User login
ANSWER
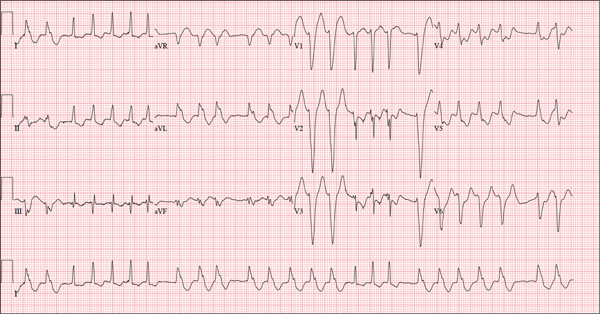
The correct interpretation of this ECG is atrial fibrillation with a rapid ventricular response and aberrantly conducted QRS complexes. The latter were misinterpreted as ventricular tachycardia. Although they represent a wide complex at a rate of more than 100 beats/min, the rhythm is irregular and the intrinsic (initial) inflection of normally conducted and aberrant beats is the same. (See lead I rhythm strip at bottom.)
What is unusual (and doesn’t make sense) regarding this ECG is the machine’s reading of the PR interval (128 ms) and the QRS duration (88 ms). For one thing, there is no measurable PR interval. And for another, the measured QRS duration accounts for the normally conducted complex and not the aberrantly conducted ones.
The technician was reassured, and the patient underwent successful cardioversion back to normal sinus rhythm.
ANSWER
The correct interpretation of this ECG is atrial fibrillation with a rapid ventricular response and aberrantly conducted QRS complexes. The latter were misinterpreted as ventricular tachycardia. Although they represent a wide complex at a rate of more than 100 beats/min, the rhythm is irregular and the intrinsic (initial) inflection of normally conducted and aberrant beats is the same. (See lead I rhythm strip at bottom.)
What is unusual (and doesn’t make sense) regarding this ECG is the machine’s reading of the PR interval (128 ms) and the QRS duration (88 ms). For one thing, there is no measurable PR interval. And for another, the measured QRS duration accounts for the normally conducted complex and not the aberrantly conducted ones.
The technician was reassured, and the patient underwent successful cardioversion back to normal sinus rhythm.
ANSWER
The correct interpretation of this ECG is atrial fibrillation with a rapid ventricular response and aberrantly conducted QRS complexes. The latter were misinterpreted as ventricular tachycardia. Although they represent a wide complex at a rate of more than 100 beats/min, the rhythm is irregular and the intrinsic (initial) inflection of normally conducted and aberrant beats is the same. (See lead I rhythm strip at bottom.)
What is unusual (and doesn’t make sense) regarding this ECG is the machine’s reading of the PR interval (128 ms) and the QRS duration (88 ms). For one thing, there is no measurable PR interval. And for another, the measured QRS duration accounts for the normally conducted complex and not the aberrantly conducted ones.
The technician was reassured, and the patient underwent successful cardioversion back to normal sinus rhythm.
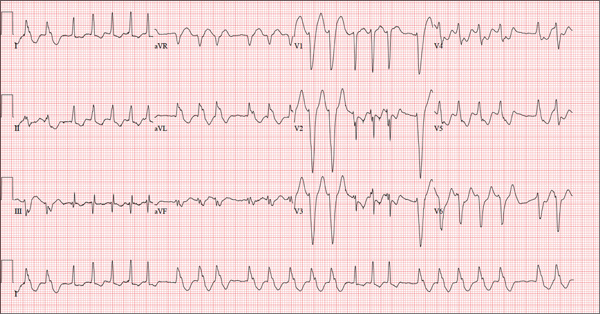
A 72-year-old woman with recurring palpitations and a rapid heart rate presents for evaluation stating that her heart started racing early yesterday morning. It began while she was sleeping, which is normal for her, but while the problem usually resolves within hours, this time it lasted longer. She had an MI about seven years ago, at which time she was told she had atrial fibrillation. Since then, she has had multiple episodes requiring cardioversion and suspects that is what is required this time. She has brought along a copy of her baseline ECG, which shows normal sinus rhythm, an old inferior MI, and an intraventricular conduction delay. Her history includes hypertension, hyperlipidemia, and diabetes. Surgical history is remarkable for coronary stenting (right coronary artery, first diagonal coronary artery, and an obtuse marginal coronary artery). She also has a remote history of hysterectomy and appendectomy. Her current medications include metoprolol, atorvastatin, amiodarone, metformin, and glyburide; she takes an OTC stool softener daily. She is allergic to sulfa. The patient, a retired schoolteacher and the matriarch of her church, is married and has two grown children. She has two siblings, both of whom have diabetes and hypertension. She smoked 1.5 packs of cigarettes per day until her MI, at which point she quit. She does not drink alcohol and has never used recreational drugs. Review of systems is positive for increasingly worsening eyesight, particularly halos around lights at night; she says she was told this might happen when she started taking amiodarone. She has intermittent episodes of diarrhea that she attributes to the stool softener, adding that she considers this consequence “better than the alternative.” The rest of the review is unremarkable. Vital signs include a blood pressure of 148/92 mm Hg; pulse, 140 beats/min and irregular; temperature, 98.4°F; and O2 saturation, 97% on room air. She is 64 in tall and weighs 169 lb. Physical exam reveals a very spry-appearing woman in no distress; in fact, she jokingly complains that she’s too young to have “old people’s diseases” and proudly points out that she has no symptoms of arthritis or dementia. She wears corrective lenses and hearing aids. The exam reveals no thyromegaly or jugular venous distention; clear lung fields; and an irregularly irregular heart rate of 146 beats/min. Her heart rate is too rapid to assess for murmurs or extra heart sounds. The abdomen is benign, and the patient has strong bilateral peripheral pulses in all extremities. The neurologic exam is intact. Suspecting that the patient is in atrial fibrillation, you ask the new ECG technician to obtain a reading. Five minutes later, he calls for help because “the patient is in ventricular tachycardia.” But when you walk into the room, the patient looks quite comfortable on the exam table and exhibits no distress. Reviewing the ECG, you note a ventricular rate of 152 beats/min; PR interval, 128 ms; QRS duration, 88 ms; QT/QTc interval, 280/445 ms; P axis, 27°; R axis, 23°; and T axis, 232°. What is your interpretation of this ECG—and what findings are inconsistent with the machine’s “interpretation”?