User login
We thank Dr Zorian and colleagues for their editorial1 addressing our retrospective multicenter cohort study, “Morning Discharges and Patient Length-of-Stay in Inpatient General Internal Medicine.”2 Dr Zorian and colleagues raised a question about whether morning discharges were associated with emergency department (ED) boarding times (ie, the time between the decision to admit a patient and their departure from the ED). We also received correspondence from other readers expressing interest in this metric.
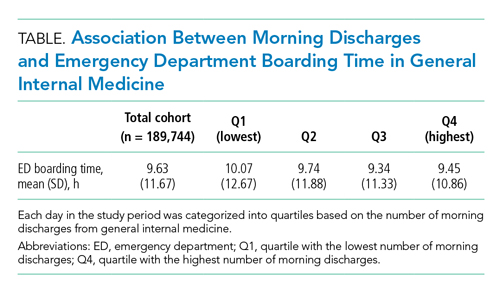
We measured the association between morning discharges from general internal medicine (GIM) and ED boarding time using the same methodology and cohort as previously described in our article.2 A total of 37 admissions out of 189,781 admissions (<0.1%) did not have an ED boarding time available and were excluded. The mean (SD) boarding time for the remaining cohort (n = 189,744) was 9.63 (11.67) hours. After categorizing days in the study period into quartiles based on the number of morning discharges from GIM, we did not find a strong unadjusted association with ED boarding times (Table). After multivariable adjustment with negative binomial regression models, as previously described,2 there was a weak, statistically significant association between the number of morning discharges and ED boarding time (adjusted rate ratio, 0.995; 95% CI, 0.991-1.000), corresponding to 2.4 minutes less in ED boarding time for every additional morning discharge. Ultimately, we agree with Dr Zorian and colleagues that instead of focusing on discharge-before-noon, hospitals should consider patient flow and discharge quality more holistically.
1. Zorian A, Shine D, Mourad M. Discharge by noon: toward a better understanding of benefits and costs. J Hosp Med. 2021;16(6):384. https://doi.org/10.12788/jhm.3613
2. Kirubarajan A, Shin S, Fralick M, et al. Morning discharges and patient length of stay in inpatient general internal medicine. J Hosp Med. 2021;16(6):333-338. https://10.12788/jhm.3605
We thank Dr Zorian and colleagues for their editorial1 addressing our retrospective multicenter cohort study, “Morning Discharges and Patient Length-of-Stay in Inpatient General Internal Medicine.”2 Dr Zorian and colleagues raised a question about whether morning discharges were associated with emergency department (ED) boarding times (ie, the time between the decision to admit a patient and their departure from the ED). We also received correspondence from other readers expressing interest in this metric.
We measured the association between morning discharges from general internal medicine (GIM) and ED boarding time using the same methodology and cohort as previously described in our article.2 A total of 37 admissions out of 189,781 admissions (<0.1%) did not have an ED boarding time available and were excluded. The mean (SD) boarding time for the remaining cohort (n = 189,744) was 9.63 (11.67) hours. After categorizing days in the study period into quartiles based on the number of morning discharges from GIM, we did not find a strong unadjusted association with ED boarding times (Table). After multivariable adjustment with negative binomial regression models, as previously described,2 there was a weak, statistically significant association between the number of morning discharges and ED boarding time (adjusted rate ratio, 0.995; 95% CI, 0.991-1.000), corresponding to 2.4 minutes less in ED boarding time for every additional morning discharge. Ultimately, we agree with Dr Zorian and colleagues that instead of focusing on discharge-before-noon, hospitals should consider patient flow and discharge quality more holistically.
We thank Dr Zorian and colleagues for their editorial1 addressing our retrospective multicenter cohort study, “Morning Discharges and Patient Length-of-Stay in Inpatient General Internal Medicine.”2 Dr Zorian and colleagues raised a question about whether morning discharges were associated with emergency department (ED) boarding times (ie, the time between the decision to admit a patient and their departure from the ED). We also received correspondence from other readers expressing interest in this metric.
We measured the association between morning discharges from general internal medicine (GIM) and ED boarding time using the same methodology and cohort as previously described in our article.2 A total of 37 admissions out of 189,781 admissions (<0.1%) did not have an ED boarding time available and were excluded. The mean (SD) boarding time for the remaining cohort (n = 189,744) was 9.63 (11.67) hours. After categorizing days in the study period into quartiles based on the number of morning discharges from GIM, we did not find a strong unadjusted association with ED boarding times (Table). After multivariable adjustment with negative binomial regression models, as previously described,2 there was a weak, statistically significant association between the number of morning discharges and ED boarding time (adjusted rate ratio, 0.995; 95% CI, 0.991-1.000), corresponding to 2.4 minutes less in ED boarding time for every additional morning discharge. Ultimately, we agree with Dr Zorian and colleagues that instead of focusing on discharge-before-noon, hospitals should consider patient flow and discharge quality more holistically.
1. Zorian A, Shine D, Mourad M. Discharge by noon: toward a better understanding of benefits and costs. J Hosp Med. 2021;16(6):384. https://doi.org/10.12788/jhm.3613
2. Kirubarajan A, Shin S, Fralick M, et al. Morning discharges and patient length of stay in inpatient general internal medicine. J Hosp Med. 2021;16(6):333-338. https://10.12788/jhm.3605
1. Zorian A, Shine D, Mourad M. Discharge by noon: toward a better understanding of benefits and costs. J Hosp Med. 2021;16(6):384. https://doi.org/10.12788/jhm.3613
2. Kirubarajan A, Shin S, Fralick M, et al. Morning discharges and patient length of stay in inpatient general internal medicine. J Hosp Med. 2021;16(6):333-338. https://10.12788/jhm.3605
© 2021 Society of Hospital Medicine