User login
Death while on clozapine for schizophrenia is often associated with substandard treatment of cardiometabolic risk factors, Sharon Taub, MD, reported at the virtual congress of the European College of Neuropsychopharmacology.
“Inadequate treatment for metabolic syndrome was found to be a mortality predictor while on clozapine therapy. Patients who died were less likely to receive appropriate treatment for hyperlipidemia and type 2 diabetes, despite having been diagnosed with those conditions,” she said in presenting the results of her retrospective cohort study.
“Better preventive care, with special attention to those conditions, might prevent morbidity and improve life expectancy in this population,” concluded Dr. Taub of Geha Mental Health Center in Petah Tikva, Israel, and Tel Aviv University.
She reported on all 1,817 patients on clozapine for schizophrenia included in a large Israeli health care electronic medical records database, of whom 112, or 6.2%, died during 2 years of follow-up. Mortality while on the atypical antipsychotic was associated with a higher prevalence of hyperlipidemia, type 2 diabetes, hypertension, known ischemic heart disease, and a history of acute MI, compared with survivors.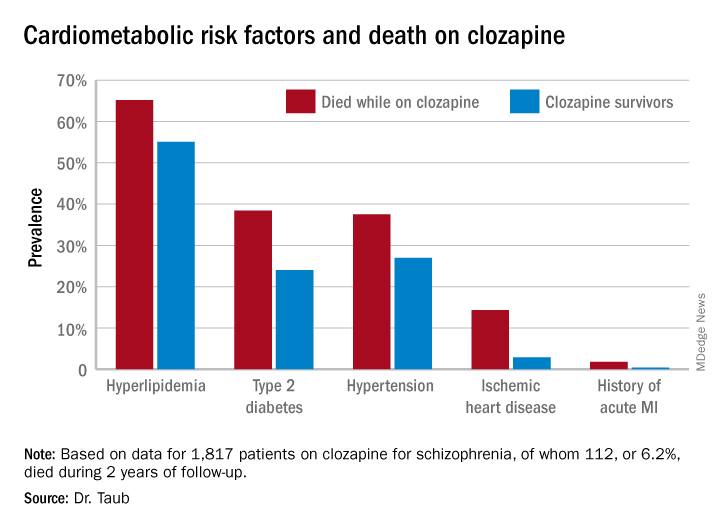
Similarly, only 16.3% of those known to have type 2 diabetes who died while on clozapine were on hypoglycemic agents, compared with 67.1% of diabetic survivors. The between-group difference in the use of antihypertensive drug therapy for patients diagnosed with hypertension – 28.6% in nonsurvivors on clozapine, 40.1% in survivors – did not achieve statistical significance.
In a multivariate analysis adjusted for age, sex, and socioeconomic status, schizophrenia patients with type 2 diabetes who weren’t on hypoglycemic medication were at 695% increased risk of mortality, compared with those who were. Similarly, hyperlipidemic patients on clozapine who weren’t on a statin had a 579% increase in mortality risk.
Patients who died while on clozapine had no increased risk of use of medical services while living in the community.
This evidence of a pattern of inadequate care with regard to management of cardiometabolic risk factors in patients on clozapine is disturbing for several reasons. For one, clozapine is known to be associated with increased risk of serious side effects, including development or worsening of metabolic syndrome. Also, clozapine is an important drug in psychiatric practice: “Clozapine is the only antipsychotic indicated for refractory schizophrenia. It is highly effective in treatment-resistant disease, present in 25%-30% of individuals with schizophrenia,” Dr. Taub noted. “Clozapine is underused, mostly because of severe side effects. Its administration is often postponed.”
She reported having no financial conflicts regarding her study, which was voted by conference attendees one of the top presentations at ECNP 2020.
Death while on clozapine for schizophrenia is often associated with substandard treatment of cardiometabolic risk factors, Sharon Taub, MD, reported at the virtual congress of the European College of Neuropsychopharmacology.
“Inadequate treatment for metabolic syndrome was found to be a mortality predictor while on clozapine therapy. Patients who died were less likely to receive appropriate treatment for hyperlipidemia and type 2 diabetes, despite having been diagnosed with those conditions,” she said in presenting the results of her retrospective cohort study.
“Better preventive care, with special attention to those conditions, might prevent morbidity and improve life expectancy in this population,” concluded Dr. Taub of Geha Mental Health Center in Petah Tikva, Israel, and Tel Aviv University.
She reported on all 1,817 patients on clozapine for schizophrenia included in a large Israeli health care electronic medical records database, of whom 112, or 6.2%, died during 2 years of follow-up. Mortality while on the atypical antipsychotic was associated with a higher prevalence of hyperlipidemia, type 2 diabetes, hypertension, known ischemic heart disease, and a history of acute MI, compared with survivors.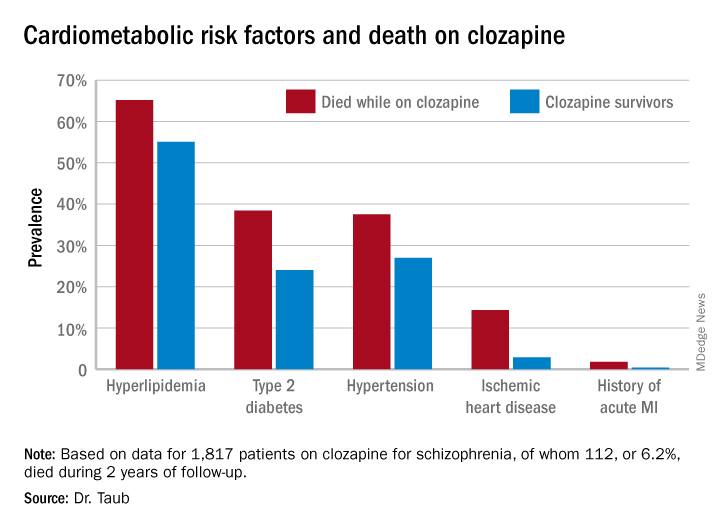
Similarly, only 16.3% of those known to have type 2 diabetes who died while on clozapine were on hypoglycemic agents, compared with 67.1% of diabetic survivors. The between-group difference in the use of antihypertensive drug therapy for patients diagnosed with hypertension – 28.6% in nonsurvivors on clozapine, 40.1% in survivors – did not achieve statistical significance.
In a multivariate analysis adjusted for age, sex, and socioeconomic status, schizophrenia patients with type 2 diabetes who weren’t on hypoglycemic medication were at 695% increased risk of mortality, compared with those who were. Similarly, hyperlipidemic patients on clozapine who weren’t on a statin had a 579% increase in mortality risk.
Patients who died while on clozapine had no increased risk of use of medical services while living in the community.
This evidence of a pattern of inadequate care with regard to management of cardiometabolic risk factors in patients on clozapine is disturbing for several reasons. For one, clozapine is known to be associated with increased risk of serious side effects, including development or worsening of metabolic syndrome. Also, clozapine is an important drug in psychiatric practice: “Clozapine is the only antipsychotic indicated for refractory schizophrenia. It is highly effective in treatment-resistant disease, present in 25%-30% of individuals with schizophrenia,” Dr. Taub noted. “Clozapine is underused, mostly because of severe side effects. Its administration is often postponed.”
She reported having no financial conflicts regarding her study, which was voted by conference attendees one of the top presentations at ECNP 2020.
Death while on clozapine for schizophrenia is often associated with substandard treatment of cardiometabolic risk factors, Sharon Taub, MD, reported at the virtual congress of the European College of Neuropsychopharmacology.
“Inadequate treatment for metabolic syndrome was found to be a mortality predictor while on clozapine therapy. Patients who died were less likely to receive appropriate treatment for hyperlipidemia and type 2 diabetes, despite having been diagnosed with those conditions,” she said in presenting the results of her retrospective cohort study.
“Better preventive care, with special attention to those conditions, might prevent morbidity and improve life expectancy in this population,” concluded Dr. Taub of Geha Mental Health Center in Petah Tikva, Israel, and Tel Aviv University.
She reported on all 1,817 patients on clozapine for schizophrenia included in a large Israeli health care electronic medical records database, of whom 112, or 6.2%, died during 2 years of follow-up. Mortality while on the atypical antipsychotic was associated with a higher prevalence of hyperlipidemia, type 2 diabetes, hypertension, known ischemic heart disease, and a history of acute MI, compared with survivors.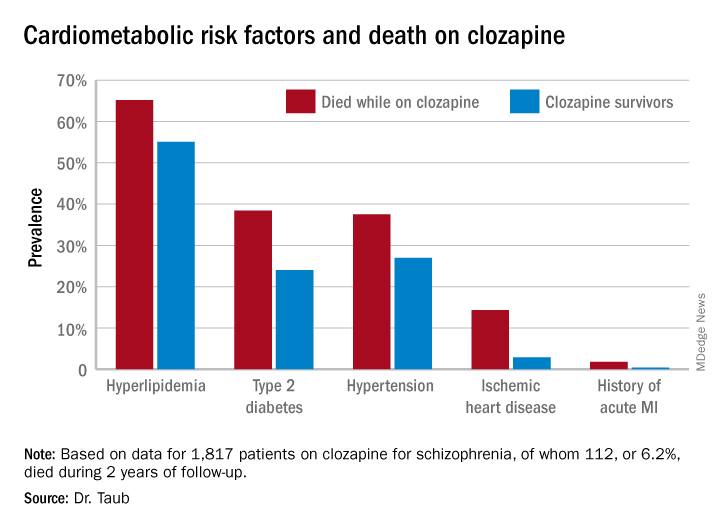
Similarly, only 16.3% of those known to have type 2 diabetes who died while on clozapine were on hypoglycemic agents, compared with 67.1% of diabetic survivors. The between-group difference in the use of antihypertensive drug therapy for patients diagnosed with hypertension – 28.6% in nonsurvivors on clozapine, 40.1% in survivors – did not achieve statistical significance.
In a multivariate analysis adjusted for age, sex, and socioeconomic status, schizophrenia patients with type 2 diabetes who weren’t on hypoglycemic medication were at 695% increased risk of mortality, compared with those who were. Similarly, hyperlipidemic patients on clozapine who weren’t on a statin had a 579% increase in mortality risk.
Patients who died while on clozapine had no increased risk of use of medical services while living in the community.
This evidence of a pattern of inadequate care with regard to management of cardiometabolic risk factors in patients on clozapine is disturbing for several reasons. For one, clozapine is known to be associated with increased risk of serious side effects, including development or worsening of metabolic syndrome. Also, clozapine is an important drug in psychiatric practice: “Clozapine is the only antipsychotic indicated for refractory schizophrenia. It is highly effective in treatment-resistant disease, present in 25%-30% of individuals with schizophrenia,” Dr. Taub noted. “Clozapine is underused, mostly because of severe side effects. Its administration is often postponed.”
She reported having no financial conflicts regarding her study, which was voted by conference attendees one of the top presentations at ECNP 2020.
FROM ECNP 2020