User login
BARCELONA – Lithium and valproic acid are the treatments of choice for patients with bipolar disorder at increased risk for suicide, according to the findings of a large Finnish national study.
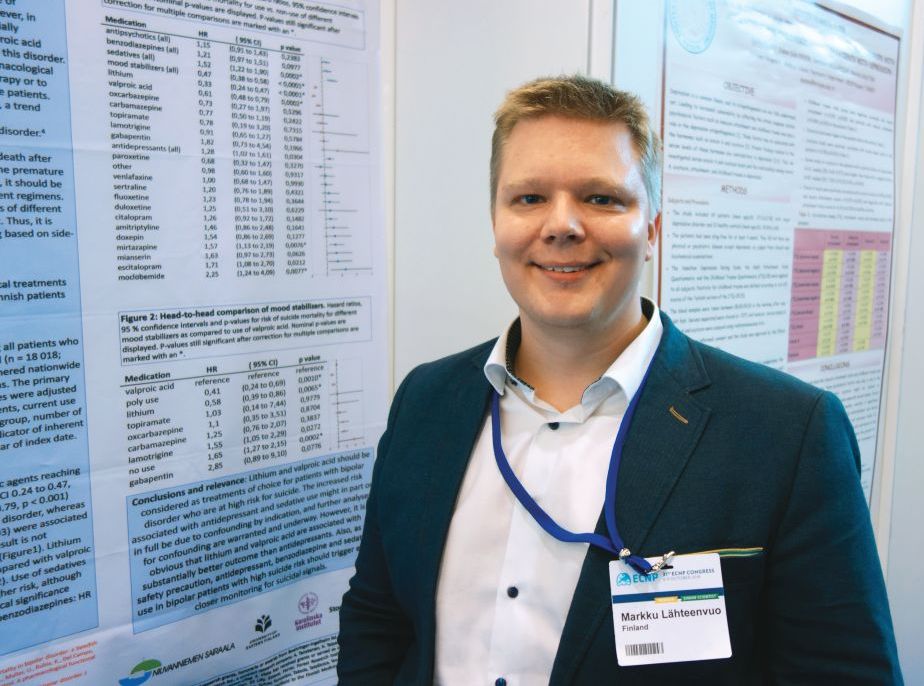
“We found that – surprise, surprise – lithium and valproic acid had the lowest risk of anyone committing suicide on them. And funnily enough, some antidepressants seemed to be correlated with a higher risk of committing suicide,” Markku Lähteenvuo, MD, PhD, said at the annual congress of the European College of Neuropsychopharmacology.
However, he suspects that the correlation between antidepressant therapy and suicide in bipolar patients probably was caused by confounding by indication.
“I wouldn’t have as a take-home message that SSRI [selective serotonin reuptake inhibitor] antidepressants are bad for you; it’s probably rather that these are really bad cases, treatment gets initiated when someone gets worse, and the antidepressants just aren’t quick enough to really give an effect. It takes 3-4 weeks for an SSRI to really kick in, whereas mood stabilizers like lithium and valproic acid usually kick in almost immediately, within a couple of days to a week,” explained Dr. Lähteenvuo, a forensic psychiatrist at Niuvanniemi Hospital and the University of Eastern Finland, in Kuopio.
He presented a study of all suicides among the 18,018 Finnish patients hospitalized for bipolar disorder nationwide during 1996-2012. Using prospective national databases to follow patients for a mean of 7.2 years, he and his coinvestigators were able to determine what medications they were on when they committed suicide and the likelihood they were actually taking their prescribed medications at the time.
In a multivariate proportional hazards analysis adjusted for concomitant psychotropic medications, duration of bipolar illness, intervals of drug exposure and nonexposure, age, sex, and number of hospitalizations for suicidality within the prior 2 years, bipolar patients on lithium had a 67% lower risk of suicide than did those not on the drug. Those on valproic acid were 39% less likely to commit suicide than those not on that mood stabilizer. And bipolar patients on lithium were 42% less likely to die from suicide than those on valproic acid.
At the other extreme, patients on antidepressants were in aggregate 28% more likely to commit suicide than those who were not. This risk varied considerably according to the specific antidepressant: for example, escitalopram and mirtazapine were associated with 71% and 57% greater risks of suicide, respectively, than in patients not on those antidepressants, while patients on paroxetine, venlafaxine, or sertraline were not at increased risk.
Also, the use of sedatives was associated with a 52% greater likelihood of suicide, and benzodiazepines were linked to a 21% increase in risk. Again, as with antidepressants, these associations with increased risk of completed suicide could be attributable in part or in whole to confounding by indication, the psychiatrist noted. He and his colleagues are conducting further analyses examining that possibility.
Pending the outcome of that closer look, however, Dr. Lähteenvuo believes the study’s message to clinicians is clear: “The use of lithium is getting less and less common all the time because of side effects. That’s also true for valproic acid. Many bipolar patients are now prescribed only antidepressants, even though all the guidelines advise against it due to the risk of hypomania. We think that this is a bad trend and that lithium and valproic acid should be prescribed more. Also, as a safety precaution, anyone with bipolar disorder on antidepressants or benzodiazepines or sedatives should be followed especially closely for suicidal signals, because they could carry a really highly increased risk – up to 50% – due to the medication as well.”
He reported having no financial conflicts regarding the study, funded by the Finnish government.
Dr. Lähteenvuo also was first author of a recent study showing that among the various drugs prescribed for treatment of bipolar disorder, lithium was the clear winner for prevention of rehospitalization in the same national Finnish population of more than 18,000 bipolar patients (JAMA Psychiatry. 2018;75[4]:347-55). One expert named this among the top four studies of the year in the field of mood disorders.
BARCELONA – Lithium and valproic acid are the treatments of choice for patients with bipolar disorder at increased risk for suicide, according to the findings of a large Finnish national study.
“We found that – surprise, surprise – lithium and valproic acid had the lowest risk of anyone committing suicide on them. And funnily enough, some antidepressants seemed to be correlated with a higher risk of committing suicide,” Markku Lähteenvuo, MD, PhD, said at the annual congress of the European College of Neuropsychopharmacology.
However, he suspects that the correlation between antidepressant therapy and suicide in bipolar patients probably was caused by confounding by indication.
“I wouldn’t have as a take-home message that SSRI [selective serotonin reuptake inhibitor] antidepressants are bad for you; it’s probably rather that these are really bad cases, treatment gets initiated when someone gets worse, and the antidepressants just aren’t quick enough to really give an effect. It takes 3-4 weeks for an SSRI to really kick in, whereas mood stabilizers like lithium and valproic acid usually kick in almost immediately, within a couple of days to a week,” explained Dr. Lähteenvuo, a forensic psychiatrist at Niuvanniemi Hospital and the University of Eastern Finland, in Kuopio.
He presented a study of all suicides among the 18,018 Finnish patients hospitalized for bipolar disorder nationwide during 1996-2012. Using prospective national databases to follow patients for a mean of 7.2 years, he and his coinvestigators were able to determine what medications they were on when they committed suicide and the likelihood they were actually taking their prescribed medications at the time.
In a multivariate proportional hazards analysis adjusted for concomitant psychotropic medications, duration of bipolar illness, intervals of drug exposure and nonexposure, age, sex, and number of hospitalizations for suicidality within the prior 2 years, bipolar patients on lithium had a 67% lower risk of suicide than did those not on the drug. Those on valproic acid were 39% less likely to commit suicide than those not on that mood stabilizer. And bipolar patients on lithium were 42% less likely to die from suicide than those on valproic acid.
At the other extreme, patients on antidepressants were in aggregate 28% more likely to commit suicide than those who were not. This risk varied considerably according to the specific antidepressant: for example, escitalopram and mirtazapine were associated with 71% and 57% greater risks of suicide, respectively, than in patients not on those antidepressants, while patients on paroxetine, venlafaxine, or sertraline were not at increased risk.
Also, the use of sedatives was associated with a 52% greater likelihood of suicide, and benzodiazepines were linked to a 21% increase in risk. Again, as with antidepressants, these associations with increased risk of completed suicide could be attributable in part or in whole to confounding by indication, the psychiatrist noted. He and his colleagues are conducting further analyses examining that possibility.
Pending the outcome of that closer look, however, Dr. Lähteenvuo believes the study’s message to clinicians is clear: “The use of lithium is getting less and less common all the time because of side effects. That’s also true for valproic acid. Many bipolar patients are now prescribed only antidepressants, even though all the guidelines advise against it due to the risk of hypomania. We think that this is a bad trend and that lithium and valproic acid should be prescribed more. Also, as a safety precaution, anyone with bipolar disorder on antidepressants or benzodiazepines or sedatives should be followed especially closely for suicidal signals, because they could carry a really highly increased risk – up to 50% – due to the medication as well.”
He reported having no financial conflicts regarding the study, funded by the Finnish government.
Dr. Lähteenvuo also was first author of a recent study showing that among the various drugs prescribed for treatment of bipolar disorder, lithium was the clear winner for prevention of rehospitalization in the same national Finnish population of more than 18,000 bipolar patients (JAMA Psychiatry. 2018;75[4]:347-55). One expert named this among the top four studies of the year in the field of mood disorders.
BARCELONA – Lithium and valproic acid are the treatments of choice for patients with bipolar disorder at increased risk for suicide, according to the findings of a large Finnish national study.
“We found that – surprise, surprise – lithium and valproic acid had the lowest risk of anyone committing suicide on them. And funnily enough, some antidepressants seemed to be correlated with a higher risk of committing suicide,” Markku Lähteenvuo, MD, PhD, said at the annual congress of the European College of Neuropsychopharmacology.
However, he suspects that the correlation between antidepressant therapy and suicide in bipolar patients probably was caused by confounding by indication.
“I wouldn’t have as a take-home message that SSRI [selective serotonin reuptake inhibitor] antidepressants are bad for you; it’s probably rather that these are really bad cases, treatment gets initiated when someone gets worse, and the antidepressants just aren’t quick enough to really give an effect. It takes 3-4 weeks for an SSRI to really kick in, whereas mood stabilizers like lithium and valproic acid usually kick in almost immediately, within a couple of days to a week,” explained Dr. Lähteenvuo, a forensic psychiatrist at Niuvanniemi Hospital and the University of Eastern Finland, in Kuopio.
He presented a study of all suicides among the 18,018 Finnish patients hospitalized for bipolar disorder nationwide during 1996-2012. Using prospective national databases to follow patients for a mean of 7.2 years, he and his coinvestigators were able to determine what medications they were on when they committed suicide and the likelihood they were actually taking their prescribed medications at the time.
In a multivariate proportional hazards analysis adjusted for concomitant psychotropic medications, duration of bipolar illness, intervals of drug exposure and nonexposure, age, sex, and number of hospitalizations for suicidality within the prior 2 years, bipolar patients on lithium had a 67% lower risk of suicide than did those not on the drug. Those on valproic acid were 39% less likely to commit suicide than those not on that mood stabilizer. And bipolar patients on lithium were 42% less likely to die from suicide than those on valproic acid.
At the other extreme, patients on antidepressants were in aggregate 28% more likely to commit suicide than those who were not. This risk varied considerably according to the specific antidepressant: for example, escitalopram and mirtazapine were associated with 71% and 57% greater risks of suicide, respectively, than in patients not on those antidepressants, while patients on paroxetine, venlafaxine, or sertraline were not at increased risk.
Also, the use of sedatives was associated with a 52% greater likelihood of suicide, and benzodiazepines were linked to a 21% increase in risk. Again, as with antidepressants, these associations with increased risk of completed suicide could be attributable in part or in whole to confounding by indication, the psychiatrist noted. He and his colleagues are conducting further analyses examining that possibility.
Pending the outcome of that closer look, however, Dr. Lähteenvuo believes the study’s message to clinicians is clear: “The use of lithium is getting less and less common all the time because of side effects. That’s also true for valproic acid. Many bipolar patients are now prescribed only antidepressants, even though all the guidelines advise against it due to the risk of hypomania. We think that this is a bad trend and that lithium and valproic acid should be prescribed more. Also, as a safety precaution, anyone with bipolar disorder on antidepressants or benzodiazepines or sedatives should be followed especially closely for suicidal signals, because they could carry a really highly increased risk – up to 50% – due to the medication as well.”
He reported having no financial conflicts regarding the study, funded by the Finnish government.
Dr. Lähteenvuo also was first author of a recent study showing that among the various drugs prescribed for treatment of bipolar disorder, lithium was the clear winner for prevention of rehospitalization in the same national Finnish population of more than 18,000 bipolar patients (JAMA Psychiatry. 2018;75[4]:347-55). One expert named this among the top four studies of the year in the field of mood disorders.
REPORTING FROM THE ECNP CONGRESS
Key clinical point: Lithium and valproic acid protect patients with bipolar disorder from suicide.
Major finding: The likelihood of suicide was reduced by two-thirds in bipolar patients on lithium, compared with that of patients not on the mood stabilizer.
Study details: This was a retrospective study of more than 18,000 Finnish patients hospitalized at some point for bipolar disorder and the medications they were on when a subset of them committed suicide.
Disclosures: The presenter reported having no financial conflicts regarding the study, funded by the Finnish government.