User login
How apps are changing family medicine
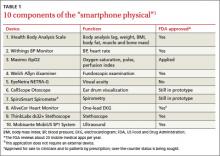
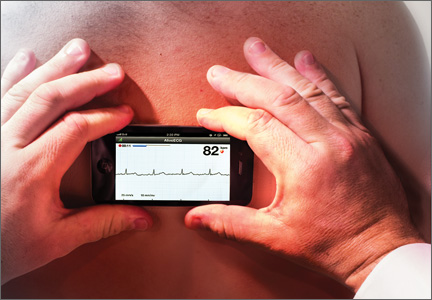
In April, hundreds of attendees at TEDMED, a conference on medical innovation, waited in line for a “smartphone physical.” Curated by Shiv Gaglani, a medical student and an editor at the medical technology journal Medgadget, the exam involved 10 apps that turn an ordinary smartphone into a medical device (TABLE 1).1 Among them were the AliveCor Heart Monitor (pictured at right), which produces a one-lead EKG in seconds when a patient’s fingers or chest are pressed against the electrodes embedded in the back of what is essentially a phone case2; a pulse oximeter, and an ultrasound that can capture images of the carotid arteries.1
All but one of the apps is paired with a physical component, such as an ultrasound wand or otoscope. The exception is SpiroSmart, an app that uses the phone’s The AliveCor app and Heart Monitor—a smartphone case fitted with sensors—can generate a one-lead EKG tracing in seconds.built-in microphone and lip reverberations to assess lung function. Shwetak Patel, PhD, of the University of Washington, one of its developers, told JFP that the accuracy of SpiroSmart has been found to be within 5% of traditional spirometry results.3
While smartphone physicals are not likely to be integrated into family practice for some time to come, Glen Stream, MD, board chair of the American Academy of Family Physicians, predicts that integration of some of their features is not too far away. “The spirometry application is an especially good one; it addresses one of the top 5 chronic conditions that contribute to health care costs,” Dr. Stream said. The apps will be beneficial, he added, as long as they “are used in a way that contributes, to, rather than detracts from, collaboration between patients and physicians.”
For now, Dr. Stream and many of his fellow FPs use mobile devices and medical apps primarily to access reference materials, both in and out of the exam room. Some have begun “prescribing” apps to tech-savvy patients. Still others have never used a medical app, either because they prefer a desktop or laptop computer to a smartphone or tablet or because, as one FP put it, "I have a dumb phone."
Wherever you fall on the spectrum, it’s a safe bet that you’re going to be increasingly inundated by the many manifestations of mobile health (mHealth).
Epocrates is No. 1 reference app
The number of medical/health apps for smart-phones or tablets is difficult to pin down; estimates range from 17,000 to more than 40,000, and growing.4 More is known about physician use of smartphones and tablets.
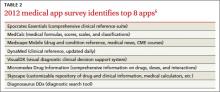
A March 2013 survey of nearly 3000 physicians found that 74% use smartphones at work and 43% use them to look up drug information.5 The favorite tool? A 2012 survey conducted by the University of Pennsylvania’s Perelman School of Medicine to identify the best medical apps put Epocrates at the top of the list (TABLE 2).6 Epocrates was the very first app cited by virtually all the FPs interviewed for this article, as well.
Other drug references cited tend to be patient-specific. Colan Kennelly, MD, a clinical educator at the Good Samaritan Family Medicine Residency in Phoenix, finds LactMed particularly useful. Developed by the National Library of Medicine and part of its Toxicology Data Network, the app lets you pull up medications quickly and see whether and how they will affect breastfeeding.
Another favorite of Kennelly’s is the Agency for Healthcare Research and Quality’s ePSS (electronic Preventive Services Selector) app designed to help primary care clinicians identify the preventive services that are appropriate for their patients. “You just plug in a patient’s age and sex”—(pregnancy, tobacco use, and whether the patient is sexually active are also considered)—“and it tells you what you should be checking for,” Dr. Kennelly said.
The benefits of mobile textbooks
Textbook apps and online texts are slowly gaining in popularity. A recent survey by Manhattan Research found that in 2013 for the first time, usage of electronic medical texts surpassed that of print editions.7 Part of the appeal is that mobile texts are easy to tote. “Apps make it possible to carry around information from a number of textbooks with no added weight,” said Richard Usatine, MD, of the University of Texas Health Science Center at San Antonio and editor of JFP’s Photo Rounds column. Dr. Usatine is also a principal of Usatine Media, which turns medical reference materials into apps.
Dr. Usatine’s own experience is a case in point. He recently used a textbook app to prepare to take his boards (for the fifth time). “I’ve brushed up each time,” he said, “but this time I really studied because it was fun.
“With a print textbook you have to cover up the answers so you don’t see them. Here, you don’t get to see the answer until you commit to one of the multiple choice answers. Then you get told what the correct answer is and why you got it right or wrong,” Dr. Usatine said. Interactivity, including the opportunity to watch a video, say, of a procedure to review how it’s done before embarking on it yourself, is a big part of the value of apps, he said.
Rx: App
In January, Eric Topol, MD, a prominent cardiologist and chief academic officer of Scripps Health in La Jolla, Calif., demonstrated the AliveCor heart monitor and other mobile devices on NBC’s Rock Center.8 In March, he went on The Colbert Report and examined Stephen Colbert’s ear with an otoscope smartphone accessory (CellScope) like the one used in Gaglani’s smartphone physical.9 Dr. Topol’s use of the mobile heart monitor to assess an airplane passenger in distress midflight also received widespread news coverage.
In response to an interviewer’s question, Dr. Topol said he is now more likely to prescribe an app than a drug.8 While it’s unlikely that any FP could make such a claim, many have begun recommending apps to tech-savvy patients.
Smartphones as symptom trackers
A January 2013 Pew Internet study found that 7 in 10 US adults track at least one health indicator, for themselves or a loved one. Six in 10 reported tracking weight, diet, or exercise, and one in 3 said they track indicators of medical problems, such as blood pressure, glucose levels, headaches, or sleep patterns—usually without the aid of a smartphone.10
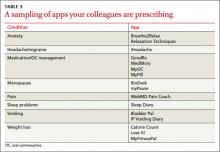
In fact, half of those who report tracking health measures said they keep the information “in their head,” and a third still use pencil and paper.10 That could change, of course, if their physicians suggest they do otherwise (TABLE 3).
Kelly M. Latimer, MD, an FP in the Navy stationed in Djibouti, Africa, routinely asks patients whether they have a smartphone and often recommends apps to those who do.
“It sounds like you have a lot of different symptoms,” she might say to a patient who complains of frequent headaches. “It will help me if you keep a headache diary.”
She used to give such patients paper and pen, Dr. Latimer noted. “Now I ask them to download the app (iHeadache, in this case) right then and there and do a quick review” so they’re ready to use it at home.
Apps are also a good way to help people with anxiety, Dr. Latimer has found. She frequently recommends apps like Relaxation Techniques and Breathe2Relax, and often suggests apps like Calorie Count and MyFitnessPal to boost patients’ efforts to lose weight and get in shape.
Abigail Lowther, MD, an FP at the University of Michigan in Ann Arbor, also recommends apps frequently. But she typically broaches the subject only with patients who have their smartphones out when she walks into the room.
Among the apps Dr. Lowther prescribes are myPause to track menopausal symptoms and Bladder Pal, a voiding diary for women struggling with incontinence. She advises women taking oral contraceptives to use the timer function on their phone to remember to take a pill at the same time every day. But there are apps (myPill, for one) that do that, too.
The upside of patient apps. A smartphone is ideal for keeping a symptom diary because it’s something that most people are never without. Anyone can use the notes function on a phone or tablet to jot down details about exacerbations, but those using disease-specific apps tend to capture more precise information. Some patients print out the information they’ve gathered and bring a hard copy to an office visit, while others simply show their physician what’s on their smartphone.
Can apps affect outcomes? There are few high-quality studies and the jury is still out, but “the smartphone has a very bright future in the world of medicine,” the authors of a review of smartphones in the medical arena concluded. After examining the use of apps to track (literally) wandering dementia patients; calculate and recommend insulin dosages for patients with type 1 diabetes; and teach yoga, to name a few, the researchers concluded that “the smartphone may one day be recognized as a diagnostic and therapeutic tool…as irreplaceable as the stethoscope.”11
Dr. Lowther recalls an obese patient who found MyFitnessPal to be helpful where other, more traditional diet programs had failed. The reason? He was less than truthful with the people overseeing the weight loss programs about what he’d eaten when he tried—and failed—to follow diets like Weight Watchers. He then ended up feeling so guilty that he abandoned the effort entirely. But, he told her, he “wouldn’t lie” to an app.
…and the downside. Even physicians who haven’t begun A weight loss app would be more likely to help this patient reach his goal than other diet programs because he "wouldn't lie" to an app.recommending apps to patients are aware that carefully tracking measures related to chronic conditions like hypertension or diabetes often results in better control. But in some cases, there may be too much of a good thing. Evidence suggests that for some patients with type 2 diabetes, glucose self-monitoring is associated with depression and may do more harm than good.12
Dr. Lowther has witnessed a similar phenomenon in patients using disease-tracking apps. “Sometimes people get too focused on the problem and drive themselves crazy,” she observed, adding that those with high blood pressure are particularly at risk. “I think sometimes it’s hard for patients to understand the concept of an average value and normal fluctuation,” Dr. Lowther said. When that happens, “I have to tell them to back off.”
Who's minding the (app) store?
The mHealth arena has been called “the wild West.”13 With at least one app for virtually every aspect of health and medicine you can think of, it’s not hard to understand why.
In an article on the use of symptom diaries in outpatient care, Bryan Hodge, DO, an FP in Hendersonville, NC, mentions mobile self-tracking apps as one of a number of ways for patients to keep symptom diaries.14 Given the fact that few of these apps have been validated, Dr. Hodge writes, “The best approach is to familiarize yourself with a few options that you can offer to your patients.”14
That depends on the nature of the app. An app that tracks calories consumed or simply keeps an organized file of patient symptoms may do little harm; an app that conveys physical measurements that a patient or physician may act on or calculates medication dosages requires a higher level of vigilance.
A recent study of smartphone apps that calculate opioid dosage conversion, for example, found a lack of consistency that raised a red flag about the reliability of information provided by unvalidated apps. Better regulation of medical apps is crucial to ensure that patient safety is maintained, the authors concluded.15
The FDA’s role
The US Food and Drug Administration, which has approved more than 75 medical apps, issued a proposed approach to its oversight of the apps in 2011.16
Under the proposed rules, the agency would regulate mobile apps that were either used as an accessory to a medical device already regulated by the FDA or that transform a smartphone or tablet into a regulated medical device. A final rule has not yet been issued, but a spokesperson told Congress that it will be forthcoming before the end of the year.17
False claims are a target of federal regulation, as well. In 2011, the Federal Trade Commission pulled 2 acne apps off the market because both advertised—without scientific evidence—that the light emitted by smartphones equipped with the apps could treat acne. “Smartphones make our lives easier in countless ways, but unfortunately, when it comes to curing acne, there’s no app for that,” the FTC chairman stated in a press release.18
In May 2013, the FDA sent an “It has come to our attention letter” to Biosense Technologies regarding its uChek urine analyzer app. The problem, the letter stated, is that the dipsticks that the app allows a mobile phone to analyze are cleared by the FDA only when interpreted by direct visual reading. But the phone and device together function “as an automated strip reader”—a urinalysis test system for which new FDA Smartphones make our lives easier in countless ways, but unfortunately, when it comes to curing acne, there's no app for that," the chairman of the Federal Trade Commission stated in a press release. clearance is required.19
Other ways of evaluating apps
Happtique, a mobile health solutions company, recently announced the launch of its Health App Certification Program—a voluntary program designed to help clinicians and patients easily identify apps that are credible and safe.20 “We will be certifying medical, health, and fitness apps, Corey Ackerman, president and CEO of Happtique, told JFP. The program is currently accepting medical education and nursing apps for review, and “discussions are underway with numerous other organizations that will provide experts for apps in additional subject matter areas,” Mr. Ackerman said.
There are other means of evaluating mobile medical apps that fall outside of the medical device realm, of course—starting by perusing the reviews posted at the app stores. Exchanging information with other clinicians using an app you’re interested in is another way to learn more about its efficacy. (Yes, there’s an app for that, too: Doximity, the professional network for clinicians.)
Other suggestions for safe use of apps:
- Peruse iMedicalApps (imedicalapps.com), the self-described leading physician publication on mobile medicine. Its physician editors and team of clinicians research and review medical apps.
- Consider the source. An app that has been developed by a medical society, federal agency, or prestigious medical school, for example, is more trustworthy than one from an unknown source (a point you would be wise to pass on to your patients).
- Try the app yourself before you recommend it to a patient.
Finally, keep the privacy provision in the Health Insurance Portability and Accountability Act in mind. Before using any app through which private patient health information can be transmitted or stored, ensure that the data will be encrypted and that your mobile device is password-protected, advises mHIMSS, the mobile branch of the Healthcare Information and Management Systems Society.21
1. TEDMED. The smartphone physical. Available at: http://www.smartphonephysical.org/tedmed.html. Accessed June 14, 2013.
2. AliveCor. AliveCor heart monitor. Available at: http://www.alivecor.com/. Accessed June 14, 2013.
3. Ubiquitous Computing Lab, University of Washington. Mobile phone spirometry. Available at: http://ubicomplab.cs.washington.edu/wiki/SpiroSmart. Accessed June 19, 2013.
4. Association of American Medical Colleges. Explosive growth in health care apps raises oversight questions. Available at: https://www.aamc.org/newsroom/reporter/october2012/308516/health-care-apps.html. Accessed June 14, 2013.
5. Alvarez A. How are physicians using smartphones for professional purposes? April 22, 2013. Available at: www.kantarmedia-healthcare.com/how-are-physicians-using-smartphones-for-professional-purposes. Accessed June 14, 2013.
6. Penn Medical Student Government. 2012 Medical app survey results. February 9, 2013. Available at: http://msg.med.upenn.edu/?p=17784. Accessed June 19, 2013.
7. Comstock J. Manhattan: 72% of physicians have tablets. April 18, 2013. Available at: http://mobihealthnews.com/21733/manhattan-72-percent-of-physicians-have-tablets/. Accessed June 19, 2013.
8. Dr. Eric Topol on NBC’s Rock Center. January 24, 2013. Available at: http://www.youtube.com/watch?v=0B-jUOOrtks. Accessed June 14, 2013.
9. Comstock J. Topol turns Colbert around on digital health. March 27, 2013. Available at: http://mobihealthnews.com/21263/topol-turns-colbert-around-on-digital-health/.Accessed June 14,2013.
10. Pew Research Center. Tracking for health. January 28, 2013. Available at: http://pewinternet.org/Press-Releases/2013/Tracking-for-health. Accessed June 14, 2013.
11. Ozdalga E, Ozdalga A, Ahuja N. The smartphone in medicine: a review of current and potential use among physicians and students. J Med Internet Res. 2012;14:e128.
12. Mendoza M, Rosenberg T. Self-management of type 2 diabetes: a good idea or not? J Fam Pract. 2013;62:244-248.
13. McMillan R. iPad: ‘Wild West’ of medical apps seeks sheriff. December 12, 2011. Available at: http://www.wired.com/wiredenterprise/2011/12/fda_apps/. Accessed June 14, 2013.
14. Hodge B. The use of symptom diaries in outpatient care. Fam Pract Manag. 2013;20:24-28.
15. Haffey F, Brady RR, Maxwell S. A comparison of the reliability of smartphone apps for opioid conversion. Drug Saf. 2013;36:111-117.
16. US Food and Drug Administration. FDA proposes health “app” guidelines. July 19, 2011. Available at: http://www.fda.gov/forconsumers/consumerupdates/ucm263332.htm. Accessed June 14, 2013.
17. Pavlovic P. 10 issues that mobile medical app developers should keep in mind. April 18, 2013. Available at: http://www.mhimss.org/news/10-issues-mobile-medical-app-developers-should-keep-mind. Accessed June 14, 2013.
18. Federal Trade Commission. “Acne cure” mobile app marketers will drop baseless claims under FTC settlements. September 8, 2011. Available at: http://www.ftc.gov/opa/2011/09/acnecure.shtm. Accessed June 14, 2013.
19. FDA. Letter to Biosense Technologies Private Limited concerning the uChek urine analyzer. Available at: http://www.fda.gov/MedicalDevices/ResourcesforYou/Industry/ucm353513.htm. Accessed June 14, 2013.
20. Happtique publishes final standards for mobile health app certification program. February 27, 2013. Available at: http://www.happtique.com/happtique-publishes-final-standards-for-mobile-health-app-certification-program/. Accessed June 19, 2013.
21. mHIMSS. Privacy and security. Available at: http://www.mhimss.org/resource-topics/privacy-security. Accessed June 14, 2013.
In April, hundreds of attendees at TEDMED, a conference on medical innovation, waited in line for a “smartphone physical.” Curated by Shiv Gaglani, a medical student and an editor at the medical technology journal Medgadget, the exam involved 10 apps that turn an ordinary smartphone into a medical device (TABLE 1).1 Among them were the AliveCor Heart Monitor (pictured at right), which produces a one-lead EKG in seconds when a patient’s fingers or chest are pressed against the electrodes embedded in the back of what is essentially a phone case2; a pulse oximeter, and an ultrasound that can capture images of the carotid arteries.1
All but one of the apps is paired with a physical component, such as an ultrasound wand or otoscope. The exception is SpiroSmart, an app that uses the phone’s The AliveCor app and Heart Monitor—a smartphone case fitted with sensors—can generate a one-lead EKG tracing in seconds.built-in microphone and lip reverberations to assess lung function. Shwetak Patel, PhD, of the University of Washington, one of its developers, told JFP that the accuracy of SpiroSmart has been found to be within 5% of traditional spirometry results.3
While smartphone physicals are not likely to be integrated into family practice for some time to come, Glen Stream, MD, board chair of the American Academy of Family Physicians, predicts that integration of some of their features is not too far away. “The spirometry application is an especially good one; it addresses one of the top 5 chronic conditions that contribute to health care costs,” Dr. Stream said. The apps will be beneficial, he added, as long as they “are used in a way that contributes, to, rather than detracts from, collaboration between patients and physicians.”
For now, Dr. Stream and many of his fellow FPs use mobile devices and medical apps primarily to access reference materials, both in and out of the exam room. Some have begun “prescribing” apps to tech-savvy patients. Still others have never used a medical app, either because they prefer a desktop or laptop computer to a smartphone or tablet or because, as one FP put it, "I have a dumb phone."
Wherever you fall on the spectrum, it’s a safe bet that you’re going to be increasingly inundated by the many manifestations of mobile health (mHealth).
Epocrates is No. 1 reference app
The number of medical/health apps for smart-phones or tablets is difficult to pin down; estimates range from 17,000 to more than 40,000, and growing.4 More is known about physician use of smartphones and tablets.
A March 2013 survey of nearly 3000 physicians found that 74% use smartphones at work and 43% use them to look up drug information.5 The favorite tool? A 2012 survey conducted by the University of Pennsylvania’s Perelman School of Medicine to identify the best medical apps put Epocrates at the top of the list (TABLE 2).6 Epocrates was the very first app cited by virtually all the FPs interviewed for this article, as well.
Other drug references cited tend to be patient-specific. Colan Kennelly, MD, a clinical educator at the Good Samaritan Family Medicine Residency in Phoenix, finds LactMed particularly useful. Developed by the National Library of Medicine and part of its Toxicology Data Network, the app lets you pull up medications quickly and see whether and how they will affect breastfeeding.
Another favorite of Kennelly’s is the Agency for Healthcare Research and Quality’s ePSS (electronic Preventive Services Selector) app designed to help primary care clinicians identify the preventive services that are appropriate for their patients. “You just plug in a patient’s age and sex”—(pregnancy, tobacco use, and whether the patient is sexually active are also considered)—“and it tells you what you should be checking for,” Dr. Kennelly said.
The benefits of mobile textbooks
Textbook apps and online texts are slowly gaining in popularity. A recent survey by Manhattan Research found that in 2013 for the first time, usage of electronic medical texts surpassed that of print editions.7 Part of the appeal is that mobile texts are easy to tote. “Apps make it possible to carry around information from a number of textbooks with no added weight,” said Richard Usatine, MD, of the University of Texas Health Science Center at San Antonio and editor of JFP’s Photo Rounds column. Dr. Usatine is also a principal of Usatine Media, which turns medical reference materials into apps.
Dr. Usatine’s own experience is a case in point. He recently used a textbook app to prepare to take his boards (for the fifth time). “I’ve brushed up each time,” he said, “but this time I really studied because it was fun.
“With a print textbook you have to cover up the answers so you don’t see them. Here, you don’t get to see the answer until you commit to one of the multiple choice answers. Then you get told what the correct answer is and why you got it right or wrong,” Dr. Usatine said. Interactivity, including the opportunity to watch a video, say, of a procedure to review how it’s done before embarking on it yourself, is a big part of the value of apps, he said.
Rx: App
In January, Eric Topol, MD, a prominent cardiologist and chief academic officer of Scripps Health in La Jolla, Calif., demonstrated the AliveCor heart monitor and other mobile devices on NBC’s Rock Center.8 In March, he went on The Colbert Report and examined Stephen Colbert’s ear with an otoscope smartphone accessory (CellScope) like the one used in Gaglani’s smartphone physical.9 Dr. Topol’s use of the mobile heart monitor to assess an airplane passenger in distress midflight also received widespread news coverage.
In response to an interviewer’s question, Dr. Topol said he is now more likely to prescribe an app than a drug.8 While it’s unlikely that any FP could make such a claim, many have begun recommending apps to tech-savvy patients.
Smartphones as symptom trackers
A January 2013 Pew Internet study found that 7 in 10 US adults track at least one health indicator, for themselves or a loved one. Six in 10 reported tracking weight, diet, or exercise, and one in 3 said they track indicators of medical problems, such as blood pressure, glucose levels, headaches, or sleep patterns—usually without the aid of a smartphone.10
In fact, half of those who report tracking health measures said they keep the information “in their head,” and a third still use pencil and paper.10 That could change, of course, if their physicians suggest they do otherwise (TABLE 3).
Kelly M. Latimer, MD, an FP in the Navy stationed in Djibouti, Africa, routinely asks patients whether they have a smartphone and often recommends apps to those who do.
“It sounds like you have a lot of different symptoms,” she might say to a patient who complains of frequent headaches. “It will help me if you keep a headache diary.”
She used to give such patients paper and pen, Dr. Latimer noted. “Now I ask them to download the app (iHeadache, in this case) right then and there and do a quick review” so they’re ready to use it at home.
Apps are also a good way to help people with anxiety, Dr. Latimer has found. She frequently recommends apps like Relaxation Techniques and Breathe2Relax, and often suggests apps like Calorie Count and MyFitnessPal to boost patients’ efforts to lose weight and get in shape.
Abigail Lowther, MD, an FP at the University of Michigan in Ann Arbor, also recommends apps frequently. But she typically broaches the subject only with patients who have their smartphones out when she walks into the room.
Among the apps Dr. Lowther prescribes are myPause to track menopausal symptoms and Bladder Pal, a voiding diary for women struggling with incontinence. She advises women taking oral contraceptives to use the timer function on their phone to remember to take a pill at the same time every day. But there are apps (myPill, for one) that do that, too.
The upside of patient apps. A smartphone is ideal for keeping a symptom diary because it’s something that most people are never without. Anyone can use the notes function on a phone or tablet to jot down details about exacerbations, but those using disease-specific apps tend to capture more precise information. Some patients print out the information they’ve gathered and bring a hard copy to an office visit, while others simply show their physician what’s on their smartphone.
Can apps affect outcomes? There are few high-quality studies and the jury is still out, but “the smartphone has a very bright future in the world of medicine,” the authors of a review of smartphones in the medical arena concluded. After examining the use of apps to track (literally) wandering dementia patients; calculate and recommend insulin dosages for patients with type 1 diabetes; and teach yoga, to name a few, the researchers concluded that “the smartphone may one day be recognized as a diagnostic and therapeutic tool…as irreplaceable as the stethoscope.”11
Dr. Lowther recalls an obese patient who found MyFitnessPal to be helpful where other, more traditional diet programs had failed. The reason? He was less than truthful with the people overseeing the weight loss programs about what he’d eaten when he tried—and failed—to follow diets like Weight Watchers. He then ended up feeling so guilty that he abandoned the effort entirely. But, he told her, he “wouldn’t lie” to an app.
…and the downside. Even physicians who haven’t begun A weight loss app would be more likely to help this patient reach his goal than other diet programs because he "wouldn't lie" to an app.recommending apps to patients are aware that carefully tracking measures related to chronic conditions like hypertension or diabetes often results in better control. But in some cases, there may be too much of a good thing. Evidence suggests that for some patients with type 2 diabetes, glucose self-monitoring is associated with depression and may do more harm than good.12
Dr. Lowther has witnessed a similar phenomenon in patients using disease-tracking apps. “Sometimes people get too focused on the problem and drive themselves crazy,” she observed, adding that those with high blood pressure are particularly at risk. “I think sometimes it’s hard for patients to understand the concept of an average value and normal fluctuation,” Dr. Lowther said. When that happens, “I have to tell them to back off.”
Who's minding the (app) store?
The mHealth arena has been called “the wild West.”13 With at least one app for virtually every aspect of health and medicine you can think of, it’s not hard to understand why.
In an article on the use of symptom diaries in outpatient care, Bryan Hodge, DO, an FP in Hendersonville, NC, mentions mobile self-tracking apps as one of a number of ways for patients to keep symptom diaries.14 Given the fact that few of these apps have been validated, Dr. Hodge writes, “The best approach is to familiarize yourself with a few options that you can offer to your patients.”14
That depends on the nature of the app. An app that tracks calories consumed or simply keeps an organized file of patient symptoms may do little harm; an app that conveys physical measurements that a patient or physician may act on or calculates medication dosages requires a higher level of vigilance.
A recent study of smartphone apps that calculate opioid dosage conversion, for example, found a lack of consistency that raised a red flag about the reliability of information provided by unvalidated apps. Better regulation of medical apps is crucial to ensure that patient safety is maintained, the authors concluded.15
The FDA’s role
The US Food and Drug Administration, which has approved more than 75 medical apps, issued a proposed approach to its oversight of the apps in 2011.16
Under the proposed rules, the agency would regulate mobile apps that were either used as an accessory to a medical device already regulated by the FDA or that transform a smartphone or tablet into a regulated medical device. A final rule has not yet been issued, but a spokesperson told Congress that it will be forthcoming before the end of the year.17
False claims are a target of federal regulation, as well. In 2011, the Federal Trade Commission pulled 2 acne apps off the market because both advertised—without scientific evidence—that the light emitted by smartphones equipped with the apps could treat acne. “Smartphones make our lives easier in countless ways, but unfortunately, when it comes to curing acne, there’s no app for that,” the FTC chairman stated in a press release.18
In May 2013, the FDA sent an “It has come to our attention letter” to Biosense Technologies regarding its uChek urine analyzer app. The problem, the letter stated, is that the dipsticks that the app allows a mobile phone to analyze are cleared by the FDA only when interpreted by direct visual reading. But the phone and device together function “as an automated strip reader”—a urinalysis test system for which new FDA Smartphones make our lives easier in countless ways, but unfortunately, when it comes to curing acne, there's no app for that," the chairman of the Federal Trade Commission stated in a press release. clearance is required.19
Other ways of evaluating apps
Happtique, a mobile health solutions company, recently announced the launch of its Health App Certification Program—a voluntary program designed to help clinicians and patients easily identify apps that are credible and safe.20 “We will be certifying medical, health, and fitness apps, Corey Ackerman, president and CEO of Happtique, told JFP. The program is currently accepting medical education and nursing apps for review, and “discussions are underway with numerous other organizations that will provide experts for apps in additional subject matter areas,” Mr. Ackerman said.
There are other means of evaluating mobile medical apps that fall outside of the medical device realm, of course—starting by perusing the reviews posted at the app stores. Exchanging information with other clinicians using an app you’re interested in is another way to learn more about its efficacy. (Yes, there’s an app for that, too: Doximity, the professional network for clinicians.)
Other suggestions for safe use of apps:
- Peruse iMedicalApps (imedicalapps.com), the self-described leading physician publication on mobile medicine. Its physician editors and team of clinicians research and review medical apps.
- Consider the source. An app that has been developed by a medical society, federal agency, or prestigious medical school, for example, is more trustworthy than one from an unknown source (a point you would be wise to pass on to your patients).
- Try the app yourself before you recommend it to a patient.
Finally, keep the privacy provision in the Health Insurance Portability and Accountability Act in mind. Before using any app through which private patient health information can be transmitted or stored, ensure that the data will be encrypted and that your mobile device is password-protected, advises mHIMSS, the mobile branch of the Healthcare Information and Management Systems Society.21
In April, hundreds of attendees at TEDMED, a conference on medical innovation, waited in line for a “smartphone physical.” Curated by Shiv Gaglani, a medical student and an editor at the medical technology journal Medgadget, the exam involved 10 apps that turn an ordinary smartphone into a medical device (TABLE 1).1 Among them were the AliveCor Heart Monitor (pictured at right), which produces a one-lead EKG in seconds when a patient’s fingers or chest are pressed against the electrodes embedded in the back of what is essentially a phone case2; a pulse oximeter, and an ultrasound that can capture images of the carotid arteries.1
All but one of the apps is paired with a physical component, such as an ultrasound wand or otoscope. The exception is SpiroSmart, an app that uses the phone’s The AliveCor app and Heart Monitor—a smartphone case fitted with sensors—can generate a one-lead EKG tracing in seconds.built-in microphone and lip reverberations to assess lung function. Shwetak Patel, PhD, of the University of Washington, one of its developers, told JFP that the accuracy of SpiroSmart has been found to be within 5% of traditional spirometry results.3
While smartphone physicals are not likely to be integrated into family practice for some time to come, Glen Stream, MD, board chair of the American Academy of Family Physicians, predicts that integration of some of their features is not too far away. “The spirometry application is an especially good one; it addresses one of the top 5 chronic conditions that contribute to health care costs,” Dr. Stream said. The apps will be beneficial, he added, as long as they “are used in a way that contributes, to, rather than detracts from, collaboration between patients and physicians.”
For now, Dr. Stream and many of his fellow FPs use mobile devices and medical apps primarily to access reference materials, both in and out of the exam room. Some have begun “prescribing” apps to tech-savvy patients. Still others have never used a medical app, either because they prefer a desktop or laptop computer to a smartphone or tablet or because, as one FP put it, "I have a dumb phone."
Wherever you fall on the spectrum, it’s a safe bet that you’re going to be increasingly inundated by the many manifestations of mobile health (mHealth).
Epocrates is No. 1 reference app
The number of medical/health apps for smart-phones or tablets is difficult to pin down; estimates range from 17,000 to more than 40,000, and growing.4 More is known about physician use of smartphones and tablets.
A March 2013 survey of nearly 3000 physicians found that 74% use smartphones at work and 43% use them to look up drug information.5 The favorite tool? A 2012 survey conducted by the University of Pennsylvania’s Perelman School of Medicine to identify the best medical apps put Epocrates at the top of the list (TABLE 2).6 Epocrates was the very first app cited by virtually all the FPs interviewed for this article, as well.
Other drug references cited tend to be patient-specific. Colan Kennelly, MD, a clinical educator at the Good Samaritan Family Medicine Residency in Phoenix, finds LactMed particularly useful. Developed by the National Library of Medicine and part of its Toxicology Data Network, the app lets you pull up medications quickly and see whether and how they will affect breastfeeding.
Another favorite of Kennelly’s is the Agency for Healthcare Research and Quality’s ePSS (electronic Preventive Services Selector) app designed to help primary care clinicians identify the preventive services that are appropriate for their patients. “You just plug in a patient’s age and sex”—(pregnancy, tobacco use, and whether the patient is sexually active are also considered)—“and it tells you what you should be checking for,” Dr. Kennelly said.
The benefits of mobile textbooks
Textbook apps and online texts are slowly gaining in popularity. A recent survey by Manhattan Research found that in 2013 for the first time, usage of electronic medical texts surpassed that of print editions.7 Part of the appeal is that mobile texts are easy to tote. “Apps make it possible to carry around information from a number of textbooks with no added weight,” said Richard Usatine, MD, of the University of Texas Health Science Center at San Antonio and editor of JFP’s Photo Rounds column. Dr. Usatine is also a principal of Usatine Media, which turns medical reference materials into apps.
Dr. Usatine’s own experience is a case in point. He recently used a textbook app to prepare to take his boards (for the fifth time). “I’ve brushed up each time,” he said, “but this time I really studied because it was fun.
“With a print textbook you have to cover up the answers so you don’t see them. Here, you don’t get to see the answer until you commit to one of the multiple choice answers. Then you get told what the correct answer is and why you got it right or wrong,” Dr. Usatine said. Interactivity, including the opportunity to watch a video, say, of a procedure to review how it’s done before embarking on it yourself, is a big part of the value of apps, he said.
Rx: App
In January, Eric Topol, MD, a prominent cardiologist and chief academic officer of Scripps Health in La Jolla, Calif., demonstrated the AliveCor heart monitor and other mobile devices on NBC’s Rock Center.8 In March, he went on The Colbert Report and examined Stephen Colbert’s ear with an otoscope smartphone accessory (CellScope) like the one used in Gaglani’s smartphone physical.9 Dr. Topol’s use of the mobile heart monitor to assess an airplane passenger in distress midflight also received widespread news coverage.
In response to an interviewer’s question, Dr. Topol said he is now more likely to prescribe an app than a drug.8 While it’s unlikely that any FP could make such a claim, many have begun recommending apps to tech-savvy patients.
Smartphones as symptom trackers
A January 2013 Pew Internet study found that 7 in 10 US adults track at least one health indicator, for themselves or a loved one. Six in 10 reported tracking weight, diet, or exercise, and one in 3 said they track indicators of medical problems, such as blood pressure, glucose levels, headaches, or sleep patterns—usually without the aid of a smartphone.10
In fact, half of those who report tracking health measures said they keep the information “in their head,” and a third still use pencil and paper.10 That could change, of course, if their physicians suggest they do otherwise (TABLE 3).
Kelly M. Latimer, MD, an FP in the Navy stationed in Djibouti, Africa, routinely asks patients whether they have a smartphone and often recommends apps to those who do.
“It sounds like you have a lot of different symptoms,” she might say to a patient who complains of frequent headaches. “It will help me if you keep a headache diary.”
She used to give such patients paper and pen, Dr. Latimer noted. “Now I ask them to download the app (iHeadache, in this case) right then and there and do a quick review” so they’re ready to use it at home.
Apps are also a good way to help people with anxiety, Dr. Latimer has found. She frequently recommends apps like Relaxation Techniques and Breathe2Relax, and often suggests apps like Calorie Count and MyFitnessPal to boost patients’ efforts to lose weight and get in shape.
Abigail Lowther, MD, an FP at the University of Michigan in Ann Arbor, also recommends apps frequently. But she typically broaches the subject only with patients who have their smartphones out when she walks into the room.
Among the apps Dr. Lowther prescribes are myPause to track menopausal symptoms and Bladder Pal, a voiding diary for women struggling with incontinence. She advises women taking oral contraceptives to use the timer function on their phone to remember to take a pill at the same time every day. But there are apps (myPill, for one) that do that, too.
The upside of patient apps. A smartphone is ideal for keeping a symptom diary because it’s something that most people are never without. Anyone can use the notes function on a phone or tablet to jot down details about exacerbations, but those using disease-specific apps tend to capture more precise information. Some patients print out the information they’ve gathered and bring a hard copy to an office visit, while others simply show their physician what’s on their smartphone.
Can apps affect outcomes? There are few high-quality studies and the jury is still out, but “the smartphone has a very bright future in the world of medicine,” the authors of a review of smartphones in the medical arena concluded. After examining the use of apps to track (literally) wandering dementia patients; calculate and recommend insulin dosages for patients with type 1 diabetes; and teach yoga, to name a few, the researchers concluded that “the smartphone may one day be recognized as a diagnostic and therapeutic tool…as irreplaceable as the stethoscope.”11
Dr. Lowther recalls an obese patient who found MyFitnessPal to be helpful where other, more traditional diet programs had failed. The reason? He was less than truthful with the people overseeing the weight loss programs about what he’d eaten when he tried—and failed—to follow diets like Weight Watchers. He then ended up feeling so guilty that he abandoned the effort entirely. But, he told her, he “wouldn’t lie” to an app.
…and the downside. Even physicians who haven’t begun A weight loss app would be more likely to help this patient reach his goal than other diet programs because he "wouldn't lie" to an app.recommending apps to patients are aware that carefully tracking measures related to chronic conditions like hypertension or diabetes often results in better control. But in some cases, there may be too much of a good thing. Evidence suggests that for some patients with type 2 diabetes, glucose self-monitoring is associated with depression and may do more harm than good.12
Dr. Lowther has witnessed a similar phenomenon in patients using disease-tracking apps. “Sometimes people get too focused on the problem and drive themselves crazy,” she observed, adding that those with high blood pressure are particularly at risk. “I think sometimes it’s hard for patients to understand the concept of an average value and normal fluctuation,” Dr. Lowther said. When that happens, “I have to tell them to back off.”
Who's minding the (app) store?
The mHealth arena has been called “the wild West.”13 With at least one app for virtually every aspect of health and medicine you can think of, it’s not hard to understand why.
In an article on the use of symptom diaries in outpatient care, Bryan Hodge, DO, an FP in Hendersonville, NC, mentions mobile self-tracking apps as one of a number of ways for patients to keep symptom diaries.14 Given the fact that few of these apps have been validated, Dr. Hodge writes, “The best approach is to familiarize yourself with a few options that you can offer to your patients.”14
That depends on the nature of the app. An app that tracks calories consumed or simply keeps an organized file of patient symptoms may do little harm; an app that conveys physical measurements that a patient or physician may act on or calculates medication dosages requires a higher level of vigilance.
A recent study of smartphone apps that calculate opioid dosage conversion, for example, found a lack of consistency that raised a red flag about the reliability of information provided by unvalidated apps. Better regulation of medical apps is crucial to ensure that patient safety is maintained, the authors concluded.15
The FDA’s role
The US Food and Drug Administration, which has approved more than 75 medical apps, issued a proposed approach to its oversight of the apps in 2011.16
Under the proposed rules, the agency would regulate mobile apps that were either used as an accessory to a medical device already regulated by the FDA or that transform a smartphone or tablet into a regulated medical device. A final rule has not yet been issued, but a spokesperson told Congress that it will be forthcoming before the end of the year.17
False claims are a target of federal regulation, as well. In 2011, the Federal Trade Commission pulled 2 acne apps off the market because both advertised—without scientific evidence—that the light emitted by smartphones equipped with the apps could treat acne. “Smartphones make our lives easier in countless ways, but unfortunately, when it comes to curing acne, there’s no app for that,” the FTC chairman stated in a press release.18
In May 2013, the FDA sent an “It has come to our attention letter” to Biosense Technologies regarding its uChek urine analyzer app. The problem, the letter stated, is that the dipsticks that the app allows a mobile phone to analyze are cleared by the FDA only when interpreted by direct visual reading. But the phone and device together function “as an automated strip reader”—a urinalysis test system for which new FDA Smartphones make our lives easier in countless ways, but unfortunately, when it comes to curing acne, there's no app for that," the chairman of the Federal Trade Commission stated in a press release. clearance is required.19
Other ways of evaluating apps
Happtique, a mobile health solutions company, recently announced the launch of its Health App Certification Program—a voluntary program designed to help clinicians and patients easily identify apps that are credible and safe.20 “We will be certifying medical, health, and fitness apps, Corey Ackerman, president and CEO of Happtique, told JFP. The program is currently accepting medical education and nursing apps for review, and “discussions are underway with numerous other organizations that will provide experts for apps in additional subject matter areas,” Mr. Ackerman said.
There are other means of evaluating mobile medical apps that fall outside of the medical device realm, of course—starting by perusing the reviews posted at the app stores. Exchanging information with other clinicians using an app you’re interested in is another way to learn more about its efficacy. (Yes, there’s an app for that, too: Doximity, the professional network for clinicians.)
Other suggestions for safe use of apps:
- Peruse iMedicalApps (imedicalapps.com), the self-described leading physician publication on mobile medicine. Its physician editors and team of clinicians research and review medical apps.
- Consider the source. An app that has been developed by a medical society, federal agency, or prestigious medical school, for example, is more trustworthy than one from an unknown source (a point you would be wise to pass on to your patients).
- Try the app yourself before you recommend it to a patient.
Finally, keep the privacy provision in the Health Insurance Portability and Accountability Act in mind. Before using any app through which private patient health information can be transmitted or stored, ensure that the data will be encrypted and that your mobile device is password-protected, advises mHIMSS, the mobile branch of the Healthcare Information and Management Systems Society.21
1. TEDMED. The smartphone physical. Available at: http://www.smartphonephysical.org/tedmed.html. Accessed June 14, 2013.
2. AliveCor. AliveCor heart monitor. Available at: http://www.alivecor.com/. Accessed June 14, 2013.
3. Ubiquitous Computing Lab, University of Washington. Mobile phone spirometry. Available at: http://ubicomplab.cs.washington.edu/wiki/SpiroSmart. Accessed June 19, 2013.
4. Association of American Medical Colleges. Explosive growth in health care apps raises oversight questions. Available at: https://www.aamc.org/newsroom/reporter/october2012/308516/health-care-apps.html. Accessed June 14, 2013.
5. Alvarez A. How are physicians using smartphones for professional purposes? April 22, 2013. Available at: www.kantarmedia-healthcare.com/how-are-physicians-using-smartphones-for-professional-purposes. Accessed June 14, 2013.
6. Penn Medical Student Government. 2012 Medical app survey results. February 9, 2013. Available at: http://msg.med.upenn.edu/?p=17784. Accessed June 19, 2013.
7. Comstock J. Manhattan: 72% of physicians have tablets. April 18, 2013. Available at: http://mobihealthnews.com/21733/manhattan-72-percent-of-physicians-have-tablets/. Accessed June 19, 2013.
8. Dr. Eric Topol on NBC’s Rock Center. January 24, 2013. Available at: http://www.youtube.com/watch?v=0B-jUOOrtks. Accessed June 14, 2013.
9. Comstock J. Topol turns Colbert around on digital health. March 27, 2013. Available at: http://mobihealthnews.com/21263/topol-turns-colbert-around-on-digital-health/.Accessed June 14,2013.
10. Pew Research Center. Tracking for health. January 28, 2013. Available at: http://pewinternet.org/Press-Releases/2013/Tracking-for-health. Accessed June 14, 2013.
11. Ozdalga E, Ozdalga A, Ahuja N. The smartphone in medicine: a review of current and potential use among physicians and students. J Med Internet Res. 2012;14:e128.
12. Mendoza M, Rosenberg T. Self-management of type 2 diabetes: a good idea or not? J Fam Pract. 2013;62:244-248.
13. McMillan R. iPad: ‘Wild West’ of medical apps seeks sheriff. December 12, 2011. Available at: http://www.wired.com/wiredenterprise/2011/12/fda_apps/. Accessed June 14, 2013.
14. Hodge B. The use of symptom diaries in outpatient care. Fam Pract Manag. 2013;20:24-28.
15. Haffey F, Brady RR, Maxwell S. A comparison of the reliability of smartphone apps for opioid conversion. Drug Saf. 2013;36:111-117.
16. US Food and Drug Administration. FDA proposes health “app” guidelines. July 19, 2011. Available at: http://www.fda.gov/forconsumers/consumerupdates/ucm263332.htm. Accessed June 14, 2013.
17. Pavlovic P. 10 issues that mobile medical app developers should keep in mind. April 18, 2013. Available at: http://www.mhimss.org/news/10-issues-mobile-medical-app-developers-should-keep-mind. Accessed June 14, 2013.
18. Federal Trade Commission. “Acne cure” mobile app marketers will drop baseless claims under FTC settlements. September 8, 2011. Available at: http://www.ftc.gov/opa/2011/09/acnecure.shtm. Accessed June 14, 2013.
19. FDA. Letter to Biosense Technologies Private Limited concerning the uChek urine analyzer. Available at: http://www.fda.gov/MedicalDevices/ResourcesforYou/Industry/ucm353513.htm. Accessed June 14, 2013.
20. Happtique publishes final standards for mobile health app certification program. February 27, 2013. Available at: http://www.happtique.com/happtique-publishes-final-standards-for-mobile-health-app-certification-program/. Accessed June 19, 2013.
21. mHIMSS. Privacy and security. Available at: http://www.mhimss.org/resource-topics/privacy-security. Accessed June 14, 2013.
1. TEDMED. The smartphone physical. Available at: http://www.smartphonephysical.org/tedmed.html. Accessed June 14, 2013.
2. AliveCor. AliveCor heart monitor. Available at: http://www.alivecor.com/. Accessed June 14, 2013.
3. Ubiquitous Computing Lab, University of Washington. Mobile phone spirometry. Available at: http://ubicomplab.cs.washington.edu/wiki/SpiroSmart. Accessed June 19, 2013.
4. Association of American Medical Colleges. Explosive growth in health care apps raises oversight questions. Available at: https://www.aamc.org/newsroom/reporter/october2012/308516/health-care-apps.html. Accessed June 14, 2013.
5. Alvarez A. How are physicians using smartphones for professional purposes? April 22, 2013. Available at: www.kantarmedia-healthcare.com/how-are-physicians-using-smartphones-for-professional-purposes. Accessed June 14, 2013.
6. Penn Medical Student Government. 2012 Medical app survey results. February 9, 2013. Available at: http://msg.med.upenn.edu/?p=17784. Accessed June 19, 2013.
7. Comstock J. Manhattan: 72% of physicians have tablets. April 18, 2013. Available at: http://mobihealthnews.com/21733/manhattan-72-percent-of-physicians-have-tablets/. Accessed June 19, 2013.
8. Dr. Eric Topol on NBC’s Rock Center. January 24, 2013. Available at: http://www.youtube.com/watch?v=0B-jUOOrtks. Accessed June 14, 2013.
9. Comstock J. Topol turns Colbert around on digital health. March 27, 2013. Available at: http://mobihealthnews.com/21263/topol-turns-colbert-around-on-digital-health/.Accessed June 14,2013.
10. Pew Research Center. Tracking for health. January 28, 2013. Available at: http://pewinternet.org/Press-Releases/2013/Tracking-for-health. Accessed June 14, 2013.
11. Ozdalga E, Ozdalga A, Ahuja N. The smartphone in medicine: a review of current and potential use among physicians and students. J Med Internet Res. 2012;14:e128.
12. Mendoza M, Rosenberg T. Self-management of type 2 diabetes: a good idea or not? J Fam Pract. 2013;62:244-248.
13. McMillan R. iPad: ‘Wild West’ of medical apps seeks sheriff. December 12, 2011. Available at: http://www.wired.com/wiredenterprise/2011/12/fda_apps/. Accessed June 14, 2013.
14. Hodge B. The use of symptom diaries in outpatient care. Fam Pract Manag. 2013;20:24-28.
15. Haffey F, Brady RR, Maxwell S. A comparison of the reliability of smartphone apps for opioid conversion. Drug Saf. 2013;36:111-117.
16. US Food and Drug Administration. FDA proposes health “app” guidelines. July 19, 2011. Available at: http://www.fda.gov/forconsumers/consumerupdates/ucm263332.htm. Accessed June 14, 2013.
17. Pavlovic P. 10 issues that mobile medical app developers should keep in mind. April 18, 2013. Available at: http://www.mhimss.org/news/10-issues-mobile-medical-app-developers-should-keep-mind. Accessed June 14, 2013.
18. Federal Trade Commission. “Acne cure” mobile app marketers will drop baseless claims under FTC settlements. September 8, 2011. Available at: http://www.ftc.gov/opa/2011/09/acnecure.shtm. Accessed June 14, 2013.
19. FDA. Letter to Biosense Technologies Private Limited concerning the uChek urine analyzer. Available at: http://www.fda.gov/MedicalDevices/ResourcesforYou/Industry/ucm353513.htm. Accessed June 14, 2013.
20. Happtique publishes final standards for mobile health app certification program. February 27, 2013. Available at: http://www.happtique.com/happtique-publishes-final-standards-for-mobile-health-app-certification-program/. Accessed June 19, 2013.
21. mHIMSS. Privacy and security. Available at: http://www.mhimss.org/resource-topics/privacy-security. Accessed June 14, 2013.
Is your patient sick—or hungry?
Late last year, news outlets nationwide confirmed what many had long suspected: America’s middle class is shrinking. The latest data from the US Census Bureau found that nearly half (48%) of Americans are poor or low income.1,2
That means 46.2 million people—more than 15% of US citizens—are living below the federal poverty level (FPL), which is $23,050 for a family of 4. Another 97.3 million (about 33%) meet the criterion for low income—earning between $23,050 and $45,869 for a family of 4.1,2 These numbers are based on the Census Bureau’s new supplemental poverty measure, which considers costs like medical and housing and benefits such as food stamps in calculating poverty.3
The way that census data are analyzed is a key consideration for policy makers and legislators. For primary care physicians, the findings simply serve as a critical reminder that millions of Americans—including some of your patients—are struggling to stay afloat.
In some cases, the problems patients face will be so severe that there won’t be much you can do about them. In others, there are steps you can take to lend a helping hand (TABLE).
TABLE
Help the poor and uninsured: 9 things you can do
|
Death by poverty?
That’s the title of a summary of a recent study, posted on the Web site of Columbia University’s Mailman School of Public Health.4 The researchers found that poverty, low levels of education, and a lack of social support, among other “social” factors, account for as many deaths as heart attack, stroke, and lung cancer.5
A related study, also by researchers at Columbia, attempted to quantify the health impact of some leading medical and nonmedical factors. Their findings: The detrimental effects of poverty, smoking, and being a high school dropout exceed those of binge drinking, being overweight or obese, and being uninsured.6 The average low-income individual loses 8.2 years of good health simply because of his or her economic status, the lead researcher reported. In contrast, the average loss associated with obesity is 4.2 years and 6.6 years with smoking. The overall health of the US population won’t improve until poverty rates are reduced and educational deficits are addressed, the lead researcher concluded.7
That’s not to negate the importance of health coverage, however: A Kaiser Family Foundation study of low-income adults found that fully half (51%) of those who lacked health insurance had not gone to a doctor or clinic in the previous 12 months—and 69% had received no preventive care in the course of the year.8
Another survey, completed in 2007, asked adults younger than 65 about their use of medication. About 1 in 7 (13.9%) said they had failed to fill a prescription in the previous year because they couldn’t afford it. Four years earlier, 10.3% had done so.9
Recently, however, the situation appears to have gotten even worse. In a 2011 Consumer Reports survey, just under half of adults taking prescription medication reported that they had cut costs by engaging in what the surveyors described as “risky health care tradeoffs”—eg, not filling a prescription, skipping doses, or taking an expired medication.10
Poverty in childhood has long-lasting effects
Children may be less likely than adults to require prescription drugs, but they are typically the hardest hit by poverty—both in numbers and long-term effects. The poverty rate for those younger than 18 is 22%, according to the National Center for Children in Poverty.11 For kids under the age of 5, it’s more than 25%.12
Children of poor, uneducated parents have worse health and die earlier than those whose families are wealthier and better educated, research suggests.13-16 Even kids from middle class families fall short on measures of health and well-being compared with children whose families are more affluent. What’s more, being poor in early childhood appears to have lasting effects. Regardless of social or economic status or individual behavior later in life, studies suggest that the stress of poverty in the early years is associated with chronic illness and disability in adulthood.13-16
The bottom line, according to the Robert Wood Johnson Commission to Build a Healthier America: “For the first time in our history, the United States is raising a generation of children who may live sicker, shorter lives than their parents.”13 Hunger, or the lack of an adequate supply of nutritious food, is a key factor.17
Hunger hits home
In an op-ed in the San Francisco Chronicle, family physician Laura Gottlieb told the story of an 8-year-old boy whose family she’d known for years. Brought to her office because of abdominal pain, the boy underwent multiple tests, including urine and stool examinations, blood work, and imaging studies. As soon as one test came back, Dr. Gottlieb ordered another. All were negative, and no cause for GI distress was found.18
Only later did she discover that hunger was the source of the pain. “It had never even occurred to me to ask his mother about how much food there was in the house,” Dr. Gottlieb wrote.18
In a similar vein, CBS News recently ran a story about a high school football team that seemed to be down on its luck. Besides being on a losing streak, many of the players were lethargic. Eventually, an astute coach realized that a mental pickup wasn’t what the team members needed—nutrition was. In this impoverished Burke County, Georgia school, about 85% of the student body qualify for in-school breakfast and lunch. But for many kids, those 2 meals were all they had to eat.19
With the help of a school nutritionist and the federal Healthy Hunger-Free Kids Act, hundreds of students now receive dinner, too. And last season, in late 2011, the properly fueled team members went on to win the state championship.19
Who is “food insecure”? In 2010, the latest year for which figures are available, 14.5% of US households (representing a total of 48.8 million people) were “food insecure,” as the problem of having too little to eat is officially known.20 Most of these families managed without substantially disrupting their normal eating patterns or reducing their intake, the US Department of Agriculture reports. This was accomplished by cutting back on the variety of foods they ate, getting federal food assistance, or getting food from food banks, among other coping strategies. But for 6.4 million households, the problem was severe enough to disrupt normal eating patterns and cause those affected to eat less than usual at least part of the time in the course of the year.20
Here, too, the toll on children is especially high. Twenty percent of households with children face food insecurity, nearly twice the rate of childless households.20 In a child’s earliest years, too little energy, protein, and other nutrients can result in long-lasting deficits in social, cognitive, and emotional development; malnutrition and deficiencies in vitamins and minerals may even result in brain impairment.18 In addition, school-age children who don’t have enough to eat have more behavioral problems and are more likely than those who are not struggling with hunger to be in special education classes.17
The hunger and obesity link
Ironically, hunger is also associated with obesity. High calorie, high carbohydrate foods like pasta and bread typically cost considerably less than nutrient-rich low-carb foods like cheese, fruit, fish, and vegetables, and are more filling. And in poor neighborhoods, food that is high in carbohydrates and low in protein and other nutrients tends to be more available than fresh, healthy—and more perishable—food.21
What’s more, people living in poverty may find it especially difficult to exercise. In many neighborhoods, exercising outdoors can be dangerous, gyms are unaffordable, and safe parks and playgrounds may be few and far between.21
Identifying poor and hungry patients
In a survey conducted by the Childhood Hunger Initiative of Oregon, most of the nearly 200 physicians and nurse practitioners who responded expressed a desire to learn more about the consequences of hunger and how to address them. Besides being uncomfortable broaching the subject of hunger and other poverty-related issues, the providers cited time constraints as a barrier to doing so.22
Ask this question
Citing similar obstacles, Canadian researchers conducted a pilot study in search of an easy-to-use, evidence-based “case-finding” tool. They offered questionnaires to patients at 4 clinics in British Columbia to determine which questions had the highest likelihood of determining whether an individual was struggling with hunger, poverty, or homelessness. Participants, which included patients above (n=94) and below (n=51) the poverty line, were also asked how they felt about being asked such questions.23
One particular question—“Do you (ever) have difficulty making ends meet at the end of the month?”—proved to be the best predictor of poverty. Although 2 additional questions about food and housing were identified as suitable for a 3-item screening tool, this single question alone had 98% sensitivity and 60% specificity (odds ratio, 32.3; 95% confidence interval, 5.4-191.5). Equally important, 85% of study participants with income below the poverty level thought that poverty screening was important, and 67% said they felt comfortable talking to their family physician about it.23
Take this course
In response to the results of the provider survey conducted by the Childhood Hunger Initiative of Oregon, a team at the Oregon State University Extension Service developed an online training program. The free 5-module course, available at http://oregonstate.edu/instruct/dce/chi/modules.html, addresses the impact of childhood hunger and provides screening and intervention tips.24
A recommended strategy is to incorporate a question related to hunger and food insecurity into the medical history or physical assessment. Noting that you’ll learn more by asking whether a family has sufficient resources to provide a healthy diet than by simply inquiring about a balanced diet, a narrator uses this wording:
“In the past month, was there any day when you or anyone in your family went hungry because you didn’t have enough money for food?”24
What you can do to help needy patients
Some patients who are out of work, uninsured, and barely able to pay for food and shelter will simply put off doctor visits—or come in only after their condition is so dire that you have no recourse but to send them to the emergency department (ED). The result, of course, is just the opposite of what they had hoped for. They end up with a much larger bill—or, if they have coverage, with a much bigger copay—not to mention a far more serious condition than they would likely have had if they’d come in sooner.
Here are some ways you can help.
Discuss costs with uninsured patients. To encourage uninsured patients to come in before their condition worsens, make them aware of the comparatively low cost of a visit to your office vs that of, say, imaging studies, specialist visits, and lab tests, as well as ED costs. That’s one of the interventions recommended by Robert A. Forester, MD, and Richard J. Heck, MD, the authors of “What You Can Do to Help Your Uninsured Patients.”25 Consider offering discounts to low-income patients (within the bounds of Medicare and other insurance provisions), they also suggest.
Use fewer diagnostic tests. Ordering a battery of tests when a diagnosis is not readily apparent is a “cost-insensitive” way to practice medicine, authors Forester and Heck observe. Spending additional time with such patients, using your cognitive and diagnostic skills and performing a complete history and physical, frequently results in a diagnosis and treatment plan, they note.25 If patients are aware that you’re trying to minimize costs, they’ll often consent to a step-by-step diagnostic work-up that can be stopped at any time it is appropriate.
Do it yourself. Expand your practice to include a variety of minor procedures, such as removal or biopsy of common skin lesions, colposcopy, or setting simple fractures. These measures can help keep costs down to better serve poor and low-income patients. The American Academy of Family Physicians offers courses and training in various procedures that family physicians can competently perform in their own offices.
Request a courtesy consult. On occasion, you may be able to avoid a costly referral by calling a colleague and asking for a courtesy consult. The specialist will often tell you how he or she would handle a clinical presentation like the one you describe and suggest you try a similar approach, suggests Doug Campos-Outcalt, MD, MPA. Dr. Campos-Outcalt, a faculty member at the University of Arizona College of Medicine and the author of JFP’s bimonthly Practice Alert column, has extensive experience working with underserved communities.
Connect patients with community services. Poor patients typically have many social and psychological needs, as well as the need for medical care, and integrated care is particularly important for those facing hunger, homelessness, and chronic illness, says Jonathan Cartsonis, MD, medical director of Healthcare for the Homeless in Phoenix. Maintain contact with hospital social services and emergency psychiatric services, and have information—and handouts—about local food banks, homeless shelters, and community clinics, among other resources. (See the resources listed in the box.)
Feeding America Food Bank Locator
http://feedingamerica.org/foodbank-results.aspx
Insure Kids Now
http://www.insurekidsnow.gov/state/index.html/
National Association of Free and Charitable Clinics
http://www.freemedicalcamps.com
Nutrition Standards for School Meals (Healthy, Hunger-Free Kids Act)
http://www.fns.usda.gov/cnd/Governance/Legislation/nutritionstandards.htm
Partnership for Prescription Assistance
www.pparx.org
Rx Outreach
http://rxoutreach.com/
SNAP (Supplemental Nutrition Assistance Program)
http://www.fns.usda.gov/snap/applicant_recipients/eligibility.htm#income
WIC (Supplemental Nutrition Program for Women, Infants and Children)
http://stars.fns.usda.gov/wps/pages/start.jsf
In Seattle, for example, “Project Access” is an organization that helps give the underserved access to specialists. And in many parts of the country, local Rotary clubs sponsor free clinics staffed with volunteer and retired physicians, working cooperatively with local pharmacies to provide at-cost generic drugs.
Keep drug costs down
Physicians can help to insulate their poor and low-income patients from high drug costs in a number of ways:
Reduce polypharmacy. Half of Americans take at least one prescription drug, according to the 2011 Consumer Reports survey. Among this group, people with limited income—those earning less than $40,000—take, on average, 5.7 different drugs.10 Eliminating unnecessary medications, including supplements, herbs, and any other over-the-counter products, can lead to substantial savings. To determine what can be eliminated, ask patients to bring in everything they’re taking and conduct a brown bag medication review. To learn more, see “Help your patient ‘get’ what you just said: A health literacy guide” (J Fam Pract. 2012;61:190-196).
Prescribe generics. Newer brand-name drugs may not be markedly better than older, established agents. And many generics are available at major retailers like Wal-Mart for just a few dollars for a 30-day supply or at CVS for $9.99 for a 3-month supply.26 Yet some physicians routinely order newer medications, even for indigent patients.
Be upfront about drug costs. When you prescribe a new drug, whether generic or branded, it is important to discuss the cost (easily accessible online and in many electronic medical record systems) with the patient. Yet only 5% of respondents to the 2011 Consumer Reports survey said their health care providers had done so. Two-thirds of those surveyed (64%) did not discover the cost of a drug until they went to a pharmacy to pick it up.10
Think twice before handing out samples. Drug samples would appear to benefit the poor and the uninsured, but evidence suggests otherwise.27,28 In a study that assessed out-of-pocket costs associated with the use of samples, patients who had never received samples had lower out-of-pocket costs.28 That’s partly because most samples are newer, more expensive drugs, and patients who start taking them are often unable to afford the cost of a prescription. Another study found that the use of generic drugs for uninsured patients rose (from 12% to 30%) after the clinic discontinued the use of samples.27
CORRESPONDENCE Laura C. Lippman, MD, 2311 North 45th Street, No. 171, Seattle, WA 98103; lclippman@gmail.com
1. Tavernise S, Gebeloff R. New way to tally poor recasts view of poverty. New York Times. November 7, 2011. Available at: http://www.nytimes.com/2011/11/08/us/poverty-gets-new-measure-at-census-bureau.html?_r=2&scp=1&sq=poverty&st=cse. Accessed March 12, 2012.
2. Income poverty and health insurance coverage in the United States: 2010 [press release]. Washington, DC: US Census Bureau; September 13, 2011. Available at: http://www.census.gov/newsroom/releases/archives/income_wealth/cb11-157.html. Accessed March 12, 2012.
3. Short K. The research supplemental poverty measure: 2010. Washington, DC: US Census Bureau; November 2011. Available at: http://www.census.gov/hhes/povmeas/methodology/supplemental/research/Short_ResearchSPM2010.pdf. Accessed March 13, 2012.
4. University Mailman School of Public Health. Death by poverty? June 16, 2011. Available at: http://www.mailman.columbia.edu/academic-departments/epidemiology/research-service/death-poverty. Accessed March 5, 2012.
5. Galea S, Tracy M, Hoggatt KJ, et al. Estimated deaths attributable to social factors in the United States. Am J Public Health. 2011;101:1456-1465
6. Muennig P, Fiscella K, Tancredi D, et al. The relative health burden of selected social and behavioral risk factors in the United States: implications for policy. Am J Public Health. 2010;100:1758-1764.
7. Columbia University Mailman School of Public Health. Poor face greater health burden than smokers or the obese. Available at: http://www.mailman.columbia.edu/academic-departments/health-policy/news-events/poor-face-greater-health-burden-smokers-or-obese. Accessed March 13, 2012.
8. Schwartz K. How trends in the health care system affect low-income adults: identifying access problems and financial burdens. December 21, 2007. Kaiser Family Foundation. Available at: http://www.kff.org/uninsured/7705.cfm. Accessed March 2, 2012.
9. Felland LE, Reschovsky JD. More nonelderly Americans face problems affording prescription drugs. Tracking report no. 22. January 2009. Center for Studying Health System Change. Available at: http://www.hschange.com/CONTENT/1039/. Accessed January 25, 2012.
10. Consumer Reports poll: 48 percent of Americans on meds making risky health care tradeoffs [press release]. Yonkers, NY: Consumer Reports; September 27, 2011. Available at: http://www.prnewswire.com/news-releases/consumer-reports-poll—48-percent-of-americans-on-meds-making-risky-health-care-tradeoffs-130618778.html. Accessed January 3, 2012.
11. A job-loss recovery hurts children most: statistics tell an alarming story [press release] New York, NY: National Center for Children in Poverty; September 15, 2011. Available at: http://www.nccp.org/media/releases/release_135.html. Accessed January 24, 2012.
12. Child Trends Data Bank. Children in poverty. Updated September 2011. Available at: http://www.childtrendsdatabank.org/?q=node/221. Accessed March 13, 2012.
13. Robert Wood Johnson Foundation. Overcoming obstacles to health. Princeton, NJ: RWJF Commission to Build a Healthier America; February 2008. Available at: http://www.rwjf.org/files/research/obstaclestohealth.pdf. Accessed March 22, 2012.
14. Shonkoff JP, Garner AS. Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129:e232-e246.
15. Stein DJ, Scott K, Haro Abad JM, et al. Early childhood adversity and later hypertension: data from the World Mental Health Survey. Ann Clin Psychiatry. 2010;22:19-28.
16. O’Rand AM, Hamil-Luker J. Processes of cumulative adversity: childhood disadvantage and increased risk of heart attack across the life course. J Gerontol B Psychol Sci Soc Sci. 2005;60(spec no 2):117-124.
17. American Psychological Association. Effects of poverty, hunger, and homelessness on children and youth. Available at: http://www.apa.org/pi/families/poverty.aspx. Accessed November 29, 2011.
18. Gottlieb L. Funding healthy society helps cure health care. San Francisco Chronicle. August 23, 2010:A-8.
19. Doane S. High school football team battles malnutrition. December 20, 2011. CBS News. Available at: http://www.cbsnews.com/8301-18563_162-57345857/high-school-football-team-battles-malnutrition/. Accessed March 13, 2012.
20. US Department of Agriculture Economic Research Service. Food security in the United States: key statistics and graphics. Updated September 7, 2011. Available at: http://www.ers.usda.gov/Briefing/FoodSecurity/stats_graphs.htm. Accessed March 1, 2012.
21. Drewnowski A, Damon N. Food choices and diet costs: an economic analysis. J Nutr. 2005;135:900-904.
22. Survey helps doctors help hungry patients [press release]. Portland, Ore: Oregon State University Extension Service; May 27, 2008. Available at: http://extension.oregonstate.edu/news/release/2008/05/survey-helps-doctors-help-hungry-patients. Accessed February 29, 2012.
23. Brcic V, Eberdt C, Kaczorowski J. Development of a tool to identify poverty in a family practice setting: a pilot study. Int J Family Med. 2011;2011:812182.
24. Childhood food insecurity: health impacts, screening and intervention [course summary]. Corvallis, Ore: Oregon State University Extended Campus; 2010. Available at: http://oregonstate.edu/instruct/dce/chi/module5_8.html. Accessed March 13, 2012.
25. Forester RA, Heck RJ. What you can do to help your uninsured patients. Fam Pract Manag. 2009;16:21-24.
26. Byrd C. CVS drug prices takes on Wal-Mart’s generic drug prices—with a gimmicky twist. eDrugSearch. Available at: http://www.edrugsearch.com/edsblog/cvs-takes-on-wal-marts-generic-drug-prices-with-a-gimmicky-twist/. Accessed March 13, 2012.
27. Miller DP, Mansfield RJ, Woods JB, et al. The impact of drug samples on prescribing to the uninsured. South Med J. 2008;101:888-893.
28. Chimonas S, Kassirer JP. No more free drug samples? PLoS Med. 2009;6:e1000074.
Late last year, news outlets nationwide confirmed what many had long suspected: America’s middle class is shrinking. The latest data from the US Census Bureau found that nearly half (48%) of Americans are poor or low income.1,2
That means 46.2 million people—more than 15% of US citizens—are living below the federal poverty level (FPL), which is $23,050 for a family of 4. Another 97.3 million (about 33%) meet the criterion for low income—earning between $23,050 and $45,869 for a family of 4.1,2 These numbers are based on the Census Bureau’s new supplemental poverty measure, which considers costs like medical and housing and benefits such as food stamps in calculating poverty.3
The way that census data are analyzed is a key consideration for policy makers and legislators. For primary care physicians, the findings simply serve as a critical reminder that millions of Americans—including some of your patients—are struggling to stay afloat.
In some cases, the problems patients face will be so severe that there won’t be much you can do about them. In others, there are steps you can take to lend a helping hand (TABLE).
TABLE
Help the poor and uninsured: 9 things you can do
|
Death by poverty?
That’s the title of a summary of a recent study, posted on the Web site of Columbia University’s Mailman School of Public Health.4 The researchers found that poverty, low levels of education, and a lack of social support, among other “social” factors, account for as many deaths as heart attack, stroke, and lung cancer.5
A related study, also by researchers at Columbia, attempted to quantify the health impact of some leading medical and nonmedical factors. Their findings: The detrimental effects of poverty, smoking, and being a high school dropout exceed those of binge drinking, being overweight or obese, and being uninsured.6 The average low-income individual loses 8.2 years of good health simply because of his or her economic status, the lead researcher reported. In contrast, the average loss associated with obesity is 4.2 years and 6.6 years with smoking. The overall health of the US population won’t improve until poverty rates are reduced and educational deficits are addressed, the lead researcher concluded.7
That’s not to negate the importance of health coverage, however: A Kaiser Family Foundation study of low-income adults found that fully half (51%) of those who lacked health insurance had not gone to a doctor or clinic in the previous 12 months—and 69% had received no preventive care in the course of the year.8
Another survey, completed in 2007, asked adults younger than 65 about their use of medication. About 1 in 7 (13.9%) said they had failed to fill a prescription in the previous year because they couldn’t afford it. Four years earlier, 10.3% had done so.9
Recently, however, the situation appears to have gotten even worse. In a 2011 Consumer Reports survey, just under half of adults taking prescription medication reported that they had cut costs by engaging in what the surveyors described as “risky health care tradeoffs”—eg, not filling a prescription, skipping doses, or taking an expired medication.10
Poverty in childhood has long-lasting effects
Children may be less likely than adults to require prescription drugs, but they are typically the hardest hit by poverty—both in numbers and long-term effects. The poverty rate for those younger than 18 is 22%, according to the National Center for Children in Poverty.11 For kids under the age of 5, it’s more than 25%.12
Children of poor, uneducated parents have worse health and die earlier than those whose families are wealthier and better educated, research suggests.13-16 Even kids from middle class families fall short on measures of health and well-being compared with children whose families are more affluent. What’s more, being poor in early childhood appears to have lasting effects. Regardless of social or economic status or individual behavior later in life, studies suggest that the stress of poverty in the early years is associated with chronic illness and disability in adulthood.13-16
The bottom line, according to the Robert Wood Johnson Commission to Build a Healthier America: “For the first time in our history, the United States is raising a generation of children who may live sicker, shorter lives than their parents.”13 Hunger, or the lack of an adequate supply of nutritious food, is a key factor.17
Hunger hits home
In an op-ed in the San Francisco Chronicle, family physician Laura Gottlieb told the story of an 8-year-old boy whose family she’d known for years. Brought to her office because of abdominal pain, the boy underwent multiple tests, including urine and stool examinations, blood work, and imaging studies. As soon as one test came back, Dr. Gottlieb ordered another. All were negative, and no cause for GI distress was found.18
Only later did she discover that hunger was the source of the pain. “It had never even occurred to me to ask his mother about how much food there was in the house,” Dr. Gottlieb wrote.18
In a similar vein, CBS News recently ran a story about a high school football team that seemed to be down on its luck. Besides being on a losing streak, many of the players were lethargic. Eventually, an astute coach realized that a mental pickup wasn’t what the team members needed—nutrition was. In this impoverished Burke County, Georgia school, about 85% of the student body qualify for in-school breakfast and lunch. But for many kids, those 2 meals were all they had to eat.19
With the help of a school nutritionist and the federal Healthy Hunger-Free Kids Act, hundreds of students now receive dinner, too. And last season, in late 2011, the properly fueled team members went on to win the state championship.19
Who is “food insecure”? In 2010, the latest year for which figures are available, 14.5% of US households (representing a total of 48.8 million people) were “food insecure,” as the problem of having too little to eat is officially known.20 Most of these families managed without substantially disrupting their normal eating patterns or reducing their intake, the US Department of Agriculture reports. This was accomplished by cutting back on the variety of foods they ate, getting federal food assistance, or getting food from food banks, among other coping strategies. But for 6.4 million households, the problem was severe enough to disrupt normal eating patterns and cause those affected to eat less than usual at least part of the time in the course of the year.20
Here, too, the toll on children is especially high. Twenty percent of households with children face food insecurity, nearly twice the rate of childless households.20 In a child’s earliest years, too little energy, protein, and other nutrients can result in long-lasting deficits in social, cognitive, and emotional development; malnutrition and deficiencies in vitamins and minerals may even result in brain impairment.18 In addition, school-age children who don’t have enough to eat have more behavioral problems and are more likely than those who are not struggling with hunger to be in special education classes.17
The hunger and obesity link
Ironically, hunger is also associated with obesity. High calorie, high carbohydrate foods like pasta and bread typically cost considerably less than nutrient-rich low-carb foods like cheese, fruit, fish, and vegetables, and are more filling. And in poor neighborhoods, food that is high in carbohydrates and low in protein and other nutrients tends to be more available than fresh, healthy—and more perishable—food.21
What’s more, people living in poverty may find it especially difficult to exercise. In many neighborhoods, exercising outdoors can be dangerous, gyms are unaffordable, and safe parks and playgrounds may be few and far between.21
Identifying poor and hungry patients
In a survey conducted by the Childhood Hunger Initiative of Oregon, most of the nearly 200 physicians and nurse practitioners who responded expressed a desire to learn more about the consequences of hunger and how to address them. Besides being uncomfortable broaching the subject of hunger and other poverty-related issues, the providers cited time constraints as a barrier to doing so.22
Ask this question
Citing similar obstacles, Canadian researchers conducted a pilot study in search of an easy-to-use, evidence-based “case-finding” tool. They offered questionnaires to patients at 4 clinics in British Columbia to determine which questions had the highest likelihood of determining whether an individual was struggling with hunger, poverty, or homelessness. Participants, which included patients above (n=94) and below (n=51) the poverty line, were also asked how they felt about being asked such questions.23
One particular question—“Do you (ever) have difficulty making ends meet at the end of the month?”—proved to be the best predictor of poverty. Although 2 additional questions about food and housing were identified as suitable for a 3-item screening tool, this single question alone had 98% sensitivity and 60% specificity (odds ratio, 32.3; 95% confidence interval, 5.4-191.5). Equally important, 85% of study participants with income below the poverty level thought that poverty screening was important, and 67% said they felt comfortable talking to their family physician about it.23
Take this course
In response to the results of the provider survey conducted by the Childhood Hunger Initiative of Oregon, a team at the Oregon State University Extension Service developed an online training program. The free 5-module course, available at http://oregonstate.edu/instruct/dce/chi/modules.html, addresses the impact of childhood hunger and provides screening and intervention tips.24
A recommended strategy is to incorporate a question related to hunger and food insecurity into the medical history or physical assessment. Noting that you’ll learn more by asking whether a family has sufficient resources to provide a healthy diet than by simply inquiring about a balanced diet, a narrator uses this wording:
“In the past month, was there any day when you or anyone in your family went hungry because you didn’t have enough money for food?”24
What you can do to help needy patients
Some patients who are out of work, uninsured, and barely able to pay for food and shelter will simply put off doctor visits—or come in only after their condition is so dire that you have no recourse but to send them to the emergency department (ED). The result, of course, is just the opposite of what they had hoped for. They end up with a much larger bill—or, if they have coverage, with a much bigger copay—not to mention a far more serious condition than they would likely have had if they’d come in sooner.
Here are some ways you can help.
Discuss costs with uninsured patients. To encourage uninsured patients to come in before their condition worsens, make them aware of the comparatively low cost of a visit to your office vs that of, say, imaging studies, specialist visits, and lab tests, as well as ED costs. That’s one of the interventions recommended by Robert A. Forester, MD, and Richard J. Heck, MD, the authors of “What You Can Do to Help Your Uninsured Patients.”25 Consider offering discounts to low-income patients (within the bounds of Medicare and other insurance provisions), they also suggest.
Use fewer diagnostic tests. Ordering a battery of tests when a diagnosis is not readily apparent is a “cost-insensitive” way to practice medicine, authors Forester and Heck observe. Spending additional time with such patients, using your cognitive and diagnostic skills and performing a complete history and physical, frequently results in a diagnosis and treatment plan, they note.25 If patients are aware that you’re trying to minimize costs, they’ll often consent to a step-by-step diagnostic work-up that can be stopped at any time it is appropriate.
Do it yourself. Expand your practice to include a variety of minor procedures, such as removal or biopsy of common skin lesions, colposcopy, or setting simple fractures. These measures can help keep costs down to better serve poor and low-income patients. The American Academy of Family Physicians offers courses and training in various procedures that family physicians can competently perform in their own offices.
Request a courtesy consult. On occasion, you may be able to avoid a costly referral by calling a colleague and asking for a courtesy consult. The specialist will often tell you how he or she would handle a clinical presentation like the one you describe and suggest you try a similar approach, suggests Doug Campos-Outcalt, MD, MPA. Dr. Campos-Outcalt, a faculty member at the University of Arizona College of Medicine and the author of JFP’s bimonthly Practice Alert column, has extensive experience working with underserved communities.
Connect patients with community services. Poor patients typically have many social and psychological needs, as well as the need for medical care, and integrated care is particularly important for those facing hunger, homelessness, and chronic illness, says Jonathan Cartsonis, MD, medical director of Healthcare for the Homeless in Phoenix. Maintain contact with hospital social services and emergency psychiatric services, and have information—and handouts—about local food banks, homeless shelters, and community clinics, among other resources. (See the resources listed in the box.)
Feeding America Food Bank Locator
http://feedingamerica.org/foodbank-results.aspx
Insure Kids Now
http://www.insurekidsnow.gov/state/index.html/
National Association of Free and Charitable Clinics
http://www.freemedicalcamps.com
Nutrition Standards for School Meals (Healthy, Hunger-Free Kids Act)
http://www.fns.usda.gov/cnd/Governance/Legislation/nutritionstandards.htm
Partnership for Prescription Assistance
www.pparx.org
Rx Outreach
http://rxoutreach.com/
SNAP (Supplemental Nutrition Assistance Program)
http://www.fns.usda.gov/snap/applicant_recipients/eligibility.htm#income
WIC (Supplemental Nutrition Program for Women, Infants and Children)
http://stars.fns.usda.gov/wps/pages/start.jsf
In Seattle, for example, “Project Access” is an organization that helps give the underserved access to specialists. And in many parts of the country, local Rotary clubs sponsor free clinics staffed with volunteer and retired physicians, working cooperatively with local pharmacies to provide at-cost generic drugs.
Keep drug costs down
Physicians can help to insulate their poor and low-income patients from high drug costs in a number of ways:
Reduce polypharmacy. Half of Americans take at least one prescription drug, according to the 2011 Consumer Reports survey. Among this group, people with limited income—those earning less than $40,000—take, on average, 5.7 different drugs.10 Eliminating unnecessary medications, including supplements, herbs, and any other over-the-counter products, can lead to substantial savings. To determine what can be eliminated, ask patients to bring in everything they’re taking and conduct a brown bag medication review. To learn more, see “Help your patient ‘get’ what you just said: A health literacy guide” (J Fam Pract. 2012;61:190-196).
Prescribe generics. Newer brand-name drugs may not be markedly better than older, established agents. And many generics are available at major retailers like Wal-Mart for just a few dollars for a 30-day supply or at CVS for $9.99 for a 3-month supply.26 Yet some physicians routinely order newer medications, even for indigent patients.
Be upfront about drug costs. When you prescribe a new drug, whether generic or branded, it is important to discuss the cost (easily accessible online and in many electronic medical record systems) with the patient. Yet only 5% of respondents to the 2011 Consumer Reports survey said their health care providers had done so. Two-thirds of those surveyed (64%) did not discover the cost of a drug until they went to a pharmacy to pick it up.10
Think twice before handing out samples. Drug samples would appear to benefit the poor and the uninsured, but evidence suggests otherwise.27,28 In a study that assessed out-of-pocket costs associated with the use of samples, patients who had never received samples had lower out-of-pocket costs.28 That’s partly because most samples are newer, more expensive drugs, and patients who start taking them are often unable to afford the cost of a prescription. Another study found that the use of generic drugs for uninsured patients rose (from 12% to 30%) after the clinic discontinued the use of samples.27
CORRESPONDENCE Laura C. Lippman, MD, 2311 North 45th Street, No. 171, Seattle, WA 98103; lclippman@gmail.com
Late last year, news outlets nationwide confirmed what many had long suspected: America’s middle class is shrinking. The latest data from the US Census Bureau found that nearly half (48%) of Americans are poor or low income.1,2
That means 46.2 million people—more than 15% of US citizens—are living below the federal poverty level (FPL), which is $23,050 for a family of 4. Another 97.3 million (about 33%) meet the criterion for low income—earning between $23,050 and $45,869 for a family of 4.1,2 These numbers are based on the Census Bureau’s new supplemental poverty measure, which considers costs like medical and housing and benefits such as food stamps in calculating poverty.3
The way that census data are analyzed is a key consideration for policy makers and legislators. For primary care physicians, the findings simply serve as a critical reminder that millions of Americans—including some of your patients—are struggling to stay afloat.
In some cases, the problems patients face will be so severe that there won’t be much you can do about them. In others, there are steps you can take to lend a helping hand (TABLE).
TABLE
Help the poor and uninsured: 9 things you can do
|
Death by poverty?
That’s the title of a summary of a recent study, posted on the Web site of Columbia University’s Mailman School of Public Health.4 The researchers found that poverty, low levels of education, and a lack of social support, among other “social” factors, account for as many deaths as heart attack, stroke, and lung cancer.5
A related study, also by researchers at Columbia, attempted to quantify the health impact of some leading medical and nonmedical factors. Their findings: The detrimental effects of poverty, smoking, and being a high school dropout exceed those of binge drinking, being overweight or obese, and being uninsured.6 The average low-income individual loses 8.2 years of good health simply because of his or her economic status, the lead researcher reported. In contrast, the average loss associated with obesity is 4.2 years and 6.6 years with smoking. The overall health of the US population won’t improve until poverty rates are reduced and educational deficits are addressed, the lead researcher concluded.7
That’s not to negate the importance of health coverage, however: A Kaiser Family Foundation study of low-income adults found that fully half (51%) of those who lacked health insurance had not gone to a doctor or clinic in the previous 12 months—and 69% had received no preventive care in the course of the year.8
Another survey, completed in 2007, asked adults younger than 65 about their use of medication. About 1 in 7 (13.9%) said they had failed to fill a prescription in the previous year because they couldn’t afford it. Four years earlier, 10.3% had done so.9
Recently, however, the situation appears to have gotten even worse. In a 2011 Consumer Reports survey, just under half of adults taking prescription medication reported that they had cut costs by engaging in what the surveyors described as “risky health care tradeoffs”—eg, not filling a prescription, skipping doses, or taking an expired medication.10
Poverty in childhood has long-lasting effects
Children may be less likely than adults to require prescription drugs, but they are typically the hardest hit by poverty—both in numbers and long-term effects. The poverty rate for those younger than 18 is 22%, according to the National Center for Children in Poverty.11 For kids under the age of 5, it’s more than 25%.12
Children of poor, uneducated parents have worse health and die earlier than those whose families are wealthier and better educated, research suggests.13-16 Even kids from middle class families fall short on measures of health and well-being compared with children whose families are more affluent. What’s more, being poor in early childhood appears to have lasting effects. Regardless of social or economic status or individual behavior later in life, studies suggest that the stress of poverty in the early years is associated with chronic illness and disability in adulthood.13-16
The bottom line, according to the Robert Wood Johnson Commission to Build a Healthier America: “For the first time in our history, the United States is raising a generation of children who may live sicker, shorter lives than their parents.”13 Hunger, or the lack of an adequate supply of nutritious food, is a key factor.17
Hunger hits home
In an op-ed in the San Francisco Chronicle, family physician Laura Gottlieb told the story of an 8-year-old boy whose family she’d known for years. Brought to her office because of abdominal pain, the boy underwent multiple tests, including urine and stool examinations, blood work, and imaging studies. As soon as one test came back, Dr. Gottlieb ordered another. All were negative, and no cause for GI distress was found.18
Only later did she discover that hunger was the source of the pain. “It had never even occurred to me to ask his mother about how much food there was in the house,” Dr. Gottlieb wrote.18
In a similar vein, CBS News recently ran a story about a high school football team that seemed to be down on its luck. Besides being on a losing streak, many of the players were lethargic. Eventually, an astute coach realized that a mental pickup wasn’t what the team members needed—nutrition was. In this impoverished Burke County, Georgia school, about 85% of the student body qualify for in-school breakfast and lunch. But for many kids, those 2 meals were all they had to eat.19
With the help of a school nutritionist and the federal Healthy Hunger-Free Kids Act, hundreds of students now receive dinner, too. And last season, in late 2011, the properly fueled team members went on to win the state championship.19
Who is “food insecure”? In 2010, the latest year for which figures are available, 14.5% of US households (representing a total of 48.8 million people) were “food insecure,” as the problem of having too little to eat is officially known.20 Most of these families managed without substantially disrupting their normal eating patterns or reducing their intake, the US Department of Agriculture reports. This was accomplished by cutting back on the variety of foods they ate, getting federal food assistance, or getting food from food banks, among other coping strategies. But for 6.4 million households, the problem was severe enough to disrupt normal eating patterns and cause those affected to eat less than usual at least part of the time in the course of the year.20
Here, too, the toll on children is especially high. Twenty percent of households with children face food insecurity, nearly twice the rate of childless households.20 In a child’s earliest years, too little energy, protein, and other nutrients can result in long-lasting deficits in social, cognitive, and emotional development; malnutrition and deficiencies in vitamins and minerals may even result in brain impairment.18 In addition, school-age children who don’t have enough to eat have more behavioral problems and are more likely than those who are not struggling with hunger to be in special education classes.17
The hunger and obesity link
Ironically, hunger is also associated with obesity. High calorie, high carbohydrate foods like pasta and bread typically cost considerably less than nutrient-rich low-carb foods like cheese, fruit, fish, and vegetables, and are more filling. And in poor neighborhoods, food that is high in carbohydrates and low in protein and other nutrients tends to be more available than fresh, healthy—and more perishable—food.21
What’s more, people living in poverty may find it especially difficult to exercise. In many neighborhoods, exercising outdoors can be dangerous, gyms are unaffordable, and safe parks and playgrounds may be few and far between.21
Identifying poor and hungry patients
In a survey conducted by the Childhood Hunger Initiative of Oregon, most of the nearly 200 physicians and nurse practitioners who responded expressed a desire to learn more about the consequences of hunger and how to address them. Besides being uncomfortable broaching the subject of hunger and other poverty-related issues, the providers cited time constraints as a barrier to doing so.22
Ask this question
Citing similar obstacles, Canadian researchers conducted a pilot study in search of an easy-to-use, evidence-based “case-finding” tool. They offered questionnaires to patients at 4 clinics in British Columbia to determine which questions had the highest likelihood of determining whether an individual was struggling with hunger, poverty, or homelessness. Participants, which included patients above (n=94) and below (n=51) the poverty line, were also asked how they felt about being asked such questions.23
One particular question—“Do you (ever) have difficulty making ends meet at the end of the month?”—proved to be the best predictor of poverty. Although 2 additional questions about food and housing were identified as suitable for a 3-item screening tool, this single question alone had 98% sensitivity and 60% specificity (odds ratio, 32.3; 95% confidence interval, 5.4-191.5). Equally important, 85% of study participants with income below the poverty level thought that poverty screening was important, and 67% said they felt comfortable talking to their family physician about it.23
Take this course
In response to the results of the provider survey conducted by the Childhood Hunger Initiative of Oregon, a team at the Oregon State University Extension Service developed an online training program. The free 5-module course, available at http://oregonstate.edu/instruct/dce/chi/modules.html, addresses the impact of childhood hunger and provides screening and intervention tips.24
A recommended strategy is to incorporate a question related to hunger and food insecurity into the medical history or physical assessment. Noting that you’ll learn more by asking whether a family has sufficient resources to provide a healthy diet than by simply inquiring about a balanced diet, a narrator uses this wording:
“In the past month, was there any day when you or anyone in your family went hungry because you didn’t have enough money for food?”24
What you can do to help needy patients
Some patients who are out of work, uninsured, and barely able to pay for food and shelter will simply put off doctor visits—or come in only after their condition is so dire that you have no recourse but to send them to the emergency department (ED). The result, of course, is just the opposite of what they had hoped for. They end up with a much larger bill—or, if they have coverage, with a much bigger copay—not to mention a far more serious condition than they would likely have had if they’d come in sooner.
Here are some ways you can help.
Discuss costs with uninsured patients. To encourage uninsured patients to come in before their condition worsens, make them aware of the comparatively low cost of a visit to your office vs that of, say, imaging studies, specialist visits, and lab tests, as well as ED costs. That’s one of the interventions recommended by Robert A. Forester, MD, and Richard J. Heck, MD, the authors of “What You Can Do to Help Your Uninsured Patients.”25 Consider offering discounts to low-income patients (within the bounds of Medicare and other insurance provisions), they also suggest.
Use fewer diagnostic tests. Ordering a battery of tests when a diagnosis is not readily apparent is a “cost-insensitive” way to practice medicine, authors Forester and Heck observe. Spending additional time with such patients, using your cognitive and diagnostic skills and performing a complete history and physical, frequently results in a diagnosis and treatment plan, they note.25 If patients are aware that you’re trying to minimize costs, they’ll often consent to a step-by-step diagnostic work-up that can be stopped at any time it is appropriate.
Do it yourself. Expand your practice to include a variety of minor procedures, such as removal or biopsy of common skin lesions, colposcopy, or setting simple fractures. These measures can help keep costs down to better serve poor and low-income patients. The American Academy of Family Physicians offers courses and training in various procedures that family physicians can competently perform in their own offices.
Request a courtesy consult. On occasion, you may be able to avoid a costly referral by calling a colleague and asking for a courtesy consult. The specialist will often tell you how he or she would handle a clinical presentation like the one you describe and suggest you try a similar approach, suggests Doug Campos-Outcalt, MD, MPA. Dr. Campos-Outcalt, a faculty member at the University of Arizona College of Medicine and the author of JFP’s bimonthly Practice Alert column, has extensive experience working with underserved communities.
Connect patients with community services. Poor patients typically have many social and psychological needs, as well as the need for medical care, and integrated care is particularly important for those facing hunger, homelessness, and chronic illness, says Jonathan Cartsonis, MD, medical director of Healthcare for the Homeless in Phoenix. Maintain contact with hospital social services and emergency psychiatric services, and have information—and handouts—about local food banks, homeless shelters, and community clinics, among other resources. (See the resources listed in the box.)
Feeding America Food Bank Locator
http://feedingamerica.org/foodbank-results.aspx
Insure Kids Now
http://www.insurekidsnow.gov/state/index.html/
National Association of Free and Charitable Clinics
http://www.freemedicalcamps.com
Nutrition Standards for School Meals (Healthy, Hunger-Free Kids Act)
http://www.fns.usda.gov/cnd/Governance/Legislation/nutritionstandards.htm
Partnership for Prescription Assistance
www.pparx.org
Rx Outreach
http://rxoutreach.com/
SNAP (Supplemental Nutrition Assistance Program)
http://www.fns.usda.gov/snap/applicant_recipients/eligibility.htm#income
WIC (Supplemental Nutrition Program for Women, Infants and Children)
http://stars.fns.usda.gov/wps/pages/start.jsf
In Seattle, for example, “Project Access” is an organization that helps give the underserved access to specialists. And in many parts of the country, local Rotary clubs sponsor free clinics staffed with volunteer and retired physicians, working cooperatively with local pharmacies to provide at-cost generic drugs.
Keep drug costs down
Physicians can help to insulate their poor and low-income patients from high drug costs in a number of ways:
Reduce polypharmacy. Half of Americans take at least one prescription drug, according to the 2011 Consumer Reports survey. Among this group, people with limited income—those earning less than $40,000—take, on average, 5.7 different drugs.10 Eliminating unnecessary medications, including supplements, herbs, and any other over-the-counter products, can lead to substantial savings. To determine what can be eliminated, ask patients to bring in everything they’re taking and conduct a brown bag medication review. To learn more, see “Help your patient ‘get’ what you just said: A health literacy guide” (J Fam Pract. 2012;61:190-196).
Prescribe generics. Newer brand-name drugs may not be markedly better than older, established agents. And many generics are available at major retailers like Wal-Mart for just a few dollars for a 30-day supply or at CVS for $9.99 for a 3-month supply.26 Yet some physicians routinely order newer medications, even for indigent patients.
Be upfront about drug costs. When you prescribe a new drug, whether generic or branded, it is important to discuss the cost (easily accessible online and in many electronic medical record systems) with the patient. Yet only 5% of respondents to the 2011 Consumer Reports survey said their health care providers had done so. Two-thirds of those surveyed (64%) did not discover the cost of a drug until they went to a pharmacy to pick it up.10
Think twice before handing out samples. Drug samples would appear to benefit the poor and the uninsured, but evidence suggests otherwise.27,28 In a study that assessed out-of-pocket costs associated with the use of samples, patients who had never received samples had lower out-of-pocket costs.28 That’s partly because most samples are newer, more expensive drugs, and patients who start taking them are often unable to afford the cost of a prescription. Another study found that the use of generic drugs for uninsured patients rose (from 12% to 30%) after the clinic discontinued the use of samples.27
CORRESPONDENCE Laura C. Lippman, MD, 2311 North 45th Street, No. 171, Seattle, WA 98103; lclippman@gmail.com
1. Tavernise S, Gebeloff R. New way to tally poor recasts view of poverty. New York Times. November 7, 2011. Available at: http://www.nytimes.com/2011/11/08/us/poverty-gets-new-measure-at-census-bureau.html?_r=2&scp=1&sq=poverty&st=cse. Accessed March 12, 2012.
2. Income poverty and health insurance coverage in the United States: 2010 [press release]. Washington, DC: US Census Bureau; September 13, 2011. Available at: http://www.census.gov/newsroom/releases/archives/income_wealth/cb11-157.html. Accessed March 12, 2012.
3. Short K. The research supplemental poverty measure: 2010. Washington, DC: US Census Bureau; November 2011. Available at: http://www.census.gov/hhes/povmeas/methodology/supplemental/research/Short_ResearchSPM2010.pdf. Accessed March 13, 2012.
4. University Mailman School of Public Health. Death by poverty? June 16, 2011. Available at: http://www.mailman.columbia.edu/academic-departments/epidemiology/research-service/death-poverty. Accessed March 5, 2012.
5. Galea S, Tracy M, Hoggatt KJ, et al. Estimated deaths attributable to social factors in the United States. Am J Public Health. 2011;101:1456-1465
6. Muennig P, Fiscella K, Tancredi D, et al. The relative health burden of selected social and behavioral risk factors in the United States: implications for policy. Am J Public Health. 2010;100:1758-1764.
7. Columbia University Mailman School of Public Health. Poor face greater health burden than smokers or the obese. Available at: http://www.mailman.columbia.edu/academic-departments/health-policy/news-events/poor-face-greater-health-burden-smokers-or-obese. Accessed March 13, 2012.
8. Schwartz K. How trends in the health care system affect low-income adults: identifying access problems and financial burdens. December 21, 2007. Kaiser Family Foundation. Available at: http://www.kff.org/uninsured/7705.cfm. Accessed March 2, 2012.
9. Felland LE, Reschovsky JD. More nonelderly Americans face problems affording prescription drugs. Tracking report no. 22. January 2009. Center for Studying Health System Change. Available at: http://www.hschange.com/CONTENT/1039/. Accessed January 25, 2012.
10. Consumer Reports poll: 48 percent of Americans on meds making risky health care tradeoffs [press release]. Yonkers, NY: Consumer Reports; September 27, 2011. Available at: http://www.prnewswire.com/news-releases/consumer-reports-poll—48-percent-of-americans-on-meds-making-risky-health-care-tradeoffs-130618778.html. Accessed January 3, 2012.
11. A job-loss recovery hurts children most: statistics tell an alarming story [press release] New York, NY: National Center for Children in Poverty; September 15, 2011. Available at: http://www.nccp.org/media/releases/release_135.html. Accessed January 24, 2012.
12. Child Trends Data Bank. Children in poverty. Updated September 2011. Available at: http://www.childtrendsdatabank.org/?q=node/221. Accessed March 13, 2012.
13. Robert Wood Johnson Foundation. Overcoming obstacles to health. Princeton, NJ: RWJF Commission to Build a Healthier America; February 2008. Available at: http://www.rwjf.org/files/research/obstaclestohealth.pdf. Accessed March 22, 2012.
14. Shonkoff JP, Garner AS. Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129:e232-e246.
15. Stein DJ, Scott K, Haro Abad JM, et al. Early childhood adversity and later hypertension: data from the World Mental Health Survey. Ann Clin Psychiatry. 2010;22:19-28.
16. O’Rand AM, Hamil-Luker J. Processes of cumulative adversity: childhood disadvantage and increased risk of heart attack across the life course. J Gerontol B Psychol Sci Soc Sci. 2005;60(spec no 2):117-124.
17. American Psychological Association. Effects of poverty, hunger, and homelessness on children and youth. Available at: http://www.apa.org/pi/families/poverty.aspx. Accessed November 29, 2011.
18. Gottlieb L. Funding healthy society helps cure health care. San Francisco Chronicle. August 23, 2010:A-8.
19. Doane S. High school football team battles malnutrition. December 20, 2011. CBS News. Available at: http://www.cbsnews.com/8301-18563_162-57345857/high-school-football-team-battles-malnutrition/. Accessed March 13, 2012.
20. US Department of Agriculture Economic Research Service. Food security in the United States: key statistics and graphics. Updated September 7, 2011. Available at: http://www.ers.usda.gov/Briefing/FoodSecurity/stats_graphs.htm. Accessed March 1, 2012.
21. Drewnowski A, Damon N. Food choices and diet costs: an economic analysis. J Nutr. 2005;135:900-904.
22. Survey helps doctors help hungry patients [press release]. Portland, Ore: Oregon State University Extension Service; May 27, 2008. Available at: http://extension.oregonstate.edu/news/release/2008/05/survey-helps-doctors-help-hungry-patients. Accessed February 29, 2012.
23. Brcic V, Eberdt C, Kaczorowski J. Development of a tool to identify poverty in a family practice setting: a pilot study. Int J Family Med. 2011;2011:812182.
24. Childhood food insecurity: health impacts, screening and intervention [course summary]. Corvallis, Ore: Oregon State University Extended Campus; 2010. Available at: http://oregonstate.edu/instruct/dce/chi/module5_8.html. Accessed March 13, 2012.
25. Forester RA, Heck RJ. What you can do to help your uninsured patients. Fam Pract Manag. 2009;16:21-24.
26. Byrd C. CVS drug prices takes on Wal-Mart’s generic drug prices—with a gimmicky twist. eDrugSearch. Available at: http://www.edrugsearch.com/edsblog/cvs-takes-on-wal-marts-generic-drug-prices-with-a-gimmicky-twist/. Accessed March 13, 2012.
27. Miller DP, Mansfield RJ, Woods JB, et al. The impact of drug samples on prescribing to the uninsured. South Med J. 2008;101:888-893.
28. Chimonas S, Kassirer JP. No more free drug samples? PLoS Med. 2009;6:e1000074.
1. Tavernise S, Gebeloff R. New way to tally poor recasts view of poverty. New York Times. November 7, 2011. Available at: http://www.nytimes.com/2011/11/08/us/poverty-gets-new-measure-at-census-bureau.html?_r=2&scp=1&sq=poverty&st=cse. Accessed March 12, 2012.
2. Income poverty and health insurance coverage in the United States: 2010 [press release]. Washington, DC: US Census Bureau; September 13, 2011. Available at: http://www.census.gov/newsroom/releases/archives/income_wealth/cb11-157.html. Accessed March 12, 2012.
3. Short K. The research supplemental poverty measure: 2010. Washington, DC: US Census Bureau; November 2011. Available at: http://www.census.gov/hhes/povmeas/methodology/supplemental/research/Short_ResearchSPM2010.pdf. Accessed March 13, 2012.
4. University Mailman School of Public Health. Death by poverty? June 16, 2011. Available at: http://www.mailman.columbia.edu/academic-departments/epidemiology/research-service/death-poverty. Accessed March 5, 2012.
5. Galea S, Tracy M, Hoggatt KJ, et al. Estimated deaths attributable to social factors in the United States. Am J Public Health. 2011;101:1456-1465
6. Muennig P, Fiscella K, Tancredi D, et al. The relative health burden of selected social and behavioral risk factors in the United States: implications for policy. Am J Public Health. 2010;100:1758-1764.
7. Columbia University Mailman School of Public Health. Poor face greater health burden than smokers or the obese. Available at: http://www.mailman.columbia.edu/academic-departments/health-policy/news-events/poor-face-greater-health-burden-smokers-or-obese. Accessed March 13, 2012.
8. Schwartz K. How trends in the health care system affect low-income adults: identifying access problems and financial burdens. December 21, 2007. Kaiser Family Foundation. Available at: http://www.kff.org/uninsured/7705.cfm. Accessed March 2, 2012.
9. Felland LE, Reschovsky JD. More nonelderly Americans face problems affording prescription drugs. Tracking report no. 22. January 2009. Center for Studying Health System Change. Available at: http://www.hschange.com/CONTENT/1039/. Accessed January 25, 2012.
10. Consumer Reports poll: 48 percent of Americans on meds making risky health care tradeoffs [press release]. Yonkers, NY: Consumer Reports; September 27, 2011. Available at: http://www.prnewswire.com/news-releases/consumer-reports-poll—48-percent-of-americans-on-meds-making-risky-health-care-tradeoffs-130618778.html. Accessed January 3, 2012.
11. A job-loss recovery hurts children most: statistics tell an alarming story [press release] New York, NY: National Center for Children in Poverty; September 15, 2011. Available at: http://www.nccp.org/media/releases/release_135.html. Accessed January 24, 2012.
12. Child Trends Data Bank. Children in poverty. Updated September 2011. Available at: http://www.childtrendsdatabank.org/?q=node/221. Accessed March 13, 2012.
13. Robert Wood Johnson Foundation. Overcoming obstacles to health. Princeton, NJ: RWJF Commission to Build a Healthier America; February 2008. Available at: http://www.rwjf.org/files/research/obstaclestohealth.pdf. Accessed March 22, 2012.
14. Shonkoff JP, Garner AS. Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129:e232-e246.
15. Stein DJ, Scott K, Haro Abad JM, et al. Early childhood adversity and later hypertension: data from the World Mental Health Survey. Ann Clin Psychiatry. 2010;22:19-28.
16. O’Rand AM, Hamil-Luker J. Processes of cumulative adversity: childhood disadvantage and increased risk of heart attack across the life course. J Gerontol B Psychol Sci Soc Sci. 2005;60(spec no 2):117-124.
17. American Psychological Association. Effects of poverty, hunger, and homelessness on children and youth. Available at: http://www.apa.org/pi/families/poverty.aspx. Accessed November 29, 2011.
18. Gottlieb L. Funding healthy society helps cure health care. San Francisco Chronicle. August 23, 2010:A-8.
19. Doane S. High school football team battles malnutrition. December 20, 2011. CBS News. Available at: http://www.cbsnews.com/8301-18563_162-57345857/high-school-football-team-battles-malnutrition/. Accessed March 13, 2012.
20. US Department of Agriculture Economic Research Service. Food security in the United States: key statistics and graphics. Updated September 7, 2011. Available at: http://www.ers.usda.gov/Briefing/FoodSecurity/stats_graphs.htm. Accessed March 1, 2012.
21. Drewnowski A, Damon N. Food choices and diet costs: an economic analysis. J Nutr. 2005;135:900-904.
22. Survey helps doctors help hungry patients [press release]. Portland, Ore: Oregon State University Extension Service; May 27, 2008. Available at: http://extension.oregonstate.edu/news/release/2008/05/survey-helps-doctors-help-hungry-patients. Accessed February 29, 2012.
23. Brcic V, Eberdt C, Kaczorowski J. Development of a tool to identify poverty in a family practice setting: a pilot study. Int J Family Med. 2011;2011:812182.
24. Childhood food insecurity: health impacts, screening and intervention [course summary]. Corvallis, Ore: Oregon State University Extended Campus; 2010. Available at: http://oregonstate.edu/instruct/dce/chi/module5_8.html. Accessed March 13, 2012.
25. Forester RA, Heck RJ. What you can do to help your uninsured patients. Fam Pract Manag. 2009;16:21-24.
26. Byrd C. CVS drug prices takes on Wal-Mart’s generic drug prices—with a gimmicky twist. eDrugSearch. Available at: http://www.edrugsearch.com/edsblog/cvs-takes-on-wal-marts-generic-drug-prices-with-a-gimmicky-twist/. Accessed March 13, 2012.
27. Miller DP, Mansfield RJ, Woods JB, et al. The impact of drug samples on prescribing to the uninsured. South Med J. 2008;101:888-893.
28. Chimonas S, Kassirer JP. No more free drug samples? PLoS Med. 2009;6:e1000074.
Patient dismissal: The right way to do it
• Unless a single incident irreparably damaged your relationship with a patient, exhaust all efforts at resolution before deciding on dismissal. C
• Establish policies that help you set limits on problem behavior—eg, drug-seeking or angry outbursts—while continuing to care for the patient. C
• When dismissal is unavoidable, inform the patient in writing that you will be available to handle medical emergencies until he or she has found another physician. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Susan L, a 53-year-old who’d been a patient of Dr. O’s for the past 6 years, received a bill for a visit that had occurred nearly 2 years earlier. She called the office and told the receptionist that she had never been billed for this visit and didn’t think she should have to pay after such a lengthy delay. When she received a past due notice, Susan called and asked to speak to the physician—and to schedule an appointment. She was told that she could do neither until her account was current.
Eventually, the unpaid bill was sent to a collection agency, and Susan received a letter threatening legal action. In response, she sent a letter of her own—certified, return receipt requested—detailing her reason for not paying and threatening to sue Dr. O for abandonment.*
*Adapted from actual cases, with details changed to protect the privacy of the parties involved.
With the national unemployment rate hovering at a record high, unpaid medical bills may be your most pressing problem—and potential grounds for patient dismissal. Judging from a recent survey in which primary care physicians identified nearly one patient in 5 as “difficult,"1 it’s unlikely that nonpayment is the only patient conundrum you face.
Indeed, there are many ways a patient can be difficult, including exhibiting habitual hostility, chronic drug-seeking behavior, or consistent noncompliance; breaking appointments at the last minute; or being a no-show. You may wish you could “fire” the worst off enders but be concerned about professional and ethical responsibilities and the legal risk you might face. Ironically, though, struggling to maintain a chronically stressed physician-patient relationship is often riskier than a well-timed termination.2
The key here, however, is the persistent or extreme nature of the difficulty.3 When a dismissal is prompted by a one-time occurrence or lower-level offense, what constitutes a reasonable response is not always clear-cut.
Under what circumstances is it appropriate to end your relationship with a patient? When you do terminate the relationship, what steps can you take to safeguard the patient and avoid charges of abandonment? Here’s a look at these questions—and some answers.
Professional responsibility: How far does it go?
As a physician, you’ve pledged to “do no harm.” And you’ve likely been taught—as it states in the American College of Physicians (ACP) ethics manual—that you have “a moral duty to care for all patients.” 4 The American Medical Association’s code of ethics cites a similar standard: the obligation to place patients’ welfare above your own interests.5
According to the ACP, the physician-patient relationship should be discontinued only under “exceptional circumstances."6 But not everyone agrees, not only on what constitutes “exceptional,” but on whether that is the correct threshold for termination.
A health care attorney writing in American Medical News, for example, takes a more liberal view. It’s time to dismiss, he asserts, when the doctor-patient relationship doesn’t work.7 By that standard, virtually any ongoing problem could be construed as evidence of an “irreparable breakdown” of the physician-patient relationship (TABLE).
TABLE
Key reasons to "fire" a patient
|
| Sources: Kodner C. FP Essentials. 2008.3 Harris S. Am Med News. 2008.7 |
We can work it out
Legally, a doctor can dismiss a patient for virtually any reason, or fail to give any explanation at all.2 Ethically, dismissal should be your last option, not your first choice.
In a home study course titled “Challenging physician-patient interactions,” the American Academy of Family Physicians (AAFP) advises doctors to be certain they have exhausted every reasonable effort to communicate, set achievable goals, and meet the patient’s needs.3 The steps you take to try to mend a damaged patient relationship, of course, will depend on what caused the rift in the first place. Here are some examples.
Nonpayment. You are not compelled (or expected) to indefinitely continue to treat a patient who’s unable—or unwilling—to pay you, of course. But if he or she is out of work and has fallen on hard times or has a single unpaid bill, discussing the problem and attempting to accommodate the patient’s financial limitations (and establish a realistic payment plan) is a reasonable approach.
Having a billing clerk handle most communications regarding unpaid bills may be a good idea. But when a situation escalates, as in the case of Susan L (CASE 1), foregoing a direct discussion and expecting a subordinate to handle an abrupt patient termination is not (ethically or legally) appropriate.7
Laura K, age 34, had always been a challenging patient. She suffered from a collection of pain-producing maladies, including migraines, fibromyalgia, and low back pain. Controlling her pain required increasing amounts of narcotics, sometimes in doses that exceeded therapeutic recommendations.
Recently she’d begun calling her primary care physician’s office for early refills; more than once, she claimed her prescription had been lost or stolen. When Laura called to report that the oxycodone prescribed 4 days ago had been stolen from her purse and to request a refill, the physician refused to speak with her—and instructed the receptionist to tell her she needed to find another physician.
Laura called several other local physicians, but none was able to see her. She then went to the emergency department. The ED physician evaluated her and offered her a prescription for a mild analgesic, but refused her request for oxycodone.
That night, Laura attempted suicide. Although she survived, she was left with significant neurologic deficits. She sued the physician who had refused to speak to her on a variety of counts of negligence, including a charge of abandonment.
At deposition, experts for the plaintiff testified that refusing to see and evaluate a current patient for her ongoing problems without giving substantial notice constituted abandonment—and was a substantial cause of Laura’s suicide attempt. On the advice of counsel, the physician agreed to a $150,000 settlement.
Drug-seeking. Behavior like that of Laura K (CASE 2), whose requests for narcotics and claims of lost pills or prescriptions occurred with increasing regularity, can’t be ignored. The AAFP course, which states that patients should not be dismissed “on the grounds of drug-seeking behaviors alone,"3 recommends that physicians develop policies for prescribing controlled substances and handling drug-seeking patients. Such a policy—which might include limits on the frequency of renewals and the duration of a single prescription, among other provisions—should be communicated to every patient who seeks opioid analgesics.3 The Federation of State Medical Boards recommends the use of a written agreement, spelling out your responsibilities as well as those of the patient, for individuals at high risk of abuse (http://www.fsmb.org/pdf/2004_grpol_Controlled_Substances.pdf).
While the existence of a policy or written contract may not alter the behavior of a drug-seeking patient, it can prevent you from being caught off -guard or reacting as rashly as Laura K’s physician did. Indeed, Laura’s doctor made 2 key missteps: acting without warning, and expecting a receptionist to deliver the dismissal message.
A better approach, from the AAFP’s perspective, is to calmly maintain the limits you’ve set, remind the patient that you want to help, and offer treatment alternatives, such as nonopioid analgesics.3 Discussions in response to drug-seeking behavior, of course, should always be delivered—and documented—by the physician.
Noncompliance. This is a particularly complex problem, as issues of patient autonomy and physician authority are involved. A case study presented in the AAFP home study course describes the thoughts and feelings of a physician who considered dismissing a pediatric patient because the child’s mother refused to allow him to be vaccinated. The physician ultimately decided to continue to treat the child, after determining that the physician-patient relationship could still be beneficial and planning to revisit the vaccination issue with the mother at a later date.3 (Another physician, faced with a similar issue, wrote a New York Times article about his decision to dismiss a young patient. His reasoning? Accepting the mother’s refusal to allow her son to get a tetanus booster would compromise “my conscience and my professional ethics. I couldn’t do that."8)
Although it is important to recognize the difference between noncompliance and an individual’s right to refuse recommended treatment,9 you, too, may encounter situations in which a patient’s, or parent’s, repeated failure—to follow an agreed-upon therapeutic regimen, perhaps, or adhere to a schedule of visits needed to manage a chronic condition— causes your relationship with the patient to deteriorate to a point where dismissal is warranted. Here, as with other potential causes of dismissal, the patient should be adequately warned, the discussion documented, and action taken only if nothing changes.
Anger. As is the case with drug-seeking, the AAFP course advises physicians to anticipate and develop policies for handling situations in which a patient’s anger escalates and creates a real or perceived threat.3 While this is commonly done in acute care facilities, it is often overlooked in outpatient settings.
Among the issues to address: equipping offices and exam rooms with an emergency call button or intercom, knowing where to position yourself to ensure that you can’t be trapped in a room by a threatening patient, and considering how to respond in a way that defuses—rather than escalates—the anger. Calmly ask the patient what he or she is upset about, listen carefully, and apologize, if appropriate, for your role in the upsetting incident. Then move on to the purpose of the visit, stating, for example, “Now, what brings you in today?” 3
It is crucial to set boundaries (although it’s probably not a good idea to attempt it at the time of the outburst), making it clear, for example, that profanity is not acceptable; directing anger at nurses or other staff members is not permitted; and what the consequences of continued outbursts will be. 3
A single incident that’s grounds for dismissal
Despite the emphasis on resolving problems with patients, there are times when dismissal can and should occur, with little warning and no negotiation. In its home study course, the AAFP describes this as a “sentinel incident"— a single occurrence so egregious that it damages the physician-patient relationship beyond repair.3
A threat of violence or a physical assault itself would rise to that level. Some other examples: a sexual assault or blatant sexual advance, falsifying medical records, and theft or another type of criminal activity carried out in the physician’s office.
When a sentinel incident occurs, the best course is likely to be to forego any attempt at resolution, call the police or your facility’s security officer, and, if appropriate, to immediately prepare to “fire” the patient.
Dismissal without abandonment: Here’s how
In the vast majority of cases, dismissing a patient does not in and of itself constitute patient abandonment. Even if the termination is unduly abrupt, as was the case for Susan (CASE 1) and Laura (CASE 2), it doesn’t constitute abandonment unless the patient is dismissed during a course of treatment and unable to find a physician to provide ongoing care.
Neither was true in Susan’s case, and her threat of a lawsuit based on charges of abandonment never came to fruition. Not so for Laura, who was abruptly terminated during ongoing treatment—and who nonetheless made numerous attempts to find another doctor to care for her, without success. The attorney for Laura’s physician advised that the severe consequences of dismissing without going through the proper channels made a trial defense untenable.
Although most charges of patient abandonment never rise to the level required for a successful lawsuit, attorneys often include it in a litany of charges in an attempt to damage the physician’s credibility with a jury. You can usually avoid that scenario by taking the right steps when you dismiss a patient.
CASE 3 Pregnant patient, rural physician
As part of his rural family medicine practice, Dr. J provided obstetrical care. Dr. J had a partner and they alternated call nights, but his partner did not do OB. Dr. J made it a point, however, to always be on call for his obstetrical patients as they neared delivery. Having no patients imminently due, he took a one-week vacation out of town.
One of his patients went into premature labor and went to the local hospital. Dr. J’s partner was called to attend, but indicated he did not do OB work and advised the emergency physician to call “any obstetrician around.” One obstetrical group covered the region and the on-call physician was at another hospital doing a C-section and requested that the patient be transferred to that hospital for evaluation. After a series of delays, the patient was transferred and delivered a preterm infant who showed signs of neurological injury after a lengthy ICU stay.
The family sued all providers involved on several grounds, including patient abandonment. Plaintiff experts testified that the standard of care would be for Dr. J to be in attendance for such emergencies or, failing that, to provide for adequate coverage of his pregnant patient. They also testified that it was reasonable for the patient to have gone to the local hospital where her delivery was planned and that Dr. J should have arranged for the local OB group to provide emergency coverage. The case concluded with an $800,000 pretrial settlement.
Ensure that dismissal is an option
While we’ve already established that physicians have the legal right to dismiss patients, regardless of the reason, there are instances that make it far more difficult—and legally risky—to do so.
A primary care physician in a rural area is a case in point (CASE 3). If you are the only doctor in the area and the patient has no viable means of getting care from another provider, you may want to reconsider the dismissal. It is far easier to establish that a patient in such an underserved area was abandoned, even— as Dr. J found out—for failing to ensure full coverage during a vacation or leave of absence.
Rural physicians can help prevent charges of abandonment by advising patients of the special call challenges a rural setting presents. Doctors should make sure their patients know what to do if an emergency occurs when the practice is closed or a physician is out of town, and document the discussion in the medical record.
A physician in a staff-model HMO may face similar problems. Unless the HMO has another outpatient clinic in the vicinity, dismissal could leave the patient with no means of receiving affordable health care.
Options in such a case might include asking a colleague at the same clinic to accept a patient whom you would like to dismiss or finding a way to manage the patient’s behavior. If a patient has been excessively angry or threatening in the past, for example, it is often advisable to sit down with the patient (with security nearby) to discuss the parameters of expected behavior and develop a contract for future care. The contract might include a requirement that the patient call in advance so that security can be present when he or she arrives, for example, or that the patient agree to abstain from profanity and threats.
Know the laws in your state. Before you terminate a patient, check with your state medical board or local medical society to make sure your actions will be in compliance with any relevant state rules and regulations.
When you dismiss, cover all bases
Send a letter to the patient by certified mail, return receipt requested, notifying him or her of the dismissal and agreeing to provide emergency care for a reasonable time—typically, 30 days—while the patient seeks another physician. It is advisable, too, to help the patient locate other potential clinicians—by, say, including contact information for your county medical society or the patient’s health insurer’s list of in-network providers, or referring an indigent patient to Medicaid or a sliding scale clinic. It is a good idea to offer to transfer records to the new physician, as well.
It is not mandatory to document the reason for the dismissal in the letter, but some sources recommend that you do so. If you’re uncertain how to proceed, check with legal counsel before you send the letter. (You can find sample dismissal letters at www.ttuhsc.edu/som/clinic/forms/ACForm8.11.A.pdf and in “Terminating a patient: Is it time to part ways?” at http://www.aafp.org/fpm/2005/0900/p34.html.)
The events that led up to the dismissal, however, including any discussions you had with the patient about them, must be documented in the medical record. Put a copy of the letter and the certified mail receipt in the chart, as well. JFP
CORRESPONDENCE John Davenport, MD, JD, 13 Redonda, Irvine, CA 92620; john.y.davenport@kp.org
1. Hinchey SA, Jackson JL. A cohort study assessing difficult patient encounters in a walk-in primary care clinic, predictors and outcomes. J Gen Intern Med. 2011;Jan 25 [Epub ahead of print].
2. Schleiter K. Difficult patient-physician relationships and the risk of medical malpractice litigation. Virtual Mentor. 2009;11:242-246.
3. Kodner C. Challenging physician-patient interactions. FP Essentials. ed 354. AAFP home study. Leawood, Kan: American Academy of Family Physicians; November 2008.
4. Snyder L, Leffler C. Ethics and Human Rights Committee American College of Physicians. Ethics manual: fifth ed. Ann Intern Med. 2005;142:560-582.
5. American Medical Association (AMA). Opinion 10.015. The patient-physician relationship. Code of Medical Ethics. Chicago, Ill: AMA. 2008. Available at: http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion10015.shtml. Accessed February 11, 2011.
6. American College of Physicians. Ethical considerations for the use of patient incentives to promote personal responsibility for health: West Virginia Medicaid and beyond [position paper]. Philadelphia: American College of Physicians; 2010.
7. Harris SM. Take care when firing a patient. Am Med News. February 4, 2008. Available at: http://www.ama-assn.org/amednews/2008/02/04/bica0204.htm. Accessed February 11, 2011.
8. Parikh RK. Showing the patient the door, permanently. New York Times. June 10, 2008. Available at: http://www.nytimes.com/2008/06/10/health/views/10case.html. Accessed February 15, 2011.
9. Summey-Lowman B. Patient non-compliance—a powerful legal defense. Healthcare Risk Manag. 2009;15:1-2.
• Unless a single incident irreparably damaged your relationship with a patient, exhaust all efforts at resolution before deciding on dismissal. C
• Establish policies that help you set limits on problem behavior—eg, drug-seeking or angry outbursts—while continuing to care for the patient. C
• When dismissal is unavoidable, inform the patient in writing that you will be available to handle medical emergencies until he or she has found another physician. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Susan L, a 53-year-old who’d been a patient of Dr. O’s for the past 6 years, received a bill for a visit that had occurred nearly 2 years earlier. She called the office and told the receptionist that she had never been billed for this visit and didn’t think she should have to pay after such a lengthy delay. When she received a past due notice, Susan called and asked to speak to the physician—and to schedule an appointment. She was told that she could do neither until her account was current.
Eventually, the unpaid bill was sent to a collection agency, and Susan received a letter threatening legal action. In response, she sent a letter of her own—certified, return receipt requested—detailing her reason for not paying and threatening to sue Dr. O for abandonment.*
*Adapted from actual cases, with details changed to protect the privacy of the parties involved.
With the national unemployment rate hovering at a record high, unpaid medical bills may be your most pressing problem—and potential grounds for patient dismissal. Judging from a recent survey in which primary care physicians identified nearly one patient in 5 as “difficult,"1 it’s unlikely that nonpayment is the only patient conundrum you face.
Indeed, there are many ways a patient can be difficult, including exhibiting habitual hostility, chronic drug-seeking behavior, or consistent noncompliance; breaking appointments at the last minute; or being a no-show. You may wish you could “fire” the worst off enders but be concerned about professional and ethical responsibilities and the legal risk you might face. Ironically, though, struggling to maintain a chronically stressed physician-patient relationship is often riskier than a well-timed termination.2
The key here, however, is the persistent or extreme nature of the difficulty.3 When a dismissal is prompted by a one-time occurrence or lower-level offense, what constitutes a reasonable response is not always clear-cut.
Under what circumstances is it appropriate to end your relationship with a patient? When you do terminate the relationship, what steps can you take to safeguard the patient and avoid charges of abandonment? Here’s a look at these questions—and some answers.
Professional responsibility: How far does it go?
As a physician, you’ve pledged to “do no harm.” And you’ve likely been taught—as it states in the American College of Physicians (ACP) ethics manual—that you have “a moral duty to care for all patients.” 4 The American Medical Association’s code of ethics cites a similar standard: the obligation to place patients’ welfare above your own interests.5
According to the ACP, the physician-patient relationship should be discontinued only under “exceptional circumstances."6 But not everyone agrees, not only on what constitutes “exceptional,” but on whether that is the correct threshold for termination.
A health care attorney writing in American Medical News, for example, takes a more liberal view. It’s time to dismiss, he asserts, when the doctor-patient relationship doesn’t work.7 By that standard, virtually any ongoing problem could be construed as evidence of an “irreparable breakdown” of the physician-patient relationship (TABLE).
TABLE
Key reasons to "fire" a patient
|
| Sources: Kodner C. FP Essentials. 2008.3 Harris S. Am Med News. 2008.7 |
We can work it out
Legally, a doctor can dismiss a patient for virtually any reason, or fail to give any explanation at all.2 Ethically, dismissal should be your last option, not your first choice.
In a home study course titled “Challenging physician-patient interactions,” the American Academy of Family Physicians (AAFP) advises doctors to be certain they have exhausted every reasonable effort to communicate, set achievable goals, and meet the patient’s needs.3 The steps you take to try to mend a damaged patient relationship, of course, will depend on what caused the rift in the first place. Here are some examples.
Nonpayment. You are not compelled (or expected) to indefinitely continue to treat a patient who’s unable—or unwilling—to pay you, of course. But if he or she is out of work and has fallen on hard times or has a single unpaid bill, discussing the problem and attempting to accommodate the patient’s financial limitations (and establish a realistic payment plan) is a reasonable approach.
Having a billing clerk handle most communications regarding unpaid bills may be a good idea. But when a situation escalates, as in the case of Susan L (CASE 1), foregoing a direct discussion and expecting a subordinate to handle an abrupt patient termination is not (ethically or legally) appropriate.7
Laura K, age 34, had always been a challenging patient. She suffered from a collection of pain-producing maladies, including migraines, fibromyalgia, and low back pain. Controlling her pain required increasing amounts of narcotics, sometimes in doses that exceeded therapeutic recommendations.
Recently she’d begun calling her primary care physician’s office for early refills; more than once, she claimed her prescription had been lost or stolen. When Laura called to report that the oxycodone prescribed 4 days ago had been stolen from her purse and to request a refill, the physician refused to speak with her—and instructed the receptionist to tell her she needed to find another physician.
Laura called several other local physicians, but none was able to see her. She then went to the emergency department. The ED physician evaluated her and offered her a prescription for a mild analgesic, but refused her request for oxycodone.
That night, Laura attempted suicide. Although she survived, she was left with significant neurologic deficits. She sued the physician who had refused to speak to her on a variety of counts of negligence, including a charge of abandonment.
At deposition, experts for the plaintiff testified that refusing to see and evaluate a current patient for her ongoing problems without giving substantial notice constituted abandonment—and was a substantial cause of Laura’s suicide attempt. On the advice of counsel, the physician agreed to a $150,000 settlement.
Drug-seeking. Behavior like that of Laura K (CASE 2), whose requests for narcotics and claims of lost pills or prescriptions occurred with increasing regularity, can’t be ignored. The AAFP course, which states that patients should not be dismissed “on the grounds of drug-seeking behaviors alone,"3 recommends that physicians develop policies for prescribing controlled substances and handling drug-seeking patients. Such a policy—which might include limits on the frequency of renewals and the duration of a single prescription, among other provisions—should be communicated to every patient who seeks opioid analgesics.3 The Federation of State Medical Boards recommends the use of a written agreement, spelling out your responsibilities as well as those of the patient, for individuals at high risk of abuse (http://www.fsmb.org/pdf/2004_grpol_Controlled_Substances.pdf).
While the existence of a policy or written contract may not alter the behavior of a drug-seeking patient, it can prevent you from being caught off -guard or reacting as rashly as Laura K’s physician did. Indeed, Laura’s doctor made 2 key missteps: acting without warning, and expecting a receptionist to deliver the dismissal message.
A better approach, from the AAFP’s perspective, is to calmly maintain the limits you’ve set, remind the patient that you want to help, and offer treatment alternatives, such as nonopioid analgesics.3 Discussions in response to drug-seeking behavior, of course, should always be delivered—and documented—by the physician.
Noncompliance. This is a particularly complex problem, as issues of patient autonomy and physician authority are involved. A case study presented in the AAFP home study course describes the thoughts and feelings of a physician who considered dismissing a pediatric patient because the child’s mother refused to allow him to be vaccinated. The physician ultimately decided to continue to treat the child, after determining that the physician-patient relationship could still be beneficial and planning to revisit the vaccination issue with the mother at a later date.3 (Another physician, faced with a similar issue, wrote a New York Times article about his decision to dismiss a young patient. His reasoning? Accepting the mother’s refusal to allow her son to get a tetanus booster would compromise “my conscience and my professional ethics. I couldn’t do that."8)
Although it is important to recognize the difference between noncompliance and an individual’s right to refuse recommended treatment,9 you, too, may encounter situations in which a patient’s, or parent’s, repeated failure—to follow an agreed-upon therapeutic regimen, perhaps, or adhere to a schedule of visits needed to manage a chronic condition— causes your relationship with the patient to deteriorate to a point where dismissal is warranted. Here, as with other potential causes of dismissal, the patient should be adequately warned, the discussion documented, and action taken only if nothing changes.
Anger. As is the case with drug-seeking, the AAFP course advises physicians to anticipate and develop policies for handling situations in which a patient’s anger escalates and creates a real or perceived threat.3 While this is commonly done in acute care facilities, it is often overlooked in outpatient settings.
Among the issues to address: equipping offices and exam rooms with an emergency call button or intercom, knowing where to position yourself to ensure that you can’t be trapped in a room by a threatening patient, and considering how to respond in a way that defuses—rather than escalates—the anger. Calmly ask the patient what he or she is upset about, listen carefully, and apologize, if appropriate, for your role in the upsetting incident. Then move on to the purpose of the visit, stating, for example, “Now, what brings you in today?” 3
It is crucial to set boundaries (although it’s probably not a good idea to attempt it at the time of the outburst), making it clear, for example, that profanity is not acceptable; directing anger at nurses or other staff members is not permitted; and what the consequences of continued outbursts will be. 3
A single incident that’s grounds for dismissal
Despite the emphasis on resolving problems with patients, there are times when dismissal can and should occur, with little warning and no negotiation. In its home study course, the AAFP describes this as a “sentinel incident"— a single occurrence so egregious that it damages the physician-patient relationship beyond repair.3
A threat of violence or a physical assault itself would rise to that level. Some other examples: a sexual assault or blatant sexual advance, falsifying medical records, and theft or another type of criminal activity carried out in the physician’s office.
When a sentinel incident occurs, the best course is likely to be to forego any attempt at resolution, call the police or your facility’s security officer, and, if appropriate, to immediately prepare to “fire” the patient.
Dismissal without abandonment: Here’s how
In the vast majority of cases, dismissing a patient does not in and of itself constitute patient abandonment. Even if the termination is unduly abrupt, as was the case for Susan (CASE 1) and Laura (CASE 2), it doesn’t constitute abandonment unless the patient is dismissed during a course of treatment and unable to find a physician to provide ongoing care.
Neither was true in Susan’s case, and her threat of a lawsuit based on charges of abandonment never came to fruition. Not so for Laura, who was abruptly terminated during ongoing treatment—and who nonetheless made numerous attempts to find another doctor to care for her, without success. The attorney for Laura’s physician advised that the severe consequences of dismissing without going through the proper channels made a trial defense untenable.
Although most charges of patient abandonment never rise to the level required for a successful lawsuit, attorneys often include it in a litany of charges in an attempt to damage the physician’s credibility with a jury. You can usually avoid that scenario by taking the right steps when you dismiss a patient.
CASE 3 Pregnant patient, rural physician
As part of his rural family medicine practice, Dr. J provided obstetrical care. Dr. J had a partner and they alternated call nights, but his partner did not do OB. Dr. J made it a point, however, to always be on call for his obstetrical patients as they neared delivery. Having no patients imminently due, he took a one-week vacation out of town.
One of his patients went into premature labor and went to the local hospital. Dr. J’s partner was called to attend, but indicated he did not do OB work and advised the emergency physician to call “any obstetrician around.” One obstetrical group covered the region and the on-call physician was at another hospital doing a C-section and requested that the patient be transferred to that hospital for evaluation. After a series of delays, the patient was transferred and delivered a preterm infant who showed signs of neurological injury after a lengthy ICU stay.
The family sued all providers involved on several grounds, including patient abandonment. Plaintiff experts testified that the standard of care would be for Dr. J to be in attendance for such emergencies or, failing that, to provide for adequate coverage of his pregnant patient. They also testified that it was reasonable for the patient to have gone to the local hospital where her delivery was planned and that Dr. J should have arranged for the local OB group to provide emergency coverage. The case concluded with an $800,000 pretrial settlement.
Ensure that dismissal is an option
While we’ve already established that physicians have the legal right to dismiss patients, regardless of the reason, there are instances that make it far more difficult—and legally risky—to do so.
A primary care physician in a rural area is a case in point (CASE 3). If you are the only doctor in the area and the patient has no viable means of getting care from another provider, you may want to reconsider the dismissal. It is far easier to establish that a patient in such an underserved area was abandoned, even— as Dr. J found out—for failing to ensure full coverage during a vacation or leave of absence.
Rural physicians can help prevent charges of abandonment by advising patients of the special call challenges a rural setting presents. Doctors should make sure their patients know what to do if an emergency occurs when the practice is closed or a physician is out of town, and document the discussion in the medical record.
A physician in a staff-model HMO may face similar problems. Unless the HMO has another outpatient clinic in the vicinity, dismissal could leave the patient with no means of receiving affordable health care.
Options in such a case might include asking a colleague at the same clinic to accept a patient whom you would like to dismiss or finding a way to manage the patient’s behavior. If a patient has been excessively angry or threatening in the past, for example, it is often advisable to sit down with the patient (with security nearby) to discuss the parameters of expected behavior and develop a contract for future care. The contract might include a requirement that the patient call in advance so that security can be present when he or she arrives, for example, or that the patient agree to abstain from profanity and threats.
Know the laws in your state. Before you terminate a patient, check with your state medical board or local medical society to make sure your actions will be in compliance with any relevant state rules and regulations.
When you dismiss, cover all bases
Send a letter to the patient by certified mail, return receipt requested, notifying him or her of the dismissal and agreeing to provide emergency care for a reasonable time—typically, 30 days—while the patient seeks another physician. It is advisable, too, to help the patient locate other potential clinicians—by, say, including contact information for your county medical society or the patient’s health insurer’s list of in-network providers, or referring an indigent patient to Medicaid or a sliding scale clinic. It is a good idea to offer to transfer records to the new physician, as well.
It is not mandatory to document the reason for the dismissal in the letter, but some sources recommend that you do so. If you’re uncertain how to proceed, check with legal counsel before you send the letter. (You can find sample dismissal letters at www.ttuhsc.edu/som/clinic/forms/ACForm8.11.A.pdf and in “Terminating a patient: Is it time to part ways?” at http://www.aafp.org/fpm/2005/0900/p34.html.)
The events that led up to the dismissal, however, including any discussions you had with the patient about them, must be documented in the medical record. Put a copy of the letter and the certified mail receipt in the chart, as well. JFP
CORRESPONDENCE John Davenport, MD, JD, 13 Redonda, Irvine, CA 92620; john.y.davenport@kp.org
• Unless a single incident irreparably damaged your relationship with a patient, exhaust all efforts at resolution before deciding on dismissal. C
• Establish policies that help you set limits on problem behavior—eg, drug-seeking or angry outbursts—while continuing to care for the patient. C
• When dismissal is unavoidable, inform the patient in writing that you will be available to handle medical emergencies until he or she has found another physician. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Susan L, a 53-year-old who’d been a patient of Dr. O’s for the past 6 years, received a bill for a visit that had occurred nearly 2 years earlier. She called the office and told the receptionist that she had never been billed for this visit and didn’t think she should have to pay after such a lengthy delay. When she received a past due notice, Susan called and asked to speak to the physician—and to schedule an appointment. She was told that she could do neither until her account was current.
Eventually, the unpaid bill was sent to a collection agency, and Susan received a letter threatening legal action. In response, she sent a letter of her own—certified, return receipt requested—detailing her reason for not paying and threatening to sue Dr. O for abandonment.*
*Adapted from actual cases, with details changed to protect the privacy of the parties involved.
With the national unemployment rate hovering at a record high, unpaid medical bills may be your most pressing problem—and potential grounds for patient dismissal. Judging from a recent survey in which primary care physicians identified nearly one patient in 5 as “difficult,"1 it’s unlikely that nonpayment is the only patient conundrum you face.
Indeed, there are many ways a patient can be difficult, including exhibiting habitual hostility, chronic drug-seeking behavior, or consistent noncompliance; breaking appointments at the last minute; or being a no-show. You may wish you could “fire” the worst off enders but be concerned about professional and ethical responsibilities and the legal risk you might face. Ironically, though, struggling to maintain a chronically stressed physician-patient relationship is often riskier than a well-timed termination.2
The key here, however, is the persistent or extreme nature of the difficulty.3 When a dismissal is prompted by a one-time occurrence or lower-level offense, what constitutes a reasonable response is not always clear-cut.
Under what circumstances is it appropriate to end your relationship with a patient? When you do terminate the relationship, what steps can you take to safeguard the patient and avoid charges of abandonment? Here’s a look at these questions—and some answers.
Professional responsibility: How far does it go?
As a physician, you’ve pledged to “do no harm.” And you’ve likely been taught—as it states in the American College of Physicians (ACP) ethics manual—that you have “a moral duty to care for all patients.” 4 The American Medical Association’s code of ethics cites a similar standard: the obligation to place patients’ welfare above your own interests.5
According to the ACP, the physician-patient relationship should be discontinued only under “exceptional circumstances."6 But not everyone agrees, not only on what constitutes “exceptional,” but on whether that is the correct threshold for termination.
A health care attorney writing in American Medical News, for example, takes a more liberal view. It’s time to dismiss, he asserts, when the doctor-patient relationship doesn’t work.7 By that standard, virtually any ongoing problem could be construed as evidence of an “irreparable breakdown” of the physician-patient relationship (TABLE).
TABLE
Key reasons to "fire" a patient
|
| Sources: Kodner C. FP Essentials. 2008.3 Harris S. Am Med News. 2008.7 |
We can work it out
Legally, a doctor can dismiss a patient for virtually any reason, or fail to give any explanation at all.2 Ethically, dismissal should be your last option, not your first choice.
In a home study course titled “Challenging physician-patient interactions,” the American Academy of Family Physicians (AAFP) advises doctors to be certain they have exhausted every reasonable effort to communicate, set achievable goals, and meet the patient’s needs.3 The steps you take to try to mend a damaged patient relationship, of course, will depend on what caused the rift in the first place. Here are some examples.
Nonpayment. You are not compelled (or expected) to indefinitely continue to treat a patient who’s unable—or unwilling—to pay you, of course. But if he or she is out of work and has fallen on hard times or has a single unpaid bill, discussing the problem and attempting to accommodate the patient’s financial limitations (and establish a realistic payment plan) is a reasonable approach.
Having a billing clerk handle most communications regarding unpaid bills may be a good idea. But when a situation escalates, as in the case of Susan L (CASE 1), foregoing a direct discussion and expecting a subordinate to handle an abrupt patient termination is not (ethically or legally) appropriate.7
Laura K, age 34, had always been a challenging patient. She suffered from a collection of pain-producing maladies, including migraines, fibromyalgia, and low back pain. Controlling her pain required increasing amounts of narcotics, sometimes in doses that exceeded therapeutic recommendations.
Recently she’d begun calling her primary care physician’s office for early refills; more than once, she claimed her prescription had been lost or stolen. When Laura called to report that the oxycodone prescribed 4 days ago had been stolen from her purse and to request a refill, the physician refused to speak with her—and instructed the receptionist to tell her she needed to find another physician.
Laura called several other local physicians, but none was able to see her. She then went to the emergency department. The ED physician evaluated her and offered her a prescription for a mild analgesic, but refused her request for oxycodone.
That night, Laura attempted suicide. Although she survived, she was left with significant neurologic deficits. She sued the physician who had refused to speak to her on a variety of counts of negligence, including a charge of abandonment.
At deposition, experts for the plaintiff testified that refusing to see and evaluate a current patient for her ongoing problems without giving substantial notice constituted abandonment—and was a substantial cause of Laura’s suicide attempt. On the advice of counsel, the physician agreed to a $150,000 settlement.
Drug-seeking. Behavior like that of Laura K (CASE 2), whose requests for narcotics and claims of lost pills or prescriptions occurred with increasing regularity, can’t be ignored. The AAFP course, which states that patients should not be dismissed “on the grounds of drug-seeking behaviors alone,"3 recommends that physicians develop policies for prescribing controlled substances and handling drug-seeking patients. Such a policy—which might include limits on the frequency of renewals and the duration of a single prescription, among other provisions—should be communicated to every patient who seeks opioid analgesics.3 The Federation of State Medical Boards recommends the use of a written agreement, spelling out your responsibilities as well as those of the patient, for individuals at high risk of abuse (http://www.fsmb.org/pdf/2004_grpol_Controlled_Substances.pdf).
While the existence of a policy or written contract may not alter the behavior of a drug-seeking patient, it can prevent you from being caught off -guard or reacting as rashly as Laura K’s physician did. Indeed, Laura’s doctor made 2 key missteps: acting without warning, and expecting a receptionist to deliver the dismissal message.
A better approach, from the AAFP’s perspective, is to calmly maintain the limits you’ve set, remind the patient that you want to help, and offer treatment alternatives, such as nonopioid analgesics.3 Discussions in response to drug-seeking behavior, of course, should always be delivered—and documented—by the physician.
Noncompliance. This is a particularly complex problem, as issues of patient autonomy and physician authority are involved. A case study presented in the AAFP home study course describes the thoughts and feelings of a physician who considered dismissing a pediatric patient because the child’s mother refused to allow him to be vaccinated. The physician ultimately decided to continue to treat the child, after determining that the physician-patient relationship could still be beneficial and planning to revisit the vaccination issue with the mother at a later date.3 (Another physician, faced with a similar issue, wrote a New York Times article about his decision to dismiss a young patient. His reasoning? Accepting the mother’s refusal to allow her son to get a tetanus booster would compromise “my conscience and my professional ethics. I couldn’t do that."8)
Although it is important to recognize the difference between noncompliance and an individual’s right to refuse recommended treatment,9 you, too, may encounter situations in which a patient’s, or parent’s, repeated failure—to follow an agreed-upon therapeutic regimen, perhaps, or adhere to a schedule of visits needed to manage a chronic condition— causes your relationship with the patient to deteriorate to a point where dismissal is warranted. Here, as with other potential causes of dismissal, the patient should be adequately warned, the discussion documented, and action taken only if nothing changes.
Anger. As is the case with drug-seeking, the AAFP course advises physicians to anticipate and develop policies for handling situations in which a patient’s anger escalates and creates a real or perceived threat.3 While this is commonly done in acute care facilities, it is often overlooked in outpatient settings.
Among the issues to address: equipping offices and exam rooms with an emergency call button or intercom, knowing where to position yourself to ensure that you can’t be trapped in a room by a threatening patient, and considering how to respond in a way that defuses—rather than escalates—the anger. Calmly ask the patient what he or she is upset about, listen carefully, and apologize, if appropriate, for your role in the upsetting incident. Then move on to the purpose of the visit, stating, for example, “Now, what brings you in today?” 3
It is crucial to set boundaries (although it’s probably not a good idea to attempt it at the time of the outburst), making it clear, for example, that profanity is not acceptable; directing anger at nurses or other staff members is not permitted; and what the consequences of continued outbursts will be. 3
A single incident that’s grounds for dismissal
Despite the emphasis on resolving problems with patients, there are times when dismissal can and should occur, with little warning and no negotiation. In its home study course, the AAFP describes this as a “sentinel incident"— a single occurrence so egregious that it damages the physician-patient relationship beyond repair.3
A threat of violence or a physical assault itself would rise to that level. Some other examples: a sexual assault or blatant sexual advance, falsifying medical records, and theft or another type of criminal activity carried out in the physician’s office.
When a sentinel incident occurs, the best course is likely to be to forego any attempt at resolution, call the police or your facility’s security officer, and, if appropriate, to immediately prepare to “fire” the patient.
Dismissal without abandonment: Here’s how
In the vast majority of cases, dismissing a patient does not in and of itself constitute patient abandonment. Even if the termination is unduly abrupt, as was the case for Susan (CASE 1) and Laura (CASE 2), it doesn’t constitute abandonment unless the patient is dismissed during a course of treatment and unable to find a physician to provide ongoing care.
Neither was true in Susan’s case, and her threat of a lawsuit based on charges of abandonment never came to fruition. Not so for Laura, who was abruptly terminated during ongoing treatment—and who nonetheless made numerous attempts to find another doctor to care for her, without success. The attorney for Laura’s physician advised that the severe consequences of dismissing without going through the proper channels made a trial defense untenable.
Although most charges of patient abandonment never rise to the level required for a successful lawsuit, attorneys often include it in a litany of charges in an attempt to damage the physician’s credibility with a jury. You can usually avoid that scenario by taking the right steps when you dismiss a patient.
CASE 3 Pregnant patient, rural physician
As part of his rural family medicine practice, Dr. J provided obstetrical care. Dr. J had a partner and they alternated call nights, but his partner did not do OB. Dr. J made it a point, however, to always be on call for his obstetrical patients as they neared delivery. Having no patients imminently due, he took a one-week vacation out of town.
One of his patients went into premature labor and went to the local hospital. Dr. J’s partner was called to attend, but indicated he did not do OB work and advised the emergency physician to call “any obstetrician around.” One obstetrical group covered the region and the on-call physician was at another hospital doing a C-section and requested that the patient be transferred to that hospital for evaluation. After a series of delays, the patient was transferred and delivered a preterm infant who showed signs of neurological injury after a lengthy ICU stay.
The family sued all providers involved on several grounds, including patient abandonment. Plaintiff experts testified that the standard of care would be for Dr. J to be in attendance for such emergencies or, failing that, to provide for adequate coverage of his pregnant patient. They also testified that it was reasonable for the patient to have gone to the local hospital where her delivery was planned and that Dr. J should have arranged for the local OB group to provide emergency coverage. The case concluded with an $800,000 pretrial settlement.
Ensure that dismissal is an option
While we’ve already established that physicians have the legal right to dismiss patients, regardless of the reason, there are instances that make it far more difficult—and legally risky—to do so.
A primary care physician in a rural area is a case in point (CASE 3). If you are the only doctor in the area and the patient has no viable means of getting care from another provider, you may want to reconsider the dismissal. It is far easier to establish that a patient in such an underserved area was abandoned, even— as Dr. J found out—for failing to ensure full coverage during a vacation or leave of absence.
Rural physicians can help prevent charges of abandonment by advising patients of the special call challenges a rural setting presents. Doctors should make sure their patients know what to do if an emergency occurs when the practice is closed or a physician is out of town, and document the discussion in the medical record.
A physician in a staff-model HMO may face similar problems. Unless the HMO has another outpatient clinic in the vicinity, dismissal could leave the patient with no means of receiving affordable health care.
Options in such a case might include asking a colleague at the same clinic to accept a patient whom you would like to dismiss or finding a way to manage the patient’s behavior. If a patient has been excessively angry or threatening in the past, for example, it is often advisable to sit down with the patient (with security nearby) to discuss the parameters of expected behavior and develop a contract for future care. The contract might include a requirement that the patient call in advance so that security can be present when he or she arrives, for example, or that the patient agree to abstain from profanity and threats.
Know the laws in your state. Before you terminate a patient, check with your state medical board or local medical society to make sure your actions will be in compliance with any relevant state rules and regulations.
When you dismiss, cover all bases
Send a letter to the patient by certified mail, return receipt requested, notifying him or her of the dismissal and agreeing to provide emergency care for a reasonable time—typically, 30 days—while the patient seeks another physician. It is advisable, too, to help the patient locate other potential clinicians—by, say, including contact information for your county medical society or the patient’s health insurer’s list of in-network providers, or referring an indigent patient to Medicaid or a sliding scale clinic. It is a good idea to offer to transfer records to the new physician, as well.
It is not mandatory to document the reason for the dismissal in the letter, but some sources recommend that you do so. If you’re uncertain how to proceed, check with legal counsel before you send the letter. (You can find sample dismissal letters at www.ttuhsc.edu/som/clinic/forms/ACForm8.11.A.pdf and in “Terminating a patient: Is it time to part ways?” at http://www.aafp.org/fpm/2005/0900/p34.html.)
The events that led up to the dismissal, however, including any discussions you had with the patient about them, must be documented in the medical record. Put a copy of the letter and the certified mail receipt in the chart, as well. JFP
CORRESPONDENCE John Davenport, MD, JD, 13 Redonda, Irvine, CA 92620; john.y.davenport@kp.org
1. Hinchey SA, Jackson JL. A cohort study assessing difficult patient encounters in a walk-in primary care clinic, predictors and outcomes. J Gen Intern Med. 2011;Jan 25 [Epub ahead of print].
2. Schleiter K. Difficult patient-physician relationships and the risk of medical malpractice litigation. Virtual Mentor. 2009;11:242-246.
3. Kodner C. Challenging physician-patient interactions. FP Essentials. ed 354. AAFP home study. Leawood, Kan: American Academy of Family Physicians; November 2008.
4. Snyder L, Leffler C. Ethics and Human Rights Committee American College of Physicians. Ethics manual: fifth ed. Ann Intern Med. 2005;142:560-582.
5. American Medical Association (AMA). Opinion 10.015. The patient-physician relationship. Code of Medical Ethics. Chicago, Ill: AMA. 2008. Available at: http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion10015.shtml. Accessed February 11, 2011.
6. American College of Physicians. Ethical considerations for the use of patient incentives to promote personal responsibility for health: West Virginia Medicaid and beyond [position paper]. Philadelphia: American College of Physicians; 2010.
7. Harris SM. Take care when firing a patient. Am Med News. February 4, 2008. Available at: http://www.ama-assn.org/amednews/2008/02/04/bica0204.htm. Accessed February 11, 2011.
8. Parikh RK. Showing the patient the door, permanently. New York Times. June 10, 2008. Available at: http://www.nytimes.com/2008/06/10/health/views/10case.html. Accessed February 15, 2011.
9. Summey-Lowman B. Patient non-compliance—a powerful legal defense. Healthcare Risk Manag. 2009;15:1-2.
1. Hinchey SA, Jackson JL. A cohort study assessing difficult patient encounters in a walk-in primary care clinic, predictors and outcomes. J Gen Intern Med. 2011;Jan 25 [Epub ahead of print].
2. Schleiter K. Difficult patient-physician relationships and the risk of medical malpractice litigation. Virtual Mentor. 2009;11:242-246.
3. Kodner C. Challenging physician-patient interactions. FP Essentials. ed 354. AAFP home study. Leawood, Kan: American Academy of Family Physicians; November 2008.
4. Snyder L, Leffler C. Ethics and Human Rights Committee American College of Physicians. Ethics manual: fifth ed. Ann Intern Med. 2005;142:560-582.
5. American Medical Association (AMA). Opinion 10.015. The patient-physician relationship. Code of Medical Ethics. Chicago, Ill: AMA. 2008. Available at: http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion10015.shtml. Accessed February 11, 2011.
6. American College of Physicians. Ethical considerations for the use of patient incentives to promote personal responsibility for health: West Virginia Medicaid and beyond [position paper]. Philadelphia: American College of Physicians; 2010.
7. Harris SM. Take care when firing a patient. Am Med News. February 4, 2008. Available at: http://www.ama-assn.org/amednews/2008/02/04/bica0204.htm. Accessed February 11, 2011.
8. Parikh RK. Showing the patient the door, permanently. New York Times. June 10, 2008. Available at: http://www.nytimes.com/2008/06/10/health/views/10case.html. Accessed February 15, 2011.
9. Summey-Lowman B. Patient non-compliance—a powerful legal defense. Healthcare Risk Manag. 2009;15:1-2.
Sued for misdiagnosis? It could happen to you
• Create a problem list for each patient, including chronic and acute conditions, unexplained signs and symptoms, medications, and allergies. C
• Avoid attributing every new symptom to the patient’s documented medical conditions. C
• Develop and adhere to “don’t-miss” lists of signs and symptoms that warrant rapid action. C
• Establish a fail-safe system to ensure that you receive notification whenever a final imaging or lab report differs from the preliminary report and document your response to each abnormal result. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Misdiagnosis accounts for more malpractice claims than medication errors—indeed, for more lawsuits than any other medical misstep.1-5 Yet until recently, diagnostic errors garnered little attention from patient safety advocates.
That’s no longer the case. In 2007, the Agency for Healthcare Research and Quality (AHRQ) identified diagnostic errors (a catchall category encompassing delayed, incorrect, and missed diagnoses) as a problem that warranted closer study.6 The inaugural conference on Diagnostic Error in Medicine, cosponsored by AHRQ and the American Medical Informatics Association, took place in 2008. The third annual Diagnostic Error in Medicine conference will be held in Canada in October, reflecting the expanding focus on uncovering root causes of diagnostic error and developing preventive measures aimed at safeguarding patients and avoiding lawsuits.
Because diagnostic errors have long been underemphasized and understudied—and remain difficult to track—it is hard to know just how often they occur. Estimates of their frequency fluctuate widely from 1 study to another, but are generally in the range of 10% to 15%.7 Fatal illnesses appear to be misdiagnosed more frequently than less severe conditions: A review of more than 50 autopsy studies found that, on average, about 1 in 4 (23.5%) major diagnoses were missed.1
Whatever the numbers, diagnostic missteps are clearly common enough to be on patients’ radar screen. In a recent survey of US adults, 55% of respondents cited misdiagnosis as their greatest concern when they see a doctor in an outpatient setting.8 In a Harris Poll commissioned by the National Patient Safety Foundation9 several years earlier, 1 in 6 adults reported having had a condition that was misdiagnosed.
Evidence suggests that while years of experience and strong diagnostic skills help prevent diagnostic errors, they do not afford full protection against the cascade of events that can result in a serious diagnostic error. In fact, overconfidence may contribute to the problem.10,11
Check out the 3 legal cases in the pages that follow from the files of John Davenport, MD, JD. Dr. Davenport, a medical malpractice attorney, provided legal representation in each of these cases.
The take-away message: No physician is immune to misdiagnosis or to a subsequent lawsuit. There are, however, steps you can take to safeguard your patients and yourself, but first you need to know where the pitfalls lie.
Misdiagnosis in primary care: What malpractice claims reveal
Diagnostic errors that result in malpractice claims undergo extensive legal review. Thus, they provide an excellent opportunity for analysis, as the authors of a study of 181 “closed,” or completed, claims from 4 malpractice insurers found.12 The errors all occurred in ambulatory settings, with primary care physicians most frequently involved.
Nearly 6 in 10 of the lawsuits were for missed or delayed cancer diagnoses, followed by misdiagnosis of infection, fracture, and myocardial infarction. Overall, 24% of the cases involved breast cancer. No other disorder came close.
The most common problems, or “breakdowns,” in the diagnostic process were:
- failure to order the appropriate diagnostic test (which occurred in 55% of the cases)
- failure to create a proper follow-up plan (45%)
- failure to obtain a thorough medical history or to perform a thorough physical examination (42%).12
Notably, however, diagnostic errors rarely had a single cause. A median of 3 breakdowns per case was identified, and more than 4 in 10 cases involved more than 1 clinician.
Additional sources of breakdowns ran the gamut from patient factors (eg, non-compliance, atypical presentation, or a delay in seeking care) to system errors (eg, delay in seeing a test result, referral delay, or a mishandled handoff). Rarely was misdiagnosis attributed to a physician’s cognitive error alone. Most diagnostic errors, the authors reported, involved “a potent combination of individual and system factors.” 12
Is it cancer? Failure to test or follow up
Cancer may not be the most frequently misdiagnosed condition, but because of the dire consequences often associated with a delay in detection, cancer is No. 1 in frequency of diagnostic error lawsuits13—with breast cancer typically at or near the top of the list. Evidence suggests that clinician preconception plays a role.
Most women who develop breast cancer are over the age of 50, but plaintiffs in breast cancer suits tend to be younger.14,15 This may be partly because of overreliance on age as a predictive factor, causing some physicians to offer a younger woman what may be unwarranted reassurance that a breast lump is due to fibrocystic tissue rather than malignancy (CASE 1).
Ordering a test is not enough. Even when physicians order the correct test, follow-up may fall short. In the closed claims study, physicians incorrectly interpreted test results in 37% of the cases.12 Other evidence suggests that about a third of women with abnormal mammograms do not receive follow-up care that’s consistent with established guidelines.16
What’s more, physicians sometimes overlook the fact that diagnostic tests are rarely 100% accurate. Mammography misses approximately 20% of breast cancer cases,17 for example, and a woman with a palpable lump should be closely watched, not dismissed on the basis of a negative mammogram result.1,15
What happens to test results? In other cases, the problem is not that a test result doesn’t match the clinical findings, but that the result is not reviewed by the physician or conveyed to the patient in a timely manner. Indeed, the title of a published report of a survey of internists starts with the quote, “I wish I had seen this test result earlier!” 18 Of the 262 internists surveyed, only 41% expressed satisfaction with their method of handling test results.
What would satisfy these physicians? Respondents said what they wanted in a test result management system were tools that would help them generate letters to patients detailing the results, prioritize their workflow, and track orders for tests to completion.
A 32-year-old woman sought care for “sore breasts” 4 months postpartum. Her primary care physician found “bilateral lumpy and tender breasts,” diagnosed fibrocystic breast disease, and prescribed a nonsteroidal anti-inflammatory drug. There was no follow-up plan documented.
She returned in 4 months, stating her symptoms were better but she still had soreness in her left breast. The physician did not examine her, but changed her medication to a different anti-inflammatory. Follow-up was to “return to clinic PRN.”
On her next visit she complained of a lump in the left breast. The physician found a “spongy irregular 2 cm lump” in the upper outer quadrant of the breast, diagnosed a fibrocystic lesion, and reassured the patient. Follow-up again was to return PRN.
Several months later, the patient saw another physician, for back pain and a painful and enlarging breast lump. The physician suspected fibrocystic disease but was unable to obtain fluid by fine needle aspiration. The patient was referred to a surgeon, who obtained a nondiagnostic needle biopsy and an excisional biopsy, which revealed breast cancer. The patient’s back pain turned out to be from metastatic breast cancer. She sued for failure to diagnose breast cancer. The case was settled for an undisclosed large sum.
Commentary: Failure to diagnose breast cancer is a leading cause of malpractice lawsuits, many of them in younger women. Plaintiff recoveries correlate with the length of the delay in diagnosis.
In this case, experts identified a series of missteps in the care of this patient which, when combined with a young, very sick, and sympathetic plaintiff, led to a large recovery. Although it may have been reasonable to diagnose fibrocystic disease on the first visit, experts cited the failure to take a family history (the patient’s aunt and maternal grandmother had had breast cancer) and the failure to document a follow-up plan as damaging to the doctor’s case. They also faulted the physician for failing to examine the breast on the second visit and failing to do fine needle aspiration or refer on the third visit, and for the nonspecific follow-up plans.
Diagnostic lesson: Although breast cancer is less common in women younger than 40, it does occur, and the same diligence in examination, charting, and follow up is required regardless of the patient’s age.
By the way, doc… Harried physician, hurried response
What physician isn’t familiar with the patient who comes in for care of 1, or several, chronic conditions, but mentions another problem as he or she is getting ready to walk out the door (CASE 2)? If that problem appears to be a transient and treatable condition, the temptation is to make a hasty diagnosis and write a prescription, without the usual degree of history taking, patient examination, contemplation, or documentation. Doing so, however, poses considerable risk, to both patient and physician.
If the condition or symptom is serious enough to address in the course of the visit, it requires the same level of attention as any other presenting problem. When time constraints prevent you from addressing the complaint with the proper diligence, it would be appropriate—assuming the symptom in question is nonurgent—to ask the patient to make another appointment. But be sure to document that you did so.
A 62-year-old man saw his family physician for routine care of hypertension, diabetes, and hyperlipidemia. During the visit, the patient mentioned that he had back pain, insomnia, and a sore tongue, which the physician diagnosed as aphthous stomatitis and for which a steroidal oral cream was prescribed.
The patient was scheduled to return for a routine visit in 4 months, but did not come in until 7 months had passed—at which time the physician noted a >1 cm nodular bleeding tongue lesion. Biopsy showed squamous cell cancer, and the patient required extensive surgery, chemotherapy, and radiation. He sued for misdiagnosis and delayed diagnosis.
The physician’s defense was that given the symptoms and findings, aphthous stomatitis was a reasonable diagnosis and that he had instructed the patient to return to the office if he didn’t feel better in a few weeks. The patient disputed this. His attorney noted that the patient had multiple risk factors for tongue cancer that were not in the medical record; nor was there documentation of a tongue examination or the claimed instructions for the return visit, indicating that the patient received substandard care. The case was settled at trial for $300,000.
Commentary: The contrast between the thorough documentation for the patient’s chronic disease history and physical exam and the absence of documentation for the sore tongue suggests that this was an instance of a “by the way, doc” conversation—and a reminder of the risk that physicians assume when managing patients with multiple conditions.
Diagnostic lesson: The law does not give physicians a pass on the standard of care, regardless of how many conditions are treated in a single visit. To avoid a diagnostic error—and a potential lawsuit—a symptom-specific history, physical, and clear instructions with a follow-up plan are necessary for every condition that’s addressed.
How sure are you of the diagnosis?
It’s human nature to see things in terms of what you’re familiar with. A doctor who has been treating a patient with migraine headaches for years, for example, is apt to assume that “the worst migraine I’ve ever had” is more of the same (CASE 3). Similarly, a clinician who has identified a disorder that matches several of a patient’s symptoms may dismiss or overlook signs and symptoms that do not fit that explanation or diagnosis. Safety advocates refer to this phenomenon as “premature closure.” It may also be a function of overconfidence.
One example of physician overconfidence comes from a study in which experienced dermatologists were asked to examine lesions and diagnose melanoma. Although the specialists confidently diagnosed melanoma in more than 50% of the test cases, 30% of their decisions were later found to be incorrect.19
A 47-year-old man with a history of migraines walked into his physician’s clinic with a complaint of a severe headache. His physician was fully booked but he was given an appointment with a per diem physician. According to the patient and a friend who accompanied him, the patient told the doctor, “This is the worst migraine of my life.” The physician simply documented, “flare of migraine.” The chart indicated that the physical revealed normal vital signs and noted that the patient was “photophobic,” but that his neurological exam was “intact.”
Over the next several hours, the patient received sumatriptan and several doses of opioid analgesics. He stated that he still had a headache but felt better and was sent home with instructions to call or come in if the headache returned.
The next morning a neighbor, unable to reach the patient on the phone, went to his house and found him in a stupor, with slurred speech. The patient was taken by ambulance to a local hospital and found to have a subarachnoid hemorrhage. After weeks in the hospital and a rehabilitation center, he was left with significant cognitive and neurological impairments. He sued for failure to diagnose and won a multimillion dollar award at trial.
Commentary: Expert testimony clearly pointed to the history and physical as being substandard. Specifically, the physical should have included, among other things, a test for nuchal rigidity. Had the patient not had a history of migraines, he might have undergone a more complete medical history and physical evaluation and his symptoms would likely have been evaluated more thoroughly.
Diagnostic lesson: Be wary of “diagnostic inertia”—the tendency to depend too much on a past diagnosis when symptoms arise. Don’t be trapped into attributing all new symptoms to an old disease.
Build a no-fault, fail-safe system
The purpose of analyzing diagnostic errors is not to assign blame or point a finger at physicians, but rather to find and fix flaws in the medical system.20 That approach has been used by patient safety advocates to address other types of errors following the publication of the Institute of Medicine’s landmark report on medical error 11 years ago.21
Since then, many physician leaders have looked to the airline industry—a field in which the consequences for not strictly adhering to a fail-safe system are likely to be fatal. That reality has led to the development of vital checklists, forcing functions (in which the user is prevented from moving to the next step until the current step is completed), and computerized reminders in an attempt to eliminate, to the extent possible, the chance of human error.
The same principle can be applied to misdiagnosis. Recommended steps—ordering diagnostic tests or referring to a specialist, for example—should be put into motion whenever a set of predetermined parameters are met, rather than relying on physician memory or choice.20
Similarly, checklists should specify questions to ask or criteria to be met under specified circumstances to prevent physicians from prematurely settling on a (possibly incorrect) diagnosis. To avoid a rush to judgment, some patient safety advocates1 stress the importance of assessing the urgency of a patient’s condition, rather than trying to arrive at a definitive diagnosis the first time he or she presents with a perplexing set of signs and symptoms. Other recommendations follow:
Mandate a second look. Develop and adhere to a set of criteria to determine when a referral to a specialist or a physician consultation is needed, rather than deciding on a case-by-case basis.
Plug the holes in your follow-up system. Develop a fail-safe system for reviewing diagnostic tests or laboratory findings and reporting them to patients without delay. This can be done with an electronic health record (EHR) system or by developing and adhering to parameters requiring, for instance, that no test result get filed until there are 2 signatures on it—that of the physician who ordered the test, indicating that he or she has seen it, and that of a staff member, indicating that the patient has been notified of the results. As an additional back-up, tell patients undergoing tests when to expect to get results, and stress the importance of calling the office if they do not receive such notification within a specified time frame.
Partner with patients. Engage patients in the pursuit of a definitive diagnosis. Discuss your preliminary findings, describe your treatment decision and what you expect to occur, and urge patients to contact you with evidence that confirms or refutes that expectation. Elicit additional feedback at each visit until either the symptoms have fully resolved or you have gathered enough information to arrive at a definitive diagnosis.
Develop “don’t-miss” checklists. One list should cover diagnostic red flags to be considered anytime you see a symptomatic patient to ensure that you don’t overlook important signs and symptoms, and include findings that warrant hospital admission, specified diagnostic tests, and immediate referral. (A patient who comes in with a “common pink eye,” but has consensual photophobia, is at risk for iritis and needs an urgent ophthalmology evaluation, for instance.) Another list you should develop is a “must-do” list for well visits, featuring clinical scenarios to address and screening tests to remember, such as an eye exam for patients with diabetes.
Question your initial diagnosis. Beware of “premature closure”—the tendency to stop looking for other signs and symptoms once you find a presumptive diagnosis—and “diagnostic inertia”—evaluating new signs and symptoms almost exclusively on the basis of past medical history. If aspects of a patient presentation do not fit your presumed diagnosis, use a decision support system, if available, to review other possibilities.
Head off hand-off errors. Develop a problem list for each patient to reduce the likelihood that crucial information will be overlooked when more than 1 clinician is involved in his or her care. Include chronic and acute conditions, unexplained signs and symptoms, medications, and allergies. Create a fail-safe system for other potential hand-off problems, as well—requiring confirmation that the findings in a preliminary radiology report are the same as those in the final report before you take action based on the preliminary report, for example, and ensuring that you receive prompt notification whenever that is not the case.
EHRs and decision support: Isn’t it time?
In 2009, 44% of office-based physicians had EHRs, according to a Centers for Disease Control and Prevention preliminary report.22 Federal funding to promote the adoption of EHRs is expected to accelerate their use. Among the benefits of EHRs are clinical reminders, system alerts, and documentation tools that can help reduce the risk of diagnostic missteps and avert misdiagnosis lawsuits.
The Department of Veterans Affairs uses a notification system called View Alert, for example, that tracks acknowledgement of abnormal radiology test results and flags those that remain unacknowledged. 23 EHR systems can also be programmed to issue automated appointment reminders that make it easier to track patients who do not show up for critical follow-up visits.
Diagnostic decision support software adds another critical element. When a clinician inputs a set of symptoms and patient-specific data, such systems produce lists of possible diagnoses, often divided by bodily system.
While many safety advocates believe that the use of such systems will increase the likelihood of accurate diagnosis, critics point out that the software is only as good as the clinician using it. One concern is that computerized systems typically come with a “macro” ability—that is, the ability to enter large amounts of information with the click of a key. This raises the possibility that an overload of patient data, some of which may be incorrect, will be added to the medical record—or that the system will generate so many possibilities that clinicians will cease to pay attention. Both can lead to inferences of inattention or raise doubts about a physician’s credibility in a legal setting.
Electronic prescribing software systems that flag potential drug interactions are a case in point. Forty-five percent of family physicians responding to a Journal of Family Practice Instant Poll about their use of such systems reported that they override them frequently. The problem, according to 1 respondent: The system gives “so many red flags that I routinely ignore them all—like the little boy who cried wolf.”
CORRESPONDENCE John Davenport, MD, JD, 13 Redonda, Irvine, CA 92620; John.y.davenport@kp.org
1. Schiff GD, Kim S, Abrams R, et al. Diagnosing diagnosis errors: lessons from a multi-institutional collaborative project. Adv Patient Safety. 2005;255:255-278.
2. Sato L. Evidence-based patient safety and risk management technology. J Qual Improv. 2001;27:435.-
3. Phillips R, Bartholomew L, Dovey S, et al. Learning from malpractice claims about negligent, adverse events in primary care in the United States. Qual Saf Health Care. 2004;13:121-126.
4. Fitzgerald N. Top five causes of malpractice claims. American Physicians Assurance Corporation. 2004. Available at: http://www.apassurance.com/RiskMgt/Articles_RM/5%20Causes%20of%20Claims_RMArticle.pdf. Accessed August 2, 2010.
5. Chandra A, Nundy S, Seabury SA. The growth of physician medical malpractice payments: evidence from the National Practitioner Data Bank. Health Aff (Millwood). 2005;W5(suppl):240-249.
6. Agency for Healthcare Research and Quality Special emphasis notice (SEN): AHRQ announces interest in research on diagnostic errors in ambulatory care settings. Available at: http://grants.nih.gv/grants/guide/notice-files-NOT-HS-08-002.html. Accessed July 30, 2010.
7. Berner ES, Graber ML. Overconfidence as a cause of diagnostic error in medicine. Am J Med. 2008;121(suppl 5A):S2-S23.
8. Isabel Healthcare. Misdiagnosis is an overlooked and growing patient safety issue and core mission of Isabel Healthcare. March 20, 2006. Available at http://www.isabelhealthcare.com/pdf/USsurveyrelease-Final.pdf. Accessed August 4, 2010.
9. Golodner L. How the public perceives patient safety. Newsletter of the National Patient Safety Foundation. 2004;1997:1-6.
10. Berner ES. Diagnostic error in medicine: introduction. Adv Health Sci Educ Theory Pract. 2009;14(suppl 1):1-5.
11. Friedman CP, Gatti GG, Franz TM, et al. Do physicians know when their diagnoses are correct? Implications for decision support and error reduction. J Gen Intern Med. 2005;20:334-339.
12. Ghandi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med. 2006;145:488-496.
13. McDonald C, Hernandez MB, Gofman Y, et al. The five most common misdiagnoses: a meta-analysis of autopsy and malpractice data. Internet J Fam Pract. 2009;7(2). Available at http://www.ispub.com/journal/the_internet_journal_of_family_practice/volume_7_number_2_19/article/the-five-most-common-misdiagnosesa-meta-analysis-of-autopsy-and-malpractice-data.html. Accessed July 23, 2010.
14. Mitnick JS, Vasquez MF, Kronovet SZ, et al. Malpractice litigation involving patients with carcinoma of the breast. J Am Coll Surg. 1995;181:315-321.
15. Failure to diagnose breast cancer. Medical Malpractice Lawyers and Attorneys Online. http://www.medical-malpractice-attorneys-lawsuits.com/pages/breast-cancer.html. Accessed August 2, 2010.
16. Poon EG, Haas JS, Puopolo AL, et al. Communication factors in the follow-up of abnormal mammograms. J Gen Intern Med. 2004;19:316-323.
17. National Cancer Institute. Fact sheet. Mammograms. Available at: http://www.cancer.gov/cancertopics/factsheet/Detection/mammograms. Accessed August 3, 2010.
18. Poon EG, Gandhi TK, Sequist TD, et al. “I wish I had seen this test result earlier!”: dissatisfaction with test result management systems in primary care. Arch Intern Med. 2004;164:2223-2228.
19. Dreistl S, Binder M. Do physicians value decision support? A look at the effect of decision support on physician opinion. Artif Intell Med. 2005;33:25-30.
20. Newman-Toker DE, Pronovost PJ. Diagnostic errors: the new frontier for patient safety. JAMA. 2009;301:1060-1062.
21. Institute of Medicine. To err is human: building a safer health system. Washington, DC: November 1, 1999.
22. Centers for Disease Control and Prevention. NCHS Health E-Stat. Electronic medical record/electronic health record use by office-based physicians: United States, 2008 and preliminary 2009. Available at: http://www.cdc.gov/nchs/data/hestat/emr_ehr/emr_ehr.htm. Accessed July 30, 2010.
23. Singh H, Arora HS, Vij MS, et al. Communication outcomes of critical imaging results in a computerized notification system. J Am Med Inform Assoc. 2007;14:459-466.
• Create a problem list for each patient, including chronic and acute conditions, unexplained signs and symptoms, medications, and allergies. C
• Avoid attributing every new symptom to the patient’s documented medical conditions. C
• Develop and adhere to “don’t-miss” lists of signs and symptoms that warrant rapid action. C
• Establish a fail-safe system to ensure that you receive notification whenever a final imaging or lab report differs from the preliminary report and document your response to each abnormal result. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Misdiagnosis accounts for more malpractice claims than medication errors—indeed, for more lawsuits than any other medical misstep.1-5 Yet until recently, diagnostic errors garnered little attention from patient safety advocates.
That’s no longer the case. In 2007, the Agency for Healthcare Research and Quality (AHRQ) identified diagnostic errors (a catchall category encompassing delayed, incorrect, and missed diagnoses) as a problem that warranted closer study.6 The inaugural conference on Diagnostic Error in Medicine, cosponsored by AHRQ and the American Medical Informatics Association, took place in 2008. The third annual Diagnostic Error in Medicine conference will be held in Canada in October, reflecting the expanding focus on uncovering root causes of diagnostic error and developing preventive measures aimed at safeguarding patients and avoiding lawsuits.
Because diagnostic errors have long been underemphasized and understudied—and remain difficult to track—it is hard to know just how often they occur. Estimates of their frequency fluctuate widely from 1 study to another, but are generally in the range of 10% to 15%.7 Fatal illnesses appear to be misdiagnosed more frequently than less severe conditions: A review of more than 50 autopsy studies found that, on average, about 1 in 4 (23.5%) major diagnoses were missed.1
Whatever the numbers, diagnostic missteps are clearly common enough to be on patients’ radar screen. In a recent survey of US adults, 55% of respondents cited misdiagnosis as their greatest concern when they see a doctor in an outpatient setting.8 In a Harris Poll commissioned by the National Patient Safety Foundation9 several years earlier, 1 in 6 adults reported having had a condition that was misdiagnosed.
Evidence suggests that while years of experience and strong diagnostic skills help prevent diagnostic errors, they do not afford full protection against the cascade of events that can result in a serious diagnostic error. In fact, overconfidence may contribute to the problem.10,11
Check out the 3 legal cases in the pages that follow from the files of John Davenport, MD, JD. Dr. Davenport, a medical malpractice attorney, provided legal representation in each of these cases.
The take-away message: No physician is immune to misdiagnosis or to a subsequent lawsuit. There are, however, steps you can take to safeguard your patients and yourself, but first you need to know where the pitfalls lie.
Misdiagnosis in primary care: What malpractice claims reveal
Diagnostic errors that result in malpractice claims undergo extensive legal review. Thus, they provide an excellent opportunity for analysis, as the authors of a study of 181 “closed,” or completed, claims from 4 malpractice insurers found.12 The errors all occurred in ambulatory settings, with primary care physicians most frequently involved.
Nearly 6 in 10 of the lawsuits were for missed or delayed cancer diagnoses, followed by misdiagnosis of infection, fracture, and myocardial infarction. Overall, 24% of the cases involved breast cancer. No other disorder came close.
The most common problems, or “breakdowns,” in the diagnostic process were:
- failure to order the appropriate diagnostic test (which occurred in 55% of the cases)
- failure to create a proper follow-up plan (45%)
- failure to obtain a thorough medical history or to perform a thorough physical examination (42%).12
Notably, however, diagnostic errors rarely had a single cause. A median of 3 breakdowns per case was identified, and more than 4 in 10 cases involved more than 1 clinician.
Additional sources of breakdowns ran the gamut from patient factors (eg, non-compliance, atypical presentation, or a delay in seeking care) to system errors (eg, delay in seeing a test result, referral delay, or a mishandled handoff). Rarely was misdiagnosis attributed to a physician’s cognitive error alone. Most diagnostic errors, the authors reported, involved “a potent combination of individual and system factors.” 12
Is it cancer? Failure to test or follow up
Cancer may not be the most frequently misdiagnosed condition, but because of the dire consequences often associated with a delay in detection, cancer is No. 1 in frequency of diagnostic error lawsuits13—with breast cancer typically at or near the top of the list. Evidence suggests that clinician preconception plays a role.
Most women who develop breast cancer are over the age of 50, but plaintiffs in breast cancer suits tend to be younger.14,15 This may be partly because of overreliance on age as a predictive factor, causing some physicians to offer a younger woman what may be unwarranted reassurance that a breast lump is due to fibrocystic tissue rather than malignancy (CASE 1).
Ordering a test is not enough. Even when physicians order the correct test, follow-up may fall short. In the closed claims study, physicians incorrectly interpreted test results in 37% of the cases.12 Other evidence suggests that about a third of women with abnormal mammograms do not receive follow-up care that’s consistent with established guidelines.16
What’s more, physicians sometimes overlook the fact that diagnostic tests are rarely 100% accurate. Mammography misses approximately 20% of breast cancer cases,17 for example, and a woman with a palpable lump should be closely watched, not dismissed on the basis of a negative mammogram result.1,15
What happens to test results? In other cases, the problem is not that a test result doesn’t match the clinical findings, but that the result is not reviewed by the physician or conveyed to the patient in a timely manner. Indeed, the title of a published report of a survey of internists starts with the quote, “I wish I had seen this test result earlier!” 18 Of the 262 internists surveyed, only 41% expressed satisfaction with their method of handling test results.
What would satisfy these physicians? Respondents said what they wanted in a test result management system were tools that would help them generate letters to patients detailing the results, prioritize their workflow, and track orders for tests to completion.
A 32-year-old woman sought care for “sore breasts” 4 months postpartum. Her primary care physician found “bilateral lumpy and tender breasts,” diagnosed fibrocystic breast disease, and prescribed a nonsteroidal anti-inflammatory drug. There was no follow-up plan documented.
She returned in 4 months, stating her symptoms were better but she still had soreness in her left breast. The physician did not examine her, but changed her medication to a different anti-inflammatory. Follow-up was to “return to clinic PRN.”
On her next visit she complained of a lump in the left breast. The physician found a “spongy irregular 2 cm lump” in the upper outer quadrant of the breast, diagnosed a fibrocystic lesion, and reassured the patient. Follow-up again was to return PRN.
Several months later, the patient saw another physician, for back pain and a painful and enlarging breast lump. The physician suspected fibrocystic disease but was unable to obtain fluid by fine needle aspiration. The patient was referred to a surgeon, who obtained a nondiagnostic needle biopsy and an excisional biopsy, which revealed breast cancer. The patient’s back pain turned out to be from metastatic breast cancer. She sued for failure to diagnose breast cancer. The case was settled for an undisclosed large sum.
Commentary: Failure to diagnose breast cancer is a leading cause of malpractice lawsuits, many of them in younger women. Plaintiff recoveries correlate with the length of the delay in diagnosis.
In this case, experts identified a series of missteps in the care of this patient which, when combined with a young, very sick, and sympathetic plaintiff, led to a large recovery. Although it may have been reasonable to diagnose fibrocystic disease on the first visit, experts cited the failure to take a family history (the patient’s aunt and maternal grandmother had had breast cancer) and the failure to document a follow-up plan as damaging to the doctor’s case. They also faulted the physician for failing to examine the breast on the second visit and failing to do fine needle aspiration or refer on the third visit, and for the nonspecific follow-up plans.
Diagnostic lesson: Although breast cancer is less common in women younger than 40, it does occur, and the same diligence in examination, charting, and follow up is required regardless of the patient’s age.
By the way, doc… Harried physician, hurried response
What physician isn’t familiar with the patient who comes in for care of 1, or several, chronic conditions, but mentions another problem as he or she is getting ready to walk out the door (CASE 2)? If that problem appears to be a transient and treatable condition, the temptation is to make a hasty diagnosis and write a prescription, without the usual degree of history taking, patient examination, contemplation, or documentation. Doing so, however, poses considerable risk, to both patient and physician.
If the condition or symptom is serious enough to address in the course of the visit, it requires the same level of attention as any other presenting problem. When time constraints prevent you from addressing the complaint with the proper diligence, it would be appropriate—assuming the symptom in question is nonurgent—to ask the patient to make another appointment. But be sure to document that you did so.
A 62-year-old man saw his family physician for routine care of hypertension, diabetes, and hyperlipidemia. During the visit, the patient mentioned that he had back pain, insomnia, and a sore tongue, which the physician diagnosed as aphthous stomatitis and for which a steroidal oral cream was prescribed.
The patient was scheduled to return for a routine visit in 4 months, but did not come in until 7 months had passed—at which time the physician noted a >1 cm nodular bleeding tongue lesion. Biopsy showed squamous cell cancer, and the patient required extensive surgery, chemotherapy, and radiation. He sued for misdiagnosis and delayed diagnosis.
The physician’s defense was that given the symptoms and findings, aphthous stomatitis was a reasonable diagnosis and that he had instructed the patient to return to the office if he didn’t feel better in a few weeks. The patient disputed this. His attorney noted that the patient had multiple risk factors for tongue cancer that were not in the medical record; nor was there documentation of a tongue examination or the claimed instructions for the return visit, indicating that the patient received substandard care. The case was settled at trial for $300,000.
Commentary: The contrast between the thorough documentation for the patient’s chronic disease history and physical exam and the absence of documentation for the sore tongue suggests that this was an instance of a “by the way, doc” conversation—and a reminder of the risk that physicians assume when managing patients with multiple conditions.
Diagnostic lesson: The law does not give physicians a pass on the standard of care, regardless of how many conditions are treated in a single visit. To avoid a diagnostic error—and a potential lawsuit—a symptom-specific history, physical, and clear instructions with a follow-up plan are necessary for every condition that’s addressed.
How sure are you of the diagnosis?
It’s human nature to see things in terms of what you’re familiar with. A doctor who has been treating a patient with migraine headaches for years, for example, is apt to assume that “the worst migraine I’ve ever had” is more of the same (CASE 3). Similarly, a clinician who has identified a disorder that matches several of a patient’s symptoms may dismiss or overlook signs and symptoms that do not fit that explanation or diagnosis. Safety advocates refer to this phenomenon as “premature closure.” It may also be a function of overconfidence.
One example of physician overconfidence comes from a study in which experienced dermatologists were asked to examine lesions and diagnose melanoma. Although the specialists confidently diagnosed melanoma in more than 50% of the test cases, 30% of their decisions were later found to be incorrect.19
A 47-year-old man with a history of migraines walked into his physician’s clinic with a complaint of a severe headache. His physician was fully booked but he was given an appointment with a per diem physician. According to the patient and a friend who accompanied him, the patient told the doctor, “This is the worst migraine of my life.” The physician simply documented, “flare of migraine.” The chart indicated that the physical revealed normal vital signs and noted that the patient was “photophobic,” but that his neurological exam was “intact.”
Over the next several hours, the patient received sumatriptan and several doses of opioid analgesics. He stated that he still had a headache but felt better and was sent home with instructions to call or come in if the headache returned.
The next morning a neighbor, unable to reach the patient on the phone, went to his house and found him in a stupor, with slurred speech. The patient was taken by ambulance to a local hospital and found to have a subarachnoid hemorrhage. After weeks in the hospital and a rehabilitation center, he was left with significant cognitive and neurological impairments. He sued for failure to diagnose and won a multimillion dollar award at trial.
Commentary: Expert testimony clearly pointed to the history and physical as being substandard. Specifically, the physical should have included, among other things, a test for nuchal rigidity. Had the patient not had a history of migraines, he might have undergone a more complete medical history and physical evaluation and his symptoms would likely have been evaluated more thoroughly.
Diagnostic lesson: Be wary of “diagnostic inertia”—the tendency to depend too much on a past diagnosis when symptoms arise. Don’t be trapped into attributing all new symptoms to an old disease.
Build a no-fault, fail-safe system
The purpose of analyzing diagnostic errors is not to assign blame or point a finger at physicians, but rather to find and fix flaws in the medical system.20 That approach has been used by patient safety advocates to address other types of errors following the publication of the Institute of Medicine’s landmark report on medical error 11 years ago.21
Since then, many physician leaders have looked to the airline industry—a field in which the consequences for not strictly adhering to a fail-safe system are likely to be fatal. That reality has led to the development of vital checklists, forcing functions (in which the user is prevented from moving to the next step until the current step is completed), and computerized reminders in an attempt to eliminate, to the extent possible, the chance of human error.
The same principle can be applied to misdiagnosis. Recommended steps—ordering diagnostic tests or referring to a specialist, for example—should be put into motion whenever a set of predetermined parameters are met, rather than relying on physician memory or choice.20
Similarly, checklists should specify questions to ask or criteria to be met under specified circumstances to prevent physicians from prematurely settling on a (possibly incorrect) diagnosis. To avoid a rush to judgment, some patient safety advocates1 stress the importance of assessing the urgency of a patient’s condition, rather than trying to arrive at a definitive diagnosis the first time he or she presents with a perplexing set of signs and symptoms. Other recommendations follow:
Mandate a second look. Develop and adhere to a set of criteria to determine when a referral to a specialist or a physician consultation is needed, rather than deciding on a case-by-case basis.
Plug the holes in your follow-up system. Develop a fail-safe system for reviewing diagnostic tests or laboratory findings and reporting them to patients without delay. This can be done with an electronic health record (EHR) system or by developing and adhering to parameters requiring, for instance, that no test result get filed until there are 2 signatures on it—that of the physician who ordered the test, indicating that he or she has seen it, and that of a staff member, indicating that the patient has been notified of the results. As an additional back-up, tell patients undergoing tests when to expect to get results, and stress the importance of calling the office if they do not receive such notification within a specified time frame.
Partner with patients. Engage patients in the pursuit of a definitive diagnosis. Discuss your preliminary findings, describe your treatment decision and what you expect to occur, and urge patients to contact you with evidence that confirms or refutes that expectation. Elicit additional feedback at each visit until either the symptoms have fully resolved or you have gathered enough information to arrive at a definitive diagnosis.
Develop “don’t-miss” checklists. One list should cover diagnostic red flags to be considered anytime you see a symptomatic patient to ensure that you don’t overlook important signs and symptoms, and include findings that warrant hospital admission, specified diagnostic tests, and immediate referral. (A patient who comes in with a “common pink eye,” but has consensual photophobia, is at risk for iritis and needs an urgent ophthalmology evaluation, for instance.) Another list you should develop is a “must-do” list for well visits, featuring clinical scenarios to address and screening tests to remember, such as an eye exam for patients with diabetes.
Question your initial diagnosis. Beware of “premature closure”—the tendency to stop looking for other signs and symptoms once you find a presumptive diagnosis—and “diagnostic inertia”—evaluating new signs and symptoms almost exclusively on the basis of past medical history. If aspects of a patient presentation do not fit your presumed diagnosis, use a decision support system, if available, to review other possibilities.
Head off hand-off errors. Develop a problem list for each patient to reduce the likelihood that crucial information will be overlooked when more than 1 clinician is involved in his or her care. Include chronic and acute conditions, unexplained signs and symptoms, medications, and allergies. Create a fail-safe system for other potential hand-off problems, as well—requiring confirmation that the findings in a preliminary radiology report are the same as those in the final report before you take action based on the preliminary report, for example, and ensuring that you receive prompt notification whenever that is not the case.
EHRs and decision support: Isn’t it time?
In 2009, 44% of office-based physicians had EHRs, according to a Centers for Disease Control and Prevention preliminary report.22 Federal funding to promote the adoption of EHRs is expected to accelerate their use. Among the benefits of EHRs are clinical reminders, system alerts, and documentation tools that can help reduce the risk of diagnostic missteps and avert misdiagnosis lawsuits.
The Department of Veterans Affairs uses a notification system called View Alert, for example, that tracks acknowledgement of abnormal radiology test results and flags those that remain unacknowledged. 23 EHR systems can also be programmed to issue automated appointment reminders that make it easier to track patients who do not show up for critical follow-up visits.
Diagnostic decision support software adds another critical element. When a clinician inputs a set of symptoms and patient-specific data, such systems produce lists of possible diagnoses, often divided by bodily system.
While many safety advocates believe that the use of such systems will increase the likelihood of accurate diagnosis, critics point out that the software is only as good as the clinician using it. One concern is that computerized systems typically come with a “macro” ability—that is, the ability to enter large amounts of information with the click of a key. This raises the possibility that an overload of patient data, some of which may be incorrect, will be added to the medical record—or that the system will generate so many possibilities that clinicians will cease to pay attention. Both can lead to inferences of inattention or raise doubts about a physician’s credibility in a legal setting.
Electronic prescribing software systems that flag potential drug interactions are a case in point. Forty-five percent of family physicians responding to a Journal of Family Practice Instant Poll about their use of such systems reported that they override them frequently. The problem, according to 1 respondent: The system gives “so many red flags that I routinely ignore them all—like the little boy who cried wolf.”
CORRESPONDENCE John Davenport, MD, JD, 13 Redonda, Irvine, CA 92620; John.y.davenport@kp.org
• Create a problem list for each patient, including chronic and acute conditions, unexplained signs and symptoms, medications, and allergies. C
• Avoid attributing every new symptom to the patient’s documented medical conditions. C
• Develop and adhere to “don’t-miss” lists of signs and symptoms that warrant rapid action. C
• Establish a fail-safe system to ensure that you receive notification whenever a final imaging or lab report differs from the preliminary report and document your response to each abnormal result. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Misdiagnosis accounts for more malpractice claims than medication errors—indeed, for more lawsuits than any other medical misstep.1-5 Yet until recently, diagnostic errors garnered little attention from patient safety advocates.
That’s no longer the case. In 2007, the Agency for Healthcare Research and Quality (AHRQ) identified diagnostic errors (a catchall category encompassing delayed, incorrect, and missed diagnoses) as a problem that warranted closer study.6 The inaugural conference on Diagnostic Error in Medicine, cosponsored by AHRQ and the American Medical Informatics Association, took place in 2008. The third annual Diagnostic Error in Medicine conference will be held in Canada in October, reflecting the expanding focus on uncovering root causes of diagnostic error and developing preventive measures aimed at safeguarding patients and avoiding lawsuits.
Because diagnostic errors have long been underemphasized and understudied—and remain difficult to track—it is hard to know just how often they occur. Estimates of their frequency fluctuate widely from 1 study to another, but are generally in the range of 10% to 15%.7 Fatal illnesses appear to be misdiagnosed more frequently than less severe conditions: A review of more than 50 autopsy studies found that, on average, about 1 in 4 (23.5%) major diagnoses were missed.1
Whatever the numbers, diagnostic missteps are clearly common enough to be on patients’ radar screen. In a recent survey of US adults, 55% of respondents cited misdiagnosis as their greatest concern when they see a doctor in an outpatient setting.8 In a Harris Poll commissioned by the National Patient Safety Foundation9 several years earlier, 1 in 6 adults reported having had a condition that was misdiagnosed.
Evidence suggests that while years of experience and strong diagnostic skills help prevent diagnostic errors, they do not afford full protection against the cascade of events that can result in a serious diagnostic error. In fact, overconfidence may contribute to the problem.10,11
Check out the 3 legal cases in the pages that follow from the files of John Davenport, MD, JD. Dr. Davenport, a medical malpractice attorney, provided legal representation in each of these cases.
The take-away message: No physician is immune to misdiagnosis or to a subsequent lawsuit. There are, however, steps you can take to safeguard your patients and yourself, but first you need to know where the pitfalls lie.
Misdiagnosis in primary care: What malpractice claims reveal
Diagnostic errors that result in malpractice claims undergo extensive legal review. Thus, they provide an excellent opportunity for analysis, as the authors of a study of 181 “closed,” or completed, claims from 4 malpractice insurers found.12 The errors all occurred in ambulatory settings, with primary care physicians most frequently involved.
Nearly 6 in 10 of the lawsuits were for missed or delayed cancer diagnoses, followed by misdiagnosis of infection, fracture, and myocardial infarction. Overall, 24% of the cases involved breast cancer. No other disorder came close.
The most common problems, or “breakdowns,” in the diagnostic process were:
- failure to order the appropriate diagnostic test (which occurred in 55% of the cases)
- failure to create a proper follow-up plan (45%)
- failure to obtain a thorough medical history or to perform a thorough physical examination (42%).12
Notably, however, diagnostic errors rarely had a single cause. A median of 3 breakdowns per case was identified, and more than 4 in 10 cases involved more than 1 clinician.
Additional sources of breakdowns ran the gamut from patient factors (eg, non-compliance, atypical presentation, or a delay in seeking care) to system errors (eg, delay in seeing a test result, referral delay, or a mishandled handoff). Rarely was misdiagnosis attributed to a physician’s cognitive error alone. Most diagnostic errors, the authors reported, involved “a potent combination of individual and system factors.” 12
Is it cancer? Failure to test or follow up
Cancer may not be the most frequently misdiagnosed condition, but because of the dire consequences often associated with a delay in detection, cancer is No. 1 in frequency of diagnostic error lawsuits13—with breast cancer typically at or near the top of the list. Evidence suggests that clinician preconception plays a role.
Most women who develop breast cancer are over the age of 50, but plaintiffs in breast cancer suits tend to be younger.14,15 This may be partly because of overreliance on age as a predictive factor, causing some physicians to offer a younger woman what may be unwarranted reassurance that a breast lump is due to fibrocystic tissue rather than malignancy (CASE 1).
Ordering a test is not enough. Even when physicians order the correct test, follow-up may fall short. In the closed claims study, physicians incorrectly interpreted test results in 37% of the cases.12 Other evidence suggests that about a third of women with abnormal mammograms do not receive follow-up care that’s consistent with established guidelines.16
What’s more, physicians sometimes overlook the fact that diagnostic tests are rarely 100% accurate. Mammography misses approximately 20% of breast cancer cases,17 for example, and a woman with a palpable lump should be closely watched, not dismissed on the basis of a negative mammogram result.1,15
What happens to test results? In other cases, the problem is not that a test result doesn’t match the clinical findings, but that the result is not reviewed by the physician or conveyed to the patient in a timely manner. Indeed, the title of a published report of a survey of internists starts with the quote, “I wish I had seen this test result earlier!” 18 Of the 262 internists surveyed, only 41% expressed satisfaction with their method of handling test results.
What would satisfy these physicians? Respondents said what they wanted in a test result management system were tools that would help them generate letters to patients detailing the results, prioritize their workflow, and track orders for tests to completion.
A 32-year-old woman sought care for “sore breasts” 4 months postpartum. Her primary care physician found “bilateral lumpy and tender breasts,” diagnosed fibrocystic breast disease, and prescribed a nonsteroidal anti-inflammatory drug. There was no follow-up plan documented.
She returned in 4 months, stating her symptoms were better but she still had soreness in her left breast. The physician did not examine her, but changed her medication to a different anti-inflammatory. Follow-up was to “return to clinic PRN.”
On her next visit she complained of a lump in the left breast. The physician found a “spongy irregular 2 cm lump” in the upper outer quadrant of the breast, diagnosed a fibrocystic lesion, and reassured the patient. Follow-up again was to return PRN.
Several months later, the patient saw another physician, for back pain and a painful and enlarging breast lump. The physician suspected fibrocystic disease but was unable to obtain fluid by fine needle aspiration. The patient was referred to a surgeon, who obtained a nondiagnostic needle biopsy and an excisional biopsy, which revealed breast cancer. The patient’s back pain turned out to be from metastatic breast cancer. She sued for failure to diagnose breast cancer. The case was settled for an undisclosed large sum.
Commentary: Failure to diagnose breast cancer is a leading cause of malpractice lawsuits, many of them in younger women. Plaintiff recoveries correlate with the length of the delay in diagnosis.
In this case, experts identified a series of missteps in the care of this patient which, when combined with a young, very sick, and sympathetic plaintiff, led to a large recovery. Although it may have been reasonable to diagnose fibrocystic disease on the first visit, experts cited the failure to take a family history (the patient’s aunt and maternal grandmother had had breast cancer) and the failure to document a follow-up plan as damaging to the doctor’s case. They also faulted the physician for failing to examine the breast on the second visit and failing to do fine needle aspiration or refer on the third visit, and for the nonspecific follow-up plans.
Diagnostic lesson: Although breast cancer is less common in women younger than 40, it does occur, and the same diligence in examination, charting, and follow up is required regardless of the patient’s age.
By the way, doc… Harried physician, hurried response
What physician isn’t familiar with the patient who comes in for care of 1, or several, chronic conditions, but mentions another problem as he or she is getting ready to walk out the door (CASE 2)? If that problem appears to be a transient and treatable condition, the temptation is to make a hasty diagnosis and write a prescription, without the usual degree of history taking, patient examination, contemplation, or documentation. Doing so, however, poses considerable risk, to both patient and physician.
If the condition or symptom is serious enough to address in the course of the visit, it requires the same level of attention as any other presenting problem. When time constraints prevent you from addressing the complaint with the proper diligence, it would be appropriate—assuming the symptom in question is nonurgent—to ask the patient to make another appointment. But be sure to document that you did so.
A 62-year-old man saw his family physician for routine care of hypertension, diabetes, and hyperlipidemia. During the visit, the patient mentioned that he had back pain, insomnia, and a sore tongue, which the physician diagnosed as aphthous stomatitis and for which a steroidal oral cream was prescribed.
The patient was scheduled to return for a routine visit in 4 months, but did not come in until 7 months had passed—at which time the physician noted a >1 cm nodular bleeding tongue lesion. Biopsy showed squamous cell cancer, and the patient required extensive surgery, chemotherapy, and radiation. He sued for misdiagnosis and delayed diagnosis.
The physician’s defense was that given the symptoms and findings, aphthous stomatitis was a reasonable diagnosis and that he had instructed the patient to return to the office if he didn’t feel better in a few weeks. The patient disputed this. His attorney noted that the patient had multiple risk factors for tongue cancer that were not in the medical record; nor was there documentation of a tongue examination or the claimed instructions for the return visit, indicating that the patient received substandard care. The case was settled at trial for $300,000.
Commentary: The contrast between the thorough documentation for the patient’s chronic disease history and physical exam and the absence of documentation for the sore tongue suggests that this was an instance of a “by the way, doc” conversation—and a reminder of the risk that physicians assume when managing patients with multiple conditions.
Diagnostic lesson: The law does not give physicians a pass on the standard of care, regardless of how many conditions are treated in a single visit. To avoid a diagnostic error—and a potential lawsuit—a symptom-specific history, physical, and clear instructions with a follow-up plan are necessary for every condition that’s addressed.
How sure are you of the diagnosis?
It’s human nature to see things in terms of what you’re familiar with. A doctor who has been treating a patient with migraine headaches for years, for example, is apt to assume that “the worst migraine I’ve ever had” is more of the same (CASE 3). Similarly, a clinician who has identified a disorder that matches several of a patient’s symptoms may dismiss or overlook signs and symptoms that do not fit that explanation or diagnosis. Safety advocates refer to this phenomenon as “premature closure.” It may also be a function of overconfidence.
One example of physician overconfidence comes from a study in which experienced dermatologists were asked to examine lesions and diagnose melanoma. Although the specialists confidently diagnosed melanoma in more than 50% of the test cases, 30% of their decisions were later found to be incorrect.19
A 47-year-old man with a history of migraines walked into his physician’s clinic with a complaint of a severe headache. His physician was fully booked but he was given an appointment with a per diem physician. According to the patient and a friend who accompanied him, the patient told the doctor, “This is the worst migraine of my life.” The physician simply documented, “flare of migraine.” The chart indicated that the physical revealed normal vital signs and noted that the patient was “photophobic,” but that his neurological exam was “intact.”
Over the next several hours, the patient received sumatriptan and several doses of opioid analgesics. He stated that he still had a headache but felt better and was sent home with instructions to call or come in if the headache returned.
The next morning a neighbor, unable to reach the patient on the phone, went to his house and found him in a stupor, with slurred speech. The patient was taken by ambulance to a local hospital and found to have a subarachnoid hemorrhage. After weeks in the hospital and a rehabilitation center, he was left with significant cognitive and neurological impairments. He sued for failure to diagnose and won a multimillion dollar award at trial.
Commentary: Expert testimony clearly pointed to the history and physical as being substandard. Specifically, the physical should have included, among other things, a test for nuchal rigidity. Had the patient not had a history of migraines, he might have undergone a more complete medical history and physical evaluation and his symptoms would likely have been evaluated more thoroughly.
Diagnostic lesson: Be wary of “diagnostic inertia”—the tendency to depend too much on a past diagnosis when symptoms arise. Don’t be trapped into attributing all new symptoms to an old disease.
Build a no-fault, fail-safe system
The purpose of analyzing diagnostic errors is not to assign blame or point a finger at physicians, but rather to find and fix flaws in the medical system.20 That approach has been used by patient safety advocates to address other types of errors following the publication of the Institute of Medicine’s landmark report on medical error 11 years ago.21
Since then, many physician leaders have looked to the airline industry—a field in which the consequences for not strictly adhering to a fail-safe system are likely to be fatal. That reality has led to the development of vital checklists, forcing functions (in which the user is prevented from moving to the next step until the current step is completed), and computerized reminders in an attempt to eliminate, to the extent possible, the chance of human error.
The same principle can be applied to misdiagnosis. Recommended steps—ordering diagnostic tests or referring to a specialist, for example—should be put into motion whenever a set of predetermined parameters are met, rather than relying on physician memory or choice.20
Similarly, checklists should specify questions to ask or criteria to be met under specified circumstances to prevent physicians from prematurely settling on a (possibly incorrect) diagnosis. To avoid a rush to judgment, some patient safety advocates1 stress the importance of assessing the urgency of a patient’s condition, rather than trying to arrive at a definitive diagnosis the first time he or she presents with a perplexing set of signs and symptoms. Other recommendations follow:
Mandate a second look. Develop and adhere to a set of criteria to determine when a referral to a specialist or a physician consultation is needed, rather than deciding on a case-by-case basis.
Plug the holes in your follow-up system. Develop a fail-safe system for reviewing diagnostic tests or laboratory findings and reporting them to patients without delay. This can be done with an electronic health record (EHR) system or by developing and adhering to parameters requiring, for instance, that no test result get filed until there are 2 signatures on it—that of the physician who ordered the test, indicating that he or she has seen it, and that of a staff member, indicating that the patient has been notified of the results. As an additional back-up, tell patients undergoing tests when to expect to get results, and stress the importance of calling the office if they do not receive such notification within a specified time frame.
Partner with patients. Engage patients in the pursuit of a definitive diagnosis. Discuss your preliminary findings, describe your treatment decision and what you expect to occur, and urge patients to contact you with evidence that confirms or refutes that expectation. Elicit additional feedback at each visit until either the symptoms have fully resolved or you have gathered enough information to arrive at a definitive diagnosis.
Develop “don’t-miss” checklists. One list should cover diagnostic red flags to be considered anytime you see a symptomatic patient to ensure that you don’t overlook important signs and symptoms, and include findings that warrant hospital admission, specified diagnostic tests, and immediate referral. (A patient who comes in with a “common pink eye,” but has consensual photophobia, is at risk for iritis and needs an urgent ophthalmology evaluation, for instance.) Another list you should develop is a “must-do” list for well visits, featuring clinical scenarios to address and screening tests to remember, such as an eye exam for patients with diabetes.
Question your initial diagnosis. Beware of “premature closure”—the tendency to stop looking for other signs and symptoms once you find a presumptive diagnosis—and “diagnostic inertia”—evaluating new signs and symptoms almost exclusively on the basis of past medical history. If aspects of a patient presentation do not fit your presumed diagnosis, use a decision support system, if available, to review other possibilities.
Head off hand-off errors. Develop a problem list for each patient to reduce the likelihood that crucial information will be overlooked when more than 1 clinician is involved in his or her care. Include chronic and acute conditions, unexplained signs and symptoms, medications, and allergies. Create a fail-safe system for other potential hand-off problems, as well—requiring confirmation that the findings in a preliminary radiology report are the same as those in the final report before you take action based on the preliminary report, for example, and ensuring that you receive prompt notification whenever that is not the case.
EHRs and decision support: Isn’t it time?
In 2009, 44% of office-based physicians had EHRs, according to a Centers for Disease Control and Prevention preliminary report.22 Federal funding to promote the adoption of EHRs is expected to accelerate their use. Among the benefits of EHRs are clinical reminders, system alerts, and documentation tools that can help reduce the risk of diagnostic missteps and avert misdiagnosis lawsuits.
The Department of Veterans Affairs uses a notification system called View Alert, for example, that tracks acknowledgement of abnormal radiology test results and flags those that remain unacknowledged. 23 EHR systems can also be programmed to issue automated appointment reminders that make it easier to track patients who do not show up for critical follow-up visits.
Diagnostic decision support software adds another critical element. When a clinician inputs a set of symptoms and patient-specific data, such systems produce lists of possible diagnoses, often divided by bodily system.
While many safety advocates believe that the use of such systems will increase the likelihood of accurate diagnosis, critics point out that the software is only as good as the clinician using it. One concern is that computerized systems typically come with a “macro” ability—that is, the ability to enter large amounts of information with the click of a key. This raises the possibility that an overload of patient data, some of which may be incorrect, will be added to the medical record—or that the system will generate so many possibilities that clinicians will cease to pay attention. Both can lead to inferences of inattention or raise doubts about a physician’s credibility in a legal setting.
Electronic prescribing software systems that flag potential drug interactions are a case in point. Forty-five percent of family physicians responding to a Journal of Family Practice Instant Poll about their use of such systems reported that they override them frequently. The problem, according to 1 respondent: The system gives “so many red flags that I routinely ignore them all—like the little boy who cried wolf.”
CORRESPONDENCE John Davenport, MD, JD, 13 Redonda, Irvine, CA 92620; John.y.davenport@kp.org
1. Schiff GD, Kim S, Abrams R, et al. Diagnosing diagnosis errors: lessons from a multi-institutional collaborative project. Adv Patient Safety. 2005;255:255-278.
2. Sato L. Evidence-based patient safety and risk management technology. J Qual Improv. 2001;27:435.-
3. Phillips R, Bartholomew L, Dovey S, et al. Learning from malpractice claims about negligent, adverse events in primary care in the United States. Qual Saf Health Care. 2004;13:121-126.
4. Fitzgerald N. Top five causes of malpractice claims. American Physicians Assurance Corporation. 2004. Available at: http://www.apassurance.com/RiskMgt/Articles_RM/5%20Causes%20of%20Claims_RMArticle.pdf. Accessed August 2, 2010.
5. Chandra A, Nundy S, Seabury SA. The growth of physician medical malpractice payments: evidence from the National Practitioner Data Bank. Health Aff (Millwood). 2005;W5(suppl):240-249.
6. Agency for Healthcare Research and Quality Special emphasis notice (SEN): AHRQ announces interest in research on diagnostic errors in ambulatory care settings. Available at: http://grants.nih.gv/grants/guide/notice-files-NOT-HS-08-002.html. Accessed July 30, 2010.
7. Berner ES, Graber ML. Overconfidence as a cause of diagnostic error in medicine. Am J Med. 2008;121(suppl 5A):S2-S23.
8. Isabel Healthcare. Misdiagnosis is an overlooked and growing patient safety issue and core mission of Isabel Healthcare. March 20, 2006. Available at http://www.isabelhealthcare.com/pdf/USsurveyrelease-Final.pdf. Accessed August 4, 2010.
9. Golodner L. How the public perceives patient safety. Newsletter of the National Patient Safety Foundation. 2004;1997:1-6.
10. Berner ES. Diagnostic error in medicine: introduction. Adv Health Sci Educ Theory Pract. 2009;14(suppl 1):1-5.
11. Friedman CP, Gatti GG, Franz TM, et al. Do physicians know when their diagnoses are correct? Implications for decision support and error reduction. J Gen Intern Med. 2005;20:334-339.
12. Ghandi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med. 2006;145:488-496.
13. McDonald C, Hernandez MB, Gofman Y, et al. The five most common misdiagnoses: a meta-analysis of autopsy and malpractice data. Internet J Fam Pract. 2009;7(2). Available at http://www.ispub.com/journal/the_internet_journal_of_family_practice/volume_7_number_2_19/article/the-five-most-common-misdiagnosesa-meta-analysis-of-autopsy-and-malpractice-data.html. Accessed July 23, 2010.
14. Mitnick JS, Vasquez MF, Kronovet SZ, et al. Malpractice litigation involving patients with carcinoma of the breast. J Am Coll Surg. 1995;181:315-321.
15. Failure to diagnose breast cancer. Medical Malpractice Lawyers and Attorneys Online. http://www.medical-malpractice-attorneys-lawsuits.com/pages/breast-cancer.html. Accessed August 2, 2010.
16. Poon EG, Haas JS, Puopolo AL, et al. Communication factors in the follow-up of abnormal mammograms. J Gen Intern Med. 2004;19:316-323.
17. National Cancer Institute. Fact sheet. Mammograms. Available at: http://www.cancer.gov/cancertopics/factsheet/Detection/mammograms. Accessed August 3, 2010.
18. Poon EG, Gandhi TK, Sequist TD, et al. “I wish I had seen this test result earlier!”: dissatisfaction with test result management systems in primary care. Arch Intern Med. 2004;164:2223-2228.
19. Dreistl S, Binder M. Do physicians value decision support? A look at the effect of decision support on physician opinion. Artif Intell Med. 2005;33:25-30.
20. Newman-Toker DE, Pronovost PJ. Diagnostic errors: the new frontier for patient safety. JAMA. 2009;301:1060-1062.
21. Institute of Medicine. To err is human: building a safer health system. Washington, DC: November 1, 1999.
22. Centers for Disease Control and Prevention. NCHS Health E-Stat. Electronic medical record/electronic health record use by office-based physicians: United States, 2008 and preliminary 2009. Available at: http://www.cdc.gov/nchs/data/hestat/emr_ehr/emr_ehr.htm. Accessed July 30, 2010.
23. Singh H, Arora HS, Vij MS, et al. Communication outcomes of critical imaging results in a computerized notification system. J Am Med Inform Assoc. 2007;14:459-466.
1. Schiff GD, Kim S, Abrams R, et al. Diagnosing diagnosis errors: lessons from a multi-institutional collaborative project. Adv Patient Safety. 2005;255:255-278.
2. Sato L. Evidence-based patient safety and risk management technology. J Qual Improv. 2001;27:435.-
3. Phillips R, Bartholomew L, Dovey S, et al. Learning from malpractice claims about negligent, adverse events in primary care in the United States. Qual Saf Health Care. 2004;13:121-126.
4. Fitzgerald N. Top five causes of malpractice claims. American Physicians Assurance Corporation. 2004. Available at: http://www.apassurance.com/RiskMgt/Articles_RM/5%20Causes%20of%20Claims_RMArticle.pdf. Accessed August 2, 2010.
5. Chandra A, Nundy S, Seabury SA. The growth of physician medical malpractice payments: evidence from the National Practitioner Data Bank. Health Aff (Millwood). 2005;W5(suppl):240-249.
6. Agency for Healthcare Research and Quality Special emphasis notice (SEN): AHRQ announces interest in research on diagnostic errors in ambulatory care settings. Available at: http://grants.nih.gv/grants/guide/notice-files-NOT-HS-08-002.html. Accessed July 30, 2010.
7. Berner ES, Graber ML. Overconfidence as a cause of diagnostic error in medicine. Am J Med. 2008;121(suppl 5A):S2-S23.
8. Isabel Healthcare. Misdiagnosis is an overlooked and growing patient safety issue and core mission of Isabel Healthcare. March 20, 2006. Available at http://www.isabelhealthcare.com/pdf/USsurveyrelease-Final.pdf. Accessed August 4, 2010.
9. Golodner L. How the public perceives patient safety. Newsletter of the National Patient Safety Foundation. 2004;1997:1-6.
10. Berner ES. Diagnostic error in medicine: introduction. Adv Health Sci Educ Theory Pract. 2009;14(suppl 1):1-5.
11. Friedman CP, Gatti GG, Franz TM, et al. Do physicians know when their diagnoses are correct? Implications for decision support and error reduction. J Gen Intern Med. 2005;20:334-339.
12. Ghandi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med. 2006;145:488-496.
13. McDonald C, Hernandez MB, Gofman Y, et al. The five most common misdiagnoses: a meta-analysis of autopsy and malpractice data. Internet J Fam Pract. 2009;7(2). Available at http://www.ispub.com/journal/the_internet_journal_of_family_practice/volume_7_number_2_19/article/the-five-most-common-misdiagnosesa-meta-analysis-of-autopsy-and-malpractice-data.html. Accessed July 23, 2010.
14. Mitnick JS, Vasquez MF, Kronovet SZ, et al. Malpractice litigation involving patients with carcinoma of the breast. J Am Coll Surg. 1995;181:315-321.
15. Failure to diagnose breast cancer. Medical Malpractice Lawyers and Attorneys Online. http://www.medical-malpractice-attorneys-lawsuits.com/pages/breast-cancer.html. Accessed August 2, 2010.
16. Poon EG, Haas JS, Puopolo AL, et al. Communication factors in the follow-up of abnormal mammograms. J Gen Intern Med. 2004;19:316-323.
17. National Cancer Institute. Fact sheet. Mammograms. Available at: http://www.cancer.gov/cancertopics/factsheet/Detection/mammograms. Accessed August 3, 2010.
18. Poon EG, Gandhi TK, Sequist TD, et al. “I wish I had seen this test result earlier!”: dissatisfaction with test result management systems in primary care. Arch Intern Med. 2004;164:2223-2228.
19. Dreistl S, Binder M. Do physicians value decision support? A look at the effect of decision support on physician opinion. Artif Intell Med. 2005;33:25-30.
20. Newman-Toker DE, Pronovost PJ. Diagnostic errors: the new frontier for patient safety. JAMA. 2009;301:1060-1062.
21. Institute of Medicine. To err is human: building a safer health system. Washington, DC: November 1, 1999.
22. Centers for Disease Control and Prevention. NCHS Health E-Stat. Electronic medical record/electronic health record use by office-based physicians: United States, 2008 and preliminary 2009. Available at: http://www.cdc.gov/nchs/data/hestat/emr_ehr/emr_ehr.htm. Accessed July 30, 2010.
23. Singh H, Arora HS, Vij MS, et al. Communication outcomes of critical imaging results in a computerized notification system. J Am Med Inform Assoc. 2007;14:459-466.