scheduled for August 16.
After returning home, the patient called the first physician with complaints that his splinted left knee, calf, and leg felt hot. The physician sent approval for the patient to undergo Doppler imaging of his left leg at a hospital in Indiana. The Doppler was performed on August 10, and the results were sent to the referring physician. The imaging was negative for any abnormalities.
On the morning of August 13, the patient presented to the Illinois medical clinic for presurgical clearance. The examination was performed by an NP, and then the patient had a presurgical consultation with the surgeon. The patient allegedly reported to the NP and the surgeon that he had continuing pain, swelling, and heat sensation in his left leg. Relying on the Doppler performed a few days earlier, the surgeon told the patient that these symptoms were related to the knee trauma he had sustained. No additional Doppler imaging was ordered.
On August 16, the patient was anesthetized in preparation for surgery and soon thereafter suffered a pulmonary embolism (PE) when a deep vein thrombosis (DVT) in his left leg detached and traveled to his lung. He went into pulmonary arrest, coded, and was declared brain dead within hours of arriving for surgery.
The decedent left behind a wife and 2 daughters, ages 12 and 14. His wife, as the administrator of her husband’s estate, sued the NP and her employer. The 2 orthopedic physicians, a treating cardiologist, and their employer were named as respondents in discovery. The physicians’ employer was ultimately added as a defendant, along with the NP’s employer. Prior to trial, the 3 physicians and the NP were dismissed from the case. The matter proceeded against the 2 employing organizations.
The estate alleged that the NP and operating surgeon/physician, each as agents of their respective employers, failed to order a second Doppler image of the decedent’s left leg during presurgical clearance procedures and in the 4 days leading up to the surgery. The estate alleged that a second Doppler was needed because the decedent had complaints that were consistent with DVT—such as continuing pain, swelling, and heat sensation—in his left leg at the August 13 visit. The estate argued that the failure to order a second Doppler led to a failure to diagnose the DVT from which the decedent was suffering symptoms. The estate alleged that the earlier Doppler was performed too soon after the decedent’s injury to show a DVT, as DVTs do not develop immediately after trauma but grow and spread over time.
Continue to: While pain, swelling, and warmth...
While pain, swelling, and warmth/heat sensation are symptoms that accompany trauma, the estate asserted that these are also symptoms of a DVT and that the surgeon, as a reasonable orthopedic physician, should have tested the decedent for a DVT on August 13, on the morning of the surgery, or any day in between and that he also should have ordered a hematologic consult. The estate’s orthopedic surgery expert testified that the surgeon violated the standard of care by failing to appreciate the symptoms and risk factors the decedent was experiencing. The expert testified that the decedent had 4 of 5 high-risk factors for a DVT: Although there was no family history of DVT, the decedent had sustained leg trauma, he was older than 40, his leg was immobilized, and he was considered obese (BMI > 30).
The same orthopedist further opined that a Doppler performed on August 13 more likely than not would have shown the DVT, and the August 16 knee surgery would have been delayed until it was treated. He added that the failure to perform a second Doppler before surgery constituted negligence that caused the decedent’s death. The estate’s hematology expert testified that the decedent was a candidate for prophylactic anticoagulation on August 13 and, if a Doppler had been performed, the need for such medication would have been discovered.
The defense argued that the decedent’s signs and symptoms did not change following the Doppler on August 10 and, therefore, there was no reason for the surgeon to order a second Doppler prior to performing surgery. The defense further argued that the NP, in the scope of her practice, was not allowed to order a Doppler, knew that the surgeon would be seeing the decedent during the same visit, and could rely on the surgeon to order the necessary presurgical tests. The defense’s orthopedics expert testified that, unless there was an increase in signs and/or symptoms, the standard of care did not require the surgeon to order another Doppler. The expert further testified that the surgeon did not place the decedent on a presurgical anticoagulant because this would have increased his risk for bleeding. The defense’s hematology expert testified that there was no guarantee an anticoagulant would have prevented the PE because of the large size of the clot. He further stated that the decedent was not a candidate for prophylactic anticoagulants prior to surgery because the Doppler was negative for clotting, and there was no increase in his symptoms after the Doppler was performed.
The estate’s NP expert testified that, while performing the presurgical clearance, the defendant NP failed to obtain the Doppler history or a full description of the patient’s symptoms (which resulted from a DVT) and failed to order a Doppler. The defense’s NP expert testified that, based on the defendant NP’s testimony, she was not allowed to order a Doppler, and that, as an NP, she would have had a document in her credentials setting forth what she can and cannot recommend. Since such a document was not produced, this could not be determined, she opined.
VERDICT
After an 11-day trial and 2.5 hours of deliberation, the jury found in favor of the plaintiff estate. The jury found the NP’s employer not liable but the physicians’ employer responsible. Damages totaling $5,511,567 were awarded to the estate.
Continue to: COMMENTARY
COMMENTARY
If the Grim Reaper had an Employee of the Month plaque, DVT would proudly see its name etched thereon about 8 months of the year. Missed bleeding takes second place (muttering under its breath, promising to “up its game” next year). You may think the pathophysiology is boring. DVTs don’t care. They just kill.
While these comments may seem flip, the intention is not to minimize the threat posed by DVTs but rather to underscore it. DVT/PE is one of the most missed clinical entities giving rise to litigation; it is legally problematic because its development is often foreseeable. There is a clear setup (eg, surgery or immobilization) and a disease process that is easily understood by even lay people. Jurors understand the concept of a “clot”—if you aren’t moving much, you are apt to get a “clog” and if the clog is discovered and “dissolved” the threat goes away, but if it “breaks loose” it could kill. Jurors need not understand highbrow concepts such as the renin-angiotensin-aldosterone system or the hypothalamic pituitary adrenal axis; it is a clog. This is common sense; during deliberations, jurors will reason that if they “get it,” why couldn’t you?
To add insult to (endothelial) injury, DVT and PE are generally curable; most patients recover fully with proper treatment. Plaintiff’s counsel can trot out the tried-and-true argument: “If a simple, painless ultrasound test had been done, [the patient] would be having dinner with his family tonight.” Furthermore, affected patients are apt to be on the younger side, with a lengthy employment life ahead of them—potentially giving rise to substantial loss-of-earnings damages.
In the case presented here, we are told that the decedent complained of “continuing pain, swelling, and heat sensation” when he saw both an NP and a surgeon for presurgical clearance. We do not know if his leg was examined, but if it had been, the positive and negative findings likely would have been discussed in the case synopsis. It appears the NP and the surgeon saw the leg in the immobilizer and decided to rely on the previous negative Doppler.
First, let’s address the diagnosis of DVT: We should all realize that Homan’s sign sucks. You have permission to elicit Homan’s sign if you are in a museum for antiquated medicine (where other artifacts include AZT monotherapy, bite-and-swallow nifedipine for hypertensive urgency, and meperidine for sphincter of Oddi spasm). Everywhere else on the planet, Homan’s sign has always been bad and is certainly not the standard of care. If you are still attempting to elicit Homan’s sign—cut it out. It is the 1970s leisure suit in your closet: never was any good, never is going to be. Declutter your clinical test arsenal and KonMari Homan’s sign straight to the junk pile.
Continue to: A diagnostic tool...
A diagnostic tool that works better is the Wells’ Criteria, which operates on a points system (with 3-8 points indicating high probability of DVT, 1-2 points indicating moderate probability, and less than 1 point indicating low probability).1 Patients are assessed according to the following criteria:
- Paralysis, paresis, or recent orthopedic casting of lower extremity (1 pt)
- Recently bedridden (> 3 d) or major surgery within past 4 weeks (1 pt)
- Localized tenderness in deep vein system (1 pt)
- Swelling of entire leg (1 pt)
- Calf swelling 3 cm greater than other leg (measured 10 cm below the tibial tuberosity) (1 pt)
- Pitting edema greater in the symptomatic leg (1 pt)
- Collateral nonvaricose superficial veins (1 pt)
- Active cancer or cancer treated within 6 months (1 pt)
- Alternative diagnosis more likely than DVT (Baker cyst, cellulitis, muscle damage, superficial venous thrombosis, postphlebitic syndrome, inguinal lymphadenopathy, external venous compression) (–2 pts).1
Moving through the Wells’ score system, we don’t have enough clinical data input for this patient. We do know he had leg pain and possibly swelling (1 pt). His knee was immobilized (albeit without plaster) (1 pt). We don’t know how “bedridden” he was. I’ll argue we should not deduct for “an alternative diagnosis more likely” because the decedent injured his knee and we can expect knee pain and knee swelling, not symptoms and findings involving the entire leg. So this patient would score at least 1 point, possibly 2, and thus be stratified as “moderate probability.”
There was an initial suspicion of DVT in this patient, and a Doppler was ordered on August 10. The patient’s symptoms persisted. However, in light of the negative Doppler results, the continued symptoms were attributed to the knee derangement and not a DVT.
Which brings us to the first malpractice trap: reliance on a prior negative study to rule out a dynamic condition. For any condition that can evolve, do not hesitate to order a repeat test when needed. DVT is a dynamic process; given the right clinical setup (in this case, immobility and ongoing/increasing symptoms), a clinician should not be bashful about ordering a follow-up study. As providers, we recognize the static nature of certain studies and have no reservations about ordering serial complete blood counts or a repeat chest film. Yet we are more reluctant to order repeat studies for equally dynamic disease processes—even when they are required by the standard of care. Here, reliance on a 3-day-old Doppler was problematic. Don’t rely on an old study if the disease under suspicion evolves rapidly.
The second trap: Do not allow yourself to be scolded (or engage in self-scolding) if a correctly ordered test is negative. A clinical decision is correct if it is based on science and in the interest of safeguarding the patient. Don’t buy into the trap that your decision needs to be validated by a positive result. Here, the persisting or worsening leg pain with entire leg swelling warranted a new study—even if the result was expected to be negative.
Continue to: When your decision to order...
When your decision to order such a test is challenged, my favorite rhetorical defense is “Those are some pretty big dice to roll.” That is what you are doing if you skip a test that should be ordered. The bounceback kid with a prior negative lumbar puncture, who now appears toxic, needs a repeat tap. Why? Because you cannot afford to miss meningitis—that would be a risky roll of the dice.
One final point about this case: The NP argued “she was not allowed to order a Doppler” and her NP expert made the argument that “she would have had a document in her credentials setting forth what she can and cannot recommend.” The expert testified she could not find such a document and “could not determine” whether the defendant NP could “recommend” that test. I don’t fault the tactical decision to use this argument, in this case, when the surgeon also saw the patient on the same day. However, we should all recognize this will not normally work. A clinician cannot credibly argue she is not “credentialed” to recommend a course of action she can’t presently deliver.
Consider a clinician employed in an urgent care center without direct access to order CT. She evaluates an 80-year-old woman on warfarin who slipped and struck her head on a marble table. The standard of care requires a CT scan (likely several) to rule out an intracranial bleed. The urgent care clinician cannot send the patient away and later claim she was “not credentialed” to recommend CT imaging to rule out an intracranial bleed. As a matter of the standard of care, our hypothetical clinician would be duty bound to advise the patient of the risk for bleeding and then take steps to arrange for that care—even though she is not in a position to personally deliver it.
IN SUMMARY
Protect your patients from evolving cases by ordering updated tests. Do not be afraid of a negative result. Instead, fear the Reaper; keep him away from your patients. Let him get his “more cowbell” somewhere else.
On August 7, 2012, a 44-year-old electrical engineer sustained a knee injury. He initially sought treatment at an emergency department (ED) in Indiana, where he lived, and was released with a splint on his leg.
On August 9, the patient presented to an Illinois medical clinic. He was seen by a physician who referred the patient to another physician at the clinic for evaluation for surgery. The procedure, to repair ruptured ligaments in the patient’s left knee, was scheduled for August 16.
After returning home, the patient called the first physician with complaints that his splinted left knee, calf, and leg felt hot. The physician sent approval for the patient to undergo Doppler imaging of his left leg at a hospital in Indiana. The Doppler was performed on August 10, and the results were sent to the referring physician. The imaging was negative for any abnormalities.
On the morning of August 13, the patient presented to the Illinois medical clinic for presurgical clearance. The examination was performed by an NP, and then the patient had a presurgical consultation with the surgeon. The patient allegedly reported to the NP and the surgeon that he had continuing pain, swelling, and heat sensation in his left leg. Relying on the Doppler performed a few days earlier, the surgeon told the patient that these symptoms were related to the knee trauma he had sustained. No additional Doppler imaging was ordered.
On August 16, the patient was anesthetized in preparation for surgery and soon thereafter suffered a pulmonary embolism (PE) when a deep vein thrombosis (DVT) in his left leg detached and traveled to his lung. He went into pulmonary arrest, coded, and was declared brain dead within hours of arriving for surgery.
The decedent left behind a wife and 2 daughters, ages 12 and 14. His wife, as the administrator of her husband’s estate, sued the NP and her employer. The 2 orthopedic physicians, a treating cardiologist, and their employer were named as respondents in discovery. The physicians’ employer was ultimately added as a defendant, along with the NP’s employer. Prior to trial, the 3 physicians and the NP were dismissed from the case. The matter proceeded against the 2 employing organizations.
The estate alleged that the NP and operating surgeon/physician, each as agents of their respective employers, failed to order a second Doppler image of the decedent’s left leg during presurgical clearance procedures and in the 4 days leading up to the surgery. The estate alleged that a second Doppler was needed because the decedent had complaints that were consistent with DVT—such as continuing pain, swelling, and heat sensation—in his left leg at the August 13 visit. The estate argued that the failure to order a second Doppler led to a failure to diagnose the DVT from which the decedent was suffering symptoms. The estate alleged that the earlier Doppler was performed too soon after the decedent’s injury to show a DVT, as DVTs do not develop immediately after trauma but grow and spread over time.
Continue to: While pain, swelling, and warmth...
While pain, swelling, and warmth/heat sensation are symptoms that accompany trauma, the estate asserted that these are also symptoms of a DVT and that the surgeon, as a reasonable orthopedic physician, should have tested the decedent for a DVT on August 13, on the morning of the surgery, or any day in between and that he also should have ordered a hematologic consult. The estate’s orthopedic surgery expert testified that the surgeon violated the standard of care by failing to appreciate the symptoms and risk factors the decedent was experiencing. The expert testified that the decedent had 4 of 5 high-risk factors for a DVT: Although there was no family history of DVT, the decedent had sustained leg trauma, he was older than 40, his leg was immobilized, and he was considered obese (BMI > 30).
The same orthopedist further opined that a Doppler performed on August 13 more likely than not would have shown the DVT, and the August 16 knee surgery would have been delayed until it was treated. He added that the failure to perform a second Doppler before surgery constituted negligence that caused the decedent’s death. The estate’s hematology expert testified that the decedent was a candidate for prophylactic anticoagulation on August 13 and, if a Doppler had been performed, the need for such medication would have been discovered.
The defense argued that the decedent’s signs and symptoms did not change following the Doppler on August 10 and, therefore, there was no reason for the surgeon to order a second Doppler prior to performing surgery. The defense further argued that the NP, in the scope of her practice, was not allowed to order a Doppler, knew that the surgeon would be seeing the decedent during the same visit, and could rely on the surgeon to order the necessary presurgical tests. The defense’s orthopedics expert testified that, unless there was an increase in signs and/or symptoms, the standard of care did not require the surgeon to order another Doppler. The expert further testified that the surgeon did not place the decedent on a presurgical anticoagulant because this would have increased his risk for bleeding. The defense’s hematology expert testified that there was no guarantee an anticoagulant would have prevented the PE because of the large size of the clot. He further stated that the decedent was not a candidate for prophylactic anticoagulants prior to surgery because the Doppler was negative for clotting, and there was no increase in his symptoms after the Doppler was performed.
The estate’s NP expert testified that, while performing the presurgical clearance, the defendant NP failed to obtain the Doppler history or a full description of the patient’s symptoms (which resulted from a DVT) and failed to order a Doppler. The defense’s NP expert testified that, based on the defendant NP’s testimony, she was not allowed to order a Doppler, and that, as an NP, she would have had a document in her credentials setting forth what she can and cannot recommend. Since such a document was not produced, this could not be determined, she opined.
VERDICT
After an 11-day trial and 2.5 hours of deliberation, the jury found in favor of the plaintiff estate. The jury found the NP’s employer not liable but the physicians’ employer responsible. Damages totaling $5,511,567 were awarded to the estate.
Continue to: COMMENTARY
COMMENTARY
If the Grim Reaper had an Employee of the Month plaque, DVT would proudly see its name etched thereon about 8 months of the year. Missed bleeding takes second place (muttering under its breath, promising to “up its game” next year). You may think the pathophysiology is boring. DVTs don’t care. They just kill.
While these comments may seem flip, the intention is not to minimize the threat posed by DVTs but rather to underscore it. DVT/PE is one of the most missed clinical entities giving rise to litigation; it is legally problematic because its development is often foreseeable. There is a clear setup (eg, surgery or immobilization) and a disease process that is easily understood by even lay people. Jurors understand the concept of a “clot”—if you aren’t moving much, you are apt to get a “clog” and if the clog is discovered and “dissolved” the threat goes away, but if it “breaks loose” it could kill. Jurors need not understand highbrow concepts such as the renin-angiotensin-aldosterone system or the hypothalamic pituitary adrenal axis; it is a clog. This is common sense; during deliberations, jurors will reason that if they “get it,” why couldn’t you?
To add insult to (endothelial) injury, DVT and PE are generally curable; most patients recover fully with proper treatment. Plaintiff’s counsel can trot out the tried-and-true argument: “If a simple, painless ultrasound test had been done, [the patient] would be having dinner with his family tonight.” Furthermore, affected patients are apt to be on the younger side, with a lengthy employment life ahead of them—potentially giving rise to substantial loss-of-earnings damages.
In the case presented here, we are told that the decedent complained of “continuing pain, swelling, and heat sensation” when he saw both an NP and a surgeon for presurgical clearance. We do not know if his leg was examined, but if it had been, the positive and negative findings likely would have been discussed in the case synopsis. It appears the NP and the surgeon saw the leg in the immobilizer and decided to rely on the previous negative Doppler.
First, let’s address the diagnosis of DVT: We should all realize that Homan’s sign sucks. You have permission to elicit Homan’s sign if you are in a museum for antiquated medicine (where other artifacts include AZT monotherapy, bite-and-swallow nifedipine for hypertensive urgency, and meperidine for sphincter of Oddi spasm). Everywhere else on the planet, Homan’s sign has always been bad and is certainly not the standard of care. If you are still attempting to elicit Homan’s sign—cut it out. It is the 1970s leisure suit in your closet: never was any good, never is going to be. Declutter your clinical test arsenal and KonMari Homan’s sign straight to the junk pile.
Continue to: A diagnostic tool...
A diagnostic tool that works better is the Wells’ Criteria, which operates on a points system (with 3-8 points indicating high probability of DVT, 1-2 points indicating moderate probability, and less than 1 point indicating low probability).1 Patients are assessed according to the following criteria:
- Paralysis, paresis, or recent orthopedic casting of lower extremity (1 pt)
- Recently bedridden (> 3 d) or major surgery within past 4 weeks (1 pt)
- Localized tenderness in deep vein system (1 pt)
- Swelling of entire leg (1 pt)
- Calf swelling 3 cm greater than other leg (measured 10 cm below the tibial tuberosity) (1 pt)
- Pitting edema greater in the symptomatic leg (1 pt)
- Collateral nonvaricose superficial veins (1 pt)
- Active cancer or cancer treated within 6 months (1 pt)
- Alternative diagnosis more likely than DVT (Baker cyst, cellulitis, muscle damage, superficial venous thrombosis, postphlebitic syndrome, inguinal lymphadenopathy, external venous compression) (–2 pts).1
Moving through the Wells’ score system, we don’t have enough clinical data input for this patient. We do know he had leg pain and possibly swelling (1 pt). His knee was immobilized (albeit without plaster) (1 pt). We don’t know how “bedridden” he was. I’ll argue we should not deduct for “an alternative diagnosis more likely” because the decedent injured his knee and we can expect knee pain and knee swelling, not symptoms and findings involving the entire leg. So this patient would score at least 1 point, possibly 2, and thus be stratified as “moderate probability.”
There was an initial suspicion of DVT in this patient, and a Doppler was ordered on August 10. The patient’s symptoms persisted. However, in light of the negative Doppler results, the continued symptoms were attributed to the knee derangement and not a DVT.
Which brings us to the first malpractice trap: reliance on a prior negative study to rule out a dynamic condition. For any condition that can evolve, do not hesitate to order a repeat test when needed. DVT is a dynamic process; given the right clinical setup (in this case, immobility and ongoing/increasing symptoms), a clinician should not be bashful about ordering a follow-up study. As providers, we recognize the static nature of certain studies and have no reservations about ordering serial complete blood counts or a repeat chest film. Yet we are more reluctant to order repeat studies for equally dynamic disease processes—even when they are required by the standard of care. Here, reliance on a 3-day-old Doppler was problematic. Don’t rely on an old study if the disease under suspicion evolves rapidly.
The second trap: Do not allow yourself to be scolded (or engage in self-scolding) if a correctly ordered test is negative. A clinical decision is correct if it is based on science and in the interest of safeguarding the patient. Don’t buy into the trap that your decision needs to be validated by a positive result. Here, the persisting or worsening leg pain with entire leg swelling warranted a new study—even if the result was expected to be negative.
Continue to: When your decision to order...
When your decision to order such a test is challenged, my favorite rhetorical defense is “Those are some pretty big dice to roll.” That is what you are doing if you skip a test that should be ordered. The bounceback kid with a prior negative lumbar puncture, who now appears toxic, needs a repeat tap. Why? Because you cannot afford to miss meningitis—that would be a risky roll of the dice.
One final point about this case: The NP argued “she was not allowed to order a Doppler” and her NP expert made the argument that “she would have had a document in her credentials setting forth what she can and cannot recommend.” The expert testified she could not find such a document and “could not determine” whether the defendant NP could “recommend” that test. I don’t fault the tactical decision to use this argument, in this case, when the surgeon also saw the patient on the same day. However, we should all recognize this will not normally work. A clinician cannot credibly argue she is not “credentialed” to recommend a course of action she can’t presently deliver.
Consider a clinician employed in an urgent care center without direct access to order CT. She evaluates an 80-year-old woman on warfarin who slipped and struck her head on a marble table. The standard of care requires a CT scan (likely several) to rule out an intracranial bleed. The urgent care clinician cannot send the patient away and later claim she was “not credentialed” to recommend CT imaging to rule out an intracranial bleed. As a matter of the standard of care, our hypothetical clinician would be duty bound to advise the patient of the risk for bleeding and then take steps to arrange for that care—even though she is not in a position to personally deliver it.
IN SUMMARY
Protect your patients from evolving cases by ordering updated tests. Do not be afraid of a negative result. Instead, fear the Reaper; keep him away from your patients. Let him get his “more cowbell” somewhere else.
1. Wells PS, Anderson DR, Bormanis J, et al. Value of assessment of pretest probability of deep-vein thrombosis in clinical management. Lancet. 1997;350(9094):1795-1798.
1. Wells PS, Anderson DR, Bormanis J, et al. Value of assessment of pretest probability of deep-vein thrombosis in clinical management. Lancet. 1997;350(9094):1795-1798.
Good Notes Can Deter Litigation
At 11:15
While in the ED, the patient was examined and treated by a PA. At approximately 12:13
Given the lack of any positive pertinent findings, the PA irrigated the patient’s wounds and applied 1% lidocaine to all affected fingers so that pain would not mask any potential physical exam findings. He also used single-layer absorbable sutures to repair the injured digits. In addition, the PA tested the plaintiff for both distal interphalangeal (DIP) and proximal interphalangeal (PIP) flexion function and recorded normal results.
The PA discharged the patient from the ED at 5:56
The PA provided no further care or treatment to the patient following the visit to the hospital’s ED. However, the patient contended that he suffered an injury to the tendons of his right hand, which ultimately required several surgical procedures. He sued the hospital, the PA, the PA’s medical office, his supervising physician, and the physician who performed the later surgical procedures. The supervising physician and the surgeon were ultimately let out of the case by summary judgment motions. The hospital, which was named as a defendant under a respondeat superior theory, was also dismissed from the case when it was established that the PA was employed by his medical office and not by the hospital directly. The PA stipulated that he was within his course and scope of employment at the time he treated the plaintiff.
Continue to: Plaintiff's counsel contended...
Plaintiff’s counsel contended that the defendant PA was negligent in his examination and evaluation of the plaintiff’s digit lacerations and that he was negligent for failing to splint the plaintiff’s hand. Counsel also contended that the defendant was negligent for failing to refer the plaintiff to a hand surgeon (either directly or through the plaintiff’s primary care provider) and/or for failing to seek the assistance of his supervising physician, who was on site at the hospital’s ED and available for consultation.
Defense counsel argued that the defendant met the applicable standard of care at all times, in all aspects of his visit with the plaintiff in the early morning hours of September 1, 2014, and that there was nothing that he either did or did not do that was a substantial factor in causing the plaintiff’s alleged injuries and damages. The defendant claimed that upon his arrival at the patient’s bedside, the plaintiff verbally indicated to him that he could move his fingers (extension and flexion). He also claimed that he visualized the plaintiff moving his fingers while they were wrapped in the dressing that the plaintiff had placed on himself after the injury-producing event. However, the plaintiff disputed the defendant’s claim, denying ever being asked to extend and flex his fingers. The plaintiff also claimed that he never was able to make a full fist with his fingers on the night in question while in the ED, either by way of passive or active flexion.
Defense counsel noted that the defendant’s dictated ED note stated that the range of motion of all the plaintiff’s phalanges were normal, with no deficits, at all times while in the ED. The defendant testified about how he tested and evaluated the plaintiff’s DIP function. He also testified that he had the plaintiff lay his hand on the table, palm side up, and then laid his own hand across the plaintiff’s hand so as to isolate the DIP joint on each finger. He explained that he then had the plaintiff flex his fingers, which allowed him to determine whether there had been any kind of injury to the flexor digitorum profundus tendon (responsible for DIP function in the hand). The defendant claimed that he did the test for all the lacerated fingers and characterized them as active (as opposed to passive) flexion. Thus, he claimed that his physical exam findings were that the plaintiff had full range of motion (ROM) intact following the DIP function testing, which helped him conclude that the plaintiff did not have completely lacerated tendons as of that visit.
The defendant further explained that if the tendons were completely lacerated, the plaintiff would have had nonexistent DIP functioning on examination. The defendant testified that if he suspected a tendon laceration in a patient such as the plaintiff, his practice would be to notify his supervising physician in the ED and then either refer the patient to a primary care provider for an orthopedic hand surgeon referral or directly refer the patient to an orthopedic hand surgeon. He claimed that he took no such actions because there was no indication, from his perspective, that the plaintiff had suffered any tendon damage based on his physical exam findings, the plaintiff’s ability to make a fist, and the x-ray results.
Continue to: VERDICT
VERDICT
After a 5-day trial and 7 hours of deliberation, the jury found in favor of the defendants.
COMMENTARY
As human beings, we do a lot with our hands. They are vulnerable to injury, and misdiagnosis may result in life-altering debility. The impact is even greater when one’s livelihood requires fine dexterity. Thus, tendon lacerations are relatively common and must be managed properly.
In this case, we are told that the PA documented in his notes that the plaintiff had range of motion in all phalanges and no deficits. We are also told the defendant testified regarding his procedure for hand examination. But we are not told that his note included the details of his exam—and by inference, we have reason to suspect it did not.
You might think, “The jury found in favor of the defense, so why does this matter?” Because a well-documented chart may prevent liability.
If you wish to avoid lawsuits, it is helpful to understand how they originate: An aggrieved patient contacts a plaintiff’s lawyer, insists he or she has been wronged, and asks the lawyer to take the case. Often faced with the ticking clock of statute of limitations (the absolute deadline to file), plaintiff’s counsel will review whatever records are available (which may not be all of them), looking for perceived deficiencies of care. The case may also be reviewed by a medical professional (generally a physician) prior to filing; some states require an affidavit of merit—an attestation that there is just cause to bring the action.
Whether reviewed only by plaintiff’s counsel or with the aid of an expert, a well-documented medical record may prevent a case from being filed. Medical malpractice cases are a huge gamble for plaintiff firms: They are expensive, time consuming, difficult to litigate, document heavy, and technically complex—falling outside the experience of most lawyers. They are also less likely than other cases to be settled, thanks to National Practitioner Data Bank recording requirements and (in several states) automatic medical board inquiry for potential adverse action against a medical or nursing professional following settlement. Clinicians will often fight tooth and nail to avoid an adverse recording, hospital credentialing woes, and state investigation. A medical malpractice case can be a trap for both the clinician and the plaintiff’s attorney stuck with a bad case.
Continue to: In the early stages...
In the early stages of potential litigation, before a case is filed in court, do yourself a favor: Help plaintiff’s counsel realize it will be a losing case. You actually start the process much earlier, by conducting the proper exam and documenting lavishly. This is particularly important with specialty exams, such as the hand exam in this case.
Here, simply noting “positive ROM and distal CSM [circulation, sensation, and motion] intact” is inadequate. Why? Because it is a conclusion, not evidence of the specialty examination that was diligently performed. The mechanism of injury and initial presentation roused the clinician’s suspicions sufficiently to conduct a thorough hand examination—but the mechanics of the exam were not included, only conclusions. The trouble is, those conclusions may have been based on sound medical evidence or they may have been hastily and improvidently drawn. A plaintiff’s firm deciding whether to take this case doesn’t know but will bet on the latter.
The clinician testified he performed a detailed and thorough examination of the plaintiff’s hand. Had plaintiff’s counsel been confronted with the full details of the exam—which showed the defendant PA tested all the PIPs and DIPs by isolating each finger—early on, this case may never have been filed. Thus, conduct and document specialty exams fully. If you need a cheat sheet for exams you don’t do often, use one—that is still solid practice. If you don’t do many pelvic exams or mental status exams, make sure you aren’t missing anything. Practicing medicine is an open-book exam; if you need materials, use them.
Good documentation leads to good defense, and any good defense lawyer will recommend the Jerry Maguire rule: “Help me help you.” Solid records make a case easier to defend and win at all phases of litigation. Of course, this is not a universal cure that will prevent all lawsuits. But even if the case is filed, the strength of your records may have convinced stronger, more capable medical malpractice firms to turn it down. This is something of value: It is “you helping you” and potent proof that your human head weighs more than 8 lb.
IN SUMMARY
A well-documented chart may prevent liability by showcasing the strength of your care and preventing no-win lawsuits from being filed. Help the plaintiff’s attorney realize, early on, that he or she is facing a costly uphill battle. The key word is early, when the medical records are first reviewed—not 18 months later, when the attorney hears your testimony at deposition and realizes that he or she has invested time and sweat in a case only to learn that your care was fabulous. Showcase that fabulous care early and short circuit the whole process by detailing the substance of a key exam (not just conclusions) in the record. Detailed notes may spare you from a visit by a sheriff you don’t know holding papers you don’t want.
At 11:15
While in the ED, the patient was examined and treated by a PA. At approximately 12:13
Given the lack of any positive pertinent findings, the PA irrigated the patient’s wounds and applied 1% lidocaine to all affected fingers so that pain would not mask any potential physical exam findings. He also used single-layer absorbable sutures to repair the injured digits. In addition, the PA tested the plaintiff for both distal interphalangeal (DIP) and proximal interphalangeal (PIP) flexion function and recorded normal results.
The PA discharged the patient from the ED at 5:56
The PA provided no further care or treatment to the patient following the visit to the hospital’s ED. However, the patient contended that he suffered an injury to the tendons of his right hand, which ultimately required several surgical procedures. He sued the hospital, the PA, the PA’s medical office, his supervising physician, and the physician who performed the later surgical procedures. The supervising physician and the surgeon were ultimately let out of the case by summary judgment motions. The hospital, which was named as a defendant under a respondeat superior theory, was also dismissed from the case when it was established that the PA was employed by his medical office and not by the hospital directly. The PA stipulated that he was within his course and scope of employment at the time he treated the plaintiff.
Continue to: Plaintiff's counsel contended...
Plaintiff’s counsel contended that the defendant PA was negligent in his examination and evaluation of the plaintiff’s digit lacerations and that he was negligent for failing to splint the plaintiff’s hand. Counsel also contended that the defendant was negligent for failing to refer the plaintiff to a hand surgeon (either directly or through the plaintiff’s primary care provider) and/or for failing to seek the assistance of his supervising physician, who was on site at the hospital’s ED and available for consultation.
Defense counsel argued that the defendant met the applicable standard of care at all times, in all aspects of his visit with the plaintiff in the early morning hours of September 1, 2014, and that there was nothing that he either did or did not do that was a substantial factor in causing the plaintiff’s alleged injuries and damages. The defendant claimed that upon his arrival at the patient’s bedside, the plaintiff verbally indicated to him that he could move his fingers (extension and flexion). He also claimed that he visualized the plaintiff moving his fingers while they were wrapped in the dressing that the plaintiff had placed on himself after the injury-producing event. However, the plaintiff disputed the defendant’s claim, denying ever being asked to extend and flex his fingers. The plaintiff also claimed that he never was able to make a full fist with his fingers on the night in question while in the ED, either by way of passive or active flexion.
Defense counsel noted that the defendant’s dictated ED note stated that the range of motion of all the plaintiff’s phalanges were normal, with no deficits, at all times while in the ED. The defendant testified about how he tested and evaluated the plaintiff’s DIP function. He also testified that he had the plaintiff lay his hand on the table, palm side up, and then laid his own hand across the plaintiff’s hand so as to isolate the DIP joint on each finger. He explained that he then had the plaintiff flex his fingers, which allowed him to determine whether there had been any kind of injury to the flexor digitorum profundus tendon (responsible for DIP function in the hand). The defendant claimed that he did the test for all the lacerated fingers and characterized them as active (as opposed to passive) flexion. Thus, he claimed that his physical exam findings were that the plaintiff had full range of motion (ROM) intact following the DIP function testing, which helped him conclude that the plaintiff did not have completely lacerated tendons as of that visit.
The defendant further explained that if the tendons were completely lacerated, the plaintiff would have had nonexistent DIP functioning on examination. The defendant testified that if he suspected a tendon laceration in a patient such as the plaintiff, his practice would be to notify his supervising physician in the ED and then either refer the patient to a primary care provider for an orthopedic hand surgeon referral or directly refer the patient to an orthopedic hand surgeon. He claimed that he took no such actions because there was no indication, from his perspective, that the plaintiff had suffered any tendon damage based on his physical exam findings, the plaintiff’s ability to make a fist, and the x-ray results.
Continue to: VERDICT
VERDICT
After a 5-day trial and 7 hours of deliberation, the jury found in favor of the defendants.
COMMENTARY
As human beings, we do a lot with our hands. They are vulnerable to injury, and misdiagnosis may result in life-altering debility. The impact is even greater when one’s livelihood requires fine dexterity. Thus, tendon lacerations are relatively common and must be managed properly.
In this case, we are told that the PA documented in his notes that the plaintiff had range of motion in all phalanges and no deficits. We are also told the defendant testified regarding his procedure for hand examination. But we are not told that his note included the details of his exam—and by inference, we have reason to suspect it did not.
You might think, “The jury found in favor of the defense, so why does this matter?” Because a well-documented chart may prevent liability.
If you wish to avoid lawsuits, it is helpful to understand how they originate: An aggrieved patient contacts a plaintiff’s lawyer, insists he or she has been wronged, and asks the lawyer to take the case. Often faced with the ticking clock of statute of limitations (the absolute deadline to file), plaintiff’s counsel will review whatever records are available (which may not be all of them), looking for perceived deficiencies of care. The case may also be reviewed by a medical professional (generally a physician) prior to filing; some states require an affidavit of merit—an attestation that there is just cause to bring the action.
Whether reviewed only by plaintiff’s counsel or with the aid of an expert, a well-documented medical record may prevent a case from being filed. Medical malpractice cases are a huge gamble for plaintiff firms: They are expensive, time consuming, difficult to litigate, document heavy, and technically complex—falling outside the experience of most lawyers. They are also less likely than other cases to be settled, thanks to National Practitioner Data Bank recording requirements and (in several states) automatic medical board inquiry for potential adverse action against a medical or nursing professional following settlement. Clinicians will often fight tooth and nail to avoid an adverse recording, hospital credentialing woes, and state investigation. A medical malpractice case can be a trap for both the clinician and the plaintiff’s attorney stuck with a bad case.
Continue to: In the early stages...
In the early stages of potential litigation, before a case is filed in court, do yourself a favor: Help plaintiff’s counsel realize it will be a losing case. You actually start the process much earlier, by conducting the proper exam and documenting lavishly. This is particularly important with specialty exams, such as the hand exam in this case.
Here, simply noting “positive ROM and distal CSM [circulation, sensation, and motion] intact” is inadequate. Why? Because it is a conclusion, not evidence of the specialty examination that was diligently performed. The mechanism of injury and initial presentation roused the clinician’s suspicions sufficiently to conduct a thorough hand examination—but the mechanics of the exam were not included, only conclusions. The trouble is, those conclusions may have been based on sound medical evidence or they may have been hastily and improvidently drawn. A plaintiff’s firm deciding whether to take this case doesn’t know but will bet on the latter.
The clinician testified he performed a detailed and thorough examination of the plaintiff’s hand. Had plaintiff’s counsel been confronted with the full details of the exam—which showed the defendant PA tested all the PIPs and DIPs by isolating each finger—early on, this case may never have been filed. Thus, conduct and document specialty exams fully. If you need a cheat sheet for exams you don’t do often, use one—that is still solid practice. If you don’t do many pelvic exams or mental status exams, make sure you aren’t missing anything. Practicing medicine is an open-book exam; if you need materials, use them.
Good documentation leads to good defense, and any good defense lawyer will recommend the Jerry Maguire rule: “Help me help you.” Solid records make a case easier to defend and win at all phases of litigation. Of course, this is not a universal cure that will prevent all lawsuits. But even if the case is filed, the strength of your records may have convinced stronger, more capable medical malpractice firms to turn it down. This is something of value: It is “you helping you” and potent proof that your human head weighs more than 8 lb.
IN SUMMARY
A well-documented chart may prevent liability by showcasing the strength of your care and preventing no-win lawsuits from being filed. Help the plaintiff’s attorney realize, early on, that he or she is facing a costly uphill battle. The key word is early, when the medical records are first reviewed—not 18 months later, when the attorney hears your testimony at deposition and realizes that he or she has invested time and sweat in a case only to learn that your care was fabulous. Showcase that fabulous care early and short circuit the whole process by detailing the substance of a key exam (not just conclusions) in the record. Detailed notes may spare you from a visit by a sheriff you don’t know holding papers you don’t want.
At 11:15
While in the ED, the patient was examined and treated by a PA. At approximately 12:13
Given the lack of any positive pertinent findings, the PA irrigated the patient’s wounds and applied 1% lidocaine to all affected fingers so that pain would not mask any potential physical exam findings. He also used single-layer absorbable sutures to repair the injured digits. In addition, the PA tested the plaintiff for both distal interphalangeal (DIP) and proximal interphalangeal (PIP) flexion function and recorded normal results.
The PA discharged the patient from the ED at 5:56
The PA provided no further care or treatment to the patient following the visit to the hospital’s ED. However, the patient contended that he suffered an injury to the tendons of his right hand, which ultimately required several surgical procedures. He sued the hospital, the PA, the PA’s medical office, his supervising physician, and the physician who performed the later surgical procedures. The supervising physician and the surgeon were ultimately let out of the case by summary judgment motions. The hospital, which was named as a defendant under a respondeat superior theory, was also dismissed from the case when it was established that the PA was employed by his medical office and not by the hospital directly. The PA stipulated that he was within his course and scope of employment at the time he treated the plaintiff.
Continue to: Plaintiff's counsel contended...
Plaintiff’s counsel contended that the defendant PA was negligent in his examination and evaluation of the plaintiff’s digit lacerations and that he was negligent for failing to splint the plaintiff’s hand. Counsel also contended that the defendant was negligent for failing to refer the plaintiff to a hand surgeon (either directly or through the plaintiff’s primary care provider) and/or for failing to seek the assistance of his supervising physician, who was on site at the hospital’s ED and available for consultation.
Defense counsel argued that the defendant met the applicable standard of care at all times, in all aspects of his visit with the plaintiff in the early morning hours of September 1, 2014, and that there was nothing that he either did or did not do that was a substantial factor in causing the plaintiff’s alleged injuries and damages. The defendant claimed that upon his arrival at the patient’s bedside, the plaintiff verbally indicated to him that he could move his fingers (extension and flexion). He also claimed that he visualized the plaintiff moving his fingers while they were wrapped in the dressing that the plaintiff had placed on himself after the injury-producing event. However, the plaintiff disputed the defendant’s claim, denying ever being asked to extend and flex his fingers. The plaintiff also claimed that he never was able to make a full fist with his fingers on the night in question while in the ED, either by way of passive or active flexion.
Defense counsel noted that the defendant’s dictated ED note stated that the range of motion of all the plaintiff’s phalanges were normal, with no deficits, at all times while in the ED. The defendant testified about how he tested and evaluated the plaintiff’s DIP function. He also testified that he had the plaintiff lay his hand on the table, palm side up, and then laid his own hand across the plaintiff’s hand so as to isolate the DIP joint on each finger. He explained that he then had the plaintiff flex his fingers, which allowed him to determine whether there had been any kind of injury to the flexor digitorum profundus tendon (responsible for DIP function in the hand). The defendant claimed that he did the test for all the lacerated fingers and characterized them as active (as opposed to passive) flexion. Thus, he claimed that his physical exam findings were that the plaintiff had full range of motion (ROM) intact following the DIP function testing, which helped him conclude that the plaintiff did not have completely lacerated tendons as of that visit.
The defendant further explained that if the tendons were completely lacerated, the plaintiff would have had nonexistent DIP functioning on examination. The defendant testified that if he suspected a tendon laceration in a patient such as the plaintiff, his practice would be to notify his supervising physician in the ED and then either refer the patient to a primary care provider for an orthopedic hand surgeon referral or directly refer the patient to an orthopedic hand surgeon. He claimed that he took no such actions because there was no indication, from his perspective, that the plaintiff had suffered any tendon damage based on his physical exam findings, the plaintiff’s ability to make a fist, and the x-ray results.
Continue to: VERDICT
VERDICT
After a 5-day trial and 7 hours of deliberation, the jury found in favor of the defendants.
COMMENTARY
As human beings, we do a lot with our hands. They are vulnerable to injury, and misdiagnosis may result in life-altering debility. The impact is even greater when one’s livelihood requires fine dexterity. Thus, tendon lacerations are relatively common and must be managed properly.
In this case, we are told that the PA documented in his notes that the plaintiff had range of motion in all phalanges and no deficits. We are also told the defendant testified regarding his procedure for hand examination. But we are not told that his note included the details of his exam—and by inference, we have reason to suspect it did not.
You might think, “The jury found in favor of the defense, so why does this matter?” Because a well-documented chart may prevent liability.
If you wish to avoid lawsuits, it is helpful to understand how they originate: An aggrieved patient contacts a plaintiff’s lawyer, insists he or she has been wronged, and asks the lawyer to take the case. Often faced with the ticking clock of statute of limitations (the absolute deadline to file), plaintiff’s counsel will review whatever records are available (which may not be all of them), looking for perceived deficiencies of care. The case may also be reviewed by a medical professional (generally a physician) prior to filing; some states require an affidavit of merit—an attestation that there is just cause to bring the action.
Whether reviewed only by plaintiff’s counsel or with the aid of an expert, a well-documented medical record may prevent a case from being filed. Medical malpractice cases are a huge gamble for plaintiff firms: They are expensive, time consuming, difficult to litigate, document heavy, and technically complex—falling outside the experience of most lawyers. They are also less likely than other cases to be settled, thanks to National Practitioner Data Bank recording requirements and (in several states) automatic medical board inquiry for potential adverse action against a medical or nursing professional following settlement. Clinicians will often fight tooth and nail to avoid an adverse recording, hospital credentialing woes, and state investigation. A medical malpractice case can be a trap for both the clinician and the plaintiff’s attorney stuck with a bad case.
Continue to: In the early stages...
In the early stages of potential litigation, before a case is filed in court, do yourself a favor: Help plaintiff’s counsel realize it will be a losing case. You actually start the process much earlier, by conducting the proper exam and documenting lavishly. This is particularly important with specialty exams, such as the hand exam in this case.
Here, simply noting “positive ROM and distal CSM [circulation, sensation, and motion] intact” is inadequate. Why? Because it is a conclusion, not evidence of the specialty examination that was diligently performed. The mechanism of injury and initial presentation roused the clinician’s suspicions sufficiently to conduct a thorough hand examination—but the mechanics of the exam were not included, only conclusions. The trouble is, those conclusions may have been based on sound medical evidence or they may have been hastily and improvidently drawn. A plaintiff’s firm deciding whether to take this case doesn’t know but will bet on the latter.
The clinician testified he performed a detailed and thorough examination of the plaintiff’s hand. Had plaintiff’s counsel been confronted with the full details of the exam—which showed the defendant PA tested all the PIPs and DIPs by isolating each finger—early on, this case may never have been filed. Thus, conduct and document specialty exams fully. If you need a cheat sheet for exams you don’t do often, use one—that is still solid practice. If you don’t do many pelvic exams or mental status exams, make sure you aren’t missing anything. Practicing medicine is an open-book exam; if you need materials, use them.
Good documentation leads to good defense, and any good defense lawyer will recommend the Jerry Maguire rule: “Help me help you.” Solid records make a case easier to defend and win at all phases of litigation. Of course, this is not a universal cure that will prevent all lawsuits. But even if the case is filed, the strength of your records may have convinced stronger, more capable medical malpractice firms to turn it down. This is something of value: It is “you helping you” and potent proof that your human head weighs more than 8 lb.
IN SUMMARY
A well-documented chart may prevent liability by showcasing the strength of your care and preventing no-win lawsuits from being filed. Help the plaintiff’s attorney realize, early on, that he or she is facing a costly uphill battle. The key word is early, when the medical records are first reviewed—not 18 months later, when the attorney hears your testimony at deposition and realizes that he or she has invested time and sweat in a case only to learn that your care was fabulous. Showcase that fabulous care early and short circuit the whole process by detailing the substance of a key exam (not just conclusions) in the record. Detailed notes may spare you from a visit by a sheriff you don’t know holding papers you don’t want.
When Diet Is an Emergency
At age 35, a woman underwent Roux-en-Y gastric bypass surgery. About 1 month later, she began vomiting and became unable to keep down any food or liquids. She was admitted to the hospital.
Two days after her admission, a dietitian evaluated the patient and recommended that she receive total parenteral nutrition (TPN). However, the attending physician did not order TPN during the patient’s 12-day hospital stay. As a result, the patient experienced vitamin deficiencies, including low thiamine. The patient developed symptoms of neurologic complications but was discharged.
Within 1 week, she was readmitted with the same symptoms, as well as signs of delirium and reduced level of consciousness. Her mental state continued to decline, and she became comatose for a period of time.
The patient now has Wernicke encephalopathy, which she alleged was caused by a lack of thiamine. She has no short-term memory, is wheelchair bound, and lives in a nursing home.
VERDICT
The jury found in favor of the plaintiff, awarding her $14,285,505.86 in damages, including $133,202 for loss of past earning capacity, $888,429 for loss of earning capacity, and $13,263,874.86 for medical care expenses.
COMMENTARY
It is foolish to think of diet as ancillary to medicine. While we often consider the long-term health implications of diet—obesity, atherosclerosis—we may overlook the urgent and emergent conditions that can result from a patient’s diet.
A familiar example is hypoglycemia. We associate it with agents used to treat diabetes. But it also can occur in the context of renal failure, tumor, severe infection, alcohol, or starvation. Similarly, thiamine deficiency would be an obvious consideration in a patient who presented in a coma or with altered mental status. But, as this case shows, thiamine deficiency can sneak up on you.
Continue to: In this case...
In this case, the patient’s altered structural anatomy rendered her more susceptible to thiamine deficiency, which was ultimately found to be causally related to the physician’s failure to order TPN. This raises an important issue in the management of patients who have had bariatric procedures.
This plaintiff had Roux-en-Y gastric bypass, a significant procedure that short circuits a sizable portion of the stomach and about 75 to 100 cm of the small intestine. This surgery carries long-term risks including bowel obstruction, hernias, ulcers, dumping syndrome, low blood sugar, and malnutrition. The last of these can manifest as low levels of B12, folate, thiamine, iron, calcium, and vitamin D.
Roux-en-Y bypass requires adherence to dietary recommendations, lifelong vitamin/mineral supplementation, and follow-up compliance. Patients who have had bariatric procedures are at increased risk for complications—which also raise malpractice risks. Clinicians must be aware that patients who have had a bariatric procedure have altered anatomy. We must take steps to understand the nature of those alterations and how they impact the present clinical picture.
In this case, the altered anatomy in combination with the failure to order TPN resulted in Wernicke encephalopathy—a condition caused by a biochemical lesion that occurs after stores of B vitamin are exhausted. Classic Wernicke encephalopathy is advertised as a triad of ophthalmoplegia, ataxia, and confusion, but only 10% of patients will demonstrate a true triad.
Wernicke encephalopathy typically occurs in the setting of alcoholism. However, certain other conditions can cause it, including recurrent dialysis, uremia, hyperemesis, thyrotoxicosis, cancer, AIDS, and starvation. It may be caused by surgical GI changes (eg, gastric bypass and banding) and nonsurgical GI causes (eg, pancreatitis, liver dysfunction, chronic diarrhea, celiac disease, and Crohn disease).
Continue to: Prognosis depends on...
Prognosis depends on how quickly the condition is recognized. Prompt treatment can lead to cure. But treatment delays (or lack of treatment) give the disorder the opportunity to progress, and memory and learning impairment may not completely resolve. Mortality in those untreated is 10% to 20%. And 80% of untreated or undertreated patients will develop Korsakoff psychosis, with severe retrograde and anterograde amnesia, disorientation, and emotional changes.
These factors make Wernicke encephalopathy a medical malpractice risk. If the diagnosis is missed, the damage is clear, substantial, and irreversible—as seen in this unfortunate case. This plaintiff’s attorney had a dream of a closing argument to make: Her client will suffer the effects of brain damage, robbing her of her life, her memory, and her very personality. This damage could have been prevented—not through use of an experimental new procedure or an investigational drug, but through use of a simple and readily available vitamin.
Worse still, cases such as this can involve a punitive element. Jurors would be invited to conclude that treating clinicians ignored the patient and left her to starve in her own bed. Always act in the patient’s best interest—and be attuned to situations that may evolve into claims that the patient was abandoned, neglected, or ignored.
Finally, you must address anything in the patient’s written record that is contrary to your plan. The fact pattern makes clear that a nutritional evaluation was obtained 2 days after the plaintiff’s admission. The dietitian recommended TPN. The record is not clear on why the physician did not order it. If you plan to take an action at odds with a prior observation or recommendation, be sure to clearly explain the rationale supporting your course of treatment. If you perform a risk-benefit analysis that leads you to a different conclusion, document that in the record—preferably with a second opinion from another clinician who supports your decision to deviate from the recommendation.
IN SUMMARY
Nutrition can be critically important. Make sure you consider both short- and long-term consequences of nutritional deficiencies. Bariatric surgery patients have altered anatomy, so be cautious with them. Consider the possibility of thiamine encephalopathy—which can be devastating—when the setting is suggestive. And make sure that all recommendations from other clinicians recorded in the patient’s chart are acted on. If you select a course of treatment that departs from prior recommendation, make clear your risk-benefit analysis and consider obtaining a second opinion in support of your decision.
At age 35, a woman underwent Roux-en-Y gastric bypass surgery. About 1 month later, she began vomiting and became unable to keep down any food or liquids. She was admitted to the hospital.
Two days after her admission, a dietitian evaluated the patient and recommended that she receive total parenteral nutrition (TPN). However, the attending physician did not order TPN during the patient’s 12-day hospital stay. As a result, the patient experienced vitamin deficiencies, including low thiamine. The patient developed symptoms of neurologic complications but was discharged.
Within 1 week, she was readmitted with the same symptoms, as well as signs of delirium and reduced level of consciousness. Her mental state continued to decline, and she became comatose for a period of time.
The patient now has Wernicke encephalopathy, which she alleged was caused by a lack of thiamine. She has no short-term memory, is wheelchair bound, and lives in a nursing home.
VERDICT
The jury found in favor of the plaintiff, awarding her $14,285,505.86 in damages, including $133,202 for loss of past earning capacity, $888,429 for loss of earning capacity, and $13,263,874.86 for medical care expenses.
COMMENTARY
It is foolish to think of diet as ancillary to medicine. While we often consider the long-term health implications of diet—obesity, atherosclerosis—we may overlook the urgent and emergent conditions that can result from a patient’s diet.
A familiar example is hypoglycemia. We associate it with agents used to treat diabetes. But it also can occur in the context of renal failure, tumor, severe infection, alcohol, or starvation. Similarly, thiamine deficiency would be an obvious consideration in a patient who presented in a coma or with altered mental status. But, as this case shows, thiamine deficiency can sneak up on you.
Continue to: In this case...
In this case, the patient’s altered structural anatomy rendered her more susceptible to thiamine deficiency, which was ultimately found to be causally related to the physician’s failure to order TPN. This raises an important issue in the management of patients who have had bariatric procedures.
This plaintiff had Roux-en-Y gastric bypass, a significant procedure that short circuits a sizable portion of the stomach and about 75 to 100 cm of the small intestine. This surgery carries long-term risks including bowel obstruction, hernias, ulcers, dumping syndrome, low blood sugar, and malnutrition. The last of these can manifest as low levels of B12, folate, thiamine, iron, calcium, and vitamin D.
Roux-en-Y bypass requires adherence to dietary recommendations, lifelong vitamin/mineral supplementation, and follow-up compliance. Patients who have had bariatric procedures are at increased risk for complications—which also raise malpractice risks. Clinicians must be aware that patients who have had a bariatric procedure have altered anatomy. We must take steps to understand the nature of those alterations and how they impact the present clinical picture.
In this case, the altered anatomy in combination with the failure to order TPN resulted in Wernicke encephalopathy—a condition caused by a biochemical lesion that occurs after stores of B vitamin are exhausted. Classic Wernicke encephalopathy is advertised as a triad of ophthalmoplegia, ataxia, and confusion, but only 10% of patients will demonstrate a true triad.
Wernicke encephalopathy typically occurs in the setting of alcoholism. However, certain other conditions can cause it, including recurrent dialysis, uremia, hyperemesis, thyrotoxicosis, cancer, AIDS, and starvation. It may be caused by surgical GI changes (eg, gastric bypass and banding) and nonsurgical GI causes (eg, pancreatitis, liver dysfunction, chronic diarrhea, celiac disease, and Crohn disease).
Continue to: Prognosis depends on...
Prognosis depends on how quickly the condition is recognized. Prompt treatment can lead to cure. But treatment delays (or lack of treatment) give the disorder the opportunity to progress, and memory and learning impairment may not completely resolve. Mortality in those untreated is 10% to 20%. And 80% of untreated or undertreated patients will develop Korsakoff psychosis, with severe retrograde and anterograde amnesia, disorientation, and emotional changes.
These factors make Wernicke encephalopathy a medical malpractice risk. If the diagnosis is missed, the damage is clear, substantial, and irreversible—as seen in this unfortunate case. This plaintiff’s attorney had a dream of a closing argument to make: Her client will suffer the effects of brain damage, robbing her of her life, her memory, and her very personality. This damage could have been prevented—not through use of an experimental new procedure or an investigational drug, but through use of a simple and readily available vitamin.
Worse still, cases such as this can involve a punitive element. Jurors would be invited to conclude that treating clinicians ignored the patient and left her to starve in her own bed. Always act in the patient’s best interest—and be attuned to situations that may evolve into claims that the patient was abandoned, neglected, or ignored.
Finally, you must address anything in the patient’s written record that is contrary to your plan. The fact pattern makes clear that a nutritional evaluation was obtained 2 days after the plaintiff’s admission. The dietitian recommended TPN. The record is not clear on why the physician did not order it. If you plan to take an action at odds with a prior observation or recommendation, be sure to clearly explain the rationale supporting your course of treatment. If you perform a risk-benefit analysis that leads you to a different conclusion, document that in the record—preferably with a second opinion from another clinician who supports your decision to deviate from the recommendation.
IN SUMMARY
Nutrition can be critically important. Make sure you consider both short- and long-term consequences of nutritional deficiencies. Bariatric surgery patients have altered anatomy, so be cautious with them. Consider the possibility of thiamine encephalopathy—which can be devastating—when the setting is suggestive. And make sure that all recommendations from other clinicians recorded in the patient’s chart are acted on. If you select a course of treatment that departs from prior recommendation, make clear your risk-benefit analysis and consider obtaining a second opinion in support of your decision.
At age 35, a woman underwent Roux-en-Y gastric bypass surgery. About 1 month later, she began vomiting and became unable to keep down any food or liquids. She was admitted to the hospital.
Two days after her admission, a dietitian evaluated the patient and recommended that she receive total parenteral nutrition (TPN). However, the attending physician did not order TPN during the patient’s 12-day hospital stay. As a result, the patient experienced vitamin deficiencies, including low thiamine. The patient developed symptoms of neurologic complications but was discharged.
Within 1 week, she was readmitted with the same symptoms, as well as signs of delirium and reduced level of consciousness. Her mental state continued to decline, and she became comatose for a period of time.
The patient now has Wernicke encephalopathy, which she alleged was caused by a lack of thiamine. She has no short-term memory, is wheelchair bound, and lives in a nursing home.
VERDICT
The jury found in favor of the plaintiff, awarding her $14,285,505.86 in damages, including $133,202 for loss of past earning capacity, $888,429 for loss of earning capacity, and $13,263,874.86 for medical care expenses.
COMMENTARY
It is foolish to think of diet as ancillary to medicine. While we often consider the long-term health implications of diet—obesity, atherosclerosis—we may overlook the urgent and emergent conditions that can result from a patient’s diet.
A familiar example is hypoglycemia. We associate it with agents used to treat diabetes. But it also can occur in the context of renal failure, tumor, severe infection, alcohol, or starvation. Similarly, thiamine deficiency would be an obvious consideration in a patient who presented in a coma or with altered mental status. But, as this case shows, thiamine deficiency can sneak up on you.
Continue to: In this case...
In this case, the patient’s altered structural anatomy rendered her more susceptible to thiamine deficiency, which was ultimately found to be causally related to the physician’s failure to order TPN. This raises an important issue in the management of patients who have had bariatric procedures.
This plaintiff had Roux-en-Y gastric bypass, a significant procedure that short circuits a sizable portion of the stomach and about 75 to 100 cm of the small intestine. This surgery carries long-term risks including bowel obstruction, hernias, ulcers, dumping syndrome, low blood sugar, and malnutrition. The last of these can manifest as low levels of B12, folate, thiamine, iron, calcium, and vitamin D.
Roux-en-Y bypass requires adherence to dietary recommendations, lifelong vitamin/mineral supplementation, and follow-up compliance. Patients who have had bariatric procedures are at increased risk for complications—which also raise malpractice risks. Clinicians must be aware that patients who have had a bariatric procedure have altered anatomy. We must take steps to understand the nature of those alterations and how they impact the present clinical picture.
In this case, the altered anatomy in combination with the failure to order TPN resulted in Wernicke encephalopathy—a condition caused by a biochemical lesion that occurs after stores of B vitamin are exhausted. Classic Wernicke encephalopathy is advertised as a triad of ophthalmoplegia, ataxia, and confusion, but only 10% of patients will demonstrate a true triad.
Wernicke encephalopathy typically occurs in the setting of alcoholism. However, certain other conditions can cause it, including recurrent dialysis, uremia, hyperemesis, thyrotoxicosis, cancer, AIDS, and starvation. It may be caused by surgical GI changes (eg, gastric bypass and banding) and nonsurgical GI causes (eg, pancreatitis, liver dysfunction, chronic diarrhea, celiac disease, and Crohn disease).
Continue to: Prognosis depends on...
Prognosis depends on how quickly the condition is recognized. Prompt treatment can lead to cure. But treatment delays (or lack of treatment) give the disorder the opportunity to progress, and memory and learning impairment may not completely resolve. Mortality in those untreated is 10% to 20%. And 80% of untreated or undertreated patients will develop Korsakoff psychosis, with severe retrograde and anterograde amnesia, disorientation, and emotional changes.
These factors make Wernicke encephalopathy a medical malpractice risk. If the diagnosis is missed, the damage is clear, substantial, and irreversible—as seen in this unfortunate case. This plaintiff’s attorney had a dream of a closing argument to make: Her client will suffer the effects of brain damage, robbing her of her life, her memory, and her very personality. This damage could have been prevented—not through use of an experimental new procedure or an investigational drug, but through use of a simple and readily available vitamin.
Worse still, cases such as this can involve a punitive element. Jurors would be invited to conclude that treating clinicians ignored the patient and left her to starve in her own bed. Always act in the patient’s best interest—and be attuned to situations that may evolve into claims that the patient was abandoned, neglected, or ignored.
Finally, you must address anything in the patient’s written record that is contrary to your plan. The fact pattern makes clear that a nutritional evaluation was obtained 2 days after the plaintiff’s admission. The dietitian recommended TPN. The record is not clear on why the physician did not order it. If you plan to take an action at odds with a prior observation or recommendation, be sure to clearly explain the rationale supporting your course of treatment. If you perform a risk-benefit analysis that leads you to a different conclusion, document that in the record—preferably with a second opinion from another clinician who supports your decision to deviate from the recommendation.
IN SUMMARY
Nutrition can be critically important. Make sure you consider both short- and long-term consequences of nutritional deficiencies. Bariatric surgery patients have altered anatomy, so be cautious with them. Consider the possibility of thiamine encephalopathy—which can be devastating—when the setting is suggestive. And make sure that all recommendations from other clinicians recorded in the patient’s chart are acted on. If you select a course of treatment that departs from prior recommendation, make clear your risk-benefit analysis and consider obtaining a second opinion in support of your decision.
Today’s Care Must Extend Beyond the Exam Room
In May 2014, a 70-year-old retiree underwent repair of a fracture of her left ankle. The procedure was performed at a local hospital. A splint was applied to the ankle, and a nurse provided crutches.
Following discharge from the hospital, the patient hailed a taxi to take her home. As she was exiting the taxi at her residence, the patient fell and sustained comminuted fractures to the distal radius and distal ulna of her right (dominant) wrist and a trimalleolar fracture to her repaired left ankle.
The plaintiff was transported back to the hospital via ambulance. She underwent closed reduction of her wrist fractures and 11 days later was transferred to another facility for open reduction and internal fixation of her left ankle fracture. Her hospitalizations totaled 13 days and were followed by a course of inpatient rehabilitative therapy; the latter lasted until late August 2014, with a brief interruption in June when she underwent open reduction and internal fixation of her wrist fractures. When she returned home in August, the patient required the assistance of visiting aides and 3 additional months of rehabilitative therapy.
At trial, the plaintiff claimed that her left ankle and her right wrist remained painful, that she sustained a mild residual diminution of each area’s range of motion, and that these residual effects hindered her performance of basic physical activities (eg, cleaning and cooking).
The plaintiff alleged that her fall while exiting the taxi resulted from unsteadiness, which was a lingering effect of morphine that was administered during the repair of her fracture. She sought recovery of damages for past and future pain and suffering from the hospital’s operator. The lawsuit alleged that the nurse had failed to provide instructions on the proper use of crutches, that the nurse had failed to undertake measures that would have diminished the plaintiff’s likelihood of falling, that the nurse’s failures constituted malpractice and negligence, and that the hospital operator was vicariously liable for the nurse’s actions.
The plaintiff claimed that she repeatedly warned that she did not believe that she could safely use the crutches provided by the nurse. She claimed that she was unsteady and lightheaded, and that when she requested a wheelchair, an escort, or an ambulance, the nurse rejected the request. The nursing standards expert for the plaintiff opined that the request should have been satisfied or alternatively, that the nurse should have explained the manner in which a crutch-dependent person could safely enter and exit a vehicle.
Defense counsel claimed that the nurse explained proper use of the crutches, the plaintiff indicated that she understood the explanation, and the plaintiff demonstrated proper use and did not express concern. The defense’s expert contended that the nurse did not have to explain how a crutch-dependent person could safely enter and exit a vehicle and that the plaintiff’s fall resulted from her own failure to exercise appropriate caution. The defense further contended that the plaintiff achieved an excellent recovery.
Continue to: After a 7-day trial...
After a 7-day trial and 3 hours and 45 minutes’ deliberation, the jury found in favor of the plaintiff. It found that the nurse was negligent in her provision of crutches and that the act was a substantial cause of the plaintiff’s injuries. The jury also found that the nurse did not properly explain the use of crutches but determined that the error was not a substantial cause of the plaintiff’s injuries.
VERDICT
The jury awarded the plaintiff a total of $850,000 in damages. The plaintiff also recovered stipulated medical expenses.
COMMENTARY
Medical malpractice litigation involves recovery for acts or omissions that constitute a departure from the standard of care. We all recognize injurious acts—improper esophageal intubation in the emergency department, transection of a nerve in the operating room, or prescription of a contraindicated medication to an allergic patient—and acknowledge damaging omissions, such as failure to screen for colon cancer or recognize treatable diabetes.
However, some cases are disposition related; they arise from how patients are discharged, what instructions they are given, where they go, and what they do after discharge. These cases involve the patient’s medical issues engrafted on his or her transportation, job, and more generally, living environment.
The lay public expects patients to have a right of self-determination, to control the nature and course of their medical care. Yet, the modern lay public also expects the medical profession to act as an authority figure—exercising a degree of paternalism to safeguard patients from harm. This expectation is commonly articulated in retrospect, after something has gone wrong. Consequently, clinicians must be aware of what will happen to the patient after discharge.
Continue to: With all interventions...
With all interventions, weigh the post-discharge consequences. If you give an injection of hydromorphone, you cannot discharge the patient to drive home 45 minutes later. If you have diagnosed vertigo in a patient, you cannot prescribe meclizine and return that patient to her job working on scaffolding 50 ft above ground. If a frail patient lives alone and cannot safely walk, and you’ve started him on furosemide, you cannot discharge him without considering how he will get to the bathroom. Other concerns are even more difficult—for example, the homeless patient who does not have the environment or resources to follow your instructions.
It is tempting to view these concerns as not our responsibility or dismiss them as “not medicine.” Clinicians can feel frustrated at being pulled into the realm of social work, where we are ill equipped to deal with and sort out the patient’s “life problems.” For one thing, we don’t often have the resources to deal with these issues. And for another, addressing the patient’s postdischarge living situation takes time—something in short supply and intangible to the other patients in the waiting room, who are expecting your attention and wondering, “What’s the holdup?”
In the case presented, the plaintiff was a 70-year-old retiree. She was discharged from the hospital with crutches. Crutches are age-old and familiar devices. Nevertheless, crutches are for people who are able to use their arms for weight bearing and propulsion and require a fair amount of physical strength, timing, and dexterity. While a potentially debatable point, an assumption that a 70-year-old patient has the arm strength and dexterity to properly propel herself with crutches may be faulty. There was disagreement between the patient, who claimed she could not safely use the crutches, and the nurse, who said the patient accepted the crutches without concern. The safest course of action would be for discharge personnel to demonstrate the use of crutches, observe the patient using the crutches, and document that in the record.
In this case, it is unclear if the nurse demonstrated how to use the crutches or witnessed the plaintiff demonstrating she could safely use them. The jury found the nurse was negligent “in her provision” of crutches—an act they deemed a substantial cause of the plaintiff’s injuries. Interestingly, the jury did not consider the lack of explanation on the crutches’ use to be a substantial cause of injury. But the bottom line is, they faulted the nurse for the act of giving this patient crutches and awarded $850,000 in damages.
Society is changing. Fifty years ago, jurors would expect people to be familiar with crutches, and if you fell while using them, that was your own fault. Modern jurors expect hospitals and providers to get more involved in what happens to a patient after discharge. The news media has heavily publicized cases of alleged “patient dumping.”
Continue to: As a result...
As a result, we see legislative changes, such as the recently passed California Senate Bill 1152, which requires that homeless patients be fed; provided weather-appropriate clothing, filled prescriptions, and vaccinations; given medical screening, examination, and evaluation that requires the “treating physician” to arrange behavioral health care; and enrolled in “any affordable health insurance coverage for which he or she is eligible.”
Whether it is appropriate to ask hospitals and clinicians to get this involved is beyond the scope of this column. What is clear is that society increasingly expects clinicians and hospitals to take responsibility for patients. This societal change has an impact on the lay public’s perception of what is expected of health care providers. Tomorrow’s juror comes to court with a belief that hospitals and clinicians owe a duty of care that extends beyond the walls of the exam room.
IN SUMMARY
Reality test your post-treatment instructions to be sure they will work for the patient and are not grossly incompatible with his or her known postdischarge environment. To the extent possible, involve discharge planning personnel in your practice. Let your record reflect that you are acting in the patient’s best interest, and evade the temptation to squint narrowly to avoid seeing circumstances in the patient’s life that prevent safe implementation of your plan.
In May 2014, a 70-year-old retiree underwent repair of a fracture of her left ankle. The procedure was performed at a local hospital. A splint was applied to the ankle, and a nurse provided crutches.
Following discharge from the hospital, the patient hailed a taxi to take her home. As she was exiting the taxi at her residence, the patient fell and sustained comminuted fractures to the distal radius and distal ulna of her right (dominant) wrist and a trimalleolar fracture to her repaired left ankle.
The plaintiff was transported back to the hospital via ambulance. She underwent closed reduction of her wrist fractures and 11 days later was transferred to another facility for open reduction and internal fixation of her left ankle fracture. Her hospitalizations totaled 13 days and were followed by a course of inpatient rehabilitative therapy; the latter lasted until late August 2014, with a brief interruption in June when she underwent open reduction and internal fixation of her wrist fractures. When she returned home in August, the patient required the assistance of visiting aides and 3 additional months of rehabilitative therapy.
At trial, the plaintiff claimed that her left ankle and her right wrist remained painful, that she sustained a mild residual diminution of each area’s range of motion, and that these residual effects hindered her performance of basic physical activities (eg, cleaning and cooking).
The plaintiff alleged that her fall while exiting the taxi resulted from unsteadiness, which was a lingering effect of morphine that was administered during the repair of her fracture. She sought recovery of damages for past and future pain and suffering from the hospital’s operator. The lawsuit alleged that the nurse had failed to provide instructions on the proper use of crutches, that the nurse had failed to undertake measures that would have diminished the plaintiff’s likelihood of falling, that the nurse’s failures constituted malpractice and negligence, and that the hospital operator was vicariously liable for the nurse’s actions.
The plaintiff claimed that she repeatedly warned that she did not believe that she could safely use the crutches provided by the nurse. She claimed that she was unsteady and lightheaded, and that when she requested a wheelchair, an escort, or an ambulance, the nurse rejected the request. The nursing standards expert for the plaintiff opined that the request should have been satisfied or alternatively, that the nurse should have explained the manner in which a crutch-dependent person could safely enter and exit a vehicle.
Defense counsel claimed that the nurse explained proper use of the crutches, the plaintiff indicated that she understood the explanation, and the plaintiff demonstrated proper use and did not express concern. The defense’s expert contended that the nurse did not have to explain how a crutch-dependent person could safely enter and exit a vehicle and that the plaintiff’s fall resulted from her own failure to exercise appropriate caution. The defense further contended that the plaintiff achieved an excellent recovery.
Continue to: After a 7-day trial...
After a 7-day trial and 3 hours and 45 minutes’ deliberation, the jury found in favor of the plaintiff. It found that the nurse was negligent in her provision of crutches and that the act was a substantial cause of the plaintiff’s injuries. The jury also found that the nurse did not properly explain the use of crutches but determined that the error was not a substantial cause of the plaintiff’s injuries.
VERDICT
The jury awarded the plaintiff a total of $850,000 in damages. The plaintiff also recovered stipulated medical expenses.
COMMENTARY
Medical malpractice litigation involves recovery for acts or omissions that constitute a departure from the standard of care. We all recognize injurious acts—improper esophageal intubation in the emergency department, transection of a nerve in the operating room, or prescription of a contraindicated medication to an allergic patient—and acknowledge damaging omissions, such as failure to screen for colon cancer or recognize treatable diabetes.
However, some cases are disposition related; they arise from how patients are discharged, what instructions they are given, where they go, and what they do after discharge. These cases involve the patient’s medical issues engrafted on his or her transportation, job, and more generally, living environment.
The lay public expects patients to have a right of self-determination, to control the nature and course of their medical care. Yet, the modern lay public also expects the medical profession to act as an authority figure—exercising a degree of paternalism to safeguard patients from harm. This expectation is commonly articulated in retrospect, after something has gone wrong. Consequently, clinicians must be aware of what will happen to the patient after discharge.
Continue to: With all interventions...
With all interventions, weigh the post-discharge consequences. If you give an injection of hydromorphone, you cannot discharge the patient to drive home 45 minutes later. If you have diagnosed vertigo in a patient, you cannot prescribe meclizine and return that patient to her job working on scaffolding 50 ft above ground. If a frail patient lives alone and cannot safely walk, and you’ve started him on furosemide, you cannot discharge him without considering how he will get to the bathroom. Other concerns are even more difficult—for example, the homeless patient who does not have the environment or resources to follow your instructions.
It is tempting to view these concerns as not our responsibility or dismiss them as “not medicine.” Clinicians can feel frustrated at being pulled into the realm of social work, where we are ill equipped to deal with and sort out the patient’s “life problems.” For one thing, we don’t often have the resources to deal with these issues. And for another, addressing the patient’s postdischarge living situation takes time—something in short supply and intangible to the other patients in the waiting room, who are expecting your attention and wondering, “What’s the holdup?”
In the case presented, the plaintiff was a 70-year-old retiree. She was discharged from the hospital with crutches. Crutches are age-old and familiar devices. Nevertheless, crutches are for people who are able to use their arms for weight bearing and propulsion and require a fair amount of physical strength, timing, and dexterity. While a potentially debatable point, an assumption that a 70-year-old patient has the arm strength and dexterity to properly propel herself with crutches may be faulty. There was disagreement between the patient, who claimed she could not safely use the crutches, and the nurse, who said the patient accepted the crutches without concern. The safest course of action would be for discharge personnel to demonstrate the use of crutches, observe the patient using the crutches, and document that in the record.
In this case, it is unclear if the nurse demonstrated how to use the crutches or witnessed the plaintiff demonstrating she could safely use them. The jury found the nurse was negligent “in her provision” of crutches—an act they deemed a substantial cause of the plaintiff’s injuries. Interestingly, the jury did not consider the lack of explanation on the crutches’ use to be a substantial cause of injury. But the bottom line is, they faulted the nurse for the act of giving this patient crutches and awarded $850,000 in damages.
Society is changing. Fifty years ago, jurors would expect people to be familiar with crutches, and if you fell while using them, that was your own fault. Modern jurors expect hospitals and providers to get more involved in what happens to a patient after discharge. The news media has heavily publicized cases of alleged “patient dumping.”
Continue to: As a result...
As a result, we see legislative changes, such as the recently passed California Senate Bill 1152, which requires that homeless patients be fed; provided weather-appropriate clothing, filled prescriptions, and vaccinations; given medical screening, examination, and evaluation that requires the “treating physician” to arrange behavioral health care; and enrolled in “any affordable health insurance coverage for which he or she is eligible.”
Whether it is appropriate to ask hospitals and clinicians to get this involved is beyond the scope of this column. What is clear is that society increasingly expects clinicians and hospitals to take responsibility for patients. This societal change has an impact on the lay public’s perception of what is expected of health care providers. Tomorrow’s juror comes to court with a belief that hospitals and clinicians owe a duty of care that extends beyond the walls of the exam room.
IN SUMMARY
Reality test your post-treatment instructions to be sure they will work for the patient and are not grossly incompatible with his or her known postdischarge environment. To the extent possible, involve discharge planning personnel in your practice. Let your record reflect that you are acting in the patient’s best interest, and evade the temptation to squint narrowly to avoid seeing circumstances in the patient’s life that prevent safe implementation of your plan.
In May 2014, a 70-year-old retiree underwent repair of a fracture of her left ankle. The procedure was performed at a local hospital. A splint was applied to the ankle, and a nurse provided crutches.
Following discharge from the hospital, the patient hailed a taxi to take her home. As she was exiting the taxi at her residence, the patient fell and sustained comminuted fractures to the distal radius and distal ulna of her right (dominant) wrist and a trimalleolar fracture to her repaired left ankle.
The plaintiff was transported back to the hospital via ambulance. She underwent closed reduction of her wrist fractures and 11 days later was transferred to another facility for open reduction and internal fixation of her left ankle fracture. Her hospitalizations totaled 13 days and were followed by a course of inpatient rehabilitative therapy; the latter lasted until late August 2014, with a brief interruption in June when she underwent open reduction and internal fixation of her wrist fractures. When she returned home in August, the patient required the assistance of visiting aides and 3 additional months of rehabilitative therapy.
At trial, the plaintiff claimed that her left ankle and her right wrist remained painful, that she sustained a mild residual diminution of each area’s range of motion, and that these residual effects hindered her performance of basic physical activities (eg, cleaning and cooking).
The plaintiff alleged that her fall while exiting the taxi resulted from unsteadiness, which was a lingering effect of morphine that was administered during the repair of her fracture. She sought recovery of damages for past and future pain and suffering from the hospital’s operator. The lawsuit alleged that the nurse had failed to provide instructions on the proper use of crutches, that the nurse had failed to undertake measures that would have diminished the plaintiff’s likelihood of falling, that the nurse’s failures constituted malpractice and negligence, and that the hospital operator was vicariously liable for the nurse’s actions.
The plaintiff claimed that she repeatedly warned that she did not believe that she could safely use the crutches provided by the nurse. She claimed that she was unsteady and lightheaded, and that when she requested a wheelchair, an escort, or an ambulance, the nurse rejected the request. The nursing standards expert for the plaintiff opined that the request should have been satisfied or alternatively, that the nurse should have explained the manner in which a crutch-dependent person could safely enter and exit a vehicle.
Defense counsel claimed that the nurse explained proper use of the crutches, the plaintiff indicated that she understood the explanation, and the plaintiff demonstrated proper use and did not express concern. The defense’s expert contended that the nurse did not have to explain how a crutch-dependent person could safely enter and exit a vehicle and that the plaintiff’s fall resulted from her own failure to exercise appropriate caution. The defense further contended that the plaintiff achieved an excellent recovery.
Continue to: After a 7-day trial...
After a 7-day trial and 3 hours and 45 minutes’ deliberation, the jury found in favor of the plaintiff. It found that the nurse was negligent in her provision of crutches and that the act was a substantial cause of the plaintiff’s injuries. The jury also found that the nurse did not properly explain the use of crutches but determined that the error was not a substantial cause of the plaintiff’s injuries.
VERDICT
The jury awarded the plaintiff a total of $850,000 in damages. The plaintiff also recovered stipulated medical expenses.
COMMENTARY
Medical malpractice litigation involves recovery for acts or omissions that constitute a departure from the standard of care. We all recognize injurious acts—improper esophageal intubation in the emergency department, transection of a nerve in the operating room, or prescription of a contraindicated medication to an allergic patient—and acknowledge damaging omissions, such as failure to screen for colon cancer or recognize treatable diabetes.
However, some cases are disposition related; they arise from how patients are discharged, what instructions they are given, where they go, and what they do after discharge. These cases involve the patient’s medical issues engrafted on his or her transportation, job, and more generally, living environment.
The lay public expects patients to have a right of self-determination, to control the nature and course of their medical care. Yet, the modern lay public also expects the medical profession to act as an authority figure—exercising a degree of paternalism to safeguard patients from harm. This expectation is commonly articulated in retrospect, after something has gone wrong. Consequently, clinicians must be aware of what will happen to the patient after discharge.
Continue to: With all interventions...
With all interventions, weigh the post-discharge consequences. If you give an injection of hydromorphone, you cannot discharge the patient to drive home 45 minutes later. If you have diagnosed vertigo in a patient, you cannot prescribe meclizine and return that patient to her job working on scaffolding 50 ft above ground. If a frail patient lives alone and cannot safely walk, and you’ve started him on furosemide, you cannot discharge him without considering how he will get to the bathroom. Other concerns are even more difficult—for example, the homeless patient who does not have the environment or resources to follow your instructions.
It is tempting to view these concerns as not our responsibility or dismiss them as “not medicine.” Clinicians can feel frustrated at being pulled into the realm of social work, where we are ill equipped to deal with and sort out the patient’s “life problems.” For one thing, we don’t often have the resources to deal with these issues. And for another, addressing the patient’s postdischarge living situation takes time—something in short supply and intangible to the other patients in the waiting room, who are expecting your attention and wondering, “What’s the holdup?”
In the case presented, the plaintiff was a 70-year-old retiree. She was discharged from the hospital with crutches. Crutches are age-old and familiar devices. Nevertheless, crutches are for people who are able to use their arms for weight bearing and propulsion and require a fair amount of physical strength, timing, and dexterity. While a potentially debatable point, an assumption that a 70-year-old patient has the arm strength and dexterity to properly propel herself with crutches may be faulty. There was disagreement between the patient, who claimed she could not safely use the crutches, and the nurse, who said the patient accepted the crutches without concern. The safest course of action would be for discharge personnel to demonstrate the use of crutches, observe the patient using the crutches, and document that in the record.
In this case, it is unclear if the nurse demonstrated how to use the crutches or witnessed the plaintiff demonstrating she could safely use them. The jury found the nurse was negligent “in her provision” of crutches—an act they deemed a substantial cause of the plaintiff’s injuries. Interestingly, the jury did not consider the lack of explanation on the crutches’ use to be a substantial cause of injury. But the bottom line is, they faulted the nurse for the act of giving this patient crutches and awarded $850,000 in damages.
Society is changing. Fifty years ago, jurors would expect people to be familiar with crutches, and if you fell while using them, that was your own fault. Modern jurors expect hospitals and providers to get more involved in what happens to a patient after discharge. The news media has heavily publicized cases of alleged “patient dumping.”
Continue to: As a result...
As a result, we see legislative changes, such as the recently passed California Senate Bill 1152, which requires that homeless patients be fed; provided weather-appropriate clothing, filled prescriptions, and vaccinations; given medical screening, examination, and evaluation that requires the “treating physician” to arrange behavioral health care; and enrolled in “any affordable health insurance coverage for which he or she is eligible.”
Whether it is appropriate to ask hospitals and clinicians to get this involved is beyond the scope of this column. What is clear is that society increasingly expects clinicians and hospitals to take responsibility for patients. This societal change has an impact on the lay public’s perception of what is expected of health care providers. Tomorrow’s juror comes to court with a belief that hospitals and clinicians owe a duty of care that extends beyond the walls of the exam room.
IN SUMMARY
Reality test your post-treatment instructions to be sure they will work for the patient and are not grossly incompatible with his or her known postdischarge environment. To the extent possible, involve discharge planning personnel in your practice. Let your record reflect that you are acting in the patient’s best interest, and evade the temptation to squint narrowly to avoid seeing circumstances in the patient’s life that prevent safe implementation of your plan.
