User login
ANSWER
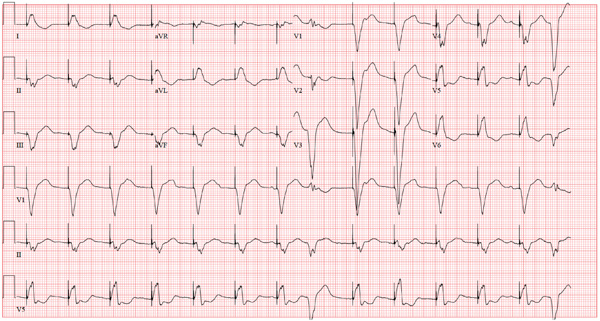
The ECG reveals an atrial-sensed and ventricular-paced rhythm of 83 beats/min. In this case, the pacemaker is functioning appropriately as programmed.
Pacemaker code consists of three letters: The first refers to the chamber(s) paced, the second to the chamber(s) sensed, and the third to the pacemaker’s response to a sensed beat. This patient has a pacing lead in the right atrium and one in the right ventricle and is programmed DDD. Each D in this case stands for dual: The first to indicate that both leads are programmed to pace, the second to indicate that both chambers may be sensed, and the third to indicate that the response to sensing can be either to inhibit or trigger a ventricular-paced beat in response to what happens in the atrium. Hence, there are four possible scenarios with a DDD pacemaker: AS-VS (atrial sensed-ventricle sensed; eg, intrinsic AV conduction requiring no pacing), AS-VP (atrial sensed-ventricle paced), AP-VS (atrial paced-ventricle sensed), and AP-VP (atrial paced-ventricle paced).
In this case, the atrial rate (83 beats/min) is faster than the pacemaker’s lower programmed rate. In order to see atrial pacing on the ECG, the intrinsic atrial rate would have to be less than the programmed rate of 60 beats/min. As soon as the pacemaker senses atrial conduction (either spontaneous or paced), it starts a timer (programmed at 130 ms in this case). If there is no spontaneous ventricular depolarization by the end of the timer, the pacemaker delivers an impulse to the ventricle, resulting in a paced ventricular beat. An often-made mistake (as this case illustrates) is the assumption that if one does not see pacing spikes, the pacemaker is not functioning properly.
ANSWER
The ECG reveals an atrial-sensed and ventricular-paced rhythm of 83 beats/min. In this case, the pacemaker is functioning appropriately as programmed.
Pacemaker code consists of three letters: The first refers to the chamber(s) paced, the second to the chamber(s) sensed, and the third to the pacemaker’s response to a sensed beat. This patient has a pacing lead in the right atrium and one in the right ventricle and is programmed DDD. Each D in this case stands for dual: The first to indicate that both leads are programmed to pace, the second to indicate that both chambers may be sensed, and the third to indicate that the response to sensing can be either to inhibit or trigger a ventricular-paced beat in response to what happens in the atrium. Hence, there are four possible scenarios with a DDD pacemaker: AS-VS (atrial sensed-ventricle sensed; eg, intrinsic AV conduction requiring no pacing), AS-VP (atrial sensed-ventricle paced), AP-VS (atrial paced-ventricle sensed), and AP-VP (atrial paced-ventricle paced).
In this case, the atrial rate (83 beats/min) is faster than the pacemaker’s lower programmed rate. In order to see atrial pacing on the ECG, the intrinsic atrial rate would have to be less than the programmed rate of 60 beats/min. As soon as the pacemaker senses atrial conduction (either spontaneous or paced), it starts a timer (programmed at 130 ms in this case). If there is no spontaneous ventricular depolarization by the end of the timer, the pacemaker delivers an impulse to the ventricle, resulting in a paced ventricular beat. An often-made mistake (as this case illustrates) is the assumption that if one does not see pacing spikes, the pacemaker is not functioning properly.
ANSWER
The ECG reveals an atrial-sensed and ventricular-paced rhythm of 83 beats/min. In this case, the pacemaker is functioning appropriately as programmed.
Pacemaker code consists of three letters: The first refers to the chamber(s) paced, the second to the chamber(s) sensed, and the third to the pacemaker’s response to a sensed beat. This patient has a pacing lead in the right atrium and one in the right ventricle and is programmed DDD. Each D in this case stands for dual: The first to indicate that both leads are programmed to pace, the second to indicate that both chambers may be sensed, and the third to indicate that the response to sensing can be either to inhibit or trigger a ventricular-paced beat in response to what happens in the atrium. Hence, there are four possible scenarios with a DDD pacemaker: AS-VS (atrial sensed-ventricle sensed; eg, intrinsic AV conduction requiring no pacing), AS-VP (atrial sensed-ventricle paced), AP-VS (atrial paced-ventricle sensed), and AP-VP (atrial paced-ventricle paced).
In this case, the atrial rate (83 beats/min) is faster than the pacemaker’s lower programmed rate. In order to see atrial pacing on the ECG, the intrinsic atrial rate would have to be less than the programmed rate of 60 beats/min. As soon as the pacemaker senses atrial conduction (either spontaneous or paced), it starts a timer (programmed at 130 ms in this case). If there is no spontaneous ventricular depolarization by the end of the timer, the pacemaker delivers an impulse to the ventricle, resulting in a paced ventricular beat. An often-made mistake (as this case illustrates) is the assumption that if one does not see pacing spikes, the pacemaker is not functioning properly.
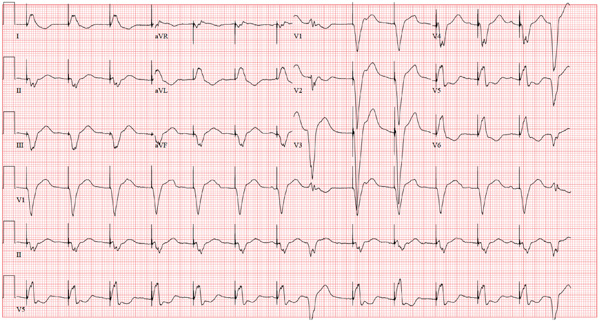
A 75-year-old man has a history of New York Heart Association Class II congestive heart failure (CHF), coronary artery disease (CAD) with coronary artery by-pass graft (CABG) surgery, and aortic stenosis with a bioprosthetic aortic valve replacement (AVR). He developed second-degree heart block (Mobitz II) following his four-vessel CABG and AVR four years ago, requiring placement of a dual-chamber pacemaker. He has been asymptomatic and plays golf two to three times per week. One week ago, he went to an urgent care center for treatment of a laceration on his leg and was told that part of his pacemaker wasn’t working. He presents to you now for follow-up on the pacemaker. Medical history is also remarkable for COPD, left inguinal hernia repair, hyperlipidemia, and bilateral cataracts. Family history is positive for CAD, diabetes, and stroke. He has a remote history of smoking and drinks one martini after each golf game. His medications include aspirin, lovastatin, and metoprolol. He has no drug allergies. The review of systems is negative except for a recent repair to a 3-cm laceration on the left leg. Physical examination reveals a well-developed, pleasant man in no distress. His height is 74” and weight, 179 lb. Blood pressure is 118/84 mm Hg; pulse, 80 beats/min and regular; respiratory rate, 14 breaths/min; temperature, 98.8°F; and O2 saturation, 97% on room air. Pertinent physical findings include a well-healed pacemaker site without signs of recent trauma. The lungs are clear in all fields, the cardiac exam is within normal limits, and there is no jugular venous distention. The abdomen is benign, and there is no peripheral edema. The laceration repair on his left leg is healing well (no erythema, induration, wound separation, or dehiscence). The pacemaker is programmed DDD at a lower rate of 60 beats/min and an upper rate of 120 beats/min, with paced and sensed atrioventricular (AV) delays programmed at 130 ms. An ECG reveals the following: a ventricular rate of 83 beats/min; PR interval, not measured; QRS duration, 162 ms; QT/QTc interval, 480/564 ms; P axis, unmeasurable; R axis, 254°; and T axis, 56°. What is your interpretation of this ECG? Is there any indication that the pacemaker is not functioning?