User login
Physicians should formulate a complete and accurate description of a patient’s condition with an equivalent plan of care for each encounter. While acuity and severity can be inferred by healthcare professionals without excessive detail or repetitive documentation of previously entered information, adequate documentation for every service date assists in conveying patient complexity during medical record review.
Regardless of how complex a patient’s condition might be, physicians tend to undervalue their services. This is due, in part, to the routine nature of patient care for seasoned physicians; it is also due in part to a general lack of understanding with respect to the documentation guidelines.
Consider the following scenario: A 68-year-old male with diabetes and a history of chronic obstructive bronchitis was hospitalized after a five-day history of progressive cough with increasing purulent sputum, shortness of breath, and fever. He was treated for an exacerbation of chronic bronchitis within the past six weeks. Upon admission, the patient had an increased temperature (102°F), increased heart rate (96 beats per minute), and increased respiratory rate (28 shallow breaths per minute). His breath sounds included in the right lower lobe rhonchi, and his pulse oximetry was 89% on room air. Chest X-ray confirmed right lower lobe infiltrates along with chronic changes.
Although some physicians would consider this “low complexity” due to the frequency in which they encounter this type of case, others will more appropriately identify this as moderately complex.
MDM Categories
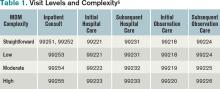
Medical decision-making (MDM) remains consistent in both the 1995 and 1997 guidelines.1,2 Complexity is categorized as straightforward, low, moderate, or high, based on the content of physician documentation. Each visit level is associated with a particular level of complexity. Only the care plan for a given date of service is considered when assigning MDM complexity. For each encounter, the physician receives credit for the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality (see Table 1).
Number of diagnoses or treatment options. Physicians should document problems addressed and managed daily despite any changes to the treatment plan. Credit is provided for each problem with an associated plan, even if the plan states “continue treatment.” Credit also depends upon the quantity of problems addressed, as well as the problem type. An established problem in which the care plan has been established by the physician or group practice member during the current hospitalization is less complex than a new problem for which a diagnosis, prognosis, or plan has not been determined. Severity of the problem affects the weight of complexity. A worsening problem is more complex than an improving problem. Physician documentation should:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- When documentation indicates a continuation of current management options (e.g. “continue meds”), be sure that the management options to be continued are noted somewhere in the progress note for that encounter (e.g. medication list).
The plan of care outlines problems that the physician personally manages and those that impact management options, even if another physician directly oversees the problem. For example, the hospitalist might primarily manage diabetes, while the pulmonologist manages pneumonia. Since the pneumonia may impact the hospitalist’s plan for diabetic management, the hospitalist can receive credit for the pneumonia diagnosis if there is a non-overlapping, hospitalist-related care plan or comment about the pneumonia.
Amount and/or complexity of data ordered/reviewed. “Data” is classified as pathology/laboratory testing, radiology, and medicine-based diagnostics. Pertinent orders or results could be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”);
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary;
- Indicate when images, tracings, or specimens are “personally reviewed”; and
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Risks of complication and/or morbidity or mortality. Risk involves the patient’s presenting problem, diagnostic procedures ordered, and management options selected. It is measured as minimal, low, moderate, or high when compared with corresponding items assigned to each risk level (see Table 2). The highest individual item detected on the table determines the overall patient risk for that encounter.
Chronic conditions and invasive procedures pose more risk than acute, uncomplicated illnesses or non-invasive procedures. Stable or improving problems are not as menacing as progressing problems; minor exacerbations are less hazardous than severe exacerbations; and medication risk varies with the type and potential for adverse effects. A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change. Physicians should:
- Status all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), when applicable;
- Document all diagnostic or therapeutic procedures considered;
- Identify surgical risk factors involving comorbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding medication (e.g. “Continue Coumadin, monitor PT/INR”).
Determining complexity of medical decision-making. The final complexity of MDM depends upon the second-highest MDM category. The physician does not have to meet the requirements for all three MDM categories. For example, if a physician satisfies the requirements for a “multiple” number of diagnoses/treatment options, “limited” data, and “high” risk, the physician achieves moderate complexity decision-making (see Table 3). Remember that decision-making is just one of three components in evaluation and management services, along with history and exam.
Beware of payor variation, as it could have a significant impact on visit-level selection.3 Become acquainted with rules applicable to the geographical area. Review insurer websites for guidelines, policies, and “frequently asked questions” that can help improve documentation skills and support billing practices.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Nov. 14, 2011.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Nov. 14, 2011.
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.
Physicians should formulate a complete and accurate description of a patient’s condition with an equivalent plan of care for each encounter. While acuity and severity can be inferred by healthcare professionals without excessive detail or repetitive documentation of previously entered information, adequate documentation for every service date assists in conveying patient complexity during medical record review.
Regardless of how complex a patient’s condition might be, physicians tend to undervalue their services. This is due, in part, to the routine nature of patient care for seasoned physicians; it is also due in part to a general lack of understanding with respect to the documentation guidelines.
Consider the following scenario: A 68-year-old male with diabetes and a history of chronic obstructive bronchitis was hospitalized after a five-day history of progressive cough with increasing purulent sputum, shortness of breath, and fever. He was treated for an exacerbation of chronic bronchitis within the past six weeks. Upon admission, the patient had an increased temperature (102°F), increased heart rate (96 beats per minute), and increased respiratory rate (28 shallow breaths per minute). His breath sounds included in the right lower lobe rhonchi, and his pulse oximetry was 89% on room air. Chest X-ray confirmed right lower lobe infiltrates along with chronic changes.
Although some physicians would consider this “low complexity” due to the frequency in which they encounter this type of case, others will more appropriately identify this as moderately complex.
MDM Categories
Medical decision-making (MDM) remains consistent in both the 1995 and 1997 guidelines.1,2 Complexity is categorized as straightforward, low, moderate, or high, based on the content of physician documentation. Each visit level is associated with a particular level of complexity. Only the care plan for a given date of service is considered when assigning MDM complexity. For each encounter, the physician receives credit for the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality (see Table 1).
Number of diagnoses or treatment options. Physicians should document problems addressed and managed daily despite any changes to the treatment plan. Credit is provided for each problem with an associated plan, even if the plan states “continue treatment.” Credit also depends upon the quantity of problems addressed, as well as the problem type. An established problem in which the care plan has been established by the physician or group practice member during the current hospitalization is less complex than a new problem for which a diagnosis, prognosis, or plan has not been determined. Severity of the problem affects the weight of complexity. A worsening problem is more complex than an improving problem. Physician documentation should:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- When documentation indicates a continuation of current management options (e.g. “continue meds”), be sure that the management options to be continued are noted somewhere in the progress note for that encounter (e.g. medication list).
The plan of care outlines problems that the physician personally manages and those that impact management options, even if another physician directly oversees the problem. For example, the hospitalist might primarily manage diabetes, while the pulmonologist manages pneumonia. Since the pneumonia may impact the hospitalist’s plan for diabetic management, the hospitalist can receive credit for the pneumonia diagnosis if there is a non-overlapping, hospitalist-related care plan or comment about the pneumonia.
Amount and/or complexity of data ordered/reviewed. “Data” is classified as pathology/laboratory testing, radiology, and medicine-based diagnostics. Pertinent orders or results could be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”);
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary;
- Indicate when images, tracings, or specimens are “personally reviewed”; and
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Risks of complication and/or morbidity or mortality. Risk involves the patient’s presenting problem, diagnostic procedures ordered, and management options selected. It is measured as minimal, low, moderate, or high when compared with corresponding items assigned to each risk level (see Table 2). The highest individual item detected on the table determines the overall patient risk for that encounter.
Chronic conditions and invasive procedures pose more risk than acute, uncomplicated illnesses or non-invasive procedures. Stable or improving problems are not as menacing as progressing problems; minor exacerbations are less hazardous than severe exacerbations; and medication risk varies with the type and potential for adverse effects. A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change. Physicians should:
- Status all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), when applicable;
- Document all diagnostic or therapeutic procedures considered;
- Identify surgical risk factors involving comorbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding medication (e.g. “Continue Coumadin, monitor PT/INR”).
Determining complexity of medical decision-making. The final complexity of MDM depends upon the second-highest MDM category. The physician does not have to meet the requirements for all three MDM categories. For example, if a physician satisfies the requirements for a “multiple” number of diagnoses/treatment options, “limited” data, and “high” risk, the physician achieves moderate complexity decision-making (see Table 3). Remember that decision-making is just one of three components in evaluation and management services, along with history and exam.
Beware of payor variation, as it could have a significant impact on visit-level selection.3 Become acquainted with rules applicable to the geographical area. Review insurer websites for guidelines, policies, and “frequently asked questions” that can help improve documentation skills and support billing practices.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Nov. 14, 2011.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Nov. 14, 2011.
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.
Physicians should formulate a complete and accurate description of a patient’s condition with an equivalent plan of care for each encounter. While acuity and severity can be inferred by healthcare professionals without excessive detail or repetitive documentation of previously entered information, adequate documentation for every service date assists in conveying patient complexity during medical record review.
Regardless of how complex a patient’s condition might be, physicians tend to undervalue their services. This is due, in part, to the routine nature of patient care for seasoned physicians; it is also due in part to a general lack of understanding with respect to the documentation guidelines.
Consider the following scenario: A 68-year-old male with diabetes and a history of chronic obstructive bronchitis was hospitalized after a five-day history of progressive cough with increasing purulent sputum, shortness of breath, and fever. He was treated for an exacerbation of chronic bronchitis within the past six weeks. Upon admission, the patient had an increased temperature (102°F), increased heart rate (96 beats per minute), and increased respiratory rate (28 shallow breaths per minute). His breath sounds included in the right lower lobe rhonchi, and his pulse oximetry was 89% on room air. Chest X-ray confirmed right lower lobe infiltrates along with chronic changes.
Although some physicians would consider this “low complexity” due to the frequency in which they encounter this type of case, others will more appropriately identify this as moderately complex.
MDM Categories
Medical decision-making (MDM) remains consistent in both the 1995 and 1997 guidelines.1,2 Complexity is categorized as straightforward, low, moderate, or high, based on the content of physician documentation. Each visit level is associated with a particular level of complexity. Only the care plan for a given date of service is considered when assigning MDM complexity. For each encounter, the physician receives credit for the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality (see Table 1).
Number of diagnoses or treatment options. Physicians should document problems addressed and managed daily despite any changes to the treatment plan. Credit is provided for each problem with an associated plan, even if the plan states “continue treatment.” Credit also depends upon the quantity of problems addressed, as well as the problem type. An established problem in which the care plan has been established by the physician or group practice member during the current hospitalization is less complex than a new problem for which a diagnosis, prognosis, or plan has not been determined. Severity of the problem affects the weight of complexity. A worsening problem is more complex than an improving problem. Physician documentation should:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- When documentation indicates a continuation of current management options (e.g. “continue meds”), be sure that the management options to be continued are noted somewhere in the progress note for that encounter (e.g. medication list).
The plan of care outlines problems that the physician personally manages and those that impact management options, even if another physician directly oversees the problem. For example, the hospitalist might primarily manage diabetes, while the pulmonologist manages pneumonia. Since the pneumonia may impact the hospitalist’s plan for diabetic management, the hospitalist can receive credit for the pneumonia diagnosis if there is a non-overlapping, hospitalist-related care plan or comment about the pneumonia.
Amount and/or complexity of data ordered/reviewed. “Data” is classified as pathology/laboratory testing, radiology, and medicine-based diagnostics. Pertinent orders or results could be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”);
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary;
- Indicate when images, tracings, or specimens are “personally reviewed”; and
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Risks of complication and/or morbidity or mortality. Risk involves the patient’s presenting problem, diagnostic procedures ordered, and management options selected. It is measured as minimal, low, moderate, or high when compared with corresponding items assigned to each risk level (see Table 2). The highest individual item detected on the table determines the overall patient risk for that encounter.
Chronic conditions and invasive procedures pose more risk than acute, uncomplicated illnesses or non-invasive procedures. Stable or improving problems are not as menacing as progressing problems; minor exacerbations are less hazardous than severe exacerbations; and medication risk varies with the type and potential for adverse effects. A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change. Physicians should:
- Status all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), when applicable;
- Document all diagnostic or therapeutic procedures considered;
- Identify surgical risk factors involving comorbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding medication (e.g. “Continue Coumadin, monitor PT/INR”).
Determining complexity of medical decision-making. The final complexity of MDM depends upon the second-highest MDM category. The physician does not have to meet the requirements for all three MDM categories. For example, if a physician satisfies the requirements for a “multiple” number of diagnoses/treatment options, “limited” data, and “high” risk, the physician achieves moderate complexity decision-making (see Table 3). Remember that decision-making is just one of three components in evaluation and management services, along with history and exam.
Beware of payor variation, as it could have a significant impact on visit-level selection.3 Become acquainted with rules applicable to the geographical area. Review insurer websites for guidelines, policies, and “frequently asked questions” that can help improve documentation skills and support billing practices.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Nov. 14, 2011.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Nov. 14, 2011.
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.