User login
By the year 2010, more than 20,000 hospitalists will be in practice, compared to 5000 rheumatologists and 8000 pulmonologists.13 The growth of this career option has been driven by an industry need to reduce healthcare costs, increase the emphasis on quality improvement of healthcare services, and improve the efficiency and delivery of care between that provided in the hospital and that provided by the primary care physician.49
While hospitalists' roots can be traced back to community hospitals in the late 1980s and early 1990s, this career option is now flourishing in academic centers, with the rise of hospitalist faculty and hospitalist faculty tracks.10, 11 One potential advantage of having faculty who are hospitalists is the availability and expertise of physicians who specialize in the care of hospitalized patients.8, 12 Additionally, hospitalist faculty have been reported to achieve high resident satisfaction scores, increase understanding of cost‐effective measures, and improve the supervision of hospital procedures.12 To our knowledge, the medical literature does not provide an estimate of the percentage of internal medicine residency programs utilizing hospitalist faculty.
Critics of hospitalist faculty point to the potential loss of teaching opportunities from shorter hospital stays, bemoan the decreased physician‐patient continuity between inpatient and outpatient arenas, and fear that the hospitalists' presence may decrease resident autonomy and decrease subspecialty consultations by fellows.5, 13, 14 Hospitalist faculty need development, education, and training to match the teaching activities they are expected to fulfill. The challenge is for hospitalist societies and national residency organizations to define, plan for, and meet their faculty development needs.
Goals
The goals of this study were to describe the current involvement of hospitalists in internal medicine residencies. More specifically, we wanted to determine: (1) the percentage of programs with hospitalists as faculty, (2) the teaching activities of hospitalists, (3) regional differences in academic hospitalist activity, and (4) the number of programs with hospitalist training tracks.
Materials and Methods
Questionnaire Development
The Survey Committee of the Association of Program Directors in Internal Medicine (APDIM) is charged with developing questionnaires to track the baseline characteristics of the 391 internal medicine residencies in the United States as well as to address current issues facing residencies and residency directors. The Survey Committee's goal is to create a longitudinal data warehouse to: (1) track changes over time, (2) create valid outcome measures, and (3) facilitate educational studies and interventions. Two of the authors (B.B. and F.M.) were members of this committee. This work contains results from 2 successive questionnaires.
The first questionnaire, completed in 2005, and its administration have been described in our previous reports.1517 The second, completed in 2007, repeated many of the baseline characteristic questions, and introduced new questions regarding current residency issues, in particular hospitalism in residencies. Whereas the 2005 questionnaire was sent as an e‐mail attachment to the residency programs, the 2007 questionnaire used a web‐based format for completion and data collection. We e‐mailed a notification of the questionnaire with a link to the website in November 2006 to each member program of APDIM (total = 381 programs in 2006), representing 97% of the training programs in internal medicine. The directions and glossary for the questionnaire provided definitions and explained that the first section about the baseline characteristics could be completed by a program administrator or an associate program director. In both surveys, we defined the term faculty as any physician who serves as an attending or preceptor, provides lectures, noon conferences, physical diagnosis rounds, etc., or attends educational conferences (eg, morning report) on a regular basis. The survey assumed that program directors identified hospitalists as physicians whose primary professional focus is the general medical care of hospitalized patients. We asked that the program director review and approve the first section, and complete the remaining questions on his or her own. We sent subsequent request e‐mails in December 2006 and January 2007. The survey was confidential with respondents tracked by numerical codes.
Data Analysis
We used SPSS for Windows 15.0.0 (SPSS, Inc., Chicago, IL) statistics program for all analyses. Each program was categorized by setting (university‐based, community‐based, military, Veterans Administration, multispecialty group), number of residents, and the state in which the program was located. Respondents were assigned a region based upon the categorization used by the U.S. Census Bureau.18 We combined response categories for variables when we found sparsely selected responses. We examined continuous variables for evidence of skewness, outliers, and nonnormality.
In order to avoid misinterpretation of the results of multiple comparisons, we are reporting only bivariate associations that are significant at the P < 0.01 level. We used Spearman's rho to find correlations with the number of hospitalists and continuous variables. Chi‐square analyses were used to compare nominal variables. Fisher's exact test was used to compare the increase in the prevalence of hospitalists at primary teaching hospitals over time. For all the analyses we used 2‐sided tests.
Results
A total of 272 (response rate 70%) programs completed the 2005 survey, and 236 (response rate 62%) completed the 2007 survey. A total of 171 programs completed both surveys. In 2007, 15 (6%) program directors reported that they were hospitalists while 118 (50%) claimed to be traditional general internists.
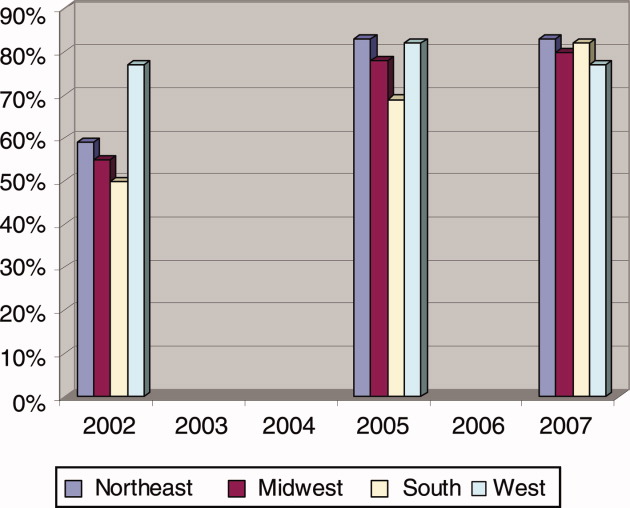
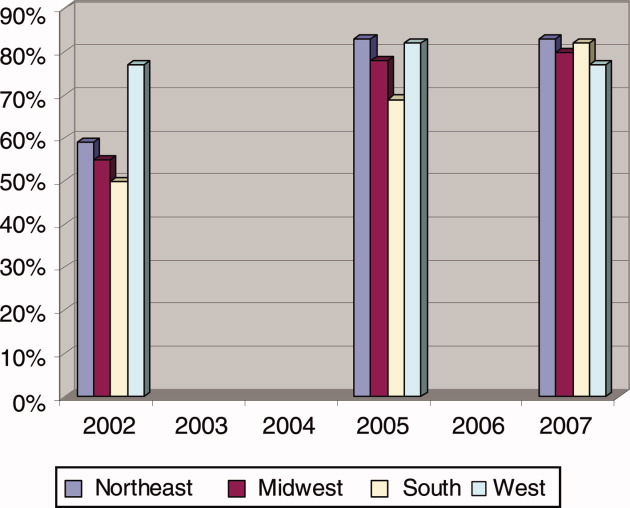
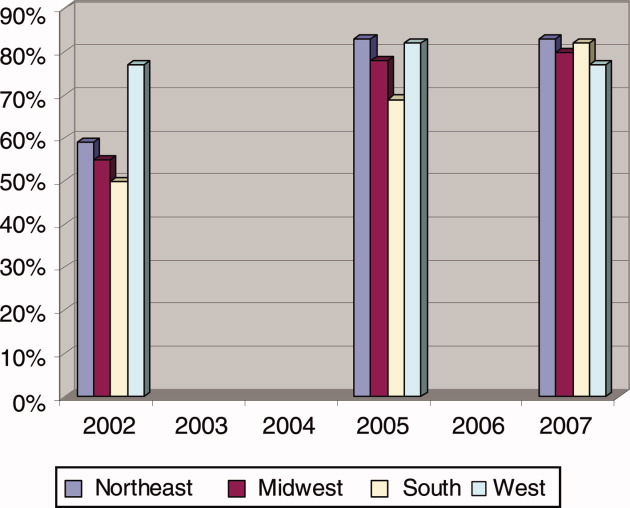
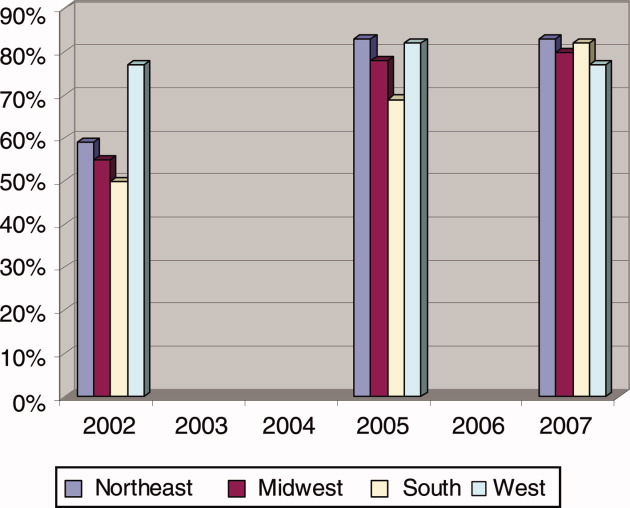
For the program directors who answered both surveys, 57% indicated that their primary teaching hospital employed hospitalists before the residency work‐hour limits were implemented (before June 2002). At the time of the survey in 2005, 77% said that hospitalists were employed, a 20% increase in 3 years. When we surveyed these same programs again in 2007, the proportion had risen to 81% (Fisher's exact P = 0.02 compared to before work‐hour limits; Figure 1).
Hospitalist Data from 2007
Eighty‐three percent of program directors identified using hospitalists as a part of their residency faculty. There was no significant difference between community‐based and university‐based residency programs (Table 1). There was an expected positive correlation (Spearman rho = 0.39, P < 0.001) between the total number of hospital beds and the number of hospitalists. The number and proportion of hospitalists had no correlation with residency program size, Residency Review Committee (RRC) cycle length (P = 0.99), or the American Board of Internal Medicine (ABIM) board exam pass rate (P = 0.60).
| Community‐Based (n = 130) | University‐Based (n = 63) | Northeast Region (n = 76) | Midwest Region (n = 53) | Southern Region (n = 59) | Western Region (n = 30) | |
|---|---|---|---|---|---|---|
| ||||||
| Does your primary teaching hospital employ hospitalists now?* | 98 (75) | 54 (86) | 61 (80) | 41 (77) | 48 (81) | 22 (73) |
| Are the hospitalists involved in teaching residents?* | 90 (91) | 47 (87) | 60 (98) | 35 (85) | 38 (79) | 22 (100) |
| If Yes, what teaching activities?* | ||||||
| Hospitalists serve as attending on resident service | 81 (92) | 43 (91) | 57 (95) | 32 (91) | 33 (87) | 20 (91) |
| Hospitalists conduct teaching rounds | 71 (79) | 39 (83) | 55 (92) | 30 (86) | 24 (63) | 18 (82) |
| Hospitalists perform direct observation of inpatient clinical skills | 60 (67) | 32 (68) | 45 (75) | 26 (74) | 20 (53) | 17 (77) |
| Hospitalists provide lectures | 56 (67) | 35 (74) | 43 (72) | 26 (74) | 19 (50) | 18 (82) |
| Hospitalists attend morning report | 43 (49) | 27 (59) | 35 (58) | 19 (54) | 19 (50) | 13 (57) |
| Hospitalists teach physical diagnosis | 41 (46) | 23 (49) | 28 (47) | 21 (60) | 14 (37) | 13 (59) |
| Hospitalists conduct interdisciplinary education rounds | 25 (28) | 18 (38) | 24 (40) | 10 (29) | 11 (29) | 7 (32) |
| Do you have a hospitalist track/focus? | 13 (11) | 6 (10) | 6 (8) | 5 (9) | 7 (12) | 5 (17) |
Teaching hospitals of the university‐based residencies employed hospitalists more often than those of community‐based programs (87% vs. 76%, P = 0.07; Table 1). And, while programs across the United States employed hospitalists at near the same proportions, programs in the Northeast (92%) and the West coast (92%) trended toward involving them in teaching residents more often (vs. Midwest 78% and South 76%, P = 0.04). Compared to programs in the Northeast, those in the Southern region generally utilize hospitalists less for common teaching activities, and in particular, significantly less (63%, P = 0.001) for conducting teaching rounds. Eleven percent of residencies had a hospitalist track or a hospitalist training focus, and this did not vary between community‐based and university‐based programs, but the Western region trended toward a higher percentage (17%, P = 0.18, compared to the Northeast 8%).
Of those programs that utilize hospitalists, program directors indicated that hospitalists contributed the following teaching activities to their residency programs (Table 1): serve as attending on resident service (92%), conduct teaching rounds (81%), perform direct observation of inpatient clinical skills (67%), provide lectures (68%), attend morning report (52%), teach physical diagnosis (48%), and conduct interdisciplinary education rounds (31%). Notable comments provided by program directors about other teaching activities of hospitalists included: accept and review night float patients, residents do inpatient consultations with hospitalists, serve as one of the associate program directors, and write curriculum updates and develop evaluation methods (ie, oral exams, multiple choice questions, etc.).
Discussion
This is the first study to document the national rise of hospitalist faculty in internal medicine residency programs. Program directors noted a 20% increase in teaching hospitals that employed hospitalists after the work‐hour regulations went into effecta trend that continued to rise. The tendency was seen first on the coasts, where managed care has higher penetration, and particularly in the Northeast, where New York's resident work‐hour reforms occurred by state mandate prior to the residency accreditation action that affected the rest of the country. Not only have hospitalists picked up the burden of service at these hospitals,19, 20 but the vast majority of programs (>80%) have utilized hospitalists as teachers in important areas of their residency. The magnitude of hospitalist involvement in residency training may have important implications.
Beyond the financial significance of hospitalists at academic teaching hospitals,21 only a few studies have addressed their impact on resident education. On the monthly evaluations at the University of California, San Francisco (San Francisco, CA), residents' satisfaction with their attendings was significantly higher when the physician was a hospitalist rather than a traditional faculty member.22 Residents believed hospitalists were more effective teachers, and provided more effective feedback. At Emory University (Atlanta, GA), a methodologically more rigorous study of postrotation assessment of faculty demonstrated that ratings of hospitalists were not different from traditional general internists; both scored higher than subspecialists.23 The hospitalists as a group had completed training more recently, which also was associated with higher scores.
Even community hospitals that sponsor residency programs have benefited from hospitalist faculty. At Norwalk Hospital (Norwalk, CT), the program had used resident teams led by a group of community physicians and a small group of employed internists. But time pressures and reimbursement concerns created tension between the workload and education balance. After hiring 2 hospitalist clinician‐educators, the length of stay and cost per case were substantially reduced, while resident evaluations indicated improved teaching rounds, conferences, and bedside teaching.24
The results of our study fit with the role of hospitalists as well as what individual programs have reported about hospitalist faculty in the past. Hospitalist faculty serve by and large (92%) as attendings on the hospital ward services. Theoretically, who better to have round with residents in the hospital than the specialists of hospital medicine. For a pulmonary curricular experience, residents work with pulmonologists. But beyond serving as attendings in the hospital, they perform the traditional functions of hospital attendings: providing teaching rounds (>80%), evaluating clinical skills (67%), and even lecturing to residents (>65%). The Southern region trends toward slower adoption of hospitalists as faculty, particularly compared with the Northeast. Overall, what is striking is how much hospitalist faculty already are filling the roles expected of all academic faculty.
We found that only 11% of programs have a hospitalist track through which internal medicine residents may develop the specialized skills and knowledge needed to function optimally in a hospitalist career.25 But given the rapid growth of this specialty, we might expect to see a similar rise in programs providing such specialized training.
Are there risks to having hospitalists teaching residents? One concern is the potential to model fragmented medical care to trainees when hospitals and ambulatory health systems neglect to ensure quality handoffs.26 In an era that heralds the demise of the primary care general internist,27 the impact of hospitalist faculty on general internal medicine nationally, the gravitation of residents toward or away from hospitalist and ambulatory careers, and the role of the traditional general internist in residency training programs in the future remain to be seen. These were not addressed by our data, but are ripe areas for study.
This study has several limitations. It relies on self‐reported data from program directors that, while knowing the intimate details of their educational program, may not have exact knowledge of the number of hospitalists employed by their hospitals. There is also the potential for recall bias by asking the group to remember the number of hospitalists before duty‐hour implementation. Both points in time of our 2 surveys (2005 and 2007) were after the incident growth of hospital medicine as evidenced by the high prevalence of hospitalists in both surveys. Yet, most program directors know that the service needs of the hospitals were acutely increased when the duty‐hours policies went into affect, and probably were fairly involved in hospital decisions to utilize hospitalist physicians to meet these needs. Finally, our study does not address hospitalism within the family medicine and pediatric specialties, both of which have a significant stake in hospital medicine.
In conclusion, our study documents the recent growth and current prevalence of hospitalists' activities in the teaching hospitals of internal medicine residencies in the United States, the duties they perform in resident education, and the magnitude of their penetration in the geographic regions of the country, both in community‐based and university‐based programs. The high degree of involvement of hospitalists in resident education may have important implications for the future of internal medicine as a discipline both with regard to the need for academic faculty development of this important sector of the education community as well as for the education and career development of the residents whom they train.
Acknowledgements
The authors thank the Mayo Clinic Survey Research Center for their assistance with survey design and data collection.
- , , , et al.Implementation of a voluntary hospitalist service at a community teaching hospital; improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- , , , et al.The United States rheumatology workforce: supply and demand, 2005–2025.Arthritis Rheum.2007;56(3):722–729.
- , , , , ;Committee on Manpower for Pulmonary and Critical Care Societies.Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population?JAMA.2000;284(21):2762–2770.
- , .The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- , , , , .Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education.JAMA.1998;279:1560–1565.
- , , .The effect of full‐time faculty hospitalists on the efficiency of care at a community teaching hospital.Ann Intern Med.1998;129:197–203.
- .An introduction to the hospitalist model.Ann Intern Med.1999;130:338–342.
- , .The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- , , , , .What effect does inpatient physician specialty and experience have on clinical outcomes and resource utilization on a general medical service?J Gen Intern Med.2004;19:395–401.
- , , , et al.The presence of hospitalists in medical education.Acad Med.2000;75(suppl):S34–S36.
- , , , et al.Assessing the value of hospitalists to academic health centers: Brigham and Women's Hospital and Harvard Medical School.Am J Med.1999;106:134–137.
- , .Role of hospitalists in medical education.Am J Med.1999;107(4):305–309.
- , .The hospitalists: new boon for internal medicine or retreat from primary care?Ann Intern Med.1999;130:382–387.
- .The hospitalist movement: caution lights flashing at the crossroads.Am J Med.1999;107:409–413.
- , , .The state of competency evaluation in internal medicine residency.J Gen Intern Med.2008;23(7):1010–1015.
- , , .Sources of satisfaction for residency program directors: a second administration of the PD‐Sat.Am J Med.2009;122(2):196–201.
- , , .What predicts residency accreditation cycle length?Acad Med.2009;84(3):356–361.
- U.S. Census Bureau. Census Regions and Divisions of the United States. Available at: http://www.census.gov/geo/www/us_regdiv.pdf. Accessed May 2009.
- , , , et al.Complying with ACGME resident duty hours restrictions: restructuring the 80‐hour workweek to enhance education and patient safety at Texas A81(12):1026–1031.
- Association of Program Directors in Internal Medicine;, , , , .Redesigning residency education in internal medicine: a position paper from the Association of Program Directors in Internal Medicine.Ann Intern Med.2006;144(12):920–926.
- , , , et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137(11):866–874.
- , , , , .Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1871.
- , , , et al.Hospitalists as teachers.J Gen Intern Med.2004;19(1):8–15.
- , , , et al.The positive impact of initiation of hospitalist clinician educators.J Gen Intern Med.2004;19(4):293–301.
- , , , , .How to use The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1:48–56.
- .The hospitalist model: perspectives of the patient, the internist, and internal medicine.Ann Intern Med.1999;130:368–372.
- American College of Physicians. The impending collapse of primary care medicine and its implications for the state of the nation's health care: a report from the American College of Physicians. January 30,2006. Available at: http://www.acponline.org/advocacy/events/state_of_healthcare/statehc06_1.pdf. Accessed May 2009.
By the year 2010, more than 20,000 hospitalists will be in practice, compared to 5000 rheumatologists and 8000 pulmonologists.13 The growth of this career option has been driven by an industry need to reduce healthcare costs, increase the emphasis on quality improvement of healthcare services, and improve the efficiency and delivery of care between that provided in the hospital and that provided by the primary care physician.49
While hospitalists' roots can be traced back to community hospitals in the late 1980s and early 1990s, this career option is now flourishing in academic centers, with the rise of hospitalist faculty and hospitalist faculty tracks.10, 11 One potential advantage of having faculty who are hospitalists is the availability and expertise of physicians who specialize in the care of hospitalized patients.8, 12 Additionally, hospitalist faculty have been reported to achieve high resident satisfaction scores, increase understanding of cost‐effective measures, and improve the supervision of hospital procedures.12 To our knowledge, the medical literature does not provide an estimate of the percentage of internal medicine residency programs utilizing hospitalist faculty.
Critics of hospitalist faculty point to the potential loss of teaching opportunities from shorter hospital stays, bemoan the decreased physician‐patient continuity between inpatient and outpatient arenas, and fear that the hospitalists' presence may decrease resident autonomy and decrease subspecialty consultations by fellows.5, 13, 14 Hospitalist faculty need development, education, and training to match the teaching activities they are expected to fulfill. The challenge is for hospitalist societies and national residency organizations to define, plan for, and meet their faculty development needs.
Goals
The goals of this study were to describe the current involvement of hospitalists in internal medicine residencies. More specifically, we wanted to determine: (1) the percentage of programs with hospitalists as faculty, (2) the teaching activities of hospitalists, (3) regional differences in academic hospitalist activity, and (4) the number of programs with hospitalist training tracks.
Materials and Methods
Questionnaire Development
The Survey Committee of the Association of Program Directors in Internal Medicine (APDIM) is charged with developing questionnaires to track the baseline characteristics of the 391 internal medicine residencies in the United States as well as to address current issues facing residencies and residency directors. The Survey Committee's goal is to create a longitudinal data warehouse to: (1) track changes over time, (2) create valid outcome measures, and (3) facilitate educational studies and interventions. Two of the authors (B.B. and F.M.) were members of this committee. This work contains results from 2 successive questionnaires.
The first questionnaire, completed in 2005, and its administration have been described in our previous reports.1517 The second, completed in 2007, repeated many of the baseline characteristic questions, and introduced new questions regarding current residency issues, in particular hospitalism in residencies. Whereas the 2005 questionnaire was sent as an e‐mail attachment to the residency programs, the 2007 questionnaire used a web‐based format for completion and data collection. We e‐mailed a notification of the questionnaire with a link to the website in November 2006 to each member program of APDIM (total = 381 programs in 2006), representing 97% of the training programs in internal medicine. The directions and glossary for the questionnaire provided definitions and explained that the first section about the baseline characteristics could be completed by a program administrator or an associate program director. In both surveys, we defined the term faculty as any physician who serves as an attending or preceptor, provides lectures, noon conferences, physical diagnosis rounds, etc., or attends educational conferences (eg, morning report) on a regular basis. The survey assumed that program directors identified hospitalists as physicians whose primary professional focus is the general medical care of hospitalized patients. We asked that the program director review and approve the first section, and complete the remaining questions on his or her own. We sent subsequent request e‐mails in December 2006 and January 2007. The survey was confidential with respondents tracked by numerical codes.
Data Analysis
We used SPSS for Windows 15.0.0 (SPSS, Inc., Chicago, IL) statistics program for all analyses. Each program was categorized by setting (university‐based, community‐based, military, Veterans Administration, multispecialty group), number of residents, and the state in which the program was located. Respondents were assigned a region based upon the categorization used by the U.S. Census Bureau.18 We combined response categories for variables when we found sparsely selected responses. We examined continuous variables for evidence of skewness, outliers, and nonnormality.
In order to avoid misinterpretation of the results of multiple comparisons, we are reporting only bivariate associations that are significant at the P < 0.01 level. We used Spearman's rho to find correlations with the number of hospitalists and continuous variables. Chi‐square analyses were used to compare nominal variables. Fisher's exact test was used to compare the increase in the prevalence of hospitalists at primary teaching hospitals over time. For all the analyses we used 2‐sided tests.
Results
A total of 272 (response rate 70%) programs completed the 2005 survey, and 236 (response rate 62%) completed the 2007 survey. A total of 171 programs completed both surveys. In 2007, 15 (6%) program directors reported that they were hospitalists while 118 (50%) claimed to be traditional general internists.
For the program directors who answered both surveys, 57% indicated that their primary teaching hospital employed hospitalists before the residency work‐hour limits were implemented (before June 2002). At the time of the survey in 2005, 77% said that hospitalists were employed, a 20% increase in 3 years. When we surveyed these same programs again in 2007, the proportion had risen to 81% (Fisher's exact P = 0.02 compared to before work‐hour limits; Figure 1).
Hospitalist Data from 2007
Eighty‐three percent of program directors identified using hospitalists as a part of their residency faculty. There was no significant difference between community‐based and university‐based residency programs (Table 1). There was an expected positive correlation (Spearman rho = 0.39, P < 0.001) between the total number of hospital beds and the number of hospitalists. The number and proportion of hospitalists had no correlation with residency program size, Residency Review Committee (RRC) cycle length (P = 0.99), or the American Board of Internal Medicine (ABIM) board exam pass rate (P = 0.60).
| Community‐Based (n = 130) | University‐Based (n = 63) | Northeast Region (n = 76) | Midwest Region (n = 53) | Southern Region (n = 59) | Western Region (n = 30) | |
|---|---|---|---|---|---|---|
| ||||||
| Does your primary teaching hospital employ hospitalists now?* | 98 (75) | 54 (86) | 61 (80) | 41 (77) | 48 (81) | 22 (73) |
| Are the hospitalists involved in teaching residents?* | 90 (91) | 47 (87) | 60 (98) | 35 (85) | 38 (79) | 22 (100) |
| If Yes, what teaching activities?* | ||||||
| Hospitalists serve as attending on resident service | 81 (92) | 43 (91) | 57 (95) | 32 (91) | 33 (87) | 20 (91) |
| Hospitalists conduct teaching rounds | 71 (79) | 39 (83) | 55 (92) | 30 (86) | 24 (63) | 18 (82) |
| Hospitalists perform direct observation of inpatient clinical skills | 60 (67) | 32 (68) | 45 (75) | 26 (74) | 20 (53) | 17 (77) |
| Hospitalists provide lectures | 56 (67) | 35 (74) | 43 (72) | 26 (74) | 19 (50) | 18 (82) |
| Hospitalists attend morning report | 43 (49) | 27 (59) | 35 (58) | 19 (54) | 19 (50) | 13 (57) |
| Hospitalists teach physical diagnosis | 41 (46) | 23 (49) | 28 (47) | 21 (60) | 14 (37) | 13 (59) |
| Hospitalists conduct interdisciplinary education rounds | 25 (28) | 18 (38) | 24 (40) | 10 (29) | 11 (29) | 7 (32) |
| Do you have a hospitalist track/focus? | 13 (11) | 6 (10) | 6 (8) | 5 (9) | 7 (12) | 5 (17) |
Teaching hospitals of the university‐based residencies employed hospitalists more often than those of community‐based programs (87% vs. 76%, P = 0.07; Table 1). And, while programs across the United States employed hospitalists at near the same proportions, programs in the Northeast (92%) and the West coast (92%) trended toward involving them in teaching residents more often (vs. Midwest 78% and South 76%, P = 0.04). Compared to programs in the Northeast, those in the Southern region generally utilize hospitalists less for common teaching activities, and in particular, significantly less (63%, P = 0.001) for conducting teaching rounds. Eleven percent of residencies had a hospitalist track or a hospitalist training focus, and this did not vary between community‐based and university‐based programs, but the Western region trended toward a higher percentage (17%, P = 0.18, compared to the Northeast 8%).
Of those programs that utilize hospitalists, program directors indicated that hospitalists contributed the following teaching activities to their residency programs (Table 1): serve as attending on resident service (92%), conduct teaching rounds (81%), perform direct observation of inpatient clinical skills (67%), provide lectures (68%), attend morning report (52%), teach physical diagnosis (48%), and conduct interdisciplinary education rounds (31%). Notable comments provided by program directors about other teaching activities of hospitalists included: accept and review night float patients, residents do inpatient consultations with hospitalists, serve as one of the associate program directors, and write curriculum updates and develop evaluation methods (ie, oral exams, multiple choice questions, etc.).
Discussion
This is the first study to document the national rise of hospitalist faculty in internal medicine residency programs. Program directors noted a 20% increase in teaching hospitals that employed hospitalists after the work‐hour regulations went into effecta trend that continued to rise. The tendency was seen first on the coasts, where managed care has higher penetration, and particularly in the Northeast, where New York's resident work‐hour reforms occurred by state mandate prior to the residency accreditation action that affected the rest of the country. Not only have hospitalists picked up the burden of service at these hospitals,19, 20 but the vast majority of programs (>80%) have utilized hospitalists as teachers in important areas of their residency. The magnitude of hospitalist involvement in residency training may have important implications.
Beyond the financial significance of hospitalists at academic teaching hospitals,21 only a few studies have addressed their impact on resident education. On the monthly evaluations at the University of California, San Francisco (San Francisco, CA), residents' satisfaction with their attendings was significantly higher when the physician was a hospitalist rather than a traditional faculty member.22 Residents believed hospitalists were more effective teachers, and provided more effective feedback. At Emory University (Atlanta, GA), a methodologically more rigorous study of postrotation assessment of faculty demonstrated that ratings of hospitalists were not different from traditional general internists; both scored higher than subspecialists.23 The hospitalists as a group had completed training more recently, which also was associated with higher scores.
Even community hospitals that sponsor residency programs have benefited from hospitalist faculty. At Norwalk Hospital (Norwalk, CT), the program had used resident teams led by a group of community physicians and a small group of employed internists. But time pressures and reimbursement concerns created tension between the workload and education balance. After hiring 2 hospitalist clinician‐educators, the length of stay and cost per case were substantially reduced, while resident evaluations indicated improved teaching rounds, conferences, and bedside teaching.24
The results of our study fit with the role of hospitalists as well as what individual programs have reported about hospitalist faculty in the past. Hospitalist faculty serve by and large (92%) as attendings on the hospital ward services. Theoretically, who better to have round with residents in the hospital than the specialists of hospital medicine. For a pulmonary curricular experience, residents work with pulmonologists. But beyond serving as attendings in the hospital, they perform the traditional functions of hospital attendings: providing teaching rounds (>80%), evaluating clinical skills (67%), and even lecturing to residents (>65%). The Southern region trends toward slower adoption of hospitalists as faculty, particularly compared with the Northeast. Overall, what is striking is how much hospitalist faculty already are filling the roles expected of all academic faculty.
We found that only 11% of programs have a hospitalist track through which internal medicine residents may develop the specialized skills and knowledge needed to function optimally in a hospitalist career.25 But given the rapid growth of this specialty, we might expect to see a similar rise in programs providing such specialized training.
Are there risks to having hospitalists teaching residents? One concern is the potential to model fragmented medical care to trainees when hospitals and ambulatory health systems neglect to ensure quality handoffs.26 In an era that heralds the demise of the primary care general internist,27 the impact of hospitalist faculty on general internal medicine nationally, the gravitation of residents toward or away from hospitalist and ambulatory careers, and the role of the traditional general internist in residency training programs in the future remain to be seen. These were not addressed by our data, but are ripe areas for study.
This study has several limitations. It relies on self‐reported data from program directors that, while knowing the intimate details of their educational program, may not have exact knowledge of the number of hospitalists employed by their hospitals. There is also the potential for recall bias by asking the group to remember the number of hospitalists before duty‐hour implementation. Both points in time of our 2 surveys (2005 and 2007) were after the incident growth of hospital medicine as evidenced by the high prevalence of hospitalists in both surveys. Yet, most program directors know that the service needs of the hospitals were acutely increased when the duty‐hours policies went into affect, and probably were fairly involved in hospital decisions to utilize hospitalist physicians to meet these needs. Finally, our study does not address hospitalism within the family medicine and pediatric specialties, both of which have a significant stake in hospital medicine.
In conclusion, our study documents the recent growth and current prevalence of hospitalists' activities in the teaching hospitals of internal medicine residencies in the United States, the duties they perform in resident education, and the magnitude of their penetration in the geographic regions of the country, both in community‐based and university‐based programs. The high degree of involvement of hospitalists in resident education may have important implications for the future of internal medicine as a discipline both with regard to the need for academic faculty development of this important sector of the education community as well as for the education and career development of the residents whom they train.
Acknowledgements
The authors thank the Mayo Clinic Survey Research Center for their assistance with survey design and data collection.
By the year 2010, more than 20,000 hospitalists will be in practice, compared to 5000 rheumatologists and 8000 pulmonologists.13 The growth of this career option has been driven by an industry need to reduce healthcare costs, increase the emphasis on quality improvement of healthcare services, and improve the efficiency and delivery of care between that provided in the hospital and that provided by the primary care physician.49
While hospitalists' roots can be traced back to community hospitals in the late 1980s and early 1990s, this career option is now flourishing in academic centers, with the rise of hospitalist faculty and hospitalist faculty tracks.10, 11 One potential advantage of having faculty who are hospitalists is the availability and expertise of physicians who specialize in the care of hospitalized patients.8, 12 Additionally, hospitalist faculty have been reported to achieve high resident satisfaction scores, increase understanding of cost‐effective measures, and improve the supervision of hospital procedures.12 To our knowledge, the medical literature does not provide an estimate of the percentage of internal medicine residency programs utilizing hospitalist faculty.
Critics of hospitalist faculty point to the potential loss of teaching opportunities from shorter hospital stays, bemoan the decreased physician‐patient continuity between inpatient and outpatient arenas, and fear that the hospitalists' presence may decrease resident autonomy and decrease subspecialty consultations by fellows.5, 13, 14 Hospitalist faculty need development, education, and training to match the teaching activities they are expected to fulfill. The challenge is for hospitalist societies and national residency organizations to define, plan for, and meet their faculty development needs.
Goals
The goals of this study were to describe the current involvement of hospitalists in internal medicine residencies. More specifically, we wanted to determine: (1) the percentage of programs with hospitalists as faculty, (2) the teaching activities of hospitalists, (3) regional differences in academic hospitalist activity, and (4) the number of programs with hospitalist training tracks.
Materials and Methods
Questionnaire Development
The Survey Committee of the Association of Program Directors in Internal Medicine (APDIM) is charged with developing questionnaires to track the baseline characteristics of the 391 internal medicine residencies in the United States as well as to address current issues facing residencies and residency directors. The Survey Committee's goal is to create a longitudinal data warehouse to: (1) track changes over time, (2) create valid outcome measures, and (3) facilitate educational studies and interventions. Two of the authors (B.B. and F.M.) were members of this committee. This work contains results from 2 successive questionnaires.
The first questionnaire, completed in 2005, and its administration have been described in our previous reports.1517 The second, completed in 2007, repeated many of the baseline characteristic questions, and introduced new questions regarding current residency issues, in particular hospitalism in residencies. Whereas the 2005 questionnaire was sent as an e‐mail attachment to the residency programs, the 2007 questionnaire used a web‐based format for completion and data collection. We e‐mailed a notification of the questionnaire with a link to the website in November 2006 to each member program of APDIM (total = 381 programs in 2006), representing 97% of the training programs in internal medicine. The directions and glossary for the questionnaire provided definitions and explained that the first section about the baseline characteristics could be completed by a program administrator or an associate program director. In both surveys, we defined the term faculty as any physician who serves as an attending or preceptor, provides lectures, noon conferences, physical diagnosis rounds, etc., or attends educational conferences (eg, morning report) on a regular basis. The survey assumed that program directors identified hospitalists as physicians whose primary professional focus is the general medical care of hospitalized patients. We asked that the program director review and approve the first section, and complete the remaining questions on his or her own. We sent subsequent request e‐mails in December 2006 and January 2007. The survey was confidential with respondents tracked by numerical codes.
Data Analysis
We used SPSS for Windows 15.0.0 (SPSS, Inc., Chicago, IL) statistics program for all analyses. Each program was categorized by setting (university‐based, community‐based, military, Veterans Administration, multispecialty group), number of residents, and the state in which the program was located. Respondents were assigned a region based upon the categorization used by the U.S. Census Bureau.18 We combined response categories for variables when we found sparsely selected responses. We examined continuous variables for evidence of skewness, outliers, and nonnormality.
In order to avoid misinterpretation of the results of multiple comparisons, we are reporting only bivariate associations that are significant at the P < 0.01 level. We used Spearman's rho to find correlations with the number of hospitalists and continuous variables. Chi‐square analyses were used to compare nominal variables. Fisher's exact test was used to compare the increase in the prevalence of hospitalists at primary teaching hospitals over time. For all the analyses we used 2‐sided tests.
Results
A total of 272 (response rate 70%) programs completed the 2005 survey, and 236 (response rate 62%) completed the 2007 survey. A total of 171 programs completed both surveys. In 2007, 15 (6%) program directors reported that they were hospitalists while 118 (50%) claimed to be traditional general internists.
For the program directors who answered both surveys, 57% indicated that their primary teaching hospital employed hospitalists before the residency work‐hour limits were implemented (before June 2002). At the time of the survey in 2005, 77% said that hospitalists were employed, a 20% increase in 3 years. When we surveyed these same programs again in 2007, the proportion had risen to 81% (Fisher's exact P = 0.02 compared to before work‐hour limits; Figure 1).
Hospitalist Data from 2007
Eighty‐three percent of program directors identified using hospitalists as a part of their residency faculty. There was no significant difference between community‐based and university‐based residency programs (Table 1). There was an expected positive correlation (Spearman rho = 0.39, P < 0.001) between the total number of hospital beds and the number of hospitalists. The number and proportion of hospitalists had no correlation with residency program size, Residency Review Committee (RRC) cycle length (P = 0.99), or the American Board of Internal Medicine (ABIM) board exam pass rate (P = 0.60).
| Community‐Based (n = 130) | University‐Based (n = 63) | Northeast Region (n = 76) | Midwest Region (n = 53) | Southern Region (n = 59) | Western Region (n = 30) | |
|---|---|---|---|---|---|---|
| ||||||
| Does your primary teaching hospital employ hospitalists now?* | 98 (75) | 54 (86) | 61 (80) | 41 (77) | 48 (81) | 22 (73) |
| Are the hospitalists involved in teaching residents?* | 90 (91) | 47 (87) | 60 (98) | 35 (85) | 38 (79) | 22 (100) |
| If Yes, what teaching activities?* | ||||||
| Hospitalists serve as attending on resident service | 81 (92) | 43 (91) | 57 (95) | 32 (91) | 33 (87) | 20 (91) |
| Hospitalists conduct teaching rounds | 71 (79) | 39 (83) | 55 (92) | 30 (86) | 24 (63) | 18 (82) |
| Hospitalists perform direct observation of inpatient clinical skills | 60 (67) | 32 (68) | 45 (75) | 26 (74) | 20 (53) | 17 (77) |
| Hospitalists provide lectures | 56 (67) | 35 (74) | 43 (72) | 26 (74) | 19 (50) | 18 (82) |
| Hospitalists attend morning report | 43 (49) | 27 (59) | 35 (58) | 19 (54) | 19 (50) | 13 (57) |
| Hospitalists teach physical diagnosis | 41 (46) | 23 (49) | 28 (47) | 21 (60) | 14 (37) | 13 (59) |
| Hospitalists conduct interdisciplinary education rounds | 25 (28) | 18 (38) | 24 (40) | 10 (29) | 11 (29) | 7 (32) |
| Do you have a hospitalist track/focus? | 13 (11) | 6 (10) | 6 (8) | 5 (9) | 7 (12) | 5 (17) |
Teaching hospitals of the university‐based residencies employed hospitalists more often than those of community‐based programs (87% vs. 76%, P = 0.07; Table 1). And, while programs across the United States employed hospitalists at near the same proportions, programs in the Northeast (92%) and the West coast (92%) trended toward involving them in teaching residents more often (vs. Midwest 78% and South 76%, P = 0.04). Compared to programs in the Northeast, those in the Southern region generally utilize hospitalists less for common teaching activities, and in particular, significantly less (63%, P = 0.001) for conducting teaching rounds. Eleven percent of residencies had a hospitalist track or a hospitalist training focus, and this did not vary between community‐based and university‐based programs, but the Western region trended toward a higher percentage (17%, P = 0.18, compared to the Northeast 8%).
Of those programs that utilize hospitalists, program directors indicated that hospitalists contributed the following teaching activities to their residency programs (Table 1): serve as attending on resident service (92%), conduct teaching rounds (81%), perform direct observation of inpatient clinical skills (67%), provide lectures (68%), attend morning report (52%), teach physical diagnosis (48%), and conduct interdisciplinary education rounds (31%). Notable comments provided by program directors about other teaching activities of hospitalists included: accept and review night float patients, residents do inpatient consultations with hospitalists, serve as one of the associate program directors, and write curriculum updates and develop evaluation methods (ie, oral exams, multiple choice questions, etc.).
Discussion
This is the first study to document the national rise of hospitalist faculty in internal medicine residency programs. Program directors noted a 20% increase in teaching hospitals that employed hospitalists after the work‐hour regulations went into effecta trend that continued to rise. The tendency was seen first on the coasts, where managed care has higher penetration, and particularly in the Northeast, where New York's resident work‐hour reforms occurred by state mandate prior to the residency accreditation action that affected the rest of the country. Not only have hospitalists picked up the burden of service at these hospitals,19, 20 but the vast majority of programs (>80%) have utilized hospitalists as teachers in important areas of their residency. The magnitude of hospitalist involvement in residency training may have important implications.
Beyond the financial significance of hospitalists at academic teaching hospitals,21 only a few studies have addressed their impact on resident education. On the monthly evaluations at the University of California, San Francisco (San Francisco, CA), residents' satisfaction with their attendings was significantly higher when the physician was a hospitalist rather than a traditional faculty member.22 Residents believed hospitalists were more effective teachers, and provided more effective feedback. At Emory University (Atlanta, GA), a methodologically more rigorous study of postrotation assessment of faculty demonstrated that ratings of hospitalists were not different from traditional general internists; both scored higher than subspecialists.23 The hospitalists as a group had completed training more recently, which also was associated with higher scores.
Even community hospitals that sponsor residency programs have benefited from hospitalist faculty. At Norwalk Hospital (Norwalk, CT), the program had used resident teams led by a group of community physicians and a small group of employed internists. But time pressures and reimbursement concerns created tension between the workload and education balance. After hiring 2 hospitalist clinician‐educators, the length of stay and cost per case were substantially reduced, while resident evaluations indicated improved teaching rounds, conferences, and bedside teaching.24
The results of our study fit with the role of hospitalists as well as what individual programs have reported about hospitalist faculty in the past. Hospitalist faculty serve by and large (92%) as attendings on the hospital ward services. Theoretically, who better to have round with residents in the hospital than the specialists of hospital medicine. For a pulmonary curricular experience, residents work with pulmonologists. But beyond serving as attendings in the hospital, they perform the traditional functions of hospital attendings: providing teaching rounds (>80%), evaluating clinical skills (67%), and even lecturing to residents (>65%). The Southern region trends toward slower adoption of hospitalists as faculty, particularly compared with the Northeast. Overall, what is striking is how much hospitalist faculty already are filling the roles expected of all academic faculty.
We found that only 11% of programs have a hospitalist track through which internal medicine residents may develop the specialized skills and knowledge needed to function optimally in a hospitalist career.25 But given the rapid growth of this specialty, we might expect to see a similar rise in programs providing such specialized training.
Are there risks to having hospitalists teaching residents? One concern is the potential to model fragmented medical care to trainees when hospitals and ambulatory health systems neglect to ensure quality handoffs.26 In an era that heralds the demise of the primary care general internist,27 the impact of hospitalist faculty on general internal medicine nationally, the gravitation of residents toward or away from hospitalist and ambulatory careers, and the role of the traditional general internist in residency training programs in the future remain to be seen. These were not addressed by our data, but are ripe areas for study.
This study has several limitations. It relies on self‐reported data from program directors that, while knowing the intimate details of their educational program, may not have exact knowledge of the number of hospitalists employed by their hospitals. There is also the potential for recall bias by asking the group to remember the number of hospitalists before duty‐hour implementation. Both points in time of our 2 surveys (2005 and 2007) were after the incident growth of hospital medicine as evidenced by the high prevalence of hospitalists in both surveys. Yet, most program directors know that the service needs of the hospitals were acutely increased when the duty‐hours policies went into affect, and probably were fairly involved in hospital decisions to utilize hospitalist physicians to meet these needs. Finally, our study does not address hospitalism within the family medicine and pediatric specialties, both of which have a significant stake in hospital medicine.
In conclusion, our study documents the recent growth and current prevalence of hospitalists' activities in the teaching hospitals of internal medicine residencies in the United States, the duties they perform in resident education, and the magnitude of their penetration in the geographic regions of the country, both in community‐based and university‐based programs. The high degree of involvement of hospitalists in resident education may have important implications for the future of internal medicine as a discipline both with regard to the need for academic faculty development of this important sector of the education community as well as for the education and career development of the residents whom they train.
Acknowledgements
The authors thank the Mayo Clinic Survey Research Center for their assistance with survey design and data collection.
- , , , et al.Implementation of a voluntary hospitalist service at a community teaching hospital; improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- , , , et al.The United States rheumatology workforce: supply and demand, 2005–2025.Arthritis Rheum.2007;56(3):722–729.
- , , , , ;Committee on Manpower for Pulmonary and Critical Care Societies.Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population?JAMA.2000;284(21):2762–2770.
- , .The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- , , , , .Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education.JAMA.1998;279:1560–1565.
- , , .The effect of full‐time faculty hospitalists on the efficiency of care at a community teaching hospital.Ann Intern Med.1998;129:197–203.
- .An introduction to the hospitalist model.Ann Intern Med.1999;130:338–342.
- , .The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- , , , , .What effect does inpatient physician specialty and experience have on clinical outcomes and resource utilization on a general medical service?J Gen Intern Med.2004;19:395–401.
- , , , et al.The presence of hospitalists in medical education.Acad Med.2000;75(suppl):S34–S36.
- , , , et al.Assessing the value of hospitalists to academic health centers: Brigham and Women's Hospital and Harvard Medical School.Am J Med.1999;106:134–137.
- , .Role of hospitalists in medical education.Am J Med.1999;107(4):305–309.
- , .The hospitalists: new boon for internal medicine or retreat from primary care?Ann Intern Med.1999;130:382–387.
- .The hospitalist movement: caution lights flashing at the crossroads.Am J Med.1999;107:409–413.
- , , .The state of competency evaluation in internal medicine residency.J Gen Intern Med.2008;23(7):1010–1015.
- , , .Sources of satisfaction for residency program directors: a second administration of the PD‐Sat.Am J Med.2009;122(2):196–201.
- , , .What predicts residency accreditation cycle length?Acad Med.2009;84(3):356–361.
- U.S. Census Bureau. Census Regions and Divisions of the United States. Available at: http://www.census.gov/geo/www/us_regdiv.pdf. Accessed May 2009.
- , , , et al.Complying with ACGME resident duty hours restrictions: restructuring the 80‐hour workweek to enhance education and patient safety at Texas A81(12):1026–1031.
- Association of Program Directors in Internal Medicine;, , , , .Redesigning residency education in internal medicine: a position paper from the Association of Program Directors in Internal Medicine.Ann Intern Med.2006;144(12):920–926.
- , , , et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137(11):866–874.
- , , , , .Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1871.
- , , , et al.Hospitalists as teachers.J Gen Intern Med.2004;19(1):8–15.
- , , , et al.The positive impact of initiation of hospitalist clinician educators.J Gen Intern Med.2004;19(4):293–301.
- , , , , .How to use The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1:48–56.
- .The hospitalist model: perspectives of the patient, the internist, and internal medicine.Ann Intern Med.1999;130:368–372.
- American College of Physicians. The impending collapse of primary care medicine and its implications for the state of the nation's health care: a report from the American College of Physicians. January 30,2006. Available at: http://www.acponline.org/advocacy/events/state_of_healthcare/statehc06_1.pdf. Accessed May 2009.
- , , , et al.Implementation of a voluntary hospitalist service at a community teaching hospital; improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- , , , et al.The United States rheumatology workforce: supply and demand, 2005–2025.Arthritis Rheum.2007;56(3):722–729.
- , , , , ;Committee on Manpower for Pulmonary and Critical Care Societies.Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population?JAMA.2000;284(21):2762–2770.
- , .The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- , , , , .Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education.JAMA.1998;279:1560–1565.
- , , .The effect of full‐time faculty hospitalists on the efficiency of care at a community teaching hospital.Ann Intern Med.1998;129:197–203.
- .An introduction to the hospitalist model.Ann Intern Med.1999;130:338–342.
- , .The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- , , , , .What effect does inpatient physician specialty and experience have on clinical outcomes and resource utilization on a general medical service?J Gen Intern Med.2004;19:395–401.
- , , , et al.The presence of hospitalists in medical education.Acad Med.2000;75(suppl):S34–S36.
- , , , et al.Assessing the value of hospitalists to academic health centers: Brigham and Women's Hospital and Harvard Medical School.Am J Med.1999;106:134–137.
- , .Role of hospitalists in medical education.Am J Med.1999;107(4):305–309.
- , .The hospitalists: new boon for internal medicine or retreat from primary care?Ann Intern Med.1999;130:382–387.
- .The hospitalist movement: caution lights flashing at the crossroads.Am J Med.1999;107:409–413.
- , , .The state of competency evaluation in internal medicine residency.J Gen Intern Med.2008;23(7):1010–1015.
- , , .Sources of satisfaction for residency program directors: a second administration of the PD‐Sat.Am J Med.2009;122(2):196–201.
- , , .What predicts residency accreditation cycle length?Acad Med.2009;84(3):356–361.
- U.S. Census Bureau. Census Regions and Divisions of the United States. Available at: http://www.census.gov/geo/www/us_regdiv.pdf. Accessed May 2009.
- , , , et al.Complying with ACGME resident duty hours restrictions: restructuring the 80‐hour workweek to enhance education and patient safety at Texas A81(12):1026–1031.
- Association of Program Directors in Internal Medicine;, , , , .Redesigning residency education in internal medicine: a position paper from the Association of Program Directors in Internal Medicine.Ann Intern Med.2006;144(12):920–926.
- , , , et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137(11):866–874.
- , , , , .Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164:1866–1871.
- , , , et al.Hospitalists as teachers.J Gen Intern Med.2004;19(1):8–15.
- , , , et al.The positive impact of initiation of hospitalist clinician educators.J Gen Intern Med.2004;19(4):293–301.
- , , , , .How to use The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1:48–56.
- .The hospitalist model: perspectives of the patient, the internist, and internal medicine.Ann Intern Med.1999;130:368–372.
- American College of Physicians. The impending collapse of primary care medicine and its implications for the state of the nation's health care: a report from the American College of Physicians. January 30,2006. Available at: http://www.acponline.org/advocacy/events/state_of_healthcare/statehc06_1.pdf. Accessed May 2009.
Copyright © 2009 Society of Hospital Medicine