User login
Satish Misra, MD, a first-year internal-medicine resident at Johns Hopkins School of Medicine in Baltimore, used to carry a guidebook—many schools refer to it as their Red Book—around the hospital; it served as a tutorial on how to handle a litany of common medical problems. Now, Dr. Misra mostly scans his iPhone.
Henry Feldman, MD, a hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston who also serves as chief information architect for Harvard Medical Faculty Physicians, used to lug around a bulky copy of Netter’s Anatomy if he wanted to visually explain to a patient how their endoscopic retrograde cholangiopancreatography (ERCP) would work. Now, he pulls up the medical illustrations via an application on his iPad.
In an increasingly technological society in which there is an “app” for nearly everything, healthcare—and HM in particular—is no exception. The growing prevalence of touchscreen technology, mostly via smartphones and tablet computers, already has had an impact on how some hospitalists do their jobs. That upward trend should continue in the coming years, as both hardware and software technology become even more sophisticated and easy to use.
Of course, there are roadblocks. Patient privacy, wireless security, and the well-known reticence of healthcare as an industry to adopt information technology (IT) changes have—and will continue to—slowed the spread of the new technologies. However, with potential or practical usage already being forged in the arenas of patient interaction, billing and coding, and quality and patient safety initiatives, the integration of interactive devices into a physician’s daily workflow could become as commonplace in 10 years as the presence of hospitalists is today.
Still, the CEO of one software company points out that the presence of innovation alone does not translate to efficacy. The value of mobile and touchscreen technology to hospitalists—both from the hardware and the software perspectives—lies in how much a physician chooses to incorporate it into their daily practice.
“The number-one factor in these things being adopted is: Can you improve the quality of documentation … without negatively impacting a physician’s interaction with the patient?” says Todd Johnson, president of Salar Inc., a Baltimore-based firm that develops software applications for clinical documentation. Touchscreen technology “absolutely does help meet that goal, but it depends on the providers. It truly is different strokes for different folks.”
Steven Peskin, MD, MBA, FACP, executive vice president and CMO of Yardley, Pa.-based MediMedia USA, has long preached the value of digital technology for inpatient care, particularly for hospitalists. He categorizes the latest wave of technology into five silos:
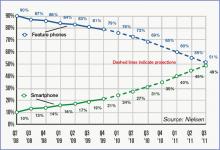
- Smartphones: Powered by operating systems that turn them into pocket-size mini-computers, the smallest and most mobile of these technologies are ubiquitous in society and hospitals alike (see Table 1, right).
- Tablet PCs: Led by the iPad’s debut in April 2010, the product is a larger version of the smartphone; the oversized screen makes it practical to use as a virtual chalkboard to explain topics to patients.
- Peripherals: From blood pressure cuffs produced by iHealth Labs (www.ihealth99.com) and Withings (www.withings.com/en/bloodpressuremonitor) to Mobisante’s prototype plug-in ultrasound probe (www.technologyreview.com/biomedicine/), there is a burgeoning marketplace for devices that serve as accessories to a smartphone or tablet, effectively turning those devices into handheld versions of costly machines. Most are connected to a mobile device via simple plug-in cables.
- Applications: According to Dr. Feldman, “It’s not the mobile device that’s the gate to any of this. It’s the applications you interact with.” App stores already feature medical specialty sections, and the number of offerings is expected to grow exponentially in the coming years.
- Cloud computing: A cloud is a metaphorical moniker for the interactivity and interoperability of different devices, systems, and servers to provide immediate connectivity and access to remote data and processes (http://csrc.nist.gov/groups/SNS/cloud-computing/).

“There’s tremendous potential and power of medical computing systems out there, but the stumbling block is they’re bulky or not effective,” says Larry Nathanson, MD, director of emergency medical informatics for BIDMC’s Department of Emergency Medicine, who served as architect and programmer of the ED Dashboard, the information system that is used at BIDMC and a number of other hospitals. “By improving the user interface, the systems become easier to use and the systems become revolutionary.”
Impact: Cloudy, Optimistic
Experts agree that the exact role mobile and touchscreen technologies will play in hospitalist groups around the country remains murky because the field is still a novel one, mostly devoid of evidence-based conclusions. In one of the first planned research studies, the two-year-old University of Central Florida College of Medicine in Orlando has provided iPads to each student in order to research the use of technology in medical education.
Regardless, physicians and tablet manufacturers alike agree that the point-of-service efficiency offered by mobile devices inherently allows their users to be more efficient. Several hospitalists have taken to the Internet, touting how mobile devices have streamlined their efficiency. One popular (and anonymous) blogger, The Happy Hospitalist (http://thehappyhospitalist.blogspot.com/), noted in two recent posts how they were able to round on 16 patients in less than 4 1/2 hours using an iPhone or iPad. On one of those days, the blogger discharged 13 of those patients.
“I no longer have to walk back and forth between patient rooms and nursing stations,” according to The Happy Hospitalist. “I can just drink my coffee at the bedside. I don’t have to fight with other doctors and nurses to log into a paucity of computers that are often way too slow and way too unpredictable. I just sync my iPhone with the patient database app on my iPhone screen and I’m up and running with a real-time update of all my patient’s information.”
The mobile devices allow faster, possibly better, interactions with patients, Dr. Feldman says. For example, a patient tells their hospitalist they need a change to their pain medication. Having a handheld touchscreen device linked to other technologies allows the order to be placed instantly. It even can send the nursing station an alert to the change. The sloppiness of a handwritten note is taken out of play; plus, rounding never misses a beat. “I’m terrible at remembering what I wrote down six patients ago,” Dr. Feldman admits. “Ultimately, for saving money, if I can get things done sooner, theoretically, length of stay can be reduced. That hasn’t been studied, but it is common sense.”
Dr. Feldman, who describes himself as a “hardcore code jockey,” says hospitalists would do well to work closely with their IT staffs to help conceptualize and design in-house applications and interoperability that would make their jobs easier. In institutions with an informatics department, that conversation could be as simple as a one-on-one conversation between an HM group leader and the IT department head.
In other hospitals, a field trip can help. “We will take IT staff out on the wards,” Dr. Feldman explains. “Come observe the process you’re automating. When they come back, they’re very sobered.”
Dr. Misra, the Johns Hopkins intern, notes that mobile devices are perfect hosts for checklists. Their ease of use can even be viewed as a potential motivator to ensure that those checklists are completed, particularly for younger physicians who have either grown up with or started their careers with more exposure to technology than previous generations.
“The biggest strength of touchscreen technology is it’s interactive,” Dr. Misra says. “It’s fun to use, much more fun than checking off boxes on a piece of paper or on a computer screen.
“It’s portable, it’s lightweight, it’s where you are.”
Trouble Spots
The virtually limitless boundaries for touchscreen technology to replace functions in the hospitalist’s workflow is, of course, limited in one glaring respect: privacy. The security of devices, applications, or peripherals must be paramount to their effectiveness, Dr. Feldman says, adding patient information must “remain sacrosanct.”
At BIDMC, digital security is accomplished in part via a bifurcated wireless network that allows physicians access to a secure connection while simultaneously and transparently maintaining a free wireless network for patients and visitors. Not all hospitals can afford the infrastructure necessary for such a setup. And even for health systems that have separate wireless systems, the connectivity cuts both ways, says Mike Stinson, vice president of marketing for Motion in Computing, an Austin, Texas, firm that produces tablet computers for multiple industries, including healthcare.
“Are you willing to have every file on your personal system viewable and accessible by the IT guys so they can make sure you don’t have access to something you shouldn’t have access to?” Stinson asks. “It seems easy and appealing, but there are larger issues.”
Stinson says the privacy and safety concerns of the technology can be addressed. Even potential fears regarding the sterility of the equipment might be simply solved. To wit, a column in the Journal of Surgical Radiology in January found that the device worked well when put in an X-ray cassette sealed off with a hemostat.1
Dr. Nathanson, an ED physician who has worked closely with hospitalists at BIDMC in the past, says it’s clear to him that making the technology easy enough to use in a medical setting is no longer the hurdle. It’s the systemic timidity of physicians who are slow to endorse and incorporate cutting-edge technology into entrenched work patterns.
“In medicine, it tends to take a long time,” he says. “The adoption of technology in medicine can be very challenging. If nothing else, we’re very early in the process.” TH
Richard Quinn is a freelance writer based in New Jersey.
Reference
- Wodajo, FM. The iPad in the hospital and operating room. Journal of Surgical Radiology website. Available at: www.surgisphere.com/SurgRad/issues/volume-2/1-january-2011—pages-1-112/152-column-the-ipad-in-the-hospital-and-operating-room.html. Accessed Jan. 3, 2011.
Satish Misra, MD, a first-year internal-medicine resident at Johns Hopkins School of Medicine in Baltimore, used to carry a guidebook—many schools refer to it as their Red Book—around the hospital; it served as a tutorial on how to handle a litany of common medical problems. Now, Dr. Misra mostly scans his iPhone.
Henry Feldman, MD, a hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston who also serves as chief information architect for Harvard Medical Faculty Physicians, used to lug around a bulky copy of Netter’s Anatomy if he wanted to visually explain to a patient how their endoscopic retrograde cholangiopancreatography (ERCP) would work. Now, he pulls up the medical illustrations via an application on his iPad.
In an increasingly technological society in which there is an “app” for nearly everything, healthcare—and HM in particular—is no exception. The growing prevalence of touchscreen technology, mostly via smartphones and tablet computers, already has had an impact on how some hospitalists do their jobs. That upward trend should continue in the coming years, as both hardware and software technology become even more sophisticated and easy to use.
Of course, there are roadblocks. Patient privacy, wireless security, and the well-known reticence of healthcare as an industry to adopt information technology (IT) changes have—and will continue to—slowed the spread of the new technologies. However, with potential or practical usage already being forged in the arenas of patient interaction, billing and coding, and quality and patient safety initiatives, the integration of interactive devices into a physician’s daily workflow could become as commonplace in 10 years as the presence of hospitalists is today.
Still, the CEO of one software company points out that the presence of innovation alone does not translate to efficacy. The value of mobile and touchscreen technology to hospitalists—both from the hardware and the software perspectives—lies in how much a physician chooses to incorporate it into their daily practice.
“The number-one factor in these things being adopted is: Can you improve the quality of documentation … without negatively impacting a physician’s interaction with the patient?” says Todd Johnson, president of Salar Inc., a Baltimore-based firm that develops software applications for clinical documentation. Touchscreen technology “absolutely does help meet that goal, but it depends on the providers. It truly is different strokes for different folks.”
Steven Peskin, MD, MBA, FACP, executive vice president and CMO of Yardley, Pa.-based MediMedia USA, has long preached the value of digital technology for inpatient care, particularly for hospitalists. He categorizes the latest wave of technology into five silos:
- Smartphones: Powered by operating systems that turn them into pocket-size mini-computers, the smallest and most mobile of these technologies are ubiquitous in society and hospitals alike (see Table 1, right).
- Tablet PCs: Led by the iPad’s debut in April 2010, the product is a larger version of the smartphone; the oversized screen makes it practical to use as a virtual chalkboard to explain topics to patients.
- Peripherals: From blood pressure cuffs produced by iHealth Labs (www.ihealth99.com) and Withings (www.withings.com/en/bloodpressuremonitor) to Mobisante’s prototype plug-in ultrasound probe (www.technologyreview.com/biomedicine/), there is a burgeoning marketplace for devices that serve as accessories to a smartphone or tablet, effectively turning those devices into handheld versions of costly machines. Most are connected to a mobile device via simple plug-in cables.
- Applications: According to Dr. Feldman, “It’s not the mobile device that’s the gate to any of this. It’s the applications you interact with.” App stores already feature medical specialty sections, and the number of offerings is expected to grow exponentially in the coming years.
- Cloud computing: A cloud is a metaphorical moniker for the interactivity and interoperability of different devices, systems, and servers to provide immediate connectivity and access to remote data and processes (http://csrc.nist.gov/groups/SNS/cloud-computing/).

“There’s tremendous potential and power of medical computing systems out there, but the stumbling block is they’re bulky or not effective,” says Larry Nathanson, MD, director of emergency medical informatics for BIDMC’s Department of Emergency Medicine, who served as architect and programmer of the ED Dashboard, the information system that is used at BIDMC and a number of other hospitals. “By improving the user interface, the systems become easier to use and the systems become revolutionary.”
Impact: Cloudy, Optimistic
Experts agree that the exact role mobile and touchscreen technologies will play in hospitalist groups around the country remains murky because the field is still a novel one, mostly devoid of evidence-based conclusions. In one of the first planned research studies, the two-year-old University of Central Florida College of Medicine in Orlando has provided iPads to each student in order to research the use of technology in medical education.
Regardless, physicians and tablet manufacturers alike agree that the point-of-service efficiency offered by mobile devices inherently allows their users to be more efficient. Several hospitalists have taken to the Internet, touting how mobile devices have streamlined their efficiency. One popular (and anonymous) blogger, The Happy Hospitalist (http://thehappyhospitalist.blogspot.com/), noted in two recent posts how they were able to round on 16 patients in less than 4 1/2 hours using an iPhone or iPad. On one of those days, the blogger discharged 13 of those patients.
“I no longer have to walk back and forth between patient rooms and nursing stations,” according to The Happy Hospitalist. “I can just drink my coffee at the bedside. I don’t have to fight with other doctors and nurses to log into a paucity of computers that are often way too slow and way too unpredictable. I just sync my iPhone with the patient database app on my iPhone screen and I’m up and running with a real-time update of all my patient’s information.”
The mobile devices allow faster, possibly better, interactions with patients, Dr. Feldman says. For example, a patient tells their hospitalist they need a change to their pain medication. Having a handheld touchscreen device linked to other technologies allows the order to be placed instantly. It even can send the nursing station an alert to the change. The sloppiness of a handwritten note is taken out of play; plus, rounding never misses a beat. “I’m terrible at remembering what I wrote down six patients ago,” Dr. Feldman admits. “Ultimately, for saving money, if I can get things done sooner, theoretically, length of stay can be reduced. That hasn’t been studied, but it is common sense.”
Dr. Feldman, who describes himself as a “hardcore code jockey,” says hospitalists would do well to work closely with their IT staffs to help conceptualize and design in-house applications and interoperability that would make their jobs easier. In institutions with an informatics department, that conversation could be as simple as a one-on-one conversation between an HM group leader and the IT department head.
In other hospitals, a field trip can help. “We will take IT staff out on the wards,” Dr. Feldman explains. “Come observe the process you’re automating. When they come back, they’re very sobered.”
Dr. Misra, the Johns Hopkins intern, notes that mobile devices are perfect hosts for checklists. Their ease of use can even be viewed as a potential motivator to ensure that those checklists are completed, particularly for younger physicians who have either grown up with or started their careers with more exposure to technology than previous generations.
“The biggest strength of touchscreen technology is it’s interactive,” Dr. Misra says. “It’s fun to use, much more fun than checking off boxes on a piece of paper or on a computer screen.
“It’s portable, it’s lightweight, it’s where you are.”
Trouble Spots
The virtually limitless boundaries for touchscreen technology to replace functions in the hospitalist’s workflow is, of course, limited in one glaring respect: privacy. The security of devices, applications, or peripherals must be paramount to their effectiveness, Dr. Feldman says, adding patient information must “remain sacrosanct.”
At BIDMC, digital security is accomplished in part via a bifurcated wireless network that allows physicians access to a secure connection while simultaneously and transparently maintaining a free wireless network for patients and visitors. Not all hospitals can afford the infrastructure necessary for such a setup. And even for health systems that have separate wireless systems, the connectivity cuts both ways, says Mike Stinson, vice president of marketing for Motion in Computing, an Austin, Texas, firm that produces tablet computers for multiple industries, including healthcare.
“Are you willing to have every file on your personal system viewable and accessible by the IT guys so they can make sure you don’t have access to something you shouldn’t have access to?” Stinson asks. “It seems easy and appealing, but there are larger issues.”
Stinson says the privacy and safety concerns of the technology can be addressed. Even potential fears regarding the sterility of the equipment might be simply solved. To wit, a column in the Journal of Surgical Radiology in January found that the device worked well when put in an X-ray cassette sealed off with a hemostat.1
Dr. Nathanson, an ED physician who has worked closely with hospitalists at BIDMC in the past, says it’s clear to him that making the technology easy enough to use in a medical setting is no longer the hurdle. It’s the systemic timidity of physicians who are slow to endorse and incorporate cutting-edge technology into entrenched work patterns.
“In medicine, it tends to take a long time,” he says. “The adoption of technology in medicine can be very challenging. If nothing else, we’re very early in the process.” TH
Richard Quinn is a freelance writer based in New Jersey.
Reference
- Wodajo, FM. The iPad in the hospital and operating room. Journal of Surgical Radiology website. Available at: www.surgisphere.com/SurgRad/issues/volume-2/1-january-2011—pages-1-112/152-column-the-ipad-in-the-hospital-and-operating-room.html. Accessed Jan. 3, 2011.
Satish Misra, MD, a first-year internal-medicine resident at Johns Hopkins School of Medicine in Baltimore, used to carry a guidebook—many schools refer to it as their Red Book—around the hospital; it served as a tutorial on how to handle a litany of common medical problems. Now, Dr. Misra mostly scans his iPhone.
Henry Feldman, MD, a hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston who also serves as chief information architect for Harvard Medical Faculty Physicians, used to lug around a bulky copy of Netter’s Anatomy if he wanted to visually explain to a patient how their endoscopic retrograde cholangiopancreatography (ERCP) would work. Now, he pulls up the medical illustrations via an application on his iPad.
In an increasingly technological society in which there is an “app” for nearly everything, healthcare—and HM in particular—is no exception. The growing prevalence of touchscreen technology, mostly via smartphones and tablet computers, already has had an impact on how some hospitalists do their jobs. That upward trend should continue in the coming years, as both hardware and software technology become even more sophisticated and easy to use.
Of course, there are roadblocks. Patient privacy, wireless security, and the well-known reticence of healthcare as an industry to adopt information technology (IT) changes have—and will continue to—slowed the spread of the new technologies. However, with potential or practical usage already being forged in the arenas of patient interaction, billing and coding, and quality and patient safety initiatives, the integration of interactive devices into a physician’s daily workflow could become as commonplace in 10 years as the presence of hospitalists is today.
Still, the CEO of one software company points out that the presence of innovation alone does not translate to efficacy. The value of mobile and touchscreen technology to hospitalists—both from the hardware and the software perspectives—lies in how much a physician chooses to incorporate it into their daily practice.
“The number-one factor in these things being adopted is: Can you improve the quality of documentation … without negatively impacting a physician’s interaction with the patient?” says Todd Johnson, president of Salar Inc., a Baltimore-based firm that develops software applications for clinical documentation. Touchscreen technology “absolutely does help meet that goal, but it depends on the providers. It truly is different strokes for different folks.”
Steven Peskin, MD, MBA, FACP, executive vice president and CMO of Yardley, Pa.-based MediMedia USA, has long preached the value of digital technology for inpatient care, particularly for hospitalists. He categorizes the latest wave of technology into five silos:
- Smartphones: Powered by operating systems that turn them into pocket-size mini-computers, the smallest and most mobile of these technologies are ubiquitous in society and hospitals alike (see Table 1, right).
- Tablet PCs: Led by the iPad’s debut in April 2010, the product is a larger version of the smartphone; the oversized screen makes it practical to use as a virtual chalkboard to explain topics to patients.
- Peripherals: From blood pressure cuffs produced by iHealth Labs (www.ihealth99.com) and Withings (www.withings.com/en/bloodpressuremonitor) to Mobisante’s prototype plug-in ultrasound probe (www.technologyreview.com/biomedicine/), there is a burgeoning marketplace for devices that serve as accessories to a smartphone or tablet, effectively turning those devices into handheld versions of costly machines. Most are connected to a mobile device via simple plug-in cables.
- Applications: According to Dr. Feldman, “It’s not the mobile device that’s the gate to any of this. It’s the applications you interact with.” App stores already feature medical specialty sections, and the number of offerings is expected to grow exponentially in the coming years.
- Cloud computing: A cloud is a metaphorical moniker for the interactivity and interoperability of different devices, systems, and servers to provide immediate connectivity and access to remote data and processes (http://csrc.nist.gov/groups/SNS/cloud-computing/).

“There’s tremendous potential and power of medical computing systems out there, but the stumbling block is they’re bulky or not effective,” says Larry Nathanson, MD, director of emergency medical informatics for BIDMC’s Department of Emergency Medicine, who served as architect and programmer of the ED Dashboard, the information system that is used at BIDMC and a number of other hospitals. “By improving the user interface, the systems become easier to use and the systems become revolutionary.”
Impact: Cloudy, Optimistic
Experts agree that the exact role mobile and touchscreen technologies will play in hospitalist groups around the country remains murky because the field is still a novel one, mostly devoid of evidence-based conclusions. In one of the first planned research studies, the two-year-old University of Central Florida College of Medicine in Orlando has provided iPads to each student in order to research the use of technology in medical education.
Regardless, physicians and tablet manufacturers alike agree that the point-of-service efficiency offered by mobile devices inherently allows their users to be more efficient. Several hospitalists have taken to the Internet, touting how mobile devices have streamlined their efficiency. One popular (and anonymous) blogger, The Happy Hospitalist (http://thehappyhospitalist.blogspot.com/), noted in two recent posts how they were able to round on 16 patients in less than 4 1/2 hours using an iPhone or iPad. On one of those days, the blogger discharged 13 of those patients.
“I no longer have to walk back and forth between patient rooms and nursing stations,” according to The Happy Hospitalist. “I can just drink my coffee at the bedside. I don’t have to fight with other doctors and nurses to log into a paucity of computers that are often way too slow and way too unpredictable. I just sync my iPhone with the patient database app on my iPhone screen and I’m up and running with a real-time update of all my patient’s information.”
The mobile devices allow faster, possibly better, interactions with patients, Dr. Feldman says. For example, a patient tells their hospitalist they need a change to their pain medication. Having a handheld touchscreen device linked to other technologies allows the order to be placed instantly. It even can send the nursing station an alert to the change. The sloppiness of a handwritten note is taken out of play; plus, rounding never misses a beat. “I’m terrible at remembering what I wrote down six patients ago,” Dr. Feldman admits. “Ultimately, for saving money, if I can get things done sooner, theoretically, length of stay can be reduced. That hasn’t been studied, but it is common sense.”
Dr. Feldman, who describes himself as a “hardcore code jockey,” says hospitalists would do well to work closely with their IT staffs to help conceptualize and design in-house applications and interoperability that would make their jobs easier. In institutions with an informatics department, that conversation could be as simple as a one-on-one conversation between an HM group leader and the IT department head.
In other hospitals, a field trip can help. “We will take IT staff out on the wards,” Dr. Feldman explains. “Come observe the process you’re automating. When they come back, they’re very sobered.”
Dr. Misra, the Johns Hopkins intern, notes that mobile devices are perfect hosts for checklists. Their ease of use can even be viewed as a potential motivator to ensure that those checklists are completed, particularly for younger physicians who have either grown up with or started their careers with more exposure to technology than previous generations.
“The biggest strength of touchscreen technology is it’s interactive,” Dr. Misra says. “It’s fun to use, much more fun than checking off boxes on a piece of paper or on a computer screen.
“It’s portable, it’s lightweight, it’s where you are.”
Trouble Spots
The virtually limitless boundaries for touchscreen technology to replace functions in the hospitalist’s workflow is, of course, limited in one glaring respect: privacy. The security of devices, applications, or peripherals must be paramount to their effectiveness, Dr. Feldman says, adding patient information must “remain sacrosanct.”
At BIDMC, digital security is accomplished in part via a bifurcated wireless network that allows physicians access to a secure connection while simultaneously and transparently maintaining a free wireless network for patients and visitors. Not all hospitals can afford the infrastructure necessary for such a setup. And even for health systems that have separate wireless systems, the connectivity cuts both ways, says Mike Stinson, vice president of marketing for Motion in Computing, an Austin, Texas, firm that produces tablet computers for multiple industries, including healthcare.
“Are you willing to have every file on your personal system viewable and accessible by the IT guys so they can make sure you don’t have access to something you shouldn’t have access to?” Stinson asks. “It seems easy and appealing, but there are larger issues.”
Stinson says the privacy and safety concerns of the technology can be addressed. Even potential fears regarding the sterility of the equipment might be simply solved. To wit, a column in the Journal of Surgical Radiology in January found that the device worked well when put in an X-ray cassette sealed off with a hemostat.1
Dr. Nathanson, an ED physician who has worked closely with hospitalists at BIDMC in the past, says it’s clear to him that making the technology easy enough to use in a medical setting is no longer the hurdle. It’s the systemic timidity of physicians who are slow to endorse and incorporate cutting-edge technology into entrenched work patterns.
“In medicine, it tends to take a long time,” he says. “The adoption of technology in medicine can be very challenging. If nothing else, we’re very early in the process.” TH
Richard Quinn is a freelance writer based in New Jersey.
Reference
- Wodajo, FM. The iPad in the hospital and operating room. Journal of Surgical Radiology website. Available at: www.surgisphere.com/SurgRad/issues/volume-2/1-january-2011—pages-1-112/152-column-the-ipad-in-the-hospital-and-operating-room.html. Accessed Jan. 3, 2011.