User login
A 57-year-old woman with no previous medical history was admitted with weakness. The patient complained of 2 months of ascending bilateral lower extremity weakness followed by subjective “numbness” of both legs. She had a normal lumbosacral MRI as an outpatient and presented to the ED with progressive symptoms. She denied back pain, bowel or bladder problems, diplopia, ataxia, or confusion. As well, there were no fevers, chills, muscle pain, or weight loss. She had no risk factors for HIV and no toxic exposures.
On admission, her vital signs were normal and her general physical exam was unremarkable. Her neurologic exam was notable for diffuse symmetric 3/5 bilateral lower extremity weakness and symmetric bilateral sensory loss in a “stocking” distribution. She had bilateral lower extremity hyperreflexia and plantar reflexes were extensor bilaterally. She had normal upper extremities, cranial nerves, and mental status. Screening laboratories including fasting glucose, B12, RPR, TSH, HIV, SPEP, and UPEP were negative. A repeat lumbosacral MRI and a lumbar puncture were nondiagnostic.
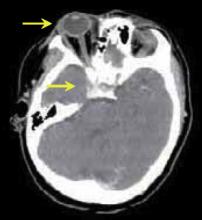
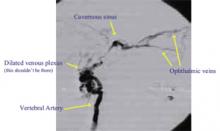
While hospitalized, the patient suffered progressive ascending weakness involving the upper extremities and the diaphragm, necessitating intubation. She was treated with high-dose steroids, IVIG, and plasmapheresis for the possibility of Guillain-Barre or transverse myelitis; there was no change in her symptoms. With no clear diagnosis, on hospital day 10, she complained of diplopia and was found to have right eye chemosis, proptosis, right abducens nerve palsy, and a loud bruit over the right eye. A CT scan revealed dilated right ophthalmic veins and an engorged cavernous sinus (Figure 1). A cerebral angiogram was performed and showed a distal right vertebral arteriovenous fistula (Figure 2), and an MRI showed increased signal in the entire cord secondary to venous hypertension.
What is the diagnosis?
Vertebral Arterio-Venous Fistula (AVF) with arterialized venous drainage to the cavernous sinus, ophthalmic veins, and the cervical epidural veins leading to her ocular symptoms and a cervical myelopathy.
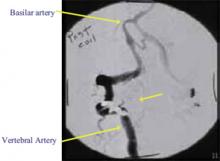
She had no history of trauma and the AVF was thought to be spontaneous. She underwent successful transarterial embolization of the right vertebral artery (see Figure 3). Her ocular symptoms rapidly improved and she was transferred to a rehabilitation facility with improving motor and sensory function.
Discussion: Vertebral arteriovenous fistulas (AVFs) are rare vascular malformations characterized by abnormal shunting between the extracranial vertebral artery and a neighboring vein. Vertebral AVFs are most often secondary to trauma including penetrating gunshot or stab wounds to the neck. Fibromuscular dysplasia and neurofibromatosis are predisposing conditions but vertebral AVFs can be spontaneous as in this case. Patients with vertebral AVFs may present with tinnitus, but frequently they have no symptoms and their fistulas are discovered as cervical bruits on routine auscultation. Neurologic syndromes in the setting of a vertebral AVF are rare and typically secondary to arterialization of venous drainage leading to local ischemia and nerve damage. There are case reports of vertigo and vertebrobasilar insufficiency, cervical radiculopathy related to nerve-root compression from engorged vertebral veins, and cervical myelopathy from venous hypertension similar to this patient. As well, there is only one case report of a vertebral AVF leading to exophthalmos, chemosis, and a bruit, mimicking a carotid-cavernous fistula. This is the first reported case of a vertebral AVF leading to both cervical cord and ocular pathology.
Vertebral AVFs can be suspected based on CT and MRI findings, but angiography is the gold standard for diagnosis. Transarterial embolization is the safest and most effective treatment, allowing for occlusion of the fistula while maintaining patency of the vertebral artery. If treated expediently, most patients experience total recovery.
Dr. Baudendistel can be contacted at BaudenT@sutterhealth.org.
References
- Ammirati M, Mirzai S, Samii M. Vertebral arteriovenous fistulae: report of two cases and review of the literature. Acta Neurochir. 1989;99:122-6.
- Gobin YP, Duckwiler GR, Vinuela F. Direct arteriovenous fistulas: diagnosis and intervention. Neuroimaging Clin North Am. 1998;8:425-43.
- Halbach VV, Higashida RT, Hieshima GB. Treatment of vertebral arteriovenous fistulas. AJR. 1988;150:405-12.
A 57-year-old woman with no previous medical history was admitted with weakness. The patient complained of 2 months of ascending bilateral lower extremity weakness followed by subjective “numbness” of both legs. She had a normal lumbosacral MRI as an outpatient and presented to the ED with progressive symptoms. She denied back pain, bowel or bladder problems, diplopia, ataxia, or confusion. As well, there were no fevers, chills, muscle pain, or weight loss. She had no risk factors for HIV and no toxic exposures.
On admission, her vital signs were normal and her general physical exam was unremarkable. Her neurologic exam was notable for diffuse symmetric 3/5 bilateral lower extremity weakness and symmetric bilateral sensory loss in a “stocking” distribution. She had bilateral lower extremity hyperreflexia and plantar reflexes were extensor bilaterally. She had normal upper extremities, cranial nerves, and mental status. Screening laboratories including fasting glucose, B12, RPR, TSH, HIV, SPEP, and UPEP were negative. A repeat lumbosacral MRI and a lumbar puncture were nondiagnostic.
While hospitalized, the patient suffered progressive ascending weakness involving the upper extremities and the diaphragm, necessitating intubation. She was treated with high-dose steroids, IVIG, and plasmapheresis for the possibility of Guillain-Barre or transverse myelitis; there was no change in her symptoms. With no clear diagnosis, on hospital day 10, she complained of diplopia and was found to have right eye chemosis, proptosis, right abducens nerve palsy, and a loud bruit over the right eye. A CT scan revealed dilated right ophthalmic veins and an engorged cavernous sinus (Figure 1). A cerebral angiogram was performed and showed a distal right vertebral arteriovenous fistula (Figure 2), and an MRI showed increased signal in the entire cord secondary to venous hypertension.
What is the diagnosis?
Vertebral Arterio-Venous Fistula (AVF) with arterialized venous drainage to the cavernous sinus, ophthalmic veins, and the cervical epidural veins leading to her ocular symptoms and a cervical myelopathy.
She had no history of trauma and the AVF was thought to be spontaneous. She underwent successful transarterial embolization of the right vertebral artery (see Figure 3). Her ocular symptoms rapidly improved and she was transferred to a rehabilitation facility with improving motor and sensory function.
Discussion: Vertebral arteriovenous fistulas (AVFs) are rare vascular malformations characterized by abnormal shunting between the extracranial vertebral artery and a neighboring vein. Vertebral AVFs are most often secondary to trauma including penetrating gunshot or stab wounds to the neck. Fibromuscular dysplasia and neurofibromatosis are predisposing conditions but vertebral AVFs can be spontaneous as in this case. Patients with vertebral AVFs may present with tinnitus, but frequently they have no symptoms and their fistulas are discovered as cervical bruits on routine auscultation. Neurologic syndromes in the setting of a vertebral AVF are rare and typically secondary to arterialization of venous drainage leading to local ischemia and nerve damage. There are case reports of vertigo and vertebrobasilar insufficiency, cervical radiculopathy related to nerve-root compression from engorged vertebral veins, and cervical myelopathy from venous hypertension similar to this patient. As well, there is only one case report of a vertebral AVF leading to exophthalmos, chemosis, and a bruit, mimicking a carotid-cavernous fistula. This is the first reported case of a vertebral AVF leading to both cervical cord and ocular pathology.
Vertebral AVFs can be suspected based on CT and MRI findings, but angiography is the gold standard for diagnosis. Transarterial embolization is the safest and most effective treatment, allowing for occlusion of the fistula while maintaining patency of the vertebral artery. If treated expediently, most patients experience total recovery.
Dr. Baudendistel can be contacted at BaudenT@sutterhealth.org.
References
- Ammirati M, Mirzai S, Samii M. Vertebral arteriovenous fistulae: report of two cases and review of the literature. Acta Neurochir. 1989;99:122-6.
- Gobin YP, Duckwiler GR, Vinuela F. Direct arteriovenous fistulas: diagnosis and intervention. Neuroimaging Clin North Am. 1998;8:425-43.
- Halbach VV, Higashida RT, Hieshima GB. Treatment of vertebral arteriovenous fistulas. AJR. 1988;150:405-12.
A 57-year-old woman with no previous medical history was admitted with weakness. The patient complained of 2 months of ascending bilateral lower extremity weakness followed by subjective “numbness” of both legs. She had a normal lumbosacral MRI as an outpatient and presented to the ED with progressive symptoms. She denied back pain, bowel or bladder problems, diplopia, ataxia, or confusion. As well, there were no fevers, chills, muscle pain, or weight loss. She had no risk factors for HIV and no toxic exposures.
On admission, her vital signs were normal and her general physical exam was unremarkable. Her neurologic exam was notable for diffuse symmetric 3/5 bilateral lower extremity weakness and symmetric bilateral sensory loss in a “stocking” distribution. She had bilateral lower extremity hyperreflexia and plantar reflexes were extensor bilaterally. She had normal upper extremities, cranial nerves, and mental status. Screening laboratories including fasting glucose, B12, RPR, TSH, HIV, SPEP, and UPEP were negative. A repeat lumbosacral MRI and a lumbar puncture were nondiagnostic.
While hospitalized, the patient suffered progressive ascending weakness involving the upper extremities and the diaphragm, necessitating intubation. She was treated with high-dose steroids, IVIG, and plasmapheresis for the possibility of Guillain-Barre or transverse myelitis; there was no change in her symptoms. With no clear diagnosis, on hospital day 10, she complained of diplopia and was found to have right eye chemosis, proptosis, right abducens nerve palsy, and a loud bruit over the right eye. A CT scan revealed dilated right ophthalmic veins and an engorged cavernous sinus (Figure 1). A cerebral angiogram was performed and showed a distal right vertebral arteriovenous fistula (Figure 2), and an MRI showed increased signal in the entire cord secondary to venous hypertension.
What is the diagnosis?
Vertebral Arterio-Venous Fistula (AVF) with arterialized venous drainage to the cavernous sinus, ophthalmic veins, and the cervical epidural veins leading to her ocular symptoms and a cervical myelopathy.
She had no history of trauma and the AVF was thought to be spontaneous. She underwent successful transarterial embolization of the right vertebral artery (see Figure 3). Her ocular symptoms rapidly improved and she was transferred to a rehabilitation facility with improving motor and sensory function.
Discussion: Vertebral arteriovenous fistulas (AVFs) are rare vascular malformations characterized by abnormal shunting between the extracranial vertebral artery and a neighboring vein. Vertebral AVFs are most often secondary to trauma including penetrating gunshot or stab wounds to the neck. Fibromuscular dysplasia and neurofibromatosis are predisposing conditions but vertebral AVFs can be spontaneous as in this case. Patients with vertebral AVFs may present with tinnitus, but frequently they have no symptoms and their fistulas are discovered as cervical bruits on routine auscultation. Neurologic syndromes in the setting of a vertebral AVF are rare and typically secondary to arterialization of venous drainage leading to local ischemia and nerve damage. There are case reports of vertigo and vertebrobasilar insufficiency, cervical radiculopathy related to nerve-root compression from engorged vertebral veins, and cervical myelopathy from venous hypertension similar to this patient. As well, there is only one case report of a vertebral AVF leading to exophthalmos, chemosis, and a bruit, mimicking a carotid-cavernous fistula. This is the first reported case of a vertebral AVF leading to both cervical cord and ocular pathology.
Vertebral AVFs can be suspected based on CT and MRI findings, but angiography is the gold standard for diagnosis. Transarterial embolization is the safest and most effective treatment, allowing for occlusion of the fistula while maintaining patency of the vertebral artery. If treated expediently, most patients experience total recovery.
Dr. Baudendistel can be contacted at BaudenT@sutterhealth.org.
References
- Ammirati M, Mirzai S, Samii M. Vertebral arteriovenous fistulae: report of two cases and review of the literature. Acta Neurochir. 1989;99:122-6.
- Gobin YP, Duckwiler GR, Vinuela F. Direct arteriovenous fistulas: diagnosis and intervention. Neuroimaging Clin North Am. 1998;8:425-43.
- Halbach VV, Higashida RT, Hieshima GB. Treatment of vertebral arteriovenous fistulas. AJR. 1988;150:405-12.