User login
Idiopathic granulomatous mastitis (IGM) is rare during pregnancy; it typically is seen in women of childbearing potential from 6 months to 6 years postpartum.1 Because of a temporal association with breastfeeding, it is believed that hyperprolactinemia2 or an immune response to local lobular secretions might play a role in pathogenesis. Early misdiagnosis as bacterial mastitis is common, prompting multiple antibiotic regimens. When antibiotics fail, patients are worked up for inflammatory breast cancer, given the nonhealing breast nodules. Mammography, ultrasonography, and fine-needle aspiration often are unable to rule out carcinoma, warranting excisional biopsies of nodules. The patient is then referred to rheumatology for potential sarcoidosis or to dermatology for IGM. In either case, the workup should be similar, but additional history focused on behavior and medications is essential in suspected IGM, given the association with hyperprolactinemia.
Because IGM is rare, there are no randomized, placebo-controlled trials of treatment efficacy. In many cases, patients undergo complete mastectomy, which is curative but may be psychologically and physically impactful in young women. In some cases, high-dose corticosteroids have been successful; however, because the IGM process can last longer than 2 years, patients treated in this manner are exposed to steroid morbidities.1
We report 3 cases of IGM that add to the literature on possible contributing factors, clinical presentations, and treatments for this disease. We also demonstrate that appropriate trigger identification and steroid-sparing agents, specifically methotrexate, can be breast-saving as they can alleviate this debilitating condition, obviating the need for radical surgical intervention.
CASE REPORTS
Patient 1
A 40-year-old woman with a 4-year history of breastfeeding noted a grape-sized nodule on the left breast that grew to the size of a grapefruit after 2 weeks. Ulceration and drainage periodically occurred, forming pink plaques along the lateral aspects of the breast after healing. Her primary care provider suspected infectious mastitis; she was given an oral antibiotic (cephalexin) and intravenous antibiotics without improvement.
Imaging
Subsequent magnetic resonance imaging revealed a large, irregular, enhancing mass within the outer left breast (6.5 cm at greatest dimension) with additional surrounding amorphous enhancement highly suspicious for malignancy. There also were multiple prominent left axillary lymph nodes, with the largest demonstrating a cortical thickness of 8 mm.
Biopsy
Core breast biopsy showed benign tissue with fat necrosis. Fine-needle aspiration revealed few benign ductal cells and rare histiocytes; because these findings were nondiagnostic and cancer was still a consideration, the patient underwent excisional biopsy.
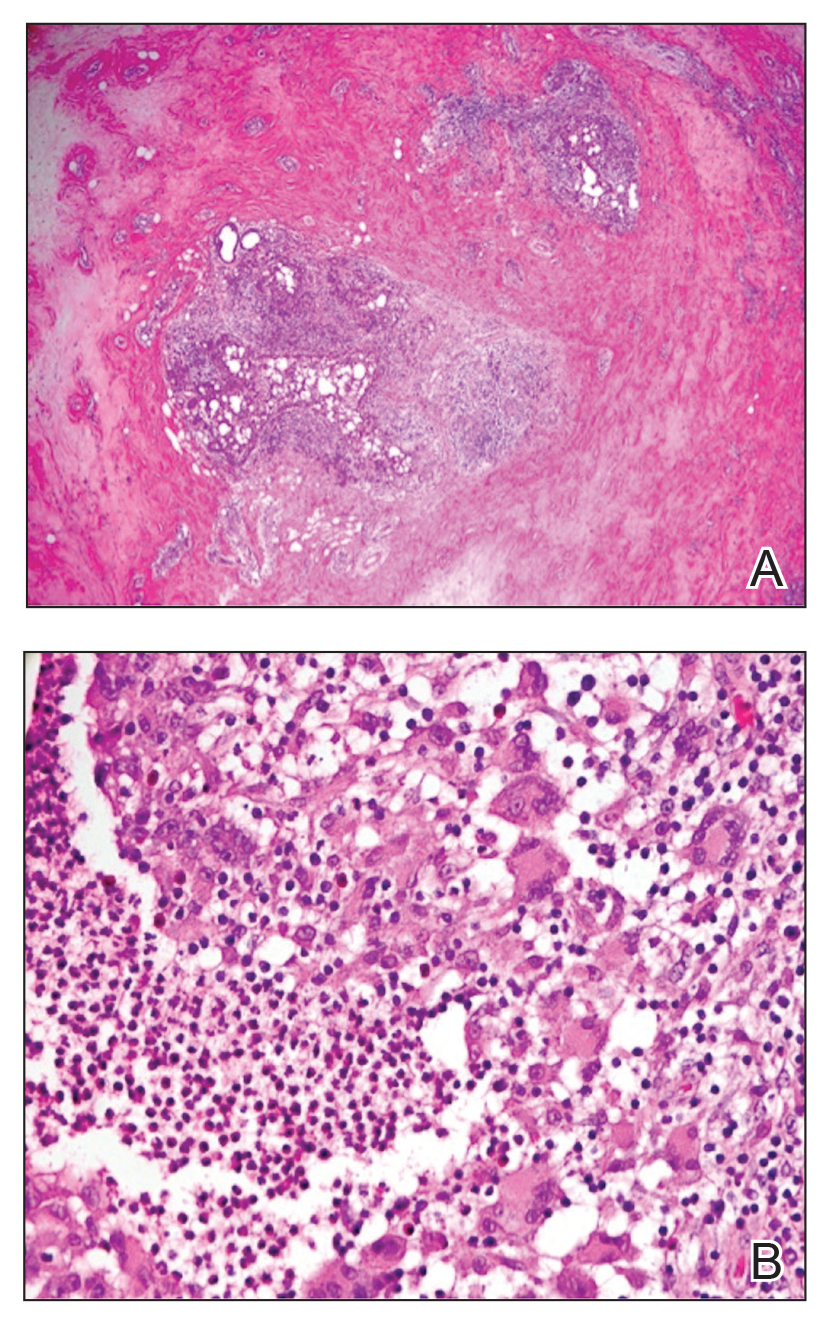
Histologic sections of breast tissue showed extensive lobulocentric inflammation comprising histiocytes and lymphocytes, with neutrophils admixed and forming microabscesses (Figure 1A). Multinucleated giant cells and single-cell necrosis were seen, but true caseous necrosis was absent (Figure 1B). Duct spaces often contained inflammatory cells or secretions. Special stains for fungal and acid-fast bacterial microorganisms were negative.
Referral to Dermatology
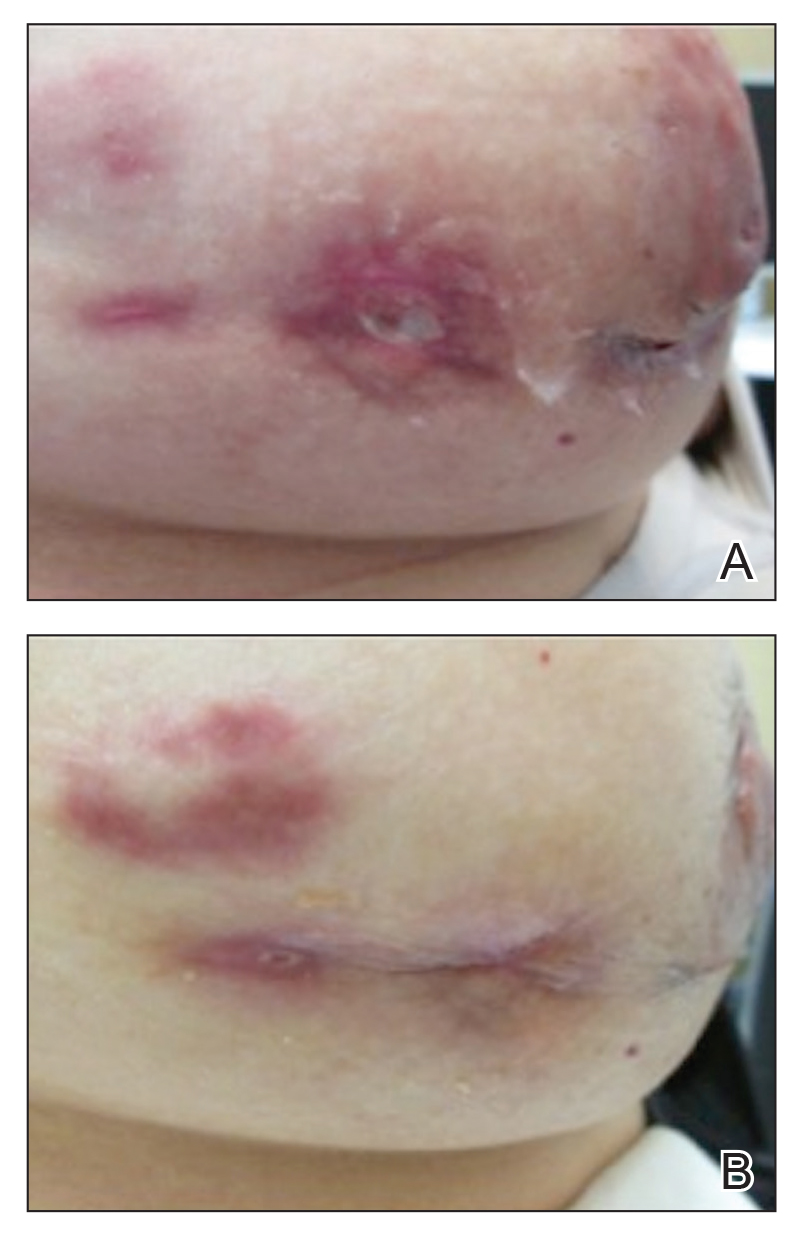
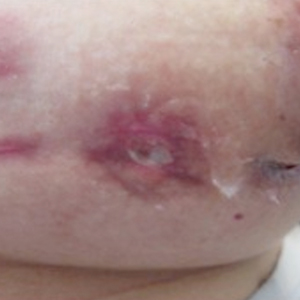
Granulomatous lobular mastitis was diagnosed, and the patient was referred to dermatology. On presentation to dermatology, the left breast showed a 6-cm area of firm induration and overlying peau d’orange change to the epidermis (Figure 2A). Based on pathologic analysis, she was worked up for a possible granulomatous etiology. Negative purified protein derivative (tuberculin)(PPD) and a normal chest radiograph ruled out tuberculosis. Normal chest radiography, serum Ca2+ and angiotensin-converting enzyme (ACE) levels, and ophthalmology examination ruled out sarcoidosis.
The patient reported she continued breastfeeding her 4-year-old son. Additionally, she had been started on trazadone and buspirone for alcohol abuse recovery, then switched to and maintained on fluoxetine 1 year before developing these symptoms.
Buspirone, fluoxetine, and prolonged breastfeeding all contribute to hyperprolactinemia, a possible trigger of IGM. The patient was therefore advised to stop breastfeeding and to be switched from fluoxetine to a medication that would not increase the prolactin level. She did not require methotrexate treatment because her condition resolved rapidly after breastfeeding and fluoxetine were discontinued (Figure 2B).
B, Resolution after discontinuation of breastfeeding and fluoxetine.
Patient 2
A 40-year-old woman with no history of breastfeeding who gave birth 4.5 years prior presented to her primary care provider with a painful breast lump and rash on the right breast of 2 months’ duration. Infectious mastitis was suspected; she was given cephalexin and clindamycin without improvement of symptoms.
Imaging
Mammography and ultrasonography were nondiagnostic.
Biopsy
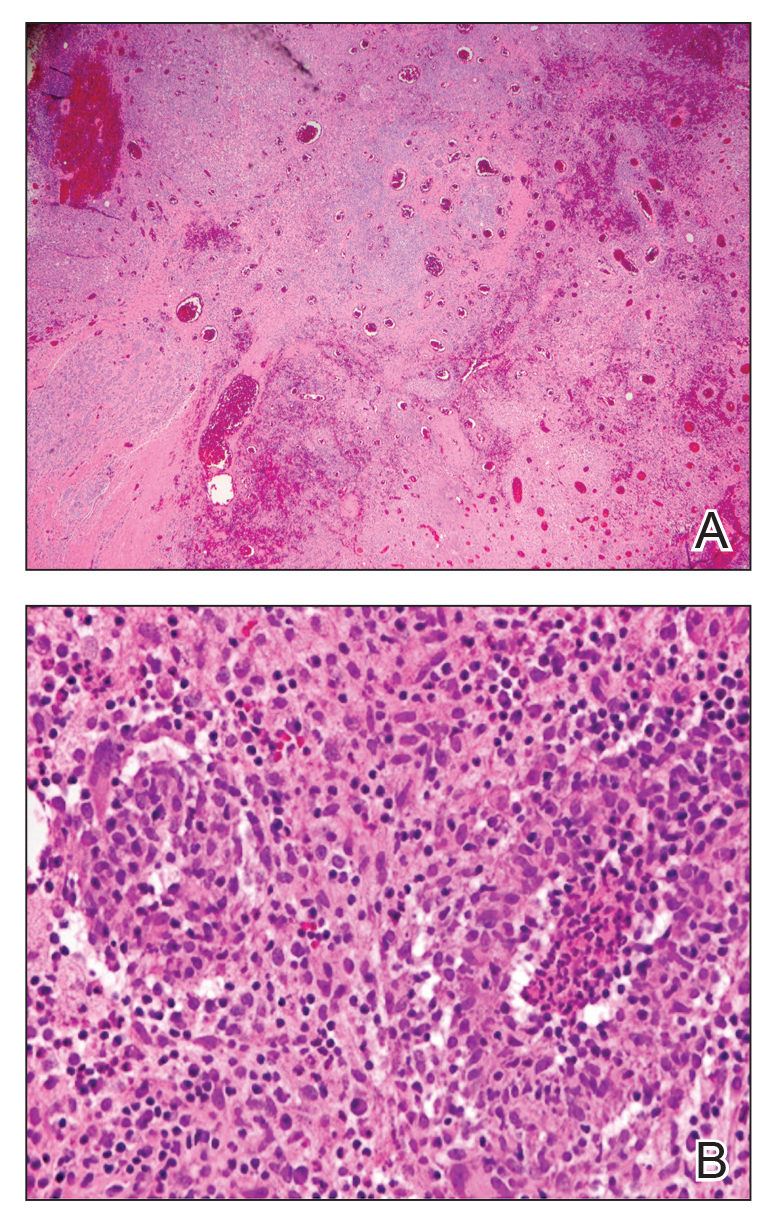
Breast biopsy showed tissue with large expanses of histiocytes, neutrophils, lymphocytes, plasma cells, and multinucleated giant cells (Figure 3A). Many discrete granulomas were seen against this mixed inflammatory background, associated with focal fat necrosis (Figure 3B). Special stains were negative for microorganisms. Histologic findings were consistent with granulomatous mastitis.
Referral to Dermatology
On presentation to dermatology, the patient was worked up for a possible granulomatous etiology, which included a negative PPD, as well as a normal chest radiograph, serum Ca2+ and ACE levels, and ophthalmology examination. Review of symptoms (ROS),medical history, and medication review were unremarkable.
By exclusion, the patient was given a diagnosis of IGM and started on methotrexate (15 mg weekly) with folic acid (1 mg daily). The condition of the right breast improved within 4 weeks of starting methotrexate; however, methotrexate was increased to 30 mg weekly because of occasional flares. The patient remained on methotrexate without further IGM flares for 8 months compared to prior unremitting pain and drainage. She was then tapered from methotrexate over 6 weeks without additional flares.
Patient 3
A 27-year-old woman who gave birth 2 years prior and discontinued breastfeeding 6 weeks after delivery noted bilateral breast rashes for several months. The lesions were growing in size, tender, and draining. Her primary care provider suspected infectious mastitis and prescribed antibiotics, which were ineffective.
Biopsy
Breast core biopsy showed histologic findings similar to patients 1 and 2, including lobulocentric mixed inflammation, neutrophilic microabscesses, and scattered discrete granulomas. Microorganisms were not found using special stains. Breast cancer was ruled out, and granulomatous mastitis was diagnosed.
Referral to Dermatology
Two years earlier, the patient tested positive for latent tuberculosis and was prescribed a 9-month regimen of isoniazid. At the current presentation, she did not have symptoms of active tuberculosis on ROS (ie, no cough, hemoptysis, weight loss, night sweats); a chest radiograph was normal. Additionally, serum Ca2+ and ACE levels as well as an ophthalmology examination were normal, and she was not taking any medications known to increase the prolactin level.
The patient was started on methotrexate (12.5 mg weekly) and folic acid (1 mg daily). She had 1 IGM flare and was given a tapering regimen of prednisone. She received methotrexate for 14 months, tapered during the final 3 months. She has been off methotrexate for 3 years without IGM flares and appears to be in complete remission.
COMMENT
We report 3 cases of IGM, which contribute to the literature on possible presentations, causes, and conservative treatment of this rare connective-tissue disorder.
Differential Diagnosis
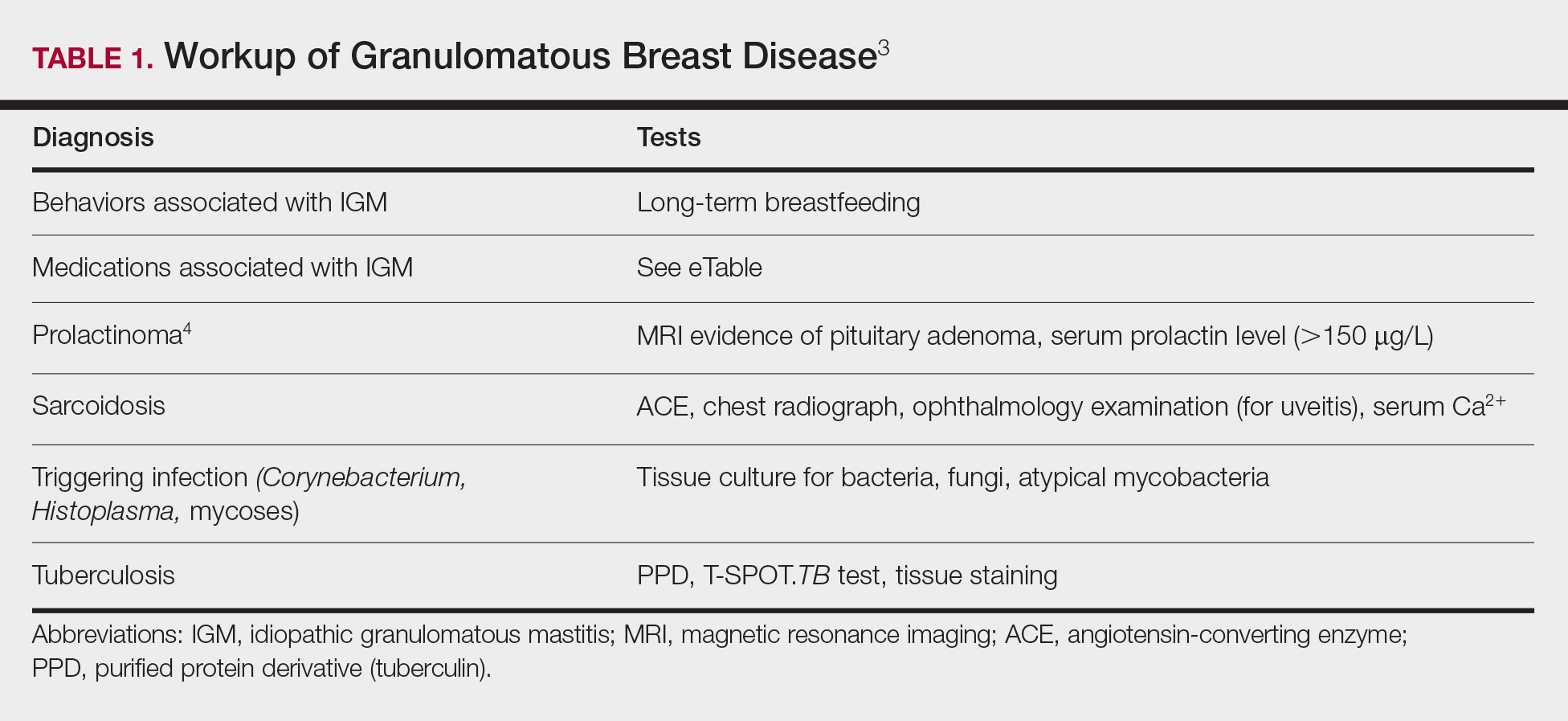
The time between recognition of symptoms and diagnosis and treatment of IGM often is prolonged because IGM can present similarly to other disorders, such as infection, breast cancer, tuberculosis, and sarcoidosis. Idiopathic granulomatous mastitis is a diagnosis of exclusion, made after obtaining evidence of granulomatous inflammation on breast biopsy and ruling out other granulomatous disorders, such as tuberculosis and sarcoidosis (Table 1).3,4
Tuberculosis
A full ROS and a PPD test or T-SPOT.TB test can be helpful in ruling out tuberculosis; because anergy occurs in some patients, tuberculosis should be evaluated in the context of known immunosuppression or human immunodeficiency virus status, or in the case of miliary tuberculosis.
Chest radiography findings classically showing upper lobe infiltrates with cavities in active tuberculosis also should be sought.3 Ziehl-Neelsen staining of 2 sputum specimens, assessed by conventional light microscopy at the time of tissue biopsy has 64% sensitivity and 98% specificity for detecting Mycobacterium tuberculosis; auramine O staining, examined with light-emitting diode fluorescence microscopy, has 73% sensitivity and 93% specificity.5
Sarcoidosis
Because more than 90% of sarcoid patients have lung disease, a chest radiograph is used to screen for hilar lymphadenopathy.3 An elevated serum ACE level also can be helpful in diagnosis, but patients do not always have increased ACE, which can occur in other diseases, such as hyperthyroidism and miliary tuberculosis. Sarcoid granulomas can increase active vitamin D production, which in turn increases serum Ca2+ in 10% of sarcoid patients. Last, an ophthalmology evaluation should be obtained to rule out anterior or posterior uveitis that can occur in sarcoidosis and initially remain asymptomatic.3 Once these other causes of granulomatous inflammation have been ruled out, a diagnosis of IGM can be made.
Prolactinoma
Prolactinoma is an important cause of hyperprolactinemia that can be screened for based on ROS and the serum prolactin level. Prolactinoma can cause oligomenorrhea or amenorrhea and galactorrhea in 90% and 80% of premenopausal women, respectively, as well as erectile dysfunction and decreased libido in men. Infertility, headache, and visual impairment may be experienced in both sexes.4
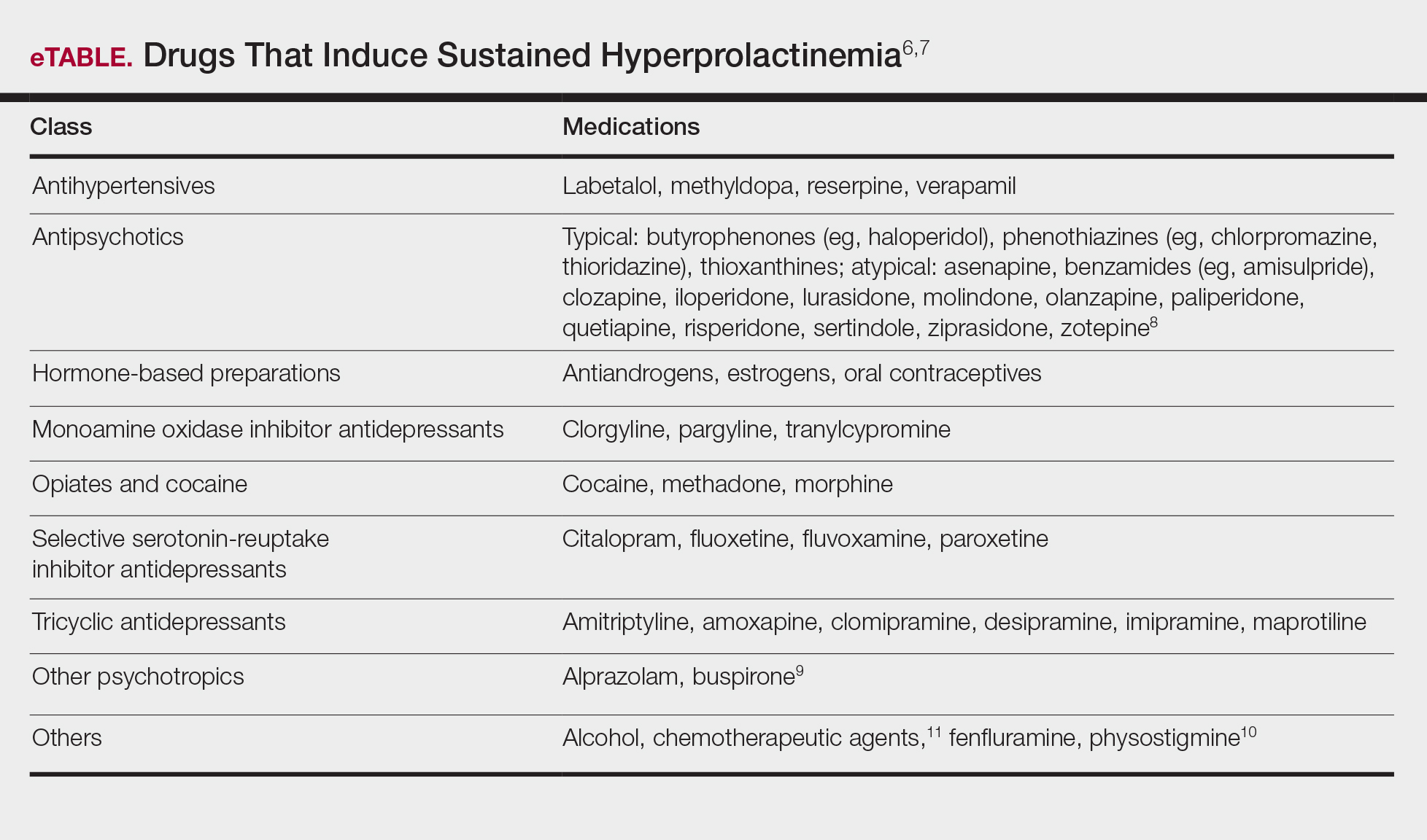
A normal prolactin level is less than 25 μg/L; more than 25 μg/L but less than 100 μg/L usually is due to certain drugs (eTable),6-11 estrogen, or idiopathic reasons; and more than 150 μg/L usually is due to prolactinoma.5 In many cases, removal of hyperprolactinemia-precipitating factors can resolve disease, as in patient 1. If symptoms continue or precipitating factors are absent, IGM symptom-based treatment should be administered.
Course and Management
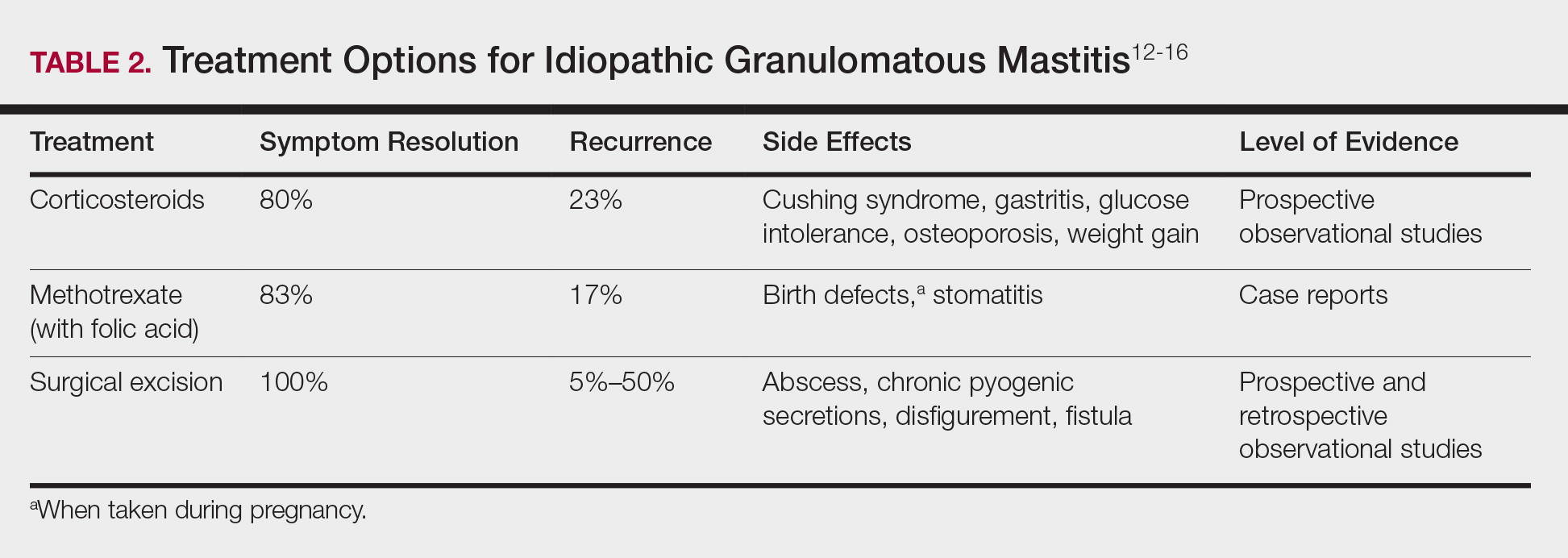
Idiopathic granulomatous mastitis is self-limited and usually resolves within 2 years. Therefore, the goal of treatment is to suppress associated pain and drainage until the active inflammatory phase of IGM self-resolves. An established protocol for treating IGM does not exist, but common treatments include corticosteroids, methotrexate, and limited or wide surgical excision (Table 2).12-16 Before beginning any of these treatments, IGM triggers, such as breastfeeding and drugs that induce hyperprolactinemia, should be removed.
It is important to consider which treatment option is best for limiting disease recurrence and adverse effects (AEs). Keep in mind that the available data are limited, as there are no randomized controlled trials looking at these treatments. Nevertheless, we recommend methotrexate as first line because it resolves granulomatous inflammation symptoms without invasive surgery, while limiting corticosteroid AEs.12
With or without concurrent use of corticosteroids, surgical excision typically is the mainstay of treatment. However, surgical excision of IGM lesions can be complicated by abscess formation, fistula, and chronic pyogenic secretions, in addition to a 5% to 50% rate of recurrence of disease.12-14 Limited excision often is insufficient; therefore, wide local excision, in which negative margins around granulomatous inflammation are obtained, is the surgical modality of choice.14 Wide local excision can be disfiguring to the breast in young women affected by IGM, making it an undesirable treatment option.
Corticosteroids often have been used to treat IGM, but their efficacy is variable, symptoms can recur upon drug removal, and remarkable AEs can result from long-term use.12 Additionally, corticosteroid therapy often is used in combination with excision, making it difficult to determine the extent to which corticosteroids or excision are more beneficial. In a prospective observational study, corticosteroid therapy alone resolved 80% of IGM symptoms after 159 days on average. After complete symptom resolution, 23% of patients had disease recurrence.9 Observed AEs included gastritis, weight gain, osteoporosis, glucose intolerance, and Cushing syndrome.12,15
Methotrexate for IGM has not been reviewed in a randomized controlled trial; case reports have shown 83% symptom resolution, with 17% recurrence and limited long-term AEs.12 Because the active phase of IGM can persist for 2 years, immunosuppressive therapy with limited AEs is necessary. Many AEs can occur when high-dose methotrexate is given for cancer treatment. Low-dose methotrexate has been extensively studied in long-term treatment of rheumatoid arthritis. Adverse effects may include gastrointestinal tract upset and hepatic dysfunction, which are limited when given with folic acid.
Regardless of folic acid cotreatment, stomatitis may occur. Women should use an effective method of birth control because severe birth defects may occur on even low-dose methotrexate.16
Compared to corticosteroid or surgical treatment, we recommend low-dose methotrexate therapy based on its high efficacy with limited AEs. An occasional mild flare of IGM symptoms with methotrexate is not unusual. If it occurs, corticosteroids can be added and tapered for as long as 2 weeks to speed up resolution of flares while reducing long-term AEs of corticosteroids.
Surgical excision can be performed in cases refractory to all systemic therapies.
CONCLUSION
Idiopathic granulomatous mastitis is a rare granulomatous breast disorder that can have a prolonged time to diagnosis, delaying proper treatment. Many cases self-resolve, but more severe cases can persist for a long period before adequate symptomatic treatment is achieved by methotrexate, corticosteroids, or surgical excision. Before using these therapies, it is important to identify and remove contributing factors, such as long-term breastfeeding and drugs that induce hyperprolactinemia. Improving the rate of IGM diagnosis and treatment would greatly benefit these patients. We report 1 case in which removal of possible precipitating IGM factors led to symptom resolution and 2 cases in which methotrexate was an effective IGM treatment that limited the need for invasive procedures and corticosteroid AEs.
1. Patel RA, Strickland P, Sankara IR, et al. Idiopathic granulomatous mastitis: case reports and review of literature. J Gen Intern Med. 2010;25:270-273.
2. Bellavia M, Damiano G, Palumbo VD, et al. Granulomatous mastitis during chronic antidepressant therapy: is it possible a conservative therapeutic approach? J Breast Cancer. 2012;15:371-372.
3. Longo D, Fauci A, Kasper D, et al. Harrison’s Principles of Internal Medicine. 18th ed. New York, NY: McGraw-Hill; 2012.
4. Davis JL, Cattamanchi A, Cuevas LE, et al. Diagnostic accuracy of same-day microscopy versus standard microscopy for pulmonary tuberculosis: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13:147-154.
5. Casanueva FF, Molitch ME, Schlechte JA, et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf). 2006;65:265-273.
6. Akbulut S, Arikanoglu Z, Senol A, et al. Is methotrexate an acceptable treatment in the management of idiopathic granulomatous mastitis? Arch Gynecol Obstet. 2011;284:1189-1195.
7. Bani-Hani KE, Yaghan RJ, Matalka II, et al. Idiopathic granulomatous mastitis: time to avoid unnecessary mastectomies. Breast J. 2004;10:318-322.
8. Asoglu O, Ozmen V, Karanlik H, et al. Feasibility of surgical management in patients with granulomatous mastitis. Breast J. 2005;11:108-114.
9. Pandey TS, Mackinnon JC, Bressler L, et al. Idiopathic granulomatous mastitis—a prospective study of 49 women and treatment outcomes with steroid therapy. Breast J. 2014;20:258-266.
10. Shea B, Swinden MV, Tanjong Ghogomu E, et al. Folic acid and folinic acid for reducing side effects in patients receiving methotrexate for rheumatoid arthritis. Cochrane Database Syst Rev. 2013;5:CD000951.
11. Molitch ME. Drugs and prolactin. Pituitary. 2008;11:209-218.
12.
13.
14.
15.
16.
Idiopathic granulomatous mastitis (IGM) is rare during pregnancy; it typically is seen in women of childbearing potential from 6 months to 6 years postpartum.1 Because of a temporal association with breastfeeding, it is believed that hyperprolactinemia2 or an immune response to local lobular secretions might play a role in pathogenesis. Early misdiagnosis as bacterial mastitis is common, prompting multiple antibiotic regimens. When antibiotics fail, patients are worked up for inflammatory breast cancer, given the nonhealing breast nodules. Mammography, ultrasonography, and fine-needle aspiration often are unable to rule out carcinoma, warranting excisional biopsies of nodules. The patient is then referred to rheumatology for potential sarcoidosis or to dermatology for IGM. In either case, the workup should be similar, but additional history focused on behavior and medications is essential in suspected IGM, given the association with hyperprolactinemia.
Because IGM is rare, there are no randomized, placebo-controlled trials of treatment efficacy. In many cases, patients undergo complete mastectomy, which is curative but may be psychologically and physically impactful in young women. In some cases, high-dose corticosteroids have been successful; however, because the IGM process can last longer than 2 years, patients treated in this manner are exposed to steroid morbidities.1
We report 3 cases of IGM that add to the literature on possible contributing factors, clinical presentations, and treatments for this disease. We also demonstrate that appropriate trigger identification and steroid-sparing agents, specifically methotrexate, can be breast-saving as they can alleviate this debilitating condition, obviating the need for radical surgical intervention.
CASE REPORTS
Patient 1
A 40-year-old woman with a 4-year history of breastfeeding noted a grape-sized nodule on the left breast that grew to the size of a grapefruit after 2 weeks. Ulceration and drainage periodically occurred, forming pink plaques along the lateral aspects of the breast after healing. Her primary care provider suspected infectious mastitis; she was given an oral antibiotic (cephalexin) and intravenous antibiotics without improvement.
Imaging
Subsequent magnetic resonance imaging revealed a large, irregular, enhancing mass within the outer left breast (6.5 cm at greatest dimension) with additional surrounding amorphous enhancement highly suspicious for malignancy. There also were multiple prominent left axillary lymph nodes, with the largest demonstrating a cortical thickness of 8 mm.
Biopsy
Core breast biopsy showed benign tissue with fat necrosis. Fine-needle aspiration revealed few benign ductal cells and rare histiocytes; because these findings were nondiagnostic and cancer was still a consideration, the patient underwent excisional biopsy.
Histologic sections of breast tissue showed extensive lobulocentric inflammation comprising histiocytes and lymphocytes, with neutrophils admixed and forming microabscesses (Figure 1A). Multinucleated giant cells and single-cell necrosis were seen, but true caseous necrosis was absent (Figure 1B). Duct spaces often contained inflammatory cells or secretions. Special stains for fungal and acid-fast bacterial microorganisms were negative.
Referral to Dermatology
Granulomatous lobular mastitis was diagnosed, and the patient was referred to dermatology. On presentation to dermatology, the left breast showed a 6-cm area of firm induration and overlying peau d’orange change to the epidermis (Figure 2A). Based on pathologic analysis, she was worked up for a possible granulomatous etiology. Negative purified protein derivative (tuberculin)(PPD) and a normal chest radiograph ruled out tuberculosis. Normal chest radiography, serum Ca2+ and angiotensin-converting enzyme (ACE) levels, and ophthalmology examination ruled out sarcoidosis.
The patient reported she continued breastfeeding her 4-year-old son. Additionally, she had been started on trazadone and buspirone for alcohol abuse recovery, then switched to and maintained on fluoxetine 1 year before developing these symptoms.
Buspirone, fluoxetine, and prolonged breastfeeding all contribute to hyperprolactinemia, a possible trigger of IGM. The patient was therefore advised to stop breastfeeding and to be switched from fluoxetine to a medication that would not increase the prolactin level. She did not require methotrexate treatment because her condition resolved rapidly after breastfeeding and fluoxetine were discontinued (Figure 2B).
B, Resolution after discontinuation of breastfeeding and fluoxetine.
Patient 2
A 40-year-old woman with no history of breastfeeding who gave birth 4.5 years prior presented to her primary care provider with a painful breast lump and rash on the right breast of 2 months’ duration. Infectious mastitis was suspected; she was given cephalexin and clindamycin without improvement of symptoms.
Imaging
Mammography and ultrasonography were nondiagnostic.
Biopsy
Breast biopsy showed tissue with large expanses of histiocytes, neutrophils, lymphocytes, plasma cells, and multinucleated giant cells (Figure 3A). Many discrete granulomas were seen against this mixed inflammatory background, associated with focal fat necrosis (Figure 3B). Special stains were negative for microorganisms. Histologic findings were consistent with granulomatous mastitis.
Referral to Dermatology
On presentation to dermatology, the patient was worked up for a possible granulomatous etiology, which included a negative PPD, as well as a normal chest radiograph, serum Ca2+ and ACE levels, and ophthalmology examination. Review of symptoms (ROS),medical history, and medication review were unremarkable.
By exclusion, the patient was given a diagnosis of IGM and started on methotrexate (15 mg weekly) with folic acid (1 mg daily). The condition of the right breast improved within 4 weeks of starting methotrexate; however, methotrexate was increased to 30 mg weekly because of occasional flares. The patient remained on methotrexate without further IGM flares for 8 months compared to prior unremitting pain and drainage. She was then tapered from methotrexate over 6 weeks without additional flares.
Patient 3
A 27-year-old woman who gave birth 2 years prior and discontinued breastfeeding 6 weeks after delivery noted bilateral breast rashes for several months. The lesions were growing in size, tender, and draining. Her primary care provider suspected infectious mastitis and prescribed antibiotics, which were ineffective.
Biopsy
Breast core biopsy showed histologic findings similar to patients 1 and 2, including lobulocentric mixed inflammation, neutrophilic microabscesses, and scattered discrete granulomas. Microorganisms were not found using special stains. Breast cancer was ruled out, and granulomatous mastitis was diagnosed.
Referral to Dermatology
Two years earlier, the patient tested positive for latent tuberculosis and was prescribed a 9-month regimen of isoniazid. At the current presentation, she did not have symptoms of active tuberculosis on ROS (ie, no cough, hemoptysis, weight loss, night sweats); a chest radiograph was normal. Additionally, serum Ca2+ and ACE levels as well as an ophthalmology examination were normal, and she was not taking any medications known to increase the prolactin level.
The patient was started on methotrexate (12.5 mg weekly) and folic acid (1 mg daily). She had 1 IGM flare and was given a tapering regimen of prednisone. She received methotrexate for 14 months, tapered during the final 3 months. She has been off methotrexate for 3 years without IGM flares and appears to be in complete remission.
COMMENT
We report 3 cases of IGM, which contribute to the literature on possible presentations, causes, and conservative treatment of this rare connective-tissue disorder.
Differential Diagnosis
The time between recognition of symptoms and diagnosis and treatment of IGM often is prolonged because IGM can present similarly to other disorders, such as infection, breast cancer, tuberculosis, and sarcoidosis. Idiopathic granulomatous mastitis is a diagnosis of exclusion, made after obtaining evidence of granulomatous inflammation on breast biopsy and ruling out other granulomatous disorders, such as tuberculosis and sarcoidosis (Table 1).3,4
Tuberculosis
A full ROS and a PPD test or T-SPOT.TB test can be helpful in ruling out tuberculosis; because anergy occurs in some patients, tuberculosis should be evaluated in the context of known immunosuppression or human immunodeficiency virus status, or in the case of miliary tuberculosis.
Chest radiography findings classically showing upper lobe infiltrates with cavities in active tuberculosis also should be sought.3 Ziehl-Neelsen staining of 2 sputum specimens, assessed by conventional light microscopy at the time of tissue biopsy has 64% sensitivity and 98% specificity for detecting Mycobacterium tuberculosis; auramine O staining, examined with light-emitting diode fluorescence microscopy, has 73% sensitivity and 93% specificity.5
Sarcoidosis
Because more than 90% of sarcoid patients have lung disease, a chest radiograph is used to screen for hilar lymphadenopathy.3 An elevated serum ACE level also can be helpful in diagnosis, but patients do not always have increased ACE, which can occur in other diseases, such as hyperthyroidism and miliary tuberculosis. Sarcoid granulomas can increase active vitamin D production, which in turn increases serum Ca2+ in 10% of sarcoid patients. Last, an ophthalmology evaluation should be obtained to rule out anterior or posterior uveitis that can occur in sarcoidosis and initially remain asymptomatic.3 Once these other causes of granulomatous inflammation have been ruled out, a diagnosis of IGM can be made.
Prolactinoma
Prolactinoma is an important cause of hyperprolactinemia that can be screened for based on ROS and the serum prolactin level. Prolactinoma can cause oligomenorrhea or amenorrhea and galactorrhea in 90% and 80% of premenopausal women, respectively, as well as erectile dysfunction and decreased libido in men. Infertility, headache, and visual impairment may be experienced in both sexes.4
A normal prolactin level is less than 25 μg/L; more than 25 μg/L but less than 100 μg/L usually is due to certain drugs (eTable),6-11 estrogen, or idiopathic reasons; and more than 150 μg/L usually is due to prolactinoma.5 In many cases, removal of hyperprolactinemia-precipitating factors can resolve disease, as in patient 1. If symptoms continue or precipitating factors are absent, IGM symptom-based treatment should be administered.
Course and Management
Idiopathic granulomatous mastitis is self-limited and usually resolves within 2 years. Therefore, the goal of treatment is to suppress associated pain and drainage until the active inflammatory phase of IGM self-resolves. An established protocol for treating IGM does not exist, but common treatments include corticosteroids, methotrexate, and limited or wide surgical excision (Table 2).12-16 Before beginning any of these treatments, IGM triggers, such as breastfeeding and drugs that induce hyperprolactinemia, should be removed.
It is important to consider which treatment option is best for limiting disease recurrence and adverse effects (AEs). Keep in mind that the available data are limited, as there are no randomized controlled trials looking at these treatments. Nevertheless, we recommend methotrexate as first line because it resolves granulomatous inflammation symptoms without invasive surgery, while limiting corticosteroid AEs.12
With or without concurrent use of corticosteroids, surgical excision typically is the mainstay of treatment. However, surgical excision of IGM lesions can be complicated by abscess formation, fistula, and chronic pyogenic secretions, in addition to a 5% to 50% rate of recurrence of disease.12-14 Limited excision often is insufficient; therefore, wide local excision, in which negative margins around granulomatous inflammation are obtained, is the surgical modality of choice.14 Wide local excision can be disfiguring to the breast in young women affected by IGM, making it an undesirable treatment option.
Corticosteroids often have been used to treat IGM, but their efficacy is variable, symptoms can recur upon drug removal, and remarkable AEs can result from long-term use.12 Additionally, corticosteroid therapy often is used in combination with excision, making it difficult to determine the extent to which corticosteroids or excision are more beneficial. In a prospective observational study, corticosteroid therapy alone resolved 80% of IGM symptoms after 159 days on average. After complete symptom resolution, 23% of patients had disease recurrence.9 Observed AEs included gastritis, weight gain, osteoporosis, glucose intolerance, and Cushing syndrome.12,15
Methotrexate for IGM has not been reviewed in a randomized controlled trial; case reports have shown 83% symptom resolution, with 17% recurrence and limited long-term AEs.12 Because the active phase of IGM can persist for 2 years, immunosuppressive therapy with limited AEs is necessary. Many AEs can occur when high-dose methotrexate is given for cancer treatment. Low-dose methotrexate has been extensively studied in long-term treatment of rheumatoid arthritis. Adverse effects may include gastrointestinal tract upset and hepatic dysfunction, which are limited when given with folic acid.
Regardless of folic acid cotreatment, stomatitis may occur. Women should use an effective method of birth control because severe birth defects may occur on even low-dose methotrexate.16
Compared to corticosteroid or surgical treatment, we recommend low-dose methotrexate therapy based on its high efficacy with limited AEs. An occasional mild flare of IGM symptoms with methotrexate is not unusual. If it occurs, corticosteroids can be added and tapered for as long as 2 weeks to speed up resolution of flares while reducing long-term AEs of corticosteroids.
Surgical excision can be performed in cases refractory to all systemic therapies.
CONCLUSION
Idiopathic granulomatous mastitis is a rare granulomatous breast disorder that can have a prolonged time to diagnosis, delaying proper treatment. Many cases self-resolve, but more severe cases can persist for a long period before adequate symptomatic treatment is achieved by methotrexate, corticosteroids, or surgical excision. Before using these therapies, it is important to identify and remove contributing factors, such as long-term breastfeeding and drugs that induce hyperprolactinemia. Improving the rate of IGM diagnosis and treatment would greatly benefit these patients. We report 1 case in which removal of possible precipitating IGM factors led to symptom resolution and 2 cases in which methotrexate was an effective IGM treatment that limited the need for invasive procedures and corticosteroid AEs.
Idiopathic granulomatous mastitis (IGM) is rare during pregnancy; it typically is seen in women of childbearing potential from 6 months to 6 years postpartum.1 Because of a temporal association with breastfeeding, it is believed that hyperprolactinemia2 or an immune response to local lobular secretions might play a role in pathogenesis. Early misdiagnosis as bacterial mastitis is common, prompting multiple antibiotic regimens. When antibiotics fail, patients are worked up for inflammatory breast cancer, given the nonhealing breast nodules. Mammography, ultrasonography, and fine-needle aspiration often are unable to rule out carcinoma, warranting excisional biopsies of nodules. The patient is then referred to rheumatology for potential sarcoidosis or to dermatology for IGM. In either case, the workup should be similar, but additional history focused on behavior and medications is essential in suspected IGM, given the association with hyperprolactinemia.
Because IGM is rare, there are no randomized, placebo-controlled trials of treatment efficacy. In many cases, patients undergo complete mastectomy, which is curative but may be psychologically and physically impactful in young women. In some cases, high-dose corticosteroids have been successful; however, because the IGM process can last longer than 2 years, patients treated in this manner are exposed to steroid morbidities.1
We report 3 cases of IGM that add to the literature on possible contributing factors, clinical presentations, and treatments for this disease. We also demonstrate that appropriate trigger identification and steroid-sparing agents, specifically methotrexate, can be breast-saving as they can alleviate this debilitating condition, obviating the need for radical surgical intervention.
CASE REPORTS
Patient 1
A 40-year-old woman with a 4-year history of breastfeeding noted a grape-sized nodule on the left breast that grew to the size of a grapefruit after 2 weeks. Ulceration and drainage periodically occurred, forming pink plaques along the lateral aspects of the breast after healing. Her primary care provider suspected infectious mastitis; she was given an oral antibiotic (cephalexin) and intravenous antibiotics without improvement.
Imaging
Subsequent magnetic resonance imaging revealed a large, irregular, enhancing mass within the outer left breast (6.5 cm at greatest dimension) with additional surrounding amorphous enhancement highly suspicious for malignancy. There also were multiple prominent left axillary lymph nodes, with the largest demonstrating a cortical thickness of 8 mm.
Biopsy
Core breast biopsy showed benign tissue with fat necrosis. Fine-needle aspiration revealed few benign ductal cells and rare histiocytes; because these findings were nondiagnostic and cancer was still a consideration, the patient underwent excisional biopsy.
Histologic sections of breast tissue showed extensive lobulocentric inflammation comprising histiocytes and lymphocytes, with neutrophils admixed and forming microabscesses (Figure 1A). Multinucleated giant cells and single-cell necrosis were seen, but true caseous necrosis was absent (Figure 1B). Duct spaces often contained inflammatory cells or secretions. Special stains for fungal and acid-fast bacterial microorganisms were negative.
Referral to Dermatology
Granulomatous lobular mastitis was diagnosed, and the patient was referred to dermatology. On presentation to dermatology, the left breast showed a 6-cm area of firm induration and overlying peau d’orange change to the epidermis (Figure 2A). Based on pathologic analysis, she was worked up for a possible granulomatous etiology. Negative purified protein derivative (tuberculin)(PPD) and a normal chest radiograph ruled out tuberculosis. Normal chest radiography, serum Ca2+ and angiotensin-converting enzyme (ACE) levels, and ophthalmology examination ruled out sarcoidosis.
The patient reported she continued breastfeeding her 4-year-old son. Additionally, she had been started on trazadone and buspirone for alcohol abuse recovery, then switched to and maintained on fluoxetine 1 year before developing these symptoms.
Buspirone, fluoxetine, and prolonged breastfeeding all contribute to hyperprolactinemia, a possible trigger of IGM. The patient was therefore advised to stop breastfeeding and to be switched from fluoxetine to a medication that would not increase the prolactin level. She did not require methotrexate treatment because her condition resolved rapidly after breastfeeding and fluoxetine were discontinued (Figure 2B).
B, Resolution after discontinuation of breastfeeding and fluoxetine.
Patient 2
A 40-year-old woman with no history of breastfeeding who gave birth 4.5 years prior presented to her primary care provider with a painful breast lump and rash on the right breast of 2 months’ duration. Infectious mastitis was suspected; she was given cephalexin and clindamycin without improvement of symptoms.
Imaging
Mammography and ultrasonography were nondiagnostic.
Biopsy
Breast biopsy showed tissue with large expanses of histiocytes, neutrophils, lymphocytes, plasma cells, and multinucleated giant cells (Figure 3A). Many discrete granulomas were seen against this mixed inflammatory background, associated with focal fat necrosis (Figure 3B). Special stains were negative for microorganisms. Histologic findings were consistent with granulomatous mastitis.
Referral to Dermatology
On presentation to dermatology, the patient was worked up for a possible granulomatous etiology, which included a negative PPD, as well as a normal chest radiograph, serum Ca2+ and ACE levels, and ophthalmology examination. Review of symptoms (ROS),medical history, and medication review were unremarkable.
By exclusion, the patient was given a diagnosis of IGM and started on methotrexate (15 mg weekly) with folic acid (1 mg daily). The condition of the right breast improved within 4 weeks of starting methotrexate; however, methotrexate was increased to 30 mg weekly because of occasional flares. The patient remained on methotrexate without further IGM flares for 8 months compared to prior unremitting pain and drainage. She was then tapered from methotrexate over 6 weeks without additional flares.
Patient 3
A 27-year-old woman who gave birth 2 years prior and discontinued breastfeeding 6 weeks after delivery noted bilateral breast rashes for several months. The lesions were growing in size, tender, and draining. Her primary care provider suspected infectious mastitis and prescribed antibiotics, which were ineffective.
Biopsy
Breast core biopsy showed histologic findings similar to patients 1 and 2, including lobulocentric mixed inflammation, neutrophilic microabscesses, and scattered discrete granulomas. Microorganisms were not found using special stains. Breast cancer was ruled out, and granulomatous mastitis was diagnosed.
Referral to Dermatology
Two years earlier, the patient tested positive for latent tuberculosis and was prescribed a 9-month regimen of isoniazid. At the current presentation, she did not have symptoms of active tuberculosis on ROS (ie, no cough, hemoptysis, weight loss, night sweats); a chest radiograph was normal. Additionally, serum Ca2+ and ACE levels as well as an ophthalmology examination were normal, and she was not taking any medications known to increase the prolactin level.
The patient was started on methotrexate (12.5 mg weekly) and folic acid (1 mg daily). She had 1 IGM flare and was given a tapering regimen of prednisone. She received methotrexate for 14 months, tapered during the final 3 months. She has been off methotrexate for 3 years without IGM flares and appears to be in complete remission.
COMMENT
We report 3 cases of IGM, which contribute to the literature on possible presentations, causes, and conservative treatment of this rare connective-tissue disorder.
Differential Diagnosis
The time between recognition of symptoms and diagnosis and treatment of IGM often is prolonged because IGM can present similarly to other disorders, such as infection, breast cancer, tuberculosis, and sarcoidosis. Idiopathic granulomatous mastitis is a diagnosis of exclusion, made after obtaining evidence of granulomatous inflammation on breast biopsy and ruling out other granulomatous disorders, such as tuberculosis and sarcoidosis (Table 1).3,4
Tuberculosis
A full ROS and a PPD test or T-SPOT.TB test can be helpful in ruling out tuberculosis; because anergy occurs in some patients, tuberculosis should be evaluated in the context of known immunosuppression or human immunodeficiency virus status, or in the case of miliary tuberculosis.
Chest radiography findings classically showing upper lobe infiltrates with cavities in active tuberculosis also should be sought.3 Ziehl-Neelsen staining of 2 sputum specimens, assessed by conventional light microscopy at the time of tissue biopsy has 64% sensitivity and 98% specificity for detecting Mycobacterium tuberculosis; auramine O staining, examined with light-emitting diode fluorescence microscopy, has 73% sensitivity and 93% specificity.5
Sarcoidosis
Because more than 90% of sarcoid patients have lung disease, a chest radiograph is used to screen for hilar lymphadenopathy.3 An elevated serum ACE level also can be helpful in diagnosis, but patients do not always have increased ACE, which can occur in other diseases, such as hyperthyroidism and miliary tuberculosis. Sarcoid granulomas can increase active vitamin D production, which in turn increases serum Ca2+ in 10% of sarcoid patients. Last, an ophthalmology evaluation should be obtained to rule out anterior or posterior uveitis that can occur in sarcoidosis and initially remain asymptomatic.3 Once these other causes of granulomatous inflammation have been ruled out, a diagnosis of IGM can be made.
Prolactinoma
Prolactinoma is an important cause of hyperprolactinemia that can be screened for based on ROS and the serum prolactin level. Prolactinoma can cause oligomenorrhea or amenorrhea and galactorrhea in 90% and 80% of premenopausal women, respectively, as well as erectile dysfunction and decreased libido in men. Infertility, headache, and visual impairment may be experienced in both sexes.4
A normal prolactin level is less than 25 μg/L; more than 25 μg/L but less than 100 μg/L usually is due to certain drugs (eTable),6-11 estrogen, or idiopathic reasons; and more than 150 μg/L usually is due to prolactinoma.5 In many cases, removal of hyperprolactinemia-precipitating factors can resolve disease, as in patient 1. If symptoms continue or precipitating factors are absent, IGM symptom-based treatment should be administered.
Course and Management
Idiopathic granulomatous mastitis is self-limited and usually resolves within 2 years. Therefore, the goal of treatment is to suppress associated pain and drainage until the active inflammatory phase of IGM self-resolves. An established protocol for treating IGM does not exist, but common treatments include corticosteroids, methotrexate, and limited or wide surgical excision (Table 2).12-16 Before beginning any of these treatments, IGM triggers, such as breastfeeding and drugs that induce hyperprolactinemia, should be removed.
It is important to consider which treatment option is best for limiting disease recurrence and adverse effects (AEs). Keep in mind that the available data are limited, as there are no randomized controlled trials looking at these treatments. Nevertheless, we recommend methotrexate as first line because it resolves granulomatous inflammation symptoms without invasive surgery, while limiting corticosteroid AEs.12
With or without concurrent use of corticosteroids, surgical excision typically is the mainstay of treatment. However, surgical excision of IGM lesions can be complicated by abscess formation, fistula, and chronic pyogenic secretions, in addition to a 5% to 50% rate of recurrence of disease.12-14 Limited excision often is insufficient; therefore, wide local excision, in which negative margins around granulomatous inflammation are obtained, is the surgical modality of choice.14 Wide local excision can be disfiguring to the breast in young women affected by IGM, making it an undesirable treatment option.
Corticosteroids often have been used to treat IGM, but their efficacy is variable, symptoms can recur upon drug removal, and remarkable AEs can result from long-term use.12 Additionally, corticosteroid therapy often is used in combination with excision, making it difficult to determine the extent to which corticosteroids or excision are more beneficial. In a prospective observational study, corticosteroid therapy alone resolved 80% of IGM symptoms after 159 days on average. After complete symptom resolution, 23% of patients had disease recurrence.9 Observed AEs included gastritis, weight gain, osteoporosis, glucose intolerance, and Cushing syndrome.12,15
Methotrexate for IGM has not been reviewed in a randomized controlled trial; case reports have shown 83% symptom resolution, with 17% recurrence and limited long-term AEs.12 Because the active phase of IGM can persist for 2 years, immunosuppressive therapy with limited AEs is necessary. Many AEs can occur when high-dose methotrexate is given for cancer treatment. Low-dose methotrexate has been extensively studied in long-term treatment of rheumatoid arthritis. Adverse effects may include gastrointestinal tract upset and hepatic dysfunction, which are limited when given with folic acid.
Regardless of folic acid cotreatment, stomatitis may occur. Women should use an effective method of birth control because severe birth defects may occur on even low-dose methotrexate.16
Compared to corticosteroid or surgical treatment, we recommend low-dose methotrexate therapy based on its high efficacy with limited AEs. An occasional mild flare of IGM symptoms with methotrexate is not unusual. If it occurs, corticosteroids can be added and tapered for as long as 2 weeks to speed up resolution of flares while reducing long-term AEs of corticosteroids.
Surgical excision can be performed in cases refractory to all systemic therapies.
CONCLUSION
Idiopathic granulomatous mastitis is a rare granulomatous breast disorder that can have a prolonged time to diagnosis, delaying proper treatment. Many cases self-resolve, but more severe cases can persist for a long period before adequate symptomatic treatment is achieved by methotrexate, corticosteroids, or surgical excision. Before using these therapies, it is important to identify and remove contributing factors, such as long-term breastfeeding and drugs that induce hyperprolactinemia. Improving the rate of IGM diagnosis and treatment would greatly benefit these patients. We report 1 case in which removal of possible precipitating IGM factors led to symptom resolution and 2 cases in which methotrexate was an effective IGM treatment that limited the need for invasive procedures and corticosteroid AEs.
1. Patel RA, Strickland P, Sankara IR, et al. Idiopathic granulomatous mastitis: case reports and review of literature. J Gen Intern Med. 2010;25:270-273.
2. Bellavia M, Damiano G, Palumbo VD, et al. Granulomatous mastitis during chronic antidepressant therapy: is it possible a conservative therapeutic approach? J Breast Cancer. 2012;15:371-372.
3. Longo D, Fauci A, Kasper D, et al. Harrison’s Principles of Internal Medicine. 18th ed. New York, NY: McGraw-Hill; 2012.
4. Davis JL, Cattamanchi A, Cuevas LE, et al. Diagnostic accuracy of same-day microscopy versus standard microscopy for pulmonary tuberculosis: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13:147-154.
5. Casanueva FF, Molitch ME, Schlechte JA, et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf). 2006;65:265-273.
6. Akbulut S, Arikanoglu Z, Senol A, et al. Is methotrexate an acceptable treatment in the management of idiopathic granulomatous mastitis? Arch Gynecol Obstet. 2011;284:1189-1195.
7. Bani-Hani KE, Yaghan RJ, Matalka II, et al. Idiopathic granulomatous mastitis: time to avoid unnecessary mastectomies. Breast J. 2004;10:318-322.
8. Asoglu O, Ozmen V, Karanlik H, et al. Feasibility of surgical management in patients with granulomatous mastitis. Breast J. 2005;11:108-114.
9. Pandey TS, Mackinnon JC, Bressler L, et al. Idiopathic granulomatous mastitis—a prospective study of 49 women and treatment outcomes with steroid therapy. Breast J. 2014;20:258-266.
10. Shea B, Swinden MV, Tanjong Ghogomu E, et al. Folic acid and folinic acid for reducing side effects in patients receiving methotrexate for rheumatoid arthritis. Cochrane Database Syst Rev. 2013;5:CD000951.
11. Molitch ME. Drugs and prolactin. Pituitary. 2008;11:209-218.
12.
13.
14.
15.
16.
1. Patel RA, Strickland P, Sankara IR, et al. Idiopathic granulomatous mastitis: case reports and review of literature. J Gen Intern Med. 2010;25:270-273.
2. Bellavia M, Damiano G, Palumbo VD, et al. Granulomatous mastitis during chronic antidepressant therapy: is it possible a conservative therapeutic approach? J Breast Cancer. 2012;15:371-372.
3. Longo D, Fauci A, Kasper D, et al. Harrison’s Principles of Internal Medicine. 18th ed. New York, NY: McGraw-Hill; 2012.
4. Davis JL, Cattamanchi A, Cuevas LE, et al. Diagnostic accuracy of same-day microscopy versus standard microscopy for pulmonary tuberculosis: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13:147-154.
5. Casanueva FF, Molitch ME, Schlechte JA, et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf). 2006;65:265-273.
6. Akbulut S, Arikanoglu Z, Senol A, et al. Is methotrexate an acceptable treatment in the management of idiopathic granulomatous mastitis? Arch Gynecol Obstet. 2011;284:1189-1195.
7. Bani-Hani KE, Yaghan RJ, Matalka II, et al. Idiopathic granulomatous mastitis: time to avoid unnecessary mastectomies. Breast J. 2004;10:318-322.
8. Asoglu O, Ozmen V, Karanlik H, et al. Feasibility of surgical management in patients with granulomatous mastitis. Breast J. 2005;11:108-114.
9. Pandey TS, Mackinnon JC, Bressler L, et al. Idiopathic granulomatous mastitis—a prospective study of 49 women and treatment outcomes with steroid therapy. Breast J. 2014;20:258-266.
10. Shea B, Swinden MV, Tanjong Ghogomu E, et al. Folic acid and folinic acid for reducing side effects in patients receiving methotrexate for rheumatoid arthritis. Cochrane Database Syst Rev. 2013;5:CD000951.
11. Molitch ME. Drugs and prolactin. Pituitary. 2008;11:209-218.
12.
13.
14.
15.
16.
Practice Points
- Idiopathic granulomatous mastitis (IGM) is a painful and scarring rare granulomatous breast disorder that can have a prolonged time to diagnosis that delays proper treatment.
- The pathogenesis of IGM remains poorly understood. The temporal association of the disorder with breastfeeding suggests that hyperprolactinemia or an immune response to local lobular secretions might play a role.
- Although many cases of IGM resolve without treatment, more severe cases can persist for a long period before adequate symptomatic treatment is provided with methotrexate, corticosteroids, or surgical excision.
- Before any of these therapies are applied, however, contributing factors, such as long-term breastfeeding and drugs that induce hyperprolactinemia, should be identified and withdrawn.