User login
SAN DIEGO – The utility of the Clinical Disease Activity Index as a simple, practical tool to quantify rheumatoid arthritis activity in everyday practice has gotten a big boost as a result of formal determination of the absolute change in the index that constitutes a minimally important difference.
"Our hope and expectation is that these MIDs [minimally important differences] for absolute change in CDAI [Clinical Disease Activity Index] can be used to determine whether patients are improving, and to help manage the patients that we see in clinic in terms of what treatments might need to be altered," Dr. Jeffrey R. Curtis explained at the annual meeting of the American College of Rheumatology.
The Disease Activity Score 28 (DAS28) has a widely accepted MID of 1.2 units, making it highly useful in defining a patient’s magnitude of clinical improvement in clinical trial settings. For example, exceeding this MID early after going on tumor necrosis factor inhibitor therapy has been shown to predict high likelihood of low disease activity at 1 year (J. Rheumatol. 2012;39:1326-33). But the DAS28 is impractical except when a real-time measurement of acute phase reactants is available, which is often not the case in everyday practice. The CDAI could be a better option for clinicians who are willing to do a joint count. Until now, however, the MID for the CDAI in real-world settings has not been defined, noted Dr. Curtis of the University of Alabama, Birmingham.
He and his coinvestigators have rectified this situation. They accomplished this by analyzing data from the Canadian Early Arthritis Cohort (CATCH), a large observational cohort of patients with early rheumatoid arthritis. After exclusion of the 8% of CATCH participants with comorbid fibromyalgia, that left 1,191 patients with rheumatologist-diagnosed rheumatoid arthritis, a mean 5.8-month duration of symptoms at enrollment, and a baseline CDAI of 28.5.
The investigators compared changes in DAS28 and CDAI during a total of more than 3,200 pairs of rheumatology patient visits spaced at 3-month intervals during the first 12 months after enrollment.
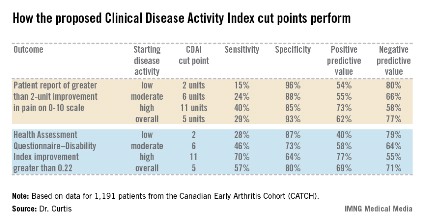
Overall, the best discriminator between a DAS28 MID indicative of significant clinical improvement as opposed to no improvement or worsening was a CDAI cut point of 5 units. That is, an absolute reduction of more than 5 units on the CDAI correlated well with a DAS28 improvement of at least 1.2 units. Indeed, the area under the receiver operator curve using a CDAI cut point of 5 units was 0.87. But there’s more to the story than that, according to Dr. Curtis.
"If at all possible, it’s preferable to use more specific CDAI MID cut points conditional on where patients are starting in terms of disease activity. Patients need less of a change in order to say that they feel better if they’re already starting out doing pretty well, with low disease activity, than if they’re starting with high disease activity," the rheumatologist said.
The generally accepted CDAI threshold for low disease activity is a score below 10. Moderate disease activity is a score of 10-22, while high disease activity is a CDAI in excess of 22. Dr. Curtis and his coworkers determined that the MID for patients with low disease activity is an absolute difference greater than 2 units. For patients with moderately active disease, it’s greater than 6 units. And for those with high disease activity, an absolute reduction of greater than 11 units defines the MID.
The investigators also tested the utility of their CDAI cut points in comparison to changes in outcomes other than the DAS28, including patient self-reported pain and Health Assessment Questionnaire-Disability Index scores (see chart).
Dr. Curtis reported receiving grants from and serving as a consultant to Amgen and Pfizer, which sponsor the CATCH study. He also receives funding from other companies as well as the National Institutes of Health.
SAN DIEGO – The utility of the Clinical Disease Activity Index as a simple, practical tool to quantify rheumatoid arthritis activity in everyday practice has gotten a big boost as a result of formal determination of the absolute change in the index that constitutes a minimally important difference.
"Our hope and expectation is that these MIDs [minimally important differences] for absolute change in CDAI [Clinical Disease Activity Index] can be used to determine whether patients are improving, and to help manage the patients that we see in clinic in terms of what treatments might need to be altered," Dr. Jeffrey R. Curtis explained at the annual meeting of the American College of Rheumatology.
The Disease Activity Score 28 (DAS28) has a widely accepted MID of 1.2 units, making it highly useful in defining a patient’s magnitude of clinical improvement in clinical trial settings. For example, exceeding this MID early after going on tumor necrosis factor inhibitor therapy has been shown to predict high likelihood of low disease activity at 1 year (J. Rheumatol. 2012;39:1326-33). But the DAS28 is impractical except when a real-time measurement of acute phase reactants is available, which is often not the case in everyday practice. The CDAI could be a better option for clinicians who are willing to do a joint count. Until now, however, the MID for the CDAI in real-world settings has not been defined, noted Dr. Curtis of the University of Alabama, Birmingham.
He and his coinvestigators have rectified this situation. They accomplished this by analyzing data from the Canadian Early Arthritis Cohort (CATCH), a large observational cohort of patients with early rheumatoid arthritis. After exclusion of the 8% of CATCH participants with comorbid fibromyalgia, that left 1,191 patients with rheumatologist-diagnosed rheumatoid arthritis, a mean 5.8-month duration of symptoms at enrollment, and a baseline CDAI of 28.5.
The investigators compared changes in DAS28 and CDAI during a total of more than 3,200 pairs of rheumatology patient visits spaced at 3-month intervals during the first 12 months after enrollment.
Overall, the best discriminator between a DAS28 MID indicative of significant clinical improvement as opposed to no improvement or worsening was a CDAI cut point of 5 units. That is, an absolute reduction of more than 5 units on the CDAI correlated well with a DAS28 improvement of at least 1.2 units. Indeed, the area under the receiver operator curve using a CDAI cut point of 5 units was 0.87. But there’s more to the story than that, according to Dr. Curtis.
"If at all possible, it’s preferable to use more specific CDAI MID cut points conditional on where patients are starting in terms of disease activity. Patients need less of a change in order to say that they feel better if they’re already starting out doing pretty well, with low disease activity, than if they’re starting with high disease activity," the rheumatologist said.
The generally accepted CDAI threshold for low disease activity is a score below 10. Moderate disease activity is a score of 10-22, while high disease activity is a CDAI in excess of 22. Dr. Curtis and his coworkers determined that the MID for patients with low disease activity is an absolute difference greater than 2 units. For patients with moderately active disease, it’s greater than 6 units. And for those with high disease activity, an absolute reduction of greater than 11 units defines the MID.
The investigators also tested the utility of their CDAI cut points in comparison to changes in outcomes other than the DAS28, including patient self-reported pain and Health Assessment Questionnaire-Disability Index scores (see chart).
Dr. Curtis reported receiving grants from and serving as a consultant to Amgen and Pfizer, which sponsor the CATCH study. He also receives funding from other companies as well as the National Institutes of Health.
SAN DIEGO – The utility of the Clinical Disease Activity Index as a simple, practical tool to quantify rheumatoid arthritis activity in everyday practice has gotten a big boost as a result of formal determination of the absolute change in the index that constitutes a minimally important difference.
"Our hope and expectation is that these MIDs [minimally important differences] for absolute change in CDAI [Clinical Disease Activity Index] can be used to determine whether patients are improving, and to help manage the patients that we see in clinic in terms of what treatments might need to be altered," Dr. Jeffrey R. Curtis explained at the annual meeting of the American College of Rheumatology.
The Disease Activity Score 28 (DAS28) has a widely accepted MID of 1.2 units, making it highly useful in defining a patient’s magnitude of clinical improvement in clinical trial settings. For example, exceeding this MID early after going on tumor necrosis factor inhibitor therapy has been shown to predict high likelihood of low disease activity at 1 year (J. Rheumatol. 2012;39:1326-33). But the DAS28 is impractical except when a real-time measurement of acute phase reactants is available, which is often not the case in everyday practice. The CDAI could be a better option for clinicians who are willing to do a joint count. Until now, however, the MID for the CDAI in real-world settings has not been defined, noted Dr. Curtis of the University of Alabama, Birmingham.
He and his coinvestigators have rectified this situation. They accomplished this by analyzing data from the Canadian Early Arthritis Cohort (CATCH), a large observational cohort of patients with early rheumatoid arthritis. After exclusion of the 8% of CATCH participants with comorbid fibromyalgia, that left 1,191 patients with rheumatologist-diagnosed rheumatoid arthritis, a mean 5.8-month duration of symptoms at enrollment, and a baseline CDAI of 28.5.
The investigators compared changes in DAS28 and CDAI during a total of more than 3,200 pairs of rheumatology patient visits spaced at 3-month intervals during the first 12 months after enrollment.
Overall, the best discriminator between a DAS28 MID indicative of significant clinical improvement as opposed to no improvement or worsening was a CDAI cut point of 5 units. That is, an absolute reduction of more than 5 units on the CDAI correlated well with a DAS28 improvement of at least 1.2 units. Indeed, the area under the receiver operator curve using a CDAI cut point of 5 units was 0.87. But there’s more to the story than that, according to Dr. Curtis.
"If at all possible, it’s preferable to use more specific CDAI MID cut points conditional on where patients are starting in terms of disease activity. Patients need less of a change in order to say that they feel better if they’re already starting out doing pretty well, with low disease activity, than if they’re starting with high disease activity," the rheumatologist said.
The generally accepted CDAI threshold for low disease activity is a score below 10. Moderate disease activity is a score of 10-22, while high disease activity is a CDAI in excess of 22. Dr. Curtis and his coworkers determined that the MID for patients with low disease activity is an absolute difference greater than 2 units. For patients with moderately active disease, it’s greater than 6 units. And for those with high disease activity, an absolute reduction of greater than 11 units defines the MID.
The investigators also tested the utility of their CDAI cut points in comparison to changes in outcomes other than the DAS28, including patient self-reported pain and Health Assessment Questionnaire-Disability Index scores (see chart).
Dr. Curtis reported receiving grants from and serving as a consultant to Amgen and Pfizer, which sponsor the CATCH study. He also receives funding from other companies as well as the National Institutes of Health.
AT THE ACR ANNUAL MEETING
Major finding: The minimally important difference on the Clinical Disease Activity Index that defines clinically meaningful improvement in rheumatoid arthritis patients is an absolute reduction greater than 5 units.
Data source: This determination was made by correlating changes in the CDAI and the Disease Activity Score 28 in 1,191 patients with early rheumatoid arthritis in the CATCH cohort.
Disclosures: Dr. Curtis reported receiving grants from and serving as a consultant to Amgen and Pfizer, which sponsor the CATCH study. He also receives funding from other companies as well as the National Institutes of Health.