User login
Why is SIADH Important to Hospitalists?
Disorders of body fluids, and particularly hyponatremia, are among the most commonly encountered problems in clinical medicine, affecting up to 30% of hospitalized patients. In a study of 303,577 laboratory samples collected from 120,137 patients, the prevalence of hyponatremia (serum [Na+] <135 mmol/L) on initial presentation to a healthcare provider was 28.2% among those treated in an acute hospital care setting, 21% among those treated in an ambulatory hospital care setting, and 7.2% in community care centers.1 Numerous other studies have corroborated a high prevalence of hyponatremia in hospitalized patients,2 which reflects the increased vulnerability of this patient population to disruptions of body fluid homeostasis. Recognizing the many possible causes of hyponatremia in hospitalized patients and implementing appropriate treatment strategies therefore are critical steps toward optimizing care and improving outcomes in hospitalized patients with hyponatremia.
In addition to its frequency, hyponatremia is also important because it has been associated with worse clinical outcomes across the entire range of inpatient care, from the general hospital population to those treated in the intensive care unit (ICU). In a study of 4123 patients age 65 years or older who were admitted to a community hospital, 3.5% had clinically significant hyponatremia (serum [Na+] <130 mmol/L) at admission. Compared with nonhyponatremic patients, those with hyponatremia were twice as likely to die during their hospital stay (relative risk [RR], 1.95; P < 0.05).3 In another study of 2188 patients admitted to a medical ICU over a 5‐year period, 13.7% had hyponatremia. The overall rate of in‐hospital mortality among all ICU patients was high at 37.7%. However, severe hyponatremia (serum [Na+] <125 mmol/L) more than doubled the risk of in‐hospital mortality (RR, 2.10; P < 0.001).4 In addition to the general hospital population, in virtually every disease ever studied, the presence of hyponatremia has been found to be an independent risk factor for increased mortality, from congestive heart failure to tuberculosis to liver failure.2
What Causes Hyponatremia in Patients with SIADH?
Hyponatremia can be caused by 1 of 2 potential disruptions in fluid balance: dilution from retained water, or depletion from electrolyte losses in excess of water. Dilutional hyponatremias are associated with either a normal (euvolemic) or an increased (hypervolemic) extracellular fluid (ECF) volume, whereas depletional hyponatremias generally are associated with a decreased ECF volume (hypovolemic). Dilutional hyponatremia can arise from a primary defect in osmoregulation, such as in SIADH, or as a result of ECF volume expansion, as seen in conditions associated with concomitant secondary hyperaldosteronism such as heart failure, hepatic cirrhosis, or nephrotic syndrome. Among some hospitalized patient groups, euvolemic hyponatremia is the most common presentation of abnormally low serum [Na+]. In a study of patients who developed clinically significant postoperative hyponatremia (defined as a serum [Na+] <130 mmol/L) in a large teaching hospital, only 8% were hypovolemic, whereas 42% were euvolemic and 21% were hypervolemic.5
Euvolemic hyponatremia results from an increase in total body water, but with normal or near‐normal total body sodium. As a result, there is an absence of clinical manifestations of ECF volume expansion, such as subcutaneous edema or ascites. It is important to recognize that although SIADH clearly represents a state of volume expansion due to water retention, it rarely causes clinically recognizable hypervolemia since the retained water is distributed across the intracellular fluid (ICF) as well as the ECF, and because volume regulatory processes act to decrease the actual degree of ECF volume expansion.6 Euvolemic hyponatremia can accompany a wide variety of pathological processes, but the most common cause by far is SIADH. Normally, increased plasma osmolality activates osmoreceptors located in the anterior hypothalamus and stimulates the secretion of arginine vasopressin (AVP), also called antidiuretic hormone (ADH), a key neurohormone that regulates fluid homeostasis. In patients with euvolemic hyponatremia due to SIADH, plasma AVP levels are not suppressed despite normal or decreased plasma osmolality.7 This can be a result of ectopic production of AVP by tumors, or stimulation of endogenous pituitary AVP secretion as a result of nonosmotic stimuli that also stimulate vasopressinergic neurons, which include hypovolemia, hypotension, angiotensin II, nausea, hypoxia, hypercarbia, hypoglycemia, stress, and physical activity. Nonsuppressed AVP levels have been documented in the majority of hyponatremic patients, including those with SIADH8 and heart failure.9
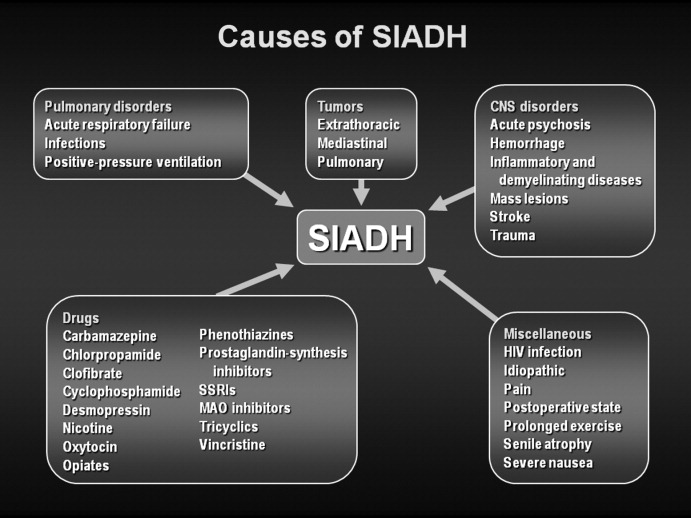
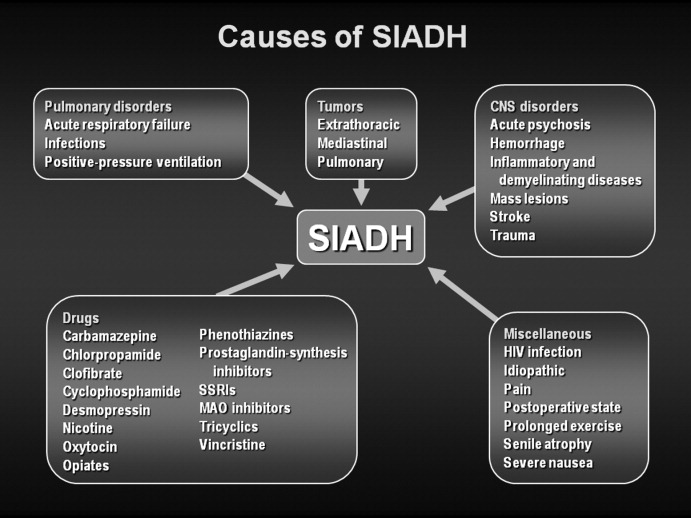
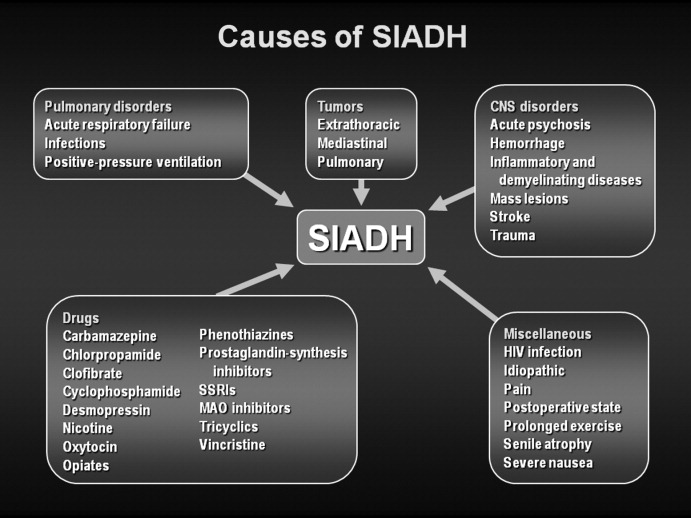
SIADH can develop as the result of many different disease processes that disrupt the normal mechanisms that regulate AVP secretion, including pneumonias and other lung infections, thoracic and extrathoracic tumors, a variety of different central nervous system disorders, the postoperative state, human immunodeficiency virus (HIV), and many different drugs (Figure 1). Given the multiplicity of disorders and drugs that can cause disrupted AVP secretion, it is not surprising that hyponatremia is the most common electrolyte abnormality seen in clinical practice.
What Symptoms are Associated With SIADH?
Symptoms of hyponatremia correlate both with the degree of decrease in the serum [Na+] and with the chronicity of the hyponatremia. Acute hyponatremia, defined as <48 hours in duration, is often associated with life‐threatening clinical features such as obtundation, seizures, coma, and respiratory arrest. These symptoms can occur abruptly, sometimes with little warning.10 In the most severe cases, death can occur as a result of cerebral edema with tentorial herniation. Hypoxia secondary to neurogenic pulmonary edema can increase the severity of brain swelling.11
In contrast, chronic hyponatremia is much less symptomatic, and the reason for the profound differences between the symptoms of acute and chronic hyponatremia is now well understood to be due to the process of brain volume regulation.12 It is essential that this process be understood in order to understand the full spectrum of hyponatremic symptoms. As the ECF [Na+] decreases, regardless of whether due to a loss of sodium or a gain of water, there is an obligate movement of water into the brain along osmotic gradients. That water shift causes swelling of the brain, or cerebral edema. If the increased brain water reaches approximately 8% in adults, it exceeds the capacity of the skull to accommodate brain expansion, leading to tentorial herniation and death from respiratory arrest and/or ischemic brain damage. However, if the patient survives the initial hyponatremia, a very strong volume regulatory process follows, consisting of loss of electrolytes and small organic molecules called osmolytes from brain cells into brain ECF, and eventually the peripheral ECF.12, 13 As the solute content of the brain decreases, the water content is allowed to normalize, eventually reaching a state in which brain edema is virtually absent, and as a result symptoms are markedly less than with acute hyponatremia. Although the time required for the brain to acieve a volume‐regulated state varies across patients, this process is completed within 48 hours in experinmental animal studies, and probably follows a similar time course in humans.
Despite this powerful adaptation process, chronic hyponatremia is frequently associated with neurological symptomatology, albeit milder and more subtle in nature. A recent report found a fairly high incidence of symptoms in 223 patients with chronic hyponatremia as a result of thiazide administration: 49% had malaise/lethargy, 47% had dizzy spells, 35% had vomiting, 17% had confusion/obtundation, 17% experienced falls, 6% had headaches, and 0.9% had seizures.14 Although dizziness can potentially be attributed to a diuretic‐induced hypovolemia, symptoms such as confusion, obtundation and seizures are more consistent with hyponatremic symptomatology. Because thiazide‐induced hyponatremia can be readily corrected by stopping the thiazide and/or administering sodium, this represents an ideal situation in which to assess improvement in hyponatremia symptomatology with normalization of the serum [Na+]; in this study, all of these symptoms improved with correction of the hyponatremia. This represents one of the best examples demonstrating reversal of the symptoms associated with chronic hyponatremia by correction of the hyponatremia, because the patients in this study did not in general have severe underlying comorbidities that might complicate interpretation of their symptoms, as is often the case in patients with SIADH.
What Is Required for Making a Diagnosis of SIADH in Hospitalized Patients?
In patients with hypotonic hypoosmolality, ascertainment of their ECF volume status (ie, hypovolemic, euvolemic, or hypervolemic) is an essential first step, as this will segregate patients into different treatment paradigms. For example, in patients who are truly clinically hypovolemic with a decreased ECF volume by clinical parameters, treatment would generally consist of solute repletion with sodium, generally isotonic saline infusion with or without potassium, until the sodium levels normalize. In patients who are hypervolemic, treatment should focus first on the underlying disease rather than addressing the serum [Na+] directly. In patients with clinical euvolemia, the standard diagnostic pathway should be followed to confirm a diagnosis of SIADH as described below.
Assessing ECF volume status can be difficult, even for the most experienced clinicians. Physical signs such as orthostatic decreases in blood pressure and increases in pulse rate, dry mucus membranes, and skin tenting indicate hypovolemic hyponatremia, while signs such as subcutaneous edema, ascites, or anasarca indicate hypervolemic hyponatremia. Patients without any of these findings are generally considered to be euvolemic. However, in any situation these signs are only applicable if there are no other reasons to suspect an altered ECF volume. Along with a complete history and physical examination that includes a careful neurological evaluation, several laboratory tests can help to assess the etiology of the hyponatremia, once serum sodium concentrations have been shown to be below normal ([Na+] <135 mmol/L):
-
Urine osmolality. A urine osmolality (Uosm) less than 100 mOsm/kg H2O can indicate low dietary solute intake, primary polydipsia, or a reset osmostat after suppression of AVP release by a decrease in plasma osmolality below the osmotic threshold for AVP secretion, usually as a result of increased water loading.
-
Urine sodium concentration. Excretion of sodium, as measured by a spot urine [Na+] (UNa), can indicate depletional hyponatremia if the concentration is less than 30 mmol/L.15 A low UNa reflects a volume depleted state unless the patient has secondary hyperaldosteronism from heart failure or cirrhosis. Patients with a low UNa are more likely to respond to isotonic saline. Euvolemic patients who have a normal dietary sodium intake will generally have spot UNa 30 mmol/L and will not benefit from isotonic saline administration.15 In fact, in SIADH, these patients may respond to isotonic saline with a worsening of hyponatremia, since the sodium from the isotonic saline will be excreted in a concentrated urine while the free water is reabsorbed in the kidney collecting ducts. If the patient is on diuretic therapy, urine sodium values cannot always be accurately interpreted, since a UNa 30 mmol/L may reflect the natriuretic effect of the diuretic and not a volume replete state.
-
Blood tests. Additional indicators of volume status include serum blood nitrogen (BUN) and uric acid levels. A BUN <10 mg/dL and uric acid <4 mg/dL are generally consistent with a euvolemic state, particularly when there is glomerular hyperfiltration, which is often present in SIADH. Elevated serum BUN and uric acid levels (BUN >20 mg/dL and uric acid >6 mg/dL), especially if prior values are available for comparison, can also help to establish whether ineffective vascular volume status may be contributing to the pathophysiology of the hyponatremia. In certain clinical scenarios, the B‐type natriuretic protein (BNP) can be helpful to support a clinical impression of congestive heart failure.
The criteria necessary for a diagnosis of SIADH remain essentially as defined by Bartter and Schwartz16 in 1967 (Table 1), but several points deserve emphasis.17 First, true ECF hypoosmolality must be present and hyponatremia secondary to pseudohyponatremia or hyperglycemia excluded. Second, urinary osmolality must be inappropriate for plasma hypoosmolality (Posm). This does not require a Uosm>Posm, but simply that the urine osmolality is greater than maximally dilute (ie, Uosm>100 mOsm/kg H2O in adults). Furthermore, urine osmolality need not be inappropriately elevated at all levels of Posm but simply at some level under 275 mOsm/kg H2O, since in patients with a reset osmostat, AVP secretion can be suppressed at some level of osmolality resulting in maximal urinary dilution and free water excretion at plasma osmolalities below this level.18 Although some consider a reset osmostat to be a separate disorder rather than a variant of SIADH, such cases nonetheless illustrate that some hypoosmolar patients can exhibit an appropriately dilute urine at some, though not all, plasma osmolalities. Third, clinical euvolemia must be present to diagnose SIADH, and this diagnosis cannot be made in a hypovolemic or edematous patient. Importantly, this does not mean that patients with SIADH cannot become hypovolemic for other reasons, but in such cases it is impossible to diagnose the underlying SIADH until the patient is rendered euvolemic. The fourth criterion, renal salt wasting, has probably caused the most confusion in the diagnosis of SIADH. As noted above, the importance of this criterion lies in its usefulness in differentiating hypoosmolality caused by a decreased effective intravascular volume with high aldosterone levels in which case renal Na+ conservation occurs, from dilutional disorders in which urine Na+ excretion is normal or increased due to ECF volume expansion and a suppressed renin‐angiotensin‐aldosterone system. However, UNa can also be high in renal causes of solute depletion such as diuretic use or Addison's disease, and conversely patients with SIADH can have a low UNa if they subsequently become hypovolemic or solute depleted, conditions sometimes produced by imposed salt and water restriction. Consequently, although high urinary Na+ excretion is generally the rule in most patients with SIADH, its presence does not necessarily confirm this diagnosis, nor does its absence rule out the diagnosis. The final criterion emphasizes that SIADH remains a diagnosis of exclusion, and the absence of other potential causes of hypoosmolality must always be verified. Glucocorticoid deficiency and SIADH can be especially difficult to distinguish, since both primary and secondary hypocortisolism can cause elevated plasma AVP levels in addition to direct renal effects that prevent maximal urinary dilution.19 Therefore, no patient with chronic hyponatremia should be diagnosed as having SIADH without a thorough evaluation of adrenal function, preferably via a rapid adrenocorticotropic hormone (ACTH) stimulation test. Acute hyponatremia of obvious etiology, such as postoperatively or in association with pneumonitis, may be treated without adrenal testing as long as there are no other clinical signs or symptoms suggestive of adrenal dysfunction.20
|
| Essential |
| Decreased effective osmolality of the extracellular fluid (Posm< 275 mOsm/kg H2O). |
| Inappropriate urinary concentration (Uosm >100 mOsm/kg H2O with normal renal function) at some level of hypoosmolality. |
| Clinical euvolemia, as defined by the absence of signs of hypovolemia (orthostasis, tachycardia, decreased skin turgor, dry mucous membranes) or hypervolemia (subcutaneous edema, ascites). |
| Elevated urinary sodium excretion while on a normal salt and water intake. |
| Absence of other potential causes of euvolemic hypoosmolality: hypothyroidism, hypocortisolism (Addison's disease or secondary adrenal insufficiency) and diuretic use. |
| Supplemental |
| Abnormal water load test (inability to excrete at least 90% of a 20 mL/kg water load in 4 hours and/or failure to dilute Uosm to <100 mOsm/kg H2O). |
| Plasma AVP level inappropriately elevated relative to plasma osmolality. |
| No significant correction of serum [Na+] with volume expansion but improvement after fluid restriction. |
Hyponatremia is a particularly common complication in elderly hospitalized patients, increasing in prevalence from approximately 7% in the general older population to 18% to 22% among elderly patients in chronic care facilities.21 Despite the many known causes of SIADH (Figure 1), hyponatremia is often associated with idiopathic SIADH in the elderly population. In a study of 119 nursing home residents aged 60 to 103 years, 53% had at least 1 episode of hyponatremia during the previous 12 months.22 Of these patients, 26% were diagnosed with idiopathic SIADH. In another study of elderly patients with hyponatremia and SIADH, 60% were diagnosed with idiopathic SIADH. Among remaining patients, the 2 main causes identified were pneumonia (9 cases/18%) and medications (6 cases/12%).23 Therefore, more than half of elderly patients who present with hyponatremia due to SIADH may have an idiopathic form, with no detectable underlying treatable disease.
Which Hospital Patients With SIADH are Candidates for Treatment of Hyponatremia?
Correction of hyponatremia is associated with markedly improved neurological outcomes in patients with severely symptomatic hyponatremia. In a retrospective review of patients who presented with severe neurological symptoms and serum [Na+] <125 mmol/L, prompt therapy with isotonic or hypertonic saline resulted in a correction in the range of 20 mmol/L over several days and neurological recovery in almost all cases. In contrast, in patients who were treated with fluid restriction alone, there was very little correction over the study period (<5 mmol/L over 72 hours), and the neurological outcomes were much worse, with most of these patients either dying or entering a persistently vegetative state.24 Consequently, prompt therapy to rapidly increase the serum [Na+] represents the standard‐of‐care for treatment of patients presenting with severe life‐threatening symptoms of hyponatremia.
As discussed earlier, chronic hyponatremia is much less symptomatic as a result of the process of brain volume regulation. Because of this adaptation process, chronic hyponatremia is arguably a condition that clinicians feel they may not need to be as concerned about, and in some publications this has been called asymptomatic hyponatremia. However, such patients often do have neurological symptoms, even if milder and more subtle in nature, including headaches, nausea, mood disturbances, depression, difficulty concentrating, slowed reaction times, unstable gait, increased falls, confusion, and disorientation. Consequently, any patient with hyponatremia secondary to SIADH who manifests any neurological symptoms that could be related to the hyponatremia should be considered as appropriate candidates for treatment of the hyponatremia, regardless of the chronicity of the hyponatremia or the level of serum [Na+].
What Therapies are Currently Available to Manage SIADH in Hospitalized Patients?
Conventional management strategies for euvolemic hyponatremia range from saline infusion and fluid restriction to pharmacologic adjustment of fluid balance. Consideration of treatment options should include an evaluation of the benefits as well as the potential toxicities of any therapy (Table 2). Sometimes, simply stopping treatment with an agent that is associated with hyponatremia is sufficient to reverse a low serum [Na+].
| Therapy | Targets Underlying Pathophysiology | Limitations |
|---|---|---|
| ||
| Isotonic saline | Ineffective in dilutional hyponatremias; exacerbates the volume overload if used in edema‐forming disorders; no controlled safety database. | |
| Hypertonic saline | No consensus regarding appropriate infusion rates; overcorrection can cause osmotic demyelination; exacerbates the volume overload if used in edema‐forming disorders; no controlled safety database. | |
| Fluid restriction | Slow to correct over many days; poorly tolerated due to thirst; can not be used effectively in patients with high AVP levels and urine osmolalities. | |
| Demeclocycline | ✓ | Not FDA approved for hyponatremia; slow to correct; nephrotoxic in cirrhosis and heart failure. |
| Mineralocorticoids | Only one report in elderly patients with SIADH; no safety database; exacerbates the volume overload if used in edema‐forming disorders. | |
| Urea | Not FDA‐approved for hyponatremia; poor palatability. | |
| AVP receptor antagonists (vaptans) | ✓ | Conivaptan approved only for in‐hospital use secondary to CYP3A4 inhibition; infusion‐site reactions with intravenous use. Tolvaptan must be initiated and reinitiated in the hospital, as serum sodium needs to be monitored closely to avoid overly rapid correction of hyponatremia. |
Isotonic Saline
The treatment of choice for depletional hyponatremia (ie, hypovolemic hyponatremia) is isotonic saline ([Na+] = 154 mmol/L) to restore ECF volume and ensure adequate organ perfusion. This initial therapy is appropriate for patients who either have clinical signs of hypovolemia, or in whom a spot UNa+ is <30 mmol/L. However, this therapy is ineffective for dilutional hyponatremias such as SIADH,25 and continued inappropriate administration of isotonic saline to a euvolemic patient may worsen their hyponatremia,26 and/or cause fluid overload. Although isotonic saline may improve the serum [Na+] in patients with hypervolemic hyponatremia, their volume status will generally worsen with this therapy, so unless the hyponatremia is profound isotonic saline should be avoided.
Hypertonic Saline
Acute hyponatremia presenting with severe neurological symptoms is life‐threatening, and should be treated promptly with hypertonic solutions, typically 3% NaCl ([Na+] = 513 mmol/L), as this represents the most reliable method to quickly raise the serum [Na+]. A continuous infusion of hypertonic NaCl is usually utilized in inpatient settings. Various formulae have been suggested for calculating the initial rate of infusion of hypertonic solutions,27 but perhaps the simplest utilizes the following relationship:
An alternative option for more emergent situations is administration of a 100 mL bolus of 3% NaCl, repeated once if no clinical improvement, which has been recommended by a consensus conference organized to develop guidelines for prevention and treatment of exercise‐induced hyponatremia, an acute and potentially lethal condition.28 Injecting this amount of hypertonic saline intravenously raises the serum [Na+] by an average of 2 mmol/L to 4 mmol/L, which is well below the recommended maximal daily rate of change of 10 to 12 mmol/24 hours or 18 mmol/48 hours.29 Because the brain can only accommodate an average increase of approximately 8% in brain volume before herniation occurs, quickly increasing the serum [Na+] by as little as 2 mmol/L to 4 mmol/L in acute hyponatremia can effectively reduce brain swelling and intracranial pressure.30 Unfortunately, until now there has been no consensus regarding appropriate infusion rates of 3% NaCl, and many physicians are hesitant to use it in patients with chronic hyponatremia because it can cause an overly rapid correction of serum sodium levels that can lead to the osmotic demyelination syndrome (ODS).31 Nonetheless, this remains the treatment of choice for patients with severe neurological symptoms, even when the time course of the hyponatremia is nonacute or unknown. The administration of hypertonic saline is generally not recommended for most patients with edema‐forming disorders because it acts as a volume expander and may exacerbate volume overload.
Fluid Restriction
For patients with chronic hyponatremia, fluid restriction has been the most popular and most widely accepted treatment. When SIADH is present, generally fluids should be limited to 500 to 1000 mL/24 hours. Because fluid restriction increases the serum [Na+] largely by under‐replacing the excretion of fluid by the kidneys, some have advocated an initial restriction to 500 mL less than the 24‐hour urine output.32 When instituting a fluid restriction, it is important for the nursing staff and the patient to understand that this includes all fluids that are consumed, not just water. Generally the water content of ingested food is not included in the restriction because this is balanced by insensible water losses (perspiration, exhaled air, feces, etc.), but caution should be exercised with foods that have high fluid concentrations (such as fruits and soups). Restricting fluid intake is effective when properly applied and managed, but serum sodium levels are increased only slowly (1‐2 mmol/L/day) even with severe restriction.25 In addition, this therapy is often poorly tolerated because of an associated increase in thirst. However, it is economically favorable, and some patients do respond well to this option. Fluid restriction should not be used with hypovolemic patients, and is particularly difficult to maintain in patients with very elevated urine osmolalities secondary to high AVP levels; in general, if the sum of urine Na+ and K+ exceeds the serum [Na+], most patients will not respond to a fluid restriction since an electrolyte‐free water clearance will be difficult to achieve,33, 34 and in patients in intensive care settings who often require administration of fluids as part of their therapies.
Demeclocycline
Demeclocycline, a tetracycline antibiotic, inhibits adenylyl cyclase activation after AVP binds to its V2 receptor in the kidney, and thus targets the underlying pathophysiology of SIADH. This therapy is typically used when patients find severe fluid restriction unacceptable and the underlying disorder cannot be corrected. However, demeclocycline is not approved by the U.S. Food and Drug Administration (FDA) to treat hyponatremia, and can cause nephrotoxicity in patients with heart failure and cirrhosis, although this is usually reversible if caught quickly enough.35
Mineralocorticoids
Administration of mineralocorticoids, such as fludrocortisone, has been shown to be useful in a small number of elderly patients.36 However, the initial studies of SIADH did not show it to be of benefit in patients with SIADH, and it carries the risk of fluid overload and hypertension. Consequently, it is rarely used to treat hyponatremia in the U.S.
Urea
Administration of urea has been successfully used to treat hyponatremia because it induces osmotic diuresis and augments free water excretion. Effective doses of urea for treatment of hyponatremia are 30 gm to 60 gm daily in divided doses.37 Unfortunately, its use is limited because there is no United States Pharmacopeia (USP) formulation for urea, and it is not approved by the FDA for treatment of hyponatremia. As such, urea has not been used extensively in the United States, and there are limited data to support its long‐term use. Furthermore, urea is associated with poor palatability; however, patients with feeding tubes may be excellent candidates for urea therapy since palatability is not a concern, and the use of fluid restriction may be difficult in some patients with high obligate intake of fluids as part of their nutritional and medication therapy. Although mild azotemia can be seen with urea therapy, this rarely reaches clinically significant levels.
Clinicians have used all of the above conventional therapies for hyponatremia over the past decades. However, conventional therapies for hyponatremia, although effective in specific circumstances, are suboptimal for many different reasons, including variable efficacy, slow responses, intolerable side effects, and serious toxicities, as summarized in Table 2. But perhaps the most striking deficiency of most conventional therapies is that with the exception of demeclocycline, these therapies do not directly target the underlying cause of most all dilutional hyponatremias, namely inappropriately elevated plasma AVP levels. A new class of pharmacological agents, vasopressin receptor antagonists, that directly block AVP‐mediated receptor activation have recently been approved by the FDA for treatment of euvolemic and hypervolemic hyponatremia.38
AVP Receptor (AVPR) Antagonists
Conivaptan and tolvaptan are antagonists of the AVP V2 (antidiuretic) receptor and have been approved by the FDA for the treatment of euvolemic and hypervolemic hyponatremia. These agents, also known as vaptans, compete with AVP/ADH for binding at its site of action in the kidney, thereby blocking the antidiuresis caused by elevated AVP levels and directly attacking the underlying pathophysiology of dilutional hyponatremia. AVPR antagonists produce electrolyte free water excretion (called aquaresis) without affecting renal sodium and potassium excretion.39 The overall result is a reduction in body water without natriuresis, which leads to an increase in the serum [Na+]. One of the major benefits of this class of drugs is that serum [Na+] is significantly increased within 24 to 48 hours,40, 41 which is considerably faster than the effects of fluid restriction that can take many days. Also, compliance has not been shown to be problem for vaptans, whereas this is a major problem with attempted long‐term use of fluid restriction.
Conivaptan is FDA‐approved for euvolemic and hypervolemic hyponatremia in hospitalized patients. It is available only as an intravenous preparation, and is given as a 20 mg loading dose over 30 minutes, followed by a continuous infusion of 20 or 40 mg.42 Generally, the 20 mg continuous infusion is used for the first 24 hours to gauge the initial response. If the correction of serum [Na+] is felt to be inadequate (eg, <5 mmol/L), then the infusion rate can be increased to 40 mg/day. Therapy is limited to a maximum duration of 4 days because of drug‐interaction effects with other agents metabolized by the cytochrome P450 3A4 (CYP3A4) hepatic isoenzymes. Importantly, for conivaptan and all other vaptans, it is critical that the serum [Na+] concentration is measured frequently during the active phase of correction of the hyponatremia (a minimum of every 6 hours, but more frequently in patients with risk factors for development of osmotic demyelination, such as severely low serum [Na+], malnutrition, alcoholism and hypokalemia).43 If the correction approaches 12 mmol/L in the first 24 hours, the infusion should be stopped and the patient monitored on a fluid restriction. If the correction exceeds 12 mmol/L, consideration should be given to administering sufficient water, either orally or as intravenous D5W to bring the overall correction below 12 mmol/L. The maximum correction limit should be reduced to 8 mmol/L over the first 24 hours in patients with risk factors for development of osmotic demyelination. The most common adverse effects include injection‐site reactions, which are generally mild and usually do not lead to treatment discontinuation, headache, thirst, and hypokalemia.40
Tolvaptan, an oral AVPR antagonist, is FDA‐approved for treatment of dilutional hyponatremias. In contrast to conivaptan, oral administration allows it to be used for both short‐term and long‐term treatment of hyponatremia.41 Similar to conivaptan, tolvaptan treatment must be initiated in the hospital so that the rate of correction can be monitored carefully. Patients with a serum [Na+] <125 mmol/L are eligible for therapy with tolvaptan as primary therapy; if the serum [Na+] is 125 mmol/L, tolvaptan therapy is only indicated if the patient has symptoms that could be attributable to the hyponatremia and the patient is resistant to attempts at fluid restriction.44 The starting dose of tolvaptan is 15 mg on the first day, and the dose can be titrated to 30 mg and 60 mg at 24‐hour intervals if the serum [Na+] remains <135 mmol/L or the increase in serum [Na+] has been 5 mmol/L in the previous 24 hours. As with conivaptan, it is essential that the serum [Na+] concentration is measured frequently during the active phase of correction of the hyponatremia (a minimum of every 8 hrs, but more frequently in patients with risk factors for development of osmotic demyelination). Limits for safe correction of hyponatremia and methods to compensate for overly rapid corrections are the same as described previously for conivaptan. Common side effects include dry mouth, thirst, increased urinary frequency, dizziness, nausea and orthostatic hypotension, which were relatively similar between placebo and tolvaptan groups in clinical trials.41, 44
Because inducing increased renal fluid excretion via either a diuresis or an aquaresis can cause or worsen hypotension in patients with hypovolemic hyponatremia, vaptans are contraindicated in this patient population.43 However, clinically significant hypotension was not observed in either the conivaptan or tolvaptan clinical trials in euvolemic and hypervolemic hyponatremic patients. Although vaptans are not contraindicated with decreased renal function, these agents generally will not be effective if the serum creatinine is >2.5 mg/dL.
Hyponatremia Treatment Guidelines for Hospitalized Patients With SIADH
Although various authors have published recommendations on the treatment of hyponatremia,27, 43, 45‐47 no standardized treatment algorithms have yet been widely accepted. A synthesis of existing expert recommendations for treatment of hyponatremia is illustrated in Figure 2. This algorithm is based primarily on the symptomatology of hyponatremic patients, rather than the serum [Na+] or the chronicity of the hyponatremia, which are often difficult to ascertain. A careful neurological history and assessment should always be done to identify potential causes for the patient's symptoms other than hyponatremia, although it will not always be possible to exclude an additive contribution from the hyponatremia to an underlying neurological condition. In this model, patients are divided into three groups based on their presenting symptoms.
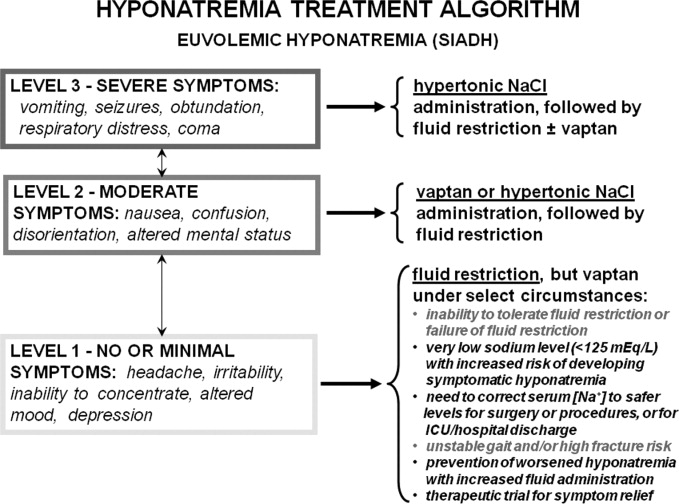
Level 1 symptoms include seizures, coma, respiratory arrest, obtundation, and vomiting, and usually imply a more acute onset or worsening of hyponatremia requiring immediate active treatment. Therapies that will quickly raise serum sodium levels are required to reduce cerebral edema and decrease the risk of potentially fatal herniation.
Level 2 symptoms, which are more moderate, include nausea, confusion, disorientation, and altered mental status. These symptoms may be either chronic or acute, but allow time to elaborate a more deliberate approach to treatment.
Level 3 symptoms range from minimal symptoms such as a headache, irritability, inability to concentrate, altered mood, and depression, to a virtual absence of discernable symptoms, and indicate that the patient may have chronic or slowly evolving hyponatremia. These symptoms necessitate a cautious approach, especially when patients have underlying comorbidities.
Patients with severe symptoms (Level 1) should be treated with hypertonic saline as first‐line therapy, followed by fluid restriction with or without AVPR antagonist therapy. Patients with moderate symptoms will benefit from a more aggressive regimen of vaptan therapy or limited hypertonic saline administration, followed by fluid restriction or long‐term vaptan therapy. Although moderate neurological symptoms can indicate that a patient is in an early stage of acute hyponatremia, they more often indicate a chronically hyponatremic state with sufficient brain volume adaptation to prevent marked symptomatology from cerebral edema. Regardless, close monitoring of these patients in a hospital setting is warranted until the symptoms improve or stabilize. Patients with no or minimal symptoms should be managed initially with fluid restriction, although treatment with vaptans may be appropriate for a wide range of specific clinical conditions, foremost of which is a failure to improve the serum [Na+] despite reasonable attempts at fluid restriction (Figure 2).
Although this classification is based on presenting symptoms at the time of initial evaluation, it should be remembered that in some cases patients initially exhibit more moderate symptoms because they are in the early stages of hyponatremia. In addition, some patients with minimal symptoms are prone to develop more symptomatic hyponatremia during periods of increased fluid ingestion. In support of this, approximately 70% of 31 patients presenting to a university hospital with symptomatic hyponatremia and a mean serum [Na+] of 119 mmol/L had preexisting asymptomatic hyponatremia as the most common risk factor identified.48 Consequently, therapy of hyponatremia should also be considered to prevent progression from lower to higher levels of symptomatic hyponatremia, particularly in patients with a past history of repeated presentations of symptomatic hyponatremia.
How Often Should Serum [Na+] Be Monitored in Hospitalized Patients With SIADH?
The frequency of serum [Na+] monitoring is dependent on both the severity of the hyponatremia and the therapy chosen. In all hyponatremic patients neurological symptomatology should be carefully assessed very early in the diagnostic evaluation to assess the symptomatic severity of the hyponatremia and to determine whether the patient requires more urgent therapy. All patients undergoing active treatment with hypertonic saline for level 1 or 2 symptomatic hyponatremia should have frequent monitoring of serum [Na+] and ECF volume status (every 2‐4 hours) to ensure that the serum [Na+] does not exceeded the recommended levels during the active phase of correction,43 since overly rapid correction of serum sodium can cause damage to the myelin sheath of nerve cells, resulting in central pontine myelinolysis, also called the ODS.31 Patients treated with vaptans for level 2 or 3 symptoms should have serum [Na+] monitored every 6 to 8 hours during the active phase of correction, which will generally be the first 24 to 48 hours of therapy. Active treatment with hypertonic saline or vaptans should be stopped when the patient's symptoms are no longer present, a safe serum [Na+] (usually >120 mmol/L) has been achieved, or the rate of correction has reached 12 mmol/L within 24 hours or 18 mmol/L within 48 hours.29, 43 Importantly, ODS has not been reported either in clinical trials or with therapeutic use of any vaptan to date. In patients with a stable level of serum [Na+] treated with fluid restriction or therapies other than hypertonic saline, measurement of serum [Na+] daily is generally sufficient, since levels will not change that quickly in the absence of active therapy or large changes in fluid intake or administration.
Potential Future Indications for Treatment of Hyponatremia
Correction of hyponatremia improves other symptoms, such as gait stability, in patients who may be considered to be asymptomatic by virtue of a normal neurological exam. In 1 study, 16 patients with hyponatremia secondary to SIADH in the range of 124 mmol/L to 130 mmol/L demonstrated a significant gait instability that normalized after correction of the hyponatremia to normal ranges.49 The functional significance of the gait instability was illustrated in a study of 122 Belgian patients with a variety of levels of hyponatremia, all judged to be asymptomatic at the time of visit to an emergency department (ED). These patients were compared with 244 age‐matched, sex‐matched, and disease‐matched controls also presenting to the ED during the same time period. Researchers found that 21% of the hyponatremic patients presented to the ED because of a recent fall, compared to only 5% of the controls, resulting in an adjusted odds ratio (OR) for presenting to the ED because of a recent fall of 67 for hyponatremia (P < 0.001).49 Consequently, this study clearly documented an increased incidence of falls in so‐called asymptomatic hyponatremic patients.
The clinical significance of the gait instability and fall data were further evaluated in a study that compared 553 patients with fractures to an equal number of age‐matched and sex‐matched controls. Hyponatremia was found in 13% of the patients presenting with fractures compared to only 4% of the controls.50 Similar findings have been reported in a 364 elderly patients with large‐bone fractures in New York.51 More recently published studies have shown that hyponatremia is associated with increased bone loss in experimental animals and a significant increased OR for osteoporosis of the femoral neck (OR, 2.87; P < 0.003) in humans over the age of 50 in the NHANES III database.52 Thus, the major clinical significance of chronic hyponatremia may be the increased morbidity and mortality associated with falls and fractures in our elderly population.
Summary
Disorders of sodium and water metabolism are commonly encountered in the hospital setting due to the wide range of disease states that can disrupt the balanced control of water and solute intake and output. In particular, the prompt identification and appropriate management of abnormally low serum [Na+] is critical if we are to reduce the increased morbidity and mortality that accompany hyponatremia in hospitalized patients. Use of an algorithm that is based primarily on the symptomatology of hyponatremic patients, rather than the chronicity of the hyponatremia or the serum [Na+], will help to choose the correct initial therapy in hospitalized hyponatremic patients. However, careful monitoring of serum [Na+] responses is required in all cases to adjust therapy appropriately in response to changing clinical conditions. Although this approach will enable efficacious and safe treatment of hyponatremic patients with SIADH at the present time, evolving knowledge of the consequences of chronic hyponatremia will likely alter treatment indications and guidelines in the future.
- .Age and gender as risk factors for hyponatremia and hypernatremia.Clin Chim Acta.2003;337(1‐2):169–172.
- ,,.Incidence and prevalence of hyponatremia.Am J Med.2006;119(7 Suppl 1):S30–S35.
- ,,.Admission hyponatremia in the elderly: factors influencing prognosis.J Gen Intern Med1994;9:89–91.
- ,,, et al.[Incidence, causes and prognostic factors of hyponatremia in intensive care].Rev Med Interne.2003;24(4):224–229.
- ,,,.Postoperative hyponatremia. A prospective study.Arch Int Med.1986;146:333–336.
- .Whole‐body volume regulation and escape from antidiuresis.Am J Med.2006;119(7 Suppl 1):S21–S29.
- ,,.Neurogenic disorders of osmoregulation.Am J Med.1982;72:339–353.
- ,,.Vasopressin function in the syndrome of inappropriate antidiuresis.Annu Rev Med.1980;31:315–327.
- ,,,,,.Radioimmunoassay of plasma arginine vasopressin in hyponatremic patients with congestive heart failure.N Eng J Med.1981;305:263–266.
- ,.Epidemiology, pathophysiology, and management of hyponatremic encephalopathy.Am J Med.1997;102:67–77.
- ,.Pulmonary complications of hyponatremic encephalopathy. noncardiogenic pulmonary edema and hypercapnic respiratory failure [see comments].Chest.1995;107(2):517–521.
- ,.Control of brain volume during hyperosmolar and hypoosmolar conditions.Annu Rev Med.1993;44:289–301.
- .Control of brain volume during hypoosmolality and hyperosmolality.Adv Exp Med Biol.2006;576:113–129.
- ,,.Clinical studies of thiazide‐induced hyponatremia.J Natl Med Assoc.2004;96(10):1305–1308.
- ,,,.Clinical assessment of extracellular fluid volume in hyponatremia.Am J Med.1987;83:905–908.
- ,.The syndrome of inappropriate secretion of antidiuretic hormone.Am J Med.1967;42:790–806.
- .Hyponatremia and Hypo‐osmolar Disorders. In: Greenberg A, Cheung AK, Coffman TM, Falk RJ, Jennette JC, eds.Primer on Kidney Diseases.Philadelphia:Saunders Elsevier,2009:52–59.
- ,,,.Reset of osmoreceptors in association with normovolemic hyponatremia.Am J Med Sci.1974;267:267–273.
- .Hyponatremia and inappropriate secretion of vasopressin (antidiuretic hormone) in patients with hypopituitarism.N Eng J Med.1989;321:492–496.
- .The Syndrome of Inappropriate Antidiuretic Hormone Secretion and Other Hypoosmolar Disorders. In: Schrier RW, ed.Diseases of the Kidney and Urinary Tract.Philadelphia:Lippincott Williams 27:156–161.
- ,,.Hyponatremia in a nursing home population.J Am Geriatr Soc.1995;43(12):1410–1413.
- ,.The syndrome of inappropriate antidiuretic hormone secretion in the elderly.Am J Med.1997;103(4):270–273.
- .Diuretic‐induced hyponatremia [editorial].Arch Intern Med.1986;146(7):1295–1296.
- ,,,.A syndrome of renal sodium loss and hyponatremia probably resulting from inappropriate secretion of antidiuretic hormone.Am J Med.1957;23:529–542.
- ,,,,,.Postoperative hyponatremia despite near‐isotonic saline infusion: a phenomenon of desalination [see comments].Ann Intern Med.1997;126(1):20–25.
- ,.Hyponatremia.N Engl J Med.2000;342(21):1581–1589.
- ,,, et al.Statement of the Second International Exercise‐Associated Hyponatremia Consensus Development Conference, New Zealand, 2007.Clin J Sport Med.2008;18(2):111–121.
- ,,,.Neurologic sequelae after treatment of severe hyponatremia: a multicenter perspective.J Am Soc Nephrol.1994;4:1522–1530.
- ,,,.Randomized, controlled trial on the effect of a 20% mannitol solution and a 7.5% saline/6% dextran solution on increased intracranial pressure after brain injury.Crit Care Med.2005;33(1):196–202.
- ,,.Osmotic demyelination syndrome following correction of hyponatremia.N Engl J Med.1986;314:1535–1542.
- .Regulation of arginine vasopressin in the syndrome of inappropriate antidiuresis.Am J Med.2006;119(7 Suppl 1):S36–S42.
- .The syndrome of inappropriate secretion of antidiuretic hormone (SIADH).Semin Nephrol.2009;29(3):239–256.
- .Impact of solute intake on urine flow and water excretion.J Am Soc Nephrol.2008;19(6):1076–1078.
- ,.Demeclocycline‐induced nephrogenic diabetes insipidus. In‐vivo and in‐ vitro studies.Ann Intern Med.1973;79(5):679–683.
- ,,, et al.Involvement of arginine vasopressin and renal sodium handling in pathogenesis of hyponatremia in elderly patients.Endocr J.1996;43(1):101–108.
- ,.Urea for long‐term treatment of syndrome of inappropriate secretion of antidiuretic hormone.Br Med J (Clin Res Ed).1981;283:1081–1083.
- ,.Vasopressin receptor antagonists.Kidney Int.2006;69(12):2124–2130.
- ,,, et al.Potent aquaretic agent. A novel nonpeptide selective vasopressin 2 antagonist (OPC‐31260) in men.J Clin Invest.1993;92(6):2653–2659.
- ,,,,.Assessment of the efficacy and safety of intravenous conivaptan in euvolemic and hypervolemic hyponatremia.Am J Nephrol.2007;27(5):447–457.
- ,,, et al.Tolvaptan, a selective oral vasopressin V2‐receptor antagonist, for hyponatremia.N Engl J Med.2006;355(20):2099–2112.
- Vaprisol (conivaptan hydrochloride injection) prescribing information.Deerfield, IL:Astellas Pharma US, Inc.,2006.
- ,,,,.Hyponatremia treatment guidelines 2007: expert panel recommendations.Am J Med.2007;120(11 Suppl 1):S1–S21.
- Otsuka Pharmaceutical Co L, Tokyo J. Samsca (tolvaptan) prescribing information.2009.
- ,.Clinical practice. The syndrome of inappropriate antidiuresis.N Engl J Med.2007;356(20):2064–2072.
- ,,.The treatment of hyponatremia.Semin Nephrol.2009;29(3):282–299.
- .Hyponatremia and Hypo‐osmolar Disorders. In: Greenberg A, Cheung AK, Coffman TM, Falk RJ, Jennette JC, eds.Primer on Kidney Diseases.Philadelphia. PA:Saunders Elsevier;2009:52–59.
- ,,,.Risk factors for symptomatic hyponatraemia: the role of pre‐existing asymptomatic hyponatraemia.Intern Med J.2007;37(3):149–155.
- ,,,,.Mild chronic hyponatremia is associated with falls, unsteadiness, and attention deficits.Am J Med.2006;119(1):71.
- ,,,,.Mild hyponatremia and risk of fracture in the ambulatory elderly.QJM.2008;101(7):583–588.
- ,,,,.Hyponatremia associated with large‐bone fracture in elderly patients.Int Urol Nephrol.2009;41(3):733–737.
- ,,, et al.Hyponatremia‐induced osteoporosis.J Bone Miner Res.2010;25(3):554–563.
Why is SIADH Important to Hospitalists?
Disorders of body fluids, and particularly hyponatremia, are among the most commonly encountered problems in clinical medicine, affecting up to 30% of hospitalized patients. In a study of 303,577 laboratory samples collected from 120,137 patients, the prevalence of hyponatremia (serum [Na+] <135 mmol/L) on initial presentation to a healthcare provider was 28.2% among those treated in an acute hospital care setting, 21% among those treated in an ambulatory hospital care setting, and 7.2% in community care centers.1 Numerous other studies have corroborated a high prevalence of hyponatremia in hospitalized patients,2 which reflects the increased vulnerability of this patient population to disruptions of body fluid homeostasis. Recognizing the many possible causes of hyponatremia in hospitalized patients and implementing appropriate treatment strategies therefore are critical steps toward optimizing care and improving outcomes in hospitalized patients with hyponatremia.
In addition to its frequency, hyponatremia is also important because it has been associated with worse clinical outcomes across the entire range of inpatient care, from the general hospital population to those treated in the intensive care unit (ICU). In a study of 4123 patients age 65 years or older who were admitted to a community hospital, 3.5% had clinically significant hyponatremia (serum [Na+] <130 mmol/L) at admission. Compared with nonhyponatremic patients, those with hyponatremia were twice as likely to die during their hospital stay (relative risk [RR], 1.95; P < 0.05).3 In another study of 2188 patients admitted to a medical ICU over a 5‐year period, 13.7% had hyponatremia. The overall rate of in‐hospital mortality among all ICU patients was high at 37.7%. However, severe hyponatremia (serum [Na+] <125 mmol/L) more than doubled the risk of in‐hospital mortality (RR, 2.10; P < 0.001).4 In addition to the general hospital population, in virtually every disease ever studied, the presence of hyponatremia has been found to be an independent risk factor for increased mortality, from congestive heart failure to tuberculosis to liver failure.2
What Causes Hyponatremia in Patients with SIADH?
Hyponatremia can be caused by 1 of 2 potential disruptions in fluid balance: dilution from retained water, or depletion from electrolyte losses in excess of water. Dilutional hyponatremias are associated with either a normal (euvolemic) or an increased (hypervolemic) extracellular fluid (ECF) volume, whereas depletional hyponatremias generally are associated with a decreased ECF volume (hypovolemic). Dilutional hyponatremia can arise from a primary defect in osmoregulation, such as in SIADH, or as a result of ECF volume expansion, as seen in conditions associated with concomitant secondary hyperaldosteronism such as heart failure, hepatic cirrhosis, or nephrotic syndrome. Among some hospitalized patient groups, euvolemic hyponatremia is the most common presentation of abnormally low serum [Na+]. In a study of patients who developed clinically significant postoperative hyponatremia (defined as a serum [Na+] <130 mmol/L) in a large teaching hospital, only 8% were hypovolemic, whereas 42% were euvolemic and 21% were hypervolemic.5
Euvolemic hyponatremia results from an increase in total body water, but with normal or near‐normal total body sodium. As a result, there is an absence of clinical manifestations of ECF volume expansion, such as subcutaneous edema or ascites. It is important to recognize that although SIADH clearly represents a state of volume expansion due to water retention, it rarely causes clinically recognizable hypervolemia since the retained water is distributed across the intracellular fluid (ICF) as well as the ECF, and because volume regulatory processes act to decrease the actual degree of ECF volume expansion.6 Euvolemic hyponatremia can accompany a wide variety of pathological processes, but the most common cause by far is SIADH. Normally, increased plasma osmolality activates osmoreceptors located in the anterior hypothalamus and stimulates the secretion of arginine vasopressin (AVP), also called antidiuretic hormone (ADH), a key neurohormone that regulates fluid homeostasis. In patients with euvolemic hyponatremia due to SIADH, plasma AVP levels are not suppressed despite normal or decreased plasma osmolality.7 This can be a result of ectopic production of AVP by tumors, or stimulation of endogenous pituitary AVP secretion as a result of nonosmotic stimuli that also stimulate vasopressinergic neurons, which include hypovolemia, hypotension, angiotensin II, nausea, hypoxia, hypercarbia, hypoglycemia, stress, and physical activity. Nonsuppressed AVP levels have been documented in the majority of hyponatremic patients, including those with SIADH8 and heart failure.9
SIADH can develop as the result of many different disease processes that disrupt the normal mechanisms that regulate AVP secretion, including pneumonias and other lung infections, thoracic and extrathoracic tumors, a variety of different central nervous system disorders, the postoperative state, human immunodeficiency virus (HIV), and many different drugs (Figure 1). Given the multiplicity of disorders and drugs that can cause disrupted AVP secretion, it is not surprising that hyponatremia is the most common electrolyte abnormality seen in clinical practice.
What Symptoms are Associated With SIADH?
Symptoms of hyponatremia correlate both with the degree of decrease in the serum [Na+] and with the chronicity of the hyponatremia. Acute hyponatremia, defined as <48 hours in duration, is often associated with life‐threatening clinical features such as obtundation, seizures, coma, and respiratory arrest. These symptoms can occur abruptly, sometimes with little warning.10 In the most severe cases, death can occur as a result of cerebral edema with tentorial herniation. Hypoxia secondary to neurogenic pulmonary edema can increase the severity of brain swelling.11
In contrast, chronic hyponatremia is much less symptomatic, and the reason for the profound differences between the symptoms of acute and chronic hyponatremia is now well understood to be due to the process of brain volume regulation.12 It is essential that this process be understood in order to understand the full spectrum of hyponatremic symptoms. As the ECF [Na+] decreases, regardless of whether due to a loss of sodium or a gain of water, there is an obligate movement of water into the brain along osmotic gradients. That water shift causes swelling of the brain, or cerebral edema. If the increased brain water reaches approximately 8% in adults, it exceeds the capacity of the skull to accommodate brain expansion, leading to tentorial herniation and death from respiratory arrest and/or ischemic brain damage. However, if the patient survives the initial hyponatremia, a very strong volume regulatory process follows, consisting of loss of electrolytes and small organic molecules called osmolytes from brain cells into brain ECF, and eventually the peripheral ECF.12, 13 As the solute content of the brain decreases, the water content is allowed to normalize, eventually reaching a state in which brain edema is virtually absent, and as a result symptoms are markedly less than with acute hyponatremia. Although the time required for the brain to acieve a volume‐regulated state varies across patients, this process is completed within 48 hours in experinmental animal studies, and probably follows a similar time course in humans.
Despite this powerful adaptation process, chronic hyponatremia is frequently associated with neurological symptomatology, albeit milder and more subtle in nature. A recent report found a fairly high incidence of symptoms in 223 patients with chronic hyponatremia as a result of thiazide administration: 49% had malaise/lethargy, 47% had dizzy spells, 35% had vomiting, 17% had confusion/obtundation, 17% experienced falls, 6% had headaches, and 0.9% had seizures.14 Although dizziness can potentially be attributed to a diuretic‐induced hypovolemia, symptoms such as confusion, obtundation and seizures are more consistent with hyponatremic symptomatology. Because thiazide‐induced hyponatremia can be readily corrected by stopping the thiazide and/or administering sodium, this represents an ideal situation in which to assess improvement in hyponatremia symptomatology with normalization of the serum [Na+]; in this study, all of these symptoms improved with correction of the hyponatremia. This represents one of the best examples demonstrating reversal of the symptoms associated with chronic hyponatremia by correction of the hyponatremia, because the patients in this study did not in general have severe underlying comorbidities that might complicate interpretation of their symptoms, as is often the case in patients with SIADH.
What Is Required for Making a Diagnosis of SIADH in Hospitalized Patients?
In patients with hypotonic hypoosmolality, ascertainment of their ECF volume status (ie, hypovolemic, euvolemic, or hypervolemic) is an essential first step, as this will segregate patients into different treatment paradigms. For example, in patients who are truly clinically hypovolemic with a decreased ECF volume by clinical parameters, treatment would generally consist of solute repletion with sodium, generally isotonic saline infusion with or without potassium, until the sodium levels normalize. In patients who are hypervolemic, treatment should focus first on the underlying disease rather than addressing the serum [Na+] directly. In patients with clinical euvolemia, the standard diagnostic pathway should be followed to confirm a diagnosis of SIADH as described below.
Assessing ECF volume status can be difficult, even for the most experienced clinicians. Physical signs such as orthostatic decreases in blood pressure and increases in pulse rate, dry mucus membranes, and skin tenting indicate hypovolemic hyponatremia, while signs such as subcutaneous edema, ascites, or anasarca indicate hypervolemic hyponatremia. Patients without any of these findings are generally considered to be euvolemic. However, in any situation these signs are only applicable if there are no other reasons to suspect an altered ECF volume. Along with a complete history and physical examination that includes a careful neurological evaluation, several laboratory tests can help to assess the etiology of the hyponatremia, once serum sodium concentrations have been shown to be below normal ([Na+] <135 mmol/L):
-
Urine osmolality. A urine osmolality (Uosm) less than 100 mOsm/kg H2O can indicate low dietary solute intake, primary polydipsia, or a reset osmostat after suppression of AVP release by a decrease in plasma osmolality below the osmotic threshold for AVP secretion, usually as a result of increased water loading.
-
Urine sodium concentration. Excretion of sodium, as measured by a spot urine [Na+] (UNa), can indicate depletional hyponatremia if the concentration is less than 30 mmol/L.15 A low UNa reflects a volume depleted state unless the patient has secondary hyperaldosteronism from heart failure or cirrhosis. Patients with a low UNa are more likely to respond to isotonic saline. Euvolemic patients who have a normal dietary sodium intake will generally have spot UNa 30 mmol/L and will not benefit from isotonic saline administration.15 In fact, in SIADH, these patients may respond to isotonic saline with a worsening of hyponatremia, since the sodium from the isotonic saline will be excreted in a concentrated urine while the free water is reabsorbed in the kidney collecting ducts. If the patient is on diuretic therapy, urine sodium values cannot always be accurately interpreted, since a UNa 30 mmol/L may reflect the natriuretic effect of the diuretic and not a volume replete state.
-
Blood tests. Additional indicators of volume status include serum blood nitrogen (BUN) and uric acid levels. A BUN <10 mg/dL and uric acid <4 mg/dL are generally consistent with a euvolemic state, particularly when there is glomerular hyperfiltration, which is often present in SIADH. Elevated serum BUN and uric acid levels (BUN >20 mg/dL and uric acid >6 mg/dL), especially if prior values are available for comparison, can also help to establish whether ineffective vascular volume status may be contributing to the pathophysiology of the hyponatremia. In certain clinical scenarios, the B‐type natriuretic protein (BNP) can be helpful to support a clinical impression of congestive heart failure.
The criteria necessary for a diagnosis of SIADH remain essentially as defined by Bartter and Schwartz16 in 1967 (Table 1), but several points deserve emphasis.17 First, true ECF hypoosmolality must be present and hyponatremia secondary to pseudohyponatremia or hyperglycemia excluded. Second, urinary osmolality must be inappropriate for plasma hypoosmolality (Posm). This does not require a Uosm>Posm, but simply that the urine osmolality is greater than maximally dilute (ie, Uosm>100 mOsm/kg H2O in adults). Furthermore, urine osmolality need not be inappropriately elevated at all levels of Posm but simply at some level under 275 mOsm/kg H2O, since in patients with a reset osmostat, AVP secretion can be suppressed at some level of osmolality resulting in maximal urinary dilution and free water excretion at plasma osmolalities below this level.18 Although some consider a reset osmostat to be a separate disorder rather than a variant of SIADH, such cases nonetheless illustrate that some hypoosmolar patients can exhibit an appropriately dilute urine at some, though not all, plasma osmolalities. Third, clinical euvolemia must be present to diagnose SIADH, and this diagnosis cannot be made in a hypovolemic or edematous patient. Importantly, this does not mean that patients with SIADH cannot become hypovolemic for other reasons, but in such cases it is impossible to diagnose the underlying SIADH until the patient is rendered euvolemic. The fourth criterion, renal salt wasting, has probably caused the most confusion in the diagnosis of SIADH. As noted above, the importance of this criterion lies in its usefulness in differentiating hypoosmolality caused by a decreased effective intravascular volume with high aldosterone levels in which case renal Na+ conservation occurs, from dilutional disorders in which urine Na+ excretion is normal or increased due to ECF volume expansion and a suppressed renin‐angiotensin‐aldosterone system. However, UNa can also be high in renal causes of solute depletion such as diuretic use or Addison's disease, and conversely patients with SIADH can have a low UNa if they subsequently become hypovolemic or solute depleted, conditions sometimes produced by imposed salt and water restriction. Consequently, although high urinary Na+ excretion is generally the rule in most patients with SIADH, its presence does not necessarily confirm this diagnosis, nor does its absence rule out the diagnosis. The final criterion emphasizes that SIADH remains a diagnosis of exclusion, and the absence of other potential causes of hypoosmolality must always be verified. Glucocorticoid deficiency and SIADH can be especially difficult to distinguish, since both primary and secondary hypocortisolism can cause elevated plasma AVP levels in addition to direct renal effects that prevent maximal urinary dilution.19 Therefore, no patient with chronic hyponatremia should be diagnosed as having SIADH without a thorough evaluation of adrenal function, preferably via a rapid adrenocorticotropic hormone (ACTH) stimulation test. Acute hyponatremia of obvious etiology, such as postoperatively or in association with pneumonitis, may be treated without adrenal testing as long as there are no other clinical signs or symptoms suggestive of adrenal dysfunction.20
|
| Essential |
| Decreased effective osmolality of the extracellular fluid (Posm< 275 mOsm/kg H2O). |
| Inappropriate urinary concentration (Uosm >100 mOsm/kg H2O with normal renal function) at some level of hypoosmolality. |
| Clinical euvolemia, as defined by the absence of signs of hypovolemia (orthostasis, tachycardia, decreased skin turgor, dry mucous membranes) or hypervolemia (subcutaneous edema, ascites). |
| Elevated urinary sodium excretion while on a normal salt and water intake. |
| Absence of other potential causes of euvolemic hypoosmolality: hypothyroidism, hypocortisolism (Addison's disease or secondary adrenal insufficiency) and diuretic use. |
| Supplemental |
| Abnormal water load test (inability to excrete at least 90% of a 20 mL/kg water load in 4 hours and/or failure to dilute Uosm to <100 mOsm/kg H2O). |
| Plasma AVP level inappropriately elevated relative to plasma osmolality. |
| No significant correction of serum [Na+] with volume expansion but improvement after fluid restriction. |
Hyponatremia is a particularly common complication in elderly hospitalized patients, increasing in prevalence from approximately 7% in the general older population to 18% to 22% among elderly patients in chronic care facilities.21 Despite the many known causes of SIADH (Figure 1), hyponatremia is often associated with idiopathic SIADH in the elderly population. In a study of 119 nursing home residents aged 60 to 103 years, 53% had at least 1 episode of hyponatremia during the previous 12 months.22 Of these patients, 26% were diagnosed with idiopathic SIADH. In another study of elderly patients with hyponatremia and SIADH, 60% were diagnosed with idiopathic SIADH. Among remaining patients, the 2 main causes identified were pneumonia (9 cases/18%) and medications (6 cases/12%).23 Therefore, more than half of elderly patients who present with hyponatremia due to SIADH may have an idiopathic form, with no detectable underlying treatable disease.
Which Hospital Patients With SIADH are Candidates for Treatment of Hyponatremia?
Correction of hyponatremia is associated with markedly improved neurological outcomes in patients with severely symptomatic hyponatremia. In a retrospective review of patients who presented with severe neurological symptoms and serum [Na+] <125 mmol/L, prompt therapy with isotonic or hypertonic saline resulted in a correction in the range of 20 mmol/L over several days and neurological recovery in almost all cases. In contrast, in patients who were treated with fluid restriction alone, there was very little correction over the study period (<5 mmol/L over 72 hours), and the neurological outcomes were much worse, with most of these patients either dying or entering a persistently vegetative state.24 Consequently, prompt therapy to rapidly increase the serum [Na+] represents the standard‐of‐care for treatment of patients presenting with severe life‐threatening symptoms of hyponatremia.
As discussed earlier, chronic hyponatremia is much less symptomatic as a result of the process of brain volume regulation. Because of this adaptation process, chronic hyponatremia is arguably a condition that clinicians feel they may not need to be as concerned about, and in some publications this has been called asymptomatic hyponatremia. However, such patients often do have neurological symptoms, even if milder and more subtle in nature, including headaches, nausea, mood disturbances, depression, difficulty concentrating, slowed reaction times, unstable gait, increased falls, confusion, and disorientation. Consequently, any patient with hyponatremia secondary to SIADH who manifests any neurological symptoms that could be related to the hyponatremia should be considered as appropriate candidates for treatment of the hyponatremia, regardless of the chronicity of the hyponatremia or the level of serum [Na+].
What Therapies are Currently Available to Manage SIADH in Hospitalized Patients?
Conventional management strategies for euvolemic hyponatremia range from saline infusion and fluid restriction to pharmacologic adjustment of fluid balance. Consideration of treatment options should include an evaluation of the benefits as well as the potential toxicities of any therapy (Table 2). Sometimes, simply stopping treatment with an agent that is associated with hyponatremia is sufficient to reverse a low serum [Na+].
| Therapy | Targets Underlying Pathophysiology | Limitations |
|---|---|---|
| ||
| Isotonic saline | Ineffective in dilutional hyponatremias; exacerbates the volume overload if used in edema‐forming disorders; no controlled safety database. | |
| Hypertonic saline | No consensus regarding appropriate infusion rates; overcorrection can cause osmotic demyelination; exacerbates the volume overload if used in edema‐forming disorders; no controlled safety database. | |
| Fluid restriction | Slow to correct over many days; poorly tolerated due to thirst; can not be used effectively in patients with high AVP levels and urine osmolalities. | |
| Demeclocycline | ✓ | Not FDA approved for hyponatremia; slow to correct; nephrotoxic in cirrhosis and heart failure. |
| Mineralocorticoids | Only one report in elderly patients with SIADH; no safety database; exacerbates the volume overload if used in edema‐forming disorders. | |
| Urea | Not FDA‐approved for hyponatremia; poor palatability. | |
| AVP receptor antagonists (vaptans) | ✓ | Conivaptan approved only for in‐hospital use secondary to CYP3A4 inhibition; infusion‐site reactions with intravenous use. Tolvaptan must be initiated and reinitiated in the hospital, as serum sodium needs to be monitored closely to avoid overly rapid correction of hyponatremia. |
Isotonic Saline
The treatment of choice for depletional hyponatremia (ie, hypovolemic hyponatremia) is isotonic saline ([Na+] = 154 mmol/L) to restore ECF volume and ensure adequate organ perfusion. This initial therapy is appropriate for patients who either have clinical signs of hypovolemia, or in whom a spot UNa+ is <30 mmol/L. However, this therapy is ineffective for dilutional hyponatremias such as SIADH,25 and continued inappropriate administration of isotonic saline to a euvolemic patient may worsen their hyponatremia,26 and/or cause fluid overload. Although isotonic saline may improve the serum [Na+] in patients with hypervolemic hyponatremia, their volume status will generally worsen with this therapy, so unless the hyponatremia is profound isotonic saline should be avoided.
Hypertonic Saline
Acute hyponatremia presenting with severe neurological symptoms is life‐threatening, and should be treated promptly with hypertonic solutions, typically 3% NaCl ([Na+] = 513 mmol/L), as this represents the most reliable method to quickly raise the serum [Na+]. A continuous infusion of hypertonic NaCl is usually utilized in inpatient settings. Various formulae have been suggested for calculating the initial rate of infusion of hypertonic solutions,27 but perhaps the simplest utilizes the following relationship:
An alternative option for more emergent situations is administration of a 100 mL bolus of 3% NaCl, repeated once if no clinical improvement, which has been recommended by a consensus conference organized to develop guidelines for prevention and treatment of exercise‐induced hyponatremia, an acute and potentially lethal condition.28 Injecting this amount of hypertonic saline intravenously raises the serum [Na+] by an average of 2 mmol/L to 4 mmol/L, which is well below the recommended maximal daily rate of change of 10 to 12 mmol/24 hours or 18 mmol/48 hours.29 Because the brain can only accommodate an average increase of approximately 8% in brain volume before herniation occurs, quickly increasing the serum [Na+] by as little as 2 mmol/L to 4 mmol/L in acute hyponatremia can effectively reduce brain swelling and intracranial pressure.30 Unfortunately, until now there has been no consensus regarding appropriate infusion rates of 3% NaCl, and many physicians are hesitant to use it in patients with chronic hyponatremia because it can cause an overly rapid correction of serum sodium levels that can lead to the osmotic demyelination syndrome (ODS).31 Nonetheless, this remains the treatment of choice for patients with severe neurological symptoms, even when the time course of the hyponatremia is nonacute or unknown. The administration of hypertonic saline is generally not recommended for most patients with edema‐forming disorders because it acts as a volume expander and may exacerbate volume overload.
Fluid Restriction
For patients with chronic hyponatremia, fluid restriction has been the most popular and most widely accepted treatment. When SIADH is present, generally fluids should be limited to 500 to 1000 mL/24 hours. Because fluid restriction increases the serum [Na+] largely by under‐replacing the excretion of fluid by the kidneys, some have advocated an initial restriction to 500 mL less than the 24‐hour urine output.32 When instituting a fluid restriction, it is important for the nursing staff and the patient to understand that this includes all fluids that are consumed, not just water. Generally the water content of ingested food is not included in the restriction because this is balanced by insensible water losses (perspiration, exhaled air, feces, etc.), but caution should be exercised with foods that have high fluid concentrations (such as fruits and soups). Restricting fluid intake is effective when properly applied and managed, but serum sodium levels are increased only slowly (1‐2 mmol/L/day) even with severe restriction.25 In addition, this therapy is often poorly tolerated because of an associated increase in thirst. However, it is economically favorable, and some patients do respond well to this option. Fluid restriction should not be used with hypovolemic patients, and is particularly difficult to maintain in patients with very elevated urine osmolalities secondary to high AVP levels; in general, if the sum of urine Na+ and K+ exceeds the serum [Na+], most patients will not respond to a fluid restriction since an electrolyte‐free water clearance will be difficult to achieve,33, 34 and in patients in intensive care settings who often require administration of fluids as part of their therapies.
Demeclocycline
Demeclocycline, a tetracycline antibiotic, inhibits adenylyl cyclase activation after AVP binds to its V2 receptor in the kidney, and thus targets the underlying pathophysiology of SIADH. This therapy is typically used when patients find severe fluid restriction unacceptable and the underlying disorder cannot be corrected. However, demeclocycline is not approved by the U.S. Food and Drug Administration (FDA) to treat hyponatremia, and can cause nephrotoxicity in patients with heart failure and cirrhosis, although this is usually reversible if caught quickly enough.35
Mineralocorticoids
Administration of mineralocorticoids, such as fludrocortisone, has been shown to be useful in a small number of elderly patients.36 However, the initial studies of SIADH did not show it to be of benefit in patients with SIADH, and it carries the risk of fluid overload and hypertension. Consequently, it is rarely used to treat hyponatremia in the U.S.
Urea
Administration of urea has been successfully used to treat hyponatremia because it induces osmotic diuresis and augments free water excretion. Effective doses of urea for treatment of hyponatremia are 30 gm to 60 gm daily in divided doses.37 Unfortunately, its use is limited because there is no United States Pharmacopeia (USP) formulation for urea, and it is not approved by the FDA for treatment of hyponatremia. As such, urea has not been used extensively in the United States, and there are limited data to support its long‐term use. Furthermore, urea is associated with poor palatability; however, patients with feeding tubes may be excellent candidates for urea therapy since palatability is not a concern, and the use of fluid restriction may be difficult in some patients with high obligate intake of fluids as part of their nutritional and medication therapy. Although mild azotemia can be seen with urea therapy, this rarely reaches clinically significant levels.
Clinicians have used all of the above conventional therapies for hyponatremia over the past decades. However, conventional therapies for hyponatremia, although effective in specific circumstances, are suboptimal for many different reasons, including variable efficacy, slow responses, intolerable side effects, and serious toxicities, as summarized in Table 2. But perhaps the most striking deficiency of most conventional therapies is that with the exception of demeclocycline, these therapies do not directly target the underlying cause of most all dilutional hyponatremias, namely inappropriately elevated plasma AVP levels. A new class of pharmacological agents, vasopressin receptor antagonists, that directly block AVP‐mediated receptor activation have recently been approved by the FDA for treatment of euvolemic and hypervolemic hyponatremia.38
AVP Receptor (AVPR) Antagonists
Conivaptan and tolvaptan are antagonists of the AVP V2 (antidiuretic) receptor and have been approved by the FDA for the treatment of euvolemic and hypervolemic hyponatremia. These agents, also known as vaptans, compete with AVP/ADH for binding at its site of action in the kidney, thereby blocking the antidiuresis caused by elevated AVP levels and directly attacking the underlying pathophysiology of dilutional hyponatremia. AVPR antagonists produce electrolyte free water excretion (called aquaresis) without affecting renal sodium and potassium excretion.39 The overall result is a reduction in body water without natriuresis, which leads to an increase in the serum [Na+]. One of the major benefits of this class of drugs is that serum [Na+] is significantly increased within 24 to 48 hours,40, 41 which is considerably faster than the effects of fluid restriction that can take many days. Also, compliance has not been shown to be problem for vaptans, whereas this is a major problem with attempted long‐term use of fluid restriction.
Conivaptan is FDA‐approved for euvolemic and hypervolemic hyponatremia in hospitalized patients. It is available only as an intravenous preparation, and is given as a 20 mg loading dose over 30 minutes, followed by a continuous infusion of 20 or 40 mg.42 Generally, the 20 mg continuous infusion is used for the first 24 hours to gauge the initial response. If the correction of serum [Na+] is felt to be inadequate (eg, <5 mmol/L), then the infusion rate can be increased to 40 mg/day. Therapy is limited to a maximum duration of 4 days because of drug‐interaction effects with other agents metabolized by the cytochrome P450 3A4 (CYP3A4) hepatic isoenzymes. Importantly, for conivaptan and all other vaptans, it is critical that the serum [Na+] concentration is measured frequently during the active phase of correction of the hyponatremia (a minimum of every 6 hours, but more frequently in patients with risk factors for development of osmotic demyelination, such as severely low serum [Na+], malnutrition, alcoholism and hypokalemia).43 If the correction approaches 12 mmol/L in the first 24 hours, the infusion should be stopped and the patient monitored on a fluid restriction. If the correction exceeds 12 mmol/L, consideration should be given to administering sufficient water, either orally or as intravenous D5W to bring the overall correction below 12 mmol/L. The maximum correction limit should be reduced to 8 mmol/L over the first 24 hours in patients with risk factors for development of osmotic demyelination. The most common adverse effects include injection‐site reactions, which are generally mild and usually do not lead to treatment discontinuation, headache, thirst, and hypokalemia.40
Tolvaptan, an oral AVPR antagonist, is FDA‐approved for treatment of dilutional hyponatremias. In contrast to conivaptan, oral administration allows it to be used for both short‐term and long‐term treatment of hyponatremia.41 Similar to conivaptan, tolvaptan treatment must be initiated in the hospital so that the rate of correction can be monitored carefully. Patients with a serum [Na+] <125 mmol/L are eligible for therapy with tolvaptan as primary therapy; if the serum [Na+] is 125 mmol/L, tolvaptan therapy is only indicated if the patient has symptoms that could be attributable to the hyponatremia and the patient is resistant to attempts at fluid restriction.44 The starting dose of tolvaptan is 15 mg on the first day, and the dose can be titrated to 30 mg and 60 mg at 24‐hour intervals if the serum [Na+] remains <135 mmol/L or the increase in serum [Na+] has been 5 mmol/L in the previous 24 hours. As with conivaptan, it is essential that the serum [Na+] concentration is measured frequently during the active phase of correction of the hyponatremia (a minimum of every 8 hrs, but more frequently in patients with risk factors for development of osmotic demyelination). Limits for safe correction of hyponatremia and methods to compensate for overly rapid corrections are the same as described previously for conivaptan. Common side effects include dry mouth, thirst, increased urinary frequency, dizziness, nausea and orthostatic hypotension, which were relatively similar between placebo and tolvaptan groups in clinical trials.41, 44
Because inducing increased renal fluid excretion via either a diuresis or an aquaresis can cause or worsen hypotension in patients with hypovolemic hyponatremia, vaptans are contraindicated in this patient population.43 However, clinically significant hypotension was not observed in either the conivaptan or tolvaptan clinical trials in euvolemic and hypervolemic hyponatremic patients. Although vaptans are not contraindicated with decreased renal function, these agents generally will not be effective if the serum creatinine is >2.5 mg/dL.
Hyponatremia Treatment Guidelines for Hospitalized Patients With SIADH
Although various authors have published recommendations on the treatment of hyponatremia,27, 43, 45‐47 no standardized treatment algorithms have yet been widely accepted. A synthesis of existing expert recommendations for treatment of hyponatremia is illustrated in Figure 2. This algorithm is based primarily on the symptomatology of hyponatremic patients, rather than the serum [Na+] or the chronicity of the hyponatremia, which are often difficult to ascertain. A careful neurological history and assessment should always be done to identify potential causes for the patient's symptoms other than hyponatremia, although it will not always be possible to exclude an additive contribution from the hyponatremia to an underlying neurological condition. In this model, patients are divided into three groups based on their presenting symptoms.
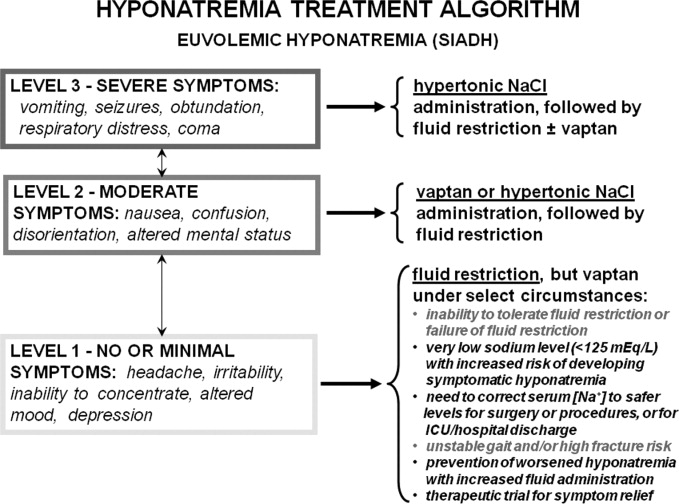
Level 1 symptoms include seizures, coma, respiratory arrest, obtundation, and vomiting, and usually imply a more acute onset or worsening of hyponatremia requiring immediate active treatment. Therapies that will quickly raise serum sodium levels are required to reduce cerebral edema and decrease the risk of potentially fatal herniation.
Level 2 symptoms, which are more moderate, include nausea, confusion, disorientation, and altered mental status. These symptoms may be either chronic or acute, but allow time to elaborate a more deliberate approach to treatment.
Level 3 symptoms range from minimal symptoms such as a headache, irritability, inability to concentrate, altered mood, and depression, to a virtual absence of discernable symptoms, and indicate that the patient may have chronic or slowly evolving hyponatremia. These symptoms necessitate a cautious approach, especially when patients have underlying comorbidities.
Patients with severe symptoms (Level 1) should be treated with hypertonic saline as first‐line therapy, followed by fluid restriction with or without AVPR antagonist therapy. Patients with moderate symptoms will benefit from a more aggressive regimen of vaptan therapy or limited hypertonic saline administration, followed by fluid restriction or long‐term vaptan therapy. Although moderate neurological symptoms can indicate that a patient is in an early stage of acute hyponatremia, they more often indicate a chronically hyponatremic state with sufficient brain volume adaptation to prevent marked symptomatology from cerebral edema. Regardless, close monitoring of these patients in a hospital setting is warranted until the symptoms improve or stabilize. Patients with no or minimal symptoms should be managed initially with fluid restriction, although treatment with vaptans may be appropriate for a wide range of specific clinical conditions, foremost of which is a failure to improve the serum [Na+] despite reasonable attempts at fluid restriction (Figure 2).
Although this classification is based on presenting symptoms at the time of initial evaluation, it should be remembered that in some cases patients initially exhibit more moderate symptoms because they are in the early stages of hyponatremia. In addition, some patients with minimal symptoms are prone to develop more symptomatic hyponatremia during periods of increased fluid ingestion. In support of this, approximately 70% of 31 patients presenting to a university hospital with symptomatic hyponatremia and a mean serum [Na+] of 119 mmol/L had preexisting asymptomatic hyponatremia as the most common risk factor identified.48 Consequently, therapy of hyponatremia should also be considered to prevent progression from lower to higher levels of symptomatic hyponatremia, particularly in patients with a past history of repeated presentations of symptomatic hyponatremia.
How Often Should Serum [Na+] Be Monitored in Hospitalized Patients With SIADH?
The frequency of serum [Na+] monitoring is dependent on both the severity of the hyponatremia and the therapy chosen. In all hyponatremic patients neurological symptomatology should be carefully assessed very early in the diagnostic evaluation to assess the symptomatic severity of the hyponatremia and to determine whether the patient requires more urgent therapy. All patients undergoing active treatment with hypertonic saline for level 1 or 2 symptomatic hyponatremia should have frequent monitoring of serum [Na+] and ECF volume status (every 2‐4 hours) to ensure that the serum [Na+] does not exceeded the recommended levels during the active phase of correction,43 since overly rapid correction of serum sodium can cause damage to the myelin sheath of nerve cells, resulting in central pontine myelinolysis, also called the ODS.31 Patients treated with vaptans for level 2 or 3 symptoms should have serum [Na+] monitored every 6 to 8 hours during the active phase of correction, which will generally be the first 24 to 48 hours of therapy. Active treatment with hypertonic saline or vaptans should be stopped when the patient's symptoms are no longer present, a safe serum [Na+] (usually >120 mmol/L) has been achieved, or the rate of correction has reached 12 mmol/L within 24 hours or 18 mmol/L within 48 hours.29, 43 Importantly, ODS has not been reported either in clinical trials or with therapeutic use of any vaptan to date. In patients with a stable level of serum [Na+] treated with fluid restriction or therapies other than hypertonic saline, measurement of serum [Na+] daily is generally sufficient, since levels will not change that quickly in the absence of active therapy or large changes in fluid intake or administration.
Potential Future Indications for Treatment of Hyponatremia
Correction of hyponatremia improves other symptoms, such as gait stability, in patients who may be considered to be asymptomatic by virtue of a normal neurological exam. In 1 study, 16 patients with hyponatremia secondary to SIADH in the range of 124 mmol/L to 130 mmol/L demonstrated a significant gait instability that normalized after correction of the hyponatremia to normal ranges.49 The functional significance of the gait instability was illustrated in a study of 122 Belgian patients with a variety of levels of hyponatremia, all judged to be asymptomatic at the time of visit to an emergency department (ED). These patients were compared with 244 age‐matched, sex‐matched, and disease‐matched controls also presenting to the ED during the same time period. Researchers found that 21% of the hyponatremic patients presented to the ED because of a recent fall, compared to only 5% of the controls, resulting in an adjusted odds ratio (OR) for presenting to the ED because of a recent fall of 67 for hyponatremia (P < 0.001).49 Consequently, this study clearly documented an increased incidence of falls in so‐called asymptomatic hyponatremic patients.
The clinical significance of the gait instability and fall data were further evaluated in a study that compared 553 patients with fractures to an equal number of age‐matched and sex‐matched controls. Hyponatremia was found in 13% of the patients presenting with fractures compared to only 4% of the controls.50 Similar findings have been reported in a 364 elderly patients with large‐bone fractures in New York.51 More recently published studies have shown that hyponatremia is associated with increased bone loss in experimental animals and a significant increased OR for osteoporosis of the femoral neck (OR, 2.87; P < 0.003) in humans over the age of 50 in the NHANES III database.52 Thus, the major clinical significance of chronic hyponatremia may be the increased morbidity and mortality associated with falls and fractures in our elderly population.
Summary
Disorders of sodium and water metabolism are commonly encountered in the hospital setting due to the wide range of disease states that can disrupt the balanced control of water and solute intake and output. In particular, the prompt identification and appropriate management of abnormally low serum [Na+] is critical if we are to reduce the increased morbidity and mortality that accompany hyponatremia in hospitalized patients. Use of an algorithm that is based primarily on the symptomatology of hyponatremic patients, rather than the chronicity of the hyponatremia or the serum [Na+], will help to choose the correct initial therapy in hospitalized hyponatremic patients. However, careful monitoring of serum [Na+] responses is required in all cases to adjust therapy appropriately in response to changing clinical conditions. Although this approach will enable efficacious and safe treatment of hyponatremic patients with SIADH at the present time, evolving knowledge of the consequences of chronic hyponatremia will likely alter treatment indications and guidelines in the future.
Why is SIADH Important to Hospitalists?
Disorders of body fluids, and particularly hyponatremia, are among the most commonly encountered problems in clinical medicine, affecting up to 30% of hospitalized patients. In a study of 303,577 laboratory samples collected from 120,137 patients, the prevalence of hyponatremia (serum [Na+] <135 mmol/L) on initial presentation to a healthcare provider was 28.2% among those treated in an acute hospital care setting, 21% among those treated in an ambulatory hospital care setting, and 7.2% in community care centers.1 Numerous other studies have corroborated a high prevalence of hyponatremia in hospitalized patients,2 which reflects the increased vulnerability of this patient population to disruptions of body fluid homeostasis. Recognizing the many possible causes of hyponatremia in hospitalized patients and implementing appropriate treatment strategies therefore are critical steps toward optimizing care and improving outcomes in hospitalized patients with hyponatremia.
In addition to its frequency, hyponatremia is also important because it has been associated with worse clinical outcomes across the entire range of inpatient care, from the general hospital population to those treated in the intensive care unit (ICU). In a study of 4123 patients age 65 years or older who were admitted to a community hospital, 3.5% had clinically significant hyponatremia (serum [Na+] <130 mmol/L) at admission. Compared with nonhyponatremic patients, those with hyponatremia were twice as likely to die during their hospital stay (relative risk [RR], 1.95; P < 0.05).3 In another study of 2188 patients admitted to a medical ICU over a 5‐year period, 13.7% had hyponatremia. The overall rate of in‐hospital mortality among all ICU patients was high at 37.7%. However, severe hyponatremia (serum [Na+] <125 mmol/L) more than doubled the risk of in‐hospital mortality (RR, 2.10; P < 0.001).4 In addition to the general hospital population, in virtually every disease ever studied, the presence of hyponatremia has been found to be an independent risk factor for increased mortality, from congestive heart failure to tuberculosis to liver failure.2
What Causes Hyponatremia in Patients with SIADH?
Hyponatremia can be caused by 1 of 2 potential disruptions in fluid balance: dilution from retained water, or depletion from electrolyte losses in excess of water. Dilutional hyponatremias are associated with either a normal (euvolemic) or an increased (hypervolemic) extracellular fluid (ECF) volume, whereas depletional hyponatremias generally are associated with a decreased ECF volume (hypovolemic). Dilutional hyponatremia can arise from a primary defect in osmoregulation, such as in SIADH, or as a result of ECF volume expansion, as seen in conditions associated with concomitant secondary hyperaldosteronism such as heart failure, hepatic cirrhosis, or nephrotic syndrome. Among some hospitalized patient groups, euvolemic hyponatremia is the most common presentation of abnormally low serum [Na+]. In a study of patients who developed clinically significant postoperative hyponatremia (defined as a serum [Na+] <130 mmol/L) in a large teaching hospital, only 8% were hypovolemic, whereas 42% were euvolemic and 21% were hypervolemic.5
Euvolemic hyponatremia results from an increase in total body water, but with normal or near‐normal total body sodium. As a result, there is an absence of clinical manifestations of ECF volume expansion, such as subcutaneous edema or ascites. It is important to recognize that although SIADH clearly represents a state of volume expansion due to water retention, it rarely causes clinically recognizable hypervolemia since the retained water is distributed across the intracellular fluid (ICF) as well as the ECF, and because volume regulatory processes act to decrease the actual degree of ECF volume expansion.6 Euvolemic hyponatremia can accompany a wide variety of pathological processes, but the most common cause by far is SIADH. Normally, increased plasma osmolality activates osmoreceptors located in the anterior hypothalamus and stimulates the secretion of arginine vasopressin (AVP), also called antidiuretic hormone (ADH), a key neurohormone that regulates fluid homeostasis. In patients with euvolemic hyponatremia due to SIADH, plasma AVP levels are not suppressed despite normal or decreased plasma osmolality.7 This can be a result of ectopic production of AVP by tumors, or stimulation of endogenous pituitary AVP secretion as a result of nonosmotic stimuli that also stimulate vasopressinergic neurons, which include hypovolemia, hypotension, angiotensin II, nausea, hypoxia, hypercarbia, hypoglycemia, stress, and physical activity. Nonsuppressed AVP levels have been documented in the majority of hyponatremic patients, including those with SIADH8 and heart failure.9
SIADH can develop as the result of many different disease processes that disrupt the normal mechanisms that regulate AVP secretion, including pneumonias and other lung infections, thoracic and extrathoracic tumors, a variety of different central nervous system disorders, the postoperative state, human immunodeficiency virus (HIV), and many different drugs (Figure 1). Given the multiplicity of disorders and drugs that can cause disrupted AVP secretion, it is not surprising that hyponatremia is the most common electrolyte abnormality seen in clinical practice.
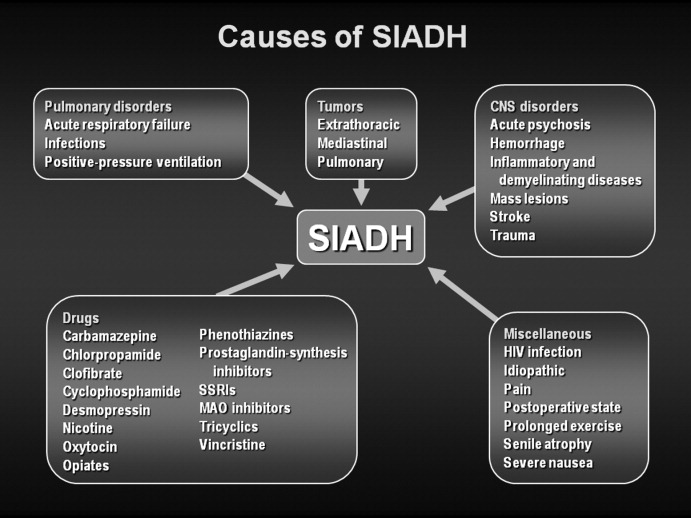
What Symptoms are Associated With SIADH?
Symptoms of hyponatremia correlate both with the degree of decrease in the serum [Na+] and with the chronicity of the hyponatremia. Acute hyponatremia, defined as <48 hours in duration, is often associated with life‐threatening clinical features such as obtundation, seizures, coma, and respiratory arrest. These symptoms can occur abruptly, sometimes with little warning.10 In the most severe cases, death can occur as a result of cerebral edema with tentorial herniation. Hypoxia secondary to neurogenic pulmonary edema can increase the severity of brain swelling.11
In contrast, chronic hyponatremia is much less symptomatic, and the reason for the profound differences between the symptoms of acute and chronic hyponatremia is now well understood to be due to the process of brain volume regulation.12 It is essential that this process be understood in order to understand the full spectrum of hyponatremic symptoms. As the ECF [Na+] decreases, regardless of whether due to a loss of sodium or a gain of water, there is an obligate movement of water into the brain along osmotic gradients. That water shift causes swelling of the brain, or cerebral edema. If the increased brain water reaches approximately 8% in adults, it exceeds the capacity of the skull to accommodate brain expansion, leading to tentorial herniation and death from respiratory arrest and/or ischemic brain damage. However, if the patient survives the initial hyponatremia, a very strong volume regulatory process follows, consisting of loss of electrolytes and small organic molecules called osmolytes from brain cells into brain ECF, and eventually the peripheral ECF.12, 13 As the solute content of the brain decreases, the water content is allowed to normalize, eventually reaching a state in which brain edema is virtually absent, and as a result symptoms are markedly less than with acute hyponatremia. Although the time required for the brain to acieve a volume‐regulated state varies across patients, this process is completed within 48 hours in experinmental animal studies, and probably follows a similar time course in humans.
Despite this powerful adaptation process, chronic hyponatremia is frequently associated with neurological symptomatology, albeit milder and more subtle in nature. A recent report found a fairly high incidence of symptoms in 223 patients with chronic hyponatremia as a result of thiazide administration: 49% had malaise/lethargy, 47% had dizzy spells, 35% had vomiting, 17% had confusion/obtundation, 17% experienced falls, 6% had headaches, and 0.9% had seizures.14 Although dizziness can potentially be attributed to a diuretic‐induced hypovolemia, symptoms such as confusion, obtundation and seizures are more consistent with hyponatremic symptomatology. Because thiazide‐induced hyponatremia can be readily corrected by stopping the thiazide and/or administering sodium, this represents an ideal situation in which to assess improvement in hyponatremia symptomatology with normalization of the serum [Na+]; in this study, all of these symptoms improved with correction of the hyponatremia. This represents one of the best examples demonstrating reversal of the symptoms associated with chronic hyponatremia by correction of the hyponatremia, because the patients in this study did not in general have severe underlying comorbidities that might complicate interpretation of their symptoms, as is often the case in patients with SIADH.
What Is Required for Making a Diagnosis of SIADH in Hospitalized Patients?
In patients with hypotonic hypoosmolality, ascertainment of their ECF volume status (ie, hypovolemic, euvolemic, or hypervolemic) is an essential first step, as this will segregate patients into different treatment paradigms. For example, in patients who are truly clinically hypovolemic with a decreased ECF volume by clinical parameters, treatment would generally consist of solute repletion with sodium, generally isotonic saline infusion with or without potassium, until the sodium levels normalize. In patients who are hypervolemic, treatment should focus first on the underlying disease rather than addressing the serum [Na+] directly. In patients with clinical euvolemia, the standard diagnostic pathway should be followed to confirm a diagnosis of SIADH as described below.
Assessing ECF volume status can be difficult, even for the most experienced clinicians. Physical signs such as orthostatic decreases in blood pressure and increases in pulse rate, dry mucus membranes, and skin tenting indicate hypovolemic hyponatremia, while signs such as subcutaneous edema, ascites, or anasarca indicate hypervolemic hyponatremia. Patients without any of these findings are generally considered to be euvolemic. However, in any situation these signs are only applicable if there are no other reasons to suspect an altered ECF volume. Along with a complete history and physical examination that includes a careful neurological evaluation, several laboratory tests can help to assess the etiology of the hyponatremia, once serum sodium concentrations have been shown to be below normal ([Na+] <135 mmol/L):
-
Urine osmolality. A urine osmolality (Uosm) less than 100 mOsm/kg H2O can indicate low dietary solute intake, primary polydipsia, or a reset osmostat after suppression of AVP release by a decrease in plasma osmolality below the osmotic threshold for AVP secretion, usually as a result of increased water loading.
-
Urine sodium concentration. Excretion of sodium, as measured by a spot urine [Na+] (UNa), can indicate depletional hyponatremia if the concentration is less than 30 mmol/L.15 A low UNa reflects a volume depleted state unless the patient has secondary hyperaldosteronism from heart failure or cirrhosis. Patients with a low UNa are more likely to respond to isotonic saline. Euvolemic patients who have a normal dietary sodium intake will generally have spot UNa 30 mmol/L and will not benefit from isotonic saline administration.15 In fact, in SIADH, these patients may respond to isotonic saline with a worsening of hyponatremia, since the sodium from the isotonic saline will be excreted in a concentrated urine while the free water is reabsorbed in the kidney collecting ducts. If the patient is on diuretic therapy, urine sodium values cannot always be accurately interpreted, since a UNa 30 mmol/L may reflect the natriuretic effect of the diuretic and not a volume replete state.
-
Blood tests. Additional indicators of volume status include serum blood nitrogen (BUN) and uric acid levels. A BUN <10 mg/dL and uric acid <4 mg/dL are generally consistent with a euvolemic state, particularly when there is glomerular hyperfiltration, which is often present in SIADH. Elevated serum BUN and uric acid levels (BUN >20 mg/dL and uric acid >6 mg/dL), especially if prior values are available for comparison, can also help to establish whether ineffective vascular volume status may be contributing to the pathophysiology of the hyponatremia. In certain clinical scenarios, the B‐type natriuretic protein (BNP) can be helpful to support a clinical impression of congestive heart failure.
The criteria necessary for a diagnosis of SIADH remain essentially as defined by Bartter and Schwartz16 in 1967 (Table 1), but several points deserve emphasis.17 First, true ECF hypoosmolality must be present and hyponatremia secondary to pseudohyponatremia or hyperglycemia excluded. Second, urinary osmolality must be inappropriate for plasma hypoosmolality (Posm). This does not require a Uosm>Posm, but simply that the urine osmolality is greater than maximally dilute (ie, Uosm>100 mOsm/kg H2O in adults). Furthermore, urine osmolality need not be inappropriately elevated at all levels of Posm but simply at some level under 275 mOsm/kg H2O, since in patients with a reset osmostat, AVP secretion can be suppressed at some level of osmolality resulting in maximal urinary dilution and free water excretion at plasma osmolalities below this level.18 Although some consider a reset osmostat to be a separate disorder rather than a variant of SIADH, such cases nonetheless illustrate that some hypoosmolar patients can exhibit an appropriately dilute urine at some, though not all, plasma osmolalities. Third, clinical euvolemia must be present to diagnose SIADH, and this diagnosis cannot be made in a hypovolemic or edematous patient. Importantly, this does not mean that patients with SIADH cannot become hypovolemic for other reasons, but in such cases it is impossible to diagnose the underlying SIADH until the patient is rendered euvolemic. The fourth criterion, renal salt wasting, has probably caused the most confusion in the diagnosis of SIADH. As noted above, the importance of this criterion lies in its usefulness in differentiating hypoosmolality caused by a decreased effective intravascular volume with high aldosterone levels in which case renal Na+ conservation occurs, from dilutional disorders in which urine Na+ excretion is normal or increased due to ECF volume expansion and a suppressed renin‐angiotensin‐aldosterone system. However, UNa can also be high in renal causes of solute depletion such as diuretic use or Addison's disease, and conversely patients with SIADH can have a low UNa if they subsequently become hypovolemic or solute depleted, conditions sometimes produced by imposed salt and water restriction. Consequently, although high urinary Na+ excretion is generally the rule in most patients with SIADH, its presence does not necessarily confirm this diagnosis, nor does its absence rule out the diagnosis. The final criterion emphasizes that SIADH remains a diagnosis of exclusion, and the absence of other potential causes of hypoosmolality must always be verified. Glucocorticoid deficiency and SIADH can be especially difficult to distinguish, since both primary and secondary hypocortisolism can cause elevated plasma AVP levels in addition to direct renal effects that prevent maximal urinary dilution.19 Therefore, no patient with chronic hyponatremia should be diagnosed as having SIADH without a thorough evaluation of adrenal function, preferably via a rapid adrenocorticotropic hormone (ACTH) stimulation test. Acute hyponatremia of obvious etiology, such as postoperatively or in association with pneumonitis, may be treated without adrenal testing as long as there are no other clinical signs or symptoms suggestive of adrenal dysfunction.20
|
| Essential |
| Decreased effective osmolality of the extracellular fluid (Posm< 275 mOsm/kg H2O). |
| Inappropriate urinary concentration (Uosm >100 mOsm/kg H2O with normal renal function) at some level of hypoosmolality. |
| Clinical euvolemia, as defined by the absence of signs of hypovolemia (orthostasis, tachycardia, decreased skin turgor, dry mucous membranes) or hypervolemia (subcutaneous edema, ascites). |
| Elevated urinary sodium excretion while on a normal salt and water intake. |
| Absence of other potential causes of euvolemic hypoosmolality: hypothyroidism, hypocortisolism (Addison's disease or secondary adrenal insufficiency) and diuretic use. |
| Supplemental |
| Abnormal water load test (inability to excrete at least 90% of a 20 mL/kg water load in 4 hours and/or failure to dilute Uosm to <100 mOsm/kg H2O). |
| Plasma AVP level inappropriately elevated relative to plasma osmolality. |
| No significant correction of serum [Na+] with volume expansion but improvement after fluid restriction. |
Hyponatremia is a particularly common complication in elderly hospitalized patients, increasing in prevalence from approximately 7% in the general older population to 18% to 22% among elderly patients in chronic care facilities.21 Despite the many known causes of SIADH (Figure 1), hyponatremia is often associated with idiopathic SIADH in the elderly population. In a study of 119 nursing home residents aged 60 to 103 years, 53% had at least 1 episode of hyponatremia during the previous 12 months.22 Of these patients, 26% were diagnosed with idiopathic SIADH. In another study of elderly patients with hyponatremia and SIADH, 60% were diagnosed with idiopathic SIADH. Among remaining patients, the 2 main causes identified were pneumonia (9 cases/18%) and medications (6 cases/12%).23 Therefore, more than half of elderly patients who present with hyponatremia due to SIADH may have an idiopathic form, with no detectable underlying treatable disease.
Which Hospital Patients With SIADH are Candidates for Treatment of Hyponatremia?
Correction of hyponatremia is associated with markedly improved neurological outcomes in patients with severely symptomatic hyponatremia. In a retrospective review of patients who presented with severe neurological symptoms and serum [Na+] <125 mmol/L, prompt therapy with isotonic or hypertonic saline resulted in a correction in the range of 20 mmol/L over several days and neurological recovery in almost all cases. In contrast, in patients who were treated with fluid restriction alone, there was very little correction over the study period (<5 mmol/L over 72 hours), and the neurological outcomes were much worse, with most of these patients either dying or entering a persistently vegetative state.24 Consequently, prompt therapy to rapidly increase the serum [Na+] represents the standard‐of‐care for treatment of patients presenting with severe life‐threatening symptoms of hyponatremia.
As discussed earlier, chronic hyponatremia is much less symptomatic as a result of the process of brain volume regulation. Because of this adaptation process, chronic hyponatremia is arguably a condition that clinicians feel they may not need to be as concerned about, and in some publications this has been called asymptomatic hyponatremia. However, such patients often do have neurological symptoms, even if milder and more subtle in nature, including headaches, nausea, mood disturbances, depression, difficulty concentrating, slowed reaction times, unstable gait, increased falls, confusion, and disorientation. Consequently, any patient with hyponatremia secondary to SIADH who manifests any neurological symptoms that could be related to the hyponatremia should be considered as appropriate candidates for treatment of the hyponatremia, regardless of the chronicity of the hyponatremia or the level of serum [Na+].
What Therapies are Currently Available to Manage SIADH in Hospitalized Patients?
Conventional management strategies for euvolemic hyponatremia range from saline infusion and fluid restriction to pharmacologic adjustment of fluid balance. Consideration of treatment options should include an evaluation of the benefits as well as the potential toxicities of any therapy (Table 2). Sometimes, simply stopping treatment with an agent that is associated with hyponatremia is sufficient to reverse a low serum [Na+].
| Therapy | Targets Underlying Pathophysiology | Limitations |
|---|---|---|
| ||
| Isotonic saline | Ineffective in dilutional hyponatremias; exacerbates the volume overload if used in edema‐forming disorders; no controlled safety database. | |
| Hypertonic saline | No consensus regarding appropriate infusion rates; overcorrection can cause osmotic demyelination; exacerbates the volume overload if used in edema‐forming disorders; no controlled safety database. | |
| Fluid restriction | Slow to correct over many days; poorly tolerated due to thirst; can not be used effectively in patients with high AVP levels and urine osmolalities. | |
| Demeclocycline | ✓ | Not FDA approved for hyponatremia; slow to correct; nephrotoxic in cirrhosis and heart failure. |
| Mineralocorticoids | Only one report in elderly patients with SIADH; no safety database; exacerbates the volume overload if used in edema‐forming disorders. | |
| Urea | Not FDA‐approved for hyponatremia; poor palatability. | |
| AVP receptor antagonists (vaptans) | ✓ | Conivaptan approved only for in‐hospital use secondary to CYP3A4 inhibition; infusion‐site reactions with intravenous use. Tolvaptan must be initiated and reinitiated in the hospital, as serum sodium needs to be monitored closely to avoid overly rapid correction of hyponatremia. |
Isotonic Saline
The treatment of choice for depletional hyponatremia (ie, hypovolemic hyponatremia) is isotonic saline ([Na+] = 154 mmol/L) to restore ECF volume and ensure adequate organ perfusion. This initial therapy is appropriate for patients who either have clinical signs of hypovolemia, or in whom a spot UNa+ is <30 mmol/L. However, this therapy is ineffective for dilutional hyponatremias such as SIADH,25 and continued inappropriate administration of isotonic saline to a euvolemic patient may worsen their hyponatremia,26 and/or cause fluid overload. Although isotonic saline may improve the serum [Na+] in patients with hypervolemic hyponatremia, their volume status will generally worsen with this therapy, so unless the hyponatremia is profound isotonic saline should be avoided.
Hypertonic Saline
Acute hyponatremia presenting with severe neurological symptoms is life‐threatening, and should be treated promptly with hypertonic solutions, typically 3% NaCl ([Na+] = 513 mmol/L), as this represents the most reliable method to quickly raise the serum [Na+]. A continuous infusion of hypertonic NaCl is usually utilized in inpatient settings. Various formulae have been suggested for calculating the initial rate of infusion of hypertonic solutions,27 but perhaps the simplest utilizes the following relationship:
An alternative option for more emergent situations is administration of a 100 mL bolus of 3% NaCl, repeated once if no clinical improvement, which has been recommended by a consensus conference organized to develop guidelines for prevention and treatment of exercise‐induced hyponatremia, an acute and potentially lethal condition.28 Injecting this amount of hypertonic saline intravenously raises the serum [Na+] by an average of 2 mmol/L to 4 mmol/L, which is well below the recommended maximal daily rate of change of 10 to 12 mmol/24 hours or 18 mmol/48 hours.29 Because the brain can only accommodate an average increase of approximately 8% in brain volume before herniation occurs, quickly increasing the serum [Na+] by as little as 2 mmol/L to 4 mmol/L in acute hyponatremia can effectively reduce brain swelling and intracranial pressure.30 Unfortunately, until now there has been no consensus regarding appropriate infusion rates of 3% NaCl, and many physicians are hesitant to use it in patients with chronic hyponatremia because it can cause an overly rapid correction of serum sodium levels that can lead to the osmotic demyelination syndrome (ODS).31 Nonetheless, this remains the treatment of choice for patients with severe neurological symptoms, even when the time course of the hyponatremia is nonacute or unknown. The administration of hypertonic saline is generally not recommended for most patients with edema‐forming disorders because it acts as a volume expander and may exacerbate volume overload.
Fluid Restriction
For patients with chronic hyponatremia, fluid restriction has been the most popular and most widely accepted treatment. When SIADH is present, generally fluids should be limited to 500 to 1000 mL/24 hours. Because fluid restriction increases the serum [Na+] largely by under‐replacing the excretion of fluid by the kidneys, some have advocated an initial restriction to 500 mL less than the 24‐hour urine output.32 When instituting a fluid restriction, it is important for the nursing staff and the patient to understand that this includes all fluids that are consumed, not just water. Generally the water content of ingested food is not included in the restriction because this is balanced by insensible water losses (perspiration, exhaled air, feces, etc.), but caution should be exercised with foods that have high fluid concentrations (such as fruits and soups). Restricting fluid intake is effective when properly applied and managed, but serum sodium levels are increased only slowly (1‐2 mmol/L/day) even with severe restriction.25 In addition, this therapy is often poorly tolerated because of an associated increase in thirst. However, it is economically favorable, and some patients do respond well to this option. Fluid restriction should not be used with hypovolemic patients, and is particularly difficult to maintain in patients with very elevated urine osmolalities secondary to high AVP levels; in general, if the sum of urine Na+ and K+ exceeds the serum [Na+], most patients will not respond to a fluid restriction since an electrolyte‐free water clearance will be difficult to achieve,33, 34 and in patients in intensive care settings who often require administration of fluids as part of their therapies.
Demeclocycline
Demeclocycline, a tetracycline antibiotic, inhibits adenylyl cyclase activation after AVP binds to its V2 receptor in the kidney, and thus targets the underlying pathophysiology of SIADH. This therapy is typically used when patients find severe fluid restriction unacceptable and the underlying disorder cannot be corrected. However, demeclocycline is not approved by the U.S. Food and Drug Administration (FDA) to treat hyponatremia, and can cause nephrotoxicity in patients with heart failure and cirrhosis, although this is usually reversible if caught quickly enough.35
Mineralocorticoids
Administration of mineralocorticoids, such as fludrocortisone, has been shown to be useful in a small number of elderly patients.36 However, the initial studies of SIADH did not show it to be of benefit in patients with SIADH, and it carries the risk of fluid overload and hypertension. Consequently, it is rarely used to treat hyponatremia in the U.S.
Urea
Administration of urea has been successfully used to treat hyponatremia because it induces osmotic diuresis and augments free water excretion. Effective doses of urea for treatment of hyponatremia are 30 gm to 60 gm daily in divided doses.37 Unfortunately, its use is limited because there is no United States Pharmacopeia (USP) formulation for urea, and it is not approved by the FDA for treatment of hyponatremia. As such, urea has not been used extensively in the United States, and there are limited data to support its long‐term use. Furthermore, urea is associated with poor palatability; however, patients with feeding tubes may be excellent candidates for urea therapy since palatability is not a concern, and the use of fluid restriction may be difficult in some patients with high obligate intake of fluids as part of their nutritional and medication therapy. Although mild azotemia can be seen with urea therapy, this rarely reaches clinically significant levels.
Clinicians have used all of the above conventional therapies for hyponatremia over the past decades. However, conventional therapies for hyponatremia, although effective in specific circumstances, are suboptimal for many different reasons, including variable efficacy, slow responses, intolerable side effects, and serious toxicities, as summarized in Table 2. But perhaps the most striking deficiency of most conventional therapies is that with the exception of demeclocycline, these therapies do not directly target the underlying cause of most all dilutional hyponatremias, namely inappropriately elevated plasma AVP levels. A new class of pharmacological agents, vasopressin receptor antagonists, that directly block AVP‐mediated receptor activation have recently been approved by the FDA for treatment of euvolemic and hypervolemic hyponatremia.38
AVP Receptor (AVPR) Antagonists
Conivaptan and tolvaptan are antagonists of the AVP V2 (antidiuretic) receptor and have been approved by the FDA for the treatment of euvolemic and hypervolemic hyponatremia. These agents, also known as vaptans, compete with AVP/ADH for binding at its site of action in the kidney, thereby blocking the antidiuresis caused by elevated AVP levels and directly attacking the underlying pathophysiology of dilutional hyponatremia. AVPR antagonists produce electrolyte free water excretion (called aquaresis) without affecting renal sodium and potassium excretion.39 The overall result is a reduction in body water without natriuresis, which leads to an increase in the serum [Na+]. One of the major benefits of this class of drugs is that serum [Na+] is significantly increased within 24 to 48 hours,40, 41 which is considerably faster than the effects of fluid restriction that can take many days. Also, compliance has not been shown to be problem for vaptans, whereas this is a major problem with attempted long‐term use of fluid restriction.
Conivaptan is FDA‐approved for euvolemic and hypervolemic hyponatremia in hospitalized patients. It is available only as an intravenous preparation, and is given as a 20 mg loading dose over 30 minutes, followed by a continuous infusion of 20 or 40 mg.42 Generally, the 20 mg continuous infusion is used for the first 24 hours to gauge the initial response. If the correction of serum [Na+] is felt to be inadequate (eg, <5 mmol/L), then the infusion rate can be increased to 40 mg/day. Therapy is limited to a maximum duration of 4 days because of drug‐interaction effects with other agents metabolized by the cytochrome P450 3A4 (CYP3A4) hepatic isoenzymes. Importantly, for conivaptan and all other vaptans, it is critical that the serum [Na+] concentration is measured frequently during the active phase of correction of the hyponatremia (a minimum of every 6 hours, but more frequently in patients with risk factors for development of osmotic demyelination, such as severely low serum [Na+], malnutrition, alcoholism and hypokalemia).43 If the correction approaches 12 mmol/L in the first 24 hours, the infusion should be stopped and the patient monitored on a fluid restriction. If the correction exceeds 12 mmol/L, consideration should be given to administering sufficient water, either orally or as intravenous D5W to bring the overall correction below 12 mmol/L. The maximum correction limit should be reduced to 8 mmol/L over the first 24 hours in patients with risk factors for development of osmotic demyelination. The most common adverse effects include injection‐site reactions, which are generally mild and usually do not lead to treatment discontinuation, headache, thirst, and hypokalemia.40
Tolvaptan, an oral AVPR antagonist, is FDA‐approved for treatment of dilutional hyponatremias. In contrast to conivaptan, oral administration allows it to be used for both short‐term and long‐term treatment of hyponatremia.41 Similar to conivaptan, tolvaptan treatment must be initiated in the hospital so that the rate of correction can be monitored carefully. Patients with a serum [Na+] <125 mmol/L are eligible for therapy with tolvaptan as primary therapy; if the serum [Na+] is 125 mmol/L, tolvaptan therapy is only indicated if the patient has symptoms that could be attributable to the hyponatremia and the patient is resistant to attempts at fluid restriction.44 The starting dose of tolvaptan is 15 mg on the first day, and the dose can be titrated to 30 mg and 60 mg at 24‐hour intervals if the serum [Na+] remains <135 mmol/L or the increase in serum [Na+] has been 5 mmol/L in the previous 24 hours. As with conivaptan, it is essential that the serum [Na+] concentration is measured frequently during the active phase of correction of the hyponatremia (a minimum of every 8 hrs, but more frequently in patients with risk factors for development of osmotic demyelination). Limits for safe correction of hyponatremia and methods to compensate for overly rapid corrections are the same as described previously for conivaptan. Common side effects include dry mouth, thirst, increased urinary frequency, dizziness, nausea and orthostatic hypotension, which were relatively similar between placebo and tolvaptan groups in clinical trials.41, 44
Because inducing increased renal fluid excretion via either a diuresis or an aquaresis can cause or worsen hypotension in patients with hypovolemic hyponatremia, vaptans are contraindicated in this patient population.43 However, clinically significant hypotension was not observed in either the conivaptan or tolvaptan clinical trials in euvolemic and hypervolemic hyponatremic patients. Although vaptans are not contraindicated with decreased renal function, these agents generally will not be effective if the serum creatinine is >2.5 mg/dL.
Hyponatremia Treatment Guidelines for Hospitalized Patients With SIADH
Although various authors have published recommendations on the treatment of hyponatremia,27, 43, 45‐47 no standardized treatment algorithms have yet been widely accepted. A synthesis of existing expert recommendations for treatment of hyponatremia is illustrated in Figure 2. This algorithm is based primarily on the symptomatology of hyponatremic patients, rather than the serum [Na+] or the chronicity of the hyponatremia, which are often difficult to ascertain. A careful neurological history and assessment should always be done to identify potential causes for the patient's symptoms other than hyponatremia, although it will not always be possible to exclude an additive contribution from the hyponatremia to an underlying neurological condition. In this model, patients are divided into three groups based on their presenting symptoms.
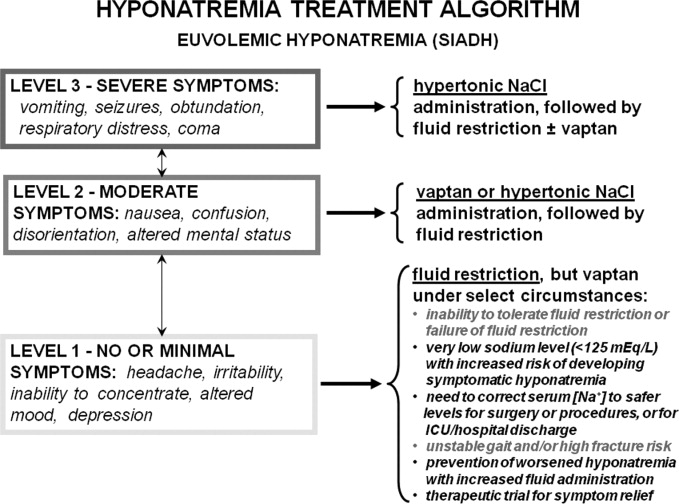
Level 1 symptoms include seizures, coma, respiratory arrest, obtundation, and vomiting, and usually imply a more acute onset or worsening of hyponatremia requiring immediate active treatment. Therapies that will quickly raise serum sodium levels are required to reduce cerebral edema and decrease the risk of potentially fatal herniation.
Level 2 symptoms, which are more moderate, include nausea, confusion, disorientation, and altered mental status. These symptoms may be either chronic or acute, but allow time to elaborate a more deliberate approach to treatment.
Level 3 symptoms range from minimal symptoms such as a headache, irritability, inability to concentrate, altered mood, and depression, to a virtual absence of discernable symptoms, and indicate that the patient may have chronic or slowly evolving hyponatremia. These symptoms necessitate a cautious approach, especially when patients have underlying comorbidities.
Patients with severe symptoms (Level 1) should be treated with hypertonic saline as first‐line therapy, followed by fluid restriction with or without AVPR antagonist therapy. Patients with moderate symptoms will benefit from a more aggressive regimen of vaptan therapy or limited hypertonic saline administration, followed by fluid restriction or long‐term vaptan therapy. Although moderate neurological symptoms can indicate that a patient is in an early stage of acute hyponatremia, they more often indicate a chronically hyponatremic state with sufficient brain volume adaptation to prevent marked symptomatology from cerebral edema. Regardless, close monitoring of these patients in a hospital setting is warranted until the symptoms improve or stabilize. Patients with no or minimal symptoms should be managed initially with fluid restriction, although treatment with vaptans may be appropriate for a wide range of specific clinical conditions, foremost of which is a failure to improve the serum [Na+] despite reasonable attempts at fluid restriction (Figure 2).
Although this classification is based on presenting symptoms at the time of initial evaluation, it should be remembered that in some cases patients initially exhibit more moderate symptoms because they are in the early stages of hyponatremia. In addition, some patients with minimal symptoms are prone to develop more symptomatic hyponatremia during periods of increased fluid ingestion. In support of this, approximately 70% of 31 patients presenting to a university hospital with symptomatic hyponatremia and a mean serum [Na+] of 119 mmol/L had preexisting asymptomatic hyponatremia as the most common risk factor identified.48 Consequently, therapy of hyponatremia should also be considered to prevent progression from lower to higher levels of symptomatic hyponatremia, particularly in patients with a past history of repeated presentations of symptomatic hyponatremia.
How Often Should Serum [Na+] Be Monitored in Hospitalized Patients With SIADH?
The frequency of serum [Na+] monitoring is dependent on both the severity of the hyponatremia and the therapy chosen. In all hyponatremic patients neurological symptomatology should be carefully assessed very early in the diagnostic evaluation to assess the symptomatic severity of the hyponatremia and to determine whether the patient requires more urgent therapy. All patients undergoing active treatment with hypertonic saline for level 1 or 2 symptomatic hyponatremia should have frequent monitoring of serum [Na+] and ECF volume status (every 2‐4 hours) to ensure that the serum [Na+] does not exceeded the recommended levels during the active phase of correction,43 since overly rapid correction of serum sodium can cause damage to the myelin sheath of nerve cells, resulting in central pontine myelinolysis, also called the ODS.31 Patients treated with vaptans for level 2 or 3 symptoms should have serum [Na+] monitored every 6 to 8 hours during the active phase of correction, which will generally be the first 24 to 48 hours of therapy. Active treatment with hypertonic saline or vaptans should be stopped when the patient's symptoms are no longer present, a safe serum [Na+] (usually >120 mmol/L) has been achieved, or the rate of correction has reached 12 mmol/L within 24 hours or 18 mmol/L within 48 hours.29, 43 Importantly, ODS has not been reported either in clinical trials or with therapeutic use of any vaptan to date. In patients with a stable level of serum [Na+] treated with fluid restriction or therapies other than hypertonic saline, measurement of serum [Na+] daily is generally sufficient, since levels will not change that quickly in the absence of active therapy or large changes in fluid intake or administration.
Potential Future Indications for Treatment of Hyponatremia
Correction of hyponatremia improves other symptoms, such as gait stability, in patients who may be considered to be asymptomatic by virtue of a normal neurological exam. In 1 study, 16 patients with hyponatremia secondary to SIADH in the range of 124 mmol/L to 130 mmol/L demonstrated a significant gait instability that normalized after correction of the hyponatremia to normal ranges.49 The functional significance of the gait instability was illustrated in a study of 122 Belgian patients with a variety of levels of hyponatremia, all judged to be asymptomatic at the time of visit to an emergency department (ED). These patients were compared with 244 age‐matched, sex‐matched, and disease‐matched controls also presenting to the ED during the same time period. Researchers found that 21% of the hyponatremic patients presented to the ED because of a recent fall, compared to only 5% of the controls, resulting in an adjusted odds ratio (OR) for presenting to the ED because of a recent fall of 67 for hyponatremia (P < 0.001).49 Consequently, this study clearly documented an increased incidence of falls in so‐called asymptomatic hyponatremic patients.
The clinical significance of the gait instability and fall data were further evaluated in a study that compared 553 patients with fractures to an equal number of age‐matched and sex‐matched controls. Hyponatremia was found in 13% of the patients presenting with fractures compared to only 4% of the controls.50 Similar findings have been reported in a 364 elderly patients with large‐bone fractures in New York.51 More recently published studies have shown that hyponatremia is associated with increased bone loss in experimental animals and a significant increased OR for osteoporosis of the femoral neck (OR, 2.87; P < 0.003) in humans over the age of 50 in the NHANES III database.52 Thus, the major clinical significance of chronic hyponatremia may be the increased morbidity and mortality associated with falls and fractures in our elderly population.
Summary
Disorders of sodium and water metabolism are commonly encountered in the hospital setting due to the wide range of disease states that can disrupt the balanced control of water and solute intake and output. In particular, the prompt identification and appropriate management of abnormally low serum [Na+] is critical if we are to reduce the increased morbidity and mortality that accompany hyponatremia in hospitalized patients. Use of an algorithm that is based primarily on the symptomatology of hyponatremic patients, rather than the chronicity of the hyponatremia or the serum [Na+], will help to choose the correct initial therapy in hospitalized hyponatremic patients. However, careful monitoring of serum [Na+] responses is required in all cases to adjust therapy appropriately in response to changing clinical conditions. Although this approach will enable efficacious and safe treatment of hyponatremic patients with SIADH at the present time, evolving knowledge of the consequences of chronic hyponatremia will likely alter treatment indications and guidelines in the future.
- .Age and gender as risk factors for hyponatremia and hypernatremia.Clin Chim Acta.2003;337(1‐2):169–172.
- ,,.Incidence and prevalence of hyponatremia.Am J Med.2006;119(7 Suppl 1):S30–S35.
- ,,.Admission hyponatremia in the elderly: factors influencing prognosis.J Gen Intern Med1994;9:89–91.
- ,,, et al.[Incidence, causes and prognostic factors of hyponatremia in intensive care].Rev Med Interne.2003;24(4):224–229.
- ,,,.Postoperative hyponatremia. A prospective study.Arch Int Med.1986;146:333–336.
- .Whole‐body volume regulation and escape from antidiuresis.Am J Med.2006;119(7 Suppl 1):S21–S29.
- ,,.Neurogenic disorders of osmoregulation.Am J Med.1982;72:339–353.
- ,,.Vasopressin function in the syndrome of inappropriate antidiuresis.Annu Rev Med.1980;31:315–327.
- ,,,,,.Radioimmunoassay of plasma arginine vasopressin in hyponatremic patients with congestive heart failure.N Eng J Med.1981;305:263–266.
- ,.Epidemiology, pathophysiology, and management of hyponatremic encephalopathy.Am J Med.1997;102:67–77.
- ,.Pulmonary complications of hyponatremic encephalopathy. noncardiogenic pulmonary edema and hypercapnic respiratory failure [see comments].Chest.1995;107(2):517–521.
- ,.Control of brain volume during hyperosmolar and hypoosmolar conditions.Annu Rev Med.1993;44:289–301.
- .Control of brain volume during hypoosmolality and hyperosmolality.Adv Exp Med Biol.2006;576:113–129.
- ,,.Clinical studies of thiazide‐induced hyponatremia.J Natl Med Assoc.2004;96(10):1305–1308.
- ,,,.Clinical assessment of extracellular fluid volume in hyponatremia.Am J Med.1987;83:905–908.
- ,.The syndrome of inappropriate secretion of antidiuretic hormone.Am J Med.1967;42:790–806.
- .Hyponatremia and Hypo‐osmolar Disorders. In: Greenberg A, Cheung AK, Coffman TM, Falk RJ, Jennette JC, eds.Primer on Kidney Diseases.Philadelphia:Saunders Elsevier,2009:52–59.
- ,,,.Reset of osmoreceptors in association with normovolemic hyponatremia.Am J Med Sci.1974;267:267–273.
- .Hyponatremia and inappropriate secretion of vasopressin (antidiuretic hormone) in patients with hypopituitarism.N Eng J Med.1989;321:492–496.
- .The Syndrome of Inappropriate Antidiuretic Hormone Secretion and Other Hypoosmolar Disorders. In: Schrier RW, ed.Diseases of the Kidney and Urinary Tract.Philadelphia:Lippincott Williams 27:156–161.
- ,,.Hyponatremia in a nursing home population.J Am Geriatr Soc.1995;43(12):1410–1413.
- ,.The syndrome of inappropriate antidiuretic hormone secretion in the elderly.Am J Med.1997;103(4):270–273.
- .Diuretic‐induced hyponatremia [editorial].Arch Intern Med.1986;146(7):1295–1296.
- ,,,.A syndrome of renal sodium loss and hyponatremia probably resulting from inappropriate secretion of antidiuretic hormone.Am J Med.1957;23:529–542.
- ,,,,,.Postoperative hyponatremia despite near‐isotonic saline infusion: a phenomenon of desalination [see comments].Ann Intern Med.1997;126(1):20–25.
- ,.Hyponatremia.N Engl J Med.2000;342(21):1581–1589.
- ,,, et al.Statement of the Second International Exercise‐Associated Hyponatremia Consensus Development Conference, New Zealand, 2007.Clin J Sport Med.2008;18(2):111–121.
- ,,,.Neurologic sequelae after treatment of severe hyponatremia: a multicenter perspective.J Am Soc Nephrol.1994;4:1522–1530.
- ,,,.Randomized, controlled trial on the effect of a 20% mannitol solution and a 7.5% saline/6% dextran solution on increased intracranial pressure after brain injury.Crit Care Med.2005;33(1):196–202.
- ,,.Osmotic demyelination syndrome following correction of hyponatremia.N Engl J Med.1986;314:1535–1542.
- .Regulation of arginine vasopressin in the syndrome of inappropriate antidiuresis.Am J Med.2006;119(7 Suppl 1):S36–S42.
- .The syndrome of inappropriate secretion of antidiuretic hormone (SIADH).Semin Nephrol.2009;29(3):239–256.
- .Impact of solute intake on urine flow and water excretion.J Am Soc Nephrol.2008;19(6):1076–1078.
- ,.Demeclocycline‐induced nephrogenic diabetes insipidus. In‐vivo and in‐ vitro studies.Ann Intern Med.1973;79(5):679–683.
- ,,, et al.Involvement of arginine vasopressin and renal sodium handling in pathogenesis of hyponatremia in elderly patients.Endocr J.1996;43(1):101–108.
- ,.Urea for long‐term treatment of syndrome of inappropriate secretion of antidiuretic hormone.Br Med J (Clin Res Ed).1981;283:1081–1083.
- ,.Vasopressin receptor antagonists.Kidney Int.2006;69(12):2124–2130.
- ,,, et al.Potent aquaretic agent. A novel nonpeptide selective vasopressin 2 antagonist (OPC‐31260) in men.J Clin Invest.1993;92(6):2653–2659.
- ,,,,.Assessment of the efficacy and safety of intravenous conivaptan in euvolemic and hypervolemic hyponatremia.Am J Nephrol.2007;27(5):447–457.
- ,,, et al.Tolvaptan, a selective oral vasopressin V2‐receptor antagonist, for hyponatremia.N Engl J Med.2006;355(20):2099–2112.
- Vaprisol (conivaptan hydrochloride injection) prescribing information.Deerfield, IL:Astellas Pharma US, Inc.,2006.
- ,,,,.Hyponatremia treatment guidelines 2007: expert panel recommendations.Am J Med.2007;120(11 Suppl 1):S1–S21.
- Otsuka Pharmaceutical Co L, Tokyo J. Samsca (tolvaptan) prescribing information.2009.
- ,.Clinical practice. The syndrome of inappropriate antidiuresis.N Engl J Med.2007;356(20):2064–2072.
- ,,.The treatment of hyponatremia.Semin Nephrol.2009;29(3):282–299.
- .Hyponatremia and Hypo‐osmolar Disorders. In: Greenberg A, Cheung AK, Coffman TM, Falk RJ, Jennette JC, eds.Primer on Kidney Diseases.Philadelphia. PA:Saunders Elsevier;2009:52–59.
- ,,,.Risk factors for symptomatic hyponatraemia: the role of pre‐existing asymptomatic hyponatraemia.Intern Med J.2007;37(3):149–155.
- ,,,,.Mild chronic hyponatremia is associated with falls, unsteadiness, and attention deficits.Am J Med.2006;119(1):71.
- ,,,,.Mild hyponatremia and risk of fracture in the ambulatory elderly.QJM.2008;101(7):583–588.
- ,,,,.Hyponatremia associated with large‐bone fracture in elderly patients.Int Urol Nephrol.2009;41(3):733–737.
- ,,, et al.Hyponatremia‐induced osteoporosis.J Bone Miner Res.2010;25(3):554–563.
- .Age and gender as risk factors for hyponatremia and hypernatremia.Clin Chim Acta.2003;337(1‐2):169–172.
- ,,.Incidence and prevalence of hyponatremia.Am J Med.2006;119(7 Suppl 1):S30–S35.
- ,,.Admission hyponatremia in the elderly: factors influencing prognosis.J Gen Intern Med1994;9:89–91.
- ,,, et al.[Incidence, causes and prognostic factors of hyponatremia in intensive care].Rev Med Interne.2003;24(4):224–229.
- ,,,.Postoperative hyponatremia. A prospective study.Arch Int Med.1986;146:333–336.
- .Whole‐body volume regulation and escape from antidiuresis.Am J Med.2006;119(7 Suppl 1):S21–S29.
- ,,.Neurogenic disorders of osmoregulation.Am J Med.1982;72:339–353.
- ,,.Vasopressin function in the syndrome of inappropriate antidiuresis.Annu Rev Med.1980;31:315–327.
- ,,,,,.Radioimmunoassay of plasma arginine vasopressin in hyponatremic patients with congestive heart failure.N Eng J Med.1981;305:263–266.
- ,.Epidemiology, pathophysiology, and management of hyponatremic encephalopathy.Am J Med.1997;102:67–77.
- ,.Pulmonary complications of hyponatremic encephalopathy. noncardiogenic pulmonary edema and hypercapnic respiratory failure [see comments].Chest.1995;107(2):517–521.
- ,.Control of brain volume during hyperosmolar and hypoosmolar conditions.Annu Rev Med.1993;44:289–301.
- .Control of brain volume during hypoosmolality and hyperosmolality.Adv Exp Med Biol.2006;576:113–129.
- ,,.Clinical studies of thiazide‐induced hyponatremia.J Natl Med Assoc.2004;96(10):1305–1308.
- ,,,.Clinical assessment of extracellular fluid volume in hyponatremia.Am J Med.1987;83:905–908.
- ,.The syndrome of inappropriate secretion of antidiuretic hormone.Am J Med.1967;42:790–806.
- .Hyponatremia and Hypo‐osmolar Disorders. In: Greenberg A, Cheung AK, Coffman TM, Falk RJ, Jennette JC, eds.Primer on Kidney Diseases.Philadelphia:Saunders Elsevier,2009:52–59.
- ,,,.Reset of osmoreceptors in association with normovolemic hyponatremia.Am J Med Sci.1974;267:267–273.
- .Hyponatremia and inappropriate secretion of vasopressin (antidiuretic hormone) in patients with hypopituitarism.N Eng J Med.1989;321:492–496.
- .The Syndrome of Inappropriate Antidiuretic Hormone Secretion and Other Hypoosmolar Disorders. In: Schrier RW, ed.Diseases of the Kidney and Urinary Tract.Philadelphia:Lippincott Williams 27:156–161.
- ,,.Hyponatremia in a nursing home population.J Am Geriatr Soc.1995;43(12):1410–1413.
- ,.The syndrome of inappropriate antidiuretic hormone secretion in the elderly.Am J Med.1997;103(4):270–273.
- .Diuretic‐induced hyponatremia [editorial].Arch Intern Med.1986;146(7):1295–1296.
- ,,,.A syndrome of renal sodium loss and hyponatremia probably resulting from inappropriate secretion of antidiuretic hormone.Am J Med.1957;23:529–542.
- ,,,,,.Postoperative hyponatremia despite near‐isotonic saline infusion: a phenomenon of desalination [see comments].Ann Intern Med.1997;126(1):20–25.
- ,.Hyponatremia.N Engl J Med.2000;342(21):1581–1589.
- ,,, et al.Statement of the Second International Exercise‐Associated Hyponatremia Consensus Development Conference, New Zealand, 2007.Clin J Sport Med.2008;18(2):111–121.
- ,,,.Neurologic sequelae after treatment of severe hyponatremia: a multicenter perspective.J Am Soc Nephrol.1994;4:1522–1530.
- ,,,.Randomized, controlled trial on the effect of a 20% mannitol solution and a 7.5% saline/6% dextran solution on increased intracranial pressure after brain injury.Crit Care Med.2005;33(1):196–202.
- ,,.Osmotic demyelination syndrome following correction of hyponatremia.N Engl J Med.1986;314:1535–1542.
- .Regulation of arginine vasopressin in the syndrome of inappropriate antidiuresis.Am J Med.2006;119(7 Suppl 1):S36–S42.
- .The syndrome of inappropriate secretion of antidiuretic hormone (SIADH).Semin Nephrol.2009;29(3):239–256.
- .Impact of solute intake on urine flow and water excretion.J Am Soc Nephrol.2008;19(6):1076–1078.
- ,.Demeclocycline‐induced nephrogenic diabetes insipidus. In‐vivo and in‐ vitro studies.Ann Intern Med.1973;79(5):679–683.
- ,,, et al.Involvement of arginine vasopressin and renal sodium handling in pathogenesis of hyponatremia in elderly patients.Endocr J.1996;43(1):101–108.
- ,.Urea for long‐term treatment of syndrome of inappropriate secretion of antidiuretic hormone.Br Med J (Clin Res Ed).1981;283:1081–1083.
- ,.Vasopressin receptor antagonists.Kidney Int.2006;69(12):2124–2130.
- ,,, et al.Potent aquaretic agent. A novel nonpeptide selective vasopressin 2 antagonist (OPC‐31260) in men.J Clin Invest.1993;92(6):2653–2659.
- ,,,,.Assessment of the efficacy and safety of intravenous conivaptan in euvolemic and hypervolemic hyponatremia.Am J Nephrol.2007;27(5):447–457.
- ,,, et al.Tolvaptan, a selective oral vasopressin V2‐receptor antagonist, for hyponatremia.N Engl J Med.2006;355(20):2099–2112.
- Vaprisol (conivaptan hydrochloride injection) prescribing information.Deerfield, IL:Astellas Pharma US, Inc.,2006.
- ,,,,.Hyponatremia treatment guidelines 2007: expert panel recommendations.Am J Med.2007;120(11 Suppl 1):S1–S21.
- Otsuka Pharmaceutical Co L, Tokyo J. Samsca (tolvaptan) prescribing information.2009.
- ,.Clinical practice. The syndrome of inappropriate antidiuresis.N Engl J Med.2007;356(20):2064–2072.
- ,,.The treatment of hyponatremia.Semin Nephrol.2009;29(3):282–299.
- .Hyponatremia and Hypo‐osmolar Disorders. In: Greenberg A, Cheung AK, Coffman TM, Falk RJ, Jennette JC, eds.Primer on Kidney Diseases.Philadelphia. PA:Saunders Elsevier;2009:52–59.
- ,,,.Risk factors for symptomatic hyponatraemia: the role of pre‐existing asymptomatic hyponatraemia.Intern Med J.2007;37(3):149–155.
- ,,,,.Mild chronic hyponatremia is associated with falls, unsteadiness, and attention deficits.Am J Med.2006;119(1):71.
- ,,,,.Mild hyponatremia and risk of fracture in the ambulatory elderly.QJM.2008;101(7):583–588.
- ,,,,.Hyponatremia associated with large‐bone fracture in elderly patients.Int Urol Nephrol.2009;41(3):733–737.
- ,,, et al.Hyponatremia‐induced osteoporosis.J Bone Miner Res.2010;25(3):554–563.