User login
Hypothyroidism—even when occult or subclinical—can cause subtle or frank changes in energy, mood, anxiety level, or cognition. Some patients’ affective symptoms remit with thyroid hormone replacement or with antidepressants only after a euthyroid state is established.
To help you recognize hypothyroidism in patients presenting with psychiatric illnesses and provide effective treatment, this article describes:
- hypothyroidism’s signs and symptoms
- primary and subclinical hypothyroidism, thyroiditis, central hypothyroidism, and thyroid hormone resistance
- laboratory screening for thyroid dysfunction in patients with psychiatric symptoms.
Overlapping clinical signs
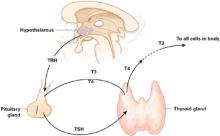
Thyroid hormone is required for the metabolic activity of every cell in the body. When patients experience symptoms related to abnormal functioning of the hypothalamic-pituitary-thyroid axis (Figure), psychiatrists often are the first professionals they consult.
Diagnosis of thyroid disorders is based on biochemical and clinical data (Box 1),1 which might not be congruent. Clinical symptoms of hypothyroidism, for example, are notoriously variable. Severe biochemical hypothyroidism may be associated with mild clinical symptoms, whereas mild biochemical hypothyroidism may be associated with severe symptoms.2
Patients with thyroid disturbance and psychiatric symptoms most often are diagnosed with a depressive-spectrum syndrome. Most common are:
- atypical depression (which may present as dysthymia)
- bipolar spectrum syndrome (including manic-depression, mixed mania, bipolar depression, rapid-cycling bipolar disorder, cyclothymia, and premenstrual syndromes)
- borderline personality disorder
- or psychotic disorder (typically paranoid psychosis).
Psychiatric symptoms of hypothyroidism (Table 1) are often prominent or even primary. Patients commonly show:
- impaired attention, concentration, learning, and memory
- psychomotor slowing
- and/or mental dullness.
Table 1
Hypothyroidism’s psychiatric signs and symptoms
| Cognitive changes | Impaired memory, psychomotor slowing, reduced attention span |
| Vegetative symptoms | Hypersomnia, sleep apnea, fatigue, lethargy, apathy, anergia, low libido |
| Mood changes | Depression, mood instability, mania, anxiety |
| Other | Psychosis |
Psychiatric patients—particularly those with mood disorders—are more likely to exhibit biochemical evidence of frank or subclinical hypothyroidism, hyperthyroidism, and autoimmune thyroiditis than the general population. In a study of 17,533 Americans,1 approximately 12% had thyroid abnormalities and 80% of these were hypothyroid. An additional 17% of women and 9% of men tested positive for antithyroid antibodies.
Biochemical hypothyroidism was defined as TSH >4.5 mIU/L, with low total T4, and subclinical hypothyroidism as TSH >4.5 mIU/L with normal T4 levels. Population studies and other data have led some endocrinologists to regard serum TSH levels >2.5 mIU/L as abnormally high.
Figure Thyroid hormone regulation: The hypothalamic-pituitary-thyroid axis
Thyroid-stimulating hormone (TSH, thyrotropin) released into circulation by the pituitary stimulates the thyroid to synthesize and release thyroid hormone, including triiodothyronine (T3) and thyroxine (T4). TSH is regulated by hypothalamic elaboration of thyrotropin-releasing hormone (TRH), which stimulates TSH release in a dose-dependent manner. Negative feedback from T3 and T4 downregulates TRH gene expression and restrains the pituitary from responding to TSH. Most T3—the active hormone—is formed in circulation or in target tissues by deiodination of T4 by selenium-containing enzymes.
Illustration for Current Psychiatry by Rich LaroccoThe degree of impairment may depend on the patient’s normal functional level. For example, a well-educated patient of mine with thyroiditis-related hypothyroidism reported word-finding difficulties. Instead of asking her husband to take a bottle of wine from the rack, she asked him to take a bottle of wine from the “thing.”
Loss of vitality, fatigue, lethargy, hypersomnia (especially if sleep apnea is present), and depressed mood also are commonly seen.
Depressive symptoms. Hypothyroid patients usually meet several criteria for a major depressive episode—such as concentration difficulties, lassitude, low libido, and sometimes pessimism or sadness—and symptoms improve after sustained thyroid hormone replacement therapy.3 Women with mild hypothyroidism who screen negative for a psychiatric syndrome show statistically significant mood improvement and improved verbal fluency after 6 months of levothyroxine replacement therapy.4
In some patients with no clear evidence of a biochemical or clinical thyroid disorder, mood symptoms nevertheless respond to thyroid hormone augmentation of antidepressants.5
Anxiety symptoms. Occasionally thyroid dysfunction is seen in patients with anxiety disorders, including panic disorder, agoraphobia, social phobia, performance anxiety, post-traumatic stress disorder, and generalized anxiety disorder.6
It may seem counterintuitive, but hypothyroidism is probably as common as hyperthyroidism in extremely anxious patients. Both hypoand hyperthyroidism are seen much more often in patients with panic-level anxiety than in the general population.
In a sample of 144 consecutive female psychiatric patients with a lifetime history of panic disorder and/or agoraphobia:
- 27% had a history of thyroid disorder
- 17% had hypothyroidism
- 8% had hyperthyroidism.7
Hypothyroid symptoms. Associated symptoms of hypothyroidism (Table 2) may include cold intolerance, lack of or reduced perspiration, dry skin, constipation, lethargy, psychomotor slowness, and subjective paresthesias and muscle pains. Edema is often present. The face typically is swollen or “puffy” in the morning, but by evening the lower legs (and not the face) are edematous.
Deep tendon reflexes usually relax slowly after initial stimulation. Vascular resistance is increased, but hypertension is not usual. Noradrenergic systems become more active in a compensatory, counter-regulatory manner; however, bradycardia—when present—is sometimes profound. Weight gain can occur but often is conspicuously absent.
Severe hypothyroidism presents with paradoxical tremendous agitation, paranoia, and aggressiveness. The skin is leathery, and facies are characteristically rough. Myxedema is fairly common, even in high-functioning patients. I have seen only one case of so-called “myxedema madness;” the female patient’s hyperarousal, yelling, cursing, grossly poor cognitive ability, and loosely conceived paranoid delusions are unforgettable.
Galactorrhea (related to hyperprolactinemia) can be a symptom of severe hypothyroidism, presumably from increased hypothalamic thyrotropin-releasing hormone (TRH) drive. TRH is the main known secretagogue for pituitary prolactin secretion. Infertility, oligomenorrhea, or amenorrhea could be part of the hypothyroid clinical picture.
Other symptoms. Macroglossia and hypertrophy of the uvula are possible; in a recent report, dysarthria resulting from these oral changes was the only presenting symptom of a hypothyroid man.8 Dysarthria promptly corrected after levothyroxine replacement.
Hypothyroidism is a primary cause of central sleep apnea caused by dysfunction of ventilatory control and/or reduction in airway aperture.
Table 2
Hypothyroidism’s other signs and symptoms
| Metabolic | Low basal body temperature/cool skin, diminished perspiration, weight gain or difficulty losing weight |
| Cardiovascular | Bradycardia, dizziness |
| Dermatologic | Dry, rough, or scaly skin; brittle nails; coarse or thinning hair (especially in women); pallor; dependent edema; myxedema/skin mucinosis (classically pretibial) |
| Digestive | Nausea, constipation, enlarged tongue |
| Reproductive | Oligomenorrhea, amenorrhea, infertility, miscarriage, delayed ejaculation |
| Musculoskeletal and peripheral nervous system | Muscle cramps, joint pain, paresthesias, numbness, weakness, reduced exercise tolerance, delayed ankle reflex |
| Sensory | Upper eyelid drooping, dysarthria, hoarseness, diminished hearing, diminished taste (hypogustia) |
Causes of thyroid disorders
Primary hypothyroidism results from thyroid gland failure. The many causes include iodine deficiency, but most cases of adult-onset or acquired hypothyroidism are attributed to autoimmune thyroiditis. In primary hypothyroidism, low serum T4 and/or T3 are seen in combination with elevated serum TSH. Circulating free T4 diminishes sooner than free T3 does as the body attempts to preserve active hormone levels. In turn, total T4 and T3 diminish sooner than free hormone concentrations. A compensatory increase in pituitary-elaborated TSH is seen as the brain and pituitary attempt to stimulate the thyroid to produce adequate thyroid hormone.
In subclinical hypothyroidism, circulating free thyroid hormone concentrations are within the normal laboratory range (typically in the lower range), but TSH is elevated. TSH concentrations >3.0 mIU/mL call for repeat or follow-up biochemistry and clinical correlation.
The decision to treat subclinical hypothyroidism with thyroid hormone replacement is less controversial in psychiatry than in endocrinology. Psychiatric patients with subclinical hypothyroidism—especially those with incomplete responses to psychotropic therapy—should usually be treated with thyroid hormone (Box 2).1
Free T3 levels in the lower 20% of the laboratory’s normal range are cause for pause in a patient with a mood or psychotic disorder and any of hypothyroidism’s clinical stigmata, even if thyroxine and TSH concentrations are normal.
Thyroiditis is characterized by thyroid gland inflammation. The thyroid may be painful or nonpainful, enlarged, fleshy, goitrous, normal in size, or atrophic and fibrotic (especially late in the course).
Postulated precipitants include viruses and other infectious agents, vaccines, iodine excess, lithium therapy (Box 3),9 tobacco smoke, environmental chemicals or toxins, irradiation, and—arguably—cortically-mediated (psychological) stress in vulnerable individuals.
Clinically, thyroiditis syndromes often have a long prodromal phase, wax and wane in severity, have an insidious and sometimes silent course, and can be serially associated with hyperthyroidism (especially early in the course), euthyroidism, or hypothyroidism (especially late in the course). Most thyroiditis syndromes appear to resolve spontaneously, but many become chronic or show evidence of subtle thyroid dysfunction years after the first occurrence or diagnosis.
Most presentations are nonspecific; symptoms may be limited to lethargy, fatigue, and depression. Increased antithyroid antibody titers have been linked with psychotic and depressive syndromes in borderline personality disorder.10
In early thyroiditis, thyroxine and triiodothyronine secretion is often elevated, with low or suppressed TSH. However, antithyroid antibody production is associated with a significantly increased risk of eventual subclinical or frank hypothyroidism. Permanent hypothyroidism develops eventually in at least one-half of women with histories of postpartum thyroiditis.11
Central hypothyroidism stems from TSH deficiency. Both pituitary thyrotrophic failure and hypothalamic failure—secondary and tertiary hypothyroidism, respectively—are considered central (or “secondary”). Hypothyroidism of pituitary and hypothalamic origins are lumped together as “central” because it is often very difficult to differentiate these pathologies.
Thyroid hormone resistance, in which end-organ or cellular resistance to thyroid hormone signals is seen, is an increasingly recognized syndrome in clinical medicine. The typical case is an euthyroid or hypothyroid individual with elevated T4 and T3 and nonsuppressed or even frankly elevated TSH. Inappropriately elevated TSH combined with high thyroid hormone levels also can be seen in TSH-secreting pituitary tumors, although the clinical picture in this case is one of hyperthyroidism.
Thyroid hormone resistance ranges from euthyroid and clinically transparent to profoundly hypothyroid, and different organs in the same patient may show different sensitivities to thyroid hormone. Clinical features vary, depending on the strength of thyroid hormone resistance.
Early emergence of resistance (as would be expected in someone with an inherited thyroid hormone receptor abnormality) leads to developmental problems, including:
- short stature
- mental or learning disabilities (including attention deficits).
In a study of 18 families with strong history of generalized resistance to thyroid hormone, 70% of affected children met diagnostic criteria for attention-deficit/hyperactivity disorder.12
Target psychiatric symptoms for prescribing replacement thyroid hormone are depression; mood cycling or instability; low energy, fatigue, or lethargy; cognitive impairment (Table 1); and psychosis, if present. Because these symptoms are not specific to thyroid dysfunction, institute thyroid hormone only when biochemical evidence of compromised or suboptimal thyroid function is also present.
Exceptions to this rule may include patients with target psychiatric symptoms and:
Patients taking lithium for mood stabilization will likely need supplemental thyroid hormone eventually because lithium is thyrotoxic. Also, patients with bipolar mood symptoms often have coexisting thyroid abnormalities, and giving supraphysiologic thyroid hormone dosages sometimes converts those who do not respond to mood stabilizers into responders.
Thyrotropin concentrations increase within 1 day after patients start taking lithium carbonate, but without commensurate increases in T3 or T4. More often, T3 and T4 concentrations decrease in the presence of lithium. Among 150 patients maintained on lithium for 10 years, hypothyroidism, autoimmune thyroiditis, or goiter developed at rates of 1.7%, 1.4%, and 2.1% per year, respectively. The study authors suggested that long-term lithium may increase the risk for hypothyroidism in women and in patients with thyroid autoimmunity.9
Laboratory screening
TSH and thyroid hormones. The basic thyroid screen is a combination of serum levels of TSH (“sensitive TSH”) and free thyroid hormones.
TSH has a circadian rhythm, with a nocturnal surge amounting to a 50% to 200% increase over daytime levels, beginning at around 6 to 8 PM. Peak TSH pulsatile activity and levels are seen after sleep begins—usually after midnight—with trough levels and fewest TSH pulses in late morning and early afternoon.13,14 This rhythm implies that the most accurate TSH measurement may be obtained by drawing blood in the morning before 9 AM. I have seen subclinical hypothyroidism missed when clinicians relied on afternoon TSH levels.
In general medicine, TSH alone frequently is used as a routine screening tool. In psychiatric practice, however, I recommend supplementing TSH with free T3 and free T4 because thyroid system dysfunction is frequent in psychiatric syndromes. If laboratory costs are a concern, free T4 with TSH usually suffices for initial screening.
Although the unbound, free fractions of T3 and T4 are of primary interest, total T4 and total T3 are necessary to assess the thyroid gland’s synthetic capacity. When clinical evidence suggests abnormal thyroid hormone function, order repeated or serial biochemical testing. Marginal biochemical results also mandate repeat thyroid function studies, expanded to include:
- total thyroid hormone concentrations (ideally T4 and T3)
- antithyroid antibodies
- serum cholesterol
- prolactin.
Antithyroid antibodies. Obtain antithyroglobulin and antithyroid microsomal antibody titers if:
- thyroid hormone indices are abnormal or marginal—in either direction
- or the patient now has, has had, or has a family history of autoimmune-mediated symptoms, such as lupus erythematosus or rheumatoid arthritis.
Negative or low antithyroid autoantibody titers do not rule out thyroiditis as a cause of hypothyroidism, as these titers are most likely to be generated during periods of active inflammation.
Many autoantibodies react with thyroid-related elements. Most clinical laboratories can quantify antibodies directed against thyroid peroxidase—also called antimicrosomal antibodies—and thyroglobulin. The presence of these antibodies is associated with thyroid inflammation and a risk of progression to thyroid failure and hypothyroidism.
Other laboratory findings of hypothyroidism include hypercholesterolemia, mild hyperprolactinemia, and types of anemia (including iron-deficiency anemia with low ferritin levels).
Related resources
- American Thyroid Association. www.thyroid.org.
- Dunn JT. Guarding our nation’s thyroid health. J Clin Endocrinol Metab 2001;872:486-8.
- Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med 2003;348:2646-55.
- Sullivan GM, Mann JJ, Oquendo MA, et al. Low cerebrospinal fluid transthyretin levels in depression: correlations with suicidal ideation and low serotonin function. Biol Psychiatry 2006;60(5):500-6.
1. Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 2002;87:489-99.
2. Zulewski H, Muller B, Exer P, et al. Estimation of tissue hypothyroidism by a new clinical score: evaluation of patients with various grades of hypothyroidism and controls. J Clin Endocrinol Metab 1997;82:771-6.
3. Gunnarsson T, Sjoberg S, Eriksson M, Nordin C. Depressive symptoms in hyothyroid disorder with some observations on biochemical correlates. Neuropsychobiology 2001;43:70-4.
4. Bono G, Fancellu R, Blandini F, Santor G, Mauri M. Cognitive and affective status in mild hypothyroidism and interactions with L-thyroxine treatment. Acta Neurol Scand 2004;110:59-66
5. Iosifescu DV. ‘Supercharge’ antidepressants by adding thyroid hormones: Why hormones help, and new data on SSRI augmentation. Current Psychiatry 2006;5(7):15-25.
6. Tancer ME, Stein MB, Gelernter CS, Uhde TW. The hypothalamic-pituitary-thyroid axis in social phobia. Am J Psychiatry 1990;147(7):929-33
7. Orenstein H, Peskind A, Raskind MA. Thyroid disorders in female psychiatric patients with panic disorder or agoraphobia. Am J Psychiatry 1988;145:1428-30.
8. Stollberger C, Finsterer J, Brand E, Tschabitscher D. Dysarthria as the leading symptom of hypothyroidism. Am J Otolaryngol 2001;22:70-2.
9. Bocchetta A, Mossa P, Velluzzi F, et al. Ten-year follow-up of thyroid function in lithium patients. J Clin Psychopharmacol 2001;21(6):594-8.
10. Geracioti TD, Kling MA, Post R, Gold PW. Antithyroid antibody-linked symptoms in borderline personality disorder. Endocrine 2003;21:153-8.
11. Premawardhana LD, Parkes AB, Ammari F, et al. Postpartum thyroiditis and long-term thyroid status: prognostic influence of thyroid peroxidase antibodies and ultrasound echogenicity. J Clin Endocrinol Metab 2000;85:71-5.
12. Hauser P, Zametkin AJ, Martinez P, et al. Attention deficithyperactivity disorder in people with generalized resistance to thyroid hormone. N Engl J Med 1993;328:997-1001.
13. Ghizzoni L, Mastorakos G, Ziveri M, et al. Interactions of leptin and thyrotropin 24-hour secretory profiles in short normal children. J Clin Endocrinol Metab 2001;86(5):2065-72.
14. Mantzoros CS, Ozata M, Negrao AB, et al. Synchronicity of frequently sampled thyrotropin (TSH) and leptin concentrations in healthy adults and leptin-deficient subjects: evidence for possible partial TSH regulation by leptin in humans. J Clin Endocrinol Metab 2001;86(7):3284-91.
15. Chopra IJ, Sabatino L. Nature and sources of circulating thyroid hormones. In: Braverman LE, Utiger RD, eds. The thyroid. A fundamental and clinical text. Philadelphia: Lippincott; 2000:120-35.
Hypothyroidism—even when occult or subclinical—can cause subtle or frank changes in energy, mood, anxiety level, or cognition. Some patients’ affective symptoms remit with thyroid hormone replacement or with antidepressants only after a euthyroid state is established.
To help you recognize hypothyroidism in patients presenting with psychiatric illnesses and provide effective treatment, this article describes:
- hypothyroidism’s signs and symptoms
- primary and subclinical hypothyroidism, thyroiditis, central hypothyroidism, and thyroid hormone resistance
- laboratory screening for thyroid dysfunction in patients with psychiatric symptoms.
Overlapping clinical signs
Thyroid hormone is required for the metabolic activity of every cell in the body. When patients experience symptoms related to abnormal functioning of the hypothalamic-pituitary-thyroid axis (Figure), psychiatrists often are the first professionals they consult.
Diagnosis of thyroid disorders is based on biochemical and clinical data (Box 1),1 which might not be congruent. Clinical symptoms of hypothyroidism, for example, are notoriously variable. Severe biochemical hypothyroidism may be associated with mild clinical symptoms, whereas mild biochemical hypothyroidism may be associated with severe symptoms.2
Patients with thyroid disturbance and psychiatric symptoms most often are diagnosed with a depressive-spectrum syndrome. Most common are:
- atypical depression (which may present as dysthymia)
- bipolar spectrum syndrome (including manic-depression, mixed mania, bipolar depression, rapid-cycling bipolar disorder, cyclothymia, and premenstrual syndromes)
- borderline personality disorder
- or psychotic disorder (typically paranoid psychosis).
Psychiatric symptoms of hypothyroidism (Table 1) are often prominent or even primary. Patients commonly show:
- impaired attention, concentration, learning, and memory
- psychomotor slowing
- and/or mental dullness.
Table 1
Hypothyroidism’s psychiatric signs and symptoms
| Cognitive changes | Impaired memory, psychomotor slowing, reduced attention span |
| Vegetative symptoms | Hypersomnia, sleep apnea, fatigue, lethargy, apathy, anergia, low libido |
| Mood changes | Depression, mood instability, mania, anxiety |
| Other | Psychosis |
Psychiatric patients—particularly those with mood disorders—are more likely to exhibit biochemical evidence of frank or subclinical hypothyroidism, hyperthyroidism, and autoimmune thyroiditis than the general population. In a study of 17,533 Americans,1 approximately 12% had thyroid abnormalities and 80% of these were hypothyroid. An additional 17% of women and 9% of men tested positive for antithyroid antibodies.
Biochemical hypothyroidism was defined as TSH >4.5 mIU/L, with low total T4, and subclinical hypothyroidism as TSH >4.5 mIU/L with normal T4 levels. Population studies and other data have led some endocrinologists to regard serum TSH levels >2.5 mIU/L as abnormally high.
Figure Thyroid hormone regulation: The hypothalamic-pituitary-thyroid axis
Thyroid-stimulating hormone (TSH, thyrotropin) released into circulation by the pituitary stimulates the thyroid to synthesize and release thyroid hormone, including triiodothyronine (T3) and thyroxine (T4). TSH is regulated by hypothalamic elaboration of thyrotropin-releasing hormone (TRH), which stimulates TSH release in a dose-dependent manner. Negative feedback from T3 and T4 downregulates TRH gene expression and restrains the pituitary from responding to TSH. Most T3—the active hormone—is formed in circulation or in target tissues by deiodination of T4 by selenium-containing enzymes.
Illustration for Current Psychiatry by Rich LaroccoThe degree of impairment may depend on the patient’s normal functional level. For example, a well-educated patient of mine with thyroiditis-related hypothyroidism reported word-finding difficulties. Instead of asking her husband to take a bottle of wine from the rack, she asked him to take a bottle of wine from the “thing.”
Loss of vitality, fatigue, lethargy, hypersomnia (especially if sleep apnea is present), and depressed mood also are commonly seen.
Depressive symptoms. Hypothyroid patients usually meet several criteria for a major depressive episode—such as concentration difficulties, lassitude, low libido, and sometimes pessimism or sadness—and symptoms improve after sustained thyroid hormone replacement therapy.3 Women with mild hypothyroidism who screen negative for a psychiatric syndrome show statistically significant mood improvement and improved verbal fluency after 6 months of levothyroxine replacement therapy.4
In some patients with no clear evidence of a biochemical or clinical thyroid disorder, mood symptoms nevertheless respond to thyroid hormone augmentation of antidepressants.5
Anxiety symptoms. Occasionally thyroid dysfunction is seen in patients with anxiety disorders, including panic disorder, agoraphobia, social phobia, performance anxiety, post-traumatic stress disorder, and generalized anxiety disorder.6
It may seem counterintuitive, but hypothyroidism is probably as common as hyperthyroidism in extremely anxious patients. Both hypoand hyperthyroidism are seen much more often in patients with panic-level anxiety than in the general population.
In a sample of 144 consecutive female psychiatric patients with a lifetime history of panic disorder and/or agoraphobia:
- 27% had a history of thyroid disorder
- 17% had hypothyroidism
- 8% had hyperthyroidism.7
Hypothyroid symptoms. Associated symptoms of hypothyroidism (Table 2) may include cold intolerance, lack of or reduced perspiration, dry skin, constipation, lethargy, psychomotor slowness, and subjective paresthesias and muscle pains. Edema is often present. The face typically is swollen or “puffy” in the morning, but by evening the lower legs (and not the face) are edematous.
Deep tendon reflexes usually relax slowly after initial stimulation. Vascular resistance is increased, but hypertension is not usual. Noradrenergic systems become more active in a compensatory, counter-regulatory manner; however, bradycardia—when present—is sometimes profound. Weight gain can occur but often is conspicuously absent.
Severe hypothyroidism presents with paradoxical tremendous agitation, paranoia, and aggressiveness. The skin is leathery, and facies are characteristically rough. Myxedema is fairly common, even in high-functioning patients. I have seen only one case of so-called “myxedema madness;” the female patient’s hyperarousal, yelling, cursing, grossly poor cognitive ability, and loosely conceived paranoid delusions are unforgettable.
Galactorrhea (related to hyperprolactinemia) can be a symptom of severe hypothyroidism, presumably from increased hypothalamic thyrotropin-releasing hormone (TRH) drive. TRH is the main known secretagogue for pituitary prolactin secretion. Infertility, oligomenorrhea, or amenorrhea could be part of the hypothyroid clinical picture.
Other symptoms. Macroglossia and hypertrophy of the uvula are possible; in a recent report, dysarthria resulting from these oral changes was the only presenting symptom of a hypothyroid man.8 Dysarthria promptly corrected after levothyroxine replacement.
Hypothyroidism is a primary cause of central sleep apnea caused by dysfunction of ventilatory control and/or reduction in airway aperture.
Table 2
Hypothyroidism’s other signs and symptoms
| Metabolic | Low basal body temperature/cool skin, diminished perspiration, weight gain or difficulty losing weight |
| Cardiovascular | Bradycardia, dizziness |
| Dermatologic | Dry, rough, or scaly skin; brittle nails; coarse or thinning hair (especially in women); pallor; dependent edema; myxedema/skin mucinosis (classically pretibial) |
| Digestive | Nausea, constipation, enlarged tongue |
| Reproductive | Oligomenorrhea, amenorrhea, infertility, miscarriage, delayed ejaculation |
| Musculoskeletal and peripheral nervous system | Muscle cramps, joint pain, paresthesias, numbness, weakness, reduced exercise tolerance, delayed ankle reflex |
| Sensory | Upper eyelid drooping, dysarthria, hoarseness, diminished hearing, diminished taste (hypogustia) |
Causes of thyroid disorders
Primary hypothyroidism results from thyroid gland failure. The many causes include iodine deficiency, but most cases of adult-onset or acquired hypothyroidism are attributed to autoimmune thyroiditis. In primary hypothyroidism, low serum T4 and/or T3 are seen in combination with elevated serum TSH. Circulating free T4 diminishes sooner than free T3 does as the body attempts to preserve active hormone levels. In turn, total T4 and T3 diminish sooner than free hormone concentrations. A compensatory increase in pituitary-elaborated TSH is seen as the brain and pituitary attempt to stimulate the thyroid to produce adequate thyroid hormone.
In subclinical hypothyroidism, circulating free thyroid hormone concentrations are within the normal laboratory range (typically in the lower range), but TSH is elevated. TSH concentrations >3.0 mIU/mL call for repeat or follow-up biochemistry and clinical correlation.
The decision to treat subclinical hypothyroidism with thyroid hormone replacement is less controversial in psychiatry than in endocrinology. Psychiatric patients with subclinical hypothyroidism—especially those with incomplete responses to psychotropic therapy—should usually be treated with thyroid hormone (Box 2).1
Free T3 levels in the lower 20% of the laboratory’s normal range are cause for pause in a patient with a mood or psychotic disorder and any of hypothyroidism’s clinical stigmata, even if thyroxine and TSH concentrations are normal.
Thyroiditis is characterized by thyroid gland inflammation. The thyroid may be painful or nonpainful, enlarged, fleshy, goitrous, normal in size, or atrophic and fibrotic (especially late in the course).
Postulated precipitants include viruses and other infectious agents, vaccines, iodine excess, lithium therapy (Box 3),9 tobacco smoke, environmental chemicals or toxins, irradiation, and—arguably—cortically-mediated (psychological) stress in vulnerable individuals.
Clinically, thyroiditis syndromes often have a long prodromal phase, wax and wane in severity, have an insidious and sometimes silent course, and can be serially associated with hyperthyroidism (especially early in the course), euthyroidism, or hypothyroidism (especially late in the course). Most thyroiditis syndromes appear to resolve spontaneously, but many become chronic or show evidence of subtle thyroid dysfunction years after the first occurrence or diagnosis.
Most presentations are nonspecific; symptoms may be limited to lethargy, fatigue, and depression. Increased antithyroid antibody titers have been linked with psychotic and depressive syndromes in borderline personality disorder.10
In early thyroiditis, thyroxine and triiodothyronine secretion is often elevated, with low or suppressed TSH. However, antithyroid antibody production is associated with a significantly increased risk of eventual subclinical or frank hypothyroidism. Permanent hypothyroidism develops eventually in at least one-half of women with histories of postpartum thyroiditis.11
Central hypothyroidism stems from TSH deficiency. Both pituitary thyrotrophic failure and hypothalamic failure—secondary and tertiary hypothyroidism, respectively—are considered central (or “secondary”). Hypothyroidism of pituitary and hypothalamic origins are lumped together as “central” because it is often very difficult to differentiate these pathologies.
Thyroid hormone resistance, in which end-organ or cellular resistance to thyroid hormone signals is seen, is an increasingly recognized syndrome in clinical medicine. The typical case is an euthyroid or hypothyroid individual with elevated T4 and T3 and nonsuppressed or even frankly elevated TSH. Inappropriately elevated TSH combined with high thyroid hormone levels also can be seen in TSH-secreting pituitary tumors, although the clinical picture in this case is one of hyperthyroidism.
Thyroid hormone resistance ranges from euthyroid and clinically transparent to profoundly hypothyroid, and different organs in the same patient may show different sensitivities to thyroid hormone. Clinical features vary, depending on the strength of thyroid hormone resistance.
Early emergence of resistance (as would be expected in someone with an inherited thyroid hormone receptor abnormality) leads to developmental problems, including:
- short stature
- mental or learning disabilities (including attention deficits).
In a study of 18 families with strong history of generalized resistance to thyroid hormone, 70% of affected children met diagnostic criteria for attention-deficit/hyperactivity disorder.12
Target psychiatric symptoms for prescribing replacement thyroid hormone are depression; mood cycling or instability; low energy, fatigue, or lethargy; cognitive impairment (Table 1); and psychosis, if present. Because these symptoms are not specific to thyroid dysfunction, institute thyroid hormone only when biochemical evidence of compromised or suboptimal thyroid function is also present.
Exceptions to this rule may include patients with target psychiatric symptoms and:
Patients taking lithium for mood stabilization will likely need supplemental thyroid hormone eventually because lithium is thyrotoxic. Also, patients with bipolar mood symptoms often have coexisting thyroid abnormalities, and giving supraphysiologic thyroid hormone dosages sometimes converts those who do not respond to mood stabilizers into responders.
Thyrotropin concentrations increase within 1 day after patients start taking lithium carbonate, but without commensurate increases in T3 or T4. More often, T3 and T4 concentrations decrease in the presence of lithium. Among 150 patients maintained on lithium for 10 years, hypothyroidism, autoimmune thyroiditis, or goiter developed at rates of 1.7%, 1.4%, and 2.1% per year, respectively. The study authors suggested that long-term lithium may increase the risk for hypothyroidism in women and in patients with thyroid autoimmunity.9
Laboratory screening
TSH and thyroid hormones. The basic thyroid screen is a combination of serum levels of TSH (“sensitive TSH”) and free thyroid hormones.
TSH has a circadian rhythm, with a nocturnal surge amounting to a 50% to 200% increase over daytime levels, beginning at around 6 to 8 PM. Peak TSH pulsatile activity and levels are seen after sleep begins—usually after midnight—with trough levels and fewest TSH pulses in late morning and early afternoon.13,14 This rhythm implies that the most accurate TSH measurement may be obtained by drawing blood in the morning before 9 AM. I have seen subclinical hypothyroidism missed when clinicians relied on afternoon TSH levels.
In general medicine, TSH alone frequently is used as a routine screening tool. In psychiatric practice, however, I recommend supplementing TSH with free T3 and free T4 because thyroid system dysfunction is frequent in psychiatric syndromes. If laboratory costs are a concern, free T4 with TSH usually suffices for initial screening.
Although the unbound, free fractions of T3 and T4 are of primary interest, total T4 and total T3 are necessary to assess the thyroid gland’s synthetic capacity. When clinical evidence suggests abnormal thyroid hormone function, order repeated or serial biochemical testing. Marginal biochemical results also mandate repeat thyroid function studies, expanded to include:
- total thyroid hormone concentrations (ideally T4 and T3)
- antithyroid antibodies
- serum cholesterol
- prolactin.
Antithyroid antibodies. Obtain antithyroglobulin and antithyroid microsomal antibody titers if:
- thyroid hormone indices are abnormal or marginal—in either direction
- or the patient now has, has had, or has a family history of autoimmune-mediated symptoms, such as lupus erythematosus or rheumatoid arthritis.
Negative or low antithyroid autoantibody titers do not rule out thyroiditis as a cause of hypothyroidism, as these titers are most likely to be generated during periods of active inflammation.
Many autoantibodies react with thyroid-related elements. Most clinical laboratories can quantify antibodies directed against thyroid peroxidase—also called antimicrosomal antibodies—and thyroglobulin. The presence of these antibodies is associated with thyroid inflammation and a risk of progression to thyroid failure and hypothyroidism.
Other laboratory findings of hypothyroidism include hypercholesterolemia, mild hyperprolactinemia, and types of anemia (including iron-deficiency anemia with low ferritin levels).
Related resources
- American Thyroid Association. www.thyroid.org.
- Dunn JT. Guarding our nation’s thyroid health. J Clin Endocrinol Metab 2001;872:486-8.
- Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med 2003;348:2646-55.
- Sullivan GM, Mann JJ, Oquendo MA, et al. Low cerebrospinal fluid transthyretin levels in depression: correlations with suicidal ideation and low serotonin function. Biol Psychiatry 2006;60(5):500-6.
Hypothyroidism—even when occult or subclinical—can cause subtle or frank changes in energy, mood, anxiety level, or cognition. Some patients’ affective symptoms remit with thyroid hormone replacement or with antidepressants only after a euthyroid state is established.
To help you recognize hypothyroidism in patients presenting with psychiatric illnesses and provide effective treatment, this article describes:
- hypothyroidism’s signs and symptoms
- primary and subclinical hypothyroidism, thyroiditis, central hypothyroidism, and thyroid hormone resistance
- laboratory screening for thyroid dysfunction in patients with psychiatric symptoms.
Overlapping clinical signs
Thyroid hormone is required for the metabolic activity of every cell in the body. When patients experience symptoms related to abnormal functioning of the hypothalamic-pituitary-thyroid axis (Figure), psychiatrists often are the first professionals they consult.
Diagnosis of thyroid disorders is based on biochemical and clinical data (Box 1),1 which might not be congruent. Clinical symptoms of hypothyroidism, for example, are notoriously variable. Severe biochemical hypothyroidism may be associated with mild clinical symptoms, whereas mild biochemical hypothyroidism may be associated with severe symptoms.2
Patients with thyroid disturbance and psychiatric symptoms most often are diagnosed with a depressive-spectrum syndrome. Most common are:
- atypical depression (which may present as dysthymia)
- bipolar spectrum syndrome (including manic-depression, mixed mania, bipolar depression, rapid-cycling bipolar disorder, cyclothymia, and premenstrual syndromes)
- borderline personality disorder
- or psychotic disorder (typically paranoid psychosis).
Psychiatric symptoms of hypothyroidism (Table 1) are often prominent or even primary. Patients commonly show:
- impaired attention, concentration, learning, and memory
- psychomotor slowing
- and/or mental dullness.
Table 1
Hypothyroidism’s psychiatric signs and symptoms
| Cognitive changes | Impaired memory, psychomotor slowing, reduced attention span |
| Vegetative symptoms | Hypersomnia, sleep apnea, fatigue, lethargy, apathy, anergia, low libido |
| Mood changes | Depression, mood instability, mania, anxiety |
| Other | Psychosis |
Psychiatric patients—particularly those with mood disorders—are more likely to exhibit biochemical evidence of frank or subclinical hypothyroidism, hyperthyroidism, and autoimmune thyroiditis than the general population. In a study of 17,533 Americans,1 approximately 12% had thyroid abnormalities and 80% of these were hypothyroid. An additional 17% of women and 9% of men tested positive for antithyroid antibodies.
Biochemical hypothyroidism was defined as TSH >4.5 mIU/L, with low total T4, and subclinical hypothyroidism as TSH >4.5 mIU/L with normal T4 levels. Population studies and other data have led some endocrinologists to regard serum TSH levels >2.5 mIU/L as abnormally high.
Figure Thyroid hormone regulation: The hypothalamic-pituitary-thyroid axis
Thyroid-stimulating hormone (TSH, thyrotropin) released into circulation by the pituitary stimulates the thyroid to synthesize and release thyroid hormone, including triiodothyronine (T3) and thyroxine (T4). TSH is regulated by hypothalamic elaboration of thyrotropin-releasing hormone (TRH), which stimulates TSH release in a dose-dependent manner. Negative feedback from T3 and T4 downregulates TRH gene expression and restrains the pituitary from responding to TSH. Most T3—the active hormone—is formed in circulation or in target tissues by deiodination of T4 by selenium-containing enzymes.
Illustration for Current Psychiatry by Rich LaroccoThe degree of impairment may depend on the patient’s normal functional level. For example, a well-educated patient of mine with thyroiditis-related hypothyroidism reported word-finding difficulties. Instead of asking her husband to take a bottle of wine from the rack, she asked him to take a bottle of wine from the “thing.”
Loss of vitality, fatigue, lethargy, hypersomnia (especially if sleep apnea is present), and depressed mood also are commonly seen.
Depressive symptoms. Hypothyroid patients usually meet several criteria for a major depressive episode—such as concentration difficulties, lassitude, low libido, and sometimes pessimism or sadness—and symptoms improve after sustained thyroid hormone replacement therapy.3 Women with mild hypothyroidism who screen negative for a psychiatric syndrome show statistically significant mood improvement and improved verbal fluency after 6 months of levothyroxine replacement therapy.4
In some patients with no clear evidence of a biochemical or clinical thyroid disorder, mood symptoms nevertheless respond to thyroid hormone augmentation of antidepressants.5
Anxiety symptoms. Occasionally thyroid dysfunction is seen in patients with anxiety disorders, including panic disorder, agoraphobia, social phobia, performance anxiety, post-traumatic stress disorder, and generalized anxiety disorder.6
It may seem counterintuitive, but hypothyroidism is probably as common as hyperthyroidism in extremely anxious patients. Both hypoand hyperthyroidism are seen much more often in patients with panic-level anxiety than in the general population.
In a sample of 144 consecutive female psychiatric patients with a lifetime history of panic disorder and/or agoraphobia:
- 27% had a history of thyroid disorder
- 17% had hypothyroidism
- 8% had hyperthyroidism.7
Hypothyroid symptoms. Associated symptoms of hypothyroidism (Table 2) may include cold intolerance, lack of or reduced perspiration, dry skin, constipation, lethargy, psychomotor slowness, and subjective paresthesias and muscle pains. Edema is often present. The face typically is swollen or “puffy” in the morning, but by evening the lower legs (and not the face) are edematous.
Deep tendon reflexes usually relax slowly after initial stimulation. Vascular resistance is increased, but hypertension is not usual. Noradrenergic systems become more active in a compensatory, counter-regulatory manner; however, bradycardia—when present—is sometimes profound. Weight gain can occur but often is conspicuously absent.
Severe hypothyroidism presents with paradoxical tremendous agitation, paranoia, and aggressiveness. The skin is leathery, and facies are characteristically rough. Myxedema is fairly common, even in high-functioning patients. I have seen only one case of so-called “myxedema madness;” the female patient’s hyperarousal, yelling, cursing, grossly poor cognitive ability, and loosely conceived paranoid delusions are unforgettable.
Galactorrhea (related to hyperprolactinemia) can be a symptom of severe hypothyroidism, presumably from increased hypothalamic thyrotropin-releasing hormone (TRH) drive. TRH is the main known secretagogue for pituitary prolactin secretion. Infertility, oligomenorrhea, or amenorrhea could be part of the hypothyroid clinical picture.
Other symptoms. Macroglossia and hypertrophy of the uvula are possible; in a recent report, dysarthria resulting from these oral changes was the only presenting symptom of a hypothyroid man.8 Dysarthria promptly corrected after levothyroxine replacement.
Hypothyroidism is a primary cause of central sleep apnea caused by dysfunction of ventilatory control and/or reduction in airway aperture.
Table 2
Hypothyroidism’s other signs and symptoms
| Metabolic | Low basal body temperature/cool skin, diminished perspiration, weight gain or difficulty losing weight |
| Cardiovascular | Bradycardia, dizziness |
| Dermatologic | Dry, rough, or scaly skin; brittle nails; coarse or thinning hair (especially in women); pallor; dependent edema; myxedema/skin mucinosis (classically pretibial) |
| Digestive | Nausea, constipation, enlarged tongue |
| Reproductive | Oligomenorrhea, amenorrhea, infertility, miscarriage, delayed ejaculation |
| Musculoskeletal and peripheral nervous system | Muscle cramps, joint pain, paresthesias, numbness, weakness, reduced exercise tolerance, delayed ankle reflex |
| Sensory | Upper eyelid drooping, dysarthria, hoarseness, diminished hearing, diminished taste (hypogustia) |
Causes of thyroid disorders
Primary hypothyroidism results from thyroid gland failure. The many causes include iodine deficiency, but most cases of adult-onset or acquired hypothyroidism are attributed to autoimmune thyroiditis. In primary hypothyroidism, low serum T4 and/or T3 are seen in combination with elevated serum TSH. Circulating free T4 diminishes sooner than free T3 does as the body attempts to preserve active hormone levels. In turn, total T4 and T3 diminish sooner than free hormone concentrations. A compensatory increase in pituitary-elaborated TSH is seen as the brain and pituitary attempt to stimulate the thyroid to produce adequate thyroid hormone.
In subclinical hypothyroidism, circulating free thyroid hormone concentrations are within the normal laboratory range (typically in the lower range), but TSH is elevated. TSH concentrations >3.0 mIU/mL call for repeat or follow-up biochemistry and clinical correlation.
The decision to treat subclinical hypothyroidism with thyroid hormone replacement is less controversial in psychiatry than in endocrinology. Psychiatric patients with subclinical hypothyroidism—especially those with incomplete responses to psychotropic therapy—should usually be treated with thyroid hormone (Box 2).1
Free T3 levels in the lower 20% of the laboratory’s normal range are cause for pause in a patient with a mood or psychotic disorder and any of hypothyroidism’s clinical stigmata, even if thyroxine and TSH concentrations are normal.
Thyroiditis is characterized by thyroid gland inflammation. The thyroid may be painful or nonpainful, enlarged, fleshy, goitrous, normal in size, or atrophic and fibrotic (especially late in the course).
Postulated precipitants include viruses and other infectious agents, vaccines, iodine excess, lithium therapy (Box 3),9 tobacco smoke, environmental chemicals or toxins, irradiation, and—arguably—cortically-mediated (psychological) stress in vulnerable individuals.
Clinically, thyroiditis syndromes often have a long prodromal phase, wax and wane in severity, have an insidious and sometimes silent course, and can be serially associated with hyperthyroidism (especially early in the course), euthyroidism, or hypothyroidism (especially late in the course). Most thyroiditis syndromes appear to resolve spontaneously, but many become chronic or show evidence of subtle thyroid dysfunction years after the first occurrence or diagnosis.
Most presentations are nonspecific; symptoms may be limited to lethargy, fatigue, and depression. Increased antithyroid antibody titers have been linked with psychotic and depressive syndromes in borderline personality disorder.10
In early thyroiditis, thyroxine and triiodothyronine secretion is often elevated, with low or suppressed TSH. However, antithyroid antibody production is associated with a significantly increased risk of eventual subclinical or frank hypothyroidism. Permanent hypothyroidism develops eventually in at least one-half of women with histories of postpartum thyroiditis.11
Central hypothyroidism stems from TSH deficiency. Both pituitary thyrotrophic failure and hypothalamic failure—secondary and tertiary hypothyroidism, respectively—are considered central (or “secondary”). Hypothyroidism of pituitary and hypothalamic origins are lumped together as “central” because it is often very difficult to differentiate these pathologies.
Thyroid hormone resistance, in which end-organ or cellular resistance to thyroid hormone signals is seen, is an increasingly recognized syndrome in clinical medicine. The typical case is an euthyroid or hypothyroid individual with elevated T4 and T3 and nonsuppressed or even frankly elevated TSH. Inappropriately elevated TSH combined with high thyroid hormone levels also can be seen in TSH-secreting pituitary tumors, although the clinical picture in this case is one of hyperthyroidism.
Thyroid hormone resistance ranges from euthyroid and clinically transparent to profoundly hypothyroid, and different organs in the same patient may show different sensitivities to thyroid hormone. Clinical features vary, depending on the strength of thyroid hormone resistance.
Early emergence of resistance (as would be expected in someone with an inherited thyroid hormone receptor abnormality) leads to developmental problems, including:
- short stature
- mental or learning disabilities (including attention deficits).
In a study of 18 families with strong history of generalized resistance to thyroid hormone, 70% of affected children met diagnostic criteria for attention-deficit/hyperactivity disorder.12
Target psychiatric symptoms for prescribing replacement thyroid hormone are depression; mood cycling or instability; low energy, fatigue, or lethargy; cognitive impairment (Table 1); and psychosis, if present. Because these symptoms are not specific to thyroid dysfunction, institute thyroid hormone only when biochemical evidence of compromised or suboptimal thyroid function is also present.
Exceptions to this rule may include patients with target psychiatric symptoms and:
Patients taking lithium for mood stabilization will likely need supplemental thyroid hormone eventually because lithium is thyrotoxic. Also, patients with bipolar mood symptoms often have coexisting thyroid abnormalities, and giving supraphysiologic thyroid hormone dosages sometimes converts those who do not respond to mood stabilizers into responders.
Thyrotropin concentrations increase within 1 day after patients start taking lithium carbonate, but without commensurate increases in T3 or T4. More often, T3 and T4 concentrations decrease in the presence of lithium. Among 150 patients maintained on lithium for 10 years, hypothyroidism, autoimmune thyroiditis, or goiter developed at rates of 1.7%, 1.4%, and 2.1% per year, respectively. The study authors suggested that long-term lithium may increase the risk for hypothyroidism in women and in patients with thyroid autoimmunity.9
Laboratory screening
TSH and thyroid hormones. The basic thyroid screen is a combination of serum levels of TSH (“sensitive TSH”) and free thyroid hormones.
TSH has a circadian rhythm, with a nocturnal surge amounting to a 50% to 200% increase over daytime levels, beginning at around 6 to 8 PM. Peak TSH pulsatile activity and levels are seen after sleep begins—usually after midnight—with trough levels and fewest TSH pulses in late morning and early afternoon.13,14 This rhythm implies that the most accurate TSH measurement may be obtained by drawing blood in the morning before 9 AM. I have seen subclinical hypothyroidism missed when clinicians relied on afternoon TSH levels.
In general medicine, TSH alone frequently is used as a routine screening tool. In psychiatric practice, however, I recommend supplementing TSH with free T3 and free T4 because thyroid system dysfunction is frequent in psychiatric syndromes. If laboratory costs are a concern, free T4 with TSH usually suffices for initial screening.
Although the unbound, free fractions of T3 and T4 are of primary interest, total T4 and total T3 are necessary to assess the thyroid gland’s synthetic capacity. When clinical evidence suggests abnormal thyroid hormone function, order repeated or serial biochemical testing. Marginal biochemical results also mandate repeat thyroid function studies, expanded to include:
- total thyroid hormone concentrations (ideally T4 and T3)
- antithyroid antibodies
- serum cholesterol
- prolactin.
Antithyroid antibodies. Obtain antithyroglobulin and antithyroid microsomal antibody titers if:
- thyroid hormone indices are abnormal or marginal—in either direction
- or the patient now has, has had, or has a family history of autoimmune-mediated symptoms, such as lupus erythematosus or rheumatoid arthritis.
Negative or low antithyroid autoantibody titers do not rule out thyroiditis as a cause of hypothyroidism, as these titers are most likely to be generated during periods of active inflammation.
Many autoantibodies react with thyroid-related elements. Most clinical laboratories can quantify antibodies directed against thyroid peroxidase—also called antimicrosomal antibodies—and thyroglobulin. The presence of these antibodies is associated with thyroid inflammation and a risk of progression to thyroid failure and hypothyroidism.
Other laboratory findings of hypothyroidism include hypercholesterolemia, mild hyperprolactinemia, and types of anemia (including iron-deficiency anemia with low ferritin levels).
Related resources
- American Thyroid Association. www.thyroid.org.
- Dunn JT. Guarding our nation’s thyroid health. J Clin Endocrinol Metab 2001;872:486-8.
- Pearce EN, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med 2003;348:2646-55.
- Sullivan GM, Mann JJ, Oquendo MA, et al. Low cerebrospinal fluid transthyretin levels in depression: correlations with suicidal ideation and low serotonin function. Biol Psychiatry 2006;60(5):500-6.
1. Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 2002;87:489-99.
2. Zulewski H, Muller B, Exer P, et al. Estimation of tissue hypothyroidism by a new clinical score: evaluation of patients with various grades of hypothyroidism and controls. J Clin Endocrinol Metab 1997;82:771-6.
3. Gunnarsson T, Sjoberg S, Eriksson M, Nordin C. Depressive symptoms in hyothyroid disorder with some observations on biochemical correlates. Neuropsychobiology 2001;43:70-4.
4. Bono G, Fancellu R, Blandini F, Santor G, Mauri M. Cognitive and affective status in mild hypothyroidism and interactions with L-thyroxine treatment. Acta Neurol Scand 2004;110:59-66
5. Iosifescu DV. ‘Supercharge’ antidepressants by adding thyroid hormones: Why hormones help, and new data on SSRI augmentation. Current Psychiatry 2006;5(7):15-25.
6. Tancer ME, Stein MB, Gelernter CS, Uhde TW. The hypothalamic-pituitary-thyroid axis in social phobia. Am J Psychiatry 1990;147(7):929-33
7. Orenstein H, Peskind A, Raskind MA. Thyroid disorders in female psychiatric patients with panic disorder or agoraphobia. Am J Psychiatry 1988;145:1428-30.
8. Stollberger C, Finsterer J, Brand E, Tschabitscher D. Dysarthria as the leading symptom of hypothyroidism. Am J Otolaryngol 2001;22:70-2.
9. Bocchetta A, Mossa P, Velluzzi F, et al. Ten-year follow-up of thyroid function in lithium patients. J Clin Psychopharmacol 2001;21(6):594-8.
10. Geracioti TD, Kling MA, Post R, Gold PW. Antithyroid antibody-linked symptoms in borderline personality disorder. Endocrine 2003;21:153-8.
11. Premawardhana LD, Parkes AB, Ammari F, et al. Postpartum thyroiditis and long-term thyroid status: prognostic influence of thyroid peroxidase antibodies and ultrasound echogenicity. J Clin Endocrinol Metab 2000;85:71-5.
12. Hauser P, Zametkin AJ, Martinez P, et al. Attention deficithyperactivity disorder in people with generalized resistance to thyroid hormone. N Engl J Med 1993;328:997-1001.
13. Ghizzoni L, Mastorakos G, Ziveri M, et al. Interactions of leptin and thyrotropin 24-hour secretory profiles in short normal children. J Clin Endocrinol Metab 2001;86(5):2065-72.
14. Mantzoros CS, Ozata M, Negrao AB, et al. Synchronicity of frequently sampled thyrotropin (TSH) and leptin concentrations in healthy adults and leptin-deficient subjects: evidence for possible partial TSH regulation by leptin in humans. J Clin Endocrinol Metab 2001;86(7):3284-91.
15. Chopra IJ, Sabatino L. Nature and sources of circulating thyroid hormones. In: Braverman LE, Utiger RD, eds. The thyroid. A fundamental and clinical text. Philadelphia: Lippincott; 2000:120-35.
1. Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 2002;87:489-99.
2. Zulewski H, Muller B, Exer P, et al. Estimation of tissue hypothyroidism by a new clinical score: evaluation of patients with various grades of hypothyroidism and controls. J Clin Endocrinol Metab 1997;82:771-6.
3. Gunnarsson T, Sjoberg S, Eriksson M, Nordin C. Depressive symptoms in hyothyroid disorder with some observations on biochemical correlates. Neuropsychobiology 2001;43:70-4.
4. Bono G, Fancellu R, Blandini F, Santor G, Mauri M. Cognitive and affective status in mild hypothyroidism and interactions with L-thyroxine treatment. Acta Neurol Scand 2004;110:59-66
5. Iosifescu DV. ‘Supercharge’ antidepressants by adding thyroid hormones: Why hormones help, and new data on SSRI augmentation. Current Psychiatry 2006;5(7):15-25.
6. Tancer ME, Stein MB, Gelernter CS, Uhde TW. The hypothalamic-pituitary-thyroid axis in social phobia. Am J Psychiatry 1990;147(7):929-33
7. Orenstein H, Peskind A, Raskind MA. Thyroid disorders in female psychiatric patients with panic disorder or agoraphobia. Am J Psychiatry 1988;145:1428-30.
8. Stollberger C, Finsterer J, Brand E, Tschabitscher D. Dysarthria as the leading symptom of hypothyroidism. Am J Otolaryngol 2001;22:70-2.
9. Bocchetta A, Mossa P, Velluzzi F, et al. Ten-year follow-up of thyroid function in lithium patients. J Clin Psychopharmacol 2001;21(6):594-8.
10. Geracioti TD, Kling MA, Post R, Gold PW. Antithyroid antibody-linked symptoms in borderline personality disorder. Endocrine 2003;21:153-8.
11. Premawardhana LD, Parkes AB, Ammari F, et al. Postpartum thyroiditis and long-term thyroid status: prognostic influence of thyroid peroxidase antibodies and ultrasound echogenicity. J Clin Endocrinol Metab 2000;85:71-5.
12. Hauser P, Zametkin AJ, Martinez P, et al. Attention deficithyperactivity disorder in people with generalized resistance to thyroid hormone. N Engl J Med 1993;328:997-1001.
13. Ghizzoni L, Mastorakos G, Ziveri M, et al. Interactions of leptin and thyrotropin 24-hour secretory profiles in short normal children. J Clin Endocrinol Metab 2001;86(5):2065-72.
14. Mantzoros CS, Ozata M, Negrao AB, et al. Synchronicity of frequently sampled thyrotropin (TSH) and leptin concentrations in healthy adults and leptin-deficient subjects: evidence for possible partial TSH regulation by leptin in humans. J Clin Endocrinol Metab 2001;86(7):3284-91.
15. Chopra IJ, Sabatino L. Nature and sources of circulating thyroid hormones. In: Braverman LE, Utiger RD, eds. The thyroid. A fundamental and clinical text. Philadelphia: Lippincott; 2000:120-35.