User login
The headlines are harrowing: corporate layoffs; foreclosures on the rise; 401(k) retirement plans halved; government bailouts adding to the national debt. The worst economic downturn since the Great Depression has generated some unexpected outcomes, yet not all of them are bad for hospitalists. Below, four vignettes highlight HM groups that have achieved success despite—or in some cases because of—these troubled times.
A Better Business Agreement
It has taken nearly two years—and sometimes as many as four meetings a week—but Rajeev Alexander, MD, and his colleagues are nearing the finish line of an evolving business arrangement. The new arrangement has come about due to the economic downturn, which forced Oregon Medical Group (OMG), a multispecialty physician group serving hospitals in the Eugene/Springfield area and the HM group’s employer since 1988, to want to divest themselves of the hospitalist group. Now, after a lengthy negotiation, Dr. Alexander’s group of eight hospitalists is busier than ever.
Through what were essentially multiple quasi-buyouts, divestitures, and mergers, Dr. Alexander’s hospitalist group “spun off” from OMG and affiliated with PeaceHealth, a nonprofit health system serving seven hospitals in Oregon, Washington, and Alaska. The new contract means Dr. Alexander’s group is directly employed by Sacred Heart Hospital, a 541-bed PeaceHealth-owned facility in Eugene.
The new contract included a non-compete clause with OMG, which currently employs five hospitalists, yet Dr. Alexander’s group has maintained its patient volume. Compensation held steady and employee benefits improved. During an independent and slow-moving negotiation, Dr. Alexander’s group has merged with another HM service that originally was employed by PeaceHealth. The two HM groups (technically competitors) now practice in the same hospital and are ironing out the terms of the merger. At the moment, the groups have created a mutually respectful joint governance council.
“We’ve tackled the thorniest of problems,” Dr. Alexander says, “first, creating a combined work schedule to distribute patients and divide the work. Those of us on the governance council figured if we could get the docs to actually work together and share patients and communicate with each other as if they were one group, then the momentum for an actual administrative/contractual merger would feel inevitable.”
Although negotiations are expected to last through the end of the year to finalize such details as compensation, recruiting, and a group mission statement, the medical staff at Sacred Heart considers the merger a “done deal” and has thrown its support behind the effort. “Community outpatient docs have been clamoring for our services, and we have been having to hand out numbers and ask them to wait in line, so to speak,” Dr. Alexander says.
Dr. Alexander says he’s learned some lessons through the extensive negotiation process:
- Stay positive. In any business venture, absolutely nothing is impossible, even dodging a noncompete clause.
- Release your preconceptions. Conspiracy theories might abound, but most hospital administrators have the best of intentions. As highly regulated organizations, hospitals might simply be following their own bylaws and fulfilling responsibilities to stakeholders. Seek out at least one administrator whom you can trust, and with whom you can communicate effectively. A mutual understanding of intentions and objectives makes the process more successful for all concerned.
- Look beyond politics. Your trust and respect for administrators and fellow physicians will go a long way toward overcoming obstacles.
- Stick to your plan. Adhere to your goal of remaining independent, if that is important to you. “Our group resisted being funneled into becoming employed by a very large national hospitalist chain,” Dr. Alexander says, “and I would encourage physicians in other parts of the country to stick to their commitments as well.”
- Trust the negotiation process. Even if all goes well, what you’re shooting for at the beginning might not be exactly what you get after negotiations are over. This does not mean you’ve failed, or that hospital administration tricked you or failed to deliver on promises. It simply means you have created a negotiated settlement; both sides have come to a new appreciation for the other’s requirements and have made necessary and respectful accommodations.
Rural Rewards
Based in Traverse City, Hospitalists of Northwest Michigan (HNM) services four community hospitals and continues to witness solid growth. Since 2000, the group has grown from nine to nearly 40 providers, and from 2005 to 2008, patient encounters doubled. “In these hard economic times, hospitals are inviting us in because we provide value to the hospitals through leadership, increased hospital revenues, and improved recruiting and retention of specialists,” says Troy W. Ahlstrom, MD, president of HNM. “We continue to see healthy growth in patient volume as we align patient care goals with the needs of the hospitals and surrounding communities we serve.”
HNM, which established a service at the regional medical center and then assumed management of HM programs at three other rural hospitals, soon will add a fifth service to its ledger. HNM also began a pediatric program at the regional referral center, and the group is exploring the possibility of providing a network of pediatric care throughout the region.
Having grown up in the region, David Friar, MD, CEO of HNM, not only has a better understanding of the needs of rural hospitals, but also a personal investment in his group’s success. “These are our communities. We don’t view the hospitals as just a place to make a profit, but a place where our neighbors work and our families get their care,” he says.
Drs. Ahlstrom and Friar offer the following advice for achieving success in these economic times:
- Optimize receipts. Concern over compliance audits leads many hospitals to sacrifice group receipts by encouraging undercoding. “We’ve found hospitals do a poor job of negotiating the provider portion of third-party payer contracts and frequently lose provider charges because they focus on the much larger facility fees,” says Dr. Ahlstrom. The group’s receipts increased more than 30% when they began using an outside billing firm and adopted productivity incentives to encourage providers to practice better documentation and charge capture. Improving documentation also supports a hospital’s ability to accurately code its patients, which allows a hospital to bill for a more profitable diagnosis-related group (DRG), and improve its case-mix index. With these changes, Hospitalists of Northwest Michigan has increased provider pay and grown their practice while improving the hospitals’ profitability.
- Encourage frugality. The cost-plus model is popular, but it doesn’t incentivize programs to contain costs. In contrast, the fixed-price model encourages hospitalists to find cheaper ways to provide good care. “Because the money we save goes to us, we’ve all found creative ways to provide quality care for a third less money than similar cost-plus programs,” Dr. Ahlstrom says.
- Align incentives. Hospitals live or die on thin margins, Dr. Ahlstrom says. His group trains its employees to ask: What can I do to make the hospital stronger? “What’s good for the hospital is good for us, so we work with the hospitals, not for the hospitals,” Dr. Friar says.
At its smaller hospitals, HNM incentivized orthopedic admissions so that more surgical cases would stay local. Hospitalists were trained to perform stress tests so the hospital can provide testing on weekends. The group pays hospitalists a bonus for each admission, so when the ED calls, the hospitalists say, “Thanks! I’ll be right there.” The group also increased staffing on weekends.
The end result: It improves the hospital’s bottom line by shortening length of stay, and improving quality of care, patient satisfaction, and group morale.
“When we align the incentives, everybody wins,” says Dr. Friar. “The system has more capacity, the patients get better care, and the hospitalists no longer feel that weekend shifts are a huge burden.”
- Build “system-ness.” Sharing providers between hospitals has helped HNM build a cohesive system of quality care. What began as a way to cover shifts has created an interinstitutional camaraderie that allows for the easier flow of patients, improved communication, and widespread use of best-practice models. Sharing such resources as billing, credentialing, benefits, recruiting, and payroll has helped the group stay competitive, Dr. Ahlstrom says.
Growth in a Down Economy
Jude R. Alexander, MD, president of Inpatient Specialists in Rockville, Md., a bedroom community about 12 miles northwest of Washington, D.C., has continued to grow his group despite the down economy. Hospital admissions in the D.C. area decreased sharply in the second half of 2008, and patient volume rebounded slowly in the first half of 2009.
Inpatient Specialists initially downsized its staff, then it used flex physicians to meet demand as volume increased.
Despite national hospital trends of budget shortfalls, downgraded bond ratings, and increases in uninsured patients, two of Inpatient Specialists’ client hospitals chose to invest in the HM program. Dr. Alexander credits the vote of confidence to his group’s track record of optimal resource utilization, which has inherent cost savings in the millions.
Dr. Alexander also recommends HM groups in tough economic circumstances should:
- Maintain good relationships with partner hospitals;
- Run a lean business;
- Focus on excellent customer service to patients, their families, and their PCPs; and
- Build strong alliances with employed physicians by eliciting and giving constructive feedback.
“Following this basic strategy, Inpatient Specialists has experienced 7% growth in patient volume in the past 12 months,” Dr. Alexander says. “We’ve expanded to 40 full-time equivalent hospitalists, and 40 part-time employees.” Inpatient Specialists has its eye on geographic expansion, as well. The group is targeting services throughout the Capitol region—Maryland, Virginia, and the District of Columbia.
Bankruptcy to Profitability in One Year
In 2007, a few months after the 99-bed Auburn Memorial Hospital in Auburn, N.Y., was forced into bankruptcy, James Leyhane, MD, and his hospitalist group were displeased that they weren’t in control of their own program. Physicians had started leaving the hospital; Dr. Leyhane himself had interviewed at another hospital. “Our CEO approached me to ask what would make it right,” Dr. Leyhane recalls. “I said, ‘We’d need to be employed by the hospital.’ ”
The hospital and the private, six-physician internal-medicine group that employed the program entered bids on the HM group. In March 2008, the HM group became contractually employed by the hospital. Dr. Leyhane was given full control as hospitalist director of Auburn Memorial Hospitalists.
As a result of the new alignment, two major shifts took place. First, the hospital CEO more aggressively recruited subspecialists and surgeons. With the HM group now affiliated with the hospital, recruiting surgeons to Auburn Memorial became much easier. Second, more primary-care physicians (PCPs) began sending their patients to Auburn Memorial.
“We were all shocked at how quickly the administration was able to recruit new subspecialists to the area,” Dr. Leyhane says. “That helped get the profitable procedures back to the hospital.”
The biggest surprise came at the end of 2008. Patient volume had risen 11.5% higher than the hospital’s best-case predictions. “As a result of our emerging from under the umbrella of one physician group, the outlying physicians became less fearful that they might lose their patients to that group,” Dr. Leyhane says. “And in good faith, we still maintain a coverage arrangement with that IM group.”
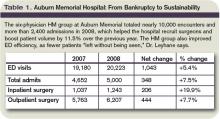
Thus, what was first seen as a bad thing turned into a very good thing for both the hospitalist group and the hospital. Auburn Memorial posted a $3.1 million profit in 2008 (see Table 1).
Dr. Leyhane suggests HM group leaders facing similar financial crunches talk to area subspecialists and find out what it would take to get them affiliated with their institution.
“In our case, a stable hospitalist program was definitely one of their top requests,” Dr. Leyhane says, adding it also would be beneficial to include PCPs in the “what do you want from our hospital?” conversation. TH
Andrea M. Sattinger is a freelance writer based in North Carolina.
Image Source: COLIN ANDERSON/GETTYIMAGES
The headlines are harrowing: corporate layoffs; foreclosures on the rise; 401(k) retirement plans halved; government bailouts adding to the national debt. The worst economic downturn since the Great Depression has generated some unexpected outcomes, yet not all of them are bad for hospitalists. Below, four vignettes highlight HM groups that have achieved success despite—or in some cases because of—these troubled times.
A Better Business Agreement
It has taken nearly two years—and sometimes as many as four meetings a week—but Rajeev Alexander, MD, and his colleagues are nearing the finish line of an evolving business arrangement. The new arrangement has come about due to the economic downturn, which forced Oregon Medical Group (OMG), a multispecialty physician group serving hospitals in the Eugene/Springfield area and the HM group’s employer since 1988, to want to divest themselves of the hospitalist group. Now, after a lengthy negotiation, Dr. Alexander’s group of eight hospitalists is busier than ever.
Through what were essentially multiple quasi-buyouts, divestitures, and mergers, Dr. Alexander’s hospitalist group “spun off” from OMG and affiliated with PeaceHealth, a nonprofit health system serving seven hospitals in Oregon, Washington, and Alaska. The new contract means Dr. Alexander’s group is directly employed by Sacred Heart Hospital, a 541-bed PeaceHealth-owned facility in Eugene.
The new contract included a non-compete clause with OMG, which currently employs five hospitalists, yet Dr. Alexander’s group has maintained its patient volume. Compensation held steady and employee benefits improved. During an independent and slow-moving negotiation, Dr. Alexander’s group has merged with another HM service that originally was employed by PeaceHealth. The two HM groups (technically competitors) now practice in the same hospital and are ironing out the terms of the merger. At the moment, the groups have created a mutually respectful joint governance council.
“We’ve tackled the thorniest of problems,” Dr. Alexander says, “first, creating a combined work schedule to distribute patients and divide the work. Those of us on the governance council figured if we could get the docs to actually work together and share patients and communicate with each other as if they were one group, then the momentum for an actual administrative/contractual merger would feel inevitable.”
Although negotiations are expected to last through the end of the year to finalize such details as compensation, recruiting, and a group mission statement, the medical staff at Sacred Heart considers the merger a “done deal” and has thrown its support behind the effort. “Community outpatient docs have been clamoring for our services, and we have been having to hand out numbers and ask them to wait in line, so to speak,” Dr. Alexander says.
Dr. Alexander says he’s learned some lessons through the extensive negotiation process:
- Stay positive. In any business venture, absolutely nothing is impossible, even dodging a noncompete clause.
- Release your preconceptions. Conspiracy theories might abound, but most hospital administrators have the best of intentions. As highly regulated organizations, hospitals might simply be following their own bylaws and fulfilling responsibilities to stakeholders. Seek out at least one administrator whom you can trust, and with whom you can communicate effectively. A mutual understanding of intentions and objectives makes the process more successful for all concerned.
- Look beyond politics. Your trust and respect for administrators and fellow physicians will go a long way toward overcoming obstacles.
- Stick to your plan. Adhere to your goal of remaining independent, if that is important to you. “Our group resisted being funneled into becoming employed by a very large national hospitalist chain,” Dr. Alexander says, “and I would encourage physicians in other parts of the country to stick to their commitments as well.”
- Trust the negotiation process. Even if all goes well, what you’re shooting for at the beginning might not be exactly what you get after negotiations are over. This does not mean you’ve failed, or that hospital administration tricked you or failed to deliver on promises. It simply means you have created a negotiated settlement; both sides have come to a new appreciation for the other’s requirements and have made necessary and respectful accommodations.
Rural Rewards
Based in Traverse City, Hospitalists of Northwest Michigan (HNM) services four community hospitals and continues to witness solid growth. Since 2000, the group has grown from nine to nearly 40 providers, and from 2005 to 2008, patient encounters doubled. “In these hard economic times, hospitals are inviting us in because we provide value to the hospitals through leadership, increased hospital revenues, and improved recruiting and retention of specialists,” says Troy W. Ahlstrom, MD, president of HNM. “We continue to see healthy growth in patient volume as we align patient care goals with the needs of the hospitals and surrounding communities we serve.”
HNM, which established a service at the regional medical center and then assumed management of HM programs at three other rural hospitals, soon will add a fifth service to its ledger. HNM also began a pediatric program at the regional referral center, and the group is exploring the possibility of providing a network of pediatric care throughout the region.
Having grown up in the region, David Friar, MD, CEO of HNM, not only has a better understanding of the needs of rural hospitals, but also a personal investment in his group’s success. “These are our communities. We don’t view the hospitals as just a place to make a profit, but a place where our neighbors work and our families get their care,” he says.
Drs. Ahlstrom and Friar offer the following advice for achieving success in these economic times:
- Optimize receipts. Concern over compliance audits leads many hospitals to sacrifice group receipts by encouraging undercoding. “We’ve found hospitals do a poor job of negotiating the provider portion of third-party payer contracts and frequently lose provider charges because they focus on the much larger facility fees,” says Dr. Ahlstrom. The group’s receipts increased more than 30% when they began using an outside billing firm and adopted productivity incentives to encourage providers to practice better documentation and charge capture. Improving documentation also supports a hospital’s ability to accurately code its patients, which allows a hospital to bill for a more profitable diagnosis-related group (DRG), and improve its case-mix index. With these changes, Hospitalists of Northwest Michigan has increased provider pay and grown their practice while improving the hospitals’ profitability.
- Encourage frugality. The cost-plus model is popular, but it doesn’t incentivize programs to contain costs. In contrast, the fixed-price model encourages hospitalists to find cheaper ways to provide good care. “Because the money we save goes to us, we’ve all found creative ways to provide quality care for a third less money than similar cost-plus programs,” Dr. Ahlstrom says.
- Align incentives. Hospitals live or die on thin margins, Dr. Ahlstrom says. His group trains its employees to ask: What can I do to make the hospital stronger? “What’s good for the hospital is good for us, so we work with the hospitals, not for the hospitals,” Dr. Friar says.
At its smaller hospitals, HNM incentivized orthopedic admissions so that more surgical cases would stay local. Hospitalists were trained to perform stress tests so the hospital can provide testing on weekends. The group pays hospitalists a bonus for each admission, so when the ED calls, the hospitalists say, “Thanks! I’ll be right there.” The group also increased staffing on weekends.
The end result: It improves the hospital’s bottom line by shortening length of stay, and improving quality of care, patient satisfaction, and group morale.
“When we align the incentives, everybody wins,” says Dr. Friar. “The system has more capacity, the patients get better care, and the hospitalists no longer feel that weekend shifts are a huge burden.”
- Build “system-ness.” Sharing providers between hospitals has helped HNM build a cohesive system of quality care. What began as a way to cover shifts has created an interinstitutional camaraderie that allows for the easier flow of patients, improved communication, and widespread use of best-practice models. Sharing such resources as billing, credentialing, benefits, recruiting, and payroll has helped the group stay competitive, Dr. Ahlstrom says.
Growth in a Down Economy
Jude R. Alexander, MD, president of Inpatient Specialists in Rockville, Md., a bedroom community about 12 miles northwest of Washington, D.C., has continued to grow his group despite the down economy. Hospital admissions in the D.C. area decreased sharply in the second half of 2008, and patient volume rebounded slowly in the first half of 2009.
Inpatient Specialists initially downsized its staff, then it used flex physicians to meet demand as volume increased.
Despite national hospital trends of budget shortfalls, downgraded bond ratings, and increases in uninsured patients, two of Inpatient Specialists’ client hospitals chose to invest in the HM program. Dr. Alexander credits the vote of confidence to his group’s track record of optimal resource utilization, which has inherent cost savings in the millions.
Dr. Alexander also recommends HM groups in tough economic circumstances should:
- Maintain good relationships with partner hospitals;
- Run a lean business;
- Focus on excellent customer service to patients, their families, and their PCPs; and
- Build strong alliances with employed physicians by eliciting and giving constructive feedback.
“Following this basic strategy, Inpatient Specialists has experienced 7% growth in patient volume in the past 12 months,” Dr. Alexander says. “We’ve expanded to 40 full-time equivalent hospitalists, and 40 part-time employees.” Inpatient Specialists has its eye on geographic expansion, as well. The group is targeting services throughout the Capitol region—Maryland, Virginia, and the District of Columbia.
Bankruptcy to Profitability in One Year
In 2007, a few months after the 99-bed Auburn Memorial Hospital in Auburn, N.Y., was forced into bankruptcy, James Leyhane, MD, and his hospitalist group were displeased that they weren’t in control of their own program. Physicians had started leaving the hospital; Dr. Leyhane himself had interviewed at another hospital. “Our CEO approached me to ask what would make it right,” Dr. Leyhane recalls. “I said, ‘We’d need to be employed by the hospital.’ ”
The hospital and the private, six-physician internal-medicine group that employed the program entered bids on the HM group. In March 2008, the HM group became contractually employed by the hospital. Dr. Leyhane was given full control as hospitalist director of Auburn Memorial Hospitalists.
As a result of the new alignment, two major shifts took place. First, the hospital CEO more aggressively recruited subspecialists and surgeons. With the HM group now affiliated with the hospital, recruiting surgeons to Auburn Memorial became much easier. Second, more primary-care physicians (PCPs) began sending their patients to Auburn Memorial.
“We were all shocked at how quickly the administration was able to recruit new subspecialists to the area,” Dr. Leyhane says. “That helped get the profitable procedures back to the hospital.”
The biggest surprise came at the end of 2008. Patient volume had risen 11.5% higher than the hospital’s best-case predictions. “As a result of our emerging from under the umbrella of one physician group, the outlying physicians became less fearful that they might lose their patients to that group,” Dr. Leyhane says. “And in good faith, we still maintain a coverage arrangement with that IM group.”
Thus, what was first seen as a bad thing turned into a very good thing for both the hospitalist group and the hospital. Auburn Memorial posted a $3.1 million profit in 2008 (see Table 1).
Dr. Leyhane suggests HM group leaders facing similar financial crunches talk to area subspecialists and find out what it would take to get them affiliated with their institution.
“In our case, a stable hospitalist program was definitely one of their top requests,” Dr. Leyhane says, adding it also would be beneficial to include PCPs in the “what do you want from our hospital?” conversation. TH
Andrea M. Sattinger is a freelance writer based in North Carolina.
Image Source: COLIN ANDERSON/GETTYIMAGES
The headlines are harrowing: corporate layoffs; foreclosures on the rise; 401(k) retirement plans halved; government bailouts adding to the national debt. The worst economic downturn since the Great Depression has generated some unexpected outcomes, yet not all of them are bad for hospitalists. Below, four vignettes highlight HM groups that have achieved success despite—or in some cases because of—these troubled times.
A Better Business Agreement
It has taken nearly two years—and sometimes as many as four meetings a week—but Rajeev Alexander, MD, and his colleagues are nearing the finish line of an evolving business arrangement. The new arrangement has come about due to the economic downturn, which forced Oregon Medical Group (OMG), a multispecialty physician group serving hospitals in the Eugene/Springfield area and the HM group’s employer since 1988, to want to divest themselves of the hospitalist group. Now, after a lengthy negotiation, Dr. Alexander’s group of eight hospitalists is busier than ever.
Through what were essentially multiple quasi-buyouts, divestitures, and mergers, Dr. Alexander’s hospitalist group “spun off” from OMG and affiliated with PeaceHealth, a nonprofit health system serving seven hospitals in Oregon, Washington, and Alaska. The new contract means Dr. Alexander’s group is directly employed by Sacred Heart Hospital, a 541-bed PeaceHealth-owned facility in Eugene.
The new contract included a non-compete clause with OMG, which currently employs five hospitalists, yet Dr. Alexander’s group has maintained its patient volume. Compensation held steady and employee benefits improved. During an independent and slow-moving negotiation, Dr. Alexander’s group has merged with another HM service that originally was employed by PeaceHealth. The two HM groups (technically competitors) now practice in the same hospital and are ironing out the terms of the merger. At the moment, the groups have created a mutually respectful joint governance council.
“We’ve tackled the thorniest of problems,” Dr. Alexander says, “first, creating a combined work schedule to distribute patients and divide the work. Those of us on the governance council figured if we could get the docs to actually work together and share patients and communicate with each other as if they were one group, then the momentum for an actual administrative/contractual merger would feel inevitable.”
Although negotiations are expected to last through the end of the year to finalize such details as compensation, recruiting, and a group mission statement, the medical staff at Sacred Heart considers the merger a “done deal” and has thrown its support behind the effort. “Community outpatient docs have been clamoring for our services, and we have been having to hand out numbers and ask them to wait in line, so to speak,” Dr. Alexander says.
Dr. Alexander says he’s learned some lessons through the extensive negotiation process:
- Stay positive. In any business venture, absolutely nothing is impossible, even dodging a noncompete clause.
- Release your preconceptions. Conspiracy theories might abound, but most hospital administrators have the best of intentions. As highly regulated organizations, hospitals might simply be following their own bylaws and fulfilling responsibilities to stakeholders. Seek out at least one administrator whom you can trust, and with whom you can communicate effectively. A mutual understanding of intentions and objectives makes the process more successful for all concerned.
- Look beyond politics. Your trust and respect for administrators and fellow physicians will go a long way toward overcoming obstacles.
- Stick to your plan. Adhere to your goal of remaining independent, if that is important to you. “Our group resisted being funneled into becoming employed by a very large national hospitalist chain,” Dr. Alexander says, “and I would encourage physicians in other parts of the country to stick to their commitments as well.”
- Trust the negotiation process. Even if all goes well, what you’re shooting for at the beginning might not be exactly what you get after negotiations are over. This does not mean you’ve failed, or that hospital administration tricked you or failed to deliver on promises. It simply means you have created a negotiated settlement; both sides have come to a new appreciation for the other’s requirements and have made necessary and respectful accommodations.
Rural Rewards
Based in Traverse City, Hospitalists of Northwest Michigan (HNM) services four community hospitals and continues to witness solid growth. Since 2000, the group has grown from nine to nearly 40 providers, and from 2005 to 2008, patient encounters doubled. “In these hard economic times, hospitals are inviting us in because we provide value to the hospitals through leadership, increased hospital revenues, and improved recruiting and retention of specialists,” says Troy W. Ahlstrom, MD, president of HNM. “We continue to see healthy growth in patient volume as we align patient care goals with the needs of the hospitals and surrounding communities we serve.”
HNM, which established a service at the regional medical center and then assumed management of HM programs at three other rural hospitals, soon will add a fifth service to its ledger. HNM also began a pediatric program at the regional referral center, and the group is exploring the possibility of providing a network of pediatric care throughout the region.
Having grown up in the region, David Friar, MD, CEO of HNM, not only has a better understanding of the needs of rural hospitals, but also a personal investment in his group’s success. “These are our communities. We don’t view the hospitals as just a place to make a profit, but a place where our neighbors work and our families get their care,” he says.
Drs. Ahlstrom and Friar offer the following advice for achieving success in these economic times:
- Optimize receipts. Concern over compliance audits leads many hospitals to sacrifice group receipts by encouraging undercoding. “We’ve found hospitals do a poor job of negotiating the provider portion of third-party payer contracts and frequently lose provider charges because they focus on the much larger facility fees,” says Dr. Ahlstrom. The group’s receipts increased more than 30% when they began using an outside billing firm and adopted productivity incentives to encourage providers to practice better documentation and charge capture. Improving documentation also supports a hospital’s ability to accurately code its patients, which allows a hospital to bill for a more profitable diagnosis-related group (DRG), and improve its case-mix index. With these changes, Hospitalists of Northwest Michigan has increased provider pay and grown their practice while improving the hospitals’ profitability.
- Encourage frugality. The cost-plus model is popular, but it doesn’t incentivize programs to contain costs. In contrast, the fixed-price model encourages hospitalists to find cheaper ways to provide good care. “Because the money we save goes to us, we’ve all found creative ways to provide quality care for a third less money than similar cost-plus programs,” Dr. Ahlstrom says.
- Align incentives. Hospitals live or die on thin margins, Dr. Ahlstrom says. His group trains its employees to ask: What can I do to make the hospital stronger? “What’s good for the hospital is good for us, so we work with the hospitals, not for the hospitals,” Dr. Friar says.
At its smaller hospitals, HNM incentivized orthopedic admissions so that more surgical cases would stay local. Hospitalists were trained to perform stress tests so the hospital can provide testing on weekends. The group pays hospitalists a bonus for each admission, so when the ED calls, the hospitalists say, “Thanks! I’ll be right there.” The group also increased staffing on weekends.
The end result: It improves the hospital’s bottom line by shortening length of stay, and improving quality of care, patient satisfaction, and group morale.
“When we align the incentives, everybody wins,” says Dr. Friar. “The system has more capacity, the patients get better care, and the hospitalists no longer feel that weekend shifts are a huge burden.”
- Build “system-ness.” Sharing providers between hospitals has helped HNM build a cohesive system of quality care. What began as a way to cover shifts has created an interinstitutional camaraderie that allows for the easier flow of patients, improved communication, and widespread use of best-practice models. Sharing such resources as billing, credentialing, benefits, recruiting, and payroll has helped the group stay competitive, Dr. Ahlstrom says.
Growth in a Down Economy
Jude R. Alexander, MD, president of Inpatient Specialists in Rockville, Md., a bedroom community about 12 miles northwest of Washington, D.C., has continued to grow his group despite the down economy. Hospital admissions in the D.C. area decreased sharply in the second half of 2008, and patient volume rebounded slowly in the first half of 2009.
Inpatient Specialists initially downsized its staff, then it used flex physicians to meet demand as volume increased.
Despite national hospital trends of budget shortfalls, downgraded bond ratings, and increases in uninsured patients, two of Inpatient Specialists’ client hospitals chose to invest in the HM program. Dr. Alexander credits the vote of confidence to his group’s track record of optimal resource utilization, which has inherent cost savings in the millions.
Dr. Alexander also recommends HM groups in tough economic circumstances should:
- Maintain good relationships with partner hospitals;
- Run a lean business;
- Focus on excellent customer service to patients, their families, and their PCPs; and
- Build strong alliances with employed physicians by eliciting and giving constructive feedback.
“Following this basic strategy, Inpatient Specialists has experienced 7% growth in patient volume in the past 12 months,” Dr. Alexander says. “We’ve expanded to 40 full-time equivalent hospitalists, and 40 part-time employees.” Inpatient Specialists has its eye on geographic expansion, as well. The group is targeting services throughout the Capitol region—Maryland, Virginia, and the District of Columbia.
Bankruptcy to Profitability in One Year
In 2007, a few months after the 99-bed Auburn Memorial Hospital in Auburn, N.Y., was forced into bankruptcy, James Leyhane, MD, and his hospitalist group were displeased that they weren’t in control of their own program. Physicians had started leaving the hospital; Dr. Leyhane himself had interviewed at another hospital. “Our CEO approached me to ask what would make it right,” Dr. Leyhane recalls. “I said, ‘We’d need to be employed by the hospital.’ ”
The hospital and the private, six-physician internal-medicine group that employed the program entered bids on the HM group. In March 2008, the HM group became contractually employed by the hospital. Dr. Leyhane was given full control as hospitalist director of Auburn Memorial Hospitalists.
As a result of the new alignment, two major shifts took place. First, the hospital CEO more aggressively recruited subspecialists and surgeons. With the HM group now affiliated with the hospital, recruiting surgeons to Auburn Memorial became much easier. Second, more primary-care physicians (PCPs) began sending their patients to Auburn Memorial.
“We were all shocked at how quickly the administration was able to recruit new subspecialists to the area,” Dr. Leyhane says. “That helped get the profitable procedures back to the hospital.”
The biggest surprise came at the end of 2008. Patient volume had risen 11.5% higher than the hospital’s best-case predictions. “As a result of our emerging from under the umbrella of one physician group, the outlying physicians became less fearful that they might lose their patients to that group,” Dr. Leyhane says. “And in good faith, we still maintain a coverage arrangement with that IM group.”
Thus, what was first seen as a bad thing turned into a very good thing for both the hospitalist group and the hospital. Auburn Memorial posted a $3.1 million profit in 2008 (see Table 1).
Dr. Leyhane suggests HM group leaders facing similar financial crunches talk to area subspecialists and find out what it would take to get them affiliated with their institution.
“In our case, a stable hospitalist program was definitely one of their top requests,” Dr. Leyhane says, adding it also would be beneficial to include PCPs in the “what do you want from our hospital?” conversation. TH
Andrea M. Sattinger is a freelance writer based in North Carolina.
Image Source: COLIN ANDERSON/GETTYIMAGES