User login
Q) I am new to practice and working in urgent care. I was discussing the diagnosis of kidney stones with my supervising physician. He said he does an intravenous pyelogram (IVP) to diagnose stones. He is a little “old school,” and I’m not sure he is right. What is “state of the art” in the work-up and acute treatment for kidney stones?
An IVP involves taking a series of x-rays following the injection of dye into a patient’s vein. As the dye moves through the bloodstream, the anatomy of the urinary system can be better visualized and the stone location identified, as the dye tends to accumulate at areas of obstruction. The downside to this test is that contrast can cause allergic reactions in some patients and can only be used in those with normal renal function. Also, a radiologist is required to be present during the procedure, and the test can take a long time to complete if a severe blockage is present.4
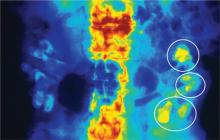
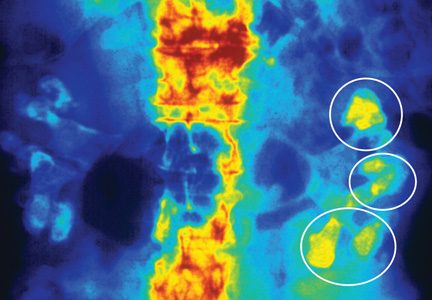
Today, noncontrast CT is considered the gold standard for imaging renal calculi because it is fast, safe (no worries for those with contrast allergy or renal impairment), and nearly 100% accurate.5
There are multiple options for treating kidney stones, though some are more invasive than others. For stones 2 cm or less identified in the upper or middle calyx and renal pelvis, extracorporeal shock wave lithotripsy (ESWL) is the treatment of choice.5,6 The goal of ESWL is to break the stone into small particles that can then be expelled through the urinary system. Adjunct measures, including mechanical percussion, diuresis, and inversion therapy, are often used following lithotripsy to facilitate passage of stone fragments. Medications such as calcium blockers and α-receptor blockers are also used to improve outcomes after lithotripsy. In the past, obese patients had less success with lithotripsy; however, technological advances have improved outcomes in depths up to 17 cm from skin to stone.6
For stones in the lower pole of the kidney (and depending on the size of the stone), ESWL, percutaneous nephrolitholapaxy, retrograde flexible ureteronephroscopy, and partial nephrectomy are options for treatment.3,7 Using an intravenous urogram, measurements and angles are calculated to help determine which procedure would be best for a particular patient.7 In simple terms, narrow angles and longer tube distances make it more difficult for stone particles to exit the urinary system. Therefore, if these problems are identified, an invasive approach may be needed to remove a stone. Other important considerations include stone size, patient symptoms, evidence of infection, or obstruction.7
ESWL is an attractive option for stone removal because it is noninvasive, has a reasonable safety profile, and is less costly than other, more invasive measures. However, advances in endoscopic instrument design are reducing complications previously associated with more invasive approaches, while improving long-term stone-free outcome rates. There may be increased utilization of procedures such as percutaneous nephrolitholapaxy and retrograde flexible ureteronephroscopy in the future.
Kristina Unterseher, CNN-NP
PeaceHealth
St. John Medical Group
Longview, WA
REFERENCES
1. Fink HA, Wilt TJ, Eidman KE, et al. Medical management to prevent recurrent nephrolithiasis in adults: a systematic review for an American College of Physicians Clinical Guideline. Ann Intern Med. 2013;158(7):535-543.
2. Hiatt RA, Ettinger B, Caan B, et al. Randomized controlled trial of a low animal protein, high fiber diet in the prevention of recurrent calcium oxalate kidney stones. Am J Epidemiol. 1996;144(1):25-33.
3. Moe OW. Kidney stones: pathophysiology and medical management. Lancet. 2006; 367(9507):333-344.
4. American College of Radiology and Radiological Society of North America. Intravenous pyelogram (2013). www.radiologyinfo.org/en/info.cfm?pg=ivp. Accessed December 16, 2013.
5. Boyce CJ, Pickhardt PJ, Lawrence EM, et al. Prevalence of urolithiasis in asymptomatic adults: objective determination using low dose noncontrast computerized tomography. J Urol. 2010;183(3):1017-1021.
6. Christian C, Thorsten B. The preferred treatment for upper tract stones is extracorporeal shock wave lithotripsy (ESWL) or ureteroscopic: pro ESWL. Urology. 2009;74(2):259-262.
7. Bourdoumis A, Papatsoris AG, Chrisofos M, Deliveliotis C. Lower pole stone management. Med Surg Urol. 2012. www.omicsonline.org/lower-pole-stone-management%20-2168-9857.S4-004.php?aid=7058?abstract _id=7058. Accessed December 16, 2013.
Q) I am new to practice and working in urgent care. I was discussing the diagnosis of kidney stones with my supervising physician. He said he does an intravenous pyelogram (IVP) to diagnose stones. He is a little “old school,” and I’m not sure he is right. What is “state of the art” in the work-up and acute treatment for kidney stones?
An IVP involves taking a series of x-rays following the injection of dye into a patient’s vein. As the dye moves through the bloodstream, the anatomy of the urinary system can be better visualized and the stone location identified, as the dye tends to accumulate at areas of obstruction. The downside to this test is that contrast can cause allergic reactions in some patients and can only be used in those with normal renal function. Also, a radiologist is required to be present during the procedure, and the test can take a long time to complete if a severe blockage is present.4
Today, noncontrast CT is considered the gold standard for imaging renal calculi because it is fast, safe (no worries for those with contrast allergy or renal impairment), and nearly 100% accurate.5
There are multiple options for treating kidney stones, though some are more invasive than others. For stones 2 cm or less identified in the upper or middle calyx and renal pelvis, extracorporeal shock wave lithotripsy (ESWL) is the treatment of choice.5,6 The goal of ESWL is to break the stone into small particles that can then be expelled through the urinary system. Adjunct measures, including mechanical percussion, diuresis, and inversion therapy, are often used following lithotripsy to facilitate passage of stone fragments. Medications such as calcium blockers and α-receptor blockers are also used to improve outcomes after lithotripsy. In the past, obese patients had less success with lithotripsy; however, technological advances have improved outcomes in depths up to 17 cm from skin to stone.6
For stones in the lower pole of the kidney (and depending on the size of the stone), ESWL, percutaneous nephrolitholapaxy, retrograde flexible ureteronephroscopy, and partial nephrectomy are options for treatment.3,7 Using an intravenous urogram, measurements and angles are calculated to help determine which procedure would be best for a particular patient.7 In simple terms, narrow angles and longer tube distances make it more difficult for stone particles to exit the urinary system. Therefore, if these problems are identified, an invasive approach may be needed to remove a stone. Other important considerations include stone size, patient symptoms, evidence of infection, or obstruction.7
ESWL is an attractive option for stone removal because it is noninvasive, has a reasonable safety profile, and is less costly than other, more invasive measures. However, advances in endoscopic instrument design are reducing complications previously associated with more invasive approaches, while improving long-term stone-free outcome rates. There may be increased utilization of procedures such as percutaneous nephrolitholapaxy and retrograde flexible ureteronephroscopy in the future.
Kristina Unterseher, CNN-NP
PeaceHealth
St. John Medical Group
Longview, WA
REFERENCES
1. Fink HA, Wilt TJ, Eidman KE, et al. Medical management to prevent recurrent nephrolithiasis in adults: a systematic review for an American College of Physicians Clinical Guideline. Ann Intern Med. 2013;158(7):535-543.
2. Hiatt RA, Ettinger B, Caan B, et al. Randomized controlled trial of a low animal protein, high fiber diet in the prevention of recurrent calcium oxalate kidney stones. Am J Epidemiol. 1996;144(1):25-33.
3. Moe OW. Kidney stones: pathophysiology and medical management. Lancet. 2006; 367(9507):333-344.
4. American College of Radiology and Radiological Society of North America. Intravenous pyelogram (2013). www.radiologyinfo.org/en/info.cfm?pg=ivp. Accessed December 16, 2013.
5. Boyce CJ, Pickhardt PJ, Lawrence EM, et al. Prevalence of urolithiasis in asymptomatic adults: objective determination using low dose noncontrast computerized tomography. J Urol. 2010;183(3):1017-1021.
6. Christian C, Thorsten B. The preferred treatment for upper tract stones is extracorporeal shock wave lithotripsy (ESWL) or ureteroscopic: pro ESWL. Urology. 2009;74(2):259-262.
7. Bourdoumis A, Papatsoris AG, Chrisofos M, Deliveliotis C. Lower pole stone management. Med Surg Urol. 2012. www.omicsonline.org/lower-pole-stone-management%20-2168-9857.S4-004.php?aid=7058?abstract _id=7058. Accessed December 16, 2013.
Q) I am new to practice and working in urgent care. I was discussing the diagnosis of kidney stones with my supervising physician. He said he does an intravenous pyelogram (IVP) to diagnose stones. He is a little “old school,” and I’m not sure he is right. What is “state of the art” in the work-up and acute treatment for kidney stones?
An IVP involves taking a series of x-rays following the injection of dye into a patient’s vein. As the dye moves through the bloodstream, the anatomy of the urinary system can be better visualized and the stone location identified, as the dye tends to accumulate at areas of obstruction. The downside to this test is that contrast can cause allergic reactions in some patients and can only be used in those with normal renal function. Also, a radiologist is required to be present during the procedure, and the test can take a long time to complete if a severe blockage is present.4
Today, noncontrast CT is considered the gold standard for imaging renal calculi because it is fast, safe (no worries for those with contrast allergy or renal impairment), and nearly 100% accurate.5
There are multiple options for treating kidney stones, though some are more invasive than others. For stones 2 cm or less identified in the upper or middle calyx and renal pelvis, extracorporeal shock wave lithotripsy (ESWL) is the treatment of choice.5,6 The goal of ESWL is to break the stone into small particles that can then be expelled through the urinary system. Adjunct measures, including mechanical percussion, diuresis, and inversion therapy, are often used following lithotripsy to facilitate passage of stone fragments. Medications such as calcium blockers and α-receptor blockers are also used to improve outcomes after lithotripsy. In the past, obese patients had less success with lithotripsy; however, technological advances have improved outcomes in depths up to 17 cm from skin to stone.6
For stones in the lower pole of the kidney (and depending on the size of the stone), ESWL, percutaneous nephrolitholapaxy, retrograde flexible ureteronephroscopy, and partial nephrectomy are options for treatment.3,7 Using an intravenous urogram, measurements and angles are calculated to help determine which procedure would be best for a particular patient.7 In simple terms, narrow angles and longer tube distances make it more difficult for stone particles to exit the urinary system. Therefore, if these problems are identified, an invasive approach may be needed to remove a stone. Other important considerations include stone size, patient symptoms, evidence of infection, or obstruction.7
ESWL is an attractive option for stone removal because it is noninvasive, has a reasonable safety profile, and is less costly than other, more invasive measures. However, advances in endoscopic instrument design are reducing complications previously associated with more invasive approaches, while improving long-term stone-free outcome rates. There may be increased utilization of procedures such as percutaneous nephrolitholapaxy and retrograde flexible ureteronephroscopy in the future.
Kristina Unterseher, CNN-NP
PeaceHealth
St. John Medical Group
Longview, WA
REFERENCES
1. Fink HA, Wilt TJ, Eidman KE, et al. Medical management to prevent recurrent nephrolithiasis in adults: a systematic review for an American College of Physicians Clinical Guideline. Ann Intern Med. 2013;158(7):535-543.
2. Hiatt RA, Ettinger B, Caan B, et al. Randomized controlled trial of a low animal protein, high fiber diet in the prevention of recurrent calcium oxalate kidney stones. Am J Epidemiol. 1996;144(1):25-33.
3. Moe OW. Kidney stones: pathophysiology and medical management. Lancet. 2006; 367(9507):333-344.
4. American College of Radiology and Radiological Society of North America. Intravenous pyelogram (2013). www.radiologyinfo.org/en/info.cfm?pg=ivp. Accessed December 16, 2013.
5. Boyce CJ, Pickhardt PJ, Lawrence EM, et al. Prevalence of urolithiasis in asymptomatic adults: objective determination using low dose noncontrast computerized tomography. J Urol. 2010;183(3):1017-1021.
6. Christian C, Thorsten B. The preferred treatment for upper tract stones is extracorporeal shock wave lithotripsy (ESWL) or ureteroscopic: pro ESWL. Urology. 2009;74(2):259-262.
7. Bourdoumis A, Papatsoris AG, Chrisofos M, Deliveliotis C. Lower pole stone management. Med Surg Urol. 2012. www.omicsonline.org/lower-pole-stone-management%20-2168-9857.S4-004.php?aid=7058?abstract _id=7058. Accessed December 16, 2013.