User login
Ulcerative colitis (UC) is a chronic inflammatory condition of the colonic mucosa. Classically, it starts in the rectum and can extend continuously from the distal to the proximal colon. The defining clinical symptom of UC is bloody diarrhea, typically accompanied by rectal urgency and mucus discharge. The natural history of this disease includes periods of exacerbations and remissions occurring spontaneously or in response to medical treatment.1
Acute severe ulcerative colitis (ASUC) is a potentially life-threatening complication of UC that typically requires hospitalization and interdisciplinary care between hospitalists, gastroenterologists, and colorectal or general surgeons. The risk of a patient with UC requiring hospitalization for ASUC ranges from 15%-25%2,3 and, in total, UC accounts for 30,000 hospital visits annually.4 The direct medical costs exceed $4 billion annually, with hospital costs of over $960 million.5 Historically, mortality from ASUC was as high as 24% but decreased substantially to 7% after the introduction of systemic corticosteroid therapy.6 Further advances in care have reduced mortality to approximately 1% or less.7,8 Nonetheless, up to 20% of patients admitted with ASUC have a colectomy on their first admission, and this rate rises to 40% after two admissions.2
DEFINING ACUTE SEVERE ULCERATIVE COLITIS
To categorize UC severity, assess patients using the Truelove and Witt’s criteria. The system classifies patients as having mild, moderate, severe, or fulminant disease. Severe disease by these criteria includes patients with >6 bloody bowel movements per day and at least one of the following clinical features: fever (>37.8°C), tachycardia (>90 bpm), anemia (hemoglobin <10.5 g/dl), or elevated inflammatory markers (traditionally, erythrocyte sedimentation rate greater than 30 mm/h or, more recently, C-reactive protein (CRP) greater than 30 mg/L. (Table 1).6,9
Fulminant colitis refers to a subgroup of patients with more than 10 stools per day, continuous bleeding, abdominal pain, colonic dilatation on abdominal X-ray film, and severe toxic symptoms including fever and anorexia. Such patients are at risk of progressing to toxic megacolon and bowel perforation.10
INDICATIONS FOR HOSPITALIZATION AND INPATIENT LEVEL OF CARE
Patients with ASUC almost always require hospitalization for their disease management. In many cases, these patients have been receiving outpatient oral prednisone 40-60 mg daily but continue to have ongoing disease activity.11 Most patients will require close clinical monitoring, frequent blood testing, endoscopic or radiologic evaluation, as well as administration of intravenous corticosteroids. The average length of stay (LOS) ranges from 4.6 to 12.5 days, depending on disease severity.12 Not surprisingly, Kelso et al. reported that predictors of hospital LOS greater than four days include initiating a biologic drug in the hospital, undergoing two or more imaging modalities and treatment with intravenous steroids,13 and so it is rare that patients do not meet billing requirements for an inpatient level of care.
INITIAL EVALUATION
The multifaceted initial inpatient evaluation of patients with ASUC aims to assess disease severity, identify and prevent potential complications, and initiate planning for potential failure of first-line pharmacologic therapy. Due to the accumulating evidence that involving physicians with expertise in managing ASUC improves outcomes, gastroenterologists should be involved in the care of patients with ASUC from the time of their admission.14,15 Additionally, creating standardized care pathways for the management of ASUC can reduce cost, LOS, and improve quality.16
History and Physical Examination
Patients should be asked about fever, abdominal pain, nausea, emesis, bloating, weight loss, and bowel movements (frequency, consistency, the presence of blood, urgency, nighttime awakenings). The number of bowel movements over a 24-hour period should be quantified as this helps assess the overall disease severity (Table 1).
The patient’s initial inflammatory bowel disease (IBD) history is also essential. The review of pertinent information regarding the patient’s initial diagnosis of UC includes the severity and anatomic extent of disease, extraintestinal manifestations, previous medical therapies, and surgical interventions. Exposure to nonsteroidal anti-inflammatory drugs (NSAIDs) or antibiotics should be identified as they may precipitate flares.17 Travel history may be pertinent as travel increases the risk of infections with food-borne or parasitic pathogens.18
Physical examination begins with an assessment of vital signs and volume status. Abdominal examination should include evaluation of bowel sounds, an assessment of distention, location, the extent of abdominal tenderness, and peritoneal signs. The abdominal exam should be interpreted in the context of the patient’s medications, as the use of steroid or analgesic therapies may affect the sensitivity for detecting complications. An external rectal exam evaluating perianal disease should be performed, as perianal disease raises concern for Crohn’s, a disease whose surgical management differs from UC.
A careful exam for extraintestinal manifestations is also essential. The skin should be evaluated for any new rashes, especially on the anterior shin consistent with erythema nodosum or ulcerated lesions on the skin suggestive of pyoderma gangrenosum. The peripheral joints should also be examined for any synovitis. Additional examinations should be performed based on any reported symptoms (eg, the ophthalmic exam for uveitis or scleritis if visual changes or eye pain are reported). Some extraintestinal manifestations require subspecialty consultation and comanagement to guide disease therapy. Patients with underlying pyoderma gangrenosum may require a dermatology consultation to guide management. Ocular inflammation requires ophthalmology involvement, and inflammatory arthritis is best comanaged with rheumatology.19
Laboratory Testing
Initial testing should include a complete blood count with differential, basic metabolic panel, and liver chemistries including alkaline phosphatase and albumin. When relevant, pregnancy testing should be performed. Measure CRP on admission so that its trajectory can be followed during therapy. However, a normal CRP does not exclude the presence of a UC flare as a subset of patients with ASUC will have a normal CRP despite severe mucosal inflammation.20
Since one-third of patients do not respond to intravenous corticosteroids and will require rescue therapy during the hospitalization with infliximab or cyclosporine, anticipatory testing for these medications should be performed on admission to avoid delays in the administration of rescue therapy.6,21 This should include an interferon-gamma release assay (eg, quantiferon gold) to test for latent tuberculosis and hepatitis B serologies in anticipation of possible treatment with infliximab. An interferon-gamma release assay is preferred to a tuberculin skin test because patients may be anergic, and a skin test does not provide a control to determine whether a negative test is due to anergy. In contrast, although a quantiferon gold test can be indeterminate in ASUC due to disease activity and systemic steroids, the results indicate if the patient is anergic so that one will not rely on a false-negative result. In the event of an equivocal result, a careful clinical assessment for risks of TB exposures should be elicited, and a chest radiograph should be obtained.22 In patients with prior high risk of tuberculosis exposures or a positive test for tuberculosis, an infectious disease specialist should be consulted early to advise if therapy should be started in preparation for the potential use of infliximab.23 In cases where cyclosporine may be considered, magnesium and total cholesterol level should be checked. Sending thiopurine methyltranferase (TPMT) enzyme activity should be considered as well, in case of a need for future thiopurine use for maintenance of disease activity.24
Infectious diarrhea may be indistinguishable from ASUC and may also be the trigger of a flare; thus, it is important to rule out infection with stool microbiologic studies. Most importantly, Clostridium difficile infection must be ruled out in all patients with ASUC. Although patients with IBD, especially those with UC, have significantly higher rates of asymptomatic C. difficile carriage than the general population, a positive polymerase chain reaction test for C. difficile in a patient with ASUC should prompt treatment with oral vancomycin.25 However, if carriage if suspected and a subsequent enzyme-linked immunoassay for C. difficile toxin is negative, treatment can be discontinued. Active C. difficile infection in patients with IBD is associated with increased disease severity, greater length of hospital stay, and increased the likelihood of colectomy and mortality.26,27 Other bacterial infections including Escherichia coli, Campylobacter, Shigella, Salmonella, Yersinia, Entamoeba histolytica, as well as other parasitic infestations may mimic UC. Testing should be considered in cases of foreign travel, immunosuppression or contact with other persons with diarrhea.7,28 Routine testing of these other enteric infections without a clear exposure risk is of little benefit and may raise costs.23,29
Radiologic Evaluation
A plain X-ray film of the abdomen should be obtained in all patients on admission to evaluate for evolving colonic dilation or undiagnosed free air. Small bowel distension >3 cm may predict an increased risk of colectomy.30 Clinicians must be mindful that steroids can mask peritoneal signs and that retroperitoneal perforations may not be apparent on plain X-ray films. Nonetheless, a CT of the abdomen is usually not necessary and should be reserved for cases with severe abdominal pain out of proportion to clinical signs in which a plain X-ray film is unrevealing. Judicious use of CT imaging is especially important in younger patients, as there is growing concern that patients with IBD may be exposed to potentially harmful cumulative levels of radiation in their lifetime from repeated CT imaging.31
Endoscopic Evaluation
Flexible sigmoidoscopy aids in the assessment of disease severity and extent and biopsies can assist in ruling out a diagnosis of cytomegalovirus (CMV) colitis in patients already on immunosuppression. For this reason, many clinicians prefer to perform a sigmoidoscopy on admission.23 If one is not performed on admission, a sigmoidoscopy is advised in all patients who are not responding adequately after 72 hours of intravenous steroid therapy in order to rule out superimposed CMV colitis.28
Sigmoidoscopy should be avoided in patients with toxic megacolon and when there is a concern for peritonitis. A complete colonoscopy is rarely indicated in the acute setting and carries a theoretical risk of colonic perforation.7
INITIAL THERAPY
The first therapeutic steps aim to reduce inflammation with the use of systemic corticosteroids, avoid colonic and extraintestinal complications, and plan for the potential need for rescue therapy.
Intravenous Corticosteroids
The cornerstone of ASUC management is treatment with intravenous corticosteroids. Their initiation should not be delayed in patients with an established diagnosis of UC while waiting for results of evaluations for infectious colitis. Even among patients who have failed oral steroids, a meta-regression analysis showed that two-thirds of patients will still respond to intravenous corticosteroids.21,32 Methylprednisolone 20 mg IV three times daily (or hydrocortisone 100 mg IV three times daily) is a standard regimen; higher doses do not provide additional benefit.21 Patients’ response to intravenous steroids should be assessed with repeat labs including CRP and an assessment of the total number of bowel movements over a 24-hour period, with special attention to their overall response after three days of treatment.33-36
Intravenous Fluids
Many patients admitted with ASUC will have significant volume depletion, and intravenous fluids should be administered in a manner like other volume-depleted or oral-intake-restricted patients.
Venous Thromboembolism Prophylaxis
The risk of VTE in hospitalized patients with IBD exceeds that of inpatients without IBD, approximately 2%, a risk similar to patients with respiratory failure.37 Additionally, VTE in hospitalized patients with IBD is associated with a 2.5-fold increase in mortality.38,39 Therefore, all patients hospitalized with ASUC should receive subcutaneous unfractionated or low molecular weight heparin or fondaparinux for VTE prophylaxis. Rectal bleeding, expected in ASUC, is not a contraindication to chemo-prophylaxis. Additionally, it is important to check if patients are receiving the ordered VTE prophylaxis.40,41 Pleet et al. found that only 7% of patients at a tertiary center had adequate prophylaxis for greater than 80% of their hospitalization.41
Unnecessary or Potentially Harmful Medications
Several medications have the potential for misuse in patients hospitalized with UC.
Antimotility Agents
Loperamide, diphenoxylate, and opiate antidiarrheals should not be used as they may provoke toxic megacolon.42 Similarly, drugs with antimotility side effects (eg, anticholinergics) should be avoided.
Opiates
In addition to their undesirable antimotility effect, the use of opiates has been associated with poor outcomes among inpatients and outpatients with IBD, including increased morbidity and mortality.43,44 Pain severe enough to require opiates should raise suspicion for toxic megacolon, perforation, or a noninflammatory etiology. If opiates are utilized, they should be ordered as one-time doses and the patient should be reassessed for each dose.
Nonsteroidal Anti-inflammatory Drugs
These drugs, which include oral NSAIDs, intravenous ketorolac, and topic diclofenac gels, may increase disease activity in inflammatory bowel disease and should be avoided.17
5-aminosalicylates (5-ASA)
A small proportion of patients experience a paradoxical worsening of diarrhea due to the use of 5-ASA agents such as mesalamine. It is reasonable to discontinue or avoid the use of 5-ASA agents in hospitalized patients, especially as there is little to no benefit from combining a 5-ASA with a biologic or immunosuppressive drug.45
Antibiotics
There is no role for the routine use of antibiotics in patients hospitalized with ASUC. 23,46,47 Inappropriate use of antibiotics raises the risk of C. difficile infection and antibiotic resistance. However, in cases of suspected toxic megacolon or perforation, antibiotics should be administered. In situations in which a patient is treated with triple immunosuppression (ie, steroids plus two other agents, cyclosporine and mercaptopurine) antibiotic prophylaxis for Pneumocystis jiroveci is advisable.48 Using a large insurance database, Long et al. reported a low absolute incidence of Pneumocystis jiroveci in IBD patients but noted that the risk in patients with IBD was still significantly higher than matched controls. While it can be considered, we typically refrain from using prophylaxis in patients on double immunosuppression (for example, steroids plus infliximab) due to the potential adverse effects of antibiotics in this population, though many advocate using prophylaxis for all patients on cyclosporine even if this is only double immunosuppressive therapy.23
Surgical Consultation
Involving a surgeon early in an ASUC patient’s care—before needing urgent colectomy—is critical. As part of the consultation, a surgeon experienced in IBD should meet with patients to discuss multistage colectomy with ileostomy and potential future J-pouch (ileal pouch-anal anastomosis) formation. Patients should be given ample opportunity to ask questions before surgery may become urgent. Also, patients should be counseled on realistic expectations of ostomy and pouch function and, ideally, meet with an ostomy nurse.23
At some centers, surgical consultation is requested on the first hospital day, but this can result in consultations for patients who ultimately respond to intravenous steroids. Therefore, some centers advocate for surgical consultation only after a patient has failed treatment with intravenous steroids (ie, day three to four) when the risk of needing surgical management increases.23
Nutrition
Bowel rest with parenteral nutrition does not improve outcomes in ASUC versus an oral diet, and there is no contraindication to allowing patients to continue on a regular diet unless they have toxic megacolon or other signs of fulminant colitis.49,50 However, patients may feel better eating less, as this will reduce their bowel movement frequency. Unfortunately, this can give a false sense of reassurance that the patient is improving. Therefore, it remains important to evaluate a patient’s symptoms in the context of their food intake.
Assessing Response to Steroids
Patients who do not respond adequately to the first-line intravenous steroid therapy will require medical or surgical rescue therapy; therefore, deciding whether a patient has responded is essential. Patients should have less than four bowel movements per day – ideally just one to two – with no blood to indicate a complete response. For more ambiguous situations, although there is no strict definition of steroid responsiveness, multiple prediction indices have attempted to identify patients who will require rescue therapy. One of the simplest, the Oxford index, illustrates two of the most critical parameters to follow, stool frequency and CRP.51 In a preinfliximab cohort, Oxford index predicted an 85% likelihood of colectomy in patients with eight or more daily bowel movements or with three to eight daily bowel movements and a CRP greater than 45 mg/L after three days of intravenous steroid treatment.52 To assist with assessing responsiveness to therapy, we ask patients to log their bowel movements – either on paper or on a whiteboard in the hospital room – so that we can review their progress daily. Other predictors of colectomy include hypoalbuminemia, scoring of endoscopic severity, and colonic dilation.53
Patients who fail to respond to intravenous corticosteroids after three days33,35 of treatment should be started on rescue therapy with infliximab or cyclosporine or undergo colectomy. A common pitfall in the treatment of ASUC is waiting for a response to steroids beyond this time frame, after which patients are unlikely to benefit.34,36 Furthermore, patients for whom surgical rescue therapy is delayed have higher operative morbidity and mortality.54,55 Because timely decision making regarding rescue therapy is crucial to optimizing outcomes, patient education efforts regarding potential rescue therapy should take place on admission or soon after, rather than waiting to ascertain steroid responsiveness.
RESCUE THERAPY FOR STEROID-REFRACTORY DISEASE
Medical options for rescue therapy include the antitumor necrosis factor (anti-TNF) agent infliximab or the calcineurin inhibitor cyclosporine. In general, infliximab and cyclosporine have been found to be roughly equivalent in efficacy in clinical trials regarding response, remission, and colectomy at 12 months.56,57 However, many clinicians prefer infliximab due to its relative ease of use, familiarity with the agent from outpatient experience, and ability to continue to use long term for maintenance of disease remission.58 In contrast to infliximab, intravenous cyclosporine requires closer monitoring and labs to assess the therapeutic trough level. The decision regarding which drug to use should be made on a case-by-case basis in conjunction with a gastroenterologist experienced in their use, and if no such specialist is available, transfer to a specialized center should be considered. Generally, successive treatment with cyclosporine or infliximab followed by third-line salvage therapy with the other drug should be avoided due to low rates of response and high rates of adverse events.59
Infliximab
Infliximab is an intravenously-administered anti-TNF monoclonal chimeric antibody that is effective both for outpatient treatment of moderate to severe UC and inpatient treatment of ASUC.1 It is relatively contraindicated in patients with untreated latent tuberculosis, demyelinating disease, advanced congestive heart failure, or uncontrolled infection.
The optimal dosing strategy for infliximab in ASUC is unknown. Infliximab clearance in the setting of ASUC is increased, partly because it is bound to albumin, which is often low in ASUC, and partly because it is excreted in the stool.60,61 As a result, accelerated loading doses may be more successful than a typical loading schedule,62 and most clinicians use alternative dosing strategies.63 Our typical approach for ASUC is an initial dose of 10 mg/kg rather than 5 mg/kg, with an additional 10 mg/kg dose 48-72 hours later if an adequate clinical response is lacking. Patients who respond to infliximab can continue to use the drug as an outpatient for maintenance of remission.
Cyclosporine
Cyclosporine is a fast-acting immunosuppressive agent that acts primarily via T-cell inhibition. Although older literature used a dose of 4 mg/kg per day, a randomized trial demonstrated similar response rates to a dose of 2 mg/kg per day.64 Patients receiving treatment with cyclosporine, which is given as a continuous infusion, must be monitored for toxicities. These can include potentially severe infection, seizures (often associated with low total cholesterol or hypomagnesemia), electrolyte abnormalities, renal impairment, hypertension, hypertrichosis, tremor, and others.65
Before initiation of treatment, serum cholesterol levels should be obtained to screen for low total cholesterol that may portend risk of seizures on the drug. Additionally, baseline creatinine and magnesium should be established. While on treatment, daily serum cyclosporine levels and electrolytes including magnesium should be measured. Patients who respond to intravenous cyclosporine must be transitioned to oral cyclosporine and have stable drug levels before discharge. Unfortunately, oral cyclosporine has not been shown to be as effective as long-term maintenance therapy. Therefore, cyclosporine can only be used as a “bridge” to another therapy. Historically, thiopurines like azathioprine or mercaptopurine have been used for this purpose because they are effective for the treatment of UC but may require months to have a full therapeutic effect. There have been promising reports of using vedolizumab similarly.66,67 Vedolizumab is a monoclonal antibody that selectively blocks lymphocyte trafficking to the gut that, like thiopurines, has an onset of action that is significantly longer than calcineurin and TNF inhibitors.
COLECTOMY
Colectomy should be considered as a second- or third-line therapy for patients who fail to respond to intravenous corticosteroids. In an analysis of 10 years of data from the Nationwide Inpatient Sample, mortality rates for colectomy in this setting varied from 0.7% at high volume centers to 4% at low volume centers.68 Therefore, if a patient is not hospitalized at a center with expertise in colectomy for UC, transfer to a specialized center should be considered. Colectomy should be performed promptly in all the patients who have failed rescue therapy with infliximab or cyclosporine or have opted against medical rescue therapy. Surgery should be performed emergently in patients with toxic megacolon, uncontrolled colonic hemorrhage or perforation.
QUALITY OF CARE AND THE USE OF CARE PATHWAYS
Physician and center-level characteristics are associated with the quality of care and outcomes in ASUC. Gastroenterologists with expertise in IBD are more likely than other gastroenterologists to request appropriate surgical consultation for steroid-refractory patients,69 and inpatients with ASUC primarily cared by gastroenterologists rather than nongastroenterologists have lower in-hospital and one-year mortality.14 Moreover, surgical outcomes differ based on center volume, with higher volume centers having lower rates of postoperative mortality.68,70 However, even at referral centers, key metrics of care quality such as rates of VTE prophylaxis, testing for C. difficile, and timely rescue therapy for steroid-refractory UC patients are suboptimal, with only 70%-82% of patients with IBD hospitalized at four referral centers in Canada meeting these metrics.71
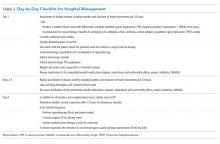
Inpatient clinical pathways reduce LOS, reduce hospital costs, and likely reduce complications.72 For this reason, a consensus group recommended the use of care pathways for the management of ASUC and, although there is little data on the use of pathways for ASUC specifically, the use of such a pathway in the United Kingdom was associated with improved metrics including LOS, time to VTE prophylaxis, testing of stool for infection, CRP measurement, and timely gastroenterologist consultation.16,18
DISCHARGE CRITERIA AND FOLLOW UP
In general, patients should enter clinical remission, defined as resolution of rectal bleeding and diarrhea or altered bowel habits,73 before discharge, and achieving this may require a relatively prolonged hospitalization. Most patients should have one to two bowel movements a day without blood but, at a minimum, all should have less than four nonbloody bowel movements per day. Patients are candidates for discharge if they remain well after transitioning to oral prednisone at a dose of 40-60 mg daily and tolerate a regular diet.
For patients who initiated infliximab during their admission, plans for outpatient infusions including insurance approval should be made before discharge, and patients who started cyclosporine should be transitioned to oral dosing and have stable serum concentrations before leaving the hospital. Patients should leave with a preliminary plan for a steroid taper, which may vary depending on their clinical presentation. Usually, gastroenterology follow-up should be arranged after two weeks following discharge, but patients on cyclosporine need sooner laboratory monitoring.
CONCLUSION
The care of patients with ASUC requires an interdisciplinary team and close collaboration between hospitalists, gastroenterologists, and surgeons. Patients should be treated with intravenous corticosteroids and monitored carefully for response and need for rescue therapy. Establishing algorithms for the management of patients with ASUC can further improve the care of these complex patients.
Disclosures
Drs. Feuerstein, Fudman, and Sattler report no potential conflict of interest.
Funding
This work was not supported by any grant.
1. Sands BE. Mount Sinai Expert Guides: Gastroenterology. Hoboken, NJ: John Wiley & Sons; 2014.
2. Dinesen LC, Walsh AJ, Protic MN, et al. The pattern and outcome of acute severe colitis. J Crohns Colitis. 2010;4(4):431-437. https://doi.org/10.1016/j.crohns.2010.02.001.
3. Edwards FC, Truelove SC. The course and prognosis of ulcerative colitis. Gut. 1963;4:299-315. https://doi.org/10.1136/gut.4.4.299.
4. Sonnenberg A, Chang J. Time trends of physician visits for Crohn’s disease and ulcerative colitis in the United States, 1960-2006. 2007;14(2):249-252. https://doi.org/10.1002/ibd.20273.
5. Nguyen GC, Tuskey A, Dassopoulos T, Harris ML, Brant SR. Rising hospitalization rates for inflammatory bowel disease in the United States between 1998 and 2004. Inflamm Bowel Dis. 2007;13(12):1529-1535. https://doi.org/10.1002/ibd.20250.
6. Truelove S, Witts L. Cortisone in ulcerative colitis. Br Med J. 1955;2:104-108.
7. Jakobovits SL, Travis S. Management of acute severe colitis. Br Med Bull. 2005;75(1):131-144. https://doi.org/10.1093/bmb/ldl001.
8. Lynch R, Lowe D, Protheroe A, Driscoll R, Rhodes J, Arnott I. Outcomes of rescue therapy in acute severe ulcerative colitis: data from the United Kingdom inflammatory bowel disease audit. Aliment Pharmacol Ther. 2013;38(8):935-945. https://doi.org/10.1111/apt.12473.
9. Magro F, Gionchetti P, Eliakim R, et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 1: definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileoanal pouch disorders. J Crohns Colitis. 2017;11(6):649-670. https://doi.org/10.1093/ecco-jcc/jjx008.
10. Kornbluth A, Sachar DB. Ulcerative colitis practice guidelines in adults: American college of gastroenterology, practice parameters committee. Am J Gastroenterol. 2010;105(3):501. https://doi.org/10.1038/ajg.2009.727.
11. Dassopoulos T, Cohen RD, Scherl EJ, Schwartz RM, Kosinski L, Regueiro MD. Ulcerative colitis care pathway. Gastroenterology. 2015;149(1):238-245. https://doi.org/10.1053/j.gastro.2015.05.036.
12. Ananthakrishnan AN, McGinley EL, Binion DG, Saeian K. A nationwide analysis of changes in severity and outcomes of inflammatory bowel disease hospitalizations. J Gastrointest Surg. 2011;15(2):267-276. https://doi.org/10.1007/s11605-010-1396-3.
13. Kelso M, Weideman RA, Cipher DJ, Feagins LA. Factors associated with length of stay in veterans with inflammatory bowel disease hospitalized for an acute flare. Inflamm Bowel Dis. 2017;24(1):5-11. https://doi.org/10.1093/ibd/izx020.
14. Murthy SK, Steinhart AH, Tinmouth J, Austin PC, Nguyen GC. Impact of gastroenterologist care on health outcomes of hospitalized ulcerative colitis patients. Gut. 2012;61(10):1410-1416. https://doi.org/10.1136/gutjnl-2011-301978.
15. Lee NS, Pola S, Groessl EJ, Rivera-Nieves J, Ho SB. Opportunities for improvement in the care of patients hospitalized for inflammatory bowel disease-related colitis. Dig Dis Sci. 2016;61(4):1003-1012. https://doi.org/10.1007/s10620-016-4046-0.
16. Neary BP, Doherty GA. A structured care pathway improves quality of care for acute severe ulcerative colitis. Gastroenterology. 2017;152(5):S218. https://doi.org/10.1016/S0016-5085(17)31028-4.
17. Klein A, Eliakim R. Nonsteroidal anti-inflammatory drugs and inflammatory bowel disease. Pharmaceuticals. 2010;3(4):1084-1092. https://doi.org/10.3390/ph3041084.
18. Chen JH, Andrews JM, Kariyawasam V, et al. Review article: acute severe ulcerative colitis - evidence-based consensus statements. Aliment Pharmacol Ther. 2016;44(2):127-144. https://doi.org/10.1111/apt.13670.
19. Vavricka SR, Schoepfer A, Scharl M, Lakatos PL, Navarini A, Rogler G. Extraintestinal manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2015;21(8):1982-1992. https://doi.org/10.1097/MIB.0000000000000392.
20. Solem CA, Loftus EV, Jr., Tremaine WJ, Harmsen WS, Zinsmeister AR, Sandborn WJ. Correlation of C-reactive protein with clinical, endoscopic, histologic, and radiographic activity in inflammatory bowel disease. Inflamm Bowel Dis. 2005;11(8):707-712. https://doi.org/10.1097/01.MIB.0000173271.18319.53.
21. Turner D, Walsh CM, Steinhart AH, Griffiths AM. Response to corticosteroids in severe ulcerative colitis: a systematic review of the literature and a meta-regression. Clin Gastroenterol Hepatol. 2007;5(1):103-110. https://doi.org/10.1016/j.cgh.2006.09.033.
22. Kaur M, Singapura P, Kalakota N, et al. Factors that contribute to indeterminate results from the QuantiFERON-TB Gold in-tube test in patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2018;16(10):1616-1621.e1. https://doi.org/10.1016/j.cgh.2017.11.038.
23. Bitton A, Buie D, Enns R, et al. Treatment of hospitalized adult patients with severe ulcerative colitis: Toronto consensus statements. Am J Gastroenterol. 2012;107(2):179-194. https://doi.org/10.1038/ajg.2011.386.
24. Feuerstein JD, Nguyen GC, Kupfer SS, Falck-Ytter Y, Singh S. American Gastroenterological Association Institute Clinical Guidelines committee. American Gastroenterological Association Institute Guideline on therapeutic drug monitoring in inflammatory bowel disease. Gastroenterology. 2017;153(3):827-834.
25. McDonald LC, Gerding DN, Johnson S, et al. Clinical Practice Guidelines for Clostridium difficile infection in adults and children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018;66(7):e1-e48. https://doi.org/10.1093/cid/cix1085.
26. Clayton EM, Rea MC, Shanahan F, et al. The vexed relationship between Clostridium difficile and inflammatory bowel disease: an assessment of carriage in an outpatient setting among patients in remission. Am J Gastroenterol. 2009;104(5):1162-1169. https://doi.org/10.1038/ajg.2009.4.
27. Nguyen GC, Kaplan GG, Harris ML, Brant SR. A national survey of the prevalence and impact of Clostridium difficile infection among hospitalized inflammatory bowel disease patients. Am J Gastroenterol. 2008;103(6):1443-1450. https://doi.org/10.1111/j.1572-0241.2007.01780.x.
28. Rahier J-F, Yazdanpanah Y, Colombel J-F, Travis S. The European (ECCO) Consensus on infection in IBD: what does it change for the clinician? Gut. 2009;58(10). https://doi.org/10.1136/gut.2008.175950.
29. Meyer AM, Ramzan NN, Loftus EV, Jr., Heigh RI, Leighton JA. The diagnostic yield of stool pathogen studies during relapses of inflammatory bowel disease. J Clin Gastroenterol. 2004;38(9):772-775. https://doi.org/10.1097/01.mcg.0000139057.05297.d6.
30. Chew C, Nolan D, Jewell D. Small bowel gas in severe ulcerative colitis. Gut. 1991;32(12):1535-1537. https://doi.org/10.1136/gut.32.12.1535.
31. Zakeri N, Pollok RC. Diagnostic imaging and radiation exposure in inflammatory bowel disease. World J Gastroenterol. 2016;22(7):2165-2178. https://doi.org/10.3748/wjg.v22.i7.2165.
32. Llaó J, Naves JE, Ruiz-Cerulla A, et al. Intravenous corticosteroids in moderately active ulcerative colitis refractory to oral corticosteroids. J Crohns Colitis. 2014;8(11):1523-1528. https://doi.org/10.1016/j.crohns.2014.06.010.
33. Seo M, Okada M, Yao T, Matake H, Maeda K. Evaluation of the clinical course of acute attacks in patients with ulcerative colitis through the use of an activity index. Journal of Gastroenterology. 2002;37(1):29-34. https://doi.org/10.1007/s535-002-8129-2.
34. Meyers S, Sachar DB, Goldberg JD, Janowitz HD. Corticotropin versus hydrocortisone in the intravenous treatment of ulcerative colitis: a prospective, randomized, double-blind clinical trial. Gastroenterology. 1983;85(2):351-357.
35. Ho G, Mowat C, Goddard C, et al. Predicting the outcome of severe ulcerative colitis: development of a novel risk score to aid early selection of patients for second‐line medical therapy or surgery. Aliment Pharmacol Ther. 2004;19(10):1079-1087. https://doi.org/10.1111/j.1365-2036.2004.01945.x.
36. Järnerot G, Rolny P, Sandberg-Gertzen H. Intensive intravenous treatment of ulcerative colitis. Gastroenterology. 1985;89(5):1005-1013. https://doi.org/10.1016/0016-5085(85)90201-X.
37. Wang JY, Terdiman JP, Vittinghoff E, Minichiello T, Varma MG. Hospitalized ulcerative colitis patients have an elevated risk of thromboembolic events. World J Gastroenterol. 2009;15(8):927-935. https://doi.org/10.3748/wjg.15.927.
38. Nguyen GC, Bernstein CN, Bitton A, et al. Consensus statements on the risk, prevention, and treatment of venous thromboembolism in inflammatory bowel disease: Canadian Association of Gastroenterology. Gastroenterology. 2014;146(3):835-848. https://doi.org/10.1053/j.gastro.2014.01.042.
39. Nguyen GC, Sam J. Rising prevalence of venous thromboembolism and its impact on mortality among hospitalized inflammatory bowel disease patients. Am J Gastroenterol. 2008;103(9):2272-2280. https://doi.org/10.1111/j.1572-0241.2008.02052.x.
40. Tinsley A, Naymagon S, Enomoto LM, Hollenbeak CS, Sands BE, Ullman TA. Rates of pharmacologic venous thromboembolism prophylaxis in hospitalized patients with active ulcerative colitis: results from a tertiary care center. J Crohns Colitis. 2013;7(12):e635-e640. https://doi.org/10.1016/j.crohns.2013.05.002.
41. Pleet JL, Vaughn BP, Morris JA, Moss AC, Cheifetz AS. The use of pharmacological prophylaxis against venous thromboembolism in hospitalized patients with severe active ulcerative colitis. Aliment Pharmacol Ther. 2014;39(9):940-948. https://doi.org/10.1111/apt.12691.
42. Gan SI, Beck PL. A new look at toxic megacolon: an update and review of incidence, etiology, pathogenesis, and management. Am J Gastroenterol. 2003;98(11):2363-2371 https://doi.org/10.1111/j.1572-0241.2003.07696.x.
43. Lichtenstein GR, Feagan BG, Cohen RD, et al. Serious infections and mortality in association with therapies for Crohn’s disease: TREAT registry. Clin Gastroenterol Hepatol. 2006;4(5):621-630. https://doi.org/10.1016/j.cgh.2006.03.002.
44. Docherty MJ, Jones III RCW, Wallace MS. Managing pain in inflammatory bowel disease. Gastroenterol Hepatol. 2011;7(9):592-601.
45. Singh S, Proudfoot JA, Dulai PS, et al. No benefit of concomitant 5-aminosalicylates in patients with ulcerative colitis escalated to biologic therapy: pooled analysis of individual participant data from clinical trials. Am J Gastroenterol. 2018;113(8):1197-1205. https://doi.org/10.1038/s41395-018-0144-2.
46. Mantzaris GJ, Hatzis A, Kontogiannis P, Triadaphyllou G. Intravenous tobramycin and metronidazole as an adjunct to corticosteroids in acute, severe ulcerative colitis. Am J Gastroenterol. 1994;89(1):43-46.
47. Mantzaris GJ, Petraki K, Archavlis E, et al. A prospective randomized controlled trial of intravenous ciprofloxacin as an adjunct to corticosteroids in acute, severe ulcerative colitis. Scand J Gastroenterol. 2001;36(9):971-974.
48. Rahier J-F, Magro F, Abreu C, et al. Second European evidence-based consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease. J Crohns Colitis. 2014;8(6):443-468. https://doi.org/10.1016/j.crohns.2013.12.013.
49. Dickinson RJ, Ashton MG, Axon AT, Smith RC, Yeung CK, Hill GL. Controlled trial of intravenous hyperalimentation and total bowel rest as an adjunct to the routine therapy of acute colitis. Gastroenterology. 1980;79(6):1199-1204.
50. McIntyre P, Powell-Tuck J, Wood S, et al. Controlled trial of bowel rest in the treatment of severe acute colitis. Gut. 1986;27(5):481-485. https://doi.org/10.1136/gut.27.5.481.
51. Travis SP, Farrant JM, Ricketts C, et al. Predicting outcome in severe ulcerative colitis. Gut. 1996;38(6):905-910. https://doi.org/10.1136/gut.38.6.905.
52. Bernardo S, Fernandes SR, Goncalves AR, et al. Predicting the course of disease in hospitalized patients with acute severe ulcerative colitis. Inflamm Bowel Dis. 2018;25(3):541-546. https://doi.org/10.1093/ibd/izy256.
53. Harbord M, Eliakim R, Bettenworth D, et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 2: current management. J Crohns Colitis. 2017;11(7):769-784. https://doi.org/10.1093/ecco-jcc/jjx009.
54. Randall J, Singh B, Warren B, Travis S, Mortensen N, George B. Delayed surgery for acute severe colitis is associated with increased risk of postoperative complications. Br J Surg. 2010;97(3):404-409. https://doi.org/10.1002/bjs.6874.
55. Bartels S, Gardenbroek T, Ubbink D, Buskens C, Tanis P, Bemelman W. Systematic review and meta‐analysis of laparoscopic versus open colectomy with end ileostomy for non‐toxic colitis. Br J Surg. 2013;100(6):726-733. https://doi.org/10.1002/bjs.9061.
56. Laharie D, Bourreille A, Branche J, et al. Ciclosporin versus infliximab in patients with severe ulcerative colitis refractory to intravenous steroids: a parallel, open-label randomized controlled trial. Lancet. 2012;380(9857):1909-1915. https://doi.org/10.1016/S0140-6736(12)61084-8.
57. Leblanc S, Allez M, Seksik P, et al. Successive treatment with cyclosporine and infliximab in steroid-refractory ulcerative colitis. Am J Gastroenterol. 2011;106(4):771-777. https://doi.org/10.1038/ajg.2011.62.
58. Narula N, Marshall JK, Colombel JF, et al. Systematic review and meta-analysis: infliximab or cyclosporine as rescue therapy in patients with severe ulcerative colitis refractory to steroids. Am J Gastroenterol. 2016;111(4):477-491. https://doi.org/10.1038/ajg.2016.7.
59. Feuerstein JD, Akbari M, Tapper EB, Cheifetz AS. Systematic review and meta-analysis of third-line salvage therapy with infliximab or cyclosporine in severe ulcerative colitis. Ann Gastroenterol. 2016;29(3):341-347. https://doi.org/10.20524/aog.2016.0032.
60. Brandse JF, Mathôt RA, van der Kleij D, et al. Pharmacokinetic features and presence of antidrug antibodies associated with response to infliximab induction therapy in patients with moderate to severe ulcerative colitis. Clin Gastroenterol Hepatol. 2016;14(2):251-258. https://doi.org/10.1016/j.cgh.2015.10.029.
61. Hindryckx P, Novak G, Vande Casteele N, et al. Review article: dose optimization of infliximab for acute severe ulcerative colitis. Aliment Pharmacol Ther. 2017;45(5):617-630. https://doi.org/10.1111/apt.13913.
62. Gibson DJ, Heetun ZS, Redmond CE, et al. An accelerated infliximab induction regimen reduces the need for early colectomy in patients with acute severe ulcerative colitis. Clin Gastroenterol Hepatol. 2015;13(2):330-335. https://doi.org/10.1016/j.cgh.2014.07.041.
63. Herfarth HH, Rogler G, Higgins PD. Pushing the pedal to the metal: should we accelerate infliximab therapy for patients with severe ulcerative colitis? Clin Gastroenterol Hepatol. 2015;13(2):336-338. https://doi.org/10.1016/j.cgh.2014.09.045.
64. Van Assche G, D’haens G, Noman M, et al. Randomized, double-blind comparison of 4 mg/kg versus 2 mg/kg intravenous cyclosporine in severe ulcerative colitis. Gastroenterology. 2003;125(4):1025-1031.
65. Arts J, D’haens G, Zeegers M, et al. Long-term outcome of treatment with intravenous cyclosporin in patients with severe ulcerative colitis. Inflamm Bowel Dis. 2004;10(2):73-78.
66. Tarabar D, El Jurdi K, Yvellez O, et al. 330-combination therapy of cyclosporine and vedolizumab is effective and safe for severe, steroid-resistant ulcerative colitis patients: a prospective study. Gastroenterology. 2018;154(6):S-82-S-83.https://doi.org/10.1016/S0016-5085(18)30725-X.
67. Szántó K, Molnár T, Farkas K. New promising combo therapy in inflammatory bowel diseases refractory to anti-TNF agents: cyclosporine plus vedolizumab. J Crohns Colitis. 2018;12(5):629. https://doi.org/10.1093/ecco-jcc/jjx179.
68. Kaplan GG, McCarthy EP, Ayanian JZ, Korzenik J, Hodin R, Sands BE. Impact of hospital volume on postoperative morbidity and mortality following a colectomy for ulcerative colitis. Gastroenterology. 2008;134(3):680-687. https://doi.org/10.1053/j.gastro.2008.01.004.
69. Spiegel BM, Ho W, Esrailian E, et al. Controversies in ulcerative colitis: a survey comparing decision making of experts versus community gastroenterologists. Clin Gastroenterol Hepatol. 2009;7(2):168-174. https://doi.org/10.1016/j.cgh.2008.08.029.
70. Ananthakrishnan AN, Issa M, Beaulieu DB, et al. History of medical hospitalization predicts future need for colectomy in patients with ulcerative colitis. Inflamm Bowel Dis. 2009;15(2):176-181. https://doi.org/10.1002/ibd.20639.
71. Nguyen GC, Murthy SK, Bressler B, et al. Quality of care and outcomes among hospitalized inflammatory bowel disease patients: a multicenter retrospective study. Inflamm Bowel Dis. 2017;23(5):695-701. https://doi.org/10.1097/MIB.0000000000001068.
72. Rotter T, Kugler J, Koch R, et al. A systematic review and meta-analysis of the effects of clinical pathways on length of stay, hospital costs, and patient outcomes. BMC Health Serv Res. 2008;8:265. https://doi.org/10.1186/1472-6963-8-265.
73. Peyrin-Biroulet L, Sandborn W, Sands BE, et al. Selecting therapeutic targets in inflammatory bowel disease (stride): determining therapeutic goals for treat-to-target. Am J Gastroenterol. 2015;110(9):1324-1338. https://doi.org/10.1038/ajg.2015.233.
Ulcerative colitis (UC) is a chronic inflammatory condition of the colonic mucosa. Classically, it starts in the rectum and can extend continuously from the distal to the proximal colon. The defining clinical symptom of UC is bloody diarrhea, typically accompanied by rectal urgency and mucus discharge. The natural history of this disease includes periods of exacerbations and remissions occurring spontaneously or in response to medical treatment.1
Acute severe ulcerative colitis (ASUC) is a potentially life-threatening complication of UC that typically requires hospitalization and interdisciplinary care between hospitalists, gastroenterologists, and colorectal or general surgeons. The risk of a patient with UC requiring hospitalization for ASUC ranges from 15%-25%2,3 and, in total, UC accounts for 30,000 hospital visits annually.4 The direct medical costs exceed $4 billion annually, with hospital costs of over $960 million.5 Historically, mortality from ASUC was as high as 24% but decreased substantially to 7% after the introduction of systemic corticosteroid therapy.6 Further advances in care have reduced mortality to approximately 1% or less.7,8 Nonetheless, up to 20% of patients admitted with ASUC have a colectomy on their first admission, and this rate rises to 40% after two admissions.2
DEFINING ACUTE SEVERE ULCERATIVE COLITIS
To categorize UC severity, assess patients using the Truelove and Witt’s criteria. The system classifies patients as having mild, moderate, severe, or fulminant disease. Severe disease by these criteria includes patients with >6 bloody bowel movements per day and at least one of the following clinical features: fever (>37.8°C), tachycardia (>90 bpm), anemia (hemoglobin <10.5 g/dl), or elevated inflammatory markers (traditionally, erythrocyte sedimentation rate greater than 30 mm/h or, more recently, C-reactive protein (CRP) greater than 30 mg/L. (Table 1).6,9
Fulminant colitis refers to a subgroup of patients with more than 10 stools per day, continuous bleeding, abdominal pain, colonic dilatation on abdominal X-ray film, and severe toxic symptoms including fever and anorexia. Such patients are at risk of progressing to toxic megacolon and bowel perforation.10
INDICATIONS FOR HOSPITALIZATION AND INPATIENT LEVEL OF CARE
Patients with ASUC almost always require hospitalization for their disease management. In many cases, these patients have been receiving outpatient oral prednisone 40-60 mg daily but continue to have ongoing disease activity.11 Most patients will require close clinical monitoring, frequent blood testing, endoscopic or radiologic evaluation, as well as administration of intravenous corticosteroids. The average length of stay (LOS) ranges from 4.6 to 12.5 days, depending on disease severity.12 Not surprisingly, Kelso et al. reported that predictors of hospital LOS greater than four days include initiating a biologic drug in the hospital, undergoing two or more imaging modalities and treatment with intravenous steroids,13 and so it is rare that patients do not meet billing requirements for an inpatient level of care.
INITIAL EVALUATION
The multifaceted initial inpatient evaluation of patients with ASUC aims to assess disease severity, identify and prevent potential complications, and initiate planning for potential failure of first-line pharmacologic therapy. Due to the accumulating evidence that involving physicians with expertise in managing ASUC improves outcomes, gastroenterologists should be involved in the care of patients with ASUC from the time of their admission.14,15 Additionally, creating standardized care pathways for the management of ASUC can reduce cost, LOS, and improve quality.16
History and Physical Examination
Patients should be asked about fever, abdominal pain, nausea, emesis, bloating, weight loss, and bowel movements (frequency, consistency, the presence of blood, urgency, nighttime awakenings). The number of bowel movements over a 24-hour period should be quantified as this helps assess the overall disease severity (Table 1).
The patient’s initial inflammatory bowel disease (IBD) history is also essential. The review of pertinent information regarding the patient’s initial diagnosis of UC includes the severity and anatomic extent of disease, extraintestinal manifestations, previous medical therapies, and surgical interventions. Exposure to nonsteroidal anti-inflammatory drugs (NSAIDs) or antibiotics should be identified as they may precipitate flares.17 Travel history may be pertinent as travel increases the risk of infections with food-borne or parasitic pathogens.18
Physical examination begins with an assessment of vital signs and volume status. Abdominal examination should include evaluation of bowel sounds, an assessment of distention, location, the extent of abdominal tenderness, and peritoneal signs. The abdominal exam should be interpreted in the context of the patient’s medications, as the use of steroid or analgesic therapies may affect the sensitivity for detecting complications. An external rectal exam evaluating perianal disease should be performed, as perianal disease raises concern for Crohn’s, a disease whose surgical management differs from UC.
A careful exam for extraintestinal manifestations is also essential. The skin should be evaluated for any new rashes, especially on the anterior shin consistent with erythema nodosum or ulcerated lesions on the skin suggestive of pyoderma gangrenosum. The peripheral joints should also be examined for any synovitis. Additional examinations should be performed based on any reported symptoms (eg, the ophthalmic exam for uveitis or scleritis if visual changes or eye pain are reported). Some extraintestinal manifestations require subspecialty consultation and comanagement to guide disease therapy. Patients with underlying pyoderma gangrenosum may require a dermatology consultation to guide management. Ocular inflammation requires ophthalmology involvement, and inflammatory arthritis is best comanaged with rheumatology.19
Laboratory Testing
Initial testing should include a complete blood count with differential, basic metabolic panel, and liver chemistries including alkaline phosphatase and albumin. When relevant, pregnancy testing should be performed. Measure CRP on admission so that its trajectory can be followed during therapy. However, a normal CRP does not exclude the presence of a UC flare as a subset of patients with ASUC will have a normal CRP despite severe mucosal inflammation.20
Since one-third of patients do not respond to intravenous corticosteroids and will require rescue therapy during the hospitalization with infliximab or cyclosporine, anticipatory testing for these medications should be performed on admission to avoid delays in the administration of rescue therapy.6,21 This should include an interferon-gamma release assay (eg, quantiferon gold) to test for latent tuberculosis and hepatitis B serologies in anticipation of possible treatment with infliximab. An interferon-gamma release assay is preferred to a tuberculin skin test because patients may be anergic, and a skin test does not provide a control to determine whether a negative test is due to anergy. In contrast, although a quantiferon gold test can be indeterminate in ASUC due to disease activity and systemic steroids, the results indicate if the patient is anergic so that one will not rely on a false-negative result. In the event of an equivocal result, a careful clinical assessment for risks of TB exposures should be elicited, and a chest radiograph should be obtained.22 In patients with prior high risk of tuberculosis exposures or a positive test for tuberculosis, an infectious disease specialist should be consulted early to advise if therapy should be started in preparation for the potential use of infliximab.23 In cases where cyclosporine may be considered, magnesium and total cholesterol level should be checked. Sending thiopurine methyltranferase (TPMT) enzyme activity should be considered as well, in case of a need for future thiopurine use for maintenance of disease activity.24
Infectious diarrhea may be indistinguishable from ASUC and may also be the trigger of a flare; thus, it is important to rule out infection with stool microbiologic studies. Most importantly, Clostridium difficile infection must be ruled out in all patients with ASUC. Although patients with IBD, especially those with UC, have significantly higher rates of asymptomatic C. difficile carriage than the general population, a positive polymerase chain reaction test for C. difficile in a patient with ASUC should prompt treatment with oral vancomycin.25 However, if carriage if suspected and a subsequent enzyme-linked immunoassay for C. difficile toxin is negative, treatment can be discontinued. Active C. difficile infection in patients with IBD is associated with increased disease severity, greater length of hospital stay, and increased the likelihood of colectomy and mortality.26,27 Other bacterial infections including Escherichia coli, Campylobacter, Shigella, Salmonella, Yersinia, Entamoeba histolytica, as well as other parasitic infestations may mimic UC. Testing should be considered in cases of foreign travel, immunosuppression or contact with other persons with diarrhea.7,28 Routine testing of these other enteric infections without a clear exposure risk is of little benefit and may raise costs.23,29
Radiologic Evaluation
A plain X-ray film of the abdomen should be obtained in all patients on admission to evaluate for evolving colonic dilation or undiagnosed free air. Small bowel distension >3 cm may predict an increased risk of colectomy.30 Clinicians must be mindful that steroids can mask peritoneal signs and that retroperitoneal perforations may not be apparent on plain X-ray films. Nonetheless, a CT of the abdomen is usually not necessary and should be reserved for cases with severe abdominal pain out of proportion to clinical signs in which a plain X-ray film is unrevealing. Judicious use of CT imaging is especially important in younger patients, as there is growing concern that patients with IBD may be exposed to potentially harmful cumulative levels of radiation in their lifetime from repeated CT imaging.31
Endoscopic Evaluation
Flexible sigmoidoscopy aids in the assessment of disease severity and extent and biopsies can assist in ruling out a diagnosis of cytomegalovirus (CMV) colitis in patients already on immunosuppression. For this reason, many clinicians prefer to perform a sigmoidoscopy on admission.23 If one is not performed on admission, a sigmoidoscopy is advised in all patients who are not responding adequately after 72 hours of intravenous steroid therapy in order to rule out superimposed CMV colitis.28
Sigmoidoscopy should be avoided in patients with toxic megacolon and when there is a concern for peritonitis. A complete colonoscopy is rarely indicated in the acute setting and carries a theoretical risk of colonic perforation.7
INITIAL THERAPY
The first therapeutic steps aim to reduce inflammation with the use of systemic corticosteroids, avoid colonic and extraintestinal complications, and plan for the potential need for rescue therapy.
Intravenous Corticosteroids
The cornerstone of ASUC management is treatment with intravenous corticosteroids. Their initiation should not be delayed in patients with an established diagnosis of UC while waiting for results of evaluations for infectious colitis. Even among patients who have failed oral steroids, a meta-regression analysis showed that two-thirds of patients will still respond to intravenous corticosteroids.21,32 Methylprednisolone 20 mg IV three times daily (or hydrocortisone 100 mg IV three times daily) is a standard regimen; higher doses do not provide additional benefit.21 Patients’ response to intravenous steroids should be assessed with repeat labs including CRP and an assessment of the total number of bowel movements over a 24-hour period, with special attention to their overall response after three days of treatment.33-36
Intravenous Fluids
Many patients admitted with ASUC will have significant volume depletion, and intravenous fluids should be administered in a manner like other volume-depleted or oral-intake-restricted patients.
Venous Thromboembolism Prophylaxis
The risk of VTE in hospitalized patients with IBD exceeds that of inpatients without IBD, approximately 2%, a risk similar to patients with respiratory failure.37 Additionally, VTE in hospitalized patients with IBD is associated with a 2.5-fold increase in mortality.38,39 Therefore, all patients hospitalized with ASUC should receive subcutaneous unfractionated or low molecular weight heparin or fondaparinux for VTE prophylaxis. Rectal bleeding, expected in ASUC, is not a contraindication to chemo-prophylaxis. Additionally, it is important to check if patients are receiving the ordered VTE prophylaxis.40,41 Pleet et al. found that only 7% of patients at a tertiary center had adequate prophylaxis for greater than 80% of their hospitalization.41
Unnecessary or Potentially Harmful Medications
Several medications have the potential for misuse in patients hospitalized with UC.
Antimotility Agents
Loperamide, diphenoxylate, and opiate antidiarrheals should not be used as they may provoke toxic megacolon.42 Similarly, drugs with antimotility side effects (eg, anticholinergics) should be avoided.
Opiates
In addition to their undesirable antimotility effect, the use of opiates has been associated with poor outcomes among inpatients and outpatients with IBD, including increased morbidity and mortality.43,44 Pain severe enough to require opiates should raise suspicion for toxic megacolon, perforation, or a noninflammatory etiology. If opiates are utilized, they should be ordered as one-time doses and the patient should be reassessed for each dose.
Nonsteroidal Anti-inflammatory Drugs
These drugs, which include oral NSAIDs, intravenous ketorolac, and topic diclofenac gels, may increase disease activity in inflammatory bowel disease and should be avoided.17
5-aminosalicylates (5-ASA)
A small proportion of patients experience a paradoxical worsening of diarrhea due to the use of 5-ASA agents such as mesalamine. It is reasonable to discontinue or avoid the use of 5-ASA agents in hospitalized patients, especially as there is little to no benefit from combining a 5-ASA with a biologic or immunosuppressive drug.45
Antibiotics
There is no role for the routine use of antibiotics in patients hospitalized with ASUC. 23,46,47 Inappropriate use of antibiotics raises the risk of C. difficile infection and antibiotic resistance. However, in cases of suspected toxic megacolon or perforation, antibiotics should be administered. In situations in which a patient is treated with triple immunosuppression (ie, steroids plus two other agents, cyclosporine and mercaptopurine) antibiotic prophylaxis for Pneumocystis jiroveci is advisable.48 Using a large insurance database, Long et al. reported a low absolute incidence of Pneumocystis jiroveci in IBD patients but noted that the risk in patients with IBD was still significantly higher than matched controls. While it can be considered, we typically refrain from using prophylaxis in patients on double immunosuppression (for example, steroids plus infliximab) due to the potential adverse effects of antibiotics in this population, though many advocate using prophylaxis for all patients on cyclosporine even if this is only double immunosuppressive therapy.23
Surgical Consultation
Involving a surgeon early in an ASUC patient’s care—before needing urgent colectomy—is critical. As part of the consultation, a surgeon experienced in IBD should meet with patients to discuss multistage colectomy with ileostomy and potential future J-pouch (ileal pouch-anal anastomosis) formation. Patients should be given ample opportunity to ask questions before surgery may become urgent. Also, patients should be counseled on realistic expectations of ostomy and pouch function and, ideally, meet with an ostomy nurse.23
At some centers, surgical consultation is requested on the first hospital day, but this can result in consultations for patients who ultimately respond to intravenous steroids. Therefore, some centers advocate for surgical consultation only after a patient has failed treatment with intravenous steroids (ie, day three to four) when the risk of needing surgical management increases.23
Nutrition
Bowel rest with parenteral nutrition does not improve outcomes in ASUC versus an oral diet, and there is no contraindication to allowing patients to continue on a regular diet unless they have toxic megacolon or other signs of fulminant colitis.49,50 However, patients may feel better eating less, as this will reduce their bowel movement frequency. Unfortunately, this can give a false sense of reassurance that the patient is improving. Therefore, it remains important to evaluate a patient’s symptoms in the context of their food intake.
Assessing Response to Steroids
Patients who do not respond adequately to the first-line intravenous steroid therapy will require medical or surgical rescue therapy; therefore, deciding whether a patient has responded is essential. Patients should have less than four bowel movements per day – ideally just one to two – with no blood to indicate a complete response. For more ambiguous situations, although there is no strict definition of steroid responsiveness, multiple prediction indices have attempted to identify patients who will require rescue therapy. One of the simplest, the Oxford index, illustrates two of the most critical parameters to follow, stool frequency and CRP.51 In a preinfliximab cohort, Oxford index predicted an 85% likelihood of colectomy in patients with eight or more daily bowel movements or with three to eight daily bowel movements and a CRP greater than 45 mg/L after three days of intravenous steroid treatment.52 To assist with assessing responsiveness to therapy, we ask patients to log their bowel movements – either on paper or on a whiteboard in the hospital room – so that we can review their progress daily. Other predictors of colectomy include hypoalbuminemia, scoring of endoscopic severity, and colonic dilation.53
Patients who fail to respond to intravenous corticosteroids after three days33,35 of treatment should be started on rescue therapy with infliximab or cyclosporine or undergo colectomy. A common pitfall in the treatment of ASUC is waiting for a response to steroids beyond this time frame, after which patients are unlikely to benefit.34,36 Furthermore, patients for whom surgical rescue therapy is delayed have higher operative morbidity and mortality.54,55 Because timely decision making regarding rescue therapy is crucial to optimizing outcomes, patient education efforts regarding potential rescue therapy should take place on admission or soon after, rather than waiting to ascertain steroid responsiveness.
RESCUE THERAPY FOR STEROID-REFRACTORY DISEASE
Medical options for rescue therapy include the antitumor necrosis factor (anti-TNF) agent infliximab or the calcineurin inhibitor cyclosporine. In general, infliximab and cyclosporine have been found to be roughly equivalent in efficacy in clinical trials regarding response, remission, and colectomy at 12 months.56,57 However, many clinicians prefer infliximab due to its relative ease of use, familiarity with the agent from outpatient experience, and ability to continue to use long term for maintenance of disease remission.58 In contrast to infliximab, intravenous cyclosporine requires closer monitoring and labs to assess the therapeutic trough level. The decision regarding which drug to use should be made on a case-by-case basis in conjunction with a gastroenterologist experienced in their use, and if no such specialist is available, transfer to a specialized center should be considered. Generally, successive treatment with cyclosporine or infliximab followed by third-line salvage therapy with the other drug should be avoided due to low rates of response and high rates of adverse events.59
Infliximab
Infliximab is an intravenously-administered anti-TNF monoclonal chimeric antibody that is effective both for outpatient treatment of moderate to severe UC and inpatient treatment of ASUC.1 It is relatively contraindicated in patients with untreated latent tuberculosis, demyelinating disease, advanced congestive heart failure, or uncontrolled infection.
The optimal dosing strategy for infliximab in ASUC is unknown. Infliximab clearance in the setting of ASUC is increased, partly because it is bound to albumin, which is often low in ASUC, and partly because it is excreted in the stool.60,61 As a result, accelerated loading doses may be more successful than a typical loading schedule,62 and most clinicians use alternative dosing strategies.63 Our typical approach for ASUC is an initial dose of 10 mg/kg rather than 5 mg/kg, with an additional 10 mg/kg dose 48-72 hours later if an adequate clinical response is lacking. Patients who respond to infliximab can continue to use the drug as an outpatient for maintenance of remission.
Cyclosporine
Cyclosporine is a fast-acting immunosuppressive agent that acts primarily via T-cell inhibition. Although older literature used a dose of 4 mg/kg per day, a randomized trial demonstrated similar response rates to a dose of 2 mg/kg per day.64 Patients receiving treatment with cyclosporine, which is given as a continuous infusion, must be monitored for toxicities. These can include potentially severe infection, seizures (often associated with low total cholesterol or hypomagnesemia), electrolyte abnormalities, renal impairment, hypertension, hypertrichosis, tremor, and others.65
Before initiation of treatment, serum cholesterol levels should be obtained to screen for low total cholesterol that may portend risk of seizures on the drug. Additionally, baseline creatinine and magnesium should be established. While on treatment, daily serum cyclosporine levels and electrolytes including magnesium should be measured. Patients who respond to intravenous cyclosporine must be transitioned to oral cyclosporine and have stable drug levels before discharge. Unfortunately, oral cyclosporine has not been shown to be as effective as long-term maintenance therapy. Therefore, cyclosporine can only be used as a “bridge” to another therapy. Historically, thiopurines like azathioprine or mercaptopurine have been used for this purpose because they are effective for the treatment of UC but may require months to have a full therapeutic effect. There have been promising reports of using vedolizumab similarly.66,67 Vedolizumab is a monoclonal antibody that selectively blocks lymphocyte trafficking to the gut that, like thiopurines, has an onset of action that is significantly longer than calcineurin and TNF inhibitors.
COLECTOMY
Colectomy should be considered as a second- or third-line therapy for patients who fail to respond to intravenous corticosteroids. In an analysis of 10 years of data from the Nationwide Inpatient Sample, mortality rates for colectomy in this setting varied from 0.7% at high volume centers to 4% at low volume centers.68 Therefore, if a patient is not hospitalized at a center with expertise in colectomy for UC, transfer to a specialized center should be considered. Colectomy should be performed promptly in all the patients who have failed rescue therapy with infliximab or cyclosporine or have opted against medical rescue therapy. Surgery should be performed emergently in patients with toxic megacolon, uncontrolled colonic hemorrhage or perforation.
QUALITY OF CARE AND THE USE OF CARE PATHWAYS
Physician and center-level characteristics are associated with the quality of care and outcomes in ASUC. Gastroenterologists with expertise in IBD are more likely than other gastroenterologists to request appropriate surgical consultation for steroid-refractory patients,69 and inpatients with ASUC primarily cared by gastroenterologists rather than nongastroenterologists have lower in-hospital and one-year mortality.14 Moreover, surgical outcomes differ based on center volume, with higher volume centers having lower rates of postoperative mortality.68,70 However, even at referral centers, key metrics of care quality such as rates of VTE prophylaxis, testing for C. difficile, and timely rescue therapy for steroid-refractory UC patients are suboptimal, with only 70%-82% of patients with IBD hospitalized at four referral centers in Canada meeting these metrics.71
Inpatient clinical pathways reduce LOS, reduce hospital costs, and likely reduce complications.72 For this reason, a consensus group recommended the use of care pathways for the management of ASUC and, although there is little data on the use of pathways for ASUC specifically, the use of such a pathway in the United Kingdom was associated with improved metrics including LOS, time to VTE prophylaxis, testing of stool for infection, CRP measurement, and timely gastroenterologist consultation.16,18
DISCHARGE CRITERIA AND FOLLOW UP
In general, patients should enter clinical remission, defined as resolution of rectal bleeding and diarrhea or altered bowel habits,73 before discharge, and achieving this may require a relatively prolonged hospitalization. Most patients should have one to two bowel movements a day without blood but, at a minimum, all should have less than four nonbloody bowel movements per day. Patients are candidates for discharge if they remain well after transitioning to oral prednisone at a dose of 40-60 mg daily and tolerate a regular diet.
For patients who initiated infliximab during their admission, plans for outpatient infusions including insurance approval should be made before discharge, and patients who started cyclosporine should be transitioned to oral dosing and have stable serum concentrations before leaving the hospital. Patients should leave with a preliminary plan for a steroid taper, which may vary depending on their clinical presentation. Usually, gastroenterology follow-up should be arranged after two weeks following discharge, but patients on cyclosporine need sooner laboratory monitoring.
CONCLUSION
The care of patients with ASUC requires an interdisciplinary team and close collaboration between hospitalists, gastroenterologists, and surgeons. Patients should be treated with intravenous corticosteroids and monitored carefully for response and need for rescue therapy. Establishing algorithms for the management of patients with ASUC can further improve the care of these complex patients.
Disclosures
Drs. Feuerstein, Fudman, and Sattler report no potential conflict of interest.
Funding
This work was not supported by any grant.
Ulcerative colitis (UC) is a chronic inflammatory condition of the colonic mucosa. Classically, it starts in the rectum and can extend continuously from the distal to the proximal colon. The defining clinical symptom of UC is bloody diarrhea, typically accompanied by rectal urgency and mucus discharge. The natural history of this disease includes periods of exacerbations and remissions occurring spontaneously or in response to medical treatment.1
Acute severe ulcerative colitis (ASUC) is a potentially life-threatening complication of UC that typically requires hospitalization and interdisciplinary care between hospitalists, gastroenterologists, and colorectal or general surgeons. The risk of a patient with UC requiring hospitalization for ASUC ranges from 15%-25%2,3 and, in total, UC accounts for 30,000 hospital visits annually.4 The direct medical costs exceed $4 billion annually, with hospital costs of over $960 million.5 Historically, mortality from ASUC was as high as 24% but decreased substantially to 7% after the introduction of systemic corticosteroid therapy.6 Further advances in care have reduced mortality to approximately 1% or less.7,8 Nonetheless, up to 20% of patients admitted with ASUC have a colectomy on their first admission, and this rate rises to 40% after two admissions.2
DEFINING ACUTE SEVERE ULCERATIVE COLITIS
To categorize UC severity, assess patients using the Truelove and Witt’s criteria. The system classifies patients as having mild, moderate, severe, or fulminant disease. Severe disease by these criteria includes patients with >6 bloody bowel movements per day and at least one of the following clinical features: fever (>37.8°C), tachycardia (>90 bpm), anemia (hemoglobin <10.5 g/dl), or elevated inflammatory markers (traditionally, erythrocyte sedimentation rate greater than 30 mm/h or, more recently, C-reactive protein (CRP) greater than 30 mg/L. (Table 1).6,9
Fulminant colitis refers to a subgroup of patients with more than 10 stools per day, continuous bleeding, abdominal pain, colonic dilatation on abdominal X-ray film, and severe toxic symptoms including fever and anorexia. Such patients are at risk of progressing to toxic megacolon and bowel perforation.10
INDICATIONS FOR HOSPITALIZATION AND INPATIENT LEVEL OF CARE
Patients with ASUC almost always require hospitalization for their disease management. In many cases, these patients have been receiving outpatient oral prednisone 40-60 mg daily but continue to have ongoing disease activity.11 Most patients will require close clinical monitoring, frequent blood testing, endoscopic or radiologic evaluation, as well as administration of intravenous corticosteroids. The average length of stay (LOS) ranges from 4.6 to 12.5 days, depending on disease severity.12 Not surprisingly, Kelso et al. reported that predictors of hospital LOS greater than four days include initiating a biologic drug in the hospital, undergoing two or more imaging modalities and treatment with intravenous steroids,13 and so it is rare that patients do not meet billing requirements for an inpatient level of care.
INITIAL EVALUATION
The multifaceted initial inpatient evaluation of patients with ASUC aims to assess disease severity, identify and prevent potential complications, and initiate planning for potential failure of first-line pharmacologic therapy. Due to the accumulating evidence that involving physicians with expertise in managing ASUC improves outcomes, gastroenterologists should be involved in the care of patients with ASUC from the time of their admission.14,15 Additionally, creating standardized care pathways for the management of ASUC can reduce cost, LOS, and improve quality.16
History and Physical Examination
Patients should be asked about fever, abdominal pain, nausea, emesis, bloating, weight loss, and bowel movements (frequency, consistency, the presence of blood, urgency, nighttime awakenings). The number of bowel movements over a 24-hour period should be quantified as this helps assess the overall disease severity (Table 1).
The patient’s initial inflammatory bowel disease (IBD) history is also essential. The review of pertinent information regarding the patient’s initial diagnosis of UC includes the severity and anatomic extent of disease, extraintestinal manifestations, previous medical therapies, and surgical interventions. Exposure to nonsteroidal anti-inflammatory drugs (NSAIDs) or antibiotics should be identified as they may precipitate flares.17 Travel history may be pertinent as travel increases the risk of infections with food-borne or parasitic pathogens.18
Physical examination begins with an assessment of vital signs and volume status. Abdominal examination should include evaluation of bowel sounds, an assessment of distention, location, the extent of abdominal tenderness, and peritoneal signs. The abdominal exam should be interpreted in the context of the patient’s medications, as the use of steroid or analgesic therapies may affect the sensitivity for detecting complications. An external rectal exam evaluating perianal disease should be performed, as perianal disease raises concern for Crohn’s, a disease whose surgical management differs from UC.
A careful exam for extraintestinal manifestations is also essential. The skin should be evaluated for any new rashes, especially on the anterior shin consistent with erythema nodosum or ulcerated lesions on the skin suggestive of pyoderma gangrenosum. The peripheral joints should also be examined for any synovitis. Additional examinations should be performed based on any reported symptoms (eg, the ophthalmic exam for uveitis or scleritis if visual changes or eye pain are reported). Some extraintestinal manifestations require subspecialty consultation and comanagement to guide disease therapy. Patients with underlying pyoderma gangrenosum may require a dermatology consultation to guide management. Ocular inflammation requires ophthalmology involvement, and inflammatory arthritis is best comanaged with rheumatology.19
Laboratory Testing
Initial testing should include a complete blood count with differential, basic metabolic panel, and liver chemistries including alkaline phosphatase and albumin. When relevant, pregnancy testing should be performed. Measure CRP on admission so that its trajectory can be followed during therapy. However, a normal CRP does not exclude the presence of a UC flare as a subset of patients with ASUC will have a normal CRP despite severe mucosal inflammation.20
Since one-third of patients do not respond to intravenous corticosteroids and will require rescue therapy during the hospitalization with infliximab or cyclosporine, anticipatory testing for these medications should be performed on admission to avoid delays in the administration of rescue therapy.6,21 This should include an interferon-gamma release assay (eg, quantiferon gold) to test for latent tuberculosis and hepatitis B serologies in anticipation of possible treatment with infliximab. An interferon-gamma release assay is preferred to a tuberculin skin test because patients may be anergic, and a skin test does not provide a control to determine whether a negative test is due to anergy. In contrast, although a quantiferon gold test can be indeterminate in ASUC due to disease activity and systemic steroids, the results indicate if the patient is anergic so that one will not rely on a false-negative result. In the event of an equivocal result, a careful clinical assessment for risks of TB exposures should be elicited, and a chest radiograph should be obtained.22 In patients with prior high risk of tuberculosis exposures or a positive test for tuberculosis, an infectious disease specialist should be consulted early to advise if therapy should be started in preparation for the potential use of infliximab.23 In cases where cyclosporine may be considered, magnesium and total cholesterol level should be checked. Sending thiopurine methyltranferase (TPMT) enzyme activity should be considered as well, in case of a need for future thiopurine use for maintenance of disease activity.24
Infectious diarrhea may be indistinguishable from ASUC and may also be the trigger of a flare; thus, it is important to rule out infection with stool microbiologic studies. Most importantly, Clostridium difficile infection must be ruled out in all patients with ASUC. Although patients with IBD, especially those with UC, have significantly higher rates of asymptomatic C. difficile carriage than the general population, a positive polymerase chain reaction test for C. difficile in a patient with ASUC should prompt treatment with oral vancomycin.25 However, if carriage if suspected and a subsequent enzyme-linked immunoassay for C. difficile toxin is negative, treatment can be discontinued. Active C. difficile infection in patients with IBD is associated with increased disease severity, greater length of hospital stay, and increased the likelihood of colectomy and mortality.26,27 Other bacterial infections including Escherichia coli, Campylobacter, Shigella, Salmonella, Yersinia, Entamoeba histolytica, as well as other parasitic infestations may mimic UC. Testing should be considered in cases of foreign travel, immunosuppression or contact with other persons with diarrhea.7,28 Routine testing of these other enteric infections without a clear exposure risk is of little benefit and may raise costs.23,29
Radiologic Evaluation
A plain X-ray film of the abdomen should be obtained in all patients on admission to evaluate for evolving colonic dilation or undiagnosed free air. Small bowel distension >3 cm may predict an increased risk of colectomy.30 Clinicians must be mindful that steroids can mask peritoneal signs and that retroperitoneal perforations may not be apparent on plain X-ray films. Nonetheless, a CT of the abdomen is usually not necessary and should be reserved for cases with severe abdominal pain out of proportion to clinical signs in which a plain X-ray film is unrevealing. Judicious use of CT imaging is especially important in younger patients, as there is growing concern that patients with IBD may be exposed to potentially harmful cumulative levels of radiation in their lifetime from repeated CT imaging.31
Endoscopic Evaluation
Flexible sigmoidoscopy aids in the assessment of disease severity and extent and biopsies can assist in ruling out a diagnosis of cytomegalovirus (CMV) colitis in patients already on immunosuppression. For this reason, many clinicians prefer to perform a sigmoidoscopy on admission.23 If one is not performed on admission, a sigmoidoscopy is advised in all patients who are not responding adequately after 72 hours of intravenous steroid therapy in order to rule out superimposed CMV colitis.28
Sigmoidoscopy should be avoided in patients with toxic megacolon and when there is a concern for peritonitis. A complete colonoscopy is rarely indicated in the acute setting and carries a theoretical risk of colonic perforation.7
INITIAL THERAPY
The first therapeutic steps aim to reduce inflammation with the use of systemic corticosteroids, avoid colonic and extraintestinal complications, and plan for the potential need for rescue therapy.
Intravenous Corticosteroids
The cornerstone of ASUC management is treatment with intravenous corticosteroids. Their initiation should not be delayed in patients with an established diagnosis of UC while waiting for results of evaluations for infectious colitis. Even among patients who have failed oral steroids, a meta-regression analysis showed that two-thirds of patients will still respond to intravenous corticosteroids.21,32 Methylprednisolone 20 mg IV three times daily (or hydrocortisone 100 mg IV three times daily) is a standard regimen; higher doses do not provide additional benefit.21 Patients’ response to intravenous steroids should be assessed with repeat labs including CRP and an assessment of the total number of bowel movements over a 24-hour period, with special attention to their overall response after three days of treatment.33-36
Intravenous Fluids
Many patients admitted with ASUC will have significant volume depletion, and intravenous fluids should be administered in a manner like other volume-depleted or oral-intake-restricted patients.
Venous Thromboembolism Prophylaxis
The risk of VTE in hospitalized patients with IBD exceeds that of inpatients without IBD, approximately 2%, a risk similar to patients with respiratory failure.37 Additionally, VTE in hospitalized patients with IBD is associated with a 2.5-fold increase in mortality.38,39 Therefore, all patients hospitalized with ASUC should receive subcutaneous unfractionated or low molecular weight heparin or fondaparinux for VTE prophylaxis. Rectal bleeding, expected in ASUC, is not a contraindication to chemo-prophylaxis. Additionally, it is important to check if patients are receiving the ordered VTE prophylaxis.40,41 Pleet et al. found that only 7% of patients at a tertiary center had adequate prophylaxis for greater than 80% of their hospitalization.41
Unnecessary or Potentially Harmful Medications
Several medications have the potential for misuse in patients hospitalized with UC.
Antimotility Agents
Loperamide, diphenoxylate, and opiate antidiarrheals should not be used as they may provoke toxic megacolon.42 Similarly, drugs with antimotility side effects (eg, anticholinergics) should be avoided.
Opiates
In addition to their undesirable antimotility effect, the use of opiates has been associated with poor outcomes among inpatients and outpatients with IBD, including increased morbidity and mortality.43,44 Pain severe enough to require opiates should raise suspicion for toxic megacolon, perforation, or a noninflammatory etiology. If opiates are utilized, they should be ordered as one-time doses and the patient should be reassessed for each dose.
Nonsteroidal Anti-inflammatory Drugs
These drugs, which include oral NSAIDs, intravenous ketorolac, and topic diclofenac gels, may increase disease activity in inflammatory bowel disease and should be avoided.17
5-aminosalicylates (5-ASA)
A small proportion of patients experience a paradoxical worsening of diarrhea due to the use of 5-ASA agents such as mesalamine. It is reasonable to discontinue or avoid the use of 5-ASA agents in hospitalized patients, especially as there is little to no benefit from combining a 5-ASA with a biologic or immunosuppressive drug.45
Antibiotics
There is no role for the routine use of antibiotics in patients hospitalized with ASUC. 23,46,47 Inappropriate use of antibiotics raises the risk of C. difficile infection and antibiotic resistance. However, in cases of suspected toxic megacolon or perforation, antibiotics should be administered. In situations in which a patient is treated with triple immunosuppression (ie, steroids plus two other agents, cyclosporine and mercaptopurine) antibiotic prophylaxis for Pneumocystis jiroveci is advisable.48 Using a large insurance database, Long et al. reported a low absolute incidence of Pneumocystis jiroveci in IBD patients but noted that the risk in patients with IBD was still significantly higher than matched controls. While it can be considered, we typically refrain from using prophylaxis in patients on double immunosuppression (for example, steroids plus infliximab) due to the potential adverse effects of antibiotics in this population, though many advocate using prophylaxis for all patients on cyclosporine even if this is only double immunosuppressive therapy.23
Surgical Consultation
Involving a surgeon early in an ASUC patient’s care—before needing urgent colectomy—is critical. As part of the consultation, a surgeon experienced in IBD should meet with patients to discuss multistage colectomy with ileostomy and potential future J-pouch (ileal pouch-anal anastomosis) formation. Patients should be given ample opportunity to ask questions before surgery may become urgent. Also, patients should be counseled on realistic expectations of ostomy and pouch function and, ideally, meet with an ostomy nurse.23
At some centers, surgical consultation is requested on the first hospital day, but this can result in consultations for patients who ultimately respond to intravenous steroids. Therefore, some centers advocate for surgical consultation only after a patient has failed treatment with intravenous steroids (ie, day three to four) when the risk of needing surgical management increases.23
Nutrition
Bowel rest with parenteral nutrition does not improve outcomes in ASUC versus an oral diet, and there is no contraindication to allowing patients to continue on a regular diet unless they have toxic megacolon or other signs of fulminant colitis.49,50 However, patients may feel better eating less, as this will reduce their bowel movement frequency. Unfortunately, this can give a false sense of reassurance that the patient is improving. Therefore, it remains important to evaluate a patient’s symptoms in the context of their food intake.
Assessing Response to Steroids
Patients who do not respond adequately to the first-line intravenous steroid therapy will require medical or surgical rescue therapy; therefore, deciding whether a patient has responded is essential. Patients should have less than four bowel movements per day – ideally just one to two – with no blood to indicate a complete response. For more ambiguous situations, although there is no strict definition of steroid responsiveness, multiple prediction indices have attempted to identify patients who will require rescue therapy. One of the simplest, the Oxford index, illustrates two of the most critical parameters to follow, stool frequency and CRP.51 In a preinfliximab cohort, Oxford index predicted an 85% likelihood of colectomy in patients with eight or more daily bowel movements or with three to eight daily bowel movements and a CRP greater than 45 mg/L after three days of intravenous steroid treatment.52 To assist with assessing responsiveness to therapy, we ask patients to log their bowel movements – either on paper or on a whiteboard in the hospital room – so that we can review their progress daily. Other predictors of colectomy include hypoalbuminemia, scoring of endoscopic severity, and colonic dilation.53
Patients who fail to respond to intravenous corticosteroids after three days33,35 of treatment should be started on rescue therapy with infliximab or cyclosporine or undergo colectomy. A common pitfall in the treatment of ASUC is waiting for a response to steroids beyond this time frame, after which patients are unlikely to benefit.34,36 Furthermore, patients for whom surgical rescue therapy is delayed have higher operative morbidity and mortality.54,55 Because timely decision making regarding rescue therapy is crucial to optimizing outcomes, patient education efforts regarding potential rescue therapy should take place on admission or soon after, rather than waiting to ascertain steroid responsiveness.
RESCUE THERAPY FOR STEROID-REFRACTORY DISEASE
Medical options for rescue therapy include the antitumor necrosis factor (anti-TNF) agent infliximab or the calcineurin inhibitor cyclosporine. In general, infliximab and cyclosporine have been found to be roughly equivalent in efficacy in clinical trials regarding response, remission, and colectomy at 12 months.56,57 However, many clinicians prefer infliximab due to its relative ease of use, familiarity with the agent from outpatient experience, and ability to continue to use long term for maintenance of disease remission.58 In contrast to infliximab, intravenous cyclosporine requires closer monitoring and labs to assess the therapeutic trough level. The decision regarding which drug to use should be made on a case-by-case basis in conjunction with a gastroenterologist experienced in their use, and if no such specialist is available, transfer to a specialized center should be considered. Generally, successive treatment with cyclosporine or infliximab followed by third-line salvage therapy with the other drug should be avoided due to low rates of response and high rates of adverse events.59
Infliximab
Infliximab is an intravenously-administered anti-TNF monoclonal chimeric antibody that is effective both for outpatient treatment of moderate to severe UC and inpatient treatment of ASUC.1 It is relatively contraindicated in patients with untreated latent tuberculosis, demyelinating disease, advanced congestive heart failure, or uncontrolled infection.
The optimal dosing strategy for infliximab in ASUC is unknown. Infliximab clearance in the setting of ASUC is increased, partly because it is bound to albumin, which is often low in ASUC, and partly because it is excreted in the stool.60,61 As a result, accelerated loading doses may be more successful than a typical loading schedule,62 and most clinicians use alternative dosing strategies.63 Our typical approach for ASUC is an initial dose of 10 mg/kg rather than 5 mg/kg, with an additional 10 mg/kg dose 48-72 hours later if an adequate clinical response is lacking. Patients who respond to infliximab can continue to use the drug as an outpatient for maintenance of remission.
Cyclosporine
Cyclosporine is a fast-acting immunosuppressive agent that acts primarily via T-cell inhibition. Although older literature used a dose of 4 mg/kg per day, a randomized trial demonstrated similar response rates to a dose of 2 mg/kg per day.64 Patients receiving treatment with cyclosporine, which is given as a continuous infusion, must be monitored for toxicities. These can include potentially severe infection, seizures (often associated with low total cholesterol or hypomagnesemia), electrolyte abnormalities, renal impairment, hypertension, hypertrichosis, tremor, and others.65
Before initiation of treatment, serum cholesterol levels should be obtained to screen for low total cholesterol that may portend risk of seizures on the drug. Additionally, baseline creatinine and magnesium should be established. While on treatment, daily serum cyclosporine levels and electrolytes including magnesium should be measured. Patients who respond to intravenous cyclosporine must be transitioned to oral cyclosporine and have stable drug levels before discharge. Unfortunately, oral cyclosporine has not been shown to be as effective as long-term maintenance therapy. Therefore, cyclosporine can only be used as a “bridge” to another therapy. Historically, thiopurines like azathioprine or mercaptopurine have been used for this purpose because they are effective for the treatment of UC but may require months to have a full therapeutic effect. There have been promising reports of using vedolizumab similarly.66,67 Vedolizumab is a monoclonal antibody that selectively blocks lymphocyte trafficking to the gut that, like thiopurines, has an onset of action that is significantly longer than calcineurin and TNF inhibitors.
COLECTOMY
Colectomy should be considered as a second- or third-line therapy for patients who fail to respond to intravenous corticosteroids. In an analysis of 10 years of data from the Nationwide Inpatient Sample, mortality rates for colectomy in this setting varied from 0.7% at high volume centers to 4% at low volume centers.68 Therefore, if a patient is not hospitalized at a center with expertise in colectomy for UC, transfer to a specialized center should be considered. Colectomy should be performed promptly in all the patients who have failed rescue therapy with infliximab or cyclosporine or have opted against medical rescue therapy. Surgery should be performed emergently in patients with toxic megacolon, uncontrolled colonic hemorrhage or perforation.
QUALITY OF CARE AND THE USE OF CARE PATHWAYS
Physician and center-level characteristics are associated with the quality of care and outcomes in ASUC. Gastroenterologists with expertise in IBD are more likely than other gastroenterologists to request appropriate surgical consultation for steroid-refractory patients,69 and inpatients with ASUC primarily cared by gastroenterologists rather than nongastroenterologists have lower in-hospital and one-year mortality.14 Moreover, surgical outcomes differ based on center volume, with higher volume centers having lower rates of postoperative mortality.68,70 However, even at referral centers, key metrics of care quality such as rates of VTE prophylaxis, testing for C. difficile, and timely rescue therapy for steroid-refractory UC patients are suboptimal, with only 70%-82% of patients with IBD hospitalized at four referral centers in Canada meeting these metrics.71
Inpatient clinical pathways reduce LOS, reduce hospital costs, and likely reduce complications.72 For this reason, a consensus group recommended the use of care pathways for the management of ASUC and, although there is little data on the use of pathways for ASUC specifically, the use of such a pathway in the United Kingdom was associated with improved metrics including LOS, time to VTE prophylaxis, testing of stool for infection, CRP measurement, and timely gastroenterologist consultation.16,18
DISCHARGE CRITERIA AND FOLLOW UP
In general, patients should enter clinical remission, defined as resolution of rectal bleeding and diarrhea or altered bowel habits,73 before discharge, and achieving this may require a relatively prolonged hospitalization. Most patients should have one to two bowel movements a day without blood but, at a minimum, all should have less than four nonbloody bowel movements per day. Patients are candidates for discharge if they remain well after transitioning to oral prednisone at a dose of 40-60 mg daily and tolerate a regular diet.
For patients who initiated infliximab during their admission, plans for outpatient infusions including insurance approval should be made before discharge, and patients who started cyclosporine should be transitioned to oral dosing and have stable serum concentrations before leaving the hospital. Patients should leave with a preliminary plan for a steroid taper, which may vary depending on their clinical presentation. Usually, gastroenterology follow-up should be arranged after two weeks following discharge, but patients on cyclosporine need sooner laboratory monitoring.
CONCLUSION
The care of patients with ASUC requires an interdisciplinary team and close collaboration between hospitalists, gastroenterologists, and surgeons. Patients should be treated with intravenous corticosteroids and monitored carefully for response and need for rescue therapy. Establishing algorithms for the management of patients with ASUC can further improve the care of these complex patients.
Disclosures
Drs. Feuerstein, Fudman, and Sattler report no potential conflict of interest.
Funding
This work was not supported by any grant.
1. Sands BE. Mount Sinai Expert Guides: Gastroenterology. Hoboken, NJ: John Wiley & Sons; 2014.
2. Dinesen LC, Walsh AJ, Protic MN, et al. The pattern and outcome of acute severe colitis. J Crohns Colitis. 2010;4(4):431-437. https://doi.org/10.1016/j.crohns.2010.02.001.
3. Edwards FC, Truelove SC. The course and prognosis of ulcerative colitis. Gut. 1963;4:299-315. https://doi.org/10.1136/gut.4.4.299.
4. Sonnenberg A, Chang J. Time trends of physician visits for Crohn’s disease and ulcerative colitis in the United States, 1960-2006. 2007;14(2):249-252. https://doi.org/10.1002/ibd.20273.
5. Nguyen GC, Tuskey A, Dassopoulos T, Harris ML, Brant SR. Rising hospitalization rates for inflammatory bowel disease in the United States between 1998 and 2004. Inflamm Bowel Dis. 2007;13(12):1529-1535. https://doi.org/10.1002/ibd.20250.
6. Truelove S, Witts L. Cortisone in ulcerative colitis. Br Med J. 1955;2:104-108.
7. Jakobovits SL, Travis S. Management of acute severe colitis. Br Med Bull. 2005;75(1):131-144. https://doi.org/10.1093/bmb/ldl001.
8. Lynch R, Lowe D, Protheroe A, Driscoll R, Rhodes J, Arnott I. Outcomes of rescue therapy in acute severe ulcerative colitis: data from the United Kingdom inflammatory bowel disease audit. Aliment Pharmacol Ther. 2013;38(8):935-945. https://doi.org/10.1111/apt.12473.
9. Magro F, Gionchetti P, Eliakim R, et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 1: definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileoanal pouch disorders. J Crohns Colitis. 2017;11(6):649-670. https://doi.org/10.1093/ecco-jcc/jjx008.
10. Kornbluth A, Sachar DB. Ulcerative colitis practice guidelines in adults: American college of gastroenterology, practice parameters committee. Am J Gastroenterol. 2010;105(3):501. https://doi.org/10.1038/ajg.2009.727.
11. Dassopoulos T, Cohen RD, Scherl EJ, Schwartz RM, Kosinski L, Regueiro MD. Ulcerative colitis care pathway. Gastroenterology. 2015;149(1):238-245. https://doi.org/10.1053/j.gastro.2015.05.036.
12. Ananthakrishnan AN, McGinley EL, Binion DG, Saeian K. A nationwide analysis of changes in severity and outcomes of inflammatory bowel disease hospitalizations. J Gastrointest Surg. 2011;15(2):267-276. https://doi.org/10.1007/s11605-010-1396-3.
13. Kelso M, Weideman RA, Cipher DJ, Feagins LA. Factors associated with length of stay in veterans with inflammatory bowel disease hospitalized for an acute flare. Inflamm Bowel Dis. 2017;24(1):5-11. https://doi.org/10.1093/ibd/izx020.
14. Murthy SK, Steinhart AH, Tinmouth J, Austin PC, Nguyen GC. Impact of gastroenterologist care on health outcomes of hospitalized ulcerative colitis patients. Gut. 2012;61(10):1410-1416. https://doi.org/10.1136/gutjnl-2011-301978.
15. Lee NS, Pola S, Groessl EJ, Rivera-Nieves J, Ho SB. Opportunities for improvement in the care of patients hospitalized for inflammatory bowel disease-related colitis. Dig Dis Sci. 2016;61(4):1003-1012. https://doi.org/10.1007/s10620-016-4046-0.
16. Neary BP, Doherty GA. A structured care pathway improves quality of care for acute severe ulcerative colitis. Gastroenterology. 2017;152(5):S218. https://doi.org/10.1016/S0016-5085(17)31028-4.
17. Klein A, Eliakim R. Nonsteroidal anti-inflammatory drugs and inflammatory bowel disease. Pharmaceuticals. 2010;3(4):1084-1092. https://doi.org/10.3390/ph3041084.
18. Chen JH, Andrews JM, Kariyawasam V, et al. Review article: acute severe ulcerative colitis - evidence-based consensus statements. Aliment Pharmacol Ther. 2016;44(2):127-144. https://doi.org/10.1111/apt.13670.
19. Vavricka SR, Schoepfer A, Scharl M, Lakatos PL, Navarini A, Rogler G. Extraintestinal manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2015;21(8):1982-1992. https://doi.org/10.1097/MIB.0000000000000392.
20. Solem CA, Loftus EV, Jr., Tremaine WJ, Harmsen WS, Zinsmeister AR, Sandborn WJ. Correlation of C-reactive protein with clinical, endoscopic, histologic, and radiographic activity in inflammatory bowel disease. Inflamm Bowel Dis. 2005;11(8):707-712. https://doi.org/10.1097/01.MIB.0000173271.18319.53.
21. Turner D, Walsh CM, Steinhart AH, Griffiths AM. Response to corticosteroids in severe ulcerative colitis: a systematic review of the literature and a meta-regression. Clin Gastroenterol Hepatol. 2007;5(1):103-110. https://doi.org/10.1016/j.cgh.2006.09.033.
22. Kaur M, Singapura P, Kalakota N, et al. Factors that contribute to indeterminate results from the QuantiFERON-TB Gold in-tube test in patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2018;16(10):1616-1621.e1. https://doi.org/10.1016/j.cgh.2017.11.038.
23. Bitton A, Buie D, Enns R, et al. Treatment of hospitalized adult patients with severe ulcerative colitis: Toronto consensus statements. Am J Gastroenterol. 2012;107(2):179-194. https://doi.org/10.1038/ajg.2011.386.
24. Feuerstein JD, Nguyen GC, Kupfer SS, Falck-Ytter Y, Singh S. American Gastroenterological Association Institute Clinical Guidelines committee. American Gastroenterological Association Institute Guideline on therapeutic drug monitoring in inflammatory bowel disease. Gastroenterology. 2017;153(3):827-834.
25. McDonald LC, Gerding DN, Johnson S, et al. Clinical Practice Guidelines for Clostridium difficile infection in adults and children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018;66(7):e1-e48. https://doi.org/10.1093/cid/cix1085.
26. Clayton EM, Rea MC, Shanahan F, et al. The vexed relationship between Clostridium difficile and inflammatory bowel disease: an assessment of carriage in an outpatient setting among patients in remission. Am J Gastroenterol. 2009;104(5):1162-1169. https://doi.org/10.1038/ajg.2009.4.
27. Nguyen GC, Kaplan GG, Harris ML, Brant SR. A national survey of the prevalence and impact of Clostridium difficile infection among hospitalized inflammatory bowel disease patients. Am J Gastroenterol. 2008;103(6):1443-1450. https://doi.org/10.1111/j.1572-0241.2007.01780.x.
28. Rahier J-F, Yazdanpanah Y, Colombel J-F, Travis S. The European (ECCO) Consensus on infection in IBD: what does it change for the clinician? Gut. 2009;58(10). https://doi.org/10.1136/gut.2008.175950.
29. Meyer AM, Ramzan NN, Loftus EV, Jr., Heigh RI, Leighton JA. The diagnostic yield of stool pathogen studies during relapses of inflammatory bowel disease. J Clin Gastroenterol. 2004;38(9):772-775. https://doi.org/10.1097/01.mcg.0000139057.05297.d6.
30. Chew C, Nolan D, Jewell D. Small bowel gas in severe ulcerative colitis. Gut. 1991;32(12):1535-1537. https://doi.org/10.1136/gut.32.12.1535.
31. Zakeri N, Pollok RC. Diagnostic imaging and radiation exposure in inflammatory bowel disease. World J Gastroenterol. 2016;22(7):2165-2178. https://doi.org/10.3748/wjg.v22.i7.2165.
32. Llaó J, Naves JE, Ruiz-Cerulla A, et al. Intravenous corticosteroids in moderately active ulcerative colitis refractory to oral corticosteroids. J Crohns Colitis. 2014;8(11):1523-1528. https://doi.org/10.1016/j.crohns.2014.06.010.
33. Seo M, Okada M, Yao T, Matake H, Maeda K. Evaluation of the clinical course of acute attacks in patients with ulcerative colitis through the use of an activity index. Journal of Gastroenterology. 2002;37(1):29-34. https://doi.org/10.1007/s535-002-8129-2.
34. Meyers S, Sachar DB, Goldberg JD, Janowitz HD. Corticotropin versus hydrocortisone in the intravenous treatment of ulcerative colitis: a prospective, randomized, double-blind clinical trial. Gastroenterology. 1983;85(2):351-357.
35. Ho G, Mowat C, Goddard C, et al. Predicting the outcome of severe ulcerative colitis: development of a novel risk score to aid early selection of patients for second‐line medical therapy or surgery. Aliment Pharmacol Ther. 2004;19(10):1079-1087. https://doi.org/10.1111/j.1365-2036.2004.01945.x.
36. Järnerot G, Rolny P, Sandberg-Gertzen H. Intensive intravenous treatment of ulcerative colitis. Gastroenterology. 1985;89(5):1005-1013. https://doi.org/10.1016/0016-5085(85)90201-X.
37. Wang JY, Terdiman JP, Vittinghoff E, Minichiello T, Varma MG. Hospitalized ulcerative colitis patients have an elevated risk of thromboembolic events. World J Gastroenterol. 2009;15(8):927-935. https://doi.org/10.3748/wjg.15.927.
38. Nguyen GC, Bernstein CN, Bitton A, et al. Consensus statements on the risk, prevention, and treatment of venous thromboembolism in inflammatory bowel disease: Canadian Association of Gastroenterology. Gastroenterology. 2014;146(3):835-848. https://doi.org/10.1053/j.gastro.2014.01.042.
39. Nguyen GC, Sam J. Rising prevalence of venous thromboembolism and its impact on mortality among hospitalized inflammatory bowel disease patients. Am J Gastroenterol. 2008;103(9):2272-2280. https://doi.org/10.1111/j.1572-0241.2008.02052.x.
40. Tinsley A, Naymagon S, Enomoto LM, Hollenbeak CS, Sands BE, Ullman TA. Rates of pharmacologic venous thromboembolism prophylaxis in hospitalized patients with active ulcerative colitis: results from a tertiary care center. J Crohns Colitis. 2013;7(12):e635-e640. https://doi.org/10.1016/j.crohns.2013.05.002.
41. Pleet JL, Vaughn BP, Morris JA, Moss AC, Cheifetz AS. The use of pharmacological prophylaxis against venous thromboembolism in hospitalized patients with severe active ulcerative colitis. Aliment Pharmacol Ther. 2014;39(9):940-948. https://doi.org/10.1111/apt.12691.
42. Gan SI, Beck PL. A new look at toxic megacolon: an update and review of incidence, etiology, pathogenesis, and management. Am J Gastroenterol. 2003;98(11):2363-2371 https://doi.org/10.1111/j.1572-0241.2003.07696.x.
43. Lichtenstein GR, Feagan BG, Cohen RD, et al. Serious infections and mortality in association with therapies for Crohn’s disease: TREAT registry. Clin Gastroenterol Hepatol. 2006;4(5):621-630. https://doi.org/10.1016/j.cgh.2006.03.002.
44. Docherty MJ, Jones III RCW, Wallace MS. Managing pain in inflammatory bowel disease. Gastroenterol Hepatol. 2011;7(9):592-601.
45. Singh S, Proudfoot JA, Dulai PS, et al. No benefit of concomitant 5-aminosalicylates in patients with ulcerative colitis escalated to biologic therapy: pooled analysis of individual participant data from clinical trials. Am J Gastroenterol. 2018;113(8):1197-1205. https://doi.org/10.1038/s41395-018-0144-2.
46. Mantzaris GJ, Hatzis A, Kontogiannis P, Triadaphyllou G. Intravenous tobramycin and metronidazole as an adjunct to corticosteroids in acute, severe ulcerative colitis. Am J Gastroenterol. 1994;89(1):43-46.
47. Mantzaris GJ, Petraki K, Archavlis E, et al. A prospective randomized controlled trial of intravenous ciprofloxacin as an adjunct to corticosteroids in acute, severe ulcerative colitis. Scand J Gastroenterol. 2001;36(9):971-974.
48. Rahier J-F, Magro F, Abreu C, et al. Second European evidence-based consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease. J Crohns Colitis. 2014;8(6):443-468. https://doi.org/10.1016/j.crohns.2013.12.013.
49. Dickinson RJ, Ashton MG, Axon AT, Smith RC, Yeung CK, Hill GL. Controlled trial of intravenous hyperalimentation and total bowel rest as an adjunct to the routine therapy of acute colitis. Gastroenterology. 1980;79(6):1199-1204.
50. McIntyre P, Powell-Tuck J, Wood S, et al. Controlled trial of bowel rest in the treatment of severe acute colitis. Gut. 1986;27(5):481-485. https://doi.org/10.1136/gut.27.5.481.
51. Travis SP, Farrant JM, Ricketts C, et al. Predicting outcome in severe ulcerative colitis. Gut. 1996;38(6):905-910. https://doi.org/10.1136/gut.38.6.905.
52. Bernardo S, Fernandes SR, Goncalves AR, et al. Predicting the course of disease in hospitalized patients with acute severe ulcerative colitis. Inflamm Bowel Dis. 2018;25(3):541-546. https://doi.org/10.1093/ibd/izy256.
53. Harbord M, Eliakim R, Bettenworth D, et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 2: current management. J Crohns Colitis. 2017;11(7):769-784. https://doi.org/10.1093/ecco-jcc/jjx009.
54. Randall J, Singh B, Warren B, Travis S, Mortensen N, George B. Delayed surgery for acute severe colitis is associated with increased risk of postoperative complications. Br J Surg. 2010;97(3):404-409. https://doi.org/10.1002/bjs.6874.
55. Bartels S, Gardenbroek T, Ubbink D, Buskens C, Tanis P, Bemelman W. Systematic review and meta‐analysis of laparoscopic versus open colectomy with end ileostomy for non‐toxic colitis. Br J Surg. 2013;100(6):726-733. https://doi.org/10.1002/bjs.9061.
56. Laharie D, Bourreille A, Branche J, et al. Ciclosporin versus infliximab in patients with severe ulcerative colitis refractory to intravenous steroids: a parallel, open-label randomized controlled trial. Lancet. 2012;380(9857):1909-1915. https://doi.org/10.1016/S0140-6736(12)61084-8.
57. Leblanc S, Allez M, Seksik P, et al. Successive treatment with cyclosporine and infliximab in steroid-refractory ulcerative colitis. Am J Gastroenterol. 2011;106(4):771-777. https://doi.org/10.1038/ajg.2011.62.
58. Narula N, Marshall JK, Colombel JF, et al. Systematic review and meta-analysis: infliximab or cyclosporine as rescue therapy in patients with severe ulcerative colitis refractory to steroids. Am J Gastroenterol. 2016;111(4):477-491. https://doi.org/10.1038/ajg.2016.7.
59. Feuerstein JD, Akbari M, Tapper EB, Cheifetz AS. Systematic review and meta-analysis of third-line salvage therapy with infliximab or cyclosporine in severe ulcerative colitis. Ann Gastroenterol. 2016;29(3):341-347. https://doi.org/10.20524/aog.2016.0032.
60. Brandse JF, Mathôt RA, van der Kleij D, et al. Pharmacokinetic features and presence of antidrug antibodies associated with response to infliximab induction therapy in patients with moderate to severe ulcerative colitis. Clin Gastroenterol Hepatol. 2016;14(2):251-258. https://doi.org/10.1016/j.cgh.2015.10.029.
61. Hindryckx P, Novak G, Vande Casteele N, et al. Review article: dose optimization of infliximab for acute severe ulcerative colitis. Aliment Pharmacol Ther. 2017;45(5):617-630. https://doi.org/10.1111/apt.13913.
62. Gibson DJ, Heetun ZS, Redmond CE, et al. An accelerated infliximab induction regimen reduces the need for early colectomy in patients with acute severe ulcerative colitis. Clin Gastroenterol Hepatol. 2015;13(2):330-335. https://doi.org/10.1016/j.cgh.2014.07.041.
63. Herfarth HH, Rogler G, Higgins PD. Pushing the pedal to the metal: should we accelerate infliximab therapy for patients with severe ulcerative colitis? Clin Gastroenterol Hepatol. 2015;13(2):336-338. https://doi.org/10.1016/j.cgh.2014.09.045.
64. Van Assche G, D’haens G, Noman M, et al. Randomized, double-blind comparison of 4 mg/kg versus 2 mg/kg intravenous cyclosporine in severe ulcerative colitis. Gastroenterology. 2003;125(4):1025-1031.
65. Arts J, D’haens G, Zeegers M, et al. Long-term outcome of treatment with intravenous cyclosporin in patients with severe ulcerative colitis. Inflamm Bowel Dis. 2004;10(2):73-78.
66. Tarabar D, El Jurdi K, Yvellez O, et al. 330-combination therapy of cyclosporine and vedolizumab is effective and safe for severe, steroid-resistant ulcerative colitis patients: a prospective study. Gastroenterology. 2018;154(6):S-82-S-83.https://doi.org/10.1016/S0016-5085(18)30725-X.
67. Szántó K, Molnár T, Farkas K. New promising combo therapy in inflammatory bowel diseases refractory to anti-TNF agents: cyclosporine plus vedolizumab. J Crohns Colitis. 2018;12(5):629. https://doi.org/10.1093/ecco-jcc/jjx179.
68. Kaplan GG, McCarthy EP, Ayanian JZ, Korzenik J, Hodin R, Sands BE. Impact of hospital volume on postoperative morbidity and mortality following a colectomy for ulcerative colitis. Gastroenterology. 2008;134(3):680-687. https://doi.org/10.1053/j.gastro.2008.01.004.
69. Spiegel BM, Ho W, Esrailian E, et al. Controversies in ulcerative colitis: a survey comparing decision making of experts versus community gastroenterologists. Clin Gastroenterol Hepatol. 2009;7(2):168-174. https://doi.org/10.1016/j.cgh.2008.08.029.
70. Ananthakrishnan AN, Issa M, Beaulieu DB, et al. History of medical hospitalization predicts future need for colectomy in patients with ulcerative colitis. Inflamm Bowel Dis. 2009;15(2):176-181. https://doi.org/10.1002/ibd.20639.
71. Nguyen GC, Murthy SK, Bressler B, et al. Quality of care and outcomes among hospitalized inflammatory bowel disease patients: a multicenter retrospective study. Inflamm Bowel Dis. 2017;23(5):695-701. https://doi.org/10.1097/MIB.0000000000001068.
72. Rotter T, Kugler J, Koch R, et al. A systematic review and meta-analysis of the effects of clinical pathways on length of stay, hospital costs, and patient outcomes. BMC Health Serv Res. 2008;8:265. https://doi.org/10.1186/1472-6963-8-265.
73. Peyrin-Biroulet L, Sandborn W, Sands BE, et al. Selecting therapeutic targets in inflammatory bowel disease (stride): determining therapeutic goals for treat-to-target. Am J Gastroenterol. 2015;110(9):1324-1338. https://doi.org/10.1038/ajg.2015.233.
1. Sands BE. Mount Sinai Expert Guides: Gastroenterology. Hoboken, NJ: John Wiley & Sons; 2014.
2. Dinesen LC, Walsh AJ, Protic MN, et al. The pattern and outcome of acute severe colitis. J Crohns Colitis. 2010;4(4):431-437. https://doi.org/10.1016/j.crohns.2010.02.001.
3. Edwards FC, Truelove SC. The course and prognosis of ulcerative colitis. Gut. 1963;4:299-315. https://doi.org/10.1136/gut.4.4.299.
4. Sonnenberg A, Chang J. Time trends of physician visits for Crohn’s disease and ulcerative colitis in the United States, 1960-2006. 2007;14(2):249-252. https://doi.org/10.1002/ibd.20273.
5. Nguyen GC, Tuskey A, Dassopoulos T, Harris ML, Brant SR. Rising hospitalization rates for inflammatory bowel disease in the United States between 1998 and 2004. Inflamm Bowel Dis. 2007;13(12):1529-1535. https://doi.org/10.1002/ibd.20250.
6. Truelove S, Witts L. Cortisone in ulcerative colitis. Br Med J. 1955;2:104-108.
7. Jakobovits SL, Travis S. Management of acute severe colitis. Br Med Bull. 2005;75(1):131-144. https://doi.org/10.1093/bmb/ldl001.
8. Lynch R, Lowe D, Protheroe A, Driscoll R, Rhodes J, Arnott I. Outcomes of rescue therapy in acute severe ulcerative colitis: data from the United Kingdom inflammatory bowel disease audit. Aliment Pharmacol Ther. 2013;38(8):935-945. https://doi.org/10.1111/apt.12473.
9. Magro F, Gionchetti P, Eliakim R, et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 1: definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileoanal pouch disorders. J Crohns Colitis. 2017;11(6):649-670. https://doi.org/10.1093/ecco-jcc/jjx008.
10. Kornbluth A, Sachar DB. Ulcerative colitis practice guidelines in adults: American college of gastroenterology, practice parameters committee. Am J Gastroenterol. 2010;105(3):501. https://doi.org/10.1038/ajg.2009.727.
11. Dassopoulos T, Cohen RD, Scherl EJ, Schwartz RM, Kosinski L, Regueiro MD. Ulcerative colitis care pathway. Gastroenterology. 2015;149(1):238-245. https://doi.org/10.1053/j.gastro.2015.05.036.
12. Ananthakrishnan AN, McGinley EL, Binion DG, Saeian K. A nationwide analysis of changes in severity and outcomes of inflammatory bowel disease hospitalizations. J Gastrointest Surg. 2011;15(2):267-276. https://doi.org/10.1007/s11605-010-1396-3.
13. Kelso M, Weideman RA, Cipher DJ, Feagins LA. Factors associated with length of stay in veterans with inflammatory bowel disease hospitalized for an acute flare. Inflamm Bowel Dis. 2017;24(1):5-11. https://doi.org/10.1093/ibd/izx020.
14. Murthy SK, Steinhart AH, Tinmouth J, Austin PC, Nguyen GC. Impact of gastroenterologist care on health outcomes of hospitalized ulcerative colitis patients. Gut. 2012;61(10):1410-1416. https://doi.org/10.1136/gutjnl-2011-301978.
15. Lee NS, Pola S, Groessl EJ, Rivera-Nieves J, Ho SB. Opportunities for improvement in the care of patients hospitalized for inflammatory bowel disease-related colitis. Dig Dis Sci. 2016;61(4):1003-1012. https://doi.org/10.1007/s10620-016-4046-0.
16. Neary BP, Doherty GA. A structured care pathway improves quality of care for acute severe ulcerative colitis. Gastroenterology. 2017;152(5):S218. https://doi.org/10.1016/S0016-5085(17)31028-4.
17. Klein A, Eliakim R. Nonsteroidal anti-inflammatory drugs and inflammatory bowel disease. Pharmaceuticals. 2010;3(4):1084-1092. https://doi.org/10.3390/ph3041084.
18. Chen JH, Andrews JM, Kariyawasam V, et al. Review article: acute severe ulcerative colitis - evidence-based consensus statements. Aliment Pharmacol Ther. 2016;44(2):127-144. https://doi.org/10.1111/apt.13670.
19. Vavricka SR, Schoepfer A, Scharl M, Lakatos PL, Navarini A, Rogler G. Extraintestinal manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2015;21(8):1982-1992. https://doi.org/10.1097/MIB.0000000000000392.
20. Solem CA, Loftus EV, Jr., Tremaine WJ, Harmsen WS, Zinsmeister AR, Sandborn WJ. Correlation of C-reactive protein with clinical, endoscopic, histologic, and radiographic activity in inflammatory bowel disease. Inflamm Bowel Dis. 2005;11(8):707-712. https://doi.org/10.1097/01.MIB.0000173271.18319.53.
21. Turner D, Walsh CM, Steinhart AH, Griffiths AM. Response to corticosteroids in severe ulcerative colitis: a systematic review of the literature and a meta-regression. Clin Gastroenterol Hepatol. 2007;5(1):103-110. https://doi.org/10.1016/j.cgh.2006.09.033.
22. Kaur M, Singapura P, Kalakota N, et al. Factors that contribute to indeterminate results from the QuantiFERON-TB Gold in-tube test in patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2018;16(10):1616-1621.e1. https://doi.org/10.1016/j.cgh.2017.11.038.
23. Bitton A, Buie D, Enns R, et al. Treatment of hospitalized adult patients with severe ulcerative colitis: Toronto consensus statements. Am J Gastroenterol. 2012;107(2):179-194. https://doi.org/10.1038/ajg.2011.386.
24. Feuerstein JD, Nguyen GC, Kupfer SS, Falck-Ytter Y, Singh S. American Gastroenterological Association Institute Clinical Guidelines committee. American Gastroenterological Association Institute Guideline on therapeutic drug monitoring in inflammatory bowel disease. Gastroenterology. 2017;153(3):827-834.
25. McDonald LC, Gerding DN, Johnson S, et al. Clinical Practice Guidelines for Clostridium difficile infection in adults and children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018;66(7):e1-e48. https://doi.org/10.1093/cid/cix1085.
26. Clayton EM, Rea MC, Shanahan F, et al. The vexed relationship between Clostridium difficile and inflammatory bowel disease: an assessment of carriage in an outpatient setting among patients in remission. Am J Gastroenterol. 2009;104(5):1162-1169. https://doi.org/10.1038/ajg.2009.4.
27. Nguyen GC, Kaplan GG, Harris ML, Brant SR. A national survey of the prevalence and impact of Clostridium difficile infection among hospitalized inflammatory bowel disease patients. Am J Gastroenterol. 2008;103(6):1443-1450. https://doi.org/10.1111/j.1572-0241.2007.01780.x.
28. Rahier J-F, Yazdanpanah Y, Colombel J-F, Travis S. The European (ECCO) Consensus on infection in IBD: what does it change for the clinician? Gut. 2009;58(10). https://doi.org/10.1136/gut.2008.175950.
29. Meyer AM, Ramzan NN, Loftus EV, Jr., Heigh RI, Leighton JA. The diagnostic yield of stool pathogen studies during relapses of inflammatory bowel disease. J Clin Gastroenterol. 2004;38(9):772-775. https://doi.org/10.1097/01.mcg.0000139057.05297.d6.
30. Chew C, Nolan D, Jewell D. Small bowel gas in severe ulcerative colitis. Gut. 1991;32(12):1535-1537. https://doi.org/10.1136/gut.32.12.1535.
31. Zakeri N, Pollok RC. Diagnostic imaging and radiation exposure in inflammatory bowel disease. World J Gastroenterol. 2016;22(7):2165-2178. https://doi.org/10.3748/wjg.v22.i7.2165.
32. Llaó J, Naves JE, Ruiz-Cerulla A, et al. Intravenous corticosteroids in moderately active ulcerative colitis refractory to oral corticosteroids. J Crohns Colitis. 2014;8(11):1523-1528. https://doi.org/10.1016/j.crohns.2014.06.010.
33. Seo M, Okada M, Yao T, Matake H, Maeda K. Evaluation of the clinical course of acute attacks in patients with ulcerative colitis through the use of an activity index. Journal of Gastroenterology. 2002;37(1):29-34. https://doi.org/10.1007/s535-002-8129-2.
34. Meyers S, Sachar DB, Goldberg JD, Janowitz HD. Corticotropin versus hydrocortisone in the intravenous treatment of ulcerative colitis: a prospective, randomized, double-blind clinical trial. Gastroenterology. 1983;85(2):351-357.
35. Ho G, Mowat C, Goddard C, et al. Predicting the outcome of severe ulcerative colitis: development of a novel risk score to aid early selection of patients for second‐line medical therapy or surgery. Aliment Pharmacol Ther. 2004;19(10):1079-1087. https://doi.org/10.1111/j.1365-2036.2004.01945.x.
36. Järnerot G, Rolny P, Sandberg-Gertzen H. Intensive intravenous treatment of ulcerative colitis. Gastroenterology. 1985;89(5):1005-1013. https://doi.org/10.1016/0016-5085(85)90201-X.
37. Wang JY, Terdiman JP, Vittinghoff E, Minichiello T, Varma MG. Hospitalized ulcerative colitis patients have an elevated risk of thromboembolic events. World J Gastroenterol. 2009;15(8):927-935. https://doi.org/10.3748/wjg.15.927.
38. Nguyen GC, Bernstein CN, Bitton A, et al. Consensus statements on the risk, prevention, and treatment of venous thromboembolism in inflammatory bowel disease: Canadian Association of Gastroenterology. Gastroenterology. 2014;146(3):835-848. https://doi.org/10.1053/j.gastro.2014.01.042.
39. Nguyen GC, Sam J. Rising prevalence of venous thromboembolism and its impact on mortality among hospitalized inflammatory bowel disease patients. Am J Gastroenterol. 2008;103(9):2272-2280. https://doi.org/10.1111/j.1572-0241.2008.02052.x.
40. Tinsley A, Naymagon S, Enomoto LM, Hollenbeak CS, Sands BE, Ullman TA. Rates of pharmacologic venous thromboembolism prophylaxis in hospitalized patients with active ulcerative colitis: results from a tertiary care center. J Crohns Colitis. 2013;7(12):e635-e640. https://doi.org/10.1016/j.crohns.2013.05.002.
41. Pleet JL, Vaughn BP, Morris JA, Moss AC, Cheifetz AS. The use of pharmacological prophylaxis against venous thromboembolism in hospitalized patients with severe active ulcerative colitis. Aliment Pharmacol Ther. 2014;39(9):940-948. https://doi.org/10.1111/apt.12691.
42. Gan SI, Beck PL. A new look at toxic megacolon: an update and review of incidence, etiology, pathogenesis, and management. Am J Gastroenterol. 2003;98(11):2363-2371 https://doi.org/10.1111/j.1572-0241.2003.07696.x.
43. Lichtenstein GR, Feagan BG, Cohen RD, et al. Serious infections and mortality in association with therapies for Crohn’s disease: TREAT registry. Clin Gastroenterol Hepatol. 2006;4(5):621-630. https://doi.org/10.1016/j.cgh.2006.03.002.
44. Docherty MJ, Jones III RCW, Wallace MS. Managing pain in inflammatory bowel disease. Gastroenterol Hepatol. 2011;7(9):592-601.
45. Singh S, Proudfoot JA, Dulai PS, et al. No benefit of concomitant 5-aminosalicylates in patients with ulcerative colitis escalated to biologic therapy: pooled analysis of individual participant data from clinical trials. Am J Gastroenterol. 2018;113(8):1197-1205. https://doi.org/10.1038/s41395-018-0144-2.
46. Mantzaris GJ, Hatzis A, Kontogiannis P, Triadaphyllou G. Intravenous tobramycin and metronidazole as an adjunct to corticosteroids in acute, severe ulcerative colitis. Am J Gastroenterol. 1994;89(1):43-46.
47. Mantzaris GJ, Petraki K, Archavlis E, et al. A prospective randomized controlled trial of intravenous ciprofloxacin as an adjunct to corticosteroids in acute, severe ulcerative colitis. Scand J Gastroenterol. 2001;36(9):971-974.
48. Rahier J-F, Magro F, Abreu C, et al. Second European evidence-based consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease. J Crohns Colitis. 2014;8(6):443-468. https://doi.org/10.1016/j.crohns.2013.12.013.
49. Dickinson RJ, Ashton MG, Axon AT, Smith RC, Yeung CK, Hill GL. Controlled trial of intravenous hyperalimentation and total bowel rest as an adjunct to the routine therapy of acute colitis. Gastroenterology. 1980;79(6):1199-1204.
50. McIntyre P, Powell-Tuck J, Wood S, et al. Controlled trial of bowel rest in the treatment of severe acute colitis. Gut. 1986;27(5):481-485. https://doi.org/10.1136/gut.27.5.481.
51. Travis SP, Farrant JM, Ricketts C, et al. Predicting outcome in severe ulcerative colitis. Gut. 1996;38(6):905-910. https://doi.org/10.1136/gut.38.6.905.
52. Bernardo S, Fernandes SR, Goncalves AR, et al. Predicting the course of disease in hospitalized patients with acute severe ulcerative colitis. Inflamm Bowel Dis. 2018;25(3):541-546. https://doi.org/10.1093/ibd/izy256.
53. Harbord M, Eliakim R, Bettenworth D, et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 2: current management. J Crohns Colitis. 2017;11(7):769-784. https://doi.org/10.1093/ecco-jcc/jjx009.
54. Randall J, Singh B, Warren B, Travis S, Mortensen N, George B. Delayed surgery for acute severe colitis is associated with increased risk of postoperative complications. Br J Surg. 2010;97(3):404-409. https://doi.org/10.1002/bjs.6874.
55. Bartels S, Gardenbroek T, Ubbink D, Buskens C, Tanis P, Bemelman W. Systematic review and meta‐analysis of laparoscopic versus open colectomy with end ileostomy for non‐toxic colitis. Br J Surg. 2013;100(6):726-733. https://doi.org/10.1002/bjs.9061.
56. Laharie D, Bourreille A, Branche J, et al. Ciclosporin versus infliximab in patients with severe ulcerative colitis refractory to intravenous steroids: a parallel, open-label randomized controlled trial. Lancet. 2012;380(9857):1909-1915. https://doi.org/10.1016/S0140-6736(12)61084-8.
57. Leblanc S, Allez M, Seksik P, et al. Successive treatment with cyclosporine and infliximab in steroid-refractory ulcerative colitis. Am J Gastroenterol. 2011;106(4):771-777. https://doi.org/10.1038/ajg.2011.62.
58. Narula N, Marshall JK, Colombel JF, et al. Systematic review and meta-analysis: infliximab or cyclosporine as rescue therapy in patients with severe ulcerative colitis refractory to steroids. Am J Gastroenterol. 2016;111(4):477-491. https://doi.org/10.1038/ajg.2016.7.
59. Feuerstein JD, Akbari M, Tapper EB, Cheifetz AS. Systematic review and meta-analysis of third-line salvage therapy with infliximab or cyclosporine in severe ulcerative colitis. Ann Gastroenterol. 2016;29(3):341-347. https://doi.org/10.20524/aog.2016.0032.
60. Brandse JF, Mathôt RA, van der Kleij D, et al. Pharmacokinetic features and presence of antidrug antibodies associated with response to infliximab induction therapy in patients with moderate to severe ulcerative colitis. Clin Gastroenterol Hepatol. 2016;14(2):251-258. https://doi.org/10.1016/j.cgh.2015.10.029.
61. Hindryckx P, Novak G, Vande Casteele N, et al. Review article: dose optimization of infliximab for acute severe ulcerative colitis. Aliment Pharmacol Ther. 2017;45(5):617-630. https://doi.org/10.1111/apt.13913.
62. Gibson DJ, Heetun ZS, Redmond CE, et al. An accelerated infliximab induction regimen reduces the need for early colectomy in patients with acute severe ulcerative colitis. Clin Gastroenterol Hepatol. 2015;13(2):330-335. https://doi.org/10.1016/j.cgh.2014.07.041.
63. Herfarth HH, Rogler G, Higgins PD. Pushing the pedal to the metal: should we accelerate infliximab therapy for patients with severe ulcerative colitis? Clin Gastroenterol Hepatol. 2015;13(2):336-338. https://doi.org/10.1016/j.cgh.2014.09.045.
64. Van Assche G, D’haens G, Noman M, et al. Randomized, double-blind comparison of 4 mg/kg versus 2 mg/kg intravenous cyclosporine in severe ulcerative colitis. Gastroenterology. 2003;125(4):1025-1031.
65. Arts J, D’haens G, Zeegers M, et al. Long-term outcome of treatment with intravenous cyclosporin in patients with severe ulcerative colitis. Inflamm Bowel Dis. 2004;10(2):73-78.
66. Tarabar D, El Jurdi K, Yvellez O, et al. 330-combination therapy of cyclosporine and vedolizumab is effective and safe for severe, steroid-resistant ulcerative colitis patients: a prospective study. Gastroenterology. 2018;154(6):S-82-S-83.https://doi.org/10.1016/S0016-5085(18)30725-X.
67. Szántó K, Molnár T, Farkas K. New promising combo therapy in inflammatory bowel diseases refractory to anti-TNF agents: cyclosporine plus vedolizumab. J Crohns Colitis. 2018;12(5):629. https://doi.org/10.1093/ecco-jcc/jjx179.
68. Kaplan GG, McCarthy EP, Ayanian JZ, Korzenik J, Hodin R, Sands BE. Impact of hospital volume on postoperative morbidity and mortality following a colectomy for ulcerative colitis. Gastroenterology. 2008;134(3):680-687. https://doi.org/10.1053/j.gastro.2008.01.004.
69. Spiegel BM, Ho W, Esrailian E, et al. Controversies in ulcerative colitis: a survey comparing decision making of experts versus community gastroenterologists. Clin Gastroenterol Hepatol. 2009;7(2):168-174. https://doi.org/10.1016/j.cgh.2008.08.029.
70. Ananthakrishnan AN, Issa M, Beaulieu DB, et al. History of medical hospitalization predicts future need for colectomy in patients with ulcerative colitis. Inflamm Bowel Dis. 2009;15(2):176-181. https://doi.org/10.1002/ibd.20639.
71. Nguyen GC, Murthy SK, Bressler B, et al. Quality of care and outcomes among hospitalized inflammatory bowel disease patients: a multicenter retrospective study. Inflamm Bowel Dis. 2017;23(5):695-701. https://doi.org/10.1097/MIB.0000000000001068.
72. Rotter T, Kugler J, Koch R, et al. A systematic review and meta-analysis of the effects of clinical pathways on length of stay, hospital costs, and patient outcomes. BMC Health Serv Res. 2008;8:265. https://doi.org/10.1186/1472-6963-8-265.
73. Peyrin-Biroulet L, Sandborn W, Sands BE, et al. Selecting therapeutic targets in inflammatory bowel disease (stride): determining therapeutic goals for treat-to-target. Am J Gastroenterol. 2015;110(9):1324-1338. https://doi.org/10.1038/ajg.2015.233.
© 2019 Society of Hospital Medicine