User login
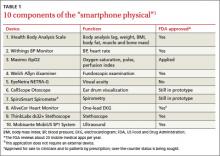
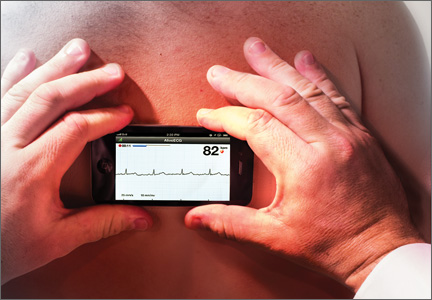
In April, hundreds of attendees at TEDMED, a conference on medical innovation, waited in line for a “smartphone physical.” Curated by Shiv Gaglani, a medical student and an editor at the medical technology journal Medgadget, the exam involved 10 apps that turn an ordinary smartphone into a medical device (TABLE 1).1 Among them were the AliveCor Heart Monitor (pictured at right), which produces a one-lead EKG in seconds when a patient’s fingers or chest are pressed against the electrodes embedded in the back of what is essentially a phone case2; a pulse oximeter, and an ultrasound that can capture images of the carotid arteries.1
All but one of the apps is paired with a physical component, such as an ultrasound wand or otoscope. The exception is SpiroSmart, an app that uses the phone’s The AliveCor app and Heart Monitor—a smartphone case fitted with sensors—can generate a one-lead EKG tracing in seconds.built-in microphone and lip reverberations to assess lung function. Shwetak Patel, PhD, of the University of Washington, one of its developers, told JFP that the accuracy of SpiroSmart has been found to be within 5% of traditional spirometry results.3
While smartphone physicals are not likely to be integrated into family practice for some time to come, Glen Stream, MD, board chair of the American Academy of Family Physicians, predicts that integration of some of their features is not too far away. “The spirometry application is an especially good one; it addresses one of the top 5 chronic conditions that contribute to health care costs,” Dr. Stream said. The apps will be beneficial, he added, as long as they “are used in a way that contributes, to, rather than detracts from, collaboration between patients and physicians.”
For now, Dr. Stream and many of his fellow FPs use mobile devices and medical apps primarily to access reference materials, both in and out of the exam room. Some have begun “prescribing” apps to tech-savvy patients. Still others have never used a medical app, either because they prefer a desktop or laptop computer to a smartphone or tablet or because, as one FP put it, "I have a dumb phone."
Wherever you fall on the spectrum, it’s a safe bet that you’re going to be increasingly inundated by the many manifestations of mobile health (mHealth).
Epocrates is No. 1 reference app
The number of medical/health apps for smart-phones or tablets is difficult to pin down; estimates range from 17,000 to more than 40,000, and growing.4 More is known about physician use of smartphones and tablets.
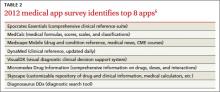
A March 2013 survey of nearly 3000 physicians found that 74% use smartphones at work and 43% use them to look up drug information.5 The favorite tool? A 2012 survey conducted by the University of Pennsylvania’s Perelman School of Medicine to identify the best medical apps put Epocrates at the top of the list (TABLE 2).6 Epocrates was the very first app cited by virtually all the FPs interviewed for this article, as well.
Other drug references cited tend to be patient-specific. Colan Kennelly, MD, a clinical educator at the Good Samaritan Family Medicine Residency in Phoenix, finds LactMed particularly useful. Developed by the National Library of Medicine and part of its Toxicology Data Network, the app lets you pull up medications quickly and see whether and how they will affect breastfeeding.
Another favorite of Kennelly’s is the Agency for Healthcare Research and Quality’s ePSS (electronic Preventive Services Selector) app designed to help primary care clinicians identify the preventive services that are appropriate for their patients. “You just plug in a patient’s age and sex”—(pregnancy, tobacco use, and whether the patient is sexually active are also considered)—“and it tells you what you should be checking for,” Dr. Kennelly said.
The benefits of mobile textbooks
Textbook apps and online texts are slowly gaining in popularity. A recent survey by Manhattan Research found that in 2013 for the first time, usage of electronic medical texts surpassed that of print editions.7 Part of the appeal is that mobile texts are easy to tote. “Apps make it possible to carry around information from a number of textbooks with no added weight,” said Richard Usatine, MD, of the University of Texas Health Science Center at San Antonio and editor of JFP’s Photo Rounds column. Dr. Usatine is also a principal of Usatine Media, which turns medical reference materials into apps.
Dr. Usatine’s own experience is a case in point. He recently used a textbook app to prepare to take his boards (for the fifth time). “I’ve brushed up each time,” he said, “but this time I really studied because it was fun.
“With a print textbook you have to cover up the answers so you don’t see them. Here, you don’t get to see the answer until you commit to one of the multiple choice answers. Then you get told what the correct answer is and why you got it right or wrong,” Dr. Usatine said. Interactivity, including the opportunity to watch a video, say, of a procedure to review how it’s done before embarking on it yourself, is a big part of the value of apps, he said.
Rx: App
In January, Eric Topol, MD, a prominent cardiologist and chief academic officer of Scripps Health in La Jolla, Calif., demonstrated the AliveCor heart monitor and other mobile devices on NBC’s Rock Center.8 In March, he went on The Colbert Report and examined Stephen Colbert’s ear with an otoscope smartphone accessory (CellScope) like the one used in Gaglani’s smartphone physical.9 Dr. Topol’s use of the mobile heart monitor to assess an airplane passenger in distress midflight also received widespread news coverage.
In response to an interviewer’s question, Dr. Topol said he is now more likely to prescribe an app than a drug.8 While it’s unlikely that any FP could make such a claim, many have begun recommending apps to tech-savvy patients.
Smartphones as symptom trackers
A January 2013 Pew Internet study found that 7 in 10 US adults track at least one health indicator, for themselves or a loved one. Six in 10 reported tracking weight, diet, or exercise, and one in 3 said they track indicators of medical problems, such as blood pressure, glucose levels, headaches, or sleep patterns—usually without the aid of a smartphone.10
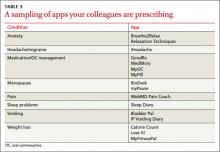
In fact, half of those who report tracking health measures said they keep the information “in their head,” and a third still use pencil and paper.10 That could change, of course, if their physicians suggest they do otherwise (TABLE 3).
Kelly M. Latimer, MD, an FP in the Navy stationed in Djibouti, Africa, routinely asks patients whether they have a smartphone and often recommends apps to those who do.
“It sounds like you have a lot of different symptoms,” she might say to a patient who complains of frequent headaches. “It will help me if you keep a headache diary.”
She used to give such patients paper and pen, Dr. Latimer noted. “Now I ask them to download the app (iHeadache, in this case) right then and there and do a quick review” so they’re ready to use it at home.
Apps are also a good way to help people with anxiety, Dr. Latimer has found. She frequently recommends apps like Relaxation Techniques and Breathe2Relax, and often suggests apps like Calorie Count and MyFitnessPal to boost patients’ efforts to lose weight and get in shape.
Abigail Lowther, MD, an FP at the University of Michigan in Ann Arbor, also recommends apps frequently. But she typically broaches the subject only with patients who have their smartphones out when she walks into the room.
Among the apps Dr. Lowther prescribes are myPause to track menopausal symptoms and Bladder Pal, a voiding diary for women struggling with incontinence. She advises women taking oral contraceptives to use the timer function on their phone to remember to take a pill at the same time every day. But there are apps (myPill, for one) that do that, too.
The upside of patient apps. A smartphone is ideal for keeping a symptom diary because it’s something that most people are never without. Anyone can use the notes function on a phone or tablet to jot down details about exacerbations, but those using disease-specific apps tend to capture more precise information. Some patients print out the information they’ve gathered and bring a hard copy to an office visit, while others simply show their physician what’s on their smartphone.
Can apps affect outcomes? There are few high-quality studies and the jury is still out, but “the smartphone has a very bright future in the world of medicine,” the authors of a review of smartphones in the medical arena concluded. After examining the use of apps to track (literally) wandering dementia patients; calculate and recommend insulin dosages for patients with type 1 diabetes; and teach yoga, to name a few, the researchers concluded that “the smartphone may one day be recognized as a diagnostic and therapeutic tool…as irreplaceable as the stethoscope.”11
Dr. Lowther recalls an obese patient who found MyFitnessPal to be helpful where other, more traditional diet programs had failed. The reason? He was less than truthful with the people overseeing the weight loss programs about what he’d eaten when he tried—and failed—to follow diets like Weight Watchers. He then ended up feeling so guilty that he abandoned the effort entirely. But, he told her, he “wouldn’t lie” to an app.
…and the downside. Even physicians who haven’t begun A weight loss app would be more likely to help this patient reach his goal than other diet programs because he "wouldn't lie" to an app.recommending apps to patients are aware that carefully tracking measures related to chronic conditions like hypertension or diabetes often results in better control. But in some cases, there may be too much of a good thing. Evidence suggests that for some patients with type 2 diabetes, glucose self-monitoring is associated with depression and may do more harm than good.12
Dr. Lowther has witnessed a similar phenomenon in patients using disease-tracking apps. “Sometimes people get too focused on the problem and drive themselves crazy,” she observed, adding that those with high blood pressure are particularly at risk. “I think sometimes it’s hard for patients to understand the concept of an average value and normal fluctuation,” Dr. Lowther said. When that happens, “I have to tell them to back off.”
Who's minding the (app) store?
The mHealth arena has been called “the wild West.”13 With at least one app for virtually every aspect of health and medicine you can think of, it’s not hard to understand why.
In an article on the use of symptom diaries in outpatient care, Bryan Hodge, DO, an FP in Hendersonville, NC, mentions mobile self-tracking apps as one of a number of ways for patients to keep symptom diaries.14 Given the fact that few of these apps have been validated, Dr. Hodge writes, “The best approach is to familiarize yourself with a few options that you can offer to your patients.”14
That depends on the nature of the app. An app that tracks calories consumed or simply keeps an organized file of patient symptoms may do little harm; an app that conveys physical measurements that a patient or physician may act on or calculates medication dosages requires a higher level of vigilance.
A recent study of smartphone apps that calculate opioid dosage conversion, for example, found a lack of consistency that raised a red flag about the reliability of information provided by unvalidated apps. Better regulation of medical apps is crucial to ensure that patient safety is maintained, the authors concluded.15
The FDA’s role
The US Food and Drug Administration, which has approved more than 75 medical apps, issued a proposed approach to its oversight of the apps in 2011.16
Under the proposed rules, the agency would regulate mobile apps that were either used as an accessory to a medical device already regulated by the FDA or that transform a smartphone or tablet into a regulated medical device. A final rule has not yet been issued, but a spokesperson told Congress that it will be forthcoming before the end of the year.17
False claims are a target of federal regulation, as well. In 2011, the Federal Trade Commission pulled 2 acne apps off the market because both advertised—without scientific evidence—that the light emitted by smartphones equipped with the apps could treat acne. “Smartphones make our lives easier in countless ways, but unfortunately, when it comes to curing acne, there’s no app for that,” the FTC chairman stated in a press release.18
In May 2013, the FDA sent an “It has come to our attention letter” to Biosense Technologies regarding its uChek urine analyzer app. The problem, the letter stated, is that the dipsticks that the app allows a mobile phone to analyze are cleared by the FDA only when interpreted by direct visual reading. But the phone and device together function “as an automated strip reader”—a urinalysis test system for which new FDA Smartphones make our lives easier in countless ways, but unfortunately, when it comes to curing acne, there's no app for that," the chairman of the Federal Trade Commission stated in a press release. clearance is required.19
Other ways of evaluating apps
Happtique, a mobile health solutions company, recently announced the launch of its Health App Certification Program—a voluntary program designed to help clinicians and patients easily identify apps that are credible and safe.20 “We will be certifying medical, health, and fitness apps, Corey Ackerman, president and CEO of Happtique, told JFP. The program is currently accepting medical education and nursing apps for review, and “discussions are underway with numerous other organizations that will provide experts for apps in additional subject matter areas,” Mr. Ackerman said.
There are other means of evaluating mobile medical apps that fall outside of the medical device realm, of course—starting by perusing the reviews posted at the app stores. Exchanging information with other clinicians using an app you’re interested in is another way to learn more about its efficacy. (Yes, there’s an app for that, too: Doximity, the professional network for clinicians.)
Other suggestions for safe use of apps:
- Peruse iMedicalApps (imedicalapps.com), the self-described leading physician publication on mobile medicine. Its physician editors and team of clinicians research and review medical apps.
- Consider the source. An app that has been developed by a medical society, federal agency, or prestigious medical school, for example, is more trustworthy than one from an unknown source (a point you would be wise to pass on to your patients).
- Try the app yourself before you recommend it to a patient.
Finally, keep the privacy provision in the Health Insurance Portability and Accountability Act in mind. Before using any app through which private patient health information can be transmitted or stored, ensure that the data will be encrypted and that your mobile device is password-protected, advises mHIMSS, the mobile branch of the Healthcare Information and Management Systems Society.21
1. TEDMED. The smartphone physical. Available at: http://www.smartphonephysical.org/tedmed.html. Accessed June 14, 2013.
2. AliveCor. AliveCor heart monitor. Available at: http://www.alivecor.com/. Accessed June 14, 2013.
3. Ubiquitous Computing Lab, University of Washington. Mobile phone spirometry. Available at: http://ubicomplab.cs.washington.edu/wiki/SpiroSmart. Accessed June 19, 2013.
4. Association of American Medical Colleges. Explosive growth in health care apps raises oversight questions. Available at: https://www.aamc.org/newsroom/reporter/october2012/308516/health-care-apps.html. Accessed June 14, 2013.
5. Alvarez A. How are physicians using smartphones for professional purposes? April 22, 2013. Available at: www.kantarmedia-healthcare.com/how-are-physicians-using-smartphones-for-professional-purposes. Accessed June 14, 2013.
6. Penn Medical Student Government. 2012 Medical app survey results. February 9, 2013. Available at: http://msg.med.upenn.edu/?p=17784. Accessed June 19, 2013.
7. Comstock J. Manhattan: 72% of physicians have tablets. April 18, 2013. Available at: http://mobihealthnews.com/21733/manhattan-72-percent-of-physicians-have-tablets/. Accessed June 19, 2013.
8. Dr. Eric Topol on NBC’s Rock Center. January 24, 2013. Available at: http://www.youtube.com/watch?v=0B-jUOOrtks. Accessed June 14, 2013.
9. Comstock J. Topol turns Colbert around on digital health. March 27, 2013. Available at: http://mobihealthnews.com/21263/topol-turns-colbert-around-on-digital-health/.Accessed June 14,2013.
10. Pew Research Center. Tracking for health. January 28, 2013. Available at: http://pewinternet.org/Press-Releases/2013/Tracking-for-health. Accessed June 14, 2013.
11. Ozdalga E, Ozdalga A, Ahuja N. The smartphone in medicine: a review of current and potential use among physicians and students. J Med Internet Res. 2012;14:e128.
12. Mendoza M, Rosenberg T. Self-management of type 2 diabetes: a good idea or not? J Fam Pract. 2013;62:244-248.
13. McMillan R. iPad: ‘Wild West’ of medical apps seeks sheriff. December 12, 2011. Available at: http://www.wired.com/wiredenterprise/2011/12/fda_apps/. Accessed June 14, 2013.
14. Hodge B. The use of symptom diaries in outpatient care. Fam Pract Manag. 2013;20:24-28.
15. Haffey F, Brady RR, Maxwell S. A comparison of the reliability of smartphone apps for opioid conversion. Drug Saf. 2013;36:111-117.
16. US Food and Drug Administration. FDA proposes health “app” guidelines. July 19, 2011. Available at: http://www.fda.gov/forconsumers/consumerupdates/ucm263332.htm. Accessed June 14, 2013.
17. Pavlovic P. 10 issues that mobile medical app developers should keep in mind. April 18, 2013. Available at: http://www.mhimss.org/news/10-issues-mobile-medical-app-developers-should-keep-mind. Accessed June 14, 2013.
18. Federal Trade Commission. “Acne cure” mobile app marketers will drop baseless claims under FTC settlements. September 8, 2011. Available at: http://www.ftc.gov/opa/2011/09/acnecure.shtm. Accessed June 14, 2013.
19. FDA. Letter to Biosense Technologies Private Limited concerning the uChek urine analyzer. Available at: http://www.fda.gov/MedicalDevices/ResourcesforYou/Industry/ucm353513.htm. Accessed June 14, 2013.
20. Happtique publishes final standards for mobile health app certification program. February 27, 2013. Available at: http://www.happtique.com/happtique-publishes-final-standards-for-mobile-health-app-certification-program/. Accessed June 19, 2013.
21. mHIMSS. Privacy and security. Available at: http://www.mhimss.org/resource-topics/privacy-security. Accessed June 14, 2013.
In April, hundreds of attendees at TEDMED, a conference on medical innovation, waited in line for a “smartphone physical.” Curated by Shiv Gaglani, a medical student and an editor at the medical technology journal Medgadget, the exam involved 10 apps that turn an ordinary smartphone into a medical device (TABLE 1).1 Among them were the AliveCor Heart Monitor (pictured at right), which produces a one-lead EKG in seconds when a patient’s fingers or chest are pressed against the electrodes embedded in the back of what is essentially a phone case2; a pulse oximeter, and an ultrasound that can capture images of the carotid arteries.1
All but one of the apps is paired with a physical component, such as an ultrasound wand or otoscope. The exception is SpiroSmart, an app that uses the phone’s The AliveCor app and Heart Monitor—a smartphone case fitted with sensors—can generate a one-lead EKG tracing in seconds.built-in microphone and lip reverberations to assess lung function. Shwetak Patel, PhD, of the University of Washington, one of its developers, told JFP that the accuracy of SpiroSmart has been found to be within 5% of traditional spirometry results.3
While smartphone physicals are not likely to be integrated into family practice for some time to come, Glen Stream, MD, board chair of the American Academy of Family Physicians, predicts that integration of some of their features is not too far away. “The spirometry application is an especially good one; it addresses one of the top 5 chronic conditions that contribute to health care costs,” Dr. Stream said. The apps will be beneficial, he added, as long as they “are used in a way that contributes, to, rather than detracts from, collaboration between patients and physicians.”
For now, Dr. Stream and many of his fellow FPs use mobile devices and medical apps primarily to access reference materials, both in and out of the exam room. Some have begun “prescribing” apps to tech-savvy patients. Still others have never used a medical app, either because they prefer a desktop or laptop computer to a smartphone or tablet or because, as one FP put it, "I have a dumb phone."
Wherever you fall on the spectrum, it’s a safe bet that you’re going to be increasingly inundated by the many manifestations of mobile health (mHealth).
Epocrates is No. 1 reference app
The number of medical/health apps for smart-phones or tablets is difficult to pin down; estimates range from 17,000 to more than 40,000, and growing.4 More is known about physician use of smartphones and tablets.
A March 2013 survey of nearly 3000 physicians found that 74% use smartphones at work and 43% use them to look up drug information.5 The favorite tool? A 2012 survey conducted by the University of Pennsylvania’s Perelman School of Medicine to identify the best medical apps put Epocrates at the top of the list (TABLE 2).6 Epocrates was the very first app cited by virtually all the FPs interviewed for this article, as well.
Other drug references cited tend to be patient-specific. Colan Kennelly, MD, a clinical educator at the Good Samaritan Family Medicine Residency in Phoenix, finds LactMed particularly useful. Developed by the National Library of Medicine and part of its Toxicology Data Network, the app lets you pull up medications quickly and see whether and how they will affect breastfeeding.
Another favorite of Kennelly’s is the Agency for Healthcare Research and Quality’s ePSS (electronic Preventive Services Selector) app designed to help primary care clinicians identify the preventive services that are appropriate for their patients. “You just plug in a patient’s age and sex”—(pregnancy, tobacco use, and whether the patient is sexually active are also considered)—“and it tells you what you should be checking for,” Dr. Kennelly said.
The benefits of mobile textbooks
Textbook apps and online texts are slowly gaining in popularity. A recent survey by Manhattan Research found that in 2013 for the first time, usage of electronic medical texts surpassed that of print editions.7 Part of the appeal is that mobile texts are easy to tote. “Apps make it possible to carry around information from a number of textbooks with no added weight,” said Richard Usatine, MD, of the University of Texas Health Science Center at San Antonio and editor of JFP’s Photo Rounds column. Dr. Usatine is also a principal of Usatine Media, which turns medical reference materials into apps.
Dr. Usatine’s own experience is a case in point. He recently used a textbook app to prepare to take his boards (for the fifth time). “I’ve brushed up each time,” he said, “but this time I really studied because it was fun.
“With a print textbook you have to cover up the answers so you don’t see them. Here, you don’t get to see the answer until you commit to one of the multiple choice answers. Then you get told what the correct answer is and why you got it right or wrong,” Dr. Usatine said. Interactivity, including the opportunity to watch a video, say, of a procedure to review how it’s done before embarking on it yourself, is a big part of the value of apps, he said.
Rx: App
In January, Eric Topol, MD, a prominent cardiologist and chief academic officer of Scripps Health in La Jolla, Calif., demonstrated the AliveCor heart monitor and other mobile devices on NBC’s Rock Center.8 In March, he went on The Colbert Report and examined Stephen Colbert’s ear with an otoscope smartphone accessory (CellScope) like the one used in Gaglani’s smartphone physical.9 Dr. Topol’s use of the mobile heart monitor to assess an airplane passenger in distress midflight also received widespread news coverage.
In response to an interviewer’s question, Dr. Topol said he is now more likely to prescribe an app than a drug.8 While it’s unlikely that any FP could make such a claim, many have begun recommending apps to tech-savvy patients.
Smartphones as symptom trackers
A January 2013 Pew Internet study found that 7 in 10 US adults track at least one health indicator, for themselves or a loved one. Six in 10 reported tracking weight, diet, or exercise, and one in 3 said they track indicators of medical problems, such as blood pressure, glucose levels, headaches, or sleep patterns—usually without the aid of a smartphone.10
In fact, half of those who report tracking health measures said they keep the information “in their head,” and a third still use pencil and paper.10 That could change, of course, if their physicians suggest they do otherwise (TABLE 3).
Kelly M. Latimer, MD, an FP in the Navy stationed in Djibouti, Africa, routinely asks patients whether they have a smartphone and often recommends apps to those who do.
“It sounds like you have a lot of different symptoms,” she might say to a patient who complains of frequent headaches. “It will help me if you keep a headache diary.”
She used to give such patients paper and pen, Dr. Latimer noted. “Now I ask them to download the app (iHeadache, in this case) right then and there and do a quick review” so they’re ready to use it at home.
Apps are also a good way to help people with anxiety, Dr. Latimer has found. She frequently recommends apps like Relaxation Techniques and Breathe2Relax, and often suggests apps like Calorie Count and MyFitnessPal to boost patients’ efforts to lose weight and get in shape.
Abigail Lowther, MD, an FP at the University of Michigan in Ann Arbor, also recommends apps frequently. But she typically broaches the subject only with patients who have their smartphones out when she walks into the room.
Among the apps Dr. Lowther prescribes are myPause to track menopausal symptoms and Bladder Pal, a voiding diary for women struggling with incontinence. She advises women taking oral contraceptives to use the timer function on their phone to remember to take a pill at the same time every day. But there are apps (myPill, for one) that do that, too.
The upside of patient apps. A smartphone is ideal for keeping a symptom diary because it’s something that most people are never without. Anyone can use the notes function on a phone or tablet to jot down details about exacerbations, but those using disease-specific apps tend to capture more precise information. Some patients print out the information they’ve gathered and bring a hard copy to an office visit, while others simply show their physician what’s on their smartphone.
Can apps affect outcomes? There are few high-quality studies and the jury is still out, but “the smartphone has a very bright future in the world of medicine,” the authors of a review of smartphones in the medical arena concluded. After examining the use of apps to track (literally) wandering dementia patients; calculate and recommend insulin dosages for patients with type 1 diabetes; and teach yoga, to name a few, the researchers concluded that “the smartphone may one day be recognized as a diagnostic and therapeutic tool…as irreplaceable as the stethoscope.”11
Dr. Lowther recalls an obese patient who found MyFitnessPal to be helpful where other, more traditional diet programs had failed. The reason? He was less than truthful with the people overseeing the weight loss programs about what he’d eaten when he tried—and failed—to follow diets like Weight Watchers. He then ended up feeling so guilty that he abandoned the effort entirely. But, he told her, he “wouldn’t lie” to an app.
…and the downside. Even physicians who haven’t begun A weight loss app would be more likely to help this patient reach his goal than other diet programs because he "wouldn't lie" to an app.recommending apps to patients are aware that carefully tracking measures related to chronic conditions like hypertension or diabetes often results in better control. But in some cases, there may be too much of a good thing. Evidence suggests that for some patients with type 2 diabetes, glucose self-monitoring is associated with depression and may do more harm than good.12
Dr. Lowther has witnessed a similar phenomenon in patients using disease-tracking apps. “Sometimes people get too focused on the problem and drive themselves crazy,” she observed, adding that those with high blood pressure are particularly at risk. “I think sometimes it’s hard for patients to understand the concept of an average value and normal fluctuation,” Dr. Lowther said. When that happens, “I have to tell them to back off.”
Who's minding the (app) store?
The mHealth arena has been called “the wild West.”13 With at least one app for virtually every aspect of health and medicine you can think of, it’s not hard to understand why.
In an article on the use of symptom diaries in outpatient care, Bryan Hodge, DO, an FP in Hendersonville, NC, mentions mobile self-tracking apps as one of a number of ways for patients to keep symptom diaries.14 Given the fact that few of these apps have been validated, Dr. Hodge writes, “The best approach is to familiarize yourself with a few options that you can offer to your patients.”14
That depends on the nature of the app. An app that tracks calories consumed or simply keeps an organized file of patient symptoms may do little harm; an app that conveys physical measurements that a patient or physician may act on or calculates medication dosages requires a higher level of vigilance.
A recent study of smartphone apps that calculate opioid dosage conversion, for example, found a lack of consistency that raised a red flag about the reliability of information provided by unvalidated apps. Better regulation of medical apps is crucial to ensure that patient safety is maintained, the authors concluded.15
The FDA’s role
The US Food and Drug Administration, which has approved more than 75 medical apps, issued a proposed approach to its oversight of the apps in 2011.16
Under the proposed rules, the agency would regulate mobile apps that were either used as an accessory to a medical device already regulated by the FDA or that transform a smartphone or tablet into a regulated medical device. A final rule has not yet been issued, but a spokesperson told Congress that it will be forthcoming before the end of the year.17
False claims are a target of federal regulation, as well. In 2011, the Federal Trade Commission pulled 2 acne apps off the market because both advertised—without scientific evidence—that the light emitted by smartphones equipped with the apps could treat acne. “Smartphones make our lives easier in countless ways, but unfortunately, when it comes to curing acne, there’s no app for that,” the FTC chairman stated in a press release.18
In May 2013, the FDA sent an “It has come to our attention letter” to Biosense Technologies regarding its uChek urine analyzer app. The problem, the letter stated, is that the dipsticks that the app allows a mobile phone to analyze are cleared by the FDA only when interpreted by direct visual reading. But the phone and device together function “as an automated strip reader”—a urinalysis test system for which new FDA Smartphones make our lives easier in countless ways, but unfortunately, when it comes to curing acne, there's no app for that," the chairman of the Federal Trade Commission stated in a press release. clearance is required.19
Other ways of evaluating apps
Happtique, a mobile health solutions company, recently announced the launch of its Health App Certification Program—a voluntary program designed to help clinicians and patients easily identify apps that are credible and safe.20 “We will be certifying medical, health, and fitness apps, Corey Ackerman, president and CEO of Happtique, told JFP. The program is currently accepting medical education and nursing apps for review, and “discussions are underway with numerous other organizations that will provide experts for apps in additional subject matter areas,” Mr. Ackerman said.
There are other means of evaluating mobile medical apps that fall outside of the medical device realm, of course—starting by perusing the reviews posted at the app stores. Exchanging information with other clinicians using an app you’re interested in is another way to learn more about its efficacy. (Yes, there’s an app for that, too: Doximity, the professional network for clinicians.)
Other suggestions for safe use of apps:
- Peruse iMedicalApps (imedicalapps.com), the self-described leading physician publication on mobile medicine. Its physician editors and team of clinicians research and review medical apps.
- Consider the source. An app that has been developed by a medical society, federal agency, or prestigious medical school, for example, is more trustworthy than one from an unknown source (a point you would be wise to pass on to your patients).
- Try the app yourself before you recommend it to a patient.
Finally, keep the privacy provision in the Health Insurance Portability and Accountability Act in mind. Before using any app through which private patient health information can be transmitted or stored, ensure that the data will be encrypted and that your mobile device is password-protected, advises mHIMSS, the mobile branch of the Healthcare Information and Management Systems Society.21
In April, hundreds of attendees at TEDMED, a conference on medical innovation, waited in line for a “smartphone physical.” Curated by Shiv Gaglani, a medical student and an editor at the medical technology journal Medgadget, the exam involved 10 apps that turn an ordinary smartphone into a medical device (TABLE 1).1 Among them were the AliveCor Heart Monitor (pictured at right), which produces a one-lead EKG in seconds when a patient’s fingers or chest are pressed against the electrodes embedded in the back of what is essentially a phone case2; a pulse oximeter, and an ultrasound that can capture images of the carotid arteries.1
All but one of the apps is paired with a physical component, such as an ultrasound wand or otoscope. The exception is SpiroSmart, an app that uses the phone’s The AliveCor app and Heart Monitor—a smartphone case fitted with sensors—can generate a one-lead EKG tracing in seconds.built-in microphone and lip reverberations to assess lung function. Shwetak Patel, PhD, of the University of Washington, one of its developers, told JFP that the accuracy of SpiroSmart has been found to be within 5% of traditional spirometry results.3
While smartphone physicals are not likely to be integrated into family practice for some time to come, Glen Stream, MD, board chair of the American Academy of Family Physicians, predicts that integration of some of their features is not too far away. “The spirometry application is an especially good one; it addresses one of the top 5 chronic conditions that contribute to health care costs,” Dr. Stream said. The apps will be beneficial, he added, as long as they “are used in a way that contributes, to, rather than detracts from, collaboration between patients and physicians.”
For now, Dr. Stream and many of his fellow FPs use mobile devices and medical apps primarily to access reference materials, both in and out of the exam room. Some have begun “prescribing” apps to tech-savvy patients. Still others have never used a medical app, either because they prefer a desktop or laptop computer to a smartphone or tablet or because, as one FP put it, "I have a dumb phone."
Wherever you fall on the spectrum, it’s a safe bet that you’re going to be increasingly inundated by the many manifestations of mobile health (mHealth).
Epocrates is No. 1 reference app
The number of medical/health apps for smart-phones or tablets is difficult to pin down; estimates range from 17,000 to more than 40,000, and growing.4 More is known about physician use of smartphones and tablets.
A March 2013 survey of nearly 3000 physicians found that 74% use smartphones at work and 43% use them to look up drug information.5 The favorite tool? A 2012 survey conducted by the University of Pennsylvania’s Perelman School of Medicine to identify the best medical apps put Epocrates at the top of the list (TABLE 2).6 Epocrates was the very first app cited by virtually all the FPs interviewed for this article, as well.
Other drug references cited tend to be patient-specific. Colan Kennelly, MD, a clinical educator at the Good Samaritan Family Medicine Residency in Phoenix, finds LactMed particularly useful. Developed by the National Library of Medicine and part of its Toxicology Data Network, the app lets you pull up medications quickly and see whether and how they will affect breastfeeding.
Another favorite of Kennelly’s is the Agency for Healthcare Research and Quality’s ePSS (electronic Preventive Services Selector) app designed to help primary care clinicians identify the preventive services that are appropriate for their patients. “You just plug in a patient’s age and sex”—(pregnancy, tobacco use, and whether the patient is sexually active are also considered)—“and it tells you what you should be checking for,” Dr. Kennelly said.
The benefits of mobile textbooks
Textbook apps and online texts are slowly gaining in popularity. A recent survey by Manhattan Research found that in 2013 for the first time, usage of electronic medical texts surpassed that of print editions.7 Part of the appeal is that mobile texts are easy to tote. “Apps make it possible to carry around information from a number of textbooks with no added weight,” said Richard Usatine, MD, of the University of Texas Health Science Center at San Antonio and editor of JFP’s Photo Rounds column. Dr. Usatine is also a principal of Usatine Media, which turns medical reference materials into apps.
Dr. Usatine’s own experience is a case in point. He recently used a textbook app to prepare to take his boards (for the fifth time). “I’ve brushed up each time,” he said, “but this time I really studied because it was fun.
“With a print textbook you have to cover up the answers so you don’t see them. Here, you don’t get to see the answer until you commit to one of the multiple choice answers. Then you get told what the correct answer is and why you got it right or wrong,” Dr. Usatine said. Interactivity, including the opportunity to watch a video, say, of a procedure to review how it’s done before embarking on it yourself, is a big part of the value of apps, he said.
Rx: App
In January, Eric Topol, MD, a prominent cardiologist and chief academic officer of Scripps Health in La Jolla, Calif., demonstrated the AliveCor heart monitor and other mobile devices on NBC’s Rock Center.8 In March, he went on The Colbert Report and examined Stephen Colbert’s ear with an otoscope smartphone accessory (CellScope) like the one used in Gaglani’s smartphone physical.9 Dr. Topol’s use of the mobile heart monitor to assess an airplane passenger in distress midflight also received widespread news coverage.
In response to an interviewer’s question, Dr. Topol said he is now more likely to prescribe an app than a drug.8 While it’s unlikely that any FP could make such a claim, many have begun recommending apps to tech-savvy patients.
Smartphones as symptom trackers
A January 2013 Pew Internet study found that 7 in 10 US adults track at least one health indicator, for themselves or a loved one. Six in 10 reported tracking weight, diet, or exercise, and one in 3 said they track indicators of medical problems, such as blood pressure, glucose levels, headaches, or sleep patterns—usually without the aid of a smartphone.10
In fact, half of those who report tracking health measures said they keep the information “in their head,” and a third still use pencil and paper.10 That could change, of course, if their physicians suggest they do otherwise (TABLE 3).
Kelly M. Latimer, MD, an FP in the Navy stationed in Djibouti, Africa, routinely asks patients whether they have a smartphone and often recommends apps to those who do.
“It sounds like you have a lot of different symptoms,” she might say to a patient who complains of frequent headaches. “It will help me if you keep a headache diary.”
She used to give such patients paper and pen, Dr. Latimer noted. “Now I ask them to download the app (iHeadache, in this case) right then and there and do a quick review” so they’re ready to use it at home.
Apps are also a good way to help people with anxiety, Dr. Latimer has found. She frequently recommends apps like Relaxation Techniques and Breathe2Relax, and often suggests apps like Calorie Count and MyFitnessPal to boost patients’ efforts to lose weight and get in shape.
Abigail Lowther, MD, an FP at the University of Michigan in Ann Arbor, also recommends apps frequently. But she typically broaches the subject only with patients who have their smartphones out when she walks into the room.
Among the apps Dr. Lowther prescribes are myPause to track menopausal symptoms and Bladder Pal, a voiding diary for women struggling with incontinence. She advises women taking oral contraceptives to use the timer function on their phone to remember to take a pill at the same time every day. But there are apps (myPill, for one) that do that, too.
The upside of patient apps. A smartphone is ideal for keeping a symptom diary because it’s something that most people are never without. Anyone can use the notes function on a phone or tablet to jot down details about exacerbations, but those using disease-specific apps tend to capture more precise information. Some patients print out the information they’ve gathered and bring a hard copy to an office visit, while others simply show their physician what’s on their smartphone.
Can apps affect outcomes? There are few high-quality studies and the jury is still out, but “the smartphone has a very bright future in the world of medicine,” the authors of a review of smartphones in the medical arena concluded. After examining the use of apps to track (literally) wandering dementia patients; calculate and recommend insulin dosages for patients with type 1 diabetes; and teach yoga, to name a few, the researchers concluded that “the smartphone may one day be recognized as a diagnostic and therapeutic tool…as irreplaceable as the stethoscope.”11
Dr. Lowther recalls an obese patient who found MyFitnessPal to be helpful where other, more traditional diet programs had failed. The reason? He was less than truthful with the people overseeing the weight loss programs about what he’d eaten when he tried—and failed—to follow diets like Weight Watchers. He then ended up feeling so guilty that he abandoned the effort entirely. But, he told her, he “wouldn’t lie” to an app.
…and the downside. Even physicians who haven’t begun A weight loss app would be more likely to help this patient reach his goal than other diet programs because he "wouldn't lie" to an app.recommending apps to patients are aware that carefully tracking measures related to chronic conditions like hypertension or diabetes often results in better control. But in some cases, there may be too much of a good thing. Evidence suggests that for some patients with type 2 diabetes, glucose self-monitoring is associated with depression and may do more harm than good.12
Dr. Lowther has witnessed a similar phenomenon in patients using disease-tracking apps. “Sometimes people get too focused on the problem and drive themselves crazy,” she observed, adding that those with high blood pressure are particularly at risk. “I think sometimes it’s hard for patients to understand the concept of an average value and normal fluctuation,” Dr. Lowther said. When that happens, “I have to tell them to back off.”
Who's minding the (app) store?
The mHealth arena has been called “the wild West.”13 With at least one app for virtually every aspect of health and medicine you can think of, it’s not hard to understand why.
In an article on the use of symptom diaries in outpatient care, Bryan Hodge, DO, an FP in Hendersonville, NC, mentions mobile self-tracking apps as one of a number of ways for patients to keep symptom diaries.14 Given the fact that few of these apps have been validated, Dr. Hodge writes, “The best approach is to familiarize yourself with a few options that you can offer to your patients.”14
That depends on the nature of the app. An app that tracks calories consumed or simply keeps an organized file of patient symptoms may do little harm; an app that conveys physical measurements that a patient or physician may act on or calculates medication dosages requires a higher level of vigilance.
A recent study of smartphone apps that calculate opioid dosage conversion, for example, found a lack of consistency that raised a red flag about the reliability of information provided by unvalidated apps. Better regulation of medical apps is crucial to ensure that patient safety is maintained, the authors concluded.15
The FDA’s role
The US Food and Drug Administration, which has approved more than 75 medical apps, issued a proposed approach to its oversight of the apps in 2011.16
Under the proposed rules, the agency would regulate mobile apps that were either used as an accessory to a medical device already regulated by the FDA or that transform a smartphone or tablet into a regulated medical device. A final rule has not yet been issued, but a spokesperson told Congress that it will be forthcoming before the end of the year.17
False claims are a target of federal regulation, as well. In 2011, the Federal Trade Commission pulled 2 acne apps off the market because both advertised—without scientific evidence—that the light emitted by smartphones equipped with the apps could treat acne. “Smartphones make our lives easier in countless ways, but unfortunately, when it comes to curing acne, there’s no app for that,” the FTC chairman stated in a press release.18
In May 2013, the FDA sent an “It has come to our attention letter” to Biosense Technologies regarding its uChek urine analyzer app. The problem, the letter stated, is that the dipsticks that the app allows a mobile phone to analyze are cleared by the FDA only when interpreted by direct visual reading. But the phone and device together function “as an automated strip reader”—a urinalysis test system for which new FDA Smartphones make our lives easier in countless ways, but unfortunately, when it comes to curing acne, there's no app for that," the chairman of the Federal Trade Commission stated in a press release. clearance is required.19
Other ways of evaluating apps
Happtique, a mobile health solutions company, recently announced the launch of its Health App Certification Program—a voluntary program designed to help clinicians and patients easily identify apps that are credible and safe.20 “We will be certifying medical, health, and fitness apps, Corey Ackerman, president and CEO of Happtique, told JFP. The program is currently accepting medical education and nursing apps for review, and “discussions are underway with numerous other organizations that will provide experts for apps in additional subject matter areas,” Mr. Ackerman said.
There are other means of evaluating mobile medical apps that fall outside of the medical device realm, of course—starting by perusing the reviews posted at the app stores. Exchanging information with other clinicians using an app you’re interested in is another way to learn more about its efficacy. (Yes, there’s an app for that, too: Doximity, the professional network for clinicians.)
Other suggestions for safe use of apps:
- Peruse iMedicalApps (imedicalapps.com), the self-described leading physician publication on mobile medicine. Its physician editors and team of clinicians research and review medical apps.
- Consider the source. An app that has been developed by a medical society, federal agency, or prestigious medical school, for example, is more trustworthy than one from an unknown source (a point you would be wise to pass on to your patients).
- Try the app yourself before you recommend it to a patient.
Finally, keep the privacy provision in the Health Insurance Portability and Accountability Act in mind. Before using any app through which private patient health information can be transmitted or stored, ensure that the data will be encrypted and that your mobile device is password-protected, advises mHIMSS, the mobile branch of the Healthcare Information and Management Systems Society.21
1. TEDMED. The smartphone physical. Available at: http://www.smartphonephysical.org/tedmed.html. Accessed June 14, 2013.
2. AliveCor. AliveCor heart monitor. Available at: http://www.alivecor.com/. Accessed June 14, 2013.
3. Ubiquitous Computing Lab, University of Washington. Mobile phone spirometry. Available at: http://ubicomplab.cs.washington.edu/wiki/SpiroSmart. Accessed June 19, 2013.
4. Association of American Medical Colleges. Explosive growth in health care apps raises oversight questions. Available at: https://www.aamc.org/newsroom/reporter/october2012/308516/health-care-apps.html. Accessed June 14, 2013.
5. Alvarez A. How are physicians using smartphones for professional purposes? April 22, 2013. Available at: www.kantarmedia-healthcare.com/how-are-physicians-using-smartphones-for-professional-purposes. Accessed June 14, 2013.
6. Penn Medical Student Government. 2012 Medical app survey results. February 9, 2013. Available at: http://msg.med.upenn.edu/?p=17784. Accessed June 19, 2013.
7. Comstock J. Manhattan: 72% of physicians have tablets. April 18, 2013. Available at: http://mobihealthnews.com/21733/manhattan-72-percent-of-physicians-have-tablets/. Accessed June 19, 2013.
8. Dr. Eric Topol on NBC’s Rock Center. January 24, 2013. Available at: http://www.youtube.com/watch?v=0B-jUOOrtks. Accessed June 14, 2013.
9. Comstock J. Topol turns Colbert around on digital health. March 27, 2013. Available at: http://mobihealthnews.com/21263/topol-turns-colbert-around-on-digital-health/.Accessed June 14,2013.
10. Pew Research Center. Tracking for health. January 28, 2013. Available at: http://pewinternet.org/Press-Releases/2013/Tracking-for-health. Accessed June 14, 2013.
11. Ozdalga E, Ozdalga A, Ahuja N. The smartphone in medicine: a review of current and potential use among physicians and students. J Med Internet Res. 2012;14:e128.
12. Mendoza M, Rosenberg T. Self-management of type 2 diabetes: a good idea or not? J Fam Pract. 2013;62:244-248.
13. McMillan R. iPad: ‘Wild West’ of medical apps seeks sheriff. December 12, 2011. Available at: http://www.wired.com/wiredenterprise/2011/12/fda_apps/. Accessed June 14, 2013.
14. Hodge B. The use of symptom diaries in outpatient care. Fam Pract Manag. 2013;20:24-28.
15. Haffey F, Brady RR, Maxwell S. A comparison of the reliability of smartphone apps for opioid conversion. Drug Saf. 2013;36:111-117.
16. US Food and Drug Administration. FDA proposes health “app” guidelines. July 19, 2011. Available at: http://www.fda.gov/forconsumers/consumerupdates/ucm263332.htm. Accessed June 14, 2013.
17. Pavlovic P. 10 issues that mobile medical app developers should keep in mind. April 18, 2013. Available at: http://www.mhimss.org/news/10-issues-mobile-medical-app-developers-should-keep-mind. Accessed June 14, 2013.
18. Federal Trade Commission. “Acne cure” mobile app marketers will drop baseless claims under FTC settlements. September 8, 2011. Available at: http://www.ftc.gov/opa/2011/09/acnecure.shtm. Accessed June 14, 2013.
19. FDA. Letter to Biosense Technologies Private Limited concerning the uChek urine analyzer. Available at: http://www.fda.gov/MedicalDevices/ResourcesforYou/Industry/ucm353513.htm. Accessed June 14, 2013.
20. Happtique publishes final standards for mobile health app certification program. February 27, 2013. Available at: http://www.happtique.com/happtique-publishes-final-standards-for-mobile-health-app-certification-program/. Accessed June 19, 2013.
21. mHIMSS. Privacy and security. Available at: http://www.mhimss.org/resource-topics/privacy-security. Accessed June 14, 2013.
1. TEDMED. The smartphone physical. Available at: http://www.smartphonephysical.org/tedmed.html. Accessed June 14, 2013.
2. AliveCor. AliveCor heart monitor. Available at: http://www.alivecor.com/. Accessed June 14, 2013.
3. Ubiquitous Computing Lab, University of Washington. Mobile phone spirometry. Available at: http://ubicomplab.cs.washington.edu/wiki/SpiroSmart. Accessed June 19, 2013.
4. Association of American Medical Colleges. Explosive growth in health care apps raises oversight questions. Available at: https://www.aamc.org/newsroom/reporter/october2012/308516/health-care-apps.html. Accessed June 14, 2013.
5. Alvarez A. How are physicians using smartphones for professional purposes? April 22, 2013. Available at: www.kantarmedia-healthcare.com/how-are-physicians-using-smartphones-for-professional-purposes. Accessed June 14, 2013.
6. Penn Medical Student Government. 2012 Medical app survey results. February 9, 2013. Available at: http://msg.med.upenn.edu/?p=17784. Accessed June 19, 2013.
7. Comstock J. Manhattan: 72% of physicians have tablets. April 18, 2013. Available at: http://mobihealthnews.com/21733/manhattan-72-percent-of-physicians-have-tablets/. Accessed June 19, 2013.
8. Dr. Eric Topol on NBC’s Rock Center. January 24, 2013. Available at: http://www.youtube.com/watch?v=0B-jUOOrtks. Accessed June 14, 2013.
9. Comstock J. Topol turns Colbert around on digital health. March 27, 2013. Available at: http://mobihealthnews.com/21263/topol-turns-colbert-around-on-digital-health/.Accessed June 14,2013.
10. Pew Research Center. Tracking for health. January 28, 2013. Available at: http://pewinternet.org/Press-Releases/2013/Tracking-for-health. Accessed June 14, 2013.
11. Ozdalga E, Ozdalga A, Ahuja N. The smartphone in medicine: a review of current and potential use among physicians and students. J Med Internet Res. 2012;14:e128.
12. Mendoza M, Rosenberg T. Self-management of type 2 diabetes: a good idea or not? J Fam Pract. 2013;62:244-248.
13. McMillan R. iPad: ‘Wild West’ of medical apps seeks sheriff. December 12, 2011. Available at: http://www.wired.com/wiredenterprise/2011/12/fda_apps/. Accessed June 14, 2013.
14. Hodge B. The use of symptom diaries in outpatient care. Fam Pract Manag. 2013;20:24-28.
15. Haffey F, Brady RR, Maxwell S. A comparison of the reliability of smartphone apps for opioid conversion. Drug Saf. 2013;36:111-117.
16. US Food and Drug Administration. FDA proposes health “app” guidelines. July 19, 2011. Available at: http://www.fda.gov/forconsumers/consumerupdates/ucm263332.htm. Accessed June 14, 2013.
17. Pavlovic P. 10 issues that mobile medical app developers should keep in mind. April 18, 2013. Available at: http://www.mhimss.org/news/10-issues-mobile-medical-app-developers-should-keep-mind. Accessed June 14, 2013.
18. Federal Trade Commission. “Acne cure” mobile app marketers will drop baseless claims under FTC settlements. September 8, 2011. Available at: http://www.ftc.gov/opa/2011/09/acnecure.shtm. Accessed June 14, 2013.
19. FDA. Letter to Biosense Technologies Private Limited concerning the uChek urine analyzer. Available at: http://www.fda.gov/MedicalDevices/ResourcesforYou/Industry/ucm353513.htm. Accessed June 14, 2013.
20. Happtique publishes final standards for mobile health app certification program. February 27, 2013. Available at: http://www.happtique.com/happtique-publishes-final-standards-for-mobile-health-app-certification-program/. Accessed June 19, 2013.
21. mHIMSS. Privacy and security. Available at: http://www.mhimss.org/resource-topics/privacy-security. Accessed June 14, 2013.