User login
Providing Extraordinary Availability
In 1994, Jack Rosenbloom was admitted to an Indiana hospital after suffering a serious heart attack. While in the critical care unit (CCU) of the healthcare facility, he experienced a major relapse, prompting a “code blue” situation. Although the floor nurse called for assistance instantaneously a physician did not arrive in CCU until 1 hour later — too late to save Jack Rosenbloom. Convinced that the immediate presence of a physician could have spared her husband’s life and surprised that round-the-clock, on-site coverage was not required in a hospital setting, Myra Rosenbloom decided to pursue Federal legislation that would mandate such a policy and ensure the safety of all patients in the future. The result was the drafting of The Physician Availability Act, which directs any hospital with at least 100 beds to have a minimum of one physician on duty at all times to exclusively serve non-emergency room patients. In June 2003, Pete Visclosky (D-Indiana) introduced H.R. 2389 to the U.S. House of Representatives; it has since been referred to the Energy and Commerce Committee’s subcommittee on health.
Although it is not clear if or when HR. 2389 might become law, the bill is emblematic of the pressure hospitals are experiencing to provide round-the-clock physician coverage. Hospital administrators are keenly aware of the importance of creating and implementing protective and preventive measures to ensure the best possible quality care and safety for all inpatients. Charles B. Inlander, president of the People’s Medical Society, a consumer advocacy group, emphasizes that patients expect to see a doctor, regardless of the hour or day. “If there is no doctor to treat the patient, it’s like going to a major league baseball game and seeing minor league players,” he says. More important, Inlander notes that the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) is considering the addition of requirements similar to the ones specified in the pending Physician Availability Act (1).
Today, most hospitals use traditional physician on-call systems to provide overnight coverage. These systems are not always effective or efficient for patients, physicians, nursing staff, and other hospital departments. Delay of care may jeopardize a patient’s medical well-being. Nurses become frustrated trying unsuccessfully to locate on-call physicians in a timely fashion in the case of a medical emergency. On-call physicians cannot enjoy a normal lifestyle and may suffer from overwork. The emergency room may experience a backlog of patients waiting for admission until the doctor arrives in the morning, creating logjams for other hospital departments.
Direct and Indirect Value
Hospitalists can alleviate these issues and add direct value to a healthcare facility through the implementation of a 24/7 program. Their positive impact affects patients, first and foremost, as well as various hospital departments and staff, hospital recruitment efforts, and the healthcare facility’s fiscal status.
Emergency Department (ED)
As an on-site fully trained physician, the hospitalist is available to conduct emergency room evaluations and enable the timely admission of patients. By tending to ED cases immediately, the hospitalist can prevent unnecessary delays and ensure efficiency in this department. Also, this prompt action prevents the need for “bridging orders,” whereby an ED physician writes temporary orders until the patient can be seen and admitted in the morning by the primary care physician (PCP). The absence of lag time between an emergent situation and the on-site presence of a physician might mean the difference between short-term treatment/rapid discharge and a lengthy hospital stay.
Admissions
Depending on medical staff bylaws, some hospitals routinely handle late night and early morning admissions over the telephone. In a traditional on-call system, the attending physician may provide orders over the phone to admit a patient following a discussion with the ED physician. Formal evaluation of the patient would not take place until the following morning at rounds or later in the evening after office hours. This practice may result in delays in patient management and often increases the duration of hospitalization.
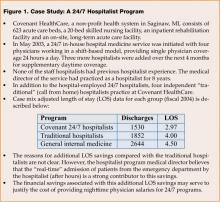
Healthcare facilities with 24/7 hospital medicine programs operate in “real time” and can evaluate and admit the patient immediately, potentially reducing the length of stay (LOS) and cost per stay, and positively impacting the hospital’s bottom line. As illustrated in Figure 1, Covenant HealthCare System in Michigan collected data after 1 year’s operation of its hospital medicine program and found that the 24/7 coverage shortened the average LOS by 1 day when compared with a traditional, non-24/7 hospitalist program and 1.5 days when compared with a general internist (2). Also, patients that present before midnight incur an additional day of professional fees when seen upon arrival at the hospital by a 24/7 hospitalist. This extraordinary availability realizes a dual benefit: LOS savings and increased professional fee generation.
Inpatient Unit
Regardless of the hour, hospitalists can provide consultations for surgical and medical cases on the inpatient unit. Sudden changes in patient condition, such as fever, chest pain, hypotension, and mental status, can be addressed immediately. Traditionally, these problems might be managed over the phone at the discretion of the covering physician without direct patient evaluation. An on-site 24/7 hospital medicine program provides trained physicians who can personally evaluate the patient and diagnose any developing problems resulting in improved quality of care. From a financial perspective, a hospitalist providing this level of service may result in additional revenue.
Nursing Staff
In May 2001, Sister Mary Roch Rocklage, then chair-elect of the American Hospital Association (AHA), informed the Senate Health, Education, Labor and Pensions Committee that by 2020, this country would need 1.7 million nurses. However, the healthcare industry’s ongoing failure to attract individuals to the nursing profession means that the supply will be 65% short of demand by that time. Troy Hutson, director of legal and clinical policy at the Washington State Hospital Association (WSHA), indicates that the two major reasons that nurses are unhappy in their work environment are a lack of control and voice in their environment and less time spent on patient care.
The advent of 24/7 hospitalists is considered to be one way to improve the situation. Chief nursing officer at Emory Northlake Regional Medical Center in Atlanta, GA, Denise Hook asserts that the round-the-clock presence of a hospitalist benefits the nursing staff by providing support and relieving the burden of making decisions more aptly handled by physicians. She adds that the support of a physician late at night is critical since newer, inexperienced nurses are often assigned to these shifts. Beverly Ventura, vice president of patient care services at Mercy Medical Center in Springfield, MA, notes that the 24/7 coverage by hospitalists “has improved our ability to respond rapidly to crisis and has improved continuity of care for the patients” (3).
Additionally, 24/7 coverage means that physicians can visit more often with patients, reducing the time nurses must spend updating the doctor on the patient’s condition and progress. Nurses find, too, that family members have greater access to physicians involved in 24/7 programs; queries regarding a patient’s status can be answered directly by the doctor, and family conferences can take place more readily allowing the nurse to fulfill her role in other, more productive ways. Marcia Johnson, RN, MN, MHA, Vice President of Patient Care Services at Overlake Hospital Medical Center in Bellevue, WA and board member of the Northwest Organization of Nurse Executives, says, “Nurses who feel they are respected have a voice in care and the management of care. They have a real ‘throughout the day’ working relationship with physicians, and are supported by hospital-based physicians. [They] will be much more willing and able to shoulder the other issues that burden nurses” (3).
Physician Recruitment
The appeal of a 24/7 hospitalist program may also affect a healthcare facility’s ability to successfully recruit quailifled physicians. With the knowledge that inpatients will be under the constant care of a trained on-site hospitalist, a PCP can anticipate a predictable schedule that allows for much better work—life balance.
Changing Times
John R. Nelson, MD, FACP, is co-founder of the National Association of Inpatient Physicians, now the Society of Hospital Medicine (SHM), a hospitalist, and the medical director at Overlake Medical Center. In the 1970s, working as an orderly, he found that, although the census was typically high, the night shift was not very busy. Most patients were routine cases awaiting tests, labs, and other simple procedures the next morning. Today patients are sicker on admission. Rapidly changing status at any time of the day or night presents a real challenge to medical staff. Nelson believes that the on-call system of 25 years ago has outlived its usefulness for patients, community physicians or PCPs and nursing staff. To meet the expectations of all involved, an on-site physician is necessary, he asserts. While PCPs are reluctant to return to the hospital after working a full day, the 24/7 hospitalist, by virtue of his role, expects to tend to patients’ needs and face various medical issues throughout his shift (4).
Mark V. Williams, MD, Director of the Hospital Medicine Unit at Emory University’s School of Medicine, emphasizes that on-site, in-person health care offers a vastly superior model to “phone practice” (5). In addition to providing immediate response — which nurses consider a value-added service — 24/7 hospitalists are able to evaluate firsthand changing medical conditions, says Lawrence Vidrine, the national medical director of inpatient services of Team Health in Knoxville, TN (6).
According to Winthrop Whitcomb, MD, SHM’s other co-founder and director of the hospital medicine program at Mercy Medical Center in Springfield, MA, a “new paradigm” has evolved for the practice of more efficient and effective hospital medicine. It is his perspective that the country is now experiencing a shift from a “push system” to a “pull system.” Inherently ineffective, the former model attempts to “push” the patient into the hospital relying on the attending physician’s availability to come to the hospital for the admission process. The newer “pull” system involves a hospitalist who expects to be called and a facility that has established inpatient capacity. When a patient is ready for admission, the hospitalist “pulls” that individual up through the system since capacity has already been built-in (7).
Leapfrog Initiative
In an effort to improve the safety and quality of care patients receive while in the CCU, the Leapfrog Initiative Group in collaboration with the Health Care Financing Administration (HCFA) and the U.S. Office of Personnel Management set standards to achieve this goal in 1998. According to these principles, physicians are encouraged to have Advanced Cardiac Life Support (ACLS) training and the Fundamentals of Critical Care Support (FCCS) certification, which enable them to adequately and appropriately respond to acute patient status changes. Hospitalists who have earned these certifications can provide a different level of service and generate higher professional fees. At Covenant Health Care in Sagina MI, all hospitalists hold these credentials, according to Stacy Goldsholl, MD, director of Covenant’s hospital medicine program. In such cases, adequately trained hospitalists qualify as Leapfrog intensivist extenders (8). John Kosanovich, Vice President of Medical Affairs, reiterates the importance, both professionally and financially, of compliance with Leapfrog guidelines. In addition to strengthening the bottom line, ACLS/FCCS certified hospitalists contribute to improved quality of patient care (9).
Stakeholder Analysis
A 24/7 hospital medicine program most directly impacts four categories of stakeholders. With patient safety as top priority, closely followed by quality of care, hospitalists who engage in 24/7 coverage programs can effectively and appropriately address the physical, psychological, occupational and fiscal status of the stakeholders in Table 1.
Survey Data/Statistics
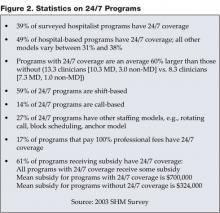
SHM conducted a survey that assessed the productivity levels of hospitalists as well as various compensation figures for 2003—2004. Figure 2 lists some facts from that survey related to 24/7 programs (10).
Conclusion
Quality of care and patient safety rank as the primary reasons for implementing a 24/7 program. Patients benefit the most from round-the-clock medical attention as continuity of care increases their chance for quick recovery and reduces the potential for decompensation. Furthermore, length of stay and healthcare costs can be reduced, improving hospital financial performance and throughput.
In this era of increased scrutiny of the healthcare industry, there is a growing expectation that a physician will be available around-the-clock to attend to patients. Myra Rosenbloom’s efforts aspire to make this possibility a reality. The use of hospitalists on a 24/7 basis may serve to alleviate the evolutionary pressure being applied to hospitals and, over the short-term, provide a strategic advantage that appeals to a hospital’s patient community.
Dr. Goldsholl can be contacted at stacygoldsholl@msn.com
References
- Inlander CB. President, People’s Medical Society, Allentown, PA. Personal interview. August 9, 2004.
- Unpublished report, Covenant HealthCare Hospitalist Program FY 2004, Saginaw, MI.
- Freeman L Can hospitalists improve nurse recruitment and retention? The Hospitalist. 2001;5(6):7-8.
- Nelson J. Medical director, hospitalist program at Overlake Medical Center, Bellevue, WA. Personal interview. August 18, 2004.
- Williams MV. Director, Hospital Medicine Unit, Emory University School of Medicine. Email interview. August 13, 2004.
- Vidrine L National medical director, inpatient services Team Health, Knoxville, TN, August 20, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA. Personal interview. August 23, 2004.
- Goldsholl S. Director, hospitalist program, Covenant Health Care, Saginaw, MI. Personal interview. August 23, 2004.
- Kosanovich J. Vice President, Medical Affairs, Covenant Health Care, Saginaw, MI. Personal interview. August 11, 2004.
- Society of Hospital Medicine Productivity and Compensation Survey, 2003-2004.
In 1994, Jack Rosenbloom was admitted to an Indiana hospital after suffering a serious heart attack. While in the critical care unit (CCU) of the healthcare facility, he experienced a major relapse, prompting a “code blue” situation. Although the floor nurse called for assistance instantaneously a physician did not arrive in CCU until 1 hour later — too late to save Jack Rosenbloom. Convinced that the immediate presence of a physician could have spared her husband’s life and surprised that round-the-clock, on-site coverage was not required in a hospital setting, Myra Rosenbloom decided to pursue Federal legislation that would mandate such a policy and ensure the safety of all patients in the future. The result was the drafting of The Physician Availability Act, which directs any hospital with at least 100 beds to have a minimum of one physician on duty at all times to exclusively serve non-emergency room patients. In June 2003, Pete Visclosky (D-Indiana) introduced H.R. 2389 to the U.S. House of Representatives; it has since been referred to the Energy and Commerce Committee’s subcommittee on health.
Although it is not clear if or when HR. 2389 might become law, the bill is emblematic of the pressure hospitals are experiencing to provide round-the-clock physician coverage. Hospital administrators are keenly aware of the importance of creating and implementing protective and preventive measures to ensure the best possible quality care and safety for all inpatients. Charles B. Inlander, president of the People’s Medical Society, a consumer advocacy group, emphasizes that patients expect to see a doctor, regardless of the hour or day. “If there is no doctor to treat the patient, it’s like going to a major league baseball game and seeing minor league players,” he says. More important, Inlander notes that the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) is considering the addition of requirements similar to the ones specified in the pending Physician Availability Act (1).
Today, most hospitals use traditional physician on-call systems to provide overnight coverage. These systems are not always effective or efficient for patients, physicians, nursing staff, and other hospital departments. Delay of care may jeopardize a patient’s medical well-being. Nurses become frustrated trying unsuccessfully to locate on-call physicians in a timely fashion in the case of a medical emergency. On-call physicians cannot enjoy a normal lifestyle and may suffer from overwork. The emergency room may experience a backlog of patients waiting for admission until the doctor arrives in the morning, creating logjams for other hospital departments.
Direct and Indirect Value
Hospitalists can alleviate these issues and add direct value to a healthcare facility through the implementation of a 24/7 program. Their positive impact affects patients, first and foremost, as well as various hospital departments and staff, hospital recruitment efforts, and the healthcare facility’s fiscal status.
Emergency Department (ED)
As an on-site fully trained physician, the hospitalist is available to conduct emergency room evaluations and enable the timely admission of patients. By tending to ED cases immediately, the hospitalist can prevent unnecessary delays and ensure efficiency in this department. Also, this prompt action prevents the need for “bridging orders,” whereby an ED physician writes temporary orders until the patient can be seen and admitted in the morning by the primary care physician (PCP). The absence of lag time between an emergent situation and the on-site presence of a physician might mean the difference between short-term treatment/rapid discharge and a lengthy hospital stay.
Admissions
Depending on medical staff bylaws, some hospitals routinely handle late night and early morning admissions over the telephone. In a traditional on-call system, the attending physician may provide orders over the phone to admit a patient following a discussion with the ED physician. Formal evaluation of the patient would not take place until the following morning at rounds or later in the evening after office hours. This practice may result in delays in patient management and often increases the duration of hospitalization.
Healthcare facilities with 24/7 hospital medicine programs operate in “real time” and can evaluate and admit the patient immediately, potentially reducing the length of stay (LOS) and cost per stay, and positively impacting the hospital’s bottom line. As illustrated in Figure 1, Covenant HealthCare System in Michigan collected data after 1 year’s operation of its hospital medicine program and found that the 24/7 coverage shortened the average LOS by 1 day when compared with a traditional, non-24/7 hospitalist program and 1.5 days when compared with a general internist (2). Also, patients that present before midnight incur an additional day of professional fees when seen upon arrival at the hospital by a 24/7 hospitalist. This extraordinary availability realizes a dual benefit: LOS savings and increased professional fee generation.
Inpatient Unit
Regardless of the hour, hospitalists can provide consultations for surgical and medical cases on the inpatient unit. Sudden changes in patient condition, such as fever, chest pain, hypotension, and mental status, can be addressed immediately. Traditionally, these problems might be managed over the phone at the discretion of the covering physician without direct patient evaluation. An on-site 24/7 hospital medicine program provides trained physicians who can personally evaluate the patient and diagnose any developing problems resulting in improved quality of care. From a financial perspective, a hospitalist providing this level of service may result in additional revenue.
Nursing Staff
In May 2001, Sister Mary Roch Rocklage, then chair-elect of the American Hospital Association (AHA), informed the Senate Health, Education, Labor and Pensions Committee that by 2020, this country would need 1.7 million nurses. However, the healthcare industry’s ongoing failure to attract individuals to the nursing profession means that the supply will be 65% short of demand by that time. Troy Hutson, director of legal and clinical policy at the Washington State Hospital Association (WSHA), indicates that the two major reasons that nurses are unhappy in their work environment are a lack of control and voice in their environment and less time spent on patient care.
The advent of 24/7 hospitalists is considered to be one way to improve the situation. Chief nursing officer at Emory Northlake Regional Medical Center in Atlanta, GA, Denise Hook asserts that the round-the-clock presence of a hospitalist benefits the nursing staff by providing support and relieving the burden of making decisions more aptly handled by physicians. She adds that the support of a physician late at night is critical since newer, inexperienced nurses are often assigned to these shifts. Beverly Ventura, vice president of patient care services at Mercy Medical Center in Springfield, MA, notes that the 24/7 coverage by hospitalists “has improved our ability to respond rapidly to crisis and has improved continuity of care for the patients” (3).
Additionally, 24/7 coverage means that physicians can visit more often with patients, reducing the time nurses must spend updating the doctor on the patient’s condition and progress. Nurses find, too, that family members have greater access to physicians involved in 24/7 programs; queries regarding a patient’s status can be answered directly by the doctor, and family conferences can take place more readily allowing the nurse to fulfill her role in other, more productive ways. Marcia Johnson, RN, MN, MHA, Vice President of Patient Care Services at Overlake Hospital Medical Center in Bellevue, WA and board member of the Northwest Organization of Nurse Executives, says, “Nurses who feel they are respected have a voice in care and the management of care. They have a real ‘throughout the day’ working relationship with physicians, and are supported by hospital-based physicians. [They] will be much more willing and able to shoulder the other issues that burden nurses” (3).
Physician Recruitment
The appeal of a 24/7 hospitalist program may also affect a healthcare facility’s ability to successfully recruit quailifled physicians. With the knowledge that inpatients will be under the constant care of a trained on-site hospitalist, a PCP can anticipate a predictable schedule that allows for much better work—life balance.
Changing Times
John R. Nelson, MD, FACP, is co-founder of the National Association of Inpatient Physicians, now the Society of Hospital Medicine (SHM), a hospitalist, and the medical director at Overlake Medical Center. In the 1970s, working as an orderly, he found that, although the census was typically high, the night shift was not very busy. Most patients were routine cases awaiting tests, labs, and other simple procedures the next morning. Today patients are sicker on admission. Rapidly changing status at any time of the day or night presents a real challenge to medical staff. Nelson believes that the on-call system of 25 years ago has outlived its usefulness for patients, community physicians or PCPs and nursing staff. To meet the expectations of all involved, an on-site physician is necessary, he asserts. While PCPs are reluctant to return to the hospital after working a full day, the 24/7 hospitalist, by virtue of his role, expects to tend to patients’ needs and face various medical issues throughout his shift (4).
Mark V. Williams, MD, Director of the Hospital Medicine Unit at Emory University’s School of Medicine, emphasizes that on-site, in-person health care offers a vastly superior model to “phone practice” (5). In addition to providing immediate response — which nurses consider a value-added service — 24/7 hospitalists are able to evaluate firsthand changing medical conditions, says Lawrence Vidrine, the national medical director of inpatient services of Team Health in Knoxville, TN (6).
According to Winthrop Whitcomb, MD, SHM’s other co-founder and director of the hospital medicine program at Mercy Medical Center in Springfield, MA, a “new paradigm” has evolved for the practice of more efficient and effective hospital medicine. It is his perspective that the country is now experiencing a shift from a “push system” to a “pull system.” Inherently ineffective, the former model attempts to “push” the patient into the hospital relying on the attending physician’s availability to come to the hospital for the admission process. The newer “pull” system involves a hospitalist who expects to be called and a facility that has established inpatient capacity. When a patient is ready for admission, the hospitalist “pulls” that individual up through the system since capacity has already been built-in (7).
Leapfrog Initiative
In an effort to improve the safety and quality of care patients receive while in the CCU, the Leapfrog Initiative Group in collaboration with the Health Care Financing Administration (HCFA) and the U.S. Office of Personnel Management set standards to achieve this goal in 1998. According to these principles, physicians are encouraged to have Advanced Cardiac Life Support (ACLS) training and the Fundamentals of Critical Care Support (FCCS) certification, which enable them to adequately and appropriately respond to acute patient status changes. Hospitalists who have earned these certifications can provide a different level of service and generate higher professional fees. At Covenant Health Care in Sagina MI, all hospitalists hold these credentials, according to Stacy Goldsholl, MD, director of Covenant’s hospital medicine program. In such cases, adequately trained hospitalists qualify as Leapfrog intensivist extenders (8). John Kosanovich, Vice President of Medical Affairs, reiterates the importance, both professionally and financially, of compliance with Leapfrog guidelines. In addition to strengthening the bottom line, ACLS/FCCS certified hospitalists contribute to improved quality of patient care (9).
Stakeholder Analysis
A 24/7 hospital medicine program most directly impacts four categories of stakeholders. With patient safety as top priority, closely followed by quality of care, hospitalists who engage in 24/7 coverage programs can effectively and appropriately address the physical, psychological, occupational and fiscal status of the stakeholders in Table 1.
Survey Data/Statistics
SHM conducted a survey that assessed the productivity levels of hospitalists as well as various compensation figures for 2003—2004. Figure 2 lists some facts from that survey related to 24/7 programs (10).
Conclusion
Quality of care and patient safety rank as the primary reasons for implementing a 24/7 program. Patients benefit the most from round-the-clock medical attention as continuity of care increases their chance for quick recovery and reduces the potential for decompensation. Furthermore, length of stay and healthcare costs can be reduced, improving hospital financial performance and throughput.
In this era of increased scrutiny of the healthcare industry, there is a growing expectation that a physician will be available around-the-clock to attend to patients. Myra Rosenbloom’s efforts aspire to make this possibility a reality. The use of hospitalists on a 24/7 basis may serve to alleviate the evolutionary pressure being applied to hospitals and, over the short-term, provide a strategic advantage that appeals to a hospital’s patient community.
Dr. Goldsholl can be contacted at stacygoldsholl@msn.com
References
- Inlander CB. President, People’s Medical Society, Allentown, PA. Personal interview. August 9, 2004.
- Unpublished report, Covenant HealthCare Hospitalist Program FY 2004, Saginaw, MI.
- Freeman L Can hospitalists improve nurse recruitment and retention? The Hospitalist. 2001;5(6):7-8.
- Nelson J. Medical director, hospitalist program at Overlake Medical Center, Bellevue, WA. Personal interview. August 18, 2004.
- Williams MV. Director, Hospital Medicine Unit, Emory University School of Medicine. Email interview. August 13, 2004.
- Vidrine L National medical director, inpatient services Team Health, Knoxville, TN, August 20, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA. Personal interview. August 23, 2004.
- Goldsholl S. Director, hospitalist program, Covenant Health Care, Saginaw, MI. Personal interview. August 23, 2004.
- Kosanovich J. Vice President, Medical Affairs, Covenant Health Care, Saginaw, MI. Personal interview. August 11, 2004.
- Society of Hospital Medicine Productivity and Compensation Survey, 2003-2004.
In 1994, Jack Rosenbloom was admitted to an Indiana hospital after suffering a serious heart attack. While in the critical care unit (CCU) of the healthcare facility, he experienced a major relapse, prompting a “code blue” situation. Although the floor nurse called for assistance instantaneously a physician did not arrive in CCU until 1 hour later — too late to save Jack Rosenbloom. Convinced that the immediate presence of a physician could have spared her husband’s life and surprised that round-the-clock, on-site coverage was not required in a hospital setting, Myra Rosenbloom decided to pursue Federal legislation that would mandate such a policy and ensure the safety of all patients in the future. The result was the drafting of The Physician Availability Act, which directs any hospital with at least 100 beds to have a minimum of one physician on duty at all times to exclusively serve non-emergency room patients. In June 2003, Pete Visclosky (D-Indiana) introduced H.R. 2389 to the U.S. House of Representatives; it has since been referred to the Energy and Commerce Committee’s subcommittee on health.
Although it is not clear if or when HR. 2389 might become law, the bill is emblematic of the pressure hospitals are experiencing to provide round-the-clock physician coverage. Hospital administrators are keenly aware of the importance of creating and implementing protective and preventive measures to ensure the best possible quality care and safety for all inpatients. Charles B. Inlander, president of the People’s Medical Society, a consumer advocacy group, emphasizes that patients expect to see a doctor, regardless of the hour or day. “If there is no doctor to treat the patient, it’s like going to a major league baseball game and seeing minor league players,” he says. More important, Inlander notes that the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) is considering the addition of requirements similar to the ones specified in the pending Physician Availability Act (1).
Today, most hospitals use traditional physician on-call systems to provide overnight coverage. These systems are not always effective or efficient for patients, physicians, nursing staff, and other hospital departments. Delay of care may jeopardize a patient’s medical well-being. Nurses become frustrated trying unsuccessfully to locate on-call physicians in a timely fashion in the case of a medical emergency. On-call physicians cannot enjoy a normal lifestyle and may suffer from overwork. The emergency room may experience a backlog of patients waiting for admission until the doctor arrives in the morning, creating logjams for other hospital departments.
Direct and Indirect Value
Hospitalists can alleviate these issues and add direct value to a healthcare facility through the implementation of a 24/7 program. Their positive impact affects patients, first and foremost, as well as various hospital departments and staff, hospital recruitment efforts, and the healthcare facility’s fiscal status.
Emergency Department (ED)
As an on-site fully trained physician, the hospitalist is available to conduct emergency room evaluations and enable the timely admission of patients. By tending to ED cases immediately, the hospitalist can prevent unnecessary delays and ensure efficiency in this department. Also, this prompt action prevents the need for “bridging orders,” whereby an ED physician writes temporary orders until the patient can be seen and admitted in the morning by the primary care physician (PCP). The absence of lag time between an emergent situation and the on-site presence of a physician might mean the difference between short-term treatment/rapid discharge and a lengthy hospital stay.
Admissions
Depending on medical staff bylaws, some hospitals routinely handle late night and early morning admissions over the telephone. In a traditional on-call system, the attending physician may provide orders over the phone to admit a patient following a discussion with the ED physician. Formal evaluation of the patient would not take place until the following morning at rounds or later in the evening after office hours. This practice may result in delays in patient management and often increases the duration of hospitalization.
Healthcare facilities with 24/7 hospital medicine programs operate in “real time” and can evaluate and admit the patient immediately, potentially reducing the length of stay (LOS) and cost per stay, and positively impacting the hospital’s bottom line. As illustrated in Figure 1, Covenant HealthCare System in Michigan collected data after 1 year’s operation of its hospital medicine program and found that the 24/7 coverage shortened the average LOS by 1 day when compared with a traditional, non-24/7 hospitalist program and 1.5 days when compared with a general internist (2). Also, patients that present before midnight incur an additional day of professional fees when seen upon arrival at the hospital by a 24/7 hospitalist. This extraordinary availability realizes a dual benefit: LOS savings and increased professional fee generation.
Inpatient Unit
Regardless of the hour, hospitalists can provide consultations for surgical and medical cases on the inpatient unit. Sudden changes in patient condition, such as fever, chest pain, hypotension, and mental status, can be addressed immediately. Traditionally, these problems might be managed over the phone at the discretion of the covering physician without direct patient evaluation. An on-site 24/7 hospital medicine program provides trained physicians who can personally evaluate the patient and diagnose any developing problems resulting in improved quality of care. From a financial perspective, a hospitalist providing this level of service may result in additional revenue.
Nursing Staff
In May 2001, Sister Mary Roch Rocklage, then chair-elect of the American Hospital Association (AHA), informed the Senate Health, Education, Labor and Pensions Committee that by 2020, this country would need 1.7 million nurses. However, the healthcare industry’s ongoing failure to attract individuals to the nursing profession means that the supply will be 65% short of demand by that time. Troy Hutson, director of legal and clinical policy at the Washington State Hospital Association (WSHA), indicates that the two major reasons that nurses are unhappy in their work environment are a lack of control and voice in their environment and less time spent on patient care.
The advent of 24/7 hospitalists is considered to be one way to improve the situation. Chief nursing officer at Emory Northlake Regional Medical Center in Atlanta, GA, Denise Hook asserts that the round-the-clock presence of a hospitalist benefits the nursing staff by providing support and relieving the burden of making decisions more aptly handled by physicians. She adds that the support of a physician late at night is critical since newer, inexperienced nurses are often assigned to these shifts. Beverly Ventura, vice president of patient care services at Mercy Medical Center in Springfield, MA, notes that the 24/7 coverage by hospitalists “has improved our ability to respond rapidly to crisis and has improved continuity of care for the patients” (3).
Additionally, 24/7 coverage means that physicians can visit more often with patients, reducing the time nurses must spend updating the doctor on the patient’s condition and progress. Nurses find, too, that family members have greater access to physicians involved in 24/7 programs; queries regarding a patient’s status can be answered directly by the doctor, and family conferences can take place more readily allowing the nurse to fulfill her role in other, more productive ways. Marcia Johnson, RN, MN, MHA, Vice President of Patient Care Services at Overlake Hospital Medical Center in Bellevue, WA and board member of the Northwest Organization of Nurse Executives, says, “Nurses who feel they are respected have a voice in care and the management of care. They have a real ‘throughout the day’ working relationship with physicians, and are supported by hospital-based physicians. [They] will be much more willing and able to shoulder the other issues that burden nurses” (3).
Physician Recruitment
The appeal of a 24/7 hospitalist program may also affect a healthcare facility’s ability to successfully recruit quailifled physicians. With the knowledge that inpatients will be under the constant care of a trained on-site hospitalist, a PCP can anticipate a predictable schedule that allows for much better work—life balance.
Changing Times
John R. Nelson, MD, FACP, is co-founder of the National Association of Inpatient Physicians, now the Society of Hospital Medicine (SHM), a hospitalist, and the medical director at Overlake Medical Center. In the 1970s, working as an orderly, he found that, although the census was typically high, the night shift was not very busy. Most patients were routine cases awaiting tests, labs, and other simple procedures the next morning. Today patients are sicker on admission. Rapidly changing status at any time of the day or night presents a real challenge to medical staff. Nelson believes that the on-call system of 25 years ago has outlived its usefulness for patients, community physicians or PCPs and nursing staff. To meet the expectations of all involved, an on-site physician is necessary, he asserts. While PCPs are reluctant to return to the hospital after working a full day, the 24/7 hospitalist, by virtue of his role, expects to tend to patients’ needs and face various medical issues throughout his shift (4).
Mark V. Williams, MD, Director of the Hospital Medicine Unit at Emory University’s School of Medicine, emphasizes that on-site, in-person health care offers a vastly superior model to “phone practice” (5). In addition to providing immediate response — which nurses consider a value-added service — 24/7 hospitalists are able to evaluate firsthand changing medical conditions, says Lawrence Vidrine, the national medical director of inpatient services of Team Health in Knoxville, TN (6).
According to Winthrop Whitcomb, MD, SHM’s other co-founder and director of the hospital medicine program at Mercy Medical Center in Springfield, MA, a “new paradigm” has evolved for the practice of more efficient and effective hospital medicine. It is his perspective that the country is now experiencing a shift from a “push system” to a “pull system.” Inherently ineffective, the former model attempts to “push” the patient into the hospital relying on the attending physician’s availability to come to the hospital for the admission process. The newer “pull” system involves a hospitalist who expects to be called and a facility that has established inpatient capacity. When a patient is ready for admission, the hospitalist “pulls” that individual up through the system since capacity has already been built-in (7).
Leapfrog Initiative
In an effort to improve the safety and quality of care patients receive while in the CCU, the Leapfrog Initiative Group in collaboration with the Health Care Financing Administration (HCFA) and the U.S. Office of Personnel Management set standards to achieve this goal in 1998. According to these principles, physicians are encouraged to have Advanced Cardiac Life Support (ACLS) training and the Fundamentals of Critical Care Support (FCCS) certification, which enable them to adequately and appropriately respond to acute patient status changes. Hospitalists who have earned these certifications can provide a different level of service and generate higher professional fees. At Covenant Health Care in Sagina MI, all hospitalists hold these credentials, according to Stacy Goldsholl, MD, director of Covenant’s hospital medicine program. In such cases, adequately trained hospitalists qualify as Leapfrog intensivist extenders (8). John Kosanovich, Vice President of Medical Affairs, reiterates the importance, both professionally and financially, of compliance with Leapfrog guidelines. In addition to strengthening the bottom line, ACLS/FCCS certified hospitalists contribute to improved quality of patient care (9).
Stakeholder Analysis
A 24/7 hospital medicine program most directly impacts four categories of stakeholders. With patient safety as top priority, closely followed by quality of care, hospitalists who engage in 24/7 coverage programs can effectively and appropriately address the physical, psychological, occupational and fiscal status of the stakeholders in Table 1.
Survey Data/Statistics
SHM conducted a survey that assessed the productivity levels of hospitalists as well as various compensation figures for 2003—2004. Figure 2 lists some facts from that survey related to 24/7 programs (10).
Conclusion
Quality of care and patient safety rank as the primary reasons for implementing a 24/7 program. Patients benefit the most from round-the-clock medical attention as continuity of care increases their chance for quick recovery and reduces the potential for decompensation. Furthermore, length of stay and healthcare costs can be reduced, improving hospital financial performance and throughput.
In this era of increased scrutiny of the healthcare industry, there is a growing expectation that a physician will be available around-the-clock to attend to patients. Myra Rosenbloom’s efforts aspire to make this possibility a reality. The use of hospitalists on a 24/7 basis may serve to alleviate the evolutionary pressure being applied to hospitals and, over the short-term, provide a strategic advantage that appeals to a hospital’s patient community.
Dr. Goldsholl can be contacted at stacygoldsholl@msn.com
References
- Inlander CB. President, People’s Medical Society, Allentown, PA. Personal interview. August 9, 2004.
- Unpublished report, Covenant HealthCare Hospitalist Program FY 2004, Saginaw, MI.
- Freeman L Can hospitalists improve nurse recruitment and retention? The Hospitalist. 2001;5(6):7-8.
- Nelson J. Medical director, hospitalist program at Overlake Medical Center, Bellevue, WA. Personal interview. August 18, 2004.
- Williams MV. Director, Hospital Medicine Unit, Emory University School of Medicine. Email interview. August 13, 2004.
- Vidrine L National medical director, inpatient services Team Health, Knoxville, TN, August 20, 2004.
- Whitcomb WF. Director, Mercy Inpatient Medicine Service, Mercy Medical Center, Springfield, MA. Personal interview. August 23, 2004.
- Goldsholl S. Director, hospitalist program, Covenant Health Care, Saginaw, MI. Personal interview. August 23, 2004.
- Kosanovich J. Vice President, Medical Affairs, Covenant Health Care, Saginaw, MI. Personal interview. August 11, 2004.
- Society of Hospital Medicine Productivity and Compensation Survey, 2003-2004.