User login
Maximizing Throughput and Improving Patient Flow
According to data from the American Hospital Association (1), in 1985, the United States had 5732 operational community hospitals; by 2002, the latest year for which figures are available, the number had decreased to 4927, a loss of approximately 14% (1). In that same timeframe, these hospitals lost approximately 18% of their beds, dropping from just over 1 million to 820,653 beds. This reduction in bed capacity has been accompanied by hospital cost-cutting efforts, staff downsizing, and elimination of services. Many explanations for these trends have been suggested, including changes in Medicare reimbursement and the growth of managed care organizations (MCOs).
However, as the current baby boom generation ages, rising inpatient demands are presenting hospitals with significant challenges. According to a 2001 report from Solucient (2), who maintains the nation’s largest health care database, the senior population—individuals age 65 and older—are projected to experience an 85% growth rate over the next two decades. Since this age group utilizes inpatient services 4.5 times more than younger populations, the number of admissions and beds to accommodate those cases will soar. By the year 2027, hospitals can anticipate a 46% rise in demand for acute inpatient beds as admissions escalate by approximately 13 million cases. Currently, the nation’s healthcare facilities admit 31 million cases; this number will jump to more than 44 million, representing a 41% growth from present admissions figures. For hospitals that maintain an 80% census rate, an additional 238,000 beds will be needed to meet demands (1).
Adding to this increase in demand and pressure on bed capacity, hospitals must address the requirements of the Emergency Medical Treatment and Active Labor Act (EMTALA) passed by the US Congress in 1986 as part of the Consolidated Omnibus Reconciliation Act (COBRA). The law’s initial intent was to ensure patient access to emergency medical care and to prevent the practice of patient dumping, in which uninsured patients were transferred, solely for financial reasons, from private to public hospitals without consideration of their medical condition or stability for the transfer (3). EMTALA mandates that hospitals rank the severity of patients. Thus, tertiary referral centers are required to admit the sickest patients first. This directive presents a significant challenge to many healthcare facilities. High census rates prohibit the admission of elective surgical cases, which, although profitable, are considered second tier. Routine medical cases or complicated emergency surgical cases have the potential to adversely affect the institution’s financial performance.
In addition to the challenge of increased bed demands and EMTALA, hospitals also cite an increasingly smaller number of on-site community physicians. Longstanding trends from inpatient to outpatient care have prompted many community physicians to concentrate their efforts on serving the needs of office-based patients, limiting their accessibility to hospital cases.
To address these pressures, hospitals must execute innovative strategies that deliver efficient throughput and enhance revenue, while still preserving high-quality services. Since 1996, hospital medicine programs have demonstrated a positive impact on the healthcare facility’s ability to increase overall productivity and profitability and still maintain high quality Patients today present to the doctor sicker than in the past and require more careful and frequent outpatient care. Since hospitalists operate solely on an inpatient basis, their availability to efficiently admit and manage hospitalized patients enables delivery of quality care that expedites appropriate treatment and shortens length of stay.
Two Roles of the Hospitalist
According to the Society of Hospital Medicine (SHM), “Hospitalists are physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to hospital medicine.” Coined by Drs. Robert Wachter and Lee Goldman in 1996 (4), the term implies an additional point of emphasis. Part of a new paradigm in clinical care, the hospitalist enhances the processes of care surrounding patients and adopts an attitude of accountability for that care. In practice, hospitalists play two key roles.
Primarily, the hospitalist is a practicing clinician — managing throughput on a case-by-case, patient-by-patient basis. In addition, a hospitalist performs a non-clinical role as an “inpatient expert,” taking the lead in creating system changes and communicating those changes to other hospital personnel as well as to community physicians. As an inpatient expert, hospitalists are often asked to lead organization-wide throughput initiatives to identify and implement strategies to facilitate patient flow and efficiency. As dedicated members of multi-disciplinary in-house teams, the hospitalist is in a prime position to foster change and improve systems.
Throughput as Continuum of Care
As suggested by Heffner (5), the process of admission, hospitalization, and discharge resembles a “bell-shaped curve.” To achieve effective throughput, hospitals must expedite patient care and also maintain careful oversight throughout a patient’s entire hospital stay. The hospitalist, as an integral part of a multidisciplinary team, coordinates care to promote a positive outcome and shorten length of stay. Drawing on strong leadership qualities, as well as on intimate knowledge of hospital procedures, layout design and infrastructure, and available community resources, the hospitalist plays a pivotal role in creating efficient throughput from admission to discharge.
Emergency Department
At the front end of the bell-shaped curve, the hospitalist may be engaged by emergency department (ED) physicians to assist in ensuring smooth patient flow and, more important, identifies the “intensity of service” needed. Through the use of clinical criteria, such as lnterQual, the hospitalist, together with the ED physician, may be asked to quantitatively rate the patient’s illness for degree of severity.
Timely patient evaluation helps prevent a backlog of ED cases and enables more patients to be seen. Immediate attention to and initiation of appropriate therapy guarantees a better outcome while minimizing the potential risk for complications, which could possibly lead to longer inpatient stays.
Inpatient Unit
Once a patient has been admitted to an inpatient unit, the hospitalist, together with a multidisciplinary team, facilitates care and determines the inpatient services that will optimize patient recovery through strong interdepartmental communications. Working together with admissions, medical records, nursing, laboratory and diagnostic services, information technology and other pertinent departments, the hospitalist maintains a pulse on all activity surrounding the patient and his care.
Judicious inpatient consultations and treatment decisions result in timely changes in therapy, potentially reducing the length of stay. The frequency with which the hospitalist sees the patient allows him to monitor any changes in condition and reduce possible decompensation, a practice known as vertical continuity (6). Such careful attention may reduce inpatient length of stay significantly. When aggressive management is mandated, the presence of the hospitalist enables initiation of effective therapy and results in quicker discharge and a reduction in potential readmission (7).
Surgery
The surgeon and hospitalist are ideally suited to work together in managing a surgical patient. The hospitalist focuses on the peri-operative management of medical issues and risk reduction, which allows the surgeon to concentrate more on surgical indications and the surgery itself. The hospitalist’s role in the management of a surgical patient enables vertical continuity when the surgeon may be occupied in the operating room with another patient as documented by Huddleston’s Hospitalist Orthopedic Team (HOT) approach (8).
Intensive Care Unit (ICU)
In many hospitals, particularly those that do not have intensivists, hospitalists are able to provide quality care to patients. Even in hospitals where intensivists manage ICU patients, hospitalists work together with the intensivist to ensure smoother transition into and out of the unit.
Discharge
Timing is a critical issue with regard to discharge. Since the hospitalist operates solely in-house and in collaboration with a multidisciplinary team, he is able to round early in the day to discharge patients by mid- or late-morning, freeing a bed for a new patient. In some cases, the hospitalist, in anticipation of early discharge, may begin pre-planning the day prior to discharge, which further expedites the process. Early discharge applies to the ICU, step-down areas and general inpatient care areas, as well as to full discharge from the healthcare facility. Moving a patient from one of these areas enables other patients to fill those empty beds thus optimizing throughput.
Having managed the patient throughout his hospital stay, the hospitalist — again working together with a multidisciplinary team —can facilitate arrangements to send the patient home or to a rehabilitation or skilled nursing facility or alternative housing situation upon discharge, as well as coordinating post-discharge care, whether it be arranging for a visiting nursing or social services or communicating with the primary care physician regarding follow-up appointments. If additional outpatient care is prescribed, the hospitalist will work with the discharge planning staff to contact various community agencies to arrange services best suited to the patient’s needs. Efficient discharge makes possible the admission of other, more critically ill patients, potentially enhancing the hospital’s revenue stream.
Stakeholder Analysis
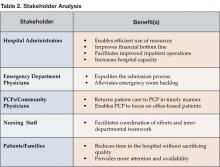
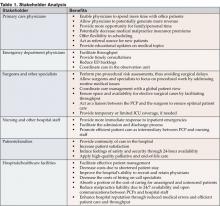
Five specific stakeholders need to be examined to document the value-added by hospitalists. Anecdotal evidence, as well as documented studies, has demonstrated numerous returns—physical, social, psychological and financial—to stakeholders involved in the hospital process. With regard to throughput, the hospitalist provides benefits to each of the stakeholders listed in Table 1.
Study Results
A dozen studies have been conducted that document the impact of hospital medicine programs on cost and clinical outcomes. Of these trials, nine found a significant decrease in the average length of stay (15%) as well as reductions in cost (9). Two other studies, one from an academic medical center and the other from a community teaching hospital, demonstrate similar reductions during a 2-year follow-up period. At the Western Penn Hospital, a 54% reduction in readmissions was reported with a 12% decrease in hospital costs, while the average LOS was 17% shorter. Additionally, an unpublished study from the University of California, San Francisco Medical Center revealed a consistent 10-15% decline in cost and length of stay between hospitalists and non-hospitalist teaching faculty. More important, those differences remained stable through 6 years of follow-up. In general, hospitals with hospitalist programs realized a 5-39% decrease in costs and a shortened average LOS of 7-25% (6).
According to Robert M. Wachter, author of the 2002 study, “If the average U.S. hospitalist cares for 600 inpatients each year and generates a 10% savings over the average medical inpatient cost of $8,000, the nation’s 4500 hospitalists save approximately $2.2 billion per year while potentially improving quality” (6).
In a study conducted by Douglas Gregory, Walter Baigelman, and Ira B. Wilson, hospitalists at Tufts-New England Medical Center in Boston, MA were found to substantially improve throughput with high baseline occupancy levels. Compared with a control group, the hospitalist group reduced LOS from 3.45 days to 2.19 days (p<.001). Additionally, the total cost of hospital admission decreased from $2,332 to $1,775 (p<.001) when hospitalists were involved. According to the study authors, improved throughput generated an incremental 266 patients per year with a related incremental hospital profitability of $1.3 million with the use of hospitalists (7).
Conclusion
As hospital administrators attempt to address the issue of expeditiously admitting, treating and discharging patients in these days of restricted budgets and increased demand, hospitalist programs are poised as an invaluable factor in the throughput process.
Dr. Cawley can be contacted at pcawley@ushosp.com.
References
- Hospital Statistics: the comprehensive reference source for analysis and comparison of hospital trends. Published annually by Health Forum, an affiliate of the American Hospital Association.
- National and local impact of long-term demographic change on inpatient acute care. 2001. Solucient, LLC.
- Zibulewsky J. The Emergency Medical Treatment and Active Labor Act (EMTALA): what it is and what it means for physicians. Baylor University Medical Center (BUMC) Proceedings. 2001;14:339-46.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Eng J Med. 1996;335:514-7.
- Heffner JE. Executive medical director, Medical University of South Carolina (MUSC). Personal interview. June 24, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA.
- Gregory D, Baigelman W, Wilson IB. Hospital economics of the hospitalist. Health Serv Res. 2003;38:905-18.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical co-management after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141:28-38.
- Wachter RM. The evolution of the hospitalist model in the United States. Med Clin North Am. 2002;86:687-706.
According to data from the American Hospital Association (1), in 1985, the United States had 5732 operational community hospitals; by 2002, the latest year for which figures are available, the number had decreased to 4927, a loss of approximately 14% (1). In that same timeframe, these hospitals lost approximately 18% of their beds, dropping from just over 1 million to 820,653 beds. This reduction in bed capacity has been accompanied by hospital cost-cutting efforts, staff downsizing, and elimination of services. Many explanations for these trends have been suggested, including changes in Medicare reimbursement and the growth of managed care organizations (MCOs).
However, as the current baby boom generation ages, rising inpatient demands are presenting hospitals with significant challenges. According to a 2001 report from Solucient (2), who maintains the nation’s largest health care database, the senior population—individuals age 65 and older—are projected to experience an 85% growth rate over the next two decades. Since this age group utilizes inpatient services 4.5 times more than younger populations, the number of admissions and beds to accommodate those cases will soar. By the year 2027, hospitals can anticipate a 46% rise in demand for acute inpatient beds as admissions escalate by approximately 13 million cases. Currently, the nation’s healthcare facilities admit 31 million cases; this number will jump to more than 44 million, representing a 41% growth from present admissions figures. For hospitals that maintain an 80% census rate, an additional 238,000 beds will be needed to meet demands (1).
Adding to this increase in demand and pressure on bed capacity, hospitals must address the requirements of the Emergency Medical Treatment and Active Labor Act (EMTALA) passed by the US Congress in 1986 as part of the Consolidated Omnibus Reconciliation Act (COBRA). The law’s initial intent was to ensure patient access to emergency medical care and to prevent the practice of patient dumping, in which uninsured patients were transferred, solely for financial reasons, from private to public hospitals without consideration of their medical condition or stability for the transfer (3). EMTALA mandates that hospitals rank the severity of patients. Thus, tertiary referral centers are required to admit the sickest patients first. This directive presents a significant challenge to many healthcare facilities. High census rates prohibit the admission of elective surgical cases, which, although profitable, are considered second tier. Routine medical cases or complicated emergency surgical cases have the potential to adversely affect the institution’s financial performance.
In addition to the challenge of increased bed demands and EMTALA, hospitals also cite an increasingly smaller number of on-site community physicians. Longstanding trends from inpatient to outpatient care have prompted many community physicians to concentrate their efforts on serving the needs of office-based patients, limiting their accessibility to hospital cases.
To address these pressures, hospitals must execute innovative strategies that deliver efficient throughput and enhance revenue, while still preserving high-quality services. Since 1996, hospital medicine programs have demonstrated a positive impact on the healthcare facility’s ability to increase overall productivity and profitability and still maintain high quality Patients today present to the doctor sicker than in the past and require more careful and frequent outpatient care. Since hospitalists operate solely on an inpatient basis, their availability to efficiently admit and manage hospitalized patients enables delivery of quality care that expedites appropriate treatment and shortens length of stay.
Two Roles of the Hospitalist
According to the Society of Hospital Medicine (SHM), “Hospitalists are physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to hospital medicine.” Coined by Drs. Robert Wachter and Lee Goldman in 1996 (4), the term implies an additional point of emphasis. Part of a new paradigm in clinical care, the hospitalist enhances the processes of care surrounding patients and adopts an attitude of accountability for that care. In practice, hospitalists play two key roles.
Primarily, the hospitalist is a practicing clinician — managing throughput on a case-by-case, patient-by-patient basis. In addition, a hospitalist performs a non-clinical role as an “inpatient expert,” taking the lead in creating system changes and communicating those changes to other hospital personnel as well as to community physicians. As an inpatient expert, hospitalists are often asked to lead organization-wide throughput initiatives to identify and implement strategies to facilitate patient flow and efficiency. As dedicated members of multi-disciplinary in-house teams, the hospitalist is in a prime position to foster change and improve systems.
Throughput as Continuum of Care
As suggested by Heffner (5), the process of admission, hospitalization, and discharge resembles a “bell-shaped curve.” To achieve effective throughput, hospitals must expedite patient care and also maintain careful oversight throughout a patient’s entire hospital stay. The hospitalist, as an integral part of a multidisciplinary team, coordinates care to promote a positive outcome and shorten length of stay. Drawing on strong leadership qualities, as well as on intimate knowledge of hospital procedures, layout design and infrastructure, and available community resources, the hospitalist plays a pivotal role in creating efficient throughput from admission to discharge.
Emergency Department
At the front end of the bell-shaped curve, the hospitalist may be engaged by emergency department (ED) physicians to assist in ensuring smooth patient flow and, more important, identifies the “intensity of service” needed. Through the use of clinical criteria, such as lnterQual, the hospitalist, together with the ED physician, may be asked to quantitatively rate the patient’s illness for degree of severity.
Timely patient evaluation helps prevent a backlog of ED cases and enables more patients to be seen. Immediate attention to and initiation of appropriate therapy guarantees a better outcome while minimizing the potential risk for complications, which could possibly lead to longer inpatient stays.
Inpatient Unit
Once a patient has been admitted to an inpatient unit, the hospitalist, together with a multidisciplinary team, facilitates care and determines the inpatient services that will optimize patient recovery through strong interdepartmental communications. Working together with admissions, medical records, nursing, laboratory and diagnostic services, information technology and other pertinent departments, the hospitalist maintains a pulse on all activity surrounding the patient and his care.
Judicious inpatient consultations and treatment decisions result in timely changes in therapy, potentially reducing the length of stay. The frequency with which the hospitalist sees the patient allows him to monitor any changes in condition and reduce possible decompensation, a practice known as vertical continuity (6). Such careful attention may reduce inpatient length of stay significantly. When aggressive management is mandated, the presence of the hospitalist enables initiation of effective therapy and results in quicker discharge and a reduction in potential readmission (7).
Surgery
The surgeon and hospitalist are ideally suited to work together in managing a surgical patient. The hospitalist focuses on the peri-operative management of medical issues and risk reduction, which allows the surgeon to concentrate more on surgical indications and the surgery itself. The hospitalist’s role in the management of a surgical patient enables vertical continuity when the surgeon may be occupied in the operating room with another patient as documented by Huddleston’s Hospitalist Orthopedic Team (HOT) approach (8).
Intensive Care Unit (ICU)
In many hospitals, particularly those that do not have intensivists, hospitalists are able to provide quality care to patients. Even in hospitals where intensivists manage ICU patients, hospitalists work together with the intensivist to ensure smoother transition into and out of the unit.
Discharge
Timing is a critical issue with regard to discharge. Since the hospitalist operates solely in-house and in collaboration with a multidisciplinary team, he is able to round early in the day to discharge patients by mid- or late-morning, freeing a bed for a new patient. In some cases, the hospitalist, in anticipation of early discharge, may begin pre-planning the day prior to discharge, which further expedites the process. Early discharge applies to the ICU, step-down areas and general inpatient care areas, as well as to full discharge from the healthcare facility. Moving a patient from one of these areas enables other patients to fill those empty beds thus optimizing throughput.
Having managed the patient throughout his hospital stay, the hospitalist — again working together with a multidisciplinary team —can facilitate arrangements to send the patient home or to a rehabilitation or skilled nursing facility or alternative housing situation upon discharge, as well as coordinating post-discharge care, whether it be arranging for a visiting nursing or social services or communicating with the primary care physician regarding follow-up appointments. If additional outpatient care is prescribed, the hospitalist will work with the discharge planning staff to contact various community agencies to arrange services best suited to the patient’s needs. Efficient discharge makes possible the admission of other, more critically ill patients, potentially enhancing the hospital’s revenue stream.
Stakeholder Analysis
Five specific stakeholders need to be examined to document the value-added by hospitalists. Anecdotal evidence, as well as documented studies, has demonstrated numerous returns—physical, social, psychological and financial—to stakeholders involved in the hospital process. With regard to throughput, the hospitalist provides benefits to each of the stakeholders listed in Table 1.
Study Results
A dozen studies have been conducted that document the impact of hospital medicine programs on cost and clinical outcomes. Of these trials, nine found a significant decrease in the average length of stay (15%) as well as reductions in cost (9). Two other studies, one from an academic medical center and the other from a community teaching hospital, demonstrate similar reductions during a 2-year follow-up period. At the Western Penn Hospital, a 54% reduction in readmissions was reported with a 12% decrease in hospital costs, while the average LOS was 17% shorter. Additionally, an unpublished study from the University of California, San Francisco Medical Center revealed a consistent 10-15% decline in cost and length of stay between hospitalists and non-hospitalist teaching faculty. More important, those differences remained stable through 6 years of follow-up. In general, hospitals with hospitalist programs realized a 5-39% decrease in costs and a shortened average LOS of 7-25% (6).
According to Robert M. Wachter, author of the 2002 study, “If the average U.S. hospitalist cares for 600 inpatients each year and generates a 10% savings over the average medical inpatient cost of $8,000, the nation’s 4500 hospitalists save approximately $2.2 billion per year while potentially improving quality” (6).
In a study conducted by Douglas Gregory, Walter Baigelman, and Ira B. Wilson, hospitalists at Tufts-New England Medical Center in Boston, MA were found to substantially improve throughput with high baseline occupancy levels. Compared with a control group, the hospitalist group reduced LOS from 3.45 days to 2.19 days (p<.001). Additionally, the total cost of hospital admission decreased from $2,332 to $1,775 (p<.001) when hospitalists were involved. According to the study authors, improved throughput generated an incremental 266 patients per year with a related incremental hospital profitability of $1.3 million with the use of hospitalists (7).
Conclusion
As hospital administrators attempt to address the issue of expeditiously admitting, treating and discharging patients in these days of restricted budgets and increased demand, hospitalist programs are poised as an invaluable factor in the throughput process.
Dr. Cawley can be contacted at pcawley@ushosp.com.
References
- Hospital Statistics: the comprehensive reference source for analysis and comparison of hospital trends. Published annually by Health Forum, an affiliate of the American Hospital Association.
- National and local impact of long-term demographic change on inpatient acute care. 2001. Solucient, LLC.
- Zibulewsky J. The Emergency Medical Treatment and Active Labor Act (EMTALA): what it is and what it means for physicians. Baylor University Medical Center (BUMC) Proceedings. 2001;14:339-46.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Eng J Med. 1996;335:514-7.
- Heffner JE. Executive medical director, Medical University of South Carolina (MUSC). Personal interview. June 24, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA.
- Gregory D, Baigelman W, Wilson IB. Hospital economics of the hospitalist. Health Serv Res. 2003;38:905-18.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical co-management after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141:28-38.
- Wachter RM. The evolution of the hospitalist model in the United States. Med Clin North Am. 2002;86:687-706.
According to data from the American Hospital Association (1), in 1985, the United States had 5732 operational community hospitals; by 2002, the latest year for which figures are available, the number had decreased to 4927, a loss of approximately 14% (1). In that same timeframe, these hospitals lost approximately 18% of their beds, dropping from just over 1 million to 820,653 beds. This reduction in bed capacity has been accompanied by hospital cost-cutting efforts, staff downsizing, and elimination of services. Many explanations for these trends have been suggested, including changes in Medicare reimbursement and the growth of managed care organizations (MCOs).
However, as the current baby boom generation ages, rising inpatient demands are presenting hospitals with significant challenges. According to a 2001 report from Solucient (2), who maintains the nation’s largest health care database, the senior population—individuals age 65 and older—are projected to experience an 85% growth rate over the next two decades. Since this age group utilizes inpatient services 4.5 times more than younger populations, the number of admissions and beds to accommodate those cases will soar. By the year 2027, hospitals can anticipate a 46% rise in demand for acute inpatient beds as admissions escalate by approximately 13 million cases. Currently, the nation’s healthcare facilities admit 31 million cases; this number will jump to more than 44 million, representing a 41% growth from present admissions figures. For hospitals that maintain an 80% census rate, an additional 238,000 beds will be needed to meet demands (1).
Adding to this increase in demand and pressure on bed capacity, hospitals must address the requirements of the Emergency Medical Treatment and Active Labor Act (EMTALA) passed by the US Congress in 1986 as part of the Consolidated Omnibus Reconciliation Act (COBRA). The law’s initial intent was to ensure patient access to emergency medical care and to prevent the practice of patient dumping, in which uninsured patients were transferred, solely for financial reasons, from private to public hospitals without consideration of their medical condition or stability for the transfer (3). EMTALA mandates that hospitals rank the severity of patients. Thus, tertiary referral centers are required to admit the sickest patients first. This directive presents a significant challenge to many healthcare facilities. High census rates prohibit the admission of elective surgical cases, which, although profitable, are considered second tier. Routine medical cases or complicated emergency surgical cases have the potential to adversely affect the institution’s financial performance.
In addition to the challenge of increased bed demands and EMTALA, hospitals also cite an increasingly smaller number of on-site community physicians. Longstanding trends from inpatient to outpatient care have prompted many community physicians to concentrate their efforts on serving the needs of office-based patients, limiting their accessibility to hospital cases.
To address these pressures, hospitals must execute innovative strategies that deliver efficient throughput and enhance revenue, while still preserving high-quality services. Since 1996, hospital medicine programs have demonstrated a positive impact on the healthcare facility’s ability to increase overall productivity and profitability and still maintain high quality Patients today present to the doctor sicker than in the past and require more careful and frequent outpatient care. Since hospitalists operate solely on an inpatient basis, their availability to efficiently admit and manage hospitalized patients enables delivery of quality care that expedites appropriate treatment and shortens length of stay.
Two Roles of the Hospitalist
According to the Society of Hospital Medicine (SHM), “Hospitalists are physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to hospital medicine.” Coined by Drs. Robert Wachter and Lee Goldman in 1996 (4), the term implies an additional point of emphasis. Part of a new paradigm in clinical care, the hospitalist enhances the processes of care surrounding patients and adopts an attitude of accountability for that care. In practice, hospitalists play two key roles.
Primarily, the hospitalist is a practicing clinician — managing throughput on a case-by-case, patient-by-patient basis. In addition, a hospitalist performs a non-clinical role as an “inpatient expert,” taking the lead in creating system changes and communicating those changes to other hospital personnel as well as to community physicians. As an inpatient expert, hospitalists are often asked to lead organization-wide throughput initiatives to identify and implement strategies to facilitate patient flow and efficiency. As dedicated members of multi-disciplinary in-house teams, the hospitalist is in a prime position to foster change and improve systems.
Throughput as Continuum of Care
As suggested by Heffner (5), the process of admission, hospitalization, and discharge resembles a “bell-shaped curve.” To achieve effective throughput, hospitals must expedite patient care and also maintain careful oversight throughout a patient’s entire hospital stay. The hospitalist, as an integral part of a multidisciplinary team, coordinates care to promote a positive outcome and shorten length of stay. Drawing on strong leadership qualities, as well as on intimate knowledge of hospital procedures, layout design and infrastructure, and available community resources, the hospitalist plays a pivotal role in creating efficient throughput from admission to discharge.
Emergency Department
At the front end of the bell-shaped curve, the hospitalist may be engaged by emergency department (ED) physicians to assist in ensuring smooth patient flow and, more important, identifies the “intensity of service” needed. Through the use of clinical criteria, such as lnterQual, the hospitalist, together with the ED physician, may be asked to quantitatively rate the patient’s illness for degree of severity.
Timely patient evaluation helps prevent a backlog of ED cases and enables more patients to be seen. Immediate attention to and initiation of appropriate therapy guarantees a better outcome while minimizing the potential risk for complications, which could possibly lead to longer inpatient stays.
Inpatient Unit
Once a patient has been admitted to an inpatient unit, the hospitalist, together with a multidisciplinary team, facilitates care and determines the inpatient services that will optimize patient recovery through strong interdepartmental communications. Working together with admissions, medical records, nursing, laboratory and diagnostic services, information technology and other pertinent departments, the hospitalist maintains a pulse on all activity surrounding the patient and his care.
Judicious inpatient consultations and treatment decisions result in timely changes in therapy, potentially reducing the length of stay. The frequency with which the hospitalist sees the patient allows him to monitor any changes in condition and reduce possible decompensation, a practice known as vertical continuity (6). Such careful attention may reduce inpatient length of stay significantly. When aggressive management is mandated, the presence of the hospitalist enables initiation of effective therapy and results in quicker discharge and a reduction in potential readmission (7).
Surgery
The surgeon and hospitalist are ideally suited to work together in managing a surgical patient. The hospitalist focuses on the peri-operative management of medical issues and risk reduction, which allows the surgeon to concentrate more on surgical indications and the surgery itself. The hospitalist’s role in the management of a surgical patient enables vertical continuity when the surgeon may be occupied in the operating room with another patient as documented by Huddleston’s Hospitalist Orthopedic Team (HOT) approach (8).
Intensive Care Unit (ICU)
In many hospitals, particularly those that do not have intensivists, hospitalists are able to provide quality care to patients. Even in hospitals where intensivists manage ICU patients, hospitalists work together with the intensivist to ensure smoother transition into and out of the unit.
Discharge
Timing is a critical issue with regard to discharge. Since the hospitalist operates solely in-house and in collaboration with a multidisciplinary team, he is able to round early in the day to discharge patients by mid- or late-morning, freeing a bed for a new patient. In some cases, the hospitalist, in anticipation of early discharge, may begin pre-planning the day prior to discharge, which further expedites the process. Early discharge applies to the ICU, step-down areas and general inpatient care areas, as well as to full discharge from the healthcare facility. Moving a patient from one of these areas enables other patients to fill those empty beds thus optimizing throughput.
Having managed the patient throughout his hospital stay, the hospitalist — again working together with a multidisciplinary team —can facilitate arrangements to send the patient home or to a rehabilitation or skilled nursing facility or alternative housing situation upon discharge, as well as coordinating post-discharge care, whether it be arranging for a visiting nursing or social services or communicating with the primary care physician regarding follow-up appointments. If additional outpatient care is prescribed, the hospitalist will work with the discharge planning staff to contact various community agencies to arrange services best suited to the patient’s needs. Efficient discharge makes possible the admission of other, more critically ill patients, potentially enhancing the hospital’s revenue stream.
Stakeholder Analysis
Five specific stakeholders need to be examined to document the value-added by hospitalists. Anecdotal evidence, as well as documented studies, has demonstrated numerous returns—physical, social, psychological and financial—to stakeholders involved in the hospital process. With regard to throughput, the hospitalist provides benefits to each of the stakeholders listed in Table 1.
Study Results
A dozen studies have been conducted that document the impact of hospital medicine programs on cost and clinical outcomes. Of these trials, nine found a significant decrease in the average length of stay (15%) as well as reductions in cost (9). Two other studies, one from an academic medical center and the other from a community teaching hospital, demonstrate similar reductions during a 2-year follow-up period. At the Western Penn Hospital, a 54% reduction in readmissions was reported with a 12% decrease in hospital costs, while the average LOS was 17% shorter. Additionally, an unpublished study from the University of California, San Francisco Medical Center revealed a consistent 10-15% decline in cost and length of stay between hospitalists and non-hospitalist teaching faculty. More important, those differences remained stable through 6 years of follow-up. In general, hospitals with hospitalist programs realized a 5-39% decrease in costs and a shortened average LOS of 7-25% (6).
According to Robert M. Wachter, author of the 2002 study, “If the average U.S. hospitalist cares for 600 inpatients each year and generates a 10% savings over the average medical inpatient cost of $8,000, the nation’s 4500 hospitalists save approximately $2.2 billion per year while potentially improving quality” (6).
In a study conducted by Douglas Gregory, Walter Baigelman, and Ira B. Wilson, hospitalists at Tufts-New England Medical Center in Boston, MA were found to substantially improve throughput with high baseline occupancy levels. Compared with a control group, the hospitalist group reduced LOS from 3.45 days to 2.19 days (p<.001). Additionally, the total cost of hospital admission decreased from $2,332 to $1,775 (p<.001) when hospitalists were involved. According to the study authors, improved throughput generated an incremental 266 patients per year with a related incremental hospital profitability of $1.3 million with the use of hospitalists (7).
Conclusion
As hospital administrators attempt to address the issue of expeditiously admitting, treating and discharging patients in these days of restricted budgets and increased demand, hospitalist programs are poised as an invaluable factor in the throughput process.
Dr. Cawley can be contacted at pcawley@ushosp.com.
References
- Hospital Statistics: the comprehensive reference source for analysis and comparison of hospital trends. Published annually by Health Forum, an affiliate of the American Hospital Association.
- National and local impact of long-term demographic change on inpatient acute care. 2001. Solucient, LLC.
- Zibulewsky J. The Emergency Medical Treatment and Active Labor Act (EMTALA): what it is and what it means for physicians. Baylor University Medical Center (BUMC) Proceedings. 2001;14:339-46.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Eng J Med. 1996;335:514-7.
- Heffner JE. Executive medical director, Medical University of South Carolina (MUSC). Personal interview. June 24, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA.
- Gregory D, Baigelman W, Wilson IB. Hospital economics of the hospitalist. Health Serv Res. 2003;38:905-18.
- Huddleston JM, Long KH, Naessens JM, et al. Medical and surgical co-management after elective hip and knee arthroplasty: a randomized, controlled trial. Ann Intern Med. 2004;141:28-38.
- Wachter RM. The evolution of the hospitalist model in the United States. Med Clin North Am. 2002;86:687-706.
Improving Resource Utilization
Today’s hospitals must address a variety of challenges stemming from the expectation to provide more services and better quality with fewer financial, material, and human resources. According to the annual survey conducted by the American Hospital Association (AHA) in 2003, total expenses for all U.S. community hospitals were more than $450 billion. In managing these expenditures, hospitals face the following pressures:
- Cost increases in medical supplies and pharmaceuticals.
- Record shortages of nurses, pharmacists, and technicians.
- A growing uncompensated patient pool.
- Annual potential reductions in Medicare and Medicaid reimbursements.
- Rising bad debt resulting from greater patient responsibility for the cost of care.
- The diversion of more profitable cases to specialty and freestanding ambulatory care facilities and surgery centers.
- Soaring costs associated with adequately serving high-risk conditions, such as cancer, heart disease, and HIV/AIDS.
- Discounted reimbursement rates with insurers.
- Increasing pressure to commit financial resources to clinical information technology.
- The need to fund infrastructure improvements and physical plant renovations as well as expansions to address increasing demand (1).
To overcome these challenges, hospitals must find innovative ways to balance revenues and expenses, fund necessary capital investments, and satisfy the public’s demand for quality, safety, and accessibility.
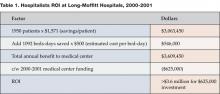
Hospitalist Programs: A Good Investment
One solution to the above-mentioned situations is a hospitalist program, which, in its short history, has already had a profound impact on inpatient care. Robert M. Wachter, MD, associate chair in the department of medicine at the University of California, San Francisco (UCSF) and medical service chief at Moffitt-Long Hospitals, coined the term Hospitalist in an article in the New England Journal of Medicine in 1996 (2). At the 2002 annual meeting of the Society of Hospital Medicine (SHM), Wachter presented findings from a study conducted at his institution. The results demonstrate a significant return on investment (ROI) of 5.8:1 when a hospitalist program is utilized (See Table 1 for details) (3).
How do hospitalists reduce length of stay (LOS) and cost per stay? William David Rifkin, MD, associate director of the Yale Primary Care Residency Program, offers three basic reasons why hospitalist programs contribute to effective and efficient use of resources. Since hospitalists are physically onsite, they are better able to react to condition changes and requests for consultations in a timely manner, he asserts. Also, being familiar with the hospital’s systems of care, the hospitalist knows who to call and how to utilize the services of social workers and other contingency staff when arranging for post-discharge care. Third, Rifkin indicates that inpatients today are sicker than they were in past years, a fact well known and understood by hospitalists. “There is an increased level of acuity,” he says. “Hospitalists are used to seeing these kinds of patients. They are more comfortable taking care of these patients and will see more of them with any given diagnosis” (4).
In one of his studies, Rifkin noted a reduction in LOS for inpatients with a pneumonia diagnosis. “The hospitalist had switched the patient from IV (intravenous) to oral antibiotics,” he says. Reacting quickly to indications that the patient was ready for a change in treatment modality facilitated an earlier discharge (5).
L. Craig Miller, MD, senior vice president of medical affairs at Baptist Health Care, reports that his hospital saved $2.56 million in 2 years as a direct result of its inpatient management program (6). Although attention to technical and clinical details is important, Miller emphasizes the critical role the human factor plays, specifically the impact of teamwork, on achieving resource utilization savings.
“Hospitalists work as a team, collaborating with physicians and ED doctors,” he says. This cooperative spirit enables the efficient use of manpower in patient care. Miller adds that at Baptist, as is the case at most hospitals, the medical complexity of patients dictates a need for cooperation in order to successfully treat illness. The presence of hospitalists facilitates the team effort, causing a positive trickle down effect regarding LOS, readmission and mortality rates, he affirms. “The hospitalist provides focused leadership to utilization resource management,” says Miller (7).
In the role of inpatient leader, the hospitalist also facilitates ED throughput, which results in another area of cost savings for the hospital. Paola Coppola, MD, ED director at Brookhaven Memorial Hospital Medical Center, says, “From an ER perspective, a call to the hospitalist replaces multiple calls to specialists. In general, hospitalists feel much more comfortable treating a wide array of conditions including infectious disease, pneumonias, strokes, and chest pain without the intervention of specialists in that field. Hence, hospital consumption of resources decreases, which in turn lowers length of stay.” He echoes Rifkin’s thoughts on quick response time. “Hospitalists provide an immediately available service, thus saving ER physicians valuable time. This ensures faster turnover, better throughput, makes more ER beds available, and services more patients, eventually helping the hospital’s bottom line,” says Coppola (8).
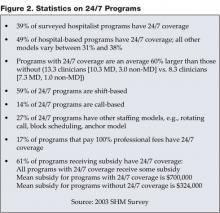
In addition to teamwork, 24/7 availability is vital to the wise utilization of resources, according to Anthony Shallash, MD, vice president of medical affairs at Brookhaven. “The fact of 24/7 presence allows rapid responses to patient condition and problems. Continuous and close monitoring of patients allows them to be upgraded or downgraded as needed,” he says. “As such, LOS is decreased and quite favorable as compared to peer practitioners for similar disease severity. Resources consumed and tests ordered also show a favorable trend” (9).
A recently published study (10) by researchers at Dartmouth Medical School documents the variation in the volume and cost of services that academic medical centers use in treating patients. Hospitals were categorized as low- and high-intensity, with significant differences in cost per case. For example, the high-intensity hospitals spent up to 47% more on care for acute myocardial infarction. In an interview in Today’s Hospitalist (11), the lead author, Elliott S. Fisher, MD, professor of medicine and community and family medicine at Dartmouth Medical School, described the importance of coordination in achieving efficient care. Fisher says, “I think there’s a real opportunity for hospitalists to improve the care of patients in both high- and low- intensity hospitals. Having ten doctors involved in a given patient’s care may not be a good thing, unless someone [i.e., the hospitalist] is doing a really good job of coordinating that care.”
Hospitalists focus only on inpatient medicine. They are familiar with managing the most common medical diagnoses, such as community acquired pneumonia, diabetes. and congestive heart failure. Hospitalist programs often develop uniform and consistent ways of treating these patients. Cogent Healthcare, a national hospitalist management company has implemented the “Cogent Care Guides,” best practice guidelines for high-volume hospital diagnoses. Ron Greeno, MD, FCCP and Cogent’s chief medical officer, says “The Cogent Care Guides ensure best practices are implemented at critical points in the patient’s care… decreasing the variability of care that results in inefficiencies.” Greeno added, “The care guidelines [also] support the timely notification of the primary care physician of nine critical landmark events related to patient status that can affect outcomes” (12).
Stacy Goldsholl, Director of the Covenant HealthCare Hospital Medicine Program in Saginaw, MI, suggests other ways that hospitalists can generate utilization savings for their hospitals. “Hospitalists often eliminate unnecessary admissions and shift work-ups to the ambulatory setting. For example, I recently arranged an outpatient colonoscopy for a pneumonia patient with a stable hemoglobin and heme positive stool. Because of my experience treating patients with pneumonia, I was able to determine that the circumstances did not require an inpatient stay.” In addition, Dr. Goldsholl has found that the hospitalists in her program are quite effective in classifying “observation” patients, eliminating reimbursement conflicts with Medicare, Medicaid, and other insurers.
Finally, because they are always in the hospital rather than sharing time between the office and hospital, hospitalists can improve inpatient continuity of care, resulting in lower costs and better outcomes. Adrienne Bennett, MD, chief of the hospital medicine service at Newton-Wellesley Hospital near Boston, examined cases managed by hospitalists and non-hospitalist community physicians, comparing the number of “handoffs” of responsibility that occur among attending physicians. Community physicians share inpatient responsibility in their practices and sometimes their partners round on their patients. Every time another physician assumes responsibility for a patient, there is the potential for a loss of information and a discontinuity of care. At Newton-Wellesley Hospital, the hospitalists work a schedule of 14 days on, followed by 7 days off. “We found that hospitalists averaged less than half the number of handoffs as the community physicians,” says Bennett. “This may be one of the reasons that hospitalists have better case mix adjusted utilization performance.”
Stakeholder Analysis
Anecdotal evidence, as well as documented studies, has demonstrated that hospitalists provide value to a wide range of stakeholders involved in the inpatient care process. With regard to resource utilization savings, the hospitalist provides benefits to each of the listed stakeholders (Table 2).
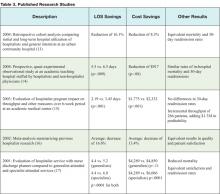
Published Research Results
Dozens of studies demonstrate the positive effects hospitalist programs have on resource utilization. Observational, retrospective, and prospective data analyses have been conducted at community-based hospitals as well as at academic medical institutions. Findings consistently indicate that hospitalist programs result in resource savings for patients, physicians. and hospital medicine. A range of studies shown in Table 3 represent the most recent efforts at tracking hospitalist programs and their effects on resource utilization.
Conclusion
According to the AHA’s 2003 survey of healthcare trends, the fiscal health of the nation’s hospitals will most likely remain fragile and variable in the coming years. The survey cites declining operating margins, a continued decrease in reimbursement, labor shortages, and rising insurance and pharmaceutical costs, as well as the need to invest in technology and facility maintenance and upkeep as key factors. However, hospitalists have proven time and again in clinical studies that they can bring value to the operation of a healthcare facility. With reduced lengths of stay, decreased overall hospital costs, and equivalent — if not superior — quality, hospitalists can contribute significantly to a hospital’s healthy bottom line.
Dr. Syed can be contacted at syed.saeed@CogentHealthcare.com.
References
- ACP Research Center, Environmental Assessment: Trends in hospital financing. 2003. www.aha.org.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514-7
- Wachter RM. Presentation, Society of Hospital Medicine (SHM) annual meeting 2002. 4. Rifkin WD. Telephone interview December 15, 2004.
- Rifkin WD, Conner D, Silver A, Eichom A. Comparison of processes and outcomes of pneumonia care between hospitalists and community-based primary care physicians. Mayo Clin Proc. 2002;77:1053-8.
- “Hospitalists save $2.5 million and decrease LOS.” Healthcare Benchmarks and Quality Improvement, May 2004.
- Miller LC. Telephone intewiew, November 16, 2004.
- Coppola P. Email interview, December 15,2004.
- Shallash A. Email interview, December17, 2004.
- Healthaffairs.org, “Use of Medicare claims data to monitor provider-specific performance among patients with severe chronic illness.” 10.1377/hlthaff.var.5. Posting date: October 7, 2004.
- Why less really can be more when it comes to teaching hospitals. Today’s Hospitalist. 2004 December.
- Greeno R. Chief medical officer, Cogent Healthcare, Irvine, California. Telephone interview. December 16, 2004.
- Everett GD, Anton MP Jackson BK, Swigert C, Uddin N. Comparison of hospital costs and length of stay associated with general internists and hospitalist physicians at a community hospital. Am J Manag Care. 2004;10:626-30.
- Kaboli PJ, Barnett MJ, Rosenthal GE. Associations with reduced length of stay and costs on an academic hospitalist service. Am J Manag Care. 2004;10:561-8.
- Gregory D, Baigelman W, Wilson IB. Hospital economics of the hospitalist. Health Services Research. 2003:38(3):905-18; discussion 919-22.
- Wachter RM, Goldman L The hospitalist movement 5 years later. JAMA. 2002;287:487-94.
- Palmer HC, Armistead NS, Elnicki DM, et al. The effect of a hospitalist service with nurse discharge planner on patient care in an academic teaching hospital. Am J Med. 2001;111:627-32.
Today’s hospitals must address a variety of challenges stemming from the expectation to provide more services and better quality with fewer financial, material, and human resources. According to the annual survey conducted by the American Hospital Association (AHA) in 2003, total expenses for all U.S. community hospitals were more than $450 billion. In managing these expenditures, hospitals face the following pressures:
- Cost increases in medical supplies and pharmaceuticals.
- Record shortages of nurses, pharmacists, and technicians.
- A growing uncompensated patient pool.
- Annual potential reductions in Medicare and Medicaid reimbursements.
- Rising bad debt resulting from greater patient responsibility for the cost of care.
- The diversion of more profitable cases to specialty and freestanding ambulatory care facilities and surgery centers.
- Soaring costs associated with adequately serving high-risk conditions, such as cancer, heart disease, and HIV/AIDS.
- Discounted reimbursement rates with insurers.
- Increasing pressure to commit financial resources to clinical information technology.
- The need to fund infrastructure improvements and physical plant renovations as well as expansions to address increasing demand (1).
To overcome these challenges, hospitals must find innovative ways to balance revenues and expenses, fund necessary capital investments, and satisfy the public’s demand for quality, safety, and accessibility.
Hospitalist Programs: A Good Investment
One solution to the above-mentioned situations is a hospitalist program, which, in its short history, has already had a profound impact on inpatient care. Robert M. Wachter, MD, associate chair in the department of medicine at the University of California, San Francisco (UCSF) and medical service chief at Moffitt-Long Hospitals, coined the term Hospitalist in an article in the New England Journal of Medicine in 1996 (2). At the 2002 annual meeting of the Society of Hospital Medicine (SHM), Wachter presented findings from a study conducted at his institution. The results demonstrate a significant return on investment (ROI) of 5.8:1 when a hospitalist program is utilized (See Table 1 for details) (3).
How do hospitalists reduce length of stay (LOS) and cost per stay? William David Rifkin, MD, associate director of the Yale Primary Care Residency Program, offers three basic reasons why hospitalist programs contribute to effective and efficient use of resources. Since hospitalists are physically onsite, they are better able to react to condition changes and requests for consultations in a timely manner, he asserts. Also, being familiar with the hospital’s systems of care, the hospitalist knows who to call and how to utilize the services of social workers and other contingency staff when arranging for post-discharge care. Third, Rifkin indicates that inpatients today are sicker than they were in past years, a fact well known and understood by hospitalists. “There is an increased level of acuity,” he says. “Hospitalists are used to seeing these kinds of patients. They are more comfortable taking care of these patients and will see more of them with any given diagnosis” (4).
In one of his studies, Rifkin noted a reduction in LOS for inpatients with a pneumonia diagnosis. “The hospitalist had switched the patient from IV (intravenous) to oral antibiotics,” he says. Reacting quickly to indications that the patient was ready for a change in treatment modality facilitated an earlier discharge (5).
L. Craig Miller, MD, senior vice president of medical affairs at Baptist Health Care, reports that his hospital saved $2.56 million in 2 years as a direct result of its inpatient management program (6). Although attention to technical and clinical details is important, Miller emphasizes the critical role the human factor plays, specifically the impact of teamwork, on achieving resource utilization savings.
“Hospitalists work as a team, collaborating with physicians and ED doctors,” he says. This cooperative spirit enables the efficient use of manpower in patient care. Miller adds that at Baptist, as is the case at most hospitals, the medical complexity of patients dictates a need for cooperation in order to successfully treat illness. The presence of hospitalists facilitates the team effort, causing a positive trickle down effect regarding LOS, readmission and mortality rates, he affirms. “The hospitalist provides focused leadership to utilization resource management,” says Miller (7).
In the role of inpatient leader, the hospitalist also facilitates ED throughput, which results in another area of cost savings for the hospital. Paola Coppola, MD, ED director at Brookhaven Memorial Hospital Medical Center, says, “From an ER perspective, a call to the hospitalist replaces multiple calls to specialists. In general, hospitalists feel much more comfortable treating a wide array of conditions including infectious disease, pneumonias, strokes, and chest pain without the intervention of specialists in that field. Hence, hospital consumption of resources decreases, which in turn lowers length of stay.” He echoes Rifkin’s thoughts on quick response time. “Hospitalists provide an immediately available service, thus saving ER physicians valuable time. This ensures faster turnover, better throughput, makes more ER beds available, and services more patients, eventually helping the hospital’s bottom line,” says Coppola (8).
In addition to teamwork, 24/7 availability is vital to the wise utilization of resources, according to Anthony Shallash, MD, vice president of medical affairs at Brookhaven. “The fact of 24/7 presence allows rapid responses to patient condition and problems. Continuous and close monitoring of patients allows them to be upgraded or downgraded as needed,” he says. “As such, LOS is decreased and quite favorable as compared to peer practitioners for similar disease severity. Resources consumed and tests ordered also show a favorable trend” (9).
A recently published study (10) by researchers at Dartmouth Medical School documents the variation in the volume and cost of services that academic medical centers use in treating patients. Hospitals were categorized as low- and high-intensity, with significant differences in cost per case. For example, the high-intensity hospitals spent up to 47% more on care for acute myocardial infarction. In an interview in Today’s Hospitalist (11), the lead author, Elliott S. Fisher, MD, professor of medicine and community and family medicine at Dartmouth Medical School, described the importance of coordination in achieving efficient care. Fisher says, “I think there’s a real opportunity for hospitalists to improve the care of patients in both high- and low- intensity hospitals. Having ten doctors involved in a given patient’s care may not be a good thing, unless someone [i.e., the hospitalist] is doing a really good job of coordinating that care.”
Hospitalists focus only on inpatient medicine. They are familiar with managing the most common medical diagnoses, such as community acquired pneumonia, diabetes. and congestive heart failure. Hospitalist programs often develop uniform and consistent ways of treating these patients. Cogent Healthcare, a national hospitalist management company has implemented the “Cogent Care Guides,” best practice guidelines for high-volume hospital diagnoses. Ron Greeno, MD, FCCP and Cogent’s chief medical officer, says “The Cogent Care Guides ensure best practices are implemented at critical points in the patient’s care… decreasing the variability of care that results in inefficiencies.” Greeno added, “The care guidelines [also] support the timely notification of the primary care physician of nine critical landmark events related to patient status that can affect outcomes” (12).
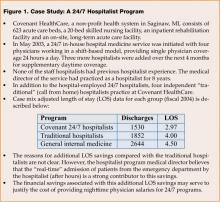
Stacy Goldsholl, Director of the Covenant HealthCare Hospital Medicine Program in Saginaw, MI, suggests other ways that hospitalists can generate utilization savings for their hospitals. “Hospitalists often eliminate unnecessary admissions and shift work-ups to the ambulatory setting. For example, I recently arranged an outpatient colonoscopy for a pneumonia patient with a stable hemoglobin and heme positive stool. Because of my experience treating patients with pneumonia, I was able to determine that the circumstances did not require an inpatient stay.” In addition, Dr. Goldsholl has found that the hospitalists in her program are quite effective in classifying “observation” patients, eliminating reimbursement conflicts with Medicare, Medicaid, and other insurers.
Finally, because they are always in the hospital rather than sharing time between the office and hospital, hospitalists can improve inpatient continuity of care, resulting in lower costs and better outcomes. Adrienne Bennett, MD, chief of the hospital medicine service at Newton-Wellesley Hospital near Boston, examined cases managed by hospitalists and non-hospitalist community physicians, comparing the number of “handoffs” of responsibility that occur among attending physicians. Community physicians share inpatient responsibility in their practices and sometimes their partners round on their patients. Every time another physician assumes responsibility for a patient, there is the potential for a loss of information and a discontinuity of care. At Newton-Wellesley Hospital, the hospitalists work a schedule of 14 days on, followed by 7 days off. “We found that hospitalists averaged less than half the number of handoffs as the community physicians,” says Bennett. “This may be one of the reasons that hospitalists have better case mix adjusted utilization performance.”
Stakeholder Analysis
Anecdotal evidence, as well as documented studies, has demonstrated that hospitalists provide value to a wide range of stakeholders involved in the inpatient care process. With regard to resource utilization savings, the hospitalist provides benefits to each of the listed stakeholders (Table 2).
Published Research Results
Dozens of studies demonstrate the positive effects hospitalist programs have on resource utilization. Observational, retrospective, and prospective data analyses have been conducted at community-based hospitals as well as at academic medical institutions. Findings consistently indicate that hospitalist programs result in resource savings for patients, physicians. and hospital medicine. A range of studies shown in Table 3 represent the most recent efforts at tracking hospitalist programs and their effects on resource utilization.
Conclusion
According to the AHA’s 2003 survey of healthcare trends, the fiscal health of the nation’s hospitals will most likely remain fragile and variable in the coming years. The survey cites declining operating margins, a continued decrease in reimbursement, labor shortages, and rising insurance and pharmaceutical costs, as well as the need to invest in technology and facility maintenance and upkeep as key factors. However, hospitalists have proven time and again in clinical studies that they can bring value to the operation of a healthcare facility. With reduced lengths of stay, decreased overall hospital costs, and equivalent — if not superior — quality, hospitalists can contribute significantly to a hospital’s healthy bottom line.
Dr. Syed can be contacted at syed.saeed@CogentHealthcare.com.
References
- ACP Research Center, Environmental Assessment: Trends in hospital financing. 2003. www.aha.org.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514-7
- Wachter RM. Presentation, Society of Hospital Medicine (SHM) annual meeting 2002. 4. Rifkin WD. Telephone interview December 15, 2004.
- Rifkin WD, Conner D, Silver A, Eichom A. Comparison of processes and outcomes of pneumonia care between hospitalists and community-based primary care physicians. Mayo Clin Proc. 2002;77:1053-8.
- “Hospitalists save $2.5 million and decrease LOS.” Healthcare Benchmarks and Quality Improvement, May 2004.
- Miller LC. Telephone intewiew, November 16, 2004.
- Coppola P. Email interview, December 15,2004.
- Shallash A. Email interview, December17, 2004.
- Healthaffairs.org, “Use of Medicare claims data to monitor provider-specific performance among patients with severe chronic illness.” 10.1377/hlthaff.var.5. Posting date: October 7, 2004.
- Why less really can be more when it comes to teaching hospitals. Today’s Hospitalist. 2004 December.
- Greeno R. Chief medical officer, Cogent Healthcare, Irvine, California. Telephone interview. December 16, 2004.
- Everett GD, Anton MP Jackson BK, Swigert C, Uddin N. Comparison of hospital costs and length of stay associated with general internists and hospitalist physicians at a community hospital. Am J Manag Care. 2004;10:626-30.
- Kaboli PJ, Barnett MJ, Rosenthal GE. Associations with reduced length of stay and costs on an academic hospitalist service. Am J Manag Care. 2004;10:561-8.
- Gregory D, Baigelman W, Wilson IB. Hospital economics of the hospitalist. Health Services Research. 2003:38(3):905-18; discussion 919-22.
- Wachter RM, Goldman L The hospitalist movement 5 years later. JAMA. 2002;287:487-94.
- Palmer HC, Armistead NS, Elnicki DM, et al. The effect of a hospitalist service with nurse discharge planner on patient care in an academic teaching hospital. Am J Med. 2001;111:627-32.
Today’s hospitals must address a variety of challenges stemming from the expectation to provide more services and better quality with fewer financial, material, and human resources. According to the annual survey conducted by the American Hospital Association (AHA) in 2003, total expenses for all U.S. community hospitals were more than $450 billion. In managing these expenditures, hospitals face the following pressures:
- Cost increases in medical supplies and pharmaceuticals.
- Record shortages of nurses, pharmacists, and technicians.
- A growing uncompensated patient pool.
- Annual potential reductions in Medicare and Medicaid reimbursements.
- Rising bad debt resulting from greater patient responsibility for the cost of care.
- The diversion of more profitable cases to specialty and freestanding ambulatory care facilities and surgery centers.
- Soaring costs associated with adequately serving high-risk conditions, such as cancer, heart disease, and HIV/AIDS.
- Discounted reimbursement rates with insurers.
- Increasing pressure to commit financial resources to clinical information technology.
- The need to fund infrastructure improvements and physical plant renovations as well as expansions to address increasing demand (1).
To overcome these challenges, hospitals must find innovative ways to balance revenues and expenses, fund necessary capital investments, and satisfy the public’s demand for quality, safety, and accessibility.
Hospitalist Programs: A Good Investment
One solution to the above-mentioned situations is a hospitalist program, which, in its short history, has already had a profound impact on inpatient care. Robert M. Wachter, MD, associate chair in the department of medicine at the University of California, San Francisco (UCSF) and medical service chief at Moffitt-Long Hospitals, coined the term Hospitalist in an article in the New England Journal of Medicine in 1996 (2). At the 2002 annual meeting of the Society of Hospital Medicine (SHM), Wachter presented findings from a study conducted at his institution. The results demonstrate a significant return on investment (ROI) of 5.8:1 when a hospitalist program is utilized (See Table 1 for details) (3).
How do hospitalists reduce length of stay (LOS) and cost per stay? William David Rifkin, MD, associate director of the Yale Primary Care Residency Program, offers three basic reasons why hospitalist programs contribute to effective and efficient use of resources. Since hospitalists are physically onsite, they are better able to react to condition changes and requests for consultations in a timely manner, he asserts. Also, being familiar with the hospital’s systems of care, the hospitalist knows who to call and how to utilize the services of social workers and other contingency staff when arranging for post-discharge care. Third, Rifkin indicates that inpatients today are sicker than they were in past years, a fact well known and understood by hospitalists. “There is an increased level of acuity,” he says. “Hospitalists are used to seeing these kinds of patients. They are more comfortable taking care of these patients and will see more of them with any given diagnosis” (4).
In one of his studies, Rifkin noted a reduction in LOS for inpatients with a pneumonia diagnosis. “The hospitalist had switched the patient from IV (intravenous) to oral antibiotics,” he says. Reacting quickly to indications that the patient was ready for a change in treatment modality facilitated an earlier discharge (5).
L. Craig Miller, MD, senior vice president of medical affairs at Baptist Health Care, reports that his hospital saved $2.56 million in 2 years as a direct result of its inpatient management program (6). Although attention to technical and clinical details is important, Miller emphasizes the critical role the human factor plays, specifically the impact of teamwork, on achieving resource utilization savings.
“Hospitalists work as a team, collaborating with physicians and ED doctors,” he says. This cooperative spirit enables the efficient use of manpower in patient care. Miller adds that at Baptist, as is the case at most hospitals, the medical complexity of patients dictates a need for cooperation in order to successfully treat illness. The presence of hospitalists facilitates the team effort, causing a positive trickle down effect regarding LOS, readmission and mortality rates, he affirms. “The hospitalist provides focused leadership to utilization resource management,” says Miller (7).
In the role of inpatient leader, the hospitalist also facilitates ED throughput, which results in another area of cost savings for the hospital. Paola Coppola, MD, ED director at Brookhaven Memorial Hospital Medical Center, says, “From an ER perspective, a call to the hospitalist replaces multiple calls to specialists. In general, hospitalists feel much more comfortable treating a wide array of conditions including infectious disease, pneumonias, strokes, and chest pain without the intervention of specialists in that field. Hence, hospital consumption of resources decreases, which in turn lowers length of stay.” He echoes Rifkin’s thoughts on quick response time. “Hospitalists provide an immediately available service, thus saving ER physicians valuable time. This ensures faster turnover, better throughput, makes more ER beds available, and services more patients, eventually helping the hospital’s bottom line,” says Coppola (8).
In addition to teamwork, 24/7 availability is vital to the wise utilization of resources, according to Anthony Shallash, MD, vice president of medical affairs at Brookhaven. “The fact of 24/7 presence allows rapid responses to patient condition and problems. Continuous and close monitoring of patients allows them to be upgraded or downgraded as needed,” he says. “As such, LOS is decreased and quite favorable as compared to peer practitioners for similar disease severity. Resources consumed and tests ordered also show a favorable trend” (9).
A recently published study (10) by researchers at Dartmouth Medical School documents the variation in the volume and cost of services that academic medical centers use in treating patients. Hospitals were categorized as low- and high-intensity, with significant differences in cost per case. For example, the high-intensity hospitals spent up to 47% more on care for acute myocardial infarction. In an interview in Today’s Hospitalist (11), the lead author, Elliott S. Fisher, MD, professor of medicine and community and family medicine at Dartmouth Medical School, described the importance of coordination in achieving efficient care. Fisher says, “I think there’s a real opportunity for hospitalists to improve the care of patients in both high- and low- intensity hospitals. Having ten doctors involved in a given patient’s care may not be a good thing, unless someone [i.e., the hospitalist] is doing a really good job of coordinating that care.”
Hospitalists focus only on inpatient medicine. They are familiar with managing the most common medical diagnoses, such as community acquired pneumonia, diabetes. and congestive heart failure. Hospitalist programs often develop uniform and consistent ways of treating these patients. Cogent Healthcare, a national hospitalist management company has implemented the “Cogent Care Guides,” best practice guidelines for high-volume hospital diagnoses. Ron Greeno, MD, FCCP and Cogent’s chief medical officer, says “The Cogent Care Guides ensure best practices are implemented at critical points in the patient’s care… decreasing the variability of care that results in inefficiencies.” Greeno added, “The care guidelines [also] support the timely notification of the primary care physician of nine critical landmark events related to patient status that can affect outcomes” (12).
Stacy Goldsholl, Director of the Covenant HealthCare Hospital Medicine Program in Saginaw, MI, suggests other ways that hospitalists can generate utilization savings for their hospitals. “Hospitalists often eliminate unnecessary admissions and shift work-ups to the ambulatory setting. For example, I recently arranged an outpatient colonoscopy for a pneumonia patient with a stable hemoglobin and heme positive stool. Because of my experience treating patients with pneumonia, I was able to determine that the circumstances did not require an inpatient stay.” In addition, Dr. Goldsholl has found that the hospitalists in her program are quite effective in classifying “observation” patients, eliminating reimbursement conflicts with Medicare, Medicaid, and other insurers.
Finally, because they are always in the hospital rather than sharing time between the office and hospital, hospitalists can improve inpatient continuity of care, resulting in lower costs and better outcomes. Adrienne Bennett, MD, chief of the hospital medicine service at Newton-Wellesley Hospital near Boston, examined cases managed by hospitalists and non-hospitalist community physicians, comparing the number of “handoffs” of responsibility that occur among attending physicians. Community physicians share inpatient responsibility in their practices and sometimes their partners round on their patients. Every time another physician assumes responsibility for a patient, there is the potential for a loss of information and a discontinuity of care. At Newton-Wellesley Hospital, the hospitalists work a schedule of 14 days on, followed by 7 days off. “We found that hospitalists averaged less than half the number of handoffs as the community physicians,” says Bennett. “This may be one of the reasons that hospitalists have better case mix adjusted utilization performance.”
Stakeholder Analysis
Anecdotal evidence, as well as documented studies, has demonstrated that hospitalists provide value to a wide range of stakeholders involved in the inpatient care process. With regard to resource utilization savings, the hospitalist provides benefits to each of the listed stakeholders (Table 2).
Published Research Results
Dozens of studies demonstrate the positive effects hospitalist programs have on resource utilization. Observational, retrospective, and prospective data analyses have been conducted at community-based hospitals as well as at academic medical institutions. Findings consistently indicate that hospitalist programs result in resource savings for patients, physicians. and hospital medicine. A range of studies shown in Table 3 represent the most recent efforts at tracking hospitalist programs and their effects on resource utilization.
Conclusion
According to the AHA’s 2003 survey of healthcare trends, the fiscal health of the nation’s hospitals will most likely remain fragile and variable in the coming years. The survey cites declining operating margins, a continued decrease in reimbursement, labor shortages, and rising insurance and pharmaceutical costs, as well as the need to invest in technology and facility maintenance and upkeep as key factors. However, hospitalists have proven time and again in clinical studies that they can bring value to the operation of a healthcare facility. With reduced lengths of stay, decreased overall hospital costs, and equivalent — if not superior — quality, hospitalists can contribute significantly to a hospital’s healthy bottom line.
Dr. Syed can be contacted at syed.saeed@CogentHealthcare.com.
References
- ACP Research Center, Environmental Assessment: Trends in hospital financing. 2003. www.aha.org.
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514-7
- Wachter RM. Presentation, Society of Hospital Medicine (SHM) annual meeting 2002. 4. Rifkin WD. Telephone interview December 15, 2004.
- Rifkin WD, Conner D, Silver A, Eichom A. Comparison of processes and outcomes of pneumonia care between hospitalists and community-based primary care physicians. Mayo Clin Proc. 2002;77:1053-8.
- “Hospitalists save $2.5 million and decrease LOS.” Healthcare Benchmarks and Quality Improvement, May 2004.
- Miller LC. Telephone intewiew, November 16, 2004.
- Coppola P. Email interview, December 15,2004.
- Shallash A. Email interview, December17, 2004.
- Healthaffairs.org, “Use of Medicare claims data to monitor provider-specific performance among patients with severe chronic illness.” 10.1377/hlthaff.var.5. Posting date: October 7, 2004.
- Why less really can be more when it comes to teaching hospitals. Today’s Hospitalist. 2004 December.
- Greeno R. Chief medical officer, Cogent Healthcare, Irvine, California. Telephone interview. December 16, 2004.
- Everett GD, Anton MP Jackson BK, Swigert C, Uddin N. Comparison of hospital costs and length of stay associated with general internists and hospitalist physicians at a community hospital. Am J Manag Care. 2004;10:626-30.
- Kaboli PJ, Barnett MJ, Rosenthal GE. Associations with reduced length of stay and costs on an academic hospitalist service. Am J Manag Care. 2004;10:561-8.
- Gregory D, Baigelman W, Wilson IB. Hospital economics of the hospitalist. Health Services Research. 2003:38(3):905-18; discussion 919-22.
- Wachter RM, Goldman L The hospitalist movement 5 years later. JAMA. 2002;287:487-94.
- Palmer HC, Armistead NS, Elnicki DM, et al. The effect of a hospitalist service with nurse discharge planner on patient care in an academic teaching hospital. Am J Med. 2001;111:627-32.
Providing Extraordinary Availability
In 1994, Jack Rosenbloom was admitted to an Indiana hospital after suffering a serious heart attack. While in the critical care unit (CCU) of the healthcare facility, he experienced a major relapse, prompting a “code blue” situation. Although the floor nurse called for assistance instantaneously a physician did not arrive in CCU until 1 hour later — too late to save Jack Rosenbloom. Convinced that the immediate presence of a physician could have spared her husband’s life and surprised that round-the-clock, on-site coverage was not required in a hospital setting, Myra Rosenbloom decided to pursue Federal legislation that would mandate such a policy and ensure the safety of all patients in the future. The result was the drafting of The Physician Availability Act, which directs any hospital with at least 100 beds to have a minimum of one physician on duty at all times to exclusively serve non-emergency room patients. In June 2003, Pete Visclosky (D-Indiana) introduced H.R. 2389 to the U.S. House of Representatives; it has since been referred to the Energy and Commerce Committee’s subcommittee on health.
Although it is not clear if or when HR. 2389 might become law, the bill is emblematic of the pressure hospitals are experiencing to provide round-the-clock physician coverage. Hospital administrators are keenly aware of the importance of creating and implementing protective and preventive measures to ensure the best possible quality care and safety for all inpatients. Charles B. Inlander, president of the People’s Medical Society, a consumer advocacy group, emphasizes that patients expect to see a doctor, regardless of the hour or day. “If there is no doctor to treat the patient, it’s like going to a major league baseball game and seeing minor league players,” he says. More important, Inlander notes that the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) is considering the addition of requirements similar to the ones specified in the pending Physician Availability Act (1).
Today, most hospitals use traditional physician on-call systems to provide overnight coverage. These systems are not always effective or efficient for patients, physicians, nursing staff, and other hospital departments. Delay of care may jeopardize a patient’s medical well-being. Nurses become frustrated trying unsuccessfully to locate on-call physicians in a timely fashion in the case of a medical emergency. On-call physicians cannot enjoy a normal lifestyle and may suffer from overwork. The emergency room may experience a backlog of patients waiting for admission until the doctor arrives in the morning, creating logjams for other hospital departments.
Direct and Indirect Value
Hospitalists can alleviate these issues and add direct value to a healthcare facility through the implementation of a 24/7 program. Their positive impact affects patients, first and foremost, as well as various hospital departments and staff, hospital recruitment efforts, and the healthcare facility’s fiscal status.
Emergency Department (ED)
As an on-site fully trained physician, the hospitalist is available to conduct emergency room evaluations and enable the timely admission of patients. By tending to ED cases immediately, the hospitalist can prevent unnecessary delays and ensure efficiency in this department. Also, this prompt action prevents the need for “bridging orders,” whereby an ED physician writes temporary orders until the patient can be seen and admitted in the morning by the primary care physician (PCP). The absence of lag time between an emergent situation and the on-site presence of a physician might mean the difference between short-term treatment/rapid discharge and a lengthy hospital stay.
Admissions
Depending on medical staff bylaws, some hospitals routinely handle late night and early morning admissions over the telephone. In a traditional on-call system, the attending physician may provide orders over the phone to admit a patient following a discussion with the ED physician. Formal evaluation of the patient would not take place until the following morning at rounds or later in the evening after office hours. This practice may result in delays in patient management and often increases the duration of hospitalization.
Healthcare facilities with 24/7 hospital medicine programs operate in “real time” and can evaluate and admit the patient immediately, potentially reducing the length of stay (LOS) and cost per stay, and positively impacting the hospital’s bottom line. As illustrated in Figure 1, Covenant HealthCare System in Michigan collected data after 1 year’s operation of its hospital medicine program and found that the 24/7 coverage shortened the average LOS by 1 day when compared with a traditional, non-24/7 hospitalist program and 1.5 days when compared with a general internist (2). Also, patients that present before midnight incur an additional day of professional fees when seen upon arrival at the hospital by a 24/7 hospitalist. This extraordinary availability realizes a dual benefit: LOS savings and increased professional fee generation.
Inpatient Unit
Regardless of the hour, hospitalists can provide consultations for surgical and medical cases on the inpatient unit. Sudden changes in patient condition, such as fever, chest pain, hypotension, and mental status, can be addressed immediately. Traditionally, these problems might be managed over the phone at the discretion of the covering physician without direct patient evaluation. An on-site 24/7 hospital medicine program provides trained physicians who can personally evaluate the patient and diagnose any developing problems resulting in improved quality of care. From a financial perspective, a hospitalist providing this level of service may result in additional revenue.
Nursing Staff
In May 2001, Sister Mary Roch Rocklage, then chair-elect of the American Hospital Association (AHA), informed the Senate Health, Education, Labor and Pensions Committee that by 2020, this country would need 1.7 million nurses. However, the healthcare industry’s ongoing failure to attract individuals to the nursing profession means that the supply will be 65% short of demand by that time. Troy Hutson, director of legal and clinical policy at the Washington State Hospital Association (WSHA), indicates that the two major reasons that nurses are unhappy in their work environment are a lack of control and voice in their environment and less time spent on patient care.
The advent of 24/7 hospitalists is considered to be one way to improve the situation. Chief nursing officer at Emory Northlake Regional Medical Center in Atlanta, GA, Denise Hook asserts that the round-the-clock presence of a hospitalist benefits the nursing staff by providing support and relieving the burden of making decisions more aptly handled by physicians. She adds that the support of a physician late at night is critical since newer, inexperienced nurses are often assigned to these shifts. Beverly Ventura, vice president of patient care services at Mercy Medical Center in Springfield, MA, notes that the 24/7 coverage by hospitalists “has improved our ability to respond rapidly to crisis and has improved continuity of care for the patients” (3).
Additionally, 24/7 coverage means that physicians can visit more often with patients, reducing the time nurses must spend updating the doctor on the patient’s condition and progress. Nurses find, too, that family members have greater access to physicians involved in 24/7 programs; queries regarding a patient’s status can be answered directly by the doctor, and family conferences can take place more readily allowing the nurse to fulfill her role in other, more productive ways. Marcia Johnson, RN, MN, MHA, Vice President of Patient Care Services at Overlake Hospital Medical Center in Bellevue, WA and board member of the Northwest Organization of Nurse Executives, says, “Nurses who feel they are respected have a voice in care and the management of care. They have a real ‘throughout the day’ working relationship with physicians, and are supported by hospital-based physicians. [They] will be much more willing and able to shoulder the other issues that burden nurses” (3).
Physician Recruitment
The appeal of a 24/7 hospitalist program may also affect a healthcare facility’s ability to successfully recruit quailifled physicians. With the knowledge that inpatients will be under the constant care of a trained on-site hospitalist, a PCP can anticipate a predictable schedule that allows for much better work—life balance.
Changing Times
John R. Nelson, MD, FACP, is co-founder of the National Association of Inpatient Physicians, now the Society of Hospital Medicine (SHM), a hospitalist, and the medical director at Overlake Medical Center. In the 1970s, working as an orderly, he found that, although the census was typically high, the night shift was not very busy. Most patients were routine cases awaiting tests, labs, and other simple procedures the next morning. Today patients are sicker on admission. Rapidly changing status at any time of the day or night presents a real challenge to medical staff. Nelson believes that the on-call system of 25 years ago has outlived its usefulness for patients, community physicians or PCPs and nursing staff. To meet the expectations of all involved, an on-site physician is necessary, he asserts. While PCPs are reluctant to return to the hospital after working a full day, the 24/7 hospitalist, by virtue of his role, expects to tend to patients’ needs and face various medical issues throughout his shift (4).
Mark V. Williams, MD, Director of the Hospital Medicine Unit at Emory University’s School of Medicine, emphasizes that on-site, in-person health care offers a vastly superior model to “phone practice” (5). In addition to providing immediate response — which nurses consider a value-added service — 24/7 hospitalists are able to evaluate firsthand changing medical conditions, says Lawrence Vidrine, the national medical director of inpatient services of Team Health in Knoxville, TN (6).
According to Winthrop Whitcomb, MD, SHM’s other co-founder and director of the hospital medicine program at Mercy Medical Center in Springfield, MA, a “new paradigm” has evolved for the practice of more efficient and effective hospital medicine. It is his perspective that the country is now experiencing a shift from a “push system” to a “pull system.” Inherently ineffective, the former model attempts to “push” the patient into the hospital relying on the attending physician’s availability to come to the hospital for the admission process. The newer “pull” system involves a hospitalist who expects to be called and a facility that has established inpatient capacity. When a patient is ready for admission, the hospitalist “pulls” that individual up through the system since capacity has already been built-in (7).
Leapfrog Initiative
In an effort to improve the safety and quality of care patients receive while in the CCU, the Leapfrog Initiative Group in collaboration with the Health Care Financing Administration (HCFA) and the U.S. Office of Personnel Management set standards to achieve this goal in 1998. According to these principles, physicians are encouraged to have Advanced Cardiac Life Support (ACLS) training and the Fundamentals of Critical Care Support (FCCS) certification, which enable them to adequately and appropriately respond to acute patient status changes. Hospitalists who have earned these certifications can provide a different level of service and generate higher professional fees. At Covenant Health Care in Sagina MI, all hospitalists hold these credentials, according to Stacy Goldsholl, MD, director of Covenant’s hospital medicine program. In such cases, adequately trained hospitalists qualify as Leapfrog intensivist extenders (8). John Kosanovich, Vice President of Medical Affairs, reiterates the importance, both professionally and financially, of compliance with Leapfrog guidelines. In addition to strengthening the bottom line, ACLS/FCCS certified hospitalists contribute to improved quality of patient care (9).
Stakeholder Analysis
A 24/7 hospital medicine program most directly impacts four categories of stakeholders. With patient safety as top priority, closely followed by quality of care, hospitalists who engage in 24/7 coverage programs can effectively and appropriately address the physical, psychological, occupational and fiscal status of the stakeholders in Table 1.
Survey Data/Statistics
SHM conducted a survey that assessed the productivity levels of hospitalists as well as various compensation figures for 2003—2004. Figure 2 lists some facts from that survey related to 24/7 programs (10).
Conclusion
Quality of care and patient safety rank as the primary reasons for implementing a 24/7 program. Patients benefit the most from round-the-clock medical attention as continuity of care increases their chance for quick recovery and reduces the potential for decompensation. Furthermore, length of stay and healthcare costs can be reduced, improving hospital financial performance and throughput.
In this era of increased scrutiny of the healthcare industry, there is a growing expectation that a physician will be available around-the-clock to attend to patients. Myra Rosenbloom’s efforts aspire to make this possibility a reality. The use of hospitalists on a 24/7 basis may serve to alleviate the evolutionary pressure being applied to hospitals and, over the short-term, provide a strategic advantage that appeals to a hospital’s patient community.
Dr. Goldsholl can be contacted at stacygoldsholl@msn.com
References
- Inlander CB. President, People’s Medical Society, Allentown, PA. Personal interview. August 9, 2004.
- Unpublished report, Covenant HealthCare Hospitalist Program FY 2004, Saginaw, MI.
- Freeman L Can hospitalists improve nurse recruitment and retention? The Hospitalist. 2001;5(6):7-8.
- Nelson J. Medical director, hospitalist program at Overlake Medical Center, Bellevue, WA. Personal interview. August 18, 2004.
- Williams MV. Director, Hospital Medicine Unit, Emory University School of Medicine. Email interview. August 13, 2004.
- Vidrine L National medical director, inpatient services Team Health, Knoxville, TN, August 20, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA. Personal interview. August 23, 2004.
- Goldsholl S. Director, hospitalist program, Covenant Health Care, Saginaw, MI. Personal interview. August 23, 2004.
- Kosanovich J. Vice President, Medical Affairs, Covenant Health Care, Saginaw, MI. Personal interview. August 11, 2004.
- Society of Hospital Medicine Productivity and Compensation Survey, 2003-2004.
In 1994, Jack Rosenbloom was admitted to an Indiana hospital after suffering a serious heart attack. While in the critical care unit (CCU) of the healthcare facility, he experienced a major relapse, prompting a “code blue” situation. Although the floor nurse called for assistance instantaneously a physician did not arrive in CCU until 1 hour later — too late to save Jack Rosenbloom. Convinced that the immediate presence of a physician could have spared her husband’s life and surprised that round-the-clock, on-site coverage was not required in a hospital setting, Myra Rosenbloom decided to pursue Federal legislation that would mandate such a policy and ensure the safety of all patients in the future. The result was the drafting of The Physician Availability Act, which directs any hospital with at least 100 beds to have a minimum of one physician on duty at all times to exclusively serve non-emergency room patients. In June 2003, Pete Visclosky (D-Indiana) introduced H.R. 2389 to the U.S. House of Representatives; it has since been referred to the Energy and Commerce Committee’s subcommittee on health.
Although it is not clear if or when HR. 2389 might become law, the bill is emblematic of the pressure hospitals are experiencing to provide round-the-clock physician coverage. Hospital administrators are keenly aware of the importance of creating and implementing protective and preventive measures to ensure the best possible quality care and safety for all inpatients. Charles B. Inlander, president of the People’s Medical Society, a consumer advocacy group, emphasizes that patients expect to see a doctor, regardless of the hour or day. “If there is no doctor to treat the patient, it’s like going to a major league baseball game and seeing minor league players,” he says. More important, Inlander notes that the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) is considering the addition of requirements similar to the ones specified in the pending Physician Availability Act (1).
Today, most hospitals use traditional physician on-call systems to provide overnight coverage. These systems are not always effective or efficient for patients, physicians, nursing staff, and other hospital departments. Delay of care may jeopardize a patient’s medical well-being. Nurses become frustrated trying unsuccessfully to locate on-call physicians in a timely fashion in the case of a medical emergency. On-call physicians cannot enjoy a normal lifestyle and may suffer from overwork. The emergency room may experience a backlog of patients waiting for admission until the doctor arrives in the morning, creating logjams for other hospital departments.
Direct and Indirect Value
Hospitalists can alleviate these issues and add direct value to a healthcare facility through the implementation of a 24/7 program. Their positive impact affects patients, first and foremost, as well as various hospital departments and staff, hospital recruitment efforts, and the healthcare facility’s fiscal status.
Emergency Department (ED)
As an on-site fully trained physician, the hospitalist is available to conduct emergency room evaluations and enable the timely admission of patients. By tending to ED cases immediately, the hospitalist can prevent unnecessary delays and ensure efficiency in this department. Also, this prompt action prevents the need for “bridging orders,” whereby an ED physician writes temporary orders until the patient can be seen and admitted in the morning by the primary care physician (PCP). The absence of lag time between an emergent situation and the on-site presence of a physician might mean the difference between short-term treatment/rapid discharge and a lengthy hospital stay.
Admissions
Depending on medical staff bylaws, some hospitals routinely handle late night and early morning admissions over the telephone. In a traditional on-call system, the attending physician may provide orders over the phone to admit a patient following a discussion with the ED physician. Formal evaluation of the patient would not take place until the following morning at rounds or later in the evening after office hours. This practice may result in delays in patient management and often increases the duration of hospitalization.
Healthcare facilities with 24/7 hospital medicine programs operate in “real time” and can evaluate and admit the patient immediately, potentially reducing the length of stay (LOS) and cost per stay, and positively impacting the hospital’s bottom line. As illustrated in Figure 1, Covenant HealthCare System in Michigan collected data after 1 year’s operation of its hospital medicine program and found that the 24/7 coverage shortened the average LOS by 1 day when compared with a traditional, non-24/7 hospitalist program and 1.5 days when compared with a general internist (2). Also, patients that present before midnight incur an additional day of professional fees when seen upon arrival at the hospital by a 24/7 hospitalist. This extraordinary availability realizes a dual benefit: LOS savings and increased professional fee generation.
Inpatient Unit
Regardless of the hour, hospitalists can provide consultations for surgical and medical cases on the inpatient unit. Sudden changes in patient condition, such as fever, chest pain, hypotension, and mental status, can be addressed immediately. Traditionally, these problems might be managed over the phone at the discretion of the covering physician without direct patient evaluation. An on-site 24/7 hospital medicine program provides trained physicians who can personally evaluate the patient and diagnose any developing problems resulting in improved quality of care. From a financial perspective, a hospitalist providing this level of service may result in additional revenue.
Nursing Staff
In May 2001, Sister Mary Roch Rocklage, then chair-elect of the American Hospital Association (AHA), informed the Senate Health, Education, Labor and Pensions Committee that by 2020, this country would need 1.7 million nurses. However, the healthcare industry’s ongoing failure to attract individuals to the nursing profession means that the supply will be 65% short of demand by that time. Troy Hutson, director of legal and clinical policy at the Washington State Hospital Association (WSHA), indicates that the two major reasons that nurses are unhappy in their work environment are a lack of control and voice in their environment and less time spent on patient care.
The advent of 24/7 hospitalists is considered to be one way to improve the situation. Chief nursing officer at Emory Northlake Regional Medical Center in Atlanta, GA, Denise Hook asserts that the round-the-clock presence of a hospitalist benefits the nursing staff by providing support and relieving the burden of making decisions more aptly handled by physicians. She adds that the support of a physician late at night is critical since newer, inexperienced nurses are often assigned to these shifts. Beverly Ventura, vice president of patient care services at Mercy Medical Center in Springfield, MA, notes that the 24/7 coverage by hospitalists “has improved our ability to respond rapidly to crisis and has improved continuity of care for the patients” (3).
Additionally, 24/7 coverage means that physicians can visit more often with patients, reducing the time nurses must spend updating the doctor on the patient’s condition and progress. Nurses find, too, that family members have greater access to physicians involved in 24/7 programs; queries regarding a patient’s status can be answered directly by the doctor, and family conferences can take place more readily allowing the nurse to fulfill her role in other, more productive ways. Marcia Johnson, RN, MN, MHA, Vice President of Patient Care Services at Overlake Hospital Medical Center in Bellevue, WA and board member of the Northwest Organization of Nurse Executives, says, “Nurses who feel they are respected have a voice in care and the management of care. They have a real ‘throughout the day’ working relationship with physicians, and are supported by hospital-based physicians. [They] will be much more willing and able to shoulder the other issues that burden nurses” (3).
Physician Recruitment
The appeal of a 24/7 hospitalist program may also affect a healthcare facility’s ability to successfully recruit quailifled physicians. With the knowledge that inpatients will be under the constant care of a trained on-site hospitalist, a PCP can anticipate a predictable schedule that allows for much better work—life balance.
Changing Times
John R. Nelson, MD, FACP, is co-founder of the National Association of Inpatient Physicians, now the Society of Hospital Medicine (SHM), a hospitalist, and the medical director at Overlake Medical Center. In the 1970s, working as an orderly, he found that, although the census was typically high, the night shift was not very busy. Most patients were routine cases awaiting tests, labs, and other simple procedures the next morning. Today patients are sicker on admission. Rapidly changing status at any time of the day or night presents a real challenge to medical staff. Nelson believes that the on-call system of 25 years ago has outlived its usefulness for patients, community physicians or PCPs and nursing staff. To meet the expectations of all involved, an on-site physician is necessary, he asserts. While PCPs are reluctant to return to the hospital after working a full day, the 24/7 hospitalist, by virtue of his role, expects to tend to patients’ needs and face various medical issues throughout his shift (4).
Mark V. Williams, MD, Director of the Hospital Medicine Unit at Emory University’s School of Medicine, emphasizes that on-site, in-person health care offers a vastly superior model to “phone practice” (5). In addition to providing immediate response — which nurses consider a value-added service — 24/7 hospitalists are able to evaluate firsthand changing medical conditions, says Lawrence Vidrine, the national medical director of inpatient services of Team Health in Knoxville, TN (6).
According to Winthrop Whitcomb, MD, SHM’s other co-founder and director of the hospital medicine program at Mercy Medical Center in Springfield, MA, a “new paradigm” has evolved for the practice of more efficient and effective hospital medicine. It is his perspective that the country is now experiencing a shift from a “push system” to a “pull system.” Inherently ineffective, the former model attempts to “push” the patient into the hospital relying on the attending physician’s availability to come to the hospital for the admission process. The newer “pull” system involves a hospitalist who expects to be called and a facility that has established inpatient capacity. When a patient is ready for admission, the hospitalist “pulls” that individual up through the system since capacity has already been built-in (7).
Leapfrog Initiative
In an effort to improve the safety and quality of care patients receive while in the CCU, the Leapfrog Initiative Group in collaboration with the Health Care Financing Administration (HCFA) and the U.S. Office of Personnel Management set standards to achieve this goal in 1998. According to these principles, physicians are encouraged to have Advanced Cardiac Life Support (ACLS) training and the Fundamentals of Critical Care Support (FCCS) certification, which enable them to adequately and appropriately respond to acute patient status changes. Hospitalists who have earned these certifications can provide a different level of service and generate higher professional fees. At Covenant Health Care in Sagina MI, all hospitalists hold these credentials, according to Stacy Goldsholl, MD, director of Covenant’s hospital medicine program. In such cases, adequately trained hospitalists qualify as Leapfrog intensivist extenders (8). John Kosanovich, Vice President of Medical Affairs, reiterates the importance, both professionally and financially, of compliance with Leapfrog guidelines. In addition to strengthening the bottom line, ACLS/FCCS certified hospitalists contribute to improved quality of patient care (9).
Stakeholder Analysis
A 24/7 hospital medicine program most directly impacts four categories of stakeholders. With patient safety as top priority, closely followed by quality of care, hospitalists who engage in 24/7 coverage programs can effectively and appropriately address the physical, psychological, occupational and fiscal status of the stakeholders in Table 1.
Survey Data/Statistics
SHM conducted a survey that assessed the productivity levels of hospitalists as well as various compensation figures for 2003—2004. Figure 2 lists some facts from that survey related to 24/7 programs (10).
Conclusion
Quality of care and patient safety rank as the primary reasons for implementing a 24/7 program. Patients benefit the most from round-the-clock medical attention as continuity of care increases their chance for quick recovery and reduces the potential for decompensation. Furthermore, length of stay and healthcare costs can be reduced, improving hospital financial performance and throughput.
In this era of increased scrutiny of the healthcare industry, there is a growing expectation that a physician will be available around-the-clock to attend to patients. Myra Rosenbloom’s efforts aspire to make this possibility a reality. The use of hospitalists on a 24/7 basis may serve to alleviate the evolutionary pressure being applied to hospitals and, over the short-term, provide a strategic advantage that appeals to a hospital’s patient community.
Dr. Goldsholl can be contacted at stacygoldsholl@msn.com
References
- Inlander CB. President, People’s Medical Society, Allentown, PA. Personal interview. August 9, 2004.
- Unpublished report, Covenant HealthCare Hospitalist Program FY 2004, Saginaw, MI.
- Freeman L Can hospitalists improve nurse recruitment and retention? The Hospitalist. 2001;5(6):7-8.
- Nelson J. Medical director, hospitalist program at Overlake Medical Center, Bellevue, WA. Personal interview. August 18, 2004.
- Williams MV. Director, Hospital Medicine Unit, Emory University School of Medicine. Email interview. August 13, 2004.
- Vidrine L National medical director, inpatient services Team Health, Knoxville, TN, August 20, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA. Personal interview. August 23, 2004.
- Goldsholl S. Director, hospitalist program, Covenant Health Care, Saginaw, MI. Personal interview. August 23, 2004.
- Kosanovich J. Vice President, Medical Affairs, Covenant Health Care, Saginaw, MI. Personal interview. August 11, 2004.
- Society of Hospital Medicine Productivity and Compensation Survey, 2003-2004.
In 1994, Jack Rosenbloom was admitted to an Indiana hospital after suffering a serious heart attack. While in the critical care unit (CCU) of the healthcare facility, he experienced a major relapse, prompting a “code blue” situation. Although the floor nurse called for assistance instantaneously a physician did not arrive in CCU until 1 hour later — too late to save Jack Rosenbloom. Convinced that the immediate presence of a physician could have spared her husband’s life and surprised that round-the-clock, on-site coverage was not required in a hospital setting, Myra Rosenbloom decided to pursue Federal legislation that would mandate such a policy and ensure the safety of all patients in the future. The result was the drafting of The Physician Availability Act, which directs any hospital with at least 100 beds to have a minimum of one physician on duty at all times to exclusively serve non-emergency room patients. In June 2003, Pete Visclosky (D-Indiana) introduced H.R. 2389 to the U.S. House of Representatives; it has since been referred to the Energy and Commerce Committee’s subcommittee on health.
Although it is not clear if or when HR. 2389 might become law, the bill is emblematic of the pressure hospitals are experiencing to provide round-the-clock physician coverage. Hospital administrators are keenly aware of the importance of creating and implementing protective and preventive measures to ensure the best possible quality care and safety for all inpatients. Charles B. Inlander, president of the People’s Medical Society, a consumer advocacy group, emphasizes that patients expect to see a doctor, regardless of the hour or day. “If there is no doctor to treat the patient, it’s like going to a major league baseball game and seeing minor league players,” he says. More important, Inlander notes that the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) is considering the addition of requirements similar to the ones specified in the pending Physician Availability Act (1).
Today, most hospitals use traditional physician on-call systems to provide overnight coverage. These systems are not always effective or efficient for patients, physicians, nursing staff, and other hospital departments. Delay of care may jeopardize a patient’s medical well-being. Nurses become frustrated trying unsuccessfully to locate on-call physicians in a timely fashion in the case of a medical emergency. On-call physicians cannot enjoy a normal lifestyle and may suffer from overwork. The emergency room may experience a backlog of patients waiting for admission until the doctor arrives in the morning, creating logjams for other hospital departments.
Direct and Indirect Value
Hospitalists can alleviate these issues and add direct value to a healthcare facility through the implementation of a 24/7 program. Their positive impact affects patients, first and foremost, as well as various hospital departments and staff, hospital recruitment efforts, and the healthcare facility’s fiscal status.
Emergency Department (ED)
As an on-site fully trained physician, the hospitalist is available to conduct emergency room evaluations and enable the timely admission of patients. By tending to ED cases immediately, the hospitalist can prevent unnecessary delays and ensure efficiency in this department. Also, this prompt action prevents the need for “bridging orders,” whereby an ED physician writes temporary orders until the patient can be seen and admitted in the morning by the primary care physician (PCP). The absence of lag time between an emergent situation and the on-site presence of a physician might mean the difference between short-term treatment/rapid discharge and a lengthy hospital stay.
Admissions
Depending on medical staff bylaws, some hospitals routinely handle late night and early morning admissions over the telephone. In a traditional on-call system, the attending physician may provide orders over the phone to admit a patient following a discussion with the ED physician. Formal evaluation of the patient would not take place until the following morning at rounds or later in the evening after office hours. This practice may result in delays in patient management and often increases the duration of hospitalization.
Healthcare facilities with 24/7 hospital medicine programs operate in “real time” and can evaluate and admit the patient immediately, potentially reducing the length of stay (LOS) and cost per stay, and positively impacting the hospital’s bottom line. As illustrated in Figure 1, Covenant HealthCare System in Michigan collected data after 1 year’s operation of its hospital medicine program and found that the 24/7 coverage shortened the average LOS by 1 day when compared with a traditional, non-24/7 hospitalist program and 1.5 days when compared with a general internist (2). Also, patients that present before midnight incur an additional day of professional fees when seen upon arrival at the hospital by a 24/7 hospitalist. This extraordinary availability realizes a dual benefit: LOS savings and increased professional fee generation.
Inpatient Unit
Regardless of the hour, hospitalists can provide consultations for surgical and medical cases on the inpatient unit. Sudden changes in patient condition, such as fever, chest pain, hypotension, and mental status, can be addressed immediately. Traditionally, these problems might be managed over the phone at the discretion of the covering physician without direct patient evaluation. An on-site 24/7 hospital medicine program provides trained physicians who can personally evaluate the patient and diagnose any developing problems resulting in improved quality of care. From a financial perspective, a hospitalist providing this level of service may result in additional revenue.
Nursing Staff
In May 2001, Sister Mary Roch Rocklage, then chair-elect of the American Hospital Association (AHA), informed the Senate Health, Education, Labor and Pensions Committee that by 2020, this country would need 1.7 million nurses. However, the healthcare industry’s ongoing failure to attract individuals to the nursing profession means that the supply will be 65% short of demand by that time. Troy Hutson, director of legal and clinical policy at the Washington State Hospital Association (WSHA), indicates that the two major reasons that nurses are unhappy in their work environment are a lack of control and voice in their environment and less time spent on patient care.
The advent of 24/7 hospitalists is considered to be one way to improve the situation. Chief nursing officer at Emory Northlake Regional Medical Center in Atlanta, GA, Denise Hook asserts that the round-the-clock presence of a hospitalist benefits the nursing staff by providing support and relieving the burden of making decisions more aptly handled by physicians. She adds that the support of a physician late at night is critical since newer, inexperienced nurses are often assigned to these shifts. Beverly Ventura, vice president of patient care services at Mercy Medical Center in Springfield, MA, notes that the 24/7 coverage by hospitalists “has improved our ability to respond rapidly to crisis and has improved continuity of care for the patients” (3).
Additionally, 24/7 coverage means that physicians can visit more often with patients, reducing the time nurses must spend updating the doctor on the patient’s condition and progress. Nurses find, too, that family members have greater access to physicians involved in 24/7 programs; queries regarding a patient’s status can be answered directly by the doctor, and family conferences can take place more readily allowing the nurse to fulfill her role in other, more productive ways. Marcia Johnson, RN, MN, MHA, Vice President of Patient Care Services at Overlake Hospital Medical Center in Bellevue, WA and board member of the Northwest Organization of Nurse Executives, says, “Nurses who feel they are respected have a voice in care and the management of care. They have a real ‘throughout the day’ working relationship with physicians, and are supported by hospital-based physicians. [They] will be much more willing and able to shoulder the other issues that burden nurses” (3).
Physician Recruitment
The appeal of a 24/7 hospitalist program may also affect a healthcare facility’s ability to successfully recruit quailifled physicians. With the knowledge that inpatients will be under the constant care of a trained on-site hospitalist, a PCP can anticipate a predictable schedule that allows for much better work—life balance.
Changing Times
John R. Nelson, MD, FACP, is co-founder of the National Association of Inpatient Physicians, now the Society of Hospital Medicine (SHM), a hospitalist, and the medical director at Overlake Medical Center. In the 1970s, working as an orderly, he found that, although the census was typically high, the night shift was not very busy. Most patients were routine cases awaiting tests, labs, and other simple procedures the next morning. Today patients are sicker on admission. Rapidly changing status at any time of the day or night presents a real challenge to medical staff. Nelson believes that the on-call system of 25 years ago has outlived its usefulness for patients, community physicians or PCPs and nursing staff. To meet the expectations of all involved, an on-site physician is necessary, he asserts. While PCPs are reluctant to return to the hospital after working a full day, the 24/7 hospitalist, by virtue of his role, expects to tend to patients’ needs and face various medical issues throughout his shift (4).
Mark V. Williams, MD, Director of the Hospital Medicine Unit at Emory University’s School of Medicine, emphasizes that on-site, in-person health care offers a vastly superior model to “phone practice” (5). In addition to providing immediate response — which nurses consider a value-added service — 24/7 hospitalists are able to evaluate firsthand changing medical conditions, says Lawrence Vidrine, the national medical director of inpatient services of Team Health in Knoxville, TN (6).
According to Winthrop Whitcomb, MD, SHM’s other co-founder and director of the hospital medicine program at Mercy Medical Center in Springfield, MA, a “new paradigm” has evolved for the practice of more efficient and effective hospital medicine. It is his perspective that the country is now experiencing a shift from a “push system” to a “pull system.” Inherently ineffective, the former model attempts to “push” the patient into the hospital relying on the attending physician’s availability to come to the hospital for the admission process. The newer “pull” system involves a hospitalist who expects to be called and a facility that has established inpatient capacity. When a patient is ready for admission, the hospitalist “pulls” that individual up through the system since capacity has already been built-in (7).
Leapfrog Initiative
In an effort to improve the safety and quality of care patients receive while in the CCU, the Leapfrog Initiative Group in collaboration with the Health Care Financing Administration (HCFA) and the U.S. Office of Personnel Management set standards to achieve this goal in 1998. According to these principles, physicians are encouraged to have Advanced Cardiac Life Support (ACLS) training and the Fundamentals of Critical Care Support (FCCS) certification, which enable them to adequately and appropriately respond to acute patient status changes. Hospitalists who have earned these certifications can provide a different level of service and generate higher professional fees. At Covenant Health Care in Sagina MI, all hospitalists hold these credentials, according to Stacy Goldsholl, MD, director of Covenant’s hospital medicine program. In such cases, adequately trained hospitalists qualify as Leapfrog intensivist extenders (8). John Kosanovich, Vice President of Medical Affairs, reiterates the importance, both professionally and financially, of compliance with Leapfrog guidelines. In addition to strengthening the bottom line, ACLS/FCCS certified hospitalists contribute to improved quality of patient care (9).
Stakeholder Analysis
A 24/7 hospital medicine program most directly impacts four categories of stakeholders. With patient safety as top priority, closely followed by quality of care, hospitalists who engage in 24/7 coverage programs can effectively and appropriately address the physical, psychological, occupational and fiscal status of the stakeholders in Table 1.
Survey Data/Statistics
SHM conducted a survey that assessed the productivity levels of hospitalists as well as various compensation figures for 2003—2004. Figure 2 lists some facts from that survey related to 24/7 programs (10).
Conclusion
Quality of care and patient safety rank as the primary reasons for implementing a 24/7 program. Patients benefit the most from round-the-clock medical attention as continuity of care increases their chance for quick recovery and reduces the potential for decompensation. Furthermore, length of stay and healthcare costs can be reduced, improving hospital financial performance and throughput.
In this era of increased scrutiny of the healthcare industry, there is a growing expectation that a physician will be available around-the-clock to attend to patients. Myra Rosenbloom’s efforts aspire to make this possibility a reality. The use of hospitalists on a 24/7 basis may serve to alleviate the evolutionary pressure being applied to hospitals and, over the short-term, provide a strategic advantage that appeals to a hospital’s patient community.
Dr. Goldsholl can be contacted at stacygoldsholl@msn.com
References
- Inlander CB. President, People’s Medical Society, Allentown, PA. Personal interview. August 9, 2004.
- Unpublished report, Covenant HealthCare Hospitalist Program FY 2004, Saginaw, MI.
- Freeman L Can hospitalists improve nurse recruitment and retention? The Hospitalist. 2001;5(6):7-8.
- Nelson J. Medical director, hospitalist program at Overlake Medical Center, Bellevue, WA. Personal interview. August 18, 2004.
- Williams MV. Director, Hospital Medicine Unit, Emory University School of Medicine. Email interview. August 13, 2004.
- Vidrine L National medical director, inpatient services Team Health, Knoxville, TN, August 20, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA. Personal interview. August 23, 2004.
- Goldsholl S. Director, hospitalist program, Covenant Health Care, Saginaw, MI. Personal interview. August 23, 2004.
- Kosanovich J. Vice President, Medical Affairs, Covenant Health Care, Saginaw, MI. Personal interview. August 11, 2004.
- Society of Hospital Medicine Productivity and Compensation Survey, 2003-2004.
Leading Hospital Medical Staffs
When Robert Lee, MD, an internist affiliated with Iowa Health Physicians, a multi-specialty group in Des Moines, was called to the hospital to see one of his patients, he faced a 50-minute round trip plus additional time to find a parking place and catch an elevator before reaching the inpatient unit. In the time it took for him to see a couple of his patients in the hospital, he could have treated five patients in the office (1).
David McAtee, MD, an osteopath at Murdock Family Medicine, a group practice of eight family-care physicians in Port Charlotte, Florida, estimates its doctors were spending 30% of their time at the hospital caring for only 5% of their patients (2).
With an eye toward enhancing their office practices and offering patients efficient and effective inpatient treatment, both the Des Moines and Port Charlotte medical groups pursued a growing trend in the healthcare industry: they turned to hospitalists. Lee notes that the change allows him to enjoy a more normal lifestyle with his family and enhances his income (1). The Murdock group’s decision to contract with hospitalists in 2003 resulted in an expansion of office hours. With more available time, the group is in the process of developing a series of programs targeting various diseases as a means of educating patients in better self-care. Additionally, McAtee expresses the hope that medical malpractice insurance premiums will decrease as a result of less time spent on inpatient care (2).
Hospitalist Impact on Primary Care Physicians
Primary care physicians (PCPs) do have reservations regarding the involvement of hospitalists in the care of their patients. Some PCPs voice concerns about the potential reduction in income if they opt to use hospitalists. According to one estimate, primary care doctors may incur an average annual decrease in income of $25,000 by forgoing hospital rounds. However, studies indicate that PCPs have the potential to earn as much as $50,000 more by spending time in the office instead of seeing inpatients (3).
Hospitalist programs that offer on-site, 24-hour availability provide other benefits. When a crisis strikes, PCPs may be difficult to reach as they are seeing office patients. The hurricanes that hit Florida in September and October 2004 clearly demonstrated the value of having continuous inpatient care by qualified physicians already at the hospital. Treacherous weather conditions prevented PCPs from driving to the hospital to see their patients. Although the hospital was unable to perform lab tests, surgeries, or diagnostic imaging procedures because of power outages, hospitalists were already on site and stabilized patients with their basic clinical skills (3). Patients who may not have heard of the term “hospitalist” were pleased that a physician was available to answer questions, address unexpected medical issues, and offer immediate support and comfort.
Admittedly, not all PCPs have embraced the hospitalist model. The perception that they might lose skill and prestige by giving up inpatient visits might prevent them from utilizing hospitalist services. In some cases, PCPs might perceive a reduction in continuity of care. These concerns are valid and warrant consideration. However, a well run hospitalist program will keep communication lines open between hospitalists and PCPs, so that patients receive optimal care as both inpatients and outpatients.
Hospitalists and Surgeons/Specialists
Robert T. Trousdale, MD, orthopedic surgeon at the Mayo Clinic in Rochester, MN, spends most of his day in the operating room or evaluating patients for surgery. An expert in hip and knee surgery he admits that many orthopedic surgeons have insufficient knowledge when it comes to treating some of the common medical problems that may occur postoperatively “Hospitalists help us co-manage patients in this area. They bring an increased level of experience to the management of the patient,” he says. Trousdale notes the added benefits of time and hospitalist availability. “I am in the operating room for 5 hours at a time. If a nurse calls to report that one of my patients has developed post-op dizziness or chest pain, I might not be able to see him for 2 hours,” he says. Hospitalists have both the expertise and the availability to address medical issues in a timelier manner and expedite recovery time.
Additionally, Trousdale admits that, although he is quite familiar with the intricacies of the musculoskeletal system, he is less certain of the necessary tests a patient might need postoperatively. “We might take a ‘shotgun’ approach and order 15 expensive tests, which is an unnecessary use of the hospital’s resources,” he says (4).
Jeanne Huddleston, MD, Director of the Inpatient Internal Medicine Program at Mayo Clinic and Assistant Professor of Medicine at the Mayo College of Medicine, led a study to determine the impact hospitalists have on the co-management of patients having hip and knee surgery. The findings, published in 2004, reveal that of 526 patients in the study, more of those managed by hospitalist-orthopedic teams were discharged with no complications (61.6% for hospitalist-orthopedic teams vs. 48.8% for traditional orthopedic surgical teams). Only 30.2% of patients co-managed by hospitalists experienced minor complications, while 44.3% of patients managed by traditional orthopedic surgical teams had similar difficulties. Huddleston notes also that most orthopedic surgeons and nurses responding to a satisfaction survey preferred the hospitalist orthopedic model (5).
Hospitalists and Emergency Department Physicians
Brent R. Asplin, MD, MPH, research director in the department of emergency medicine at Regions Hospital in St. Paul, MN, cites three ways in which hospitalists positively impact the ED: through extraordinary availability, consistent and reliable care, and their focus on the hospital. “Hospitalists are available 24 hours a day,” he says. “It’s nice to know when you send a patient to the floor, there is an experienced physician in-house to take care of them. You do not have to try and reach a PCP on the phone.” He reports that capacity is a major problem for EDs. Bottlenecks result when there are patients who are ready to be admitted from the ED but must wait for other patients to be discharged. Hospitalists are always available to maintain a smooth patient flow and facilitate throughput, according to Asplin.
As a group, hospitalists adhere to a consistent approach to patient care. Once a patient is admitted, efficient, reliable in-house care will ensure a quick recovery and discharge. Asplin says, “Hospitalists are more likely to embrace clinical pathways for the most common clinical diagnoses. This reduces variability across the board and increases patient outcome and flow.” Also, hospitalists focus exclusively on inpatient care, enabling them to devote all their attention to servicing the patient while they are hospitalized without the distractions that might divert a PCP’s concentration. Asplin says, “Regarding clinical care, operations, and quality improvement, it helps to have a group dedicated and focused on the hospital” (6).
In teaching hospitals, residents also benefit from the presence of hospitalists. According to Barbara LeTourneau, MD, an ED physician and professional physician executive consultant also based at Regions, residents have the continuous supervision of experienced practitioners who can answer questions and teach on an ongoing basis. “With hospitalists there is much quicker and better patient care,” she says.
In her role as administrator, LeTourneau has an historical perspective on the delivery of inpatient care at her hospital. Prior to the implementation of hospital medicine programs, positive changes took a longer period of time to reach agreement and execution, she reports. “Having hospitalists here provides one group of experienced physicians who see a large percentage of patients,” says LeTourneau. Managing a significant caseload enables the hospitalist to understand the system in depth. “Hospitalists can provide good feedback and make it easier to implement necessary changes” (11).
Stakeholder Analysis
Studies reveal that hospitalists improve the practices of physicians and several subspecialties in a number of ways. Not only do PCPs benefit from the presence of hospitalists, but other medical specialists, patients, families, and medical facilities gain advantages as well (see Table 1).
Research Studies
Since 1996 when the term hospitalist was first used, a number of studies have been conducted to evaluate the benefits they bring to PCPs and other physicians (see Table 2). In the past decade, the number of hospitalists has increased dramatically, lending credence to their value in an inpatient medical setting. In 2005, the Society of Hospital Medicine (SHM) estimates that there are 12,000 hospitalists in the US.
In a survey by Mitretek Healthcare, researchers asked hospital leaders to rate a number of strategies that impact on hospital-medical staff relations. Sixty-two percent of the leaders surveyed gave hospitalist programs a high rating pertaining to hospital-physician alignment (12). Other studies also support the growing belief that hospitalists can effectively and efficiently enhance physician practices.
Conclusion
Joseph Li, MD, director of the hospitalist program at Beth Israel Deaconess Medical Center in Boston, hopes to build a career based on the belief that hospitalists are leading the way in “preventing medical errors and hospital-acquired infections, managing the complex hospital environment, finding the right transition to home care or rehabilitation, and providing palliative and end-of-life care” (13). As hospital medicine programs become more prevalent and accepted, more and more PCPs are seeing the value in their presence. A major national hospitalist management company surveyed PCPs in five markets on their experiences with hospitalists. The responses revealed a 100% satisfaction rating on the quality of inpatient care (14). In the future, hospitalists like Li will strive to maintain that rating while they help improve physician practices and enhance patient care.
Dr. Kealey can be contacted at burke.tkealey@healthpartners.com
Dr. Vidrine can be contacted at larry_vidrine@teamhealth.com
References
- Jackson C. Doctors find hospitalists save time, money: primary care physicians are seeing that turning over their hospital business allows them to make more income. Amednews.com, February 19, 2001.
- Trendy hospital medicine comes to Charlotte. Sunherald.com, February 13, 2004.
- Landro L. Medicine’s fastest-growing specialty: hospital-bound doctors take the place of your physician; effort to reduce costs, errors. The Wall Street Journal Online, October 6, 2004.
- Trousdale RT, Department of Orthopedics, Mayo Clinic, Rochester, MN. Telephone interview. January 3, 2005.
- Huddleston J, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized controlled trial. Ann Intern Med. 2004;141:28-38.
- Asplin, Brent R., MD, MPH, research director, Department of Emergency Medicine, Regions Hospital, St. Paul, MN. Telephone interview January 5, 2005.
- Auerbach AD, Aronson MD, Davis RB, Phillips RS. How physicians perceive hospitalist services after implementation: anticipation vs. reality. Arch Intern Med. 2003;163:2330-6.
- Auerbach AD, Nelson EA, Lindenauer PK, et al. Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey. Am J Med. 2000;109: 648-53.
- Halpert AP, Pearson SD, LeWine HE, McKean SC. The impact of an inpatient physician program on quality utilization, and satisfaction. Am J Manag Care. 2000; 6: 549-55.
- Fernandez A, Grumbach K, Goitein L, et al. Friend or foe? How primary care physicians perceive hospitalists. Arch Intern Med. 2000;160:2902-8.
- LeTourneau B, emergency department physician, professional physician executive consultant, Regions Hospital, St. Paul, MN. Telephone interview. January 7, 2005.
- McGowan RA. Strengthening hospital-physician relationships. Healthcare Financial Management Association. December 2004. www.hfma.org/publications/HFM_Magazine/business.htm.
- Barnard A. Medical profession, patients have warmed to the ‘hospitalist’. The Boston Globe, January 30, 2002.
- PCPs and hospitalists: a new attitude? Cogent Quarterly, Vol. 1, No. 4, Fall 2001.
When Robert Lee, MD, an internist affiliated with Iowa Health Physicians, a multi-specialty group in Des Moines, was called to the hospital to see one of his patients, he faced a 50-minute round trip plus additional time to find a parking place and catch an elevator before reaching the inpatient unit. In the time it took for him to see a couple of his patients in the hospital, he could have treated five patients in the office (1).
David McAtee, MD, an osteopath at Murdock Family Medicine, a group practice of eight family-care physicians in Port Charlotte, Florida, estimates its doctors were spending 30% of their time at the hospital caring for only 5% of their patients (2).
With an eye toward enhancing their office practices and offering patients efficient and effective inpatient treatment, both the Des Moines and Port Charlotte medical groups pursued a growing trend in the healthcare industry: they turned to hospitalists. Lee notes that the change allows him to enjoy a more normal lifestyle with his family and enhances his income (1). The Murdock group’s decision to contract with hospitalists in 2003 resulted in an expansion of office hours. With more available time, the group is in the process of developing a series of programs targeting various diseases as a means of educating patients in better self-care. Additionally, McAtee expresses the hope that medical malpractice insurance premiums will decrease as a result of less time spent on inpatient care (2).
Hospitalist Impact on Primary Care Physicians
Primary care physicians (PCPs) do have reservations regarding the involvement of hospitalists in the care of their patients. Some PCPs voice concerns about the potential reduction in income if they opt to use hospitalists. According to one estimate, primary care doctors may incur an average annual decrease in income of $25,000 by forgoing hospital rounds. However, studies indicate that PCPs have the potential to earn as much as $50,000 more by spending time in the office instead of seeing inpatients (3).
Hospitalist programs that offer on-site, 24-hour availability provide other benefits. When a crisis strikes, PCPs may be difficult to reach as they are seeing office patients. The hurricanes that hit Florida in September and October 2004 clearly demonstrated the value of having continuous inpatient care by qualified physicians already at the hospital. Treacherous weather conditions prevented PCPs from driving to the hospital to see their patients. Although the hospital was unable to perform lab tests, surgeries, or diagnostic imaging procedures because of power outages, hospitalists were already on site and stabilized patients with their basic clinical skills (3). Patients who may not have heard of the term “hospitalist” were pleased that a physician was available to answer questions, address unexpected medical issues, and offer immediate support and comfort.
Admittedly, not all PCPs have embraced the hospitalist model. The perception that they might lose skill and prestige by giving up inpatient visits might prevent them from utilizing hospitalist services. In some cases, PCPs might perceive a reduction in continuity of care. These concerns are valid and warrant consideration. However, a well run hospitalist program will keep communication lines open between hospitalists and PCPs, so that patients receive optimal care as both inpatients and outpatients.
Hospitalists and Surgeons/Specialists
Robert T. Trousdale, MD, orthopedic surgeon at the Mayo Clinic in Rochester, MN, spends most of his day in the operating room or evaluating patients for surgery. An expert in hip and knee surgery he admits that many orthopedic surgeons have insufficient knowledge when it comes to treating some of the common medical problems that may occur postoperatively “Hospitalists help us co-manage patients in this area. They bring an increased level of experience to the management of the patient,” he says. Trousdale notes the added benefits of time and hospitalist availability. “I am in the operating room for 5 hours at a time. If a nurse calls to report that one of my patients has developed post-op dizziness or chest pain, I might not be able to see him for 2 hours,” he says. Hospitalists have both the expertise and the availability to address medical issues in a timelier manner and expedite recovery time.
Additionally, Trousdale admits that, although he is quite familiar with the intricacies of the musculoskeletal system, he is less certain of the necessary tests a patient might need postoperatively. “We might take a ‘shotgun’ approach and order 15 expensive tests, which is an unnecessary use of the hospital’s resources,” he says (4).
Jeanne Huddleston, MD, Director of the Inpatient Internal Medicine Program at Mayo Clinic and Assistant Professor of Medicine at the Mayo College of Medicine, led a study to determine the impact hospitalists have on the co-management of patients having hip and knee surgery. The findings, published in 2004, reveal that of 526 patients in the study, more of those managed by hospitalist-orthopedic teams were discharged with no complications (61.6% for hospitalist-orthopedic teams vs. 48.8% for traditional orthopedic surgical teams). Only 30.2% of patients co-managed by hospitalists experienced minor complications, while 44.3% of patients managed by traditional orthopedic surgical teams had similar difficulties. Huddleston notes also that most orthopedic surgeons and nurses responding to a satisfaction survey preferred the hospitalist orthopedic model (5).
Hospitalists and Emergency Department Physicians
Brent R. Asplin, MD, MPH, research director in the department of emergency medicine at Regions Hospital in St. Paul, MN, cites three ways in which hospitalists positively impact the ED: through extraordinary availability, consistent and reliable care, and their focus on the hospital. “Hospitalists are available 24 hours a day,” he says. “It’s nice to know when you send a patient to the floor, there is an experienced physician in-house to take care of them. You do not have to try and reach a PCP on the phone.” He reports that capacity is a major problem for EDs. Bottlenecks result when there are patients who are ready to be admitted from the ED but must wait for other patients to be discharged. Hospitalists are always available to maintain a smooth patient flow and facilitate throughput, according to Asplin.
As a group, hospitalists adhere to a consistent approach to patient care. Once a patient is admitted, efficient, reliable in-house care will ensure a quick recovery and discharge. Asplin says, “Hospitalists are more likely to embrace clinical pathways for the most common clinical diagnoses. This reduces variability across the board and increases patient outcome and flow.” Also, hospitalists focus exclusively on inpatient care, enabling them to devote all their attention to servicing the patient while they are hospitalized without the distractions that might divert a PCP’s concentration. Asplin says, “Regarding clinical care, operations, and quality improvement, it helps to have a group dedicated and focused on the hospital” (6).
In teaching hospitals, residents also benefit from the presence of hospitalists. According to Barbara LeTourneau, MD, an ED physician and professional physician executive consultant also based at Regions, residents have the continuous supervision of experienced practitioners who can answer questions and teach on an ongoing basis. “With hospitalists there is much quicker and better patient care,” she says.
In her role as administrator, LeTourneau has an historical perspective on the delivery of inpatient care at her hospital. Prior to the implementation of hospital medicine programs, positive changes took a longer period of time to reach agreement and execution, she reports. “Having hospitalists here provides one group of experienced physicians who see a large percentage of patients,” says LeTourneau. Managing a significant caseload enables the hospitalist to understand the system in depth. “Hospitalists can provide good feedback and make it easier to implement necessary changes” (11).
Stakeholder Analysis
Studies reveal that hospitalists improve the practices of physicians and several subspecialties in a number of ways. Not only do PCPs benefit from the presence of hospitalists, but other medical specialists, patients, families, and medical facilities gain advantages as well (see Table 1).
Research Studies
Since 1996 when the term hospitalist was first used, a number of studies have been conducted to evaluate the benefits they bring to PCPs and other physicians (see Table 2). In the past decade, the number of hospitalists has increased dramatically, lending credence to their value in an inpatient medical setting. In 2005, the Society of Hospital Medicine (SHM) estimates that there are 12,000 hospitalists in the US.
In a survey by Mitretek Healthcare, researchers asked hospital leaders to rate a number of strategies that impact on hospital-medical staff relations. Sixty-two percent of the leaders surveyed gave hospitalist programs a high rating pertaining to hospital-physician alignment (12). Other studies also support the growing belief that hospitalists can effectively and efficiently enhance physician practices.
Conclusion
Joseph Li, MD, director of the hospitalist program at Beth Israel Deaconess Medical Center in Boston, hopes to build a career based on the belief that hospitalists are leading the way in “preventing medical errors and hospital-acquired infections, managing the complex hospital environment, finding the right transition to home care or rehabilitation, and providing palliative and end-of-life care” (13). As hospital medicine programs become more prevalent and accepted, more and more PCPs are seeing the value in their presence. A major national hospitalist management company surveyed PCPs in five markets on their experiences with hospitalists. The responses revealed a 100% satisfaction rating on the quality of inpatient care (14). In the future, hospitalists like Li will strive to maintain that rating while they help improve physician practices and enhance patient care.
Dr. Kealey can be contacted at burke.tkealey@healthpartners.com
Dr. Vidrine can be contacted at larry_vidrine@teamhealth.com
References
- Jackson C. Doctors find hospitalists save time, money: primary care physicians are seeing that turning over their hospital business allows them to make more income. Amednews.com, February 19, 2001.
- Trendy hospital medicine comes to Charlotte. Sunherald.com, February 13, 2004.
- Landro L. Medicine’s fastest-growing specialty: hospital-bound doctors take the place of your physician; effort to reduce costs, errors. The Wall Street Journal Online, October 6, 2004.
- Trousdale RT, Department of Orthopedics, Mayo Clinic, Rochester, MN. Telephone interview. January 3, 2005.
- Huddleston J, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized controlled trial. Ann Intern Med. 2004;141:28-38.
- Asplin, Brent R., MD, MPH, research director, Department of Emergency Medicine, Regions Hospital, St. Paul, MN. Telephone interview January 5, 2005.
- Auerbach AD, Aronson MD, Davis RB, Phillips RS. How physicians perceive hospitalist services after implementation: anticipation vs. reality. Arch Intern Med. 2003;163:2330-6.
- Auerbach AD, Nelson EA, Lindenauer PK, et al. Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey. Am J Med. 2000;109: 648-53.
- Halpert AP, Pearson SD, LeWine HE, McKean SC. The impact of an inpatient physician program on quality utilization, and satisfaction. Am J Manag Care. 2000; 6: 549-55.
- Fernandez A, Grumbach K, Goitein L, et al. Friend or foe? How primary care physicians perceive hospitalists. Arch Intern Med. 2000;160:2902-8.
- LeTourneau B, emergency department physician, professional physician executive consultant, Regions Hospital, St. Paul, MN. Telephone interview. January 7, 2005.
- McGowan RA. Strengthening hospital-physician relationships. Healthcare Financial Management Association. December 2004. www.hfma.org/publications/HFM_Magazine/business.htm.
- Barnard A. Medical profession, patients have warmed to the ‘hospitalist’. The Boston Globe, January 30, 2002.
- PCPs and hospitalists: a new attitude? Cogent Quarterly, Vol. 1, No. 4, Fall 2001.
When Robert Lee, MD, an internist affiliated with Iowa Health Physicians, a multi-specialty group in Des Moines, was called to the hospital to see one of his patients, he faced a 50-minute round trip plus additional time to find a parking place and catch an elevator before reaching the inpatient unit. In the time it took for him to see a couple of his patients in the hospital, he could have treated five patients in the office (1).
David McAtee, MD, an osteopath at Murdock Family Medicine, a group practice of eight family-care physicians in Port Charlotte, Florida, estimates its doctors were spending 30% of their time at the hospital caring for only 5% of their patients (2).
With an eye toward enhancing their office practices and offering patients efficient and effective inpatient treatment, both the Des Moines and Port Charlotte medical groups pursued a growing trend in the healthcare industry: they turned to hospitalists. Lee notes that the change allows him to enjoy a more normal lifestyle with his family and enhances his income (1). The Murdock group’s decision to contract with hospitalists in 2003 resulted in an expansion of office hours. With more available time, the group is in the process of developing a series of programs targeting various diseases as a means of educating patients in better self-care. Additionally, McAtee expresses the hope that medical malpractice insurance premiums will decrease as a result of less time spent on inpatient care (2).
Hospitalist Impact on Primary Care Physicians
Primary care physicians (PCPs) do have reservations regarding the involvement of hospitalists in the care of their patients. Some PCPs voice concerns about the potential reduction in income if they opt to use hospitalists. According to one estimate, primary care doctors may incur an average annual decrease in income of $25,000 by forgoing hospital rounds. However, studies indicate that PCPs have the potential to earn as much as $50,000 more by spending time in the office instead of seeing inpatients (3).
Hospitalist programs that offer on-site, 24-hour availability provide other benefits. When a crisis strikes, PCPs may be difficult to reach as they are seeing office patients. The hurricanes that hit Florida in September and October 2004 clearly demonstrated the value of having continuous inpatient care by qualified physicians already at the hospital. Treacherous weather conditions prevented PCPs from driving to the hospital to see their patients. Although the hospital was unable to perform lab tests, surgeries, or diagnostic imaging procedures because of power outages, hospitalists were already on site and stabilized patients with their basic clinical skills (3). Patients who may not have heard of the term “hospitalist” were pleased that a physician was available to answer questions, address unexpected medical issues, and offer immediate support and comfort.
Admittedly, not all PCPs have embraced the hospitalist model. The perception that they might lose skill and prestige by giving up inpatient visits might prevent them from utilizing hospitalist services. In some cases, PCPs might perceive a reduction in continuity of care. These concerns are valid and warrant consideration. However, a well run hospitalist program will keep communication lines open between hospitalists and PCPs, so that patients receive optimal care as both inpatients and outpatients.
Hospitalists and Surgeons/Specialists
Robert T. Trousdale, MD, orthopedic surgeon at the Mayo Clinic in Rochester, MN, spends most of his day in the operating room or evaluating patients for surgery. An expert in hip and knee surgery he admits that many orthopedic surgeons have insufficient knowledge when it comes to treating some of the common medical problems that may occur postoperatively “Hospitalists help us co-manage patients in this area. They bring an increased level of experience to the management of the patient,” he says. Trousdale notes the added benefits of time and hospitalist availability. “I am in the operating room for 5 hours at a time. If a nurse calls to report that one of my patients has developed post-op dizziness or chest pain, I might not be able to see him for 2 hours,” he says. Hospitalists have both the expertise and the availability to address medical issues in a timelier manner and expedite recovery time.
Additionally, Trousdale admits that, although he is quite familiar with the intricacies of the musculoskeletal system, he is less certain of the necessary tests a patient might need postoperatively. “We might take a ‘shotgun’ approach and order 15 expensive tests, which is an unnecessary use of the hospital’s resources,” he says (4).
Jeanne Huddleston, MD, Director of the Inpatient Internal Medicine Program at Mayo Clinic and Assistant Professor of Medicine at the Mayo College of Medicine, led a study to determine the impact hospitalists have on the co-management of patients having hip and knee surgery. The findings, published in 2004, reveal that of 526 patients in the study, more of those managed by hospitalist-orthopedic teams were discharged with no complications (61.6% for hospitalist-orthopedic teams vs. 48.8% for traditional orthopedic surgical teams). Only 30.2% of patients co-managed by hospitalists experienced minor complications, while 44.3% of patients managed by traditional orthopedic surgical teams had similar difficulties. Huddleston notes also that most orthopedic surgeons and nurses responding to a satisfaction survey preferred the hospitalist orthopedic model (5).
Hospitalists and Emergency Department Physicians
Brent R. Asplin, MD, MPH, research director in the department of emergency medicine at Regions Hospital in St. Paul, MN, cites three ways in which hospitalists positively impact the ED: through extraordinary availability, consistent and reliable care, and their focus on the hospital. “Hospitalists are available 24 hours a day,” he says. “It’s nice to know when you send a patient to the floor, there is an experienced physician in-house to take care of them. You do not have to try and reach a PCP on the phone.” He reports that capacity is a major problem for EDs. Bottlenecks result when there are patients who are ready to be admitted from the ED but must wait for other patients to be discharged. Hospitalists are always available to maintain a smooth patient flow and facilitate throughput, according to Asplin.
As a group, hospitalists adhere to a consistent approach to patient care. Once a patient is admitted, efficient, reliable in-house care will ensure a quick recovery and discharge. Asplin says, “Hospitalists are more likely to embrace clinical pathways for the most common clinical diagnoses. This reduces variability across the board and increases patient outcome and flow.” Also, hospitalists focus exclusively on inpatient care, enabling them to devote all their attention to servicing the patient while they are hospitalized without the distractions that might divert a PCP’s concentration. Asplin says, “Regarding clinical care, operations, and quality improvement, it helps to have a group dedicated and focused on the hospital” (6).
In teaching hospitals, residents also benefit from the presence of hospitalists. According to Barbara LeTourneau, MD, an ED physician and professional physician executive consultant also based at Regions, residents have the continuous supervision of experienced practitioners who can answer questions and teach on an ongoing basis. “With hospitalists there is much quicker and better patient care,” she says.
In her role as administrator, LeTourneau has an historical perspective on the delivery of inpatient care at her hospital. Prior to the implementation of hospital medicine programs, positive changes took a longer period of time to reach agreement and execution, she reports. “Having hospitalists here provides one group of experienced physicians who see a large percentage of patients,” says LeTourneau. Managing a significant caseload enables the hospitalist to understand the system in depth. “Hospitalists can provide good feedback and make it easier to implement necessary changes” (11).
Stakeholder Analysis
Studies reveal that hospitalists improve the practices of physicians and several subspecialties in a number of ways. Not only do PCPs benefit from the presence of hospitalists, but other medical specialists, patients, families, and medical facilities gain advantages as well (see Table 1).
Research Studies
Since 1996 when the term hospitalist was first used, a number of studies have been conducted to evaluate the benefits they bring to PCPs and other physicians (see Table 2). In the past decade, the number of hospitalists has increased dramatically, lending credence to their value in an inpatient medical setting. In 2005, the Society of Hospital Medicine (SHM) estimates that there are 12,000 hospitalists in the US.
In a survey by Mitretek Healthcare, researchers asked hospital leaders to rate a number of strategies that impact on hospital-medical staff relations. Sixty-two percent of the leaders surveyed gave hospitalist programs a high rating pertaining to hospital-physician alignment (12). Other studies also support the growing belief that hospitalists can effectively and efficiently enhance physician practices.
Conclusion
Joseph Li, MD, director of the hospitalist program at Beth Israel Deaconess Medical Center in Boston, hopes to build a career based on the belief that hospitalists are leading the way in “preventing medical errors and hospital-acquired infections, managing the complex hospital environment, finding the right transition to home care or rehabilitation, and providing palliative and end-of-life care” (13). As hospital medicine programs become more prevalent and accepted, more and more PCPs are seeing the value in their presence. A major national hospitalist management company surveyed PCPs in five markets on their experiences with hospitalists. The responses revealed a 100% satisfaction rating on the quality of inpatient care (14). In the future, hospitalists like Li will strive to maintain that rating while they help improve physician practices and enhance patient care.
Dr. Kealey can be contacted at burke.tkealey@healthpartners.com
Dr. Vidrine can be contacted at larry_vidrine@teamhealth.com
References
- Jackson C. Doctors find hospitalists save time, money: primary care physicians are seeing that turning over their hospital business allows them to make more income. Amednews.com, February 19, 2001.
- Trendy hospital medicine comes to Charlotte. Sunherald.com, February 13, 2004.
- Landro L. Medicine’s fastest-growing specialty: hospital-bound doctors take the place of your physician; effort to reduce costs, errors. The Wall Street Journal Online, October 6, 2004.
- Trousdale RT, Department of Orthopedics, Mayo Clinic, Rochester, MN. Telephone interview. January 3, 2005.
- Huddleston J, Long KH, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty: a randomized controlled trial. Ann Intern Med. 2004;141:28-38.
- Asplin, Brent R., MD, MPH, research director, Department of Emergency Medicine, Regions Hospital, St. Paul, MN. Telephone interview January 5, 2005.
- Auerbach AD, Aronson MD, Davis RB, Phillips RS. How physicians perceive hospitalist services after implementation: anticipation vs. reality. Arch Intern Med. 2003;163:2330-6.
- Auerbach AD, Nelson EA, Lindenauer PK, et al. Physician attitudes toward and prevalence of the hospitalist model of care: results of a national survey. Am J Med. 2000;109: 648-53.
- Halpert AP, Pearson SD, LeWine HE, McKean SC. The impact of an inpatient physician program on quality utilization, and satisfaction. Am J Manag Care. 2000; 6: 549-55.
- Fernandez A, Grumbach K, Goitein L, et al. Friend or foe? How primary care physicians perceive hospitalists. Arch Intern Med. 2000;160:2902-8.
- LeTourneau B, emergency department physician, professional physician executive consultant, Regions Hospital, St. Paul, MN. Telephone interview. January 7, 2005.
- McGowan RA. Strengthening hospital-physician relationships. Healthcare Financial Management Association. December 2004. www.hfma.org/publications/HFM_Magazine/business.htm.
- Barnard A. Medical profession, patients have warmed to the ‘hospitalist’. The Boston Globe, January 30, 2002.
- PCPs and hospitalists: a new attitude? Cogent Quarterly, Vol. 1, No. 4, Fall 2001.