User login
When Robert Lee, MD, an internist affiliated with Iowa Health Physicians, a multi-specialty group in Des Moines, was called to the hospital to see one of his patients, he faced a 50-minute round trip plus additional time to find a parking place and catch an elevator before reaching the inpatient unit. In the time it took for him to see a couple of his patients in the hospital, he could have treated five patients in the office (1).
David McAtee, MD, an osteopath at Murdock Family Medicine, a group practice of eight family-care physicians in Port Charlotte, Florida, estimates its doctors were spending 30% of their time at the hospital caring for only 5% of their patients (2).
With an eye toward enhancing their office practices and offering patients efficient and effective inpatient treatment, both the Des Moines and Port Charlotte medical groups pursued a growing trend in the healthcare industry: they turned to hospitalists. Lee notes that the change allows him to enjoy a more normal lifestyle with his family and enhances his income (1). The Murdock group’s decision to contract with hospitalists in 2003 resulted in an expansion of office hours. With more available time, the group is in the process of developing a series of programs targeting various diseases as a means of educating patients in better self-care. Additionally, McAtee expresses the hope that medical malpractice insurance premiums will decrease as a result of less time spent on inpatient care (2).
Hospitalist Impact on Primary Care Physicians
Primary care physicians (PCPs) do have reservations regarding the involvement of hospitalists in the care of their patients. Some PCPs voice concerns about the potential reduction in income if they opt to use hospitalists. According to one estimate, primary care doctors may incur an average annual decrease in income of $25,000 by forgoing hospital rounds. However, studies indicate that PCPs have the potential to earn as much as $50,000 more by spending time in the office instead of seeing inpatients (3).
Hospitalist programs that offer on-site, 24-hour availability provide other benefits. When a crisis strikes, PCPs may be difficult to reach as they are seeing office patients. The hurricanes that hit Florida in September and October 2004 clearly demonstrated the value of having continuous inpatient care by qualified physicians already at the hospital. Treacherous weather conditions prevented PCPs from driving to the hospital to see their patients. Although the hospital was unable to perform lab tests, surgeries, or diagnostic imaging procedures because of power outages, hospitalists were already on site and stabilized patients with their basic clinical skills (3). Patients who may not have heard of the term “hospitalist” were pleased that a physician was available to answer questions, address unexpected medical issues, and offer immediate support and comfort.
Admittedly, not all PCPs have embraced the hospitalist model. The perception that they might lose skill and prestige by giving up inpatient visits might prevent them from utilizing hospitalist services. In some cases, PCPs might perceive a reduction in continuity of care. These concerns are valid and warrant consideration. However, a well run hospitalist program will keep communication lines open between hospitalists and PCPs, so that patients receive optimal care as both inpatients and outpatients.
Hospitalists and Surgeons/Specialists
Robert T. Trousdale, MD, orthopedic surgeon at the Mayo Clinic in Rochester, MN, spends most of his day in the operating room or evaluating patients for surgery. An expert in hip and knee surgery he admits that many orthopedic surgeons have insufficient knowledge when it comes to treating some of the common medical problems that may occur postoperatively “Hospitalists help us co-manage patients in this area. They bring an increased level of experience to the management of the patient,” he says. Trousdale notes the added benefits of time and hospitalist availability. “I am in the operating room for 5 hours at a time. If a nurse calls to report that one of my patients has developed post-op dizziness or chest pain, I might not be able to see him for 2 hours,” he says. Hospitalists have both the expertise and the availability to address medical issues in a timelier manner and expedite recovery time.
Additionally, Trousdale admits that, although he is quite familiar with the intricacies of the musculoskeletal system, he is less certain of the necessary tests a patient might need postoperatively. “We might take a ‘shotgun’ approach and order 15 expensive tests, which is an unnecessary use of the hospital’s resources,” he says (4).
Jeanne Huddleston, MD, Director of the Inpatient Internal Medicine Program at Mayo Clinic and Assistant Professor of Medicine at the Mayo College of Medicine, led a study to determine the impact hospitalists have on the co-management of patients having hip and knee surgery. The findings, published in 2004, reveal that of 526 patients in the study, more of those managed by hospitalist-orthopedic teams were discharged with no complications (61.6% for hospitalist-orthopedic teams vs. 48.8% for traditional orthopedic surgical teams). Only 30.2% of patients co-managed by hospitalists experienced minor complications, while 44.3% of patients managed by traditional orthopedic surgical teams had similar difficulties. Huddleston notes also that most orthopedic surgeons and nurses responding to a satisfaction survey preferred the hospitalist orthopedic model (5).
Hospitalists and Emergency Department Physicians
Brent R. Asplin, MD, MPH, research director in the department of emergency medicine at Regions Hospital in St. Paul, MN, cites three ways in which hospitalists positively impact the ED: through extraordinary availability, consistent and reliable care, and their focus on the hospital. “Hospitalists are available 24 hours a day,” he says. “It’s nice to know when you send a patient to the floor, there is an experienced physician in-house to take care of them. You do not have to try and reach a PCP on the phone.” He reports that capacity is a major problem for EDs. Bottlenecks result when there are patients who are ready to be admitted from the ED but must wait for other patients to be discharged. Hospitalists are always available to maintain a smooth patient flow and facilitate throughput, according to Asplin.
As a group, hospitalists adhere to a consistent approach to patient care. Once a patient is admitted, efficient, reliable in-house care will ensure a quick recovery and discharge. Asplin says, “Hospitalists are more likely to embrace clinical pathways for the most common clinical diagnoses. This reduces variability across the board and increases patient outcome and flow.” Also, hospitalists focus exclusively on inpatient care, enabling them to devote all their attention to servicing the patient while they are hospitalized without the distractions that might divert a PCP’s concentration. Asplin says, “Regarding clinical care, operations, and quality improvement, it helps to have a group dedicated and focused on the hospital” (6).
In teaching hospitals, residents also benefit from the presence of hospitalists. According to Barbara LeTourneau, MD, an ED physician and professional physician executive consultant also based at Regions, residents have the continuous supervision of experienced practitioners who can answer questions and teach on an ongoing basis. “With hospitalists there is much quicker and better patient care,” she says.
In her role as administrator, LeTourneau has an historical perspective on the delivery of inpatient care at her hospital. Prior to the implementation of hospital medicine programs, positive changes took a longer period of time to reach agreement and execution, she reports. “Having hospitalists here provides one group of experienced physicians who see a large percentage of patients,” says LeTourneau. Managing a significant caseload enables the hospitalist to understand the system in depth. “Hospitalists can provide good feedback and make it easier to implement necessary changes” (11).
Stakeholder Analysis
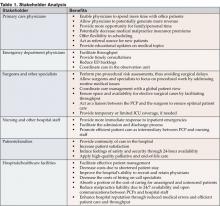
Studies reveal that hospitalists improve the practices of physicians and several subspecialties in a number of ways. Not only do PCPs benefit from the presence of hospitalists, but other medical specialists, patients, families, and medical facilities gain advantages as well (see Table 1).
Research Studies
Since 1996 when the term hospitalist was first used, a number of studies have been conducted to evaluate the benefits they bring to PCPs and other physicians (see Table 2). In the past decade, the number of hospitalists has increased dramatically, lending credence to their value in an inpatient medical setting. In 2005, the Society of Hospital Medicine (SHM) estimates that there are 12,000 hospitalists in the US.
In a survey by Mitretek Healthcare, researchers asked hospital leaders to rate a number of strategies that impact on hospital-medical staff relations. Sixty-two percent of the leaders surveyed gave hospitalist programs a high rating pertaining to hospital-physician alignment (12). Other studies also support the growing belief that hospitalists can effectively and efficiently enhance physician practices.
Conclusion
Joseph Li, MD, director of the hospitalist program at Beth Israel Deaconess Medical Center in Boston, hopes to build a career based on the belief that hospitalists are leading the way in “preventing medical errors and hospital-acquired infections, managing the complex hospital environment, finding the right transition to home care or rehabilitation, and providing palliative and end-of-life care” (13). As hospital medicine programs become more prevalent and accepted, more and more PCPs are seeing the value in their presence. A major national hospitalist management company surveyed PCPs in five markets on their experiences with hospitalists. The responses revealed a 100% satisfaction rating on the quality of inpatient care (14). In the future, hospitalists like Li will strive to maintain that rating while they help improve physician practices and enhance patient care.
Dr. Kealey can be contacted at burke.tkealey@healthpartners.com
Dr. Vidrine can be contacted at larry_vidrine@teamhealth.com
References
- Jackson C. Doctors find hospitalists save time, money: primary care physicians are seeing that turning over their hospital business allows them to make more income. Amednews.com, February 19, 2001.
- Trendy hospital medicine comes to Charlotte. Sunherald.com, February 13, 2004.
- Landro L. Medicine’s fastest-growing specialty: hospital-bound doctors take the place of your physician; effort to reduce costs, errors. The Wall Street Journal Online, October 6, 2004.
- Trousdale RT, Department of Orthopedics, Mayo Clinic, Rochester, MN. Telephone interview. January 3, 2005.
- Huddleston J, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized controlled trial. Ann Intern Med. 2004;141:28-38.
- Asplin, Brent R., MD, MPH, research director, Department of Emergency Medicine, Regions Hospital, St. Paul, MN. Telephone interview January 5, 2005.
- Auerbach AD, Aronson MD, Davis RB, Phillips RS. How physicians perceive hospitalist services after implementation: anticipation vs. reality. Arch Intern Med. 2003;163:2330-6.
- Auerbach AD, Nelson EA, Lindenauer PK, et al. Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey. Am J Med. 2000;109: 648-53.
- Halpert AP, Pearson SD, LeWine HE, McKean SC. The impact of an inpatient physician program on quality utilization, and satisfaction. Am J Manag Care. 2000; 6: 549-55.
- Fernandez A, Grumbach K, Goitein L, et al. Friend or foe? How primary care physicians perceive hospitalists. Arch Intern Med. 2000;160:2902-8.
- LeTourneau B, emergency department physician, professional physician executive consultant, Regions Hospital, St. Paul, MN. Telephone interview. January 7, 2005.
- McGowan RA. Strengthening hospital-physician relationships. Healthcare Financial Management Association. December 2004. www.hfma.org/publications/HFM_Magazine/business.htm.
- Barnard A. Medical profession, patients have warmed to the ‘hospitalist’. The Boston Globe, January 30, 2002.
- PCPs and hospitalists: a new attitude? Cogent Quarterly, Vol. 1, No. 4, Fall 2001.
When Robert Lee, MD, an internist affiliated with Iowa Health Physicians, a multi-specialty group in Des Moines, was called to the hospital to see one of his patients, he faced a 50-minute round trip plus additional time to find a parking place and catch an elevator before reaching the inpatient unit. In the time it took for him to see a couple of his patients in the hospital, he could have treated five patients in the office (1).
David McAtee, MD, an osteopath at Murdock Family Medicine, a group practice of eight family-care physicians in Port Charlotte, Florida, estimates its doctors were spending 30% of their time at the hospital caring for only 5% of their patients (2).
With an eye toward enhancing their office practices and offering patients efficient and effective inpatient treatment, both the Des Moines and Port Charlotte medical groups pursued a growing trend in the healthcare industry: they turned to hospitalists. Lee notes that the change allows him to enjoy a more normal lifestyle with his family and enhances his income (1). The Murdock group’s decision to contract with hospitalists in 2003 resulted in an expansion of office hours. With more available time, the group is in the process of developing a series of programs targeting various diseases as a means of educating patients in better self-care. Additionally, McAtee expresses the hope that medical malpractice insurance premiums will decrease as a result of less time spent on inpatient care (2).
Hospitalist Impact on Primary Care Physicians
Primary care physicians (PCPs) do have reservations regarding the involvement of hospitalists in the care of their patients. Some PCPs voice concerns about the potential reduction in income if they opt to use hospitalists. According to one estimate, primary care doctors may incur an average annual decrease in income of $25,000 by forgoing hospital rounds. However, studies indicate that PCPs have the potential to earn as much as $50,000 more by spending time in the office instead of seeing inpatients (3).
Hospitalist programs that offer on-site, 24-hour availability provide other benefits. When a crisis strikes, PCPs may be difficult to reach as they are seeing office patients. The hurricanes that hit Florida in September and October 2004 clearly demonstrated the value of having continuous inpatient care by qualified physicians already at the hospital. Treacherous weather conditions prevented PCPs from driving to the hospital to see their patients. Although the hospital was unable to perform lab tests, surgeries, or diagnostic imaging procedures because of power outages, hospitalists were already on site and stabilized patients with their basic clinical skills (3). Patients who may not have heard of the term “hospitalist” were pleased that a physician was available to answer questions, address unexpected medical issues, and offer immediate support and comfort.
Admittedly, not all PCPs have embraced the hospitalist model. The perception that they might lose skill and prestige by giving up inpatient visits might prevent them from utilizing hospitalist services. In some cases, PCPs might perceive a reduction in continuity of care. These concerns are valid and warrant consideration. However, a well run hospitalist program will keep communication lines open between hospitalists and PCPs, so that patients receive optimal care as both inpatients and outpatients.
Hospitalists and Surgeons/Specialists
Robert T. Trousdale, MD, orthopedic surgeon at the Mayo Clinic in Rochester, MN, spends most of his day in the operating room or evaluating patients for surgery. An expert in hip and knee surgery he admits that many orthopedic surgeons have insufficient knowledge when it comes to treating some of the common medical problems that may occur postoperatively “Hospitalists help us co-manage patients in this area. They bring an increased level of experience to the management of the patient,” he says. Trousdale notes the added benefits of time and hospitalist availability. “I am in the operating room for 5 hours at a time. If a nurse calls to report that one of my patients has developed post-op dizziness or chest pain, I might not be able to see him for 2 hours,” he says. Hospitalists have both the expertise and the availability to address medical issues in a timelier manner and expedite recovery time.
Additionally, Trousdale admits that, although he is quite familiar with the intricacies of the musculoskeletal system, he is less certain of the necessary tests a patient might need postoperatively. “We might take a ‘shotgun’ approach and order 15 expensive tests, which is an unnecessary use of the hospital’s resources,” he says (4).
Jeanne Huddleston, MD, Director of the Inpatient Internal Medicine Program at Mayo Clinic and Assistant Professor of Medicine at the Mayo College of Medicine, led a study to determine the impact hospitalists have on the co-management of patients having hip and knee surgery. The findings, published in 2004, reveal that of 526 patients in the study, more of those managed by hospitalist-orthopedic teams were discharged with no complications (61.6% for hospitalist-orthopedic teams vs. 48.8% for traditional orthopedic surgical teams). Only 30.2% of patients co-managed by hospitalists experienced minor complications, while 44.3% of patients managed by traditional orthopedic surgical teams had similar difficulties. Huddleston notes also that most orthopedic surgeons and nurses responding to a satisfaction survey preferred the hospitalist orthopedic model (5).
Hospitalists and Emergency Department Physicians
Brent R. Asplin, MD, MPH, research director in the department of emergency medicine at Regions Hospital in St. Paul, MN, cites three ways in which hospitalists positively impact the ED: through extraordinary availability, consistent and reliable care, and their focus on the hospital. “Hospitalists are available 24 hours a day,” he says. “It’s nice to know when you send a patient to the floor, there is an experienced physician in-house to take care of them. You do not have to try and reach a PCP on the phone.” He reports that capacity is a major problem for EDs. Bottlenecks result when there are patients who are ready to be admitted from the ED but must wait for other patients to be discharged. Hospitalists are always available to maintain a smooth patient flow and facilitate throughput, according to Asplin.
As a group, hospitalists adhere to a consistent approach to patient care. Once a patient is admitted, efficient, reliable in-house care will ensure a quick recovery and discharge. Asplin says, “Hospitalists are more likely to embrace clinical pathways for the most common clinical diagnoses. This reduces variability across the board and increases patient outcome and flow.” Also, hospitalists focus exclusively on inpatient care, enabling them to devote all their attention to servicing the patient while they are hospitalized without the distractions that might divert a PCP’s concentration. Asplin says, “Regarding clinical care, operations, and quality improvement, it helps to have a group dedicated and focused on the hospital” (6).
In teaching hospitals, residents also benefit from the presence of hospitalists. According to Barbara LeTourneau, MD, an ED physician and professional physician executive consultant also based at Regions, residents have the continuous supervision of experienced practitioners who can answer questions and teach on an ongoing basis. “With hospitalists there is much quicker and better patient care,” she says.
In her role as administrator, LeTourneau has an historical perspective on the delivery of inpatient care at her hospital. Prior to the implementation of hospital medicine programs, positive changes took a longer period of time to reach agreement and execution, she reports. “Having hospitalists here provides one group of experienced physicians who see a large percentage of patients,” says LeTourneau. Managing a significant caseload enables the hospitalist to understand the system in depth. “Hospitalists can provide good feedback and make it easier to implement necessary changes” (11).
Stakeholder Analysis
Studies reveal that hospitalists improve the practices of physicians and several subspecialties in a number of ways. Not only do PCPs benefit from the presence of hospitalists, but other medical specialists, patients, families, and medical facilities gain advantages as well (see Table 1).
Research Studies
Since 1996 when the term hospitalist was first used, a number of studies have been conducted to evaluate the benefits they bring to PCPs and other physicians (see Table 2). In the past decade, the number of hospitalists has increased dramatically, lending credence to their value in an inpatient medical setting. In 2005, the Society of Hospital Medicine (SHM) estimates that there are 12,000 hospitalists in the US.
In a survey by Mitretek Healthcare, researchers asked hospital leaders to rate a number of strategies that impact on hospital-medical staff relations. Sixty-two percent of the leaders surveyed gave hospitalist programs a high rating pertaining to hospital-physician alignment (12). Other studies also support the growing belief that hospitalists can effectively and efficiently enhance physician practices.
Conclusion
Joseph Li, MD, director of the hospitalist program at Beth Israel Deaconess Medical Center in Boston, hopes to build a career based on the belief that hospitalists are leading the way in “preventing medical errors and hospital-acquired infections, managing the complex hospital environment, finding the right transition to home care or rehabilitation, and providing palliative and end-of-life care” (13). As hospital medicine programs become more prevalent and accepted, more and more PCPs are seeing the value in their presence. A major national hospitalist management company surveyed PCPs in five markets on their experiences with hospitalists. The responses revealed a 100% satisfaction rating on the quality of inpatient care (14). In the future, hospitalists like Li will strive to maintain that rating while they help improve physician practices and enhance patient care.
Dr. Kealey can be contacted at burke.tkealey@healthpartners.com
Dr. Vidrine can be contacted at larry_vidrine@teamhealth.com
References
- Jackson C. Doctors find hospitalists save time, money: primary care physicians are seeing that turning over their hospital business allows them to make more income. Amednews.com, February 19, 2001.
- Trendy hospital medicine comes to Charlotte. Sunherald.com, February 13, 2004.
- Landro L. Medicine’s fastest-growing specialty: hospital-bound doctors take the place of your physician; effort to reduce costs, errors. The Wall Street Journal Online, October 6, 2004.
- Trousdale RT, Department of Orthopedics, Mayo Clinic, Rochester, MN. Telephone interview. January 3, 2005.
- Huddleston J, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized controlled trial. Ann Intern Med. 2004;141:28-38.
- Asplin, Brent R., MD, MPH, research director, Department of Emergency Medicine, Regions Hospital, St. Paul, MN. Telephone interview January 5, 2005.
- Auerbach AD, Aronson MD, Davis RB, Phillips RS. How physicians perceive hospitalist services after implementation: anticipation vs. reality. Arch Intern Med. 2003;163:2330-6.
- Auerbach AD, Nelson EA, Lindenauer PK, et al. Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey. Am J Med. 2000;109: 648-53.
- Halpert AP, Pearson SD, LeWine HE, McKean SC. The impact of an inpatient physician program on quality utilization, and satisfaction. Am J Manag Care. 2000; 6: 549-55.
- Fernandez A, Grumbach K, Goitein L, et al. Friend or foe? How primary care physicians perceive hospitalists. Arch Intern Med. 2000;160:2902-8.
- LeTourneau B, emergency department physician, professional physician executive consultant, Regions Hospital, St. Paul, MN. Telephone interview. January 7, 2005.
- McGowan RA. Strengthening hospital-physician relationships. Healthcare Financial Management Association. December 2004. www.hfma.org/publications/HFM_Magazine/business.htm.
- Barnard A. Medical profession, patients have warmed to the ‘hospitalist’. The Boston Globe, January 30, 2002.
- PCPs and hospitalists: a new attitude? Cogent Quarterly, Vol. 1, No. 4, Fall 2001.
When Robert Lee, MD, an internist affiliated with Iowa Health Physicians, a multi-specialty group in Des Moines, was called to the hospital to see one of his patients, he faced a 50-minute round trip plus additional time to find a parking place and catch an elevator before reaching the inpatient unit. In the time it took for him to see a couple of his patients in the hospital, he could have treated five patients in the office (1).
David McAtee, MD, an osteopath at Murdock Family Medicine, a group practice of eight family-care physicians in Port Charlotte, Florida, estimates its doctors were spending 30% of their time at the hospital caring for only 5% of their patients (2).
With an eye toward enhancing their office practices and offering patients efficient and effective inpatient treatment, both the Des Moines and Port Charlotte medical groups pursued a growing trend in the healthcare industry: they turned to hospitalists. Lee notes that the change allows him to enjoy a more normal lifestyle with his family and enhances his income (1). The Murdock group’s decision to contract with hospitalists in 2003 resulted in an expansion of office hours. With more available time, the group is in the process of developing a series of programs targeting various diseases as a means of educating patients in better self-care. Additionally, McAtee expresses the hope that medical malpractice insurance premiums will decrease as a result of less time spent on inpatient care (2).
Hospitalist Impact on Primary Care Physicians
Primary care physicians (PCPs) do have reservations regarding the involvement of hospitalists in the care of their patients. Some PCPs voice concerns about the potential reduction in income if they opt to use hospitalists. According to one estimate, primary care doctors may incur an average annual decrease in income of $25,000 by forgoing hospital rounds. However, studies indicate that PCPs have the potential to earn as much as $50,000 more by spending time in the office instead of seeing inpatients (3).
Hospitalist programs that offer on-site, 24-hour availability provide other benefits. When a crisis strikes, PCPs may be difficult to reach as they are seeing office patients. The hurricanes that hit Florida in September and October 2004 clearly demonstrated the value of having continuous inpatient care by qualified physicians already at the hospital. Treacherous weather conditions prevented PCPs from driving to the hospital to see their patients. Although the hospital was unable to perform lab tests, surgeries, or diagnostic imaging procedures because of power outages, hospitalists were already on site and stabilized patients with their basic clinical skills (3). Patients who may not have heard of the term “hospitalist” were pleased that a physician was available to answer questions, address unexpected medical issues, and offer immediate support and comfort.
Admittedly, not all PCPs have embraced the hospitalist model. The perception that they might lose skill and prestige by giving up inpatient visits might prevent them from utilizing hospitalist services. In some cases, PCPs might perceive a reduction in continuity of care. These concerns are valid and warrant consideration. However, a well run hospitalist program will keep communication lines open between hospitalists and PCPs, so that patients receive optimal care as both inpatients and outpatients.
Hospitalists and Surgeons/Specialists
Robert T. Trousdale, MD, orthopedic surgeon at the Mayo Clinic in Rochester, MN, spends most of his day in the operating room or evaluating patients for surgery. An expert in hip and knee surgery he admits that many orthopedic surgeons have insufficient knowledge when it comes to treating some of the common medical problems that may occur postoperatively “Hospitalists help us co-manage patients in this area. They bring an increased level of experience to the management of the patient,” he says. Trousdale notes the added benefits of time and hospitalist availability. “I am in the operating room for 5 hours at a time. If a nurse calls to report that one of my patients has developed post-op dizziness or chest pain, I might not be able to see him for 2 hours,” he says. Hospitalists have both the expertise and the availability to address medical issues in a timelier manner and expedite recovery time.
Additionally, Trousdale admits that, although he is quite familiar with the intricacies of the musculoskeletal system, he is less certain of the necessary tests a patient might need postoperatively. “We might take a ‘shotgun’ approach and order 15 expensive tests, which is an unnecessary use of the hospital’s resources,” he says (4).
Jeanne Huddleston, MD, Director of the Inpatient Internal Medicine Program at Mayo Clinic and Assistant Professor of Medicine at the Mayo College of Medicine, led a study to determine the impact hospitalists have on the co-management of patients having hip and knee surgery. The findings, published in 2004, reveal that of 526 patients in the study, more of those managed by hospitalist-orthopedic teams were discharged with no complications (61.6% for hospitalist-orthopedic teams vs. 48.8% for traditional orthopedic surgical teams). Only 30.2% of patients co-managed by hospitalists experienced minor complications, while 44.3% of patients managed by traditional orthopedic surgical teams had similar difficulties. Huddleston notes also that most orthopedic surgeons and nurses responding to a satisfaction survey preferred the hospitalist orthopedic model (5).
Hospitalists and Emergency Department Physicians
Brent R. Asplin, MD, MPH, research director in the department of emergency medicine at Regions Hospital in St. Paul, MN, cites three ways in which hospitalists positively impact the ED: through extraordinary availability, consistent and reliable care, and their focus on the hospital. “Hospitalists are available 24 hours a day,” he says. “It’s nice to know when you send a patient to the floor, there is an experienced physician in-house to take care of them. You do not have to try and reach a PCP on the phone.” He reports that capacity is a major problem for EDs. Bottlenecks result when there are patients who are ready to be admitted from the ED but must wait for other patients to be discharged. Hospitalists are always available to maintain a smooth patient flow and facilitate throughput, according to Asplin.
As a group, hospitalists adhere to a consistent approach to patient care. Once a patient is admitted, efficient, reliable in-house care will ensure a quick recovery and discharge. Asplin says, “Hospitalists are more likely to embrace clinical pathways for the most common clinical diagnoses. This reduces variability across the board and increases patient outcome and flow.” Also, hospitalists focus exclusively on inpatient care, enabling them to devote all their attention to servicing the patient while they are hospitalized without the distractions that might divert a PCP’s concentration. Asplin says, “Regarding clinical care, operations, and quality improvement, it helps to have a group dedicated and focused on the hospital” (6).
In teaching hospitals, residents also benefit from the presence of hospitalists. According to Barbara LeTourneau, MD, an ED physician and professional physician executive consultant also based at Regions, residents have the continuous supervision of experienced practitioners who can answer questions and teach on an ongoing basis. “With hospitalists there is much quicker and better patient care,” she says.
In her role as administrator, LeTourneau has an historical perspective on the delivery of inpatient care at her hospital. Prior to the implementation of hospital medicine programs, positive changes took a longer period of time to reach agreement and execution, she reports. “Having hospitalists here provides one group of experienced physicians who see a large percentage of patients,” says LeTourneau. Managing a significant caseload enables the hospitalist to understand the system in depth. “Hospitalists can provide good feedback and make it easier to implement necessary changes” (11).
Stakeholder Analysis
Studies reveal that hospitalists improve the practices of physicians and several subspecialties in a number of ways. Not only do PCPs benefit from the presence of hospitalists, but other medical specialists, patients, families, and medical facilities gain advantages as well (see Table 1).
Research Studies
Since 1996 when the term hospitalist was first used, a number of studies have been conducted to evaluate the benefits they bring to PCPs and other physicians (see Table 2). In the past decade, the number of hospitalists has increased dramatically, lending credence to their value in an inpatient medical setting. In 2005, the Society of Hospital Medicine (SHM) estimates that there are 12,000 hospitalists in the US.
In a survey by Mitretek Healthcare, researchers asked hospital leaders to rate a number of strategies that impact on hospital-medical staff relations. Sixty-two percent of the leaders surveyed gave hospitalist programs a high rating pertaining to hospital-physician alignment (12). Other studies also support the growing belief that hospitalists can effectively and efficiently enhance physician practices.
Conclusion
Joseph Li, MD, director of the hospitalist program at Beth Israel Deaconess Medical Center in Boston, hopes to build a career based on the belief that hospitalists are leading the way in “preventing medical errors and hospital-acquired infections, managing the complex hospital environment, finding the right transition to home care or rehabilitation, and providing palliative and end-of-life care” (13). As hospital medicine programs become more prevalent and accepted, more and more PCPs are seeing the value in their presence. A major national hospitalist management company surveyed PCPs in five markets on their experiences with hospitalists. The responses revealed a 100% satisfaction rating on the quality of inpatient care (14). In the future, hospitalists like Li will strive to maintain that rating while they help improve physician practices and enhance patient care.
Dr. Kealey can be contacted at burke.tkealey@healthpartners.com
Dr. Vidrine can be contacted at larry_vidrine@teamhealth.com
References
- Jackson C. Doctors find hospitalists save time, money: primary care physicians are seeing that turning over their hospital business allows them to make more income. Amednews.com, February 19, 2001.
- Trendy hospital medicine comes to Charlotte. Sunherald.com, February 13, 2004.
- Landro L. Medicine’s fastest-growing specialty: hospital-bound doctors take the place of your physician; effort to reduce costs, errors. The Wall Street Journal Online, October 6, 2004.
- Trousdale RT, Department of Orthopedics, Mayo Clinic, Rochester, MN. Telephone interview. January 3, 2005.
- Huddleston J, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized controlled trial. Ann Intern Med. 2004;141:28-38.
- Asplin, Brent R., MD, MPH, research director, Department of Emergency Medicine, Regions Hospital, St. Paul, MN. Telephone interview January 5, 2005.
- Auerbach AD, Aronson MD, Davis RB, Phillips RS. How physicians perceive hospitalist services after implementation: anticipation vs. reality. Arch Intern Med. 2003;163:2330-6.
- Auerbach AD, Nelson EA, Lindenauer PK, et al. Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey. Am J Med. 2000;109: 648-53.
- Halpert AP, Pearson SD, LeWine HE, McKean SC. The impact of an inpatient physician program on quality utilization, and satisfaction. Am J Manag Care. 2000; 6: 549-55.
- Fernandez A, Grumbach K, Goitein L, et al. Friend or foe? How primary care physicians perceive hospitalists. Arch Intern Med. 2000;160:2902-8.
- LeTourneau B, emergency department physician, professional physician executive consultant, Regions Hospital, St. Paul, MN. Telephone interview. January 7, 2005.
- McGowan RA. Strengthening hospital-physician relationships. Healthcare Financial Management Association. December 2004. www.hfma.org/publications/HFM_Magazine/business.htm.
- Barnard A. Medical profession, patients have warmed to the ‘hospitalist’. The Boston Globe, January 30, 2002.
- PCPs and hospitalists: a new attitude? Cogent Quarterly, Vol. 1, No. 4, Fall 2001.