User login
A new study involving both human patients and mice has confirmed a long-believed association between nonalcoholic fatty liver disease (NAFLD) and an alteration in the gut microbiome that produces high levels of alcohol.
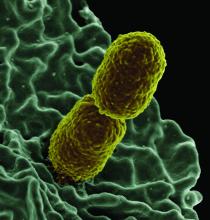
The study was initiated after the treatment of a rare case: a patient who presented with severe nonalcoholic steatohepatitis (NASH) plus auto-brewery syndrome. The patient had a very high blood alcohol concentration but an alcohol-free, high-carbohydrate diet. It was determined that strains of high alcohol-producing Klebsiella pneumoniae (HiAlc Kpn) rather than a fungal infection were the catalyst for the high blood alcohol level. As such, Jing Yuan of the Capital Institute of Pediatrics in Beijing and coauthors attempted to “connect these commensal HiAlc Kpn to the pathogenesis of hepatic damage” through this study, which was published in Cell Metabolism.
The researchers began by examining 43 patients with NAFLD and 48 healthy controls. Among the patients with NAFLD, 11 had nonalcoholic fatty liver and 32 had NASH. Specifically, they analyzed the presence and effects of HiAlc Kpn, determining that the abundance of Klebsiella pneumoniae was slightly higher in the feces of NAFLD patients, compared with healthy patients, but that their alcohol-producing ability in NAFLD patients was significantly stronger. Of the patients with NAFLD, 61% carried HiAlc and medium-alcohol-producing Kpn, compared with 6.25% of the controls.
Another phase of their study involved feeding specific pathogen-free mice either HiAlc Kpn, ethanol, or yeast extract peptone dextrose medium (pair-fed) for 4, 6, and 8 weeks. The mice that were fed HiAlc Kpn or ethanol showed clear microsteatosis and macrosteatosis in their livers at 4 and 8 weeks, compared with the pair-fed mice. In addition, the HiAlc-Kpn-fed and ethanol-fed mice had increased levels of aspartate transaminase and alanine transaminase in their serum and increased levels of triglycerides and thiobarbituric acid reactive substances in their liver. The results overall indicated that the HiAlc-Kpn-fed mice had developed hepatic steatosis.
An additional phase included the intestinal flora from a NASH patient with a specific Kpn strain being fed to germ-free mice. At the same time, two types of intestinal flora from mice with NAFLD were transplanted into healthy mice: one induced by two other specific Kpn strains and one in which those strains had been selectively eliminated. The results saw obvious steatosis in the mice who received the flora from either mice with NAFLD induced by Kpn or the NASH patient at 4 weeks and 8 weeks, respectively. The mice who received the flora win which Kpn had been eliminated saw no fat-related changes in the liver. “These results further suggest that HiAlc Kpn might be one of the major causes of NAFLD development,” the researchers wrote.
The authors acknowledged the study’s limitations, chiefly including the lack of a clinical cohort of individuals with auto brewery syndrome but without NAFLD that could be used as a control. However, they also noted a belief that “causality was shown by the transfer experiments of HiAlc Kpn” while adding that “the further analysis of the impact of ethanol in ABS [auto brewery syndrome] patients should be investigated.”
The study was funded by grants from the National Natural Science Foundation for Key Programs of China, the National Natural Science Foundation of China, Megaprojects of Science and Technology Research of China, and CAMS Innovation Fund for Medical Sciences. The authors reported no conflicts of interest.
SOURCE: Yuan J et al. Cell Metab. 2019 Sep 19. doi: 10.1016/j.cmet.2019.08.018.
A new study involving both human patients and mice has confirmed a long-believed association between nonalcoholic fatty liver disease (NAFLD) and an alteration in the gut microbiome that produces high levels of alcohol.
The study was initiated after the treatment of a rare case: a patient who presented with severe nonalcoholic steatohepatitis (NASH) plus auto-brewery syndrome. The patient had a very high blood alcohol concentration but an alcohol-free, high-carbohydrate diet. It was determined that strains of high alcohol-producing Klebsiella pneumoniae (HiAlc Kpn) rather than a fungal infection were the catalyst for the high blood alcohol level. As such, Jing Yuan of the Capital Institute of Pediatrics in Beijing and coauthors attempted to “connect these commensal HiAlc Kpn to the pathogenesis of hepatic damage” through this study, which was published in Cell Metabolism.
The researchers began by examining 43 patients with NAFLD and 48 healthy controls. Among the patients with NAFLD, 11 had nonalcoholic fatty liver and 32 had NASH. Specifically, they analyzed the presence and effects of HiAlc Kpn, determining that the abundance of Klebsiella pneumoniae was slightly higher in the feces of NAFLD patients, compared with healthy patients, but that their alcohol-producing ability in NAFLD patients was significantly stronger. Of the patients with NAFLD, 61% carried HiAlc and medium-alcohol-producing Kpn, compared with 6.25% of the controls.
Another phase of their study involved feeding specific pathogen-free mice either HiAlc Kpn, ethanol, or yeast extract peptone dextrose medium (pair-fed) for 4, 6, and 8 weeks. The mice that were fed HiAlc Kpn or ethanol showed clear microsteatosis and macrosteatosis in their livers at 4 and 8 weeks, compared with the pair-fed mice. In addition, the HiAlc-Kpn-fed and ethanol-fed mice had increased levels of aspartate transaminase and alanine transaminase in their serum and increased levels of triglycerides and thiobarbituric acid reactive substances in their liver. The results overall indicated that the HiAlc-Kpn-fed mice had developed hepatic steatosis.
An additional phase included the intestinal flora from a NASH patient with a specific Kpn strain being fed to germ-free mice. At the same time, two types of intestinal flora from mice with NAFLD were transplanted into healthy mice: one induced by two other specific Kpn strains and one in which those strains had been selectively eliminated. The results saw obvious steatosis in the mice who received the flora from either mice with NAFLD induced by Kpn or the NASH patient at 4 weeks and 8 weeks, respectively. The mice who received the flora win which Kpn had been eliminated saw no fat-related changes in the liver. “These results further suggest that HiAlc Kpn might be one of the major causes of NAFLD development,” the researchers wrote.
The authors acknowledged the study’s limitations, chiefly including the lack of a clinical cohort of individuals with auto brewery syndrome but without NAFLD that could be used as a control. However, they also noted a belief that “causality was shown by the transfer experiments of HiAlc Kpn” while adding that “the further analysis of the impact of ethanol in ABS [auto brewery syndrome] patients should be investigated.”
The study was funded by grants from the National Natural Science Foundation for Key Programs of China, the National Natural Science Foundation of China, Megaprojects of Science and Technology Research of China, and CAMS Innovation Fund for Medical Sciences. The authors reported no conflicts of interest.
SOURCE: Yuan J et al. Cell Metab. 2019 Sep 19. doi: 10.1016/j.cmet.2019.08.018.
A new study involving both human patients and mice has confirmed a long-believed association between nonalcoholic fatty liver disease (NAFLD) and an alteration in the gut microbiome that produces high levels of alcohol.
The study was initiated after the treatment of a rare case: a patient who presented with severe nonalcoholic steatohepatitis (NASH) plus auto-brewery syndrome. The patient had a very high blood alcohol concentration but an alcohol-free, high-carbohydrate diet. It was determined that strains of high alcohol-producing Klebsiella pneumoniae (HiAlc Kpn) rather than a fungal infection were the catalyst for the high blood alcohol level. As such, Jing Yuan of the Capital Institute of Pediatrics in Beijing and coauthors attempted to “connect these commensal HiAlc Kpn to the pathogenesis of hepatic damage” through this study, which was published in Cell Metabolism.
The researchers began by examining 43 patients with NAFLD and 48 healthy controls. Among the patients with NAFLD, 11 had nonalcoholic fatty liver and 32 had NASH. Specifically, they analyzed the presence and effects of HiAlc Kpn, determining that the abundance of Klebsiella pneumoniae was slightly higher in the feces of NAFLD patients, compared with healthy patients, but that their alcohol-producing ability in NAFLD patients was significantly stronger. Of the patients with NAFLD, 61% carried HiAlc and medium-alcohol-producing Kpn, compared with 6.25% of the controls.
Another phase of their study involved feeding specific pathogen-free mice either HiAlc Kpn, ethanol, or yeast extract peptone dextrose medium (pair-fed) for 4, 6, and 8 weeks. The mice that were fed HiAlc Kpn or ethanol showed clear microsteatosis and macrosteatosis in their livers at 4 and 8 weeks, compared with the pair-fed mice. In addition, the HiAlc-Kpn-fed and ethanol-fed mice had increased levels of aspartate transaminase and alanine transaminase in their serum and increased levels of triglycerides and thiobarbituric acid reactive substances in their liver. The results overall indicated that the HiAlc-Kpn-fed mice had developed hepatic steatosis.
An additional phase included the intestinal flora from a NASH patient with a specific Kpn strain being fed to germ-free mice. At the same time, two types of intestinal flora from mice with NAFLD were transplanted into healthy mice: one induced by two other specific Kpn strains and one in which those strains had been selectively eliminated. The results saw obvious steatosis in the mice who received the flora from either mice with NAFLD induced by Kpn or the NASH patient at 4 weeks and 8 weeks, respectively. The mice who received the flora win which Kpn had been eliminated saw no fat-related changes in the liver. “These results further suggest that HiAlc Kpn might be one of the major causes of NAFLD development,” the researchers wrote.
The authors acknowledged the study’s limitations, chiefly including the lack of a clinical cohort of individuals with auto brewery syndrome but without NAFLD that could be used as a control. However, they also noted a belief that “causality was shown by the transfer experiments of HiAlc Kpn” while adding that “the further analysis of the impact of ethanol in ABS [auto brewery syndrome] patients should be investigated.”
The study was funded by grants from the National Natural Science Foundation for Key Programs of China, the National Natural Science Foundation of China, Megaprojects of Science and Technology Research of China, and CAMS Innovation Fund for Medical Sciences. The authors reported no conflicts of interest.
SOURCE: Yuan J et al. Cell Metab. 2019 Sep 19. doi: 10.1016/j.cmet.2019.08.018.
FROM CELL METABOLISM
Key clinical point: Nonalcoholic fatty liver disease can be caused or exacerbated by excess levels of a high-alcohol-producing bacterial strain.
Major finding: 61% of patients with NAFLD carried high alcohol- and medium alcohol-producing Klebsiella pneumoniae (HiAlc Kpn), compared to 6.25% of healthy controls.
Study details: A multiphase study that included analysis of a 43-patient cohort with nonalcoholic fatty liver disease as well as experiments with mice and HiAlc Kpn.
Disclosures: The study was funded by grants from the National Natural Science Foundation for Key Programs of China, the National Natural Science Foundation of China, Megaprojects of Science and Technology Research of China, and CAMS Innovation Fund for Medical Sciences. The authors reported no conflicts of interest.
Source: Yuan J et al. Cell Metab. 2019 Sep 19. doi: 10.1016/j.cmet.2019.08.018.