User login
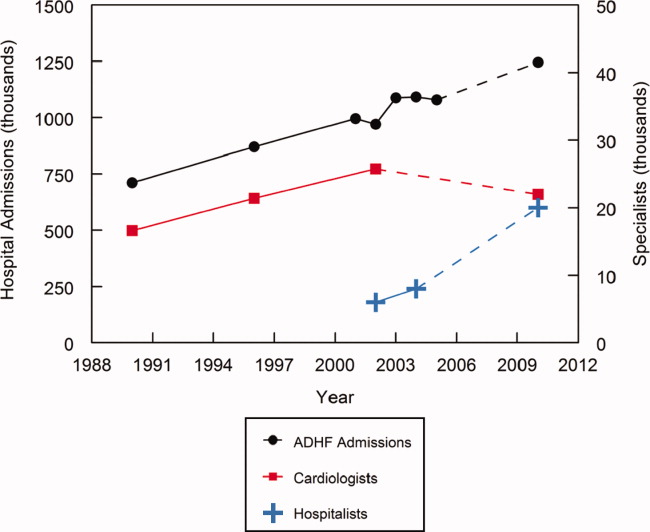
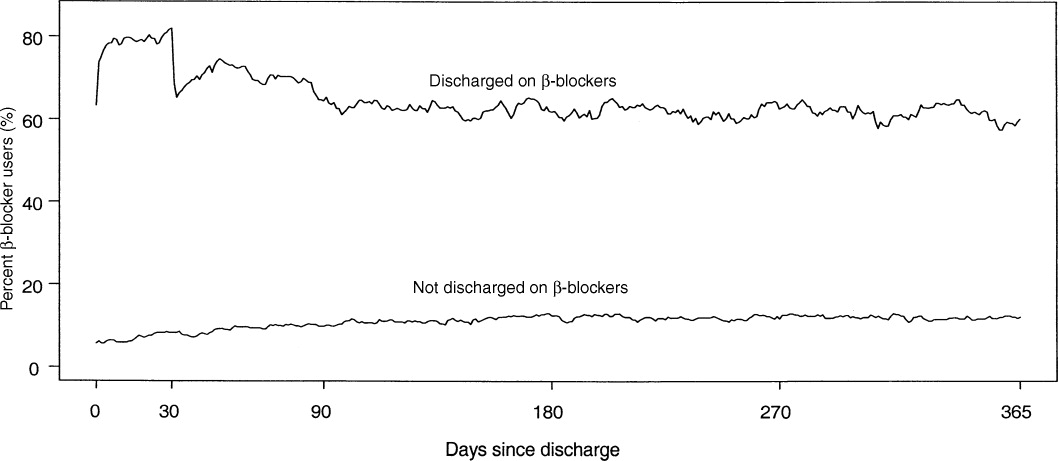
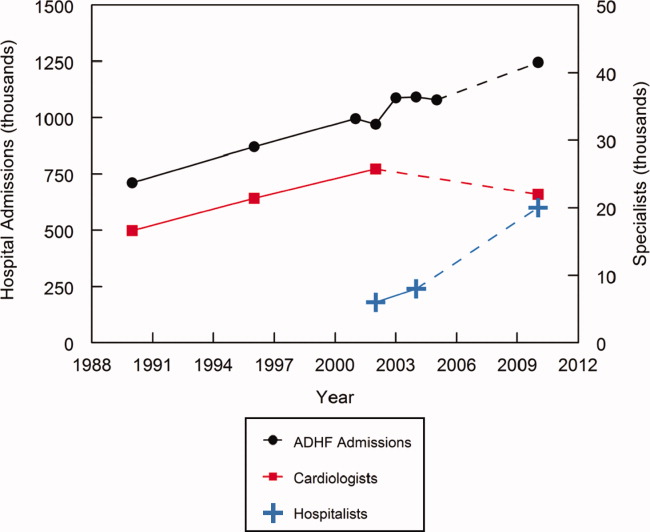
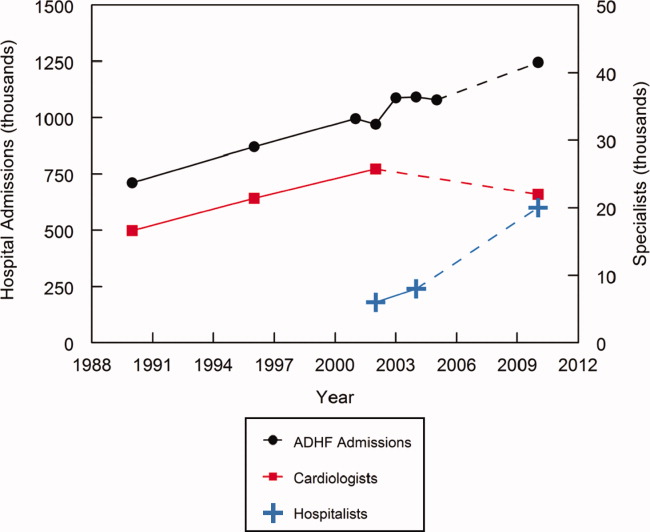
Acute decompensated heart failure (ADHF) is a common disorder that is frequently managed by hospitalists. This management is expected to expand over the next several years because of a continuing increase in the number of ADHF admissions coupled with a plateau or possible decline in the number of practicing cardiologists (Figure 1).114 In addition, 12% of fellowship training positions in cardiology were eliminated between 1995 and 2001, and the fact that the current number of training positions is inadequate to meet future demands is not recognized.15, 16 Given the severity of this disorder, the limited data from randomized, controlled clinical trials,17 and the limitations of current treatment, this management can be both challenging and rewarding. The goal of this special supplement of the Journal of Hospital Medicine is to assist hospitalists in this endeavor by summarizing the currently available data and treatment options and presenting a rational evidence‐based algorithm for the management of ADHF.
A multidisciplinary approach to heart failure has been shown to reduce cost, decrease length of stay, curtail readmissions, and improve compliance.1820 By leading and coordinating teams of physicians, pharmacists, nurses, nutritionists, physical therapists, and case managers and by developing and implementing indications for cardiology consultation, hospitalists can facilitate this multidisciplinary approach.21, 22 However, it is important to remember that hospitalists do not replace cardiologists, who remain a valuable and key component of this multidisciplinary team. Their input is vital in developing care pathways and criteria for consultation, and they, along with primary care physicians, will be the primary source of patient care following hospital discharge. Good communication between hospitalists and cardiologists is essential to optimize the care of patients with ADHF.
Maximizing the efficacy of ADHF care requires a thorough understanding of (1) the causes and potential treatments for the patient's acute decompensation, (2) the management of the patient's chronic heart failure, and (3) potential future therapies. Strategies to improve the continuum of heart failure care have been employed to help improve patient outcomes.23 For example, hospital‐based disease management programs have consistently been shown to optimize care and reduce rehospitalization rates in patients with heart failure.24 These programs involve a multidisciplinary, multifaceted approach to care in order to provide a continuum of care extending from hospitalization and into a patient's home environment.
Because of their practice location and experience, hospitalists are uniquely suited to influence acute inpatient care.25 They see patients in a variety of hospital settings and consequently tend to think of the entire system and not just an isolated component or patient.14 In addition, they have a vested interest in hospital quality improvement measures and are frequently involved in evaluating policies and procedures and developing and implementing clinical pathways, guidelines, and decision‐support tools.26 Data demonstrate that compliance is greater with evidence‐based guidelines and core performance measures when inpatient care is directed by a hospitalist.2730 Improved compliance with selected quality measures in patients with acute myocardial infarction and congestive heart failure has been observed when hospitals implement standardized admission and discharge orders.31, 32
Numerous transitions, such as outpatient to inpatient, intensive care unit to ward, and ward to home, occur during hospitalization, and these transitions are frequently associated with changes in the patient's medication regimen. During an acute illness, chronic medications may be held or discontinued, long‐acting medications may be changed to short‐acting ones to better titrate dose and achieve tighter control, and closed formularies may necessitate substituting 1 medication for another.33 A breakdown in communication during hospitalization‐associated transitions commonly affects medication regimens and can adversely impact patient care.3436 In a prospective evaluation, 53.6% [95% confidence interval (CI): 45.7%61.6%] of patients admitted to the hospital had at least 1 unintended discrepancy between their admission medication orders and their chronic outpatient regimen; 38.6% of these discrepancies were considered a potential threat to the patient.34 Likewise, 49% of patients being discharged from the hospital in another evaluation had an unexplained discrepancy between their preadmission and discharge medications.36 As a result, the Joint Commission on Accreditation of Healthcare Organizations now requires accredited facilities to perform medication reconciliation whenever a patient changes service, setting, provider, or level of care and new medication orders are written.37 This reconciliation is especially important in patients with heart failure, for whom polypharmacy is common and noncompliance with appropriate treatment regimens substantially increases readmission rates.3842
During these transition periods, hospitalists can play an important role in bridging the communication gap and providing this medication reconciliation.33 For example, actively involving hospitalists in all aspects of the reconciliation process at 1 institution resulted in a 4‐fold increase in consistency with preadmission medications.43 Similarly, because of the number of discharge summaries that they write, hospitalists are well suited to lead implementation of new policies and procedures to ensure compliance with recent changes in the Joint Commission on Accreditation of Healthcare Organizations requirements regarding these summaries.
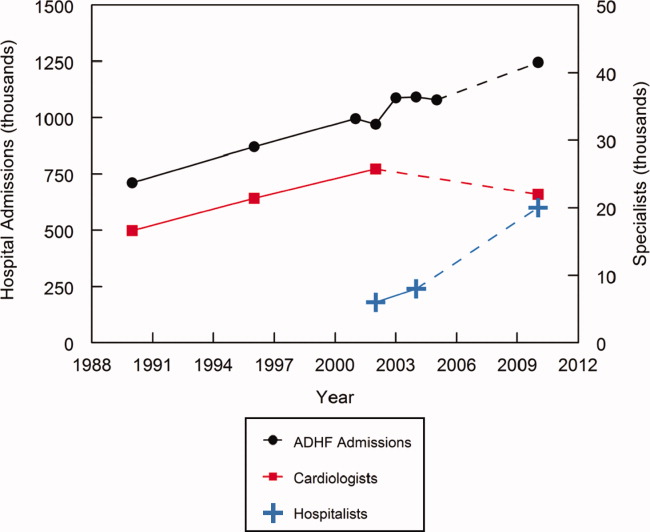
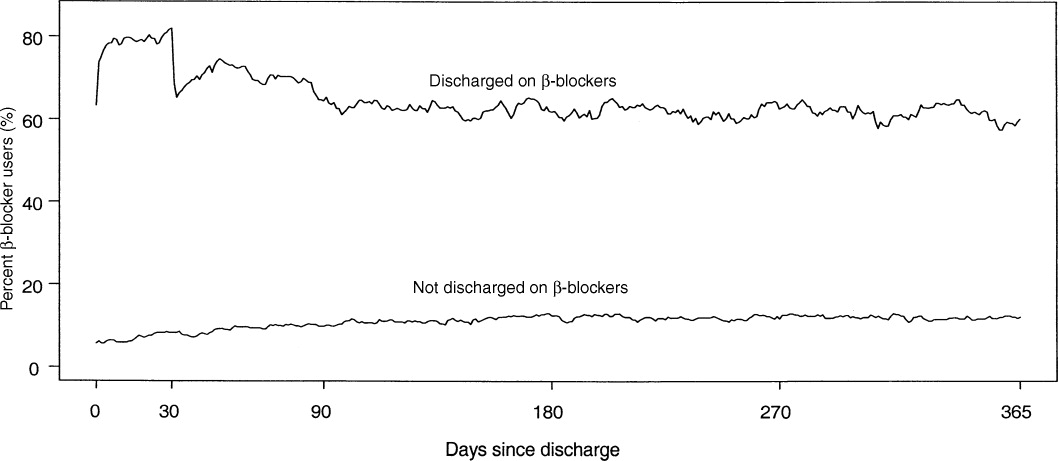
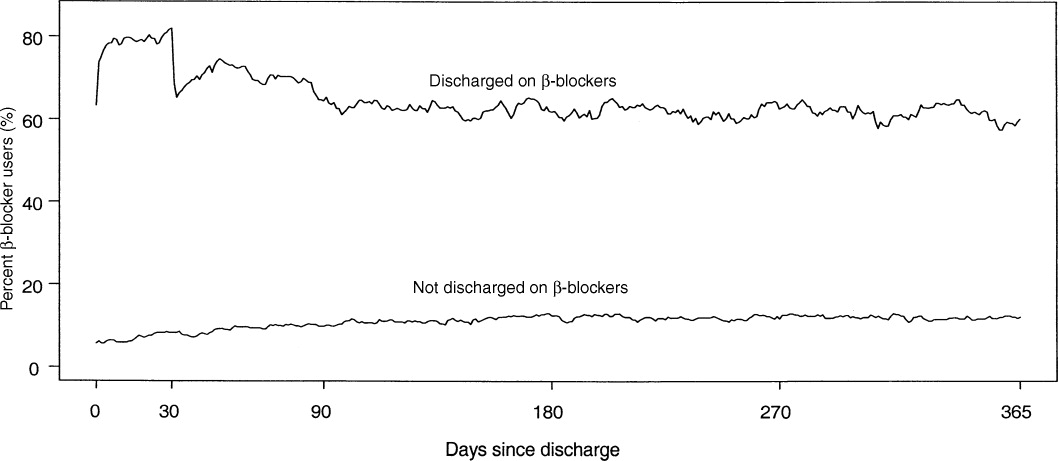
In addition to playing an active role in acute patient management, hospitalists can substantially influence long‐term care and outcomes. Consequently, hospitalists must be well versed in the management of chronic heart failure. Patients are intensely focused on their illness during the hospitalization period, and this focus enhances opportunities for meaningful education and behavior modification. Numerous studies have demonstrated that adherence to long‐term therapy is improved when this therapy is initiated before or at hospital discharge.4446 In an evaluation of data from the Organized Program To Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure Registry (OPTIMIZE‐HF), the prescription of a ‐blocker at discharge was associated with a significant reduction in 60‐ to 90‐day mortality [hazard ratio (HR): 0.48; 95% CI: 0.30‐0.79], and prescription of an angiotensin‐converting enzyme inhibitor or angiotensin receptor blocker at discharge was associated with a significant reduction in 60‐ to 90‐day mortality and/or rehospitalization (HR: 0.51; 95% CI: 0.34‐0.78).47 In the Cardiac Hospitalization Atherosclerosis Management Program (CHAMP), emphasizing initiation of chronic therapy prior to hospital discharge was associated with 3.0‐fold greater angiotensin‐converting enzyme inhibitor use and 3.2‐fold greater ‐blocker use at 1 year (both P < 0.01).46 Similarly, in patients surviving acute myocardial infarction, the strongest predictor of ‐blocker use at 30 days following discharge was receipt of a ‐blocker prescription at the time of discharge (HR: 15.8; 95% CI: 10.8‐23.3), and this beneficial effect was sustained for up to a year (Figure 2).44 Likewise, in patients with ADHF, the prevalence of ‐blocker therapy at 60 days was significantly increased when this therapy was initiated before discharge (91%) versus after discharge (73%; P < 0.001).45 This predischarge initiation of chronic therapy has been shown to reduce morbidity and mortality.
An awareness of new therapies for ADHF that are in late stages of clinical development can improve understanding of the complex pathophysiology of ADHF and enhance appropriate adaptation of these therapies once they become clinically available. These new therapies represent an attempt to improve on existing therapies, and consequently, they fall into the same 3 general categories as current therapies: diuretics, vasodilators, and inotropic agents.48, 49 Vasopressin receptor antagonists and adenosine receptor antagonists represent an attempt to stimulate aquaresis without inducing hyponatremia, hypokalemia, diminished glomerular filtration, or adverse neurohormonal activation;4854 endothelin receptor antagonists and newer natriuretic peptides represent an attempt to stimulate vasodilation and improve cardiac output without diminishing renal function;49, 55 and myosin activators and sodium‐potassium adenosine triphosphatase inhibitors represent an attempt to enhance contractility without inducing arrhythmogenicity or increasing mortality risk4859 (Table 1).
| Class/MOA | Agent(s) | Advantages/Disadvantages | References |
|---|---|---|---|
| |||
| Vasopressin receptor antagonists | Tolvaptan | Induce aquaresis without natriuresis | deGoma et al.48 |
| Conivaptan | Potentially avoid hyponatremia and hypokalemia | Tang and Hobbs49 | |
| Lixivaptan | Konstam et al.50 | ||
| SR‐121463b | Schrier et al.51 | ||
| Schweiger and Zdanowicz52 | |||
| Adenosine A1 receptor antagonists | Rolofylline | Increase renal blood flow | Tang and Hobbs49 |
| BG‐9719 | Increase intraglomerular hydraulic pressure | deGoma et al.48 | |
| BG‐9928 | May produce diuresis without adversely affecting glomerular filtration and renal function | Givertz et al.53 Greenberg et al.54 | |
| Endothelin receptor antagonists | Tezosentan | Potent vasodilator | Tang and Hobbs49 |
| Improves cardiac output | McMurray et al.55 | ||
| Hemodynamic effects have not translated into an improvement in heart failure symptoms or risk of death. | |||
| Natriuretic peptides | Ularitide | Resists inactivation by neutral endopeptidase | deGoma et al.48 |
| Improves filling pressures and dyspnea scores | Mitrovic et al.59 | ||
| No apparent deleterious effect on short‐term renal function | |||
| Myosin activators | CK‐1827452 | Tries to dissociate inotropy from arrhythmogenicity | deGoma et al.48 |
| Enhances contractility by targeting myocardial myosin, the force generating cardiac enzymes | Cytokinetics56 | ||
| Still very early in clinical development (just entered phase 2) | |||
| Sodium‐potassium ATPase inhibitors | Istaroxime | Tries to dissociate inotropy from arrhythmogenicity | deGoma et al.48 |
| Enhances contractility by stimulating calcium entry into the sarcolemmal Na/Ca exchanger | Blair et al.57 | ||
| Lusitropic | Cleland et al.58 | ||
| Still very early in clinical development (just completed first phase 2 trial) | |||
Finally, although major advancements in the medical therapy of heart failure patients have substantially improved outcomes,60 technological advances in mechanical devices,61 including automatic implantable cardioverter defibrillators, cardiac resynchronization therapy, and ventricular assist devices, as well as advances in the surgical treatment of heart failure,62 have also been used to support the failing heart. Heart failure patients being treated with mechanical devices, as well as those following cardiac transplant, require unique care. As more mechanical and surgical innovations emerge, nonpharmacologic therapy will continue to evolve as a cornerstone of the management strategy in heart failure patients. Hospitalists will need to rely on care pathways, criteria for consultation, and good communication with cardiologists to optimize the care of these patients. Hospitalists should work with their cardiology colleagues in their local institution to develop appropriate criteria for cardiology consultation, and everyone should be educated on these criteria.
The subsequent discussions in this supplement expand on these topics. First, I review the presentation and early recognition, risk stratification, and treatment of patients with ADHF and the role of the hospitalist in this assessment and treatment process. Next, Dr. Khan and Dr. Heywood review the role of diuretics, vasodilators, and ultrafiltration in the management of patients with volume overload and high filling pressures and conclude with a discussion of potential future pharmacologic treatment options, such as tolvaptan and rolofylline, and nonpharmacologic modalities, such as wireless hemodynamic monitoring through implanted devices. Finally, Dr. Michota and I discuss bridging the gap between evidence and practice in the management of patients with ADHF. We review the evidence‐based guidelines that are currently available; discuss the appropriate location for treatment based on the patient's initial history and physical, radiographic, and laboratory findings; provide a practical algorithm for this treatment; and discuss means to transition care from the inpatient setting to the outpatient setting in a manner that enhances compliance with long‐term therapy and reduces recidivism. Given the anticipated growth in ADHF and the need for hospitalists to manage this disease together with cardiologists and others, we believe that the provided information will be helpful in the management of ADHF.
- ,.National Hospital Discharge Survey: annual summary, 1996.Vital Health Stat.1999;13(140):1–46.
- ,,,.Hospitalization of patients with heart failure: National Hospital Discharge Survey, 1985 to 1995.Am Heart J.1999;137(2):352–360.
- ,,.National Hospital Discharge Survey: 2001 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2004;13(156):1–198.
- ,,.National Hospital Discharge Survey: 2002 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2005;13(158):1–199.
- ,,.National Hospital Discharge Survey: 2005 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2007;13(165):1–209.
- ,,.National Hospital Discharge Survey: 2004 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2006;13(162):1–209.
- ,,.National Hospital Discharge Survey: 2003 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2006;13(160):1–206.
- Division for Heart Disease and Stroke Prevention. Heart failure fact sheet. Available at: http://www.cdc.gov/dhdsp/library/fs_heart_failure_longdesc.htm. Accessed September2008.
- US Census Bureau. Projected population of the United States, by age and sex: 2000 to 2050. Available at: http://www.census.gov/population/www/projections/usinterimproj/natprojtab02a.pdf. Accessed September2008.
- ,,,.Demographics and cardiology, 1950–2050.J Am Coll Cardiol.2000;35(4):1067–1081.
- 35th Bethesda Conference.Cardiology's workforce crisis: a pragmatic approach. Bethesda, Maryland, 17–18 October 2003.J Am Coll Cardiol.2004;44(2):216–275.
- ,.The evolution of the hospitalist movement in the USA.Clin Med.2002;2(4):327–330.
- .Hospitalists in the United States—mission accomplished or work in progress?N Engl J Med.2004;350(19):1935–1936.
- .Identifying strategies to improve outcomes and reduce costs—a role for the hospitalist.Curr Opin Pulm Med.2004;10(suppl):S19–S22.
- ,.Cardiovascular manpower: the looming crisis.Circulation.2004;109(7):817–820.
- ,.The United States cardiovascular care deficit.Circulation.2004;109(7):821–823.
- Heart Failure Society of America.Evaluation and management of patients with acute decompensated heart failure.J Card Fail.2006;12(1):e86–e103.
- ,,,.Reduction in heart failure events by the addition of a clinical pharmacist to the heart failure management team. Results of the Pharmacist in Heart Failure Assessment Recommendation and Monitoring (PHARM) study.Arch Intern Med.1999;159(16):1939–1945.
- ,,,,.Impact of care at a multidisciplinary congestive heart failure clinic: a randomized trial.CMAJ.2005;173(1):40–45.
- ,.Implementing a congestive heart failure disease management program to decrease length of stay and cost.J Cardiovasc Nurs.1999;14(1):55–74.
- ,,,,.The core competencies in hospital medicine: a framework for curriculum development by the Society of Hospital Medicine.J Hosp Med.2006;1(suppl 1):2–95.
- ,,, et al.ASHP‐SHM joint statement on hospitalist‐pharmacist collaboration.J Hosp Med.2008;3(suppl 3). doi://10.1002/jhm.315. Available at: http://www3.interscience.wiley.com.
- ,,,,,.Heart failure: improving the continuum of care.Care Manag J.2006;7(2):58–63.
- ,,.Strategies to reduce hospitalization in the management of heart failure.Lippincotts Case Manag.2005;10(6 suppl):S1–S15.
- .Improving the management of patients after myocardial infarction, from admission to discharge.Clin Ther.2006;28(10):1509–1539.
- .The role of hospitalists in the management of acute decompensated heart failure.Am Heart Hosp J.2005;3(2):111–117.
- ,,,,.Quality of care for patients hospitalized with heart failure: assessing the impact of hospitalists.Arch Intern Med.2002;162(11):1251–1256.
- ,.Productive interdisciplinary team relationships: the hospitalist and the case manager.Lippincotts Case Manag.2006;11(3):160–164.
- .Use of pay for performance in a community hospital private hospitalist group: a preliminary report.Trans Am Clin Climatol Assoc.2007;118:263–272.
- ,,.Comparison of practice patterns of hospitalists and community physicians in the care of patients with congestive heart failure.J Hosp Med.2008;3(1):35–41.
- ,,,,,.Integrating “best of care” protocols into clinicians' workflow via care provider order entry: impact on quality‐of‐care indicators for acute myocardial infarction.J Am Med Inform Assoc.2006;13(2):188–196.
- ,,, et al.Improved compliance with quality measures at hospital discharge with a computerized physician order entry system.Am Heart J.2006;151(3):643–653.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,, et al.Unintended medication discrepancies at the time of hospital admission.Arch Intern Med.2005;165(4):424–429.
- ,,,,,.Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients.Am J Health Syst Pharm.2004;61(16):1689–1695.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166(5):565–571.
- Joint Commission on Accreditation of Healthcare Organizations. Using medication reconciliation to prevent errors. Sentinel Event Alert #35. Available at: http://www.jointcommission.org/sentinelevents/sentineleventalert/sea_35.htm. Accessed September2008.
- ,,,.Precipitating factors leading to decompensation of heart failure: traits among urban blacks.Arch Intern Med.1988;148(9):2013–2016.
- ,,,,.Early readmission of elderly patients with congestive heart failure.J Am Geriatr Soc.1990;38(12):1290–1295.
- ,.Observation unit management of heart failure.Emerg Med Clin North Am.2001;19(1):209–232.
- ,,, et al.Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Failure National Registry (ADHERE).Am Heart J.2005;149(2):209–216.
- ,,, et al.Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure.JAMA.2006;296(18):2217–2226.
- . Eliminating drug errors: hospitals adopt medication reconciliation to improve patient safety. Available at: http://www.acponline.org/clinical_information/journals_publications/acp_hospitalist/may07/drug_errors.htm. Accessed September2008.
- ,,, et al.Outpatient adherence to beta‐blocker therapy after acute myocardial infarction.JAm Coll Cardiol.2002;40(9):1589–1595.
- ,.Predischarge initiation of carvedilol in patients hospitalized for decompensated heart failure.Am J Cardiol.2004;93(9A):74B–76B.
- ,,,.Improved treatment of coronary heart disease by implementation of a Cardiac Hospitalization Atherosclerosis Management Program (CHAMP).Am J Cardiol.2001;87(7):819–822.
- ,,, et al.Association between performance measures and clinical outcomes for patients hospitalized with heart failure.JAMA.2007;297(1):61–70.
- ,,,.Emerging therapies for the management of decompensated heart failure: from bench to bedside.J Am Coll Cardiol.2006;48(12):2397–2409.
- ,.Novel strategies for the management of acute decompensated heart failure.Curr Cardiol Rev.2005;1(1):1–5.
- ,,, et al.Effects of oral tolvaptan in patients hospitalized for worsening heart failure: the EVEREST outcome trial.JAMA.2007;297(12):1319–1331.
- ,,, et al.Tolvaptan, a selective oral vasopressin V2‐receptor antagonist, for hyponatremia.N Engl J Med.2006;355(20):2099–2112.
- ,.Vasopressin‐receptor antagonists in heart failure.Am J Health Syst Pharm.2008;65(9):807–817.
- ,,,,.The effects of KW‐3902, an adenosine A1‐receptor antagonist, on diuresis and renal function in patients with acute decompensated heart failure and renal impairment or diuretic resistance.J Am Coll Cardiol.2007;50(16):1551–1560.
- ,,, et al.Effects of multiple oral doses of an A1 adenosine antagonist, BG9928, in patients with heart failure: results of a placebo‐controlled, dose‐escalation study.J Am Coll Cardiol.2007;50(7):600–606.
- ,,, et al.Effects of tezosentan on symptoms and clinical outcomes in patients with acute heart failure: the VERITAS randomized controlled trials.JAMA.2007;298(17):2009–2019.
- CK‐1827452. Cytokinetics Web site. Available at: http://www.cytokinetics.com/ck_1827452. Accessed September2008.
- ,,, et al.Rationale and design of the hemodynamic, echocardiographic and neurohormonal effects of istaroxime, a novel intravenous inotropic and lusitropic agent: a randomized controlled trial in patients hospitalized with heart failure (HORIZON‐HF) trial.Am J Ther.2008;15(3):231–240.
- ,,, et al.Clinical trials update from the American College of Cardiology 2008: CARISMA, TRENDS, meta‐analysis of Cox‐2 studies, HAT, ON‐TARGET, HYVET, ACCOMPLISH, MOMENTUM, PROTECT, HORIZON‐HF and REVERSE.Eur J Heart Fail.2008;10(6):614–620.
- ,,, et al.Haemodynamic and clinical effects of ularitide in decompensated heart failure.Eur Heart J.2006;27(23):2823–2832.
- ,,.Mechanical support in acute and chronic heart failure.Curr Cardiol Rep.2008;10(3):168–175.
- ,.Devices in acute heart failure.Crit Care Med.2008;36(1 suppl):S121–S128.
- ,.Advances in the surgical treatment of heart failure.Curr Opin Cardiol.2008;23(3):249–253.
Acute decompensated heart failure (ADHF) is a common disorder that is frequently managed by hospitalists. This management is expected to expand over the next several years because of a continuing increase in the number of ADHF admissions coupled with a plateau or possible decline in the number of practicing cardiologists (Figure 1).114 In addition, 12% of fellowship training positions in cardiology were eliminated between 1995 and 2001, and the fact that the current number of training positions is inadequate to meet future demands is not recognized.15, 16 Given the severity of this disorder, the limited data from randomized, controlled clinical trials,17 and the limitations of current treatment, this management can be both challenging and rewarding. The goal of this special supplement of the Journal of Hospital Medicine is to assist hospitalists in this endeavor by summarizing the currently available data and treatment options and presenting a rational evidence‐based algorithm for the management of ADHF.
A multidisciplinary approach to heart failure has been shown to reduce cost, decrease length of stay, curtail readmissions, and improve compliance.1820 By leading and coordinating teams of physicians, pharmacists, nurses, nutritionists, physical therapists, and case managers and by developing and implementing indications for cardiology consultation, hospitalists can facilitate this multidisciplinary approach.21, 22 However, it is important to remember that hospitalists do not replace cardiologists, who remain a valuable and key component of this multidisciplinary team. Their input is vital in developing care pathways and criteria for consultation, and they, along with primary care physicians, will be the primary source of patient care following hospital discharge. Good communication between hospitalists and cardiologists is essential to optimize the care of patients with ADHF.
Maximizing the efficacy of ADHF care requires a thorough understanding of (1) the causes and potential treatments for the patient's acute decompensation, (2) the management of the patient's chronic heart failure, and (3) potential future therapies. Strategies to improve the continuum of heart failure care have been employed to help improve patient outcomes.23 For example, hospital‐based disease management programs have consistently been shown to optimize care and reduce rehospitalization rates in patients with heart failure.24 These programs involve a multidisciplinary, multifaceted approach to care in order to provide a continuum of care extending from hospitalization and into a patient's home environment.
Because of their practice location and experience, hospitalists are uniquely suited to influence acute inpatient care.25 They see patients in a variety of hospital settings and consequently tend to think of the entire system and not just an isolated component or patient.14 In addition, they have a vested interest in hospital quality improvement measures and are frequently involved in evaluating policies and procedures and developing and implementing clinical pathways, guidelines, and decision‐support tools.26 Data demonstrate that compliance is greater with evidence‐based guidelines and core performance measures when inpatient care is directed by a hospitalist.2730 Improved compliance with selected quality measures in patients with acute myocardial infarction and congestive heart failure has been observed when hospitals implement standardized admission and discharge orders.31, 32
Numerous transitions, such as outpatient to inpatient, intensive care unit to ward, and ward to home, occur during hospitalization, and these transitions are frequently associated with changes in the patient's medication regimen. During an acute illness, chronic medications may be held or discontinued, long‐acting medications may be changed to short‐acting ones to better titrate dose and achieve tighter control, and closed formularies may necessitate substituting 1 medication for another.33 A breakdown in communication during hospitalization‐associated transitions commonly affects medication regimens and can adversely impact patient care.3436 In a prospective evaluation, 53.6% [95% confidence interval (CI): 45.7%61.6%] of patients admitted to the hospital had at least 1 unintended discrepancy between their admission medication orders and their chronic outpatient regimen; 38.6% of these discrepancies were considered a potential threat to the patient.34 Likewise, 49% of patients being discharged from the hospital in another evaluation had an unexplained discrepancy between their preadmission and discharge medications.36 As a result, the Joint Commission on Accreditation of Healthcare Organizations now requires accredited facilities to perform medication reconciliation whenever a patient changes service, setting, provider, or level of care and new medication orders are written.37 This reconciliation is especially important in patients with heart failure, for whom polypharmacy is common and noncompliance with appropriate treatment regimens substantially increases readmission rates.3842
During these transition periods, hospitalists can play an important role in bridging the communication gap and providing this medication reconciliation.33 For example, actively involving hospitalists in all aspects of the reconciliation process at 1 institution resulted in a 4‐fold increase in consistency with preadmission medications.43 Similarly, because of the number of discharge summaries that they write, hospitalists are well suited to lead implementation of new policies and procedures to ensure compliance with recent changes in the Joint Commission on Accreditation of Healthcare Organizations requirements regarding these summaries.
In addition to playing an active role in acute patient management, hospitalists can substantially influence long‐term care and outcomes. Consequently, hospitalists must be well versed in the management of chronic heart failure. Patients are intensely focused on their illness during the hospitalization period, and this focus enhances opportunities for meaningful education and behavior modification. Numerous studies have demonstrated that adherence to long‐term therapy is improved when this therapy is initiated before or at hospital discharge.4446 In an evaluation of data from the Organized Program To Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure Registry (OPTIMIZE‐HF), the prescription of a ‐blocker at discharge was associated with a significant reduction in 60‐ to 90‐day mortality [hazard ratio (HR): 0.48; 95% CI: 0.30‐0.79], and prescription of an angiotensin‐converting enzyme inhibitor or angiotensin receptor blocker at discharge was associated with a significant reduction in 60‐ to 90‐day mortality and/or rehospitalization (HR: 0.51; 95% CI: 0.34‐0.78).47 In the Cardiac Hospitalization Atherosclerosis Management Program (CHAMP), emphasizing initiation of chronic therapy prior to hospital discharge was associated with 3.0‐fold greater angiotensin‐converting enzyme inhibitor use and 3.2‐fold greater ‐blocker use at 1 year (both P < 0.01).46 Similarly, in patients surviving acute myocardial infarction, the strongest predictor of ‐blocker use at 30 days following discharge was receipt of a ‐blocker prescription at the time of discharge (HR: 15.8; 95% CI: 10.8‐23.3), and this beneficial effect was sustained for up to a year (Figure 2).44 Likewise, in patients with ADHF, the prevalence of ‐blocker therapy at 60 days was significantly increased when this therapy was initiated before discharge (91%) versus after discharge (73%; P < 0.001).45 This predischarge initiation of chronic therapy has been shown to reduce morbidity and mortality.
An awareness of new therapies for ADHF that are in late stages of clinical development can improve understanding of the complex pathophysiology of ADHF and enhance appropriate adaptation of these therapies once they become clinically available. These new therapies represent an attempt to improve on existing therapies, and consequently, they fall into the same 3 general categories as current therapies: diuretics, vasodilators, and inotropic agents.48, 49 Vasopressin receptor antagonists and adenosine receptor antagonists represent an attempt to stimulate aquaresis without inducing hyponatremia, hypokalemia, diminished glomerular filtration, or adverse neurohormonal activation;4854 endothelin receptor antagonists and newer natriuretic peptides represent an attempt to stimulate vasodilation and improve cardiac output without diminishing renal function;49, 55 and myosin activators and sodium‐potassium adenosine triphosphatase inhibitors represent an attempt to enhance contractility without inducing arrhythmogenicity or increasing mortality risk4859 (Table 1).
| Class/MOA | Agent(s) | Advantages/Disadvantages | References |
|---|---|---|---|
| |||
| Vasopressin receptor antagonists | Tolvaptan | Induce aquaresis without natriuresis | deGoma et al.48 |
| Conivaptan | Potentially avoid hyponatremia and hypokalemia | Tang and Hobbs49 | |
| Lixivaptan | Konstam et al.50 | ||
| SR‐121463b | Schrier et al.51 | ||
| Schweiger and Zdanowicz52 | |||
| Adenosine A1 receptor antagonists | Rolofylline | Increase renal blood flow | Tang and Hobbs49 |
| BG‐9719 | Increase intraglomerular hydraulic pressure | deGoma et al.48 | |
| BG‐9928 | May produce diuresis without adversely affecting glomerular filtration and renal function | Givertz et al.53 Greenberg et al.54 | |
| Endothelin receptor antagonists | Tezosentan | Potent vasodilator | Tang and Hobbs49 |
| Improves cardiac output | McMurray et al.55 | ||
| Hemodynamic effects have not translated into an improvement in heart failure symptoms or risk of death. | |||
| Natriuretic peptides | Ularitide | Resists inactivation by neutral endopeptidase | deGoma et al.48 |
| Improves filling pressures and dyspnea scores | Mitrovic et al.59 | ||
| No apparent deleterious effect on short‐term renal function | |||
| Myosin activators | CK‐1827452 | Tries to dissociate inotropy from arrhythmogenicity | deGoma et al.48 |
| Enhances contractility by targeting myocardial myosin, the force generating cardiac enzymes | Cytokinetics56 | ||
| Still very early in clinical development (just entered phase 2) | |||
| Sodium‐potassium ATPase inhibitors | Istaroxime | Tries to dissociate inotropy from arrhythmogenicity | deGoma et al.48 |
| Enhances contractility by stimulating calcium entry into the sarcolemmal Na/Ca exchanger | Blair et al.57 | ||
| Lusitropic | Cleland et al.58 | ||
| Still very early in clinical development (just completed first phase 2 trial) | |||
Finally, although major advancements in the medical therapy of heart failure patients have substantially improved outcomes,60 technological advances in mechanical devices,61 including automatic implantable cardioverter defibrillators, cardiac resynchronization therapy, and ventricular assist devices, as well as advances in the surgical treatment of heart failure,62 have also been used to support the failing heart. Heart failure patients being treated with mechanical devices, as well as those following cardiac transplant, require unique care. As more mechanical and surgical innovations emerge, nonpharmacologic therapy will continue to evolve as a cornerstone of the management strategy in heart failure patients. Hospitalists will need to rely on care pathways, criteria for consultation, and good communication with cardiologists to optimize the care of these patients. Hospitalists should work with their cardiology colleagues in their local institution to develop appropriate criteria for cardiology consultation, and everyone should be educated on these criteria.
The subsequent discussions in this supplement expand on these topics. First, I review the presentation and early recognition, risk stratification, and treatment of patients with ADHF and the role of the hospitalist in this assessment and treatment process. Next, Dr. Khan and Dr. Heywood review the role of diuretics, vasodilators, and ultrafiltration in the management of patients with volume overload and high filling pressures and conclude with a discussion of potential future pharmacologic treatment options, such as tolvaptan and rolofylline, and nonpharmacologic modalities, such as wireless hemodynamic monitoring through implanted devices. Finally, Dr. Michota and I discuss bridging the gap between evidence and practice in the management of patients with ADHF. We review the evidence‐based guidelines that are currently available; discuss the appropriate location for treatment based on the patient's initial history and physical, radiographic, and laboratory findings; provide a practical algorithm for this treatment; and discuss means to transition care from the inpatient setting to the outpatient setting in a manner that enhances compliance with long‐term therapy and reduces recidivism. Given the anticipated growth in ADHF and the need for hospitalists to manage this disease together with cardiologists and others, we believe that the provided information will be helpful in the management of ADHF.
Acute decompensated heart failure (ADHF) is a common disorder that is frequently managed by hospitalists. This management is expected to expand over the next several years because of a continuing increase in the number of ADHF admissions coupled with a plateau or possible decline in the number of practicing cardiologists (Figure 1).114 In addition, 12% of fellowship training positions in cardiology were eliminated between 1995 and 2001, and the fact that the current number of training positions is inadequate to meet future demands is not recognized.15, 16 Given the severity of this disorder, the limited data from randomized, controlled clinical trials,17 and the limitations of current treatment, this management can be both challenging and rewarding. The goal of this special supplement of the Journal of Hospital Medicine is to assist hospitalists in this endeavor by summarizing the currently available data and treatment options and presenting a rational evidence‐based algorithm for the management of ADHF.
A multidisciplinary approach to heart failure has been shown to reduce cost, decrease length of stay, curtail readmissions, and improve compliance.1820 By leading and coordinating teams of physicians, pharmacists, nurses, nutritionists, physical therapists, and case managers and by developing and implementing indications for cardiology consultation, hospitalists can facilitate this multidisciplinary approach.21, 22 However, it is important to remember that hospitalists do not replace cardiologists, who remain a valuable and key component of this multidisciplinary team. Their input is vital in developing care pathways and criteria for consultation, and they, along with primary care physicians, will be the primary source of patient care following hospital discharge. Good communication between hospitalists and cardiologists is essential to optimize the care of patients with ADHF.
Maximizing the efficacy of ADHF care requires a thorough understanding of (1) the causes and potential treatments for the patient's acute decompensation, (2) the management of the patient's chronic heart failure, and (3) potential future therapies. Strategies to improve the continuum of heart failure care have been employed to help improve patient outcomes.23 For example, hospital‐based disease management programs have consistently been shown to optimize care and reduce rehospitalization rates in patients with heart failure.24 These programs involve a multidisciplinary, multifaceted approach to care in order to provide a continuum of care extending from hospitalization and into a patient's home environment.
Because of their practice location and experience, hospitalists are uniquely suited to influence acute inpatient care.25 They see patients in a variety of hospital settings and consequently tend to think of the entire system and not just an isolated component or patient.14 In addition, they have a vested interest in hospital quality improvement measures and are frequently involved in evaluating policies and procedures and developing and implementing clinical pathways, guidelines, and decision‐support tools.26 Data demonstrate that compliance is greater with evidence‐based guidelines and core performance measures when inpatient care is directed by a hospitalist.2730 Improved compliance with selected quality measures in patients with acute myocardial infarction and congestive heart failure has been observed when hospitals implement standardized admission and discharge orders.31, 32
Numerous transitions, such as outpatient to inpatient, intensive care unit to ward, and ward to home, occur during hospitalization, and these transitions are frequently associated with changes in the patient's medication regimen. During an acute illness, chronic medications may be held or discontinued, long‐acting medications may be changed to short‐acting ones to better titrate dose and achieve tighter control, and closed formularies may necessitate substituting 1 medication for another.33 A breakdown in communication during hospitalization‐associated transitions commonly affects medication regimens and can adversely impact patient care.3436 In a prospective evaluation, 53.6% [95% confidence interval (CI): 45.7%61.6%] of patients admitted to the hospital had at least 1 unintended discrepancy between their admission medication orders and their chronic outpatient regimen; 38.6% of these discrepancies were considered a potential threat to the patient.34 Likewise, 49% of patients being discharged from the hospital in another evaluation had an unexplained discrepancy between their preadmission and discharge medications.36 As a result, the Joint Commission on Accreditation of Healthcare Organizations now requires accredited facilities to perform medication reconciliation whenever a patient changes service, setting, provider, or level of care and new medication orders are written.37 This reconciliation is especially important in patients with heart failure, for whom polypharmacy is common and noncompliance with appropriate treatment regimens substantially increases readmission rates.3842
During these transition periods, hospitalists can play an important role in bridging the communication gap and providing this medication reconciliation.33 For example, actively involving hospitalists in all aspects of the reconciliation process at 1 institution resulted in a 4‐fold increase in consistency with preadmission medications.43 Similarly, because of the number of discharge summaries that they write, hospitalists are well suited to lead implementation of new policies and procedures to ensure compliance with recent changes in the Joint Commission on Accreditation of Healthcare Organizations requirements regarding these summaries.
In addition to playing an active role in acute patient management, hospitalists can substantially influence long‐term care and outcomes. Consequently, hospitalists must be well versed in the management of chronic heart failure. Patients are intensely focused on their illness during the hospitalization period, and this focus enhances opportunities for meaningful education and behavior modification. Numerous studies have demonstrated that adherence to long‐term therapy is improved when this therapy is initiated before or at hospital discharge.4446 In an evaluation of data from the Organized Program To Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure Registry (OPTIMIZE‐HF), the prescription of a ‐blocker at discharge was associated with a significant reduction in 60‐ to 90‐day mortality [hazard ratio (HR): 0.48; 95% CI: 0.30‐0.79], and prescription of an angiotensin‐converting enzyme inhibitor or angiotensin receptor blocker at discharge was associated with a significant reduction in 60‐ to 90‐day mortality and/or rehospitalization (HR: 0.51; 95% CI: 0.34‐0.78).47 In the Cardiac Hospitalization Atherosclerosis Management Program (CHAMP), emphasizing initiation of chronic therapy prior to hospital discharge was associated with 3.0‐fold greater angiotensin‐converting enzyme inhibitor use and 3.2‐fold greater ‐blocker use at 1 year (both P < 0.01).46 Similarly, in patients surviving acute myocardial infarction, the strongest predictor of ‐blocker use at 30 days following discharge was receipt of a ‐blocker prescription at the time of discharge (HR: 15.8; 95% CI: 10.8‐23.3), and this beneficial effect was sustained for up to a year (Figure 2).44 Likewise, in patients with ADHF, the prevalence of ‐blocker therapy at 60 days was significantly increased when this therapy was initiated before discharge (91%) versus after discharge (73%; P < 0.001).45 This predischarge initiation of chronic therapy has been shown to reduce morbidity and mortality.
An awareness of new therapies for ADHF that are in late stages of clinical development can improve understanding of the complex pathophysiology of ADHF and enhance appropriate adaptation of these therapies once they become clinically available. These new therapies represent an attempt to improve on existing therapies, and consequently, they fall into the same 3 general categories as current therapies: diuretics, vasodilators, and inotropic agents.48, 49 Vasopressin receptor antagonists and adenosine receptor antagonists represent an attempt to stimulate aquaresis without inducing hyponatremia, hypokalemia, diminished glomerular filtration, or adverse neurohormonal activation;4854 endothelin receptor antagonists and newer natriuretic peptides represent an attempt to stimulate vasodilation and improve cardiac output without diminishing renal function;49, 55 and myosin activators and sodium‐potassium adenosine triphosphatase inhibitors represent an attempt to enhance contractility without inducing arrhythmogenicity or increasing mortality risk4859 (Table 1).
| Class/MOA | Agent(s) | Advantages/Disadvantages | References |
|---|---|---|---|
| |||
| Vasopressin receptor antagonists | Tolvaptan | Induce aquaresis without natriuresis | deGoma et al.48 |
| Conivaptan | Potentially avoid hyponatremia and hypokalemia | Tang and Hobbs49 | |
| Lixivaptan | Konstam et al.50 | ||
| SR‐121463b | Schrier et al.51 | ||
| Schweiger and Zdanowicz52 | |||
| Adenosine A1 receptor antagonists | Rolofylline | Increase renal blood flow | Tang and Hobbs49 |
| BG‐9719 | Increase intraglomerular hydraulic pressure | deGoma et al.48 | |
| BG‐9928 | May produce diuresis without adversely affecting glomerular filtration and renal function | Givertz et al.53 Greenberg et al.54 | |
| Endothelin receptor antagonists | Tezosentan | Potent vasodilator | Tang and Hobbs49 |
| Improves cardiac output | McMurray et al.55 | ||
| Hemodynamic effects have not translated into an improvement in heart failure symptoms or risk of death. | |||
| Natriuretic peptides | Ularitide | Resists inactivation by neutral endopeptidase | deGoma et al.48 |
| Improves filling pressures and dyspnea scores | Mitrovic et al.59 | ||
| No apparent deleterious effect on short‐term renal function | |||
| Myosin activators | CK‐1827452 | Tries to dissociate inotropy from arrhythmogenicity | deGoma et al.48 |
| Enhances contractility by targeting myocardial myosin, the force generating cardiac enzymes | Cytokinetics56 | ||
| Still very early in clinical development (just entered phase 2) | |||
| Sodium‐potassium ATPase inhibitors | Istaroxime | Tries to dissociate inotropy from arrhythmogenicity | deGoma et al.48 |
| Enhances contractility by stimulating calcium entry into the sarcolemmal Na/Ca exchanger | Blair et al.57 | ||
| Lusitropic | Cleland et al.58 | ||
| Still very early in clinical development (just completed first phase 2 trial) | |||
Finally, although major advancements in the medical therapy of heart failure patients have substantially improved outcomes,60 technological advances in mechanical devices,61 including automatic implantable cardioverter defibrillators, cardiac resynchronization therapy, and ventricular assist devices, as well as advances in the surgical treatment of heart failure,62 have also been used to support the failing heart. Heart failure patients being treated with mechanical devices, as well as those following cardiac transplant, require unique care. As more mechanical and surgical innovations emerge, nonpharmacologic therapy will continue to evolve as a cornerstone of the management strategy in heart failure patients. Hospitalists will need to rely on care pathways, criteria for consultation, and good communication with cardiologists to optimize the care of these patients. Hospitalists should work with their cardiology colleagues in their local institution to develop appropriate criteria for cardiology consultation, and everyone should be educated on these criteria.
The subsequent discussions in this supplement expand on these topics. First, I review the presentation and early recognition, risk stratification, and treatment of patients with ADHF and the role of the hospitalist in this assessment and treatment process. Next, Dr. Khan and Dr. Heywood review the role of diuretics, vasodilators, and ultrafiltration in the management of patients with volume overload and high filling pressures and conclude with a discussion of potential future pharmacologic treatment options, such as tolvaptan and rolofylline, and nonpharmacologic modalities, such as wireless hemodynamic monitoring through implanted devices. Finally, Dr. Michota and I discuss bridging the gap between evidence and practice in the management of patients with ADHF. We review the evidence‐based guidelines that are currently available; discuss the appropriate location for treatment based on the patient's initial history and physical, radiographic, and laboratory findings; provide a practical algorithm for this treatment; and discuss means to transition care from the inpatient setting to the outpatient setting in a manner that enhances compliance with long‐term therapy and reduces recidivism. Given the anticipated growth in ADHF and the need for hospitalists to manage this disease together with cardiologists and others, we believe that the provided information will be helpful in the management of ADHF.
- ,.National Hospital Discharge Survey: annual summary, 1996.Vital Health Stat.1999;13(140):1–46.
- ,,,.Hospitalization of patients with heart failure: National Hospital Discharge Survey, 1985 to 1995.Am Heart J.1999;137(2):352–360.
- ,,.National Hospital Discharge Survey: 2001 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2004;13(156):1–198.
- ,,.National Hospital Discharge Survey: 2002 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2005;13(158):1–199.
- ,,.National Hospital Discharge Survey: 2005 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2007;13(165):1–209.
- ,,.National Hospital Discharge Survey: 2004 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2006;13(162):1–209.
- ,,.National Hospital Discharge Survey: 2003 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2006;13(160):1–206.
- Division for Heart Disease and Stroke Prevention. Heart failure fact sheet. Available at: http://www.cdc.gov/dhdsp/library/fs_heart_failure_longdesc.htm. Accessed September2008.
- US Census Bureau. Projected population of the United States, by age and sex: 2000 to 2050. Available at: http://www.census.gov/population/www/projections/usinterimproj/natprojtab02a.pdf. Accessed September2008.
- ,,,.Demographics and cardiology, 1950–2050.J Am Coll Cardiol.2000;35(4):1067–1081.
- 35th Bethesda Conference.Cardiology's workforce crisis: a pragmatic approach. Bethesda, Maryland, 17–18 October 2003.J Am Coll Cardiol.2004;44(2):216–275.
- ,.The evolution of the hospitalist movement in the USA.Clin Med.2002;2(4):327–330.
- .Hospitalists in the United States—mission accomplished or work in progress?N Engl J Med.2004;350(19):1935–1936.
- .Identifying strategies to improve outcomes and reduce costs—a role for the hospitalist.Curr Opin Pulm Med.2004;10(suppl):S19–S22.
- ,.Cardiovascular manpower: the looming crisis.Circulation.2004;109(7):817–820.
- ,.The United States cardiovascular care deficit.Circulation.2004;109(7):821–823.
- Heart Failure Society of America.Evaluation and management of patients with acute decompensated heart failure.J Card Fail.2006;12(1):e86–e103.
- ,,,.Reduction in heart failure events by the addition of a clinical pharmacist to the heart failure management team. Results of the Pharmacist in Heart Failure Assessment Recommendation and Monitoring (PHARM) study.Arch Intern Med.1999;159(16):1939–1945.
- ,,,,.Impact of care at a multidisciplinary congestive heart failure clinic: a randomized trial.CMAJ.2005;173(1):40–45.
- ,.Implementing a congestive heart failure disease management program to decrease length of stay and cost.J Cardiovasc Nurs.1999;14(1):55–74.
- ,,,,.The core competencies in hospital medicine: a framework for curriculum development by the Society of Hospital Medicine.J Hosp Med.2006;1(suppl 1):2–95.
- ,,, et al.ASHP‐SHM joint statement on hospitalist‐pharmacist collaboration.J Hosp Med.2008;3(suppl 3). doi://10.1002/jhm.315. Available at: http://www3.interscience.wiley.com.
- ,,,,,.Heart failure: improving the continuum of care.Care Manag J.2006;7(2):58–63.
- ,,.Strategies to reduce hospitalization in the management of heart failure.Lippincotts Case Manag.2005;10(6 suppl):S1–S15.
- .Improving the management of patients after myocardial infarction, from admission to discharge.Clin Ther.2006;28(10):1509–1539.
- .The role of hospitalists in the management of acute decompensated heart failure.Am Heart Hosp J.2005;3(2):111–117.
- ,,,,.Quality of care for patients hospitalized with heart failure: assessing the impact of hospitalists.Arch Intern Med.2002;162(11):1251–1256.
- ,.Productive interdisciplinary team relationships: the hospitalist and the case manager.Lippincotts Case Manag.2006;11(3):160–164.
- .Use of pay for performance in a community hospital private hospitalist group: a preliminary report.Trans Am Clin Climatol Assoc.2007;118:263–272.
- ,,.Comparison of practice patterns of hospitalists and community physicians in the care of patients with congestive heart failure.J Hosp Med.2008;3(1):35–41.
- ,,,,,.Integrating “best of care” protocols into clinicians' workflow via care provider order entry: impact on quality‐of‐care indicators for acute myocardial infarction.J Am Med Inform Assoc.2006;13(2):188–196.
- ,,, et al.Improved compliance with quality measures at hospital discharge with a computerized physician order entry system.Am Heart J.2006;151(3):643–653.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,, et al.Unintended medication discrepancies at the time of hospital admission.Arch Intern Med.2005;165(4):424–429.
- ,,,,,.Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients.Am J Health Syst Pharm.2004;61(16):1689–1695.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166(5):565–571.
- Joint Commission on Accreditation of Healthcare Organizations. Using medication reconciliation to prevent errors. Sentinel Event Alert #35. Available at: http://www.jointcommission.org/sentinelevents/sentineleventalert/sea_35.htm. Accessed September2008.
- ,,,.Precipitating factors leading to decompensation of heart failure: traits among urban blacks.Arch Intern Med.1988;148(9):2013–2016.
- ,,,,.Early readmission of elderly patients with congestive heart failure.J Am Geriatr Soc.1990;38(12):1290–1295.
- ,.Observation unit management of heart failure.Emerg Med Clin North Am.2001;19(1):209–232.
- ,,, et al.Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Failure National Registry (ADHERE).Am Heart J.2005;149(2):209–216.
- ,,, et al.Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure.JAMA.2006;296(18):2217–2226.
- . Eliminating drug errors: hospitals adopt medication reconciliation to improve patient safety. Available at: http://www.acponline.org/clinical_information/journals_publications/acp_hospitalist/may07/drug_errors.htm. Accessed September2008.
- ,,, et al.Outpatient adherence to beta‐blocker therapy after acute myocardial infarction.JAm Coll Cardiol.2002;40(9):1589–1595.
- ,.Predischarge initiation of carvedilol in patients hospitalized for decompensated heart failure.Am J Cardiol.2004;93(9A):74B–76B.
- ,,,.Improved treatment of coronary heart disease by implementation of a Cardiac Hospitalization Atherosclerosis Management Program (CHAMP).Am J Cardiol.2001;87(7):819–822.
- ,,, et al.Association between performance measures and clinical outcomes for patients hospitalized with heart failure.JAMA.2007;297(1):61–70.
- ,,,.Emerging therapies for the management of decompensated heart failure: from bench to bedside.J Am Coll Cardiol.2006;48(12):2397–2409.
- ,.Novel strategies for the management of acute decompensated heart failure.Curr Cardiol Rev.2005;1(1):1–5.
- ,,, et al.Effects of oral tolvaptan in patients hospitalized for worsening heart failure: the EVEREST outcome trial.JAMA.2007;297(12):1319–1331.
- ,,, et al.Tolvaptan, a selective oral vasopressin V2‐receptor antagonist, for hyponatremia.N Engl J Med.2006;355(20):2099–2112.
- ,.Vasopressin‐receptor antagonists in heart failure.Am J Health Syst Pharm.2008;65(9):807–817.
- ,,,,.The effects of KW‐3902, an adenosine A1‐receptor antagonist, on diuresis and renal function in patients with acute decompensated heart failure and renal impairment or diuretic resistance.J Am Coll Cardiol.2007;50(16):1551–1560.
- ,,, et al.Effects of multiple oral doses of an A1 adenosine antagonist, BG9928, in patients with heart failure: results of a placebo‐controlled, dose‐escalation study.J Am Coll Cardiol.2007;50(7):600–606.
- ,,, et al.Effects of tezosentan on symptoms and clinical outcomes in patients with acute heart failure: the VERITAS randomized controlled trials.JAMA.2007;298(17):2009–2019.
- CK‐1827452. Cytokinetics Web site. Available at: http://www.cytokinetics.com/ck_1827452. Accessed September2008.
- ,,, et al.Rationale and design of the hemodynamic, echocardiographic and neurohormonal effects of istaroxime, a novel intravenous inotropic and lusitropic agent: a randomized controlled trial in patients hospitalized with heart failure (HORIZON‐HF) trial.Am J Ther.2008;15(3):231–240.
- ,,, et al.Clinical trials update from the American College of Cardiology 2008: CARISMA, TRENDS, meta‐analysis of Cox‐2 studies, HAT, ON‐TARGET, HYVET, ACCOMPLISH, MOMENTUM, PROTECT, HORIZON‐HF and REVERSE.Eur J Heart Fail.2008;10(6):614–620.
- ,,, et al.Haemodynamic and clinical effects of ularitide in decompensated heart failure.Eur Heart J.2006;27(23):2823–2832.
- ,,.Mechanical support in acute and chronic heart failure.Curr Cardiol Rep.2008;10(3):168–175.
- ,.Devices in acute heart failure.Crit Care Med.2008;36(1 suppl):S121–S128.
- ,.Advances in the surgical treatment of heart failure.Curr Opin Cardiol.2008;23(3):249–253.
- ,.National Hospital Discharge Survey: annual summary, 1996.Vital Health Stat.1999;13(140):1–46.
- ,,,.Hospitalization of patients with heart failure: National Hospital Discharge Survey, 1985 to 1995.Am Heart J.1999;137(2):352–360.
- ,,.National Hospital Discharge Survey: 2001 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2004;13(156):1–198.
- ,,.National Hospital Discharge Survey: 2002 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2005;13(158):1–199.
- ,,.National Hospital Discharge Survey: 2005 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2007;13(165):1–209.
- ,,.National Hospital Discharge Survey: 2004 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2006;13(162):1–209.
- ,,.National Hospital Discharge Survey: 2003 annual summary with detailed diagnosis and procedure data.Vital Health Stat.2006;13(160):1–206.
- Division for Heart Disease and Stroke Prevention. Heart failure fact sheet. Available at: http://www.cdc.gov/dhdsp/library/fs_heart_failure_longdesc.htm. Accessed September2008.
- US Census Bureau. Projected population of the United States, by age and sex: 2000 to 2050. Available at: http://www.census.gov/population/www/projections/usinterimproj/natprojtab02a.pdf. Accessed September2008.
- ,,,.Demographics and cardiology, 1950–2050.J Am Coll Cardiol.2000;35(4):1067–1081.
- 35th Bethesda Conference.Cardiology's workforce crisis: a pragmatic approach. Bethesda, Maryland, 17–18 October 2003.J Am Coll Cardiol.2004;44(2):216–275.
- ,.The evolution of the hospitalist movement in the USA.Clin Med.2002;2(4):327–330.
- .Hospitalists in the United States—mission accomplished or work in progress?N Engl J Med.2004;350(19):1935–1936.
- .Identifying strategies to improve outcomes and reduce costs—a role for the hospitalist.Curr Opin Pulm Med.2004;10(suppl):S19–S22.
- ,.Cardiovascular manpower: the looming crisis.Circulation.2004;109(7):817–820.
- ,.The United States cardiovascular care deficit.Circulation.2004;109(7):821–823.
- Heart Failure Society of America.Evaluation and management of patients with acute decompensated heart failure.J Card Fail.2006;12(1):e86–e103.
- ,,,.Reduction in heart failure events by the addition of a clinical pharmacist to the heart failure management team. Results of the Pharmacist in Heart Failure Assessment Recommendation and Monitoring (PHARM) study.Arch Intern Med.1999;159(16):1939–1945.
- ,,,,.Impact of care at a multidisciplinary congestive heart failure clinic: a randomized trial.CMAJ.2005;173(1):40–45.
- ,.Implementing a congestive heart failure disease management program to decrease length of stay and cost.J Cardiovasc Nurs.1999;14(1):55–74.
- ,,,,.The core competencies in hospital medicine: a framework for curriculum development by the Society of Hospital Medicine.J Hosp Med.2006;1(suppl 1):2–95.
- ,,, et al.ASHP‐SHM joint statement on hospitalist‐pharmacist collaboration.J Hosp Med.2008;3(suppl 3). doi://10.1002/jhm.315. Available at: http://www3.interscience.wiley.com.
- ,,,,,.Heart failure: improving the continuum of care.Care Manag J.2006;7(2):58–63.
- ,,.Strategies to reduce hospitalization in the management of heart failure.Lippincotts Case Manag.2005;10(6 suppl):S1–S15.
- .Improving the management of patients after myocardial infarction, from admission to discharge.Clin Ther.2006;28(10):1509–1539.
- .The role of hospitalists in the management of acute decompensated heart failure.Am Heart Hosp J.2005;3(2):111–117.
- ,,,,.Quality of care for patients hospitalized with heart failure: assessing the impact of hospitalists.Arch Intern Med.2002;162(11):1251–1256.
- ,.Productive interdisciplinary team relationships: the hospitalist and the case manager.Lippincotts Case Manag.2006;11(3):160–164.
- .Use of pay for performance in a community hospital private hospitalist group: a preliminary report.Trans Am Clin Climatol Assoc.2007;118:263–272.
- ,,.Comparison of practice patterns of hospitalists and community physicians in the care of patients with congestive heart failure.J Hosp Med.2008;3(1):35–41.
- ,,,,,.Integrating “best of care” protocols into clinicians' workflow via care provider order entry: impact on quality‐of‐care indicators for acute myocardial infarction.J Am Med Inform Assoc.2006;13(2):188–196.
- ,,, et al.Improved compliance with quality measures at hospital discharge with a computerized physician order entry system.Am Heart J.2006;151(3):643–653.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- ,,, et al.Unintended medication discrepancies at the time of hospital admission.Arch Intern Med.2005;165(4):424–429.
- ,,,,,.Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients.Am J Health Syst Pharm.2004;61(16):1689–1695.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166(5):565–571.
- Joint Commission on Accreditation of Healthcare Organizations. Using medication reconciliation to prevent errors. Sentinel Event Alert #35. Available at: http://www.jointcommission.org/sentinelevents/sentineleventalert/sea_35.htm. Accessed September2008.
- ,,,.Precipitating factors leading to decompensation of heart failure: traits among urban blacks.Arch Intern Med.1988;148(9):2013–2016.
- ,,,,.Early readmission of elderly patients with congestive heart failure.J Am Geriatr Soc.1990;38(12):1290–1295.
- ,.Observation unit management of heart failure.Emerg Med Clin North Am.2001;19(1):209–232.
- ,,, et al.Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Failure National Registry (ADHERE).Am Heart J.2005;149(2):209–216.
- ,,, et al.Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure.JAMA.2006;296(18):2217–2226.
- . Eliminating drug errors: hospitals adopt medication reconciliation to improve patient safety. Available at: http://www.acponline.org/clinical_information/journals_publications/acp_hospitalist/may07/drug_errors.htm. Accessed September2008.
- ,,, et al.Outpatient adherence to beta‐blocker therapy after acute myocardial infarction.JAm Coll Cardiol.2002;40(9):1589–1595.
- ,.Predischarge initiation of carvedilol in patients hospitalized for decompensated heart failure.Am J Cardiol.2004;93(9A):74B–76B.
- ,,,.Improved treatment of coronary heart disease by implementation of a Cardiac Hospitalization Atherosclerosis Management Program (CHAMP).Am J Cardiol.2001;87(7):819–822.
- ,,, et al.Association between performance measures and clinical outcomes for patients hospitalized with heart failure.JAMA.2007;297(1):61–70.
- ,,,.Emerging therapies for the management of decompensated heart failure: from bench to bedside.J Am Coll Cardiol.2006;48(12):2397–2409.
- ,.Novel strategies for the management of acute decompensated heart failure.Curr Cardiol Rev.2005;1(1):1–5.
- ,,, et al.Effects of oral tolvaptan in patients hospitalized for worsening heart failure: the EVEREST outcome trial.JAMA.2007;297(12):1319–1331.
- ,,, et al.Tolvaptan, a selective oral vasopressin V2‐receptor antagonist, for hyponatremia.N Engl J Med.2006;355(20):2099–2112.
- ,.Vasopressin‐receptor antagonists in heart failure.Am J Health Syst Pharm.2008;65(9):807–817.
- ,,,,.The effects of KW‐3902, an adenosine A1‐receptor antagonist, on diuresis and renal function in patients with acute decompensated heart failure and renal impairment or diuretic resistance.J Am Coll Cardiol.2007;50(16):1551–1560.
- ,,, et al.Effects of multiple oral doses of an A1 adenosine antagonist, BG9928, in patients with heart failure: results of a placebo‐controlled, dose‐escalation study.J Am Coll Cardiol.2007;50(7):600–606.
- ,,, et al.Effects of tezosentan on symptoms and clinical outcomes in patients with acute heart failure: the VERITAS randomized controlled trials.JAMA.2007;298(17):2009–2019.
- CK‐1827452. Cytokinetics Web site. Available at: http://www.cytokinetics.com/ck_1827452. Accessed September2008.
- ,,, et al.Rationale and design of the hemodynamic, echocardiographic and neurohormonal effects of istaroxime, a novel intravenous inotropic and lusitropic agent: a randomized controlled trial in patients hospitalized with heart failure (HORIZON‐HF) trial.Am J Ther.2008;15(3):231–240.
- ,,, et al.Clinical trials update from the American College of Cardiology 2008: CARISMA, TRENDS, meta‐analysis of Cox‐2 studies, HAT, ON‐TARGET, HYVET, ACCOMPLISH, MOMENTUM, PROTECT, HORIZON‐HF and REVERSE.Eur J Heart Fail.2008;10(6):614–620.
- ,,, et al.Haemodynamic and clinical effects of ularitide in decompensated heart failure.Eur Heart J.2006;27(23):2823–2832.
- ,,.Mechanical support in acute and chronic heart failure.Curr Cardiol Rep.2008;10(3):168–175.
- ,.Devices in acute heart failure.Crit Care Med.2008;36(1 suppl):S121–S128.
- ,.Advances in the surgical treatment of heart failure.Curr Opin Cardiol.2008;23(3):249–253.