User login
CE/CME No: CR-1504
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Discuss the likely causes of mumps outbreaks.
• Explain the various possible manifestations of mumps illness.
• Identify the testing methods available to confirm a mumps diagnosis.
• Describe the potential complications of mumps and their incidence.
• Know what to do in the event of a mumps outbreak.
FACULTY
Jo Hanna Friend D’Epiro is a primary care PA in Student Health Services and a doctoral student, Workforce Development and Education, at The Ohio State University in Columbus. The author has no financial relationships to disclose.
ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.0 hour of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid for one year from the issue date of April 2015.
Article begins on next page >>
Although overshadowed in the headlines by a sharp increase in measles cases, mumps too is making a comeback, with outbreaks throughout 2014 and early 2015. Many of today’s clinicians have never seen a case of mumps, let alone experienced an outbreak. Here’s what to look for and what to do if mumps makes its appearance in your practice.
In 2014, 1,151 cases of mumps were reported in the United States.1 By contrast, the typical annual rate has been in the low hundreds since 1989, when the CDC recommended a two-dose measles-mumps-rubella (MMR) vaccination regimen.1,2
Yet mumps has resurged in the past decade, with large outbreaks in 2006 (6,584 cases) and 2009-2010 (4,603 cases).3 Mumps outbreaks tend to occur among vaccinated young adults, such as college students, sports players, and campers, who live in close quarters.4
The 2014 outbreak centered around the Ohio State University campus in Columbus.5 That outbreak was declared over in October, with a total of 484 cases—more than in the entire US in 2013.1 In late 2014, at least 20 players and two officials in the National Hockey League became infected with mumps.6 More recently, Idaho announced that a 21-case outbreak that began at the University of Idaho’s Moscow campus had spread to Washington, with two additional cases reported there.7 What is responsible for these outbreaks, and what can the primary care clinician do to prevent or mitigate them?
EPIDEMIOLOGY
The mumps virus is part of the Rubulavirus genus of the Paramyxoviridae family. It affects the central nervous system (CNS) and glands—most commonly, the parotids. Uniquely human, mumps virus is found in saliva, cerebrospinal fluid, blood, breast milk, infected tissues, and urine.8,9 It is transmitted through contact with respiratory secretions and/or saliva, direct contact, or through fomites (eg, bedding, doorknobs).10
Before development of an effective vaccine, mumps was a universal childhood disease in the US; by age 14, most children had been infected.11 In the absence of widespread vaccination, mumps epidemics will occur every three to five years—as they still do in parts of the world without effective vaccination programs.12
As a result of widespread vaccination in the US, mumps incidence declined from 152,209 cases in 1967 to 2,982 cases in 1985 (see “Mumps and the MMR Vaccine”). Cases were reduced even further when administration of a second MMR dose was introduced in 1990.13 By 2000, the Healthy People 2010 goal was to eliminate mumps altogether.14
Continue for patient presentation >>
PATIENT PRESENTATION
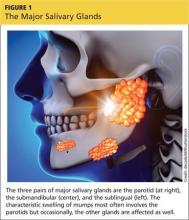
Parotitis is the classic (but not universal) physical exam finding in mumps. Parotid gland inflammation causes generalized swelling anterior to the ear and inferior to the mastoid process, with jaw angle obliteration (see Figure 1).9 If only one parotid gland is involved, the patient’s face appears asymmetric. Other significant exam findings may include fever and erythematous swelling of the Stensen (parotid) duct.10
Nonspecific symptoms—including respiratory symptoms, myalgia, anorexia, malaise, headache, and low-grade fever—may occur in more than 50% of cases.8 CNS involvement may cause nuchal rigidity (stiff neck). In postpubertal males, testicular swelling and/or induration, pain, tenderness, and enlarged inguinal lymph nodes may be present.
Mumps can be challenging to diagnose based on clinical presentation alone; for example, parotitis occurs in only 30% to 40% of cases.8 Other viruses, such as parainfluenza virus 1 and 3, coxsackievirus, adenovirus, influenza A, cytomegalovirus, and HIV, can also cause swelling of the parotid glands, but mumps is the only virus known to cause parotitis on an epidemic scale.4 Furthermore, up to 20% of cases may be asymptomatic.8,11 Because mumps is highly contagious, a history of exposure to an affected individual is a compelling factor in making the diagnosis.
The incubation period for mumps is 12 to 25 days, with parotitis usually developing 16 to 18 days after exposure.4 This relatively lengthy incubation period increases the likelihood of viral spread. The virus is contagious from three days prior to symptom onset to day 4 of active disease.8 To prevent disease transmission, it is recommended that individuals remain isolated from others until five days after the onset of salivary gland swelling.4
Next page: Laboratory confirmation >>
LABORATORY CONFIRMATION
The CDC recommends determination of any one of the following to help confirm the diagnosis of acute mumps infection.
• Presence of serum mumps IgM antibodies
• Significant rise in IgG antibody titer between the acute and convalescent-phase serum specimens
• IgG seroconversion
• Positive mumps virus culture
• Detection of virus by real-time reverse transcriptase polymerase chain reaction (RT-PCR)4
Antibody testing
At the initial visit, a serum specimen should be obtained to test for mumps IgM antibodies.4 The CDC recommends enzyme immunoassay (EIA) testing for IgM antibodies to confirm acute mumps infection.4
IgM antibodies are detectable five days after onset of symptoms and, after reaching a maximum level, remain elevated for several weeks. If the initial IgM test is negative, the test can be repeated in five to seven days.4
Either EIA or immunofluorescence antibody assay (IFA) testing for mumps IgG antibodies should be performed on both acute- and convalescent-phase serum samples. Laboratory confirmation requires a fourfold rise in the antibody titer using a quantitative assay4 or seroconversion from negative to positive.
Virus detection
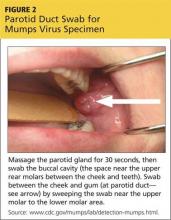
If possible, mumps virus samples should be obtained no more than three to eight days after symptom onset because delay may result in a low viral yield.4 The best viral samples are obtained via parotid duct swabs (see Figure 2). Before swabbing the buccal cavity, the parotid gland should be massaged for 30 seconds to ensure that the specimen contains gland secretions.4
Mumps virus can be detected by RT-PCR or culture. The RT-PCR is currently the most sensitive test for mumps, but most RT-PCR testing is done by public health laboratories and the CDC, and results may not be available until after the illness has resolved.4
Laboratory tests, however, are not always helpful in confirming a clinical diagnosis of mumps. Vaccinated persons may not mount a secondary immune response to mumps and consequently may not have a significant IgM response. It is also possible that a high level of IgG antibodies will cause a false-positive IgM test results.4
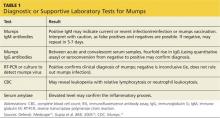
Other laboratory tests that may support a diagnosis of mumps include a complete blood cell count, which may reveal a leukopenia with relative lymphocytosis or neutrophil leukocytosis,16 and a measurement of serum amylase level which, if elevated, may confirm the inflammatory process.10 See Table 1 for a summary of tests that confirm or support a mumps diagnosis.
Mumps is a reportable illness, and the local health department should be contacted for assistance with determining where and how to ship specimens.17 However, in the absence of laboratory confirmation, only clinical cases with parotitis, other salivary gland involvement, or mumps-related complications are notifiable.11
Continue for mumps manifestations >>
MUMPS MANIFESTATIONS
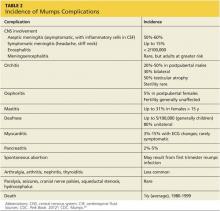
The continuum of mumps illness ranges from asymptomatic infection to parotitis (the most well-known manifestation) to rare but severe complications.8 Table 2 lists potential complications of mumps in order of frequency. Complications vary by age and sex but tend to occur more often in adults.4,11
Immunization modifies the clinical presentation of mumps11 and likely decreases complications. Although one analysis of the 2006 outbreak identified no difference in complication rates between vaccinated and unvaccinated patients, the authors attributed this to misclassification of patients’ vaccination status; they did find lower reported rates of mumps complications compared with complication rates before widespread vaccination.13 A study of the 2009-2010 outbreak found that complication rates were lower among vaccinated patients.18
RISK FACTORS FOR OUTBREAKS
Of the three components of the MMR vaccine, the least effective is the mumps portion. One dose confers 78% immunity and two doses, 88%, which the CDC characterizes as incomplete protection.1 Compare this to the measles vaccine, which is 97% effective with two doses,19 and the rubella vaccine, which is 97% effective after a single dose in conferring immunity.11
In 2000, as a result of high rates of vaccination, the US determined that endemic measles had been eliminated. A similar conclusion was reached about rubella in 2004, and both determinations were reaffirmed in 2011.20 In contrast, mumps has never been eliminated.1
Waning immunity
While antibodies to mumps as a result of vaccination persist into adulthood, they decline over time. A 2009 CDC study found that, 12 years after a second MMR dose, mumps antibody levels in adolescents and young adults had declined to levels similar to those measured before the second dose.21 Other analyses of major outbreaks suggested the need for further studies to determine optimal timing for the second MMR dose (eg, at a later age) or if a third dose would provide longer-lasting immunity.13,22 Waning immunity among young adults, coupled with high-density living environments that intensify exposure to the virus, increase risk for the disease.23
Further complicating the situation is the lack of evidence about the required level of antibodies needed to confer protection against mumps infection.17 To date, the antibody titer threshold of mumps-specific IgG at which an individual is protected from the disease is unknown.11,17
Imported risks
Mumps remains endemic in many parts of the world, with vaccination employed in only 61% of countries belonging to the World Health Organization.4 Several recent outbreaks were traced to index cases originating outside the US.13 It is likely that importation of the virus from abroad will continue.
Next page: Outbreak management >>
OUTBREAK MANAGEMENT
A mumps outbreak is defined as three or more cases linked by time and place.4 The keys to managing an outbreak are to define the population(s) at risk and their transmission setting(s) and to rapidly identify and vaccinate vulnerable individuals without evidence of immunity.4
Presumptive evidence of mumps immunity includes11
• Documentation of vaccination with two doses of live mumps virus–containing vaccine
• Laboratory evidence of immunity
• Laboratory confirmation of disease
• Birth year before 1957.
Documentation of two doses of MMR constitutes evidence of adequate vaccination for school-age children and adolescents and for young adults attending postsecondary institutions. During an outbreak, susceptible (ie, unvaccinated) students should be excluded from attendance until they have been vaccinated; those with one dose may attend but should receive the second dose.4 Those declining vaccination for medical, religious, or other reasons should be excluded until at least 26 days after the onset of parotitis in the last person with mumps at the institution.24
If the outbreak threatens the wider community (eg, preschool-age children and adults), a second MMR dose should be considered for children ages 1 to 4 or for adults who have received one MMR dose. Similarly, MMR vaccination should be considered for adults born before 1957 who have no other evidence of immunity and are at risk for exposure to the virus.11
In the workplace, health care workers’ (HCWs’) immunity status should be known, documented, and accessible in advance of an outbreak.11 If an HCW without evidence of immunity is exposed to mumps, he or she should be excluded from patient care from the time of first unprotected exposure through the 25th day after the last exposure.25 Although individuals born before 1957 are generally considered immune, if a nosocomial mumps outbreak occurs, the two-dose MMR regimen should be administered to these HCW as well.4
In 1991, the US military began to immunize recruits routinely with MMR, regardless of their immunization status.26 During the 2006 mumps outbreak, the incidence of mumps among military personnel was minimal compared to that among their civilian counterparts—perhaps due to administration of a third MMR dose to an unknown number of recruits.22
CDC researchers studied the impact of a third MMR dose for mumps outbreak control in 2012 and concluded that, while a third dose may help control outbreaks among populations with preexisting high two-dose vaccine coverage, further study is needed.27
Although insufficient data exist on which to base a recommendation for or against a third MMR dose for mumps outbreak control, the CDC has issued guidance for public health departments for targeted administration during outbreaks. Considerations include
• Intense exposure settings
• High two-dose vaccination coverage (ie, > 90%)
• High attack rates (> 5 cases per 1,000 population)
• Evidence of ongoing transmission for at least two weeks in the target population.4
TREATMENT
There is no specific treatment for mumps. Care is supportive and in the outpatient setting includes rest, cold or heat to the affected areas, and OTC pain relievers. Ice can be used to help relieve the pain of orchitis. Acidic foods may stimulate the parotid glands, causing pain and difficulty swallowing, and should be avoided.
Isolation of infectious patients is vital to preventing the spread of mumps.4 In the clinician’s office, a separate waiting area should be used for a potential mumps patient, or the patient should be located at least three feet from other patients and asked to wear a surgical mask. HCW working with potential mumps patients should follow droplet precautions (eg, wear personal protective equipment) in addition to standard precautions and should be hypervigilant about hand washing.24
CONCLUSION
Mumps is a usually benign, self-limited infectious disease that can potentially result in serious complications. It is also prone to periodic outbreaks. Control of mumps can best be accomplished by remembering these five “Ps”:
• Prevention—through widespread two-dose MMR vaccination
• Parotitis—recognize it as the primary symptom of mumps and make the diagnosis in a timely manner
• Persistence—in making the diagnosis clinically and in weighing laboratory results within the context of clinical disease
• Personal protective equipment—use it consistently in the health care setting or as needed in the home
• Protection—isolate patients with mumps to avoid spreading the disease
1. CDC. Mumps cases and outbreaks. www.cdc.gov/mumps/outbreaks.html. Accessed March 19, 2015.
2. CDC. Measles prevention: recommendations of the Immunization Practices Advisory Committee (ACIP). MMWR Morb Mortal Wkly Rep. 1989;38(suppl 9):1-18.
3. CDC. Summary of notifiable diseases—United States. 1993-2012. MMWR Morb Mortal Wkly Rep. www.cdc.gov/mmwr/mmwr_nd/index.html. Accessed March 19, 2015.
4. CDC. Mumps, chap 9. In: Manual for the Surveillance of Vaccine-Preventable Diseases. August 2012. www.cdc.gov/vaccines/pubs/surv-manual/chpt09-mumps.html. Accessed March 19, 2015.
5. Pyle E. Central Ohio mumps outbreak finally loses steam. The Columbus Dispatch. October 11, 2014. www.dispatch.com/content/stories/local/2014/10/10/Health-officials-declare-mumps-outbreak-over.html. Accessed March 19, 2015.
6. Hascup J. Three more mumps cases: Penguins’ Steve Downie, Thomas Greiss, Devils’ Patrik Elias, Michael Ryder. USA TODAY. December 27, 2014. www.usatoday.com/story/sports/nhl/2014/12/26/steve-downie-thomas-greiss-mumps-pittsburgh-penguins/20911031/. Accessed March 19, 2015.
7. Idaho public health officials warn that mumps outbreak involving University students has spread to Boise and State of Washington [news release]. Boise, ID: Idaho Department of Health and Welfare Public Information Office; February 6, 2015. www.healthandwelfare.idaho.gov/AboutUs/Newsroom/tabid/130/ctl/ArticleView/mid/3061/articleId/1819/Idaho-Public-Health-Officials-Warn-that-Mumps-Outbreak-Involving-University-Students-Has-Spread-to-Boise-and-State-of-Washington.aspx. Accessed March 19, 2015.
8. CDC. Epidemiology and prevention of vaccine-preventable diseases. Mumps, chap 12. In: The Pink Book: Course Textbook. 12th ed, 2012. www.cdc.gov/vaccines/pubs/pinkbook/mumps.html. Accessed March 19, 2015.
9. Albrecht MA. Epidemiology, clinical manifestations, diagnosis, and management of mumps. www.uptodate.com/contents/epidemiology-clin ical-manifestations-diagnosis-and-management-of-mumps. Accessed March 19, 2015.
10. Defendi GL. Mumps. http://reference.medscape.com/article/966678-overview. Accessed March 19, 2015.
11. CDC. Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2013;62(RR04):1-34.
12. Rubin S, Carbone KM. Mumps. In: Longo DL, Fauci AS, Kasper DL et al, eds. Harrison’s Principles of Internal Medicine. 18th ed. New York, NY: The McGraw-Hill Companies, Inc.; 2012:chap 194.
13. Dayan G, Quinlisk M, Parker A, et al. Recent resurgence of mumps in the United States. New Engl J Med. 2008;358:1580-1589.
14. US Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2010: Objectives for Improving Health. www.healthypeople.gov/2010/Document/HTML/Volume1 /14Immunization.htm#_Toc494510239. Accessed March 19, 2015.
15. CDC. Measles, mumps, and rubella: vaccine use and strategies for elimination of measles, rubella, and congenital rubella syndrome and control of mumps: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 1998;47(RR-8):1-57.
16. Gupta RK, Best J, MacMahon E. Mumps and the UK epidemic 2005. BMJ. 2005;(330):1132-1135.
17. CDC. Laboratory testing for mumps infection. www.cdc.gov/mumps/lab/qa-lab-test-infect.html. Accessed March 19, 2015.
18. Barskey AE, Schulte C, Rosen JB, et al. Mumps outbreak in Orthodox Jewish communities in the United States. New Engl J Med. 2012;367(18): 1704-1713.
19. CDC. Frequently asked questions about measles in the U.S. www.cdc.gov/measles/about/faqs.html. Accessed March 19, 2015.
20. Papania MJ, Wallace GS, Rota PA, et al. Elimination of endemic measles, rubella, and congenital rubella syndrome from the Western hemisphere: the US experience. JAMA Pediatr. 2014;168(2):148-155.
21. LeBaron CW, Forghani B, Beck C, et al. Persistence of mumps antibodies after 2 doses of measles-mumps-rubella vaccine. J Infect Dis. 2009; 199(4):552-560.
22. Anis E, Grotto I, Moerman L, et al. Mumps outbreak in Israel’s highly vaccinated society: are two doses enough? Epidemiol Infect. 2012; 140:439-446.
23. Sane J, Gouma S, Koopmans M, et al. Epidemic of mumps among vaccinated persons, The Netherlands, 2009-2012. Emerg Infect Dis. 2014;20(4):643-648.
24. CDC. Exposure and response. www.cdc.gov/mumps/clinical/qa-exposure-response.html. Accessed March 19, 2015.
25. CDC. Mumps prevention and control in healthcare settings. www.cdc.gov/mumps/prev-control-settings/background.html. Accessed March 19, 2015.
26. Barskey AE, Glasser JW, LeBaron CW. Mumps resurgence in the United States: a historical perspective on unexpected elements. Vaccine. 2009;27:6186-6195.
27. Ogbuanu IU, Kutty PK, Hudson JM, et al. Impact of a third dose of measles-mumps-rubella vaccine on a mumps outbreak. Pediatrics. 2012;130:e1567-e1574.
28. CDC. Physical findings and complications. www.cdc.gov/mumps/clinical/qa-physical-complic.html. Accessed March 19, 2015.
29. Conniff R. A forgotten pioneer of vaccines. The New York Times. May 6, 2013. www.nytimes.com/2013/05/07/health/maurice-hilleman-mmr-vaccines-forgotten-hero.html?_r=0. Accessed March 19, 2015.
30. CDC. MMR vaccine for mumps. www.cdc.gov/vaccines/vpd-vac/mumps/vac-faqs-tech.htm. Accessed March 19, 2015.
31. The College of Physicians of Philadelphia. The history of vaccines. www.historyofvaccines.org/content/timelines/all. Accessed March 19, 2015.
32. CDC. Travelers’ health. Mumps. wwwnc.cdc.gov/travel/diseases/mumps. Accessed March 19, 2015.
33. Wakefield AJ, Murch SH, Anthony A, et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children [retracted in Lancet. 2010;375:445]. Lancet. 1998;351:637-641.
34. Murch SH, Anthony A, Casson DH, et al. Retraction of an interpretation. Lancet. 2004;363(9411):750.
35. Deer B. How the case against the MMR vaccine was fixed. BMJ. 2011;342:1-16.
36. The Editors of The Lancet. Notice of retraction of "Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children" [retraction of: Wakefield AJ, Murch SH, Anthony A, et al. In: Lancet. 1998;351:637-641]. Lancet. 2010;375:445.
37. Whalen J. UK bans doctor who linked autism to vaccine. The Wall Street Journal. May 24, 2010. www.wsj.com/articles/SB10001424052748704113504575263994195318772. Accessed March 19, 2015.
38. CDC. Vaccine safety: measles, mumps and rubella (MMR) vaccine. www.cdc.gov/vaccinesafety/vaccines/mmr/mmr.html. Accessed March 19, 2015.
39. Madsen KM, Hviid A, Vestergaard M, et al. A population-based study of measles, mumps, and rubella vaccination and autism. N Engl J Med. 2002;347:1477-1482.
40. DeStefano F, Bhasin TK, Thompson WW, et al. Age at first measles-mumps-rubella vaccination in children with autism and school-matched control subjects: a population-based study in metropolitan Atlanta. Pediatrics. 2004;113(2):259-266.
41. Richler J, Luyster R. Risi S, et al. Is there a ‘regressive phenotype’ of autism spectrum disorder associated with the measles-mumps-rubella vaccine? A CPEA study. J Autism Dev Disord. 2006;36(3):299-316.
42. Nyhan B, Reifler J, Richey S, Freed G. Effective messages in vaccine promotion: a randomized trial. Pediatrics. 2014:133:1-8.
43. Haberman C. A discredited vaccine study’s continuing impact on public health. The New York Times. February 1, 2015. www.nytimes.com/2015/02/02/us/a-discredited-vaccine-studys-continuing-impact- on-public- health.html?_r=0. Accessed March 19, 2015.
CE/CME No: CR-1504
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Discuss the likely causes of mumps outbreaks.
• Explain the various possible manifestations of mumps illness.
• Identify the testing methods available to confirm a mumps diagnosis.
• Describe the potential complications of mumps and their incidence.
• Know what to do in the event of a mumps outbreak.
FACULTY
Jo Hanna Friend D’Epiro is a primary care PA in Student Health Services and a doctoral student, Workforce Development and Education, at The Ohio State University in Columbus. The author has no financial relationships to disclose.
ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.0 hour of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid for one year from the issue date of April 2015.
Article begins on next page >>
Although overshadowed in the headlines by a sharp increase in measles cases, mumps too is making a comeback, with outbreaks throughout 2014 and early 2015. Many of today’s clinicians have never seen a case of mumps, let alone experienced an outbreak. Here’s what to look for and what to do if mumps makes its appearance in your practice.
In 2014, 1,151 cases of mumps were reported in the United States.1 By contrast, the typical annual rate has been in the low hundreds since 1989, when the CDC recommended a two-dose measles-mumps-rubella (MMR) vaccination regimen.1,2
Yet mumps has resurged in the past decade, with large outbreaks in 2006 (6,584 cases) and 2009-2010 (4,603 cases).3 Mumps outbreaks tend to occur among vaccinated young adults, such as college students, sports players, and campers, who live in close quarters.4
The 2014 outbreak centered around the Ohio State University campus in Columbus.5 That outbreak was declared over in October, with a total of 484 cases—more than in the entire US in 2013.1 In late 2014, at least 20 players and two officials in the National Hockey League became infected with mumps.6 More recently, Idaho announced that a 21-case outbreak that began at the University of Idaho’s Moscow campus had spread to Washington, with two additional cases reported there.7 What is responsible for these outbreaks, and what can the primary care clinician do to prevent or mitigate them?
EPIDEMIOLOGY
The mumps virus is part of the Rubulavirus genus of the Paramyxoviridae family. It affects the central nervous system (CNS) and glands—most commonly, the parotids. Uniquely human, mumps virus is found in saliva, cerebrospinal fluid, blood, breast milk, infected tissues, and urine.8,9 It is transmitted through contact with respiratory secretions and/or saliva, direct contact, or through fomites (eg, bedding, doorknobs).10
Before development of an effective vaccine, mumps was a universal childhood disease in the US; by age 14, most children had been infected.11 In the absence of widespread vaccination, mumps epidemics will occur every three to five years—as they still do in parts of the world without effective vaccination programs.12
As a result of widespread vaccination in the US, mumps incidence declined from 152,209 cases in 1967 to 2,982 cases in 1985 (see “Mumps and the MMR Vaccine”). Cases were reduced even further when administration of a second MMR dose was introduced in 1990.13 By 2000, the Healthy People 2010 goal was to eliminate mumps altogether.14
Continue for patient presentation >>
PATIENT PRESENTATION
Parotitis is the classic (but not universal) physical exam finding in mumps. Parotid gland inflammation causes generalized swelling anterior to the ear and inferior to the mastoid process, with jaw angle obliteration (see Figure 1).9 If only one parotid gland is involved, the patient’s face appears asymmetric. Other significant exam findings may include fever and erythematous swelling of the Stensen (parotid) duct.10
Nonspecific symptoms—including respiratory symptoms, myalgia, anorexia, malaise, headache, and low-grade fever—may occur in more than 50% of cases.8 CNS involvement may cause nuchal rigidity (stiff neck). In postpubertal males, testicular swelling and/or induration, pain, tenderness, and enlarged inguinal lymph nodes may be present.
Mumps can be challenging to diagnose based on clinical presentation alone; for example, parotitis occurs in only 30% to 40% of cases.8 Other viruses, such as parainfluenza virus 1 and 3, coxsackievirus, adenovirus, influenza A, cytomegalovirus, and HIV, can also cause swelling of the parotid glands, but mumps is the only virus known to cause parotitis on an epidemic scale.4 Furthermore, up to 20% of cases may be asymptomatic.8,11 Because mumps is highly contagious, a history of exposure to an affected individual is a compelling factor in making the diagnosis.
The incubation period for mumps is 12 to 25 days, with parotitis usually developing 16 to 18 days after exposure.4 This relatively lengthy incubation period increases the likelihood of viral spread. The virus is contagious from three days prior to symptom onset to day 4 of active disease.8 To prevent disease transmission, it is recommended that individuals remain isolated from others until five days after the onset of salivary gland swelling.4
Next page: Laboratory confirmation >>
LABORATORY CONFIRMATION
The CDC recommends determination of any one of the following to help confirm the diagnosis of acute mumps infection.
• Presence of serum mumps IgM antibodies
• Significant rise in IgG antibody titer between the acute and convalescent-phase serum specimens
• IgG seroconversion
• Positive mumps virus culture
• Detection of virus by real-time reverse transcriptase polymerase chain reaction (RT-PCR)4
Antibody testing
At the initial visit, a serum specimen should be obtained to test for mumps IgM antibodies.4 The CDC recommends enzyme immunoassay (EIA) testing for IgM antibodies to confirm acute mumps infection.4
IgM antibodies are detectable five days after onset of symptoms and, after reaching a maximum level, remain elevated for several weeks. If the initial IgM test is negative, the test can be repeated in five to seven days.4
Either EIA or immunofluorescence antibody assay (IFA) testing for mumps IgG antibodies should be performed on both acute- and convalescent-phase serum samples. Laboratory confirmation requires a fourfold rise in the antibody titer using a quantitative assay4 or seroconversion from negative to positive.
Virus detection
If possible, mumps virus samples should be obtained no more than three to eight days after symptom onset because delay may result in a low viral yield.4 The best viral samples are obtained via parotid duct swabs (see Figure 2). Before swabbing the buccal cavity, the parotid gland should be massaged for 30 seconds to ensure that the specimen contains gland secretions.4
Mumps virus can be detected by RT-PCR or culture. The RT-PCR is currently the most sensitive test for mumps, but most RT-PCR testing is done by public health laboratories and the CDC, and results may not be available until after the illness has resolved.4
Laboratory tests, however, are not always helpful in confirming a clinical diagnosis of mumps. Vaccinated persons may not mount a secondary immune response to mumps and consequently may not have a significant IgM response. It is also possible that a high level of IgG antibodies will cause a false-positive IgM test results.4
Other laboratory tests that may support a diagnosis of mumps include a complete blood cell count, which may reveal a leukopenia with relative lymphocytosis or neutrophil leukocytosis,16 and a measurement of serum amylase level which, if elevated, may confirm the inflammatory process.10 See Table 1 for a summary of tests that confirm or support a mumps diagnosis.
Mumps is a reportable illness, and the local health department should be contacted for assistance with determining where and how to ship specimens.17 However, in the absence of laboratory confirmation, only clinical cases with parotitis, other salivary gland involvement, or mumps-related complications are notifiable.11
Continue for mumps manifestations >>
MUMPS MANIFESTATIONS
The continuum of mumps illness ranges from asymptomatic infection to parotitis (the most well-known manifestation) to rare but severe complications.8 Table 2 lists potential complications of mumps in order of frequency. Complications vary by age and sex but tend to occur more often in adults.4,11
Immunization modifies the clinical presentation of mumps11 and likely decreases complications. Although one analysis of the 2006 outbreak identified no difference in complication rates between vaccinated and unvaccinated patients, the authors attributed this to misclassification of patients’ vaccination status; they did find lower reported rates of mumps complications compared with complication rates before widespread vaccination.13 A study of the 2009-2010 outbreak found that complication rates were lower among vaccinated patients.18
RISK FACTORS FOR OUTBREAKS
Of the three components of the MMR vaccine, the least effective is the mumps portion. One dose confers 78% immunity and two doses, 88%, which the CDC characterizes as incomplete protection.1 Compare this to the measles vaccine, which is 97% effective with two doses,19 and the rubella vaccine, which is 97% effective after a single dose in conferring immunity.11
In 2000, as a result of high rates of vaccination, the US determined that endemic measles had been eliminated. A similar conclusion was reached about rubella in 2004, and both determinations were reaffirmed in 2011.20 In contrast, mumps has never been eliminated.1
Waning immunity
While antibodies to mumps as a result of vaccination persist into adulthood, they decline over time. A 2009 CDC study found that, 12 years after a second MMR dose, mumps antibody levels in adolescents and young adults had declined to levels similar to those measured before the second dose.21 Other analyses of major outbreaks suggested the need for further studies to determine optimal timing for the second MMR dose (eg, at a later age) or if a third dose would provide longer-lasting immunity.13,22 Waning immunity among young adults, coupled with high-density living environments that intensify exposure to the virus, increase risk for the disease.23
Further complicating the situation is the lack of evidence about the required level of antibodies needed to confer protection against mumps infection.17 To date, the antibody titer threshold of mumps-specific IgG at which an individual is protected from the disease is unknown.11,17
Imported risks
Mumps remains endemic in many parts of the world, with vaccination employed in only 61% of countries belonging to the World Health Organization.4 Several recent outbreaks were traced to index cases originating outside the US.13 It is likely that importation of the virus from abroad will continue.
Next page: Outbreak management >>
OUTBREAK MANAGEMENT
A mumps outbreak is defined as three or more cases linked by time and place.4 The keys to managing an outbreak are to define the population(s) at risk and their transmission setting(s) and to rapidly identify and vaccinate vulnerable individuals without evidence of immunity.4
Presumptive evidence of mumps immunity includes11
• Documentation of vaccination with two doses of live mumps virus–containing vaccine
• Laboratory evidence of immunity
• Laboratory confirmation of disease
• Birth year before 1957.
Documentation of two doses of MMR constitutes evidence of adequate vaccination for school-age children and adolescents and for young adults attending postsecondary institutions. During an outbreak, susceptible (ie, unvaccinated) students should be excluded from attendance until they have been vaccinated; those with one dose may attend but should receive the second dose.4 Those declining vaccination for medical, religious, or other reasons should be excluded until at least 26 days after the onset of parotitis in the last person with mumps at the institution.24
If the outbreak threatens the wider community (eg, preschool-age children and adults), a second MMR dose should be considered for children ages 1 to 4 or for adults who have received one MMR dose. Similarly, MMR vaccination should be considered for adults born before 1957 who have no other evidence of immunity and are at risk for exposure to the virus.11
In the workplace, health care workers’ (HCWs’) immunity status should be known, documented, and accessible in advance of an outbreak.11 If an HCW without evidence of immunity is exposed to mumps, he or she should be excluded from patient care from the time of first unprotected exposure through the 25th day after the last exposure.25 Although individuals born before 1957 are generally considered immune, if a nosocomial mumps outbreak occurs, the two-dose MMR regimen should be administered to these HCW as well.4
In 1991, the US military began to immunize recruits routinely with MMR, regardless of their immunization status.26 During the 2006 mumps outbreak, the incidence of mumps among military personnel was minimal compared to that among their civilian counterparts—perhaps due to administration of a third MMR dose to an unknown number of recruits.22
CDC researchers studied the impact of a third MMR dose for mumps outbreak control in 2012 and concluded that, while a third dose may help control outbreaks among populations with preexisting high two-dose vaccine coverage, further study is needed.27
Although insufficient data exist on which to base a recommendation for or against a third MMR dose for mumps outbreak control, the CDC has issued guidance for public health departments for targeted administration during outbreaks. Considerations include
• Intense exposure settings
• High two-dose vaccination coverage (ie, > 90%)
• High attack rates (> 5 cases per 1,000 population)
• Evidence of ongoing transmission for at least two weeks in the target population.4
TREATMENT
There is no specific treatment for mumps. Care is supportive and in the outpatient setting includes rest, cold or heat to the affected areas, and OTC pain relievers. Ice can be used to help relieve the pain of orchitis. Acidic foods may stimulate the parotid glands, causing pain and difficulty swallowing, and should be avoided.
Isolation of infectious patients is vital to preventing the spread of mumps.4 In the clinician’s office, a separate waiting area should be used for a potential mumps patient, or the patient should be located at least three feet from other patients and asked to wear a surgical mask. HCW working with potential mumps patients should follow droplet precautions (eg, wear personal protective equipment) in addition to standard precautions and should be hypervigilant about hand washing.24
CONCLUSION
Mumps is a usually benign, self-limited infectious disease that can potentially result in serious complications. It is also prone to periodic outbreaks. Control of mumps can best be accomplished by remembering these five “Ps”:
• Prevention—through widespread two-dose MMR vaccination
• Parotitis—recognize it as the primary symptom of mumps and make the diagnosis in a timely manner
• Persistence—in making the diagnosis clinically and in weighing laboratory results within the context of clinical disease
• Personal protective equipment—use it consistently in the health care setting or as needed in the home
• Protection—isolate patients with mumps to avoid spreading the disease
CE/CME No: CR-1504
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Discuss the likely causes of mumps outbreaks.
• Explain the various possible manifestations of mumps illness.
• Identify the testing methods available to confirm a mumps diagnosis.
• Describe the potential complications of mumps and their incidence.
• Know what to do in the event of a mumps outbreak.
FACULTY
Jo Hanna Friend D’Epiro is a primary care PA in Student Health Services and a doctoral student, Workforce Development and Education, at The Ohio State University in Columbus. The author has no financial relationships to disclose.
ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.0 hour of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid for one year from the issue date of April 2015.
Article begins on next page >>
Although overshadowed in the headlines by a sharp increase in measles cases, mumps too is making a comeback, with outbreaks throughout 2014 and early 2015. Many of today’s clinicians have never seen a case of mumps, let alone experienced an outbreak. Here’s what to look for and what to do if mumps makes its appearance in your practice.
In 2014, 1,151 cases of mumps were reported in the United States.1 By contrast, the typical annual rate has been in the low hundreds since 1989, when the CDC recommended a two-dose measles-mumps-rubella (MMR) vaccination regimen.1,2
Yet mumps has resurged in the past decade, with large outbreaks in 2006 (6,584 cases) and 2009-2010 (4,603 cases).3 Mumps outbreaks tend to occur among vaccinated young adults, such as college students, sports players, and campers, who live in close quarters.4
The 2014 outbreak centered around the Ohio State University campus in Columbus.5 That outbreak was declared over in October, with a total of 484 cases—more than in the entire US in 2013.1 In late 2014, at least 20 players and two officials in the National Hockey League became infected with mumps.6 More recently, Idaho announced that a 21-case outbreak that began at the University of Idaho’s Moscow campus had spread to Washington, with two additional cases reported there.7 What is responsible for these outbreaks, and what can the primary care clinician do to prevent or mitigate them?
EPIDEMIOLOGY
The mumps virus is part of the Rubulavirus genus of the Paramyxoviridae family. It affects the central nervous system (CNS) and glands—most commonly, the parotids. Uniquely human, mumps virus is found in saliva, cerebrospinal fluid, blood, breast milk, infected tissues, and urine.8,9 It is transmitted through contact with respiratory secretions and/or saliva, direct contact, or through fomites (eg, bedding, doorknobs).10
Before development of an effective vaccine, mumps was a universal childhood disease in the US; by age 14, most children had been infected.11 In the absence of widespread vaccination, mumps epidemics will occur every three to five years—as they still do in parts of the world without effective vaccination programs.12
As a result of widespread vaccination in the US, mumps incidence declined from 152,209 cases in 1967 to 2,982 cases in 1985 (see “Mumps and the MMR Vaccine”). Cases were reduced even further when administration of a second MMR dose was introduced in 1990.13 By 2000, the Healthy People 2010 goal was to eliminate mumps altogether.14
Continue for patient presentation >>
PATIENT PRESENTATION
Parotitis is the classic (but not universal) physical exam finding in mumps. Parotid gland inflammation causes generalized swelling anterior to the ear and inferior to the mastoid process, with jaw angle obliteration (see Figure 1).9 If only one parotid gland is involved, the patient’s face appears asymmetric. Other significant exam findings may include fever and erythematous swelling of the Stensen (parotid) duct.10
Nonspecific symptoms—including respiratory symptoms, myalgia, anorexia, malaise, headache, and low-grade fever—may occur in more than 50% of cases.8 CNS involvement may cause nuchal rigidity (stiff neck). In postpubertal males, testicular swelling and/or induration, pain, tenderness, and enlarged inguinal lymph nodes may be present.
Mumps can be challenging to diagnose based on clinical presentation alone; for example, parotitis occurs in only 30% to 40% of cases.8 Other viruses, such as parainfluenza virus 1 and 3, coxsackievirus, adenovirus, influenza A, cytomegalovirus, and HIV, can also cause swelling of the parotid glands, but mumps is the only virus known to cause parotitis on an epidemic scale.4 Furthermore, up to 20% of cases may be asymptomatic.8,11 Because mumps is highly contagious, a history of exposure to an affected individual is a compelling factor in making the diagnosis.
The incubation period for mumps is 12 to 25 days, with parotitis usually developing 16 to 18 days after exposure.4 This relatively lengthy incubation period increases the likelihood of viral spread. The virus is contagious from three days prior to symptom onset to day 4 of active disease.8 To prevent disease transmission, it is recommended that individuals remain isolated from others until five days after the onset of salivary gland swelling.4
Next page: Laboratory confirmation >>
LABORATORY CONFIRMATION
The CDC recommends determination of any one of the following to help confirm the diagnosis of acute mumps infection.
• Presence of serum mumps IgM antibodies
• Significant rise in IgG antibody titer between the acute and convalescent-phase serum specimens
• IgG seroconversion
• Positive mumps virus culture
• Detection of virus by real-time reverse transcriptase polymerase chain reaction (RT-PCR)4
Antibody testing
At the initial visit, a serum specimen should be obtained to test for mumps IgM antibodies.4 The CDC recommends enzyme immunoassay (EIA) testing for IgM antibodies to confirm acute mumps infection.4
IgM antibodies are detectable five days after onset of symptoms and, after reaching a maximum level, remain elevated for several weeks. If the initial IgM test is negative, the test can be repeated in five to seven days.4
Either EIA or immunofluorescence antibody assay (IFA) testing for mumps IgG antibodies should be performed on both acute- and convalescent-phase serum samples. Laboratory confirmation requires a fourfold rise in the antibody titer using a quantitative assay4 or seroconversion from negative to positive.
Virus detection
If possible, mumps virus samples should be obtained no more than three to eight days after symptom onset because delay may result in a low viral yield.4 The best viral samples are obtained via parotid duct swabs (see Figure 2). Before swabbing the buccal cavity, the parotid gland should be massaged for 30 seconds to ensure that the specimen contains gland secretions.4
Mumps virus can be detected by RT-PCR or culture. The RT-PCR is currently the most sensitive test for mumps, but most RT-PCR testing is done by public health laboratories and the CDC, and results may not be available until after the illness has resolved.4
Laboratory tests, however, are not always helpful in confirming a clinical diagnosis of mumps. Vaccinated persons may not mount a secondary immune response to mumps and consequently may not have a significant IgM response. It is also possible that a high level of IgG antibodies will cause a false-positive IgM test results.4
Other laboratory tests that may support a diagnosis of mumps include a complete blood cell count, which may reveal a leukopenia with relative lymphocytosis or neutrophil leukocytosis,16 and a measurement of serum amylase level which, if elevated, may confirm the inflammatory process.10 See Table 1 for a summary of tests that confirm or support a mumps diagnosis.
Mumps is a reportable illness, and the local health department should be contacted for assistance with determining where and how to ship specimens.17 However, in the absence of laboratory confirmation, only clinical cases with parotitis, other salivary gland involvement, or mumps-related complications are notifiable.11
Continue for mumps manifestations >>
MUMPS MANIFESTATIONS
The continuum of mumps illness ranges from asymptomatic infection to parotitis (the most well-known manifestation) to rare but severe complications.8 Table 2 lists potential complications of mumps in order of frequency. Complications vary by age and sex but tend to occur more often in adults.4,11
Immunization modifies the clinical presentation of mumps11 and likely decreases complications. Although one analysis of the 2006 outbreak identified no difference in complication rates between vaccinated and unvaccinated patients, the authors attributed this to misclassification of patients’ vaccination status; they did find lower reported rates of mumps complications compared with complication rates before widespread vaccination.13 A study of the 2009-2010 outbreak found that complication rates were lower among vaccinated patients.18
RISK FACTORS FOR OUTBREAKS
Of the three components of the MMR vaccine, the least effective is the mumps portion. One dose confers 78% immunity and two doses, 88%, which the CDC characterizes as incomplete protection.1 Compare this to the measles vaccine, which is 97% effective with two doses,19 and the rubella vaccine, which is 97% effective after a single dose in conferring immunity.11
In 2000, as a result of high rates of vaccination, the US determined that endemic measles had been eliminated. A similar conclusion was reached about rubella in 2004, and both determinations were reaffirmed in 2011.20 In contrast, mumps has never been eliminated.1
Waning immunity
While antibodies to mumps as a result of vaccination persist into adulthood, they decline over time. A 2009 CDC study found that, 12 years after a second MMR dose, mumps antibody levels in adolescents and young adults had declined to levels similar to those measured before the second dose.21 Other analyses of major outbreaks suggested the need for further studies to determine optimal timing for the second MMR dose (eg, at a later age) or if a third dose would provide longer-lasting immunity.13,22 Waning immunity among young adults, coupled with high-density living environments that intensify exposure to the virus, increase risk for the disease.23
Further complicating the situation is the lack of evidence about the required level of antibodies needed to confer protection against mumps infection.17 To date, the antibody titer threshold of mumps-specific IgG at which an individual is protected from the disease is unknown.11,17
Imported risks
Mumps remains endemic in many parts of the world, with vaccination employed in only 61% of countries belonging to the World Health Organization.4 Several recent outbreaks were traced to index cases originating outside the US.13 It is likely that importation of the virus from abroad will continue.
Next page: Outbreak management >>
OUTBREAK MANAGEMENT
A mumps outbreak is defined as three or more cases linked by time and place.4 The keys to managing an outbreak are to define the population(s) at risk and their transmission setting(s) and to rapidly identify and vaccinate vulnerable individuals without evidence of immunity.4
Presumptive evidence of mumps immunity includes11
• Documentation of vaccination with two doses of live mumps virus–containing vaccine
• Laboratory evidence of immunity
• Laboratory confirmation of disease
• Birth year before 1957.
Documentation of two doses of MMR constitutes evidence of adequate vaccination for school-age children and adolescents and for young adults attending postsecondary institutions. During an outbreak, susceptible (ie, unvaccinated) students should be excluded from attendance until they have been vaccinated; those with one dose may attend but should receive the second dose.4 Those declining vaccination for medical, religious, or other reasons should be excluded until at least 26 days after the onset of parotitis in the last person with mumps at the institution.24
If the outbreak threatens the wider community (eg, preschool-age children and adults), a second MMR dose should be considered for children ages 1 to 4 or for adults who have received one MMR dose. Similarly, MMR vaccination should be considered for adults born before 1957 who have no other evidence of immunity and are at risk for exposure to the virus.11
In the workplace, health care workers’ (HCWs’) immunity status should be known, documented, and accessible in advance of an outbreak.11 If an HCW without evidence of immunity is exposed to mumps, he or she should be excluded from patient care from the time of first unprotected exposure through the 25th day after the last exposure.25 Although individuals born before 1957 are generally considered immune, if a nosocomial mumps outbreak occurs, the two-dose MMR regimen should be administered to these HCW as well.4
In 1991, the US military began to immunize recruits routinely with MMR, regardless of their immunization status.26 During the 2006 mumps outbreak, the incidence of mumps among military personnel was minimal compared to that among their civilian counterparts—perhaps due to administration of a third MMR dose to an unknown number of recruits.22
CDC researchers studied the impact of a third MMR dose for mumps outbreak control in 2012 and concluded that, while a third dose may help control outbreaks among populations with preexisting high two-dose vaccine coverage, further study is needed.27
Although insufficient data exist on which to base a recommendation for or against a third MMR dose for mumps outbreak control, the CDC has issued guidance for public health departments for targeted administration during outbreaks. Considerations include
• Intense exposure settings
• High two-dose vaccination coverage (ie, > 90%)
• High attack rates (> 5 cases per 1,000 population)
• Evidence of ongoing transmission for at least two weeks in the target population.4
TREATMENT
There is no specific treatment for mumps. Care is supportive and in the outpatient setting includes rest, cold or heat to the affected areas, and OTC pain relievers. Ice can be used to help relieve the pain of orchitis. Acidic foods may stimulate the parotid glands, causing pain and difficulty swallowing, and should be avoided.
Isolation of infectious patients is vital to preventing the spread of mumps.4 In the clinician’s office, a separate waiting area should be used for a potential mumps patient, or the patient should be located at least three feet from other patients and asked to wear a surgical mask. HCW working with potential mumps patients should follow droplet precautions (eg, wear personal protective equipment) in addition to standard precautions and should be hypervigilant about hand washing.24
CONCLUSION
Mumps is a usually benign, self-limited infectious disease that can potentially result in serious complications. It is also prone to periodic outbreaks. Control of mumps can best be accomplished by remembering these five “Ps”:
• Prevention—through widespread two-dose MMR vaccination
• Parotitis—recognize it as the primary symptom of mumps and make the diagnosis in a timely manner
• Persistence—in making the diagnosis clinically and in weighing laboratory results within the context of clinical disease
• Personal protective equipment—use it consistently in the health care setting or as needed in the home
• Protection—isolate patients with mumps to avoid spreading the disease
1. CDC. Mumps cases and outbreaks. www.cdc.gov/mumps/outbreaks.html. Accessed March 19, 2015.
2. CDC. Measles prevention: recommendations of the Immunization Practices Advisory Committee (ACIP). MMWR Morb Mortal Wkly Rep. 1989;38(suppl 9):1-18.
3. CDC. Summary of notifiable diseases—United States. 1993-2012. MMWR Morb Mortal Wkly Rep. www.cdc.gov/mmwr/mmwr_nd/index.html. Accessed March 19, 2015.
4. CDC. Mumps, chap 9. In: Manual for the Surveillance of Vaccine-Preventable Diseases. August 2012. www.cdc.gov/vaccines/pubs/surv-manual/chpt09-mumps.html. Accessed March 19, 2015.
5. Pyle E. Central Ohio mumps outbreak finally loses steam. The Columbus Dispatch. October 11, 2014. www.dispatch.com/content/stories/local/2014/10/10/Health-officials-declare-mumps-outbreak-over.html. Accessed March 19, 2015.
6. Hascup J. Three more mumps cases: Penguins’ Steve Downie, Thomas Greiss, Devils’ Patrik Elias, Michael Ryder. USA TODAY. December 27, 2014. www.usatoday.com/story/sports/nhl/2014/12/26/steve-downie-thomas-greiss-mumps-pittsburgh-penguins/20911031/. Accessed March 19, 2015.
7. Idaho public health officials warn that mumps outbreak involving University students has spread to Boise and State of Washington [news release]. Boise, ID: Idaho Department of Health and Welfare Public Information Office; February 6, 2015. www.healthandwelfare.idaho.gov/AboutUs/Newsroom/tabid/130/ctl/ArticleView/mid/3061/articleId/1819/Idaho-Public-Health-Officials-Warn-that-Mumps-Outbreak-Involving-University-Students-Has-Spread-to-Boise-and-State-of-Washington.aspx. Accessed March 19, 2015.
8. CDC. Epidemiology and prevention of vaccine-preventable diseases. Mumps, chap 12. In: The Pink Book: Course Textbook. 12th ed, 2012. www.cdc.gov/vaccines/pubs/pinkbook/mumps.html. Accessed March 19, 2015.
9. Albrecht MA. Epidemiology, clinical manifestations, diagnosis, and management of mumps. www.uptodate.com/contents/epidemiology-clin ical-manifestations-diagnosis-and-management-of-mumps. Accessed March 19, 2015.
10. Defendi GL. Mumps. http://reference.medscape.com/article/966678-overview. Accessed March 19, 2015.
11. CDC. Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2013;62(RR04):1-34.
12. Rubin S, Carbone KM. Mumps. In: Longo DL, Fauci AS, Kasper DL et al, eds. Harrison’s Principles of Internal Medicine. 18th ed. New York, NY: The McGraw-Hill Companies, Inc.; 2012:chap 194.
13. Dayan G, Quinlisk M, Parker A, et al. Recent resurgence of mumps in the United States. New Engl J Med. 2008;358:1580-1589.
14. US Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2010: Objectives for Improving Health. www.healthypeople.gov/2010/Document/HTML/Volume1 /14Immunization.htm#_Toc494510239. Accessed March 19, 2015.
15. CDC. Measles, mumps, and rubella: vaccine use and strategies for elimination of measles, rubella, and congenital rubella syndrome and control of mumps: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 1998;47(RR-8):1-57.
16. Gupta RK, Best J, MacMahon E. Mumps and the UK epidemic 2005. BMJ. 2005;(330):1132-1135.
17. CDC. Laboratory testing for mumps infection. www.cdc.gov/mumps/lab/qa-lab-test-infect.html. Accessed March 19, 2015.
18. Barskey AE, Schulte C, Rosen JB, et al. Mumps outbreak in Orthodox Jewish communities in the United States. New Engl J Med. 2012;367(18): 1704-1713.
19. CDC. Frequently asked questions about measles in the U.S. www.cdc.gov/measles/about/faqs.html. Accessed March 19, 2015.
20. Papania MJ, Wallace GS, Rota PA, et al. Elimination of endemic measles, rubella, and congenital rubella syndrome from the Western hemisphere: the US experience. JAMA Pediatr. 2014;168(2):148-155.
21. LeBaron CW, Forghani B, Beck C, et al. Persistence of mumps antibodies after 2 doses of measles-mumps-rubella vaccine. J Infect Dis. 2009; 199(4):552-560.
22. Anis E, Grotto I, Moerman L, et al. Mumps outbreak in Israel’s highly vaccinated society: are two doses enough? Epidemiol Infect. 2012; 140:439-446.
23. Sane J, Gouma S, Koopmans M, et al. Epidemic of mumps among vaccinated persons, The Netherlands, 2009-2012. Emerg Infect Dis. 2014;20(4):643-648.
24. CDC. Exposure and response. www.cdc.gov/mumps/clinical/qa-exposure-response.html. Accessed March 19, 2015.
25. CDC. Mumps prevention and control in healthcare settings. www.cdc.gov/mumps/prev-control-settings/background.html. Accessed March 19, 2015.
26. Barskey AE, Glasser JW, LeBaron CW. Mumps resurgence in the United States: a historical perspective on unexpected elements. Vaccine. 2009;27:6186-6195.
27. Ogbuanu IU, Kutty PK, Hudson JM, et al. Impact of a third dose of measles-mumps-rubella vaccine on a mumps outbreak. Pediatrics. 2012;130:e1567-e1574.
28. CDC. Physical findings and complications. www.cdc.gov/mumps/clinical/qa-physical-complic.html. Accessed March 19, 2015.
29. Conniff R. A forgotten pioneer of vaccines. The New York Times. May 6, 2013. www.nytimes.com/2013/05/07/health/maurice-hilleman-mmr-vaccines-forgotten-hero.html?_r=0. Accessed March 19, 2015.
30. CDC. MMR vaccine for mumps. www.cdc.gov/vaccines/vpd-vac/mumps/vac-faqs-tech.htm. Accessed March 19, 2015.
31. The College of Physicians of Philadelphia. The history of vaccines. www.historyofvaccines.org/content/timelines/all. Accessed March 19, 2015.
32. CDC. Travelers’ health. Mumps. wwwnc.cdc.gov/travel/diseases/mumps. Accessed March 19, 2015.
33. Wakefield AJ, Murch SH, Anthony A, et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children [retracted in Lancet. 2010;375:445]. Lancet. 1998;351:637-641.
34. Murch SH, Anthony A, Casson DH, et al. Retraction of an interpretation. Lancet. 2004;363(9411):750.
35. Deer B. How the case against the MMR vaccine was fixed. BMJ. 2011;342:1-16.
36. The Editors of The Lancet. Notice of retraction of "Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children" [retraction of: Wakefield AJ, Murch SH, Anthony A, et al. In: Lancet. 1998;351:637-641]. Lancet. 2010;375:445.
37. Whalen J. UK bans doctor who linked autism to vaccine. The Wall Street Journal. May 24, 2010. www.wsj.com/articles/SB10001424052748704113504575263994195318772. Accessed March 19, 2015.
38. CDC. Vaccine safety: measles, mumps and rubella (MMR) vaccine. www.cdc.gov/vaccinesafety/vaccines/mmr/mmr.html. Accessed March 19, 2015.
39. Madsen KM, Hviid A, Vestergaard M, et al. A population-based study of measles, mumps, and rubella vaccination and autism. N Engl J Med. 2002;347:1477-1482.
40. DeStefano F, Bhasin TK, Thompson WW, et al. Age at first measles-mumps-rubella vaccination in children with autism and school-matched control subjects: a population-based study in metropolitan Atlanta. Pediatrics. 2004;113(2):259-266.
41. Richler J, Luyster R. Risi S, et al. Is there a ‘regressive phenotype’ of autism spectrum disorder associated with the measles-mumps-rubella vaccine? A CPEA study. J Autism Dev Disord. 2006;36(3):299-316.
42. Nyhan B, Reifler J, Richey S, Freed G. Effective messages in vaccine promotion: a randomized trial. Pediatrics. 2014:133:1-8.
43. Haberman C. A discredited vaccine study’s continuing impact on public health. The New York Times. February 1, 2015. www.nytimes.com/2015/02/02/us/a-discredited-vaccine-studys-continuing-impact- on-public- health.html?_r=0. Accessed March 19, 2015.
1. CDC. Mumps cases and outbreaks. www.cdc.gov/mumps/outbreaks.html. Accessed March 19, 2015.
2. CDC. Measles prevention: recommendations of the Immunization Practices Advisory Committee (ACIP). MMWR Morb Mortal Wkly Rep. 1989;38(suppl 9):1-18.
3. CDC. Summary of notifiable diseases—United States. 1993-2012. MMWR Morb Mortal Wkly Rep. www.cdc.gov/mmwr/mmwr_nd/index.html. Accessed March 19, 2015.
4. CDC. Mumps, chap 9. In: Manual for the Surveillance of Vaccine-Preventable Diseases. August 2012. www.cdc.gov/vaccines/pubs/surv-manual/chpt09-mumps.html. Accessed March 19, 2015.
5. Pyle E. Central Ohio mumps outbreak finally loses steam. The Columbus Dispatch. October 11, 2014. www.dispatch.com/content/stories/local/2014/10/10/Health-officials-declare-mumps-outbreak-over.html. Accessed March 19, 2015.
6. Hascup J. Three more mumps cases: Penguins’ Steve Downie, Thomas Greiss, Devils’ Patrik Elias, Michael Ryder. USA TODAY. December 27, 2014. www.usatoday.com/story/sports/nhl/2014/12/26/steve-downie-thomas-greiss-mumps-pittsburgh-penguins/20911031/. Accessed March 19, 2015.
7. Idaho public health officials warn that mumps outbreak involving University students has spread to Boise and State of Washington [news release]. Boise, ID: Idaho Department of Health and Welfare Public Information Office; February 6, 2015. www.healthandwelfare.idaho.gov/AboutUs/Newsroom/tabid/130/ctl/ArticleView/mid/3061/articleId/1819/Idaho-Public-Health-Officials-Warn-that-Mumps-Outbreak-Involving-University-Students-Has-Spread-to-Boise-and-State-of-Washington.aspx. Accessed March 19, 2015.
8. CDC. Epidemiology and prevention of vaccine-preventable diseases. Mumps, chap 12. In: The Pink Book: Course Textbook. 12th ed, 2012. www.cdc.gov/vaccines/pubs/pinkbook/mumps.html. Accessed March 19, 2015.
9. Albrecht MA. Epidemiology, clinical manifestations, diagnosis, and management of mumps. www.uptodate.com/contents/epidemiology-clin ical-manifestations-diagnosis-and-management-of-mumps. Accessed March 19, 2015.
10. Defendi GL. Mumps. http://reference.medscape.com/article/966678-overview. Accessed March 19, 2015.
11. CDC. Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2013;62(RR04):1-34.
12. Rubin S, Carbone KM. Mumps. In: Longo DL, Fauci AS, Kasper DL et al, eds. Harrison’s Principles of Internal Medicine. 18th ed. New York, NY: The McGraw-Hill Companies, Inc.; 2012:chap 194.
13. Dayan G, Quinlisk M, Parker A, et al. Recent resurgence of mumps in the United States. New Engl J Med. 2008;358:1580-1589.
14. US Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2010: Objectives for Improving Health. www.healthypeople.gov/2010/Document/HTML/Volume1 /14Immunization.htm#_Toc494510239. Accessed March 19, 2015.
15. CDC. Measles, mumps, and rubella: vaccine use and strategies for elimination of measles, rubella, and congenital rubella syndrome and control of mumps: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 1998;47(RR-8):1-57.
16. Gupta RK, Best J, MacMahon E. Mumps and the UK epidemic 2005. BMJ. 2005;(330):1132-1135.
17. CDC. Laboratory testing for mumps infection. www.cdc.gov/mumps/lab/qa-lab-test-infect.html. Accessed March 19, 2015.
18. Barskey AE, Schulte C, Rosen JB, et al. Mumps outbreak in Orthodox Jewish communities in the United States. New Engl J Med. 2012;367(18): 1704-1713.
19. CDC. Frequently asked questions about measles in the U.S. www.cdc.gov/measles/about/faqs.html. Accessed March 19, 2015.
20. Papania MJ, Wallace GS, Rota PA, et al. Elimination of endemic measles, rubella, and congenital rubella syndrome from the Western hemisphere: the US experience. JAMA Pediatr. 2014;168(2):148-155.
21. LeBaron CW, Forghani B, Beck C, et al. Persistence of mumps antibodies after 2 doses of measles-mumps-rubella vaccine. J Infect Dis. 2009; 199(4):552-560.
22. Anis E, Grotto I, Moerman L, et al. Mumps outbreak in Israel’s highly vaccinated society: are two doses enough? Epidemiol Infect. 2012; 140:439-446.
23. Sane J, Gouma S, Koopmans M, et al. Epidemic of mumps among vaccinated persons, The Netherlands, 2009-2012. Emerg Infect Dis. 2014;20(4):643-648.
24. CDC. Exposure and response. www.cdc.gov/mumps/clinical/qa-exposure-response.html. Accessed March 19, 2015.
25. CDC. Mumps prevention and control in healthcare settings. www.cdc.gov/mumps/prev-control-settings/background.html. Accessed March 19, 2015.
26. Barskey AE, Glasser JW, LeBaron CW. Mumps resurgence in the United States: a historical perspective on unexpected elements. Vaccine. 2009;27:6186-6195.
27. Ogbuanu IU, Kutty PK, Hudson JM, et al. Impact of a third dose of measles-mumps-rubella vaccine on a mumps outbreak. Pediatrics. 2012;130:e1567-e1574.
28. CDC. Physical findings and complications. www.cdc.gov/mumps/clinical/qa-physical-complic.html. Accessed March 19, 2015.
29. Conniff R. A forgotten pioneer of vaccines. The New York Times. May 6, 2013. www.nytimes.com/2013/05/07/health/maurice-hilleman-mmr-vaccines-forgotten-hero.html?_r=0. Accessed March 19, 2015.
30. CDC. MMR vaccine for mumps. www.cdc.gov/vaccines/vpd-vac/mumps/vac-faqs-tech.htm. Accessed March 19, 2015.
31. The College of Physicians of Philadelphia. The history of vaccines. www.historyofvaccines.org/content/timelines/all. Accessed March 19, 2015.
32. CDC. Travelers’ health. Mumps. wwwnc.cdc.gov/travel/diseases/mumps. Accessed March 19, 2015.
33. Wakefield AJ, Murch SH, Anthony A, et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children [retracted in Lancet. 2010;375:445]. Lancet. 1998;351:637-641.
34. Murch SH, Anthony A, Casson DH, et al. Retraction of an interpretation. Lancet. 2004;363(9411):750.
35. Deer B. How the case against the MMR vaccine was fixed. BMJ. 2011;342:1-16.
36. The Editors of The Lancet. Notice of retraction of "Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children" [retraction of: Wakefield AJ, Murch SH, Anthony A, et al. In: Lancet. 1998;351:637-641]. Lancet. 2010;375:445.
37. Whalen J. UK bans doctor who linked autism to vaccine. The Wall Street Journal. May 24, 2010. www.wsj.com/articles/SB10001424052748704113504575263994195318772. Accessed March 19, 2015.
38. CDC. Vaccine safety: measles, mumps and rubella (MMR) vaccine. www.cdc.gov/vaccinesafety/vaccines/mmr/mmr.html. Accessed March 19, 2015.
39. Madsen KM, Hviid A, Vestergaard M, et al. A population-based study of measles, mumps, and rubella vaccination and autism. N Engl J Med. 2002;347:1477-1482.
40. DeStefano F, Bhasin TK, Thompson WW, et al. Age at first measles-mumps-rubella vaccination in children with autism and school-matched control subjects: a population-based study in metropolitan Atlanta. Pediatrics. 2004;113(2):259-266.
41. Richler J, Luyster R. Risi S, et al. Is there a ‘regressive phenotype’ of autism spectrum disorder associated with the measles-mumps-rubella vaccine? A CPEA study. J Autism Dev Disord. 2006;36(3):299-316.
42. Nyhan B, Reifler J, Richey S, Freed G. Effective messages in vaccine promotion: a randomized trial. Pediatrics. 2014:133:1-8.
43. Haberman C. A discredited vaccine study’s continuing impact on public health. The New York Times. February 1, 2015. www.nytimes.com/2015/02/02/us/a-discredited-vaccine-studys-continuing-impact- on-public- health.html?_r=0. Accessed March 19, 2015.