User login
LAS VEGAS – A prospective study of pregnant women with opioid use disorder showed good success with tapering or discontinuation of medication-assisted treatment (MAT) for women who wished to reduce or eliminate opioids while pregnant.
In related work, naltrexone showed promise for MAT in pregnancy, with rapid fetal clearance and no neonatal abstinence syndrome (NAS) seen in women who were adherent to naltrexone.
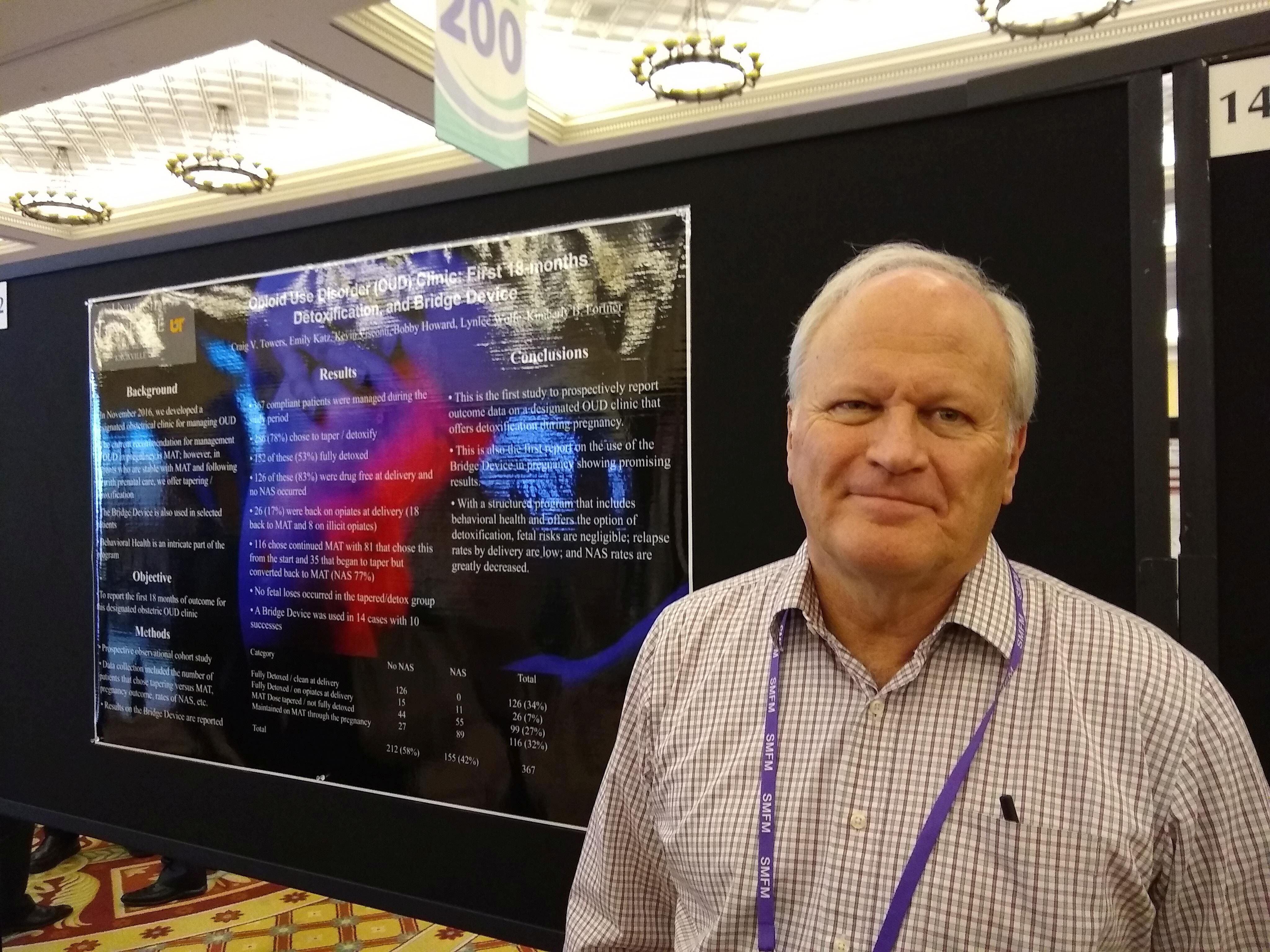
Presenting early experiences from an obstetric clinic dedicated to care of women with opioid use disorder (OUD), Craig Towers, MD, said that the clinic began seeing patients in November, 2016. “Eastern Tennessee has a high rate of opioid use disorder,” so the clinic at the University of Tennessee, Knoxville, fills an unmet need, he said, speaking during a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Women who enroll at the clinic are offered MAT; those who are stable on MAT and adherent to prenatal care also are offered the choice to taper from MAT and detoxify, said Dr. Towers, professor in the division of maternal-fetal medicine in the department of obstetrics and gynecology at the University of Tennessee – Knoxville.
The prospective observational cohort study found that, of a total of 367 compliant patients, 286 (78%) chose opioid tapering/detoxification, and of these, 152 (53%) did detoxify fully. Of these patients, 126 (83%) were taking no opioids at delivery, and their infants experienced no NAS.
At the time of delivery, 26 patients (17%) were taking opioids at delivery; 18 were back on MAT, and 8 were using illicit opioids. A total of 116 patients chose to continue MAT, whether they stayed on the regimen or converted back to stable MAT doses after beginning to taper.
Another option offered women at the OUD-dedicated obstetric clinic is the use of the Bridge device, a percutaneous nerve field stimulator, for OUD. Dr. Tower said that, in early use in 14 patients, the Bridge was successful in helping women transition off opioids completely in 10 (71%) patients.
About the larger study, Dr. Towers said, “This is the first study to prospectively report outcome data on a designated OUD clinic that offers detoxification during pregnancy.
“With a structured program that includes behavioral health and offers the option of detoxification, fetal risks are negligible, relapse rates by delivery are low, and NAS rates are greatly decreased,” wrote Dr. Towers and colleagues in the abstract accompanying the study.
In a related poster presentation, Dr. Towers reported outcomes for a subset of pregnant women with OUD who received naltrexone as MAT. Previously, said Dr. Towers, retrospective work showed no significant harm using naltrexone, which is one of the three approved options for MAT to manage OUD, along with buprenorphine and methadone. Naltrexone has the advantage of helping reduce cravings.
Of the 108 patients, 82 (76%) remained on naltrexone until delivery; in these pregnancies, there were no cases of NAS. However, among the 26 pregnancies in which women stopped taking naltrexone before delivery, there were 6 (23%) NAS cases.
Fifty-one patients were started on naltrexone before 24 weeks’ gestation, and of those patients, no changes were seen with fetal monitoring. There were no instances of spontaneous abortion or intrauterine demise in any participants.
The investigators tracked gestational age at the point of full detoxification and gestational age at the point naltrexone was started. Additionally, fetal response to naltrexone and maternal and neonatal outcomes were recorded.
“This is the first prospective study and largest to date on the use of naltrexone in pregnancy,” Dr. Towers and his colleagues wrote in the poster accompanying the presentation. “These data demonstrate that naltrexone MAT is a viable option for managing OUD in pregnancy.”
Dr. Towers reported no conflicts of interest and no outside sources of funding.
LAS VEGAS – A prospective study of pregnant women with opioid use disorder showed good success with tapering or discontinuation of medication-assisted treatment (MAT) for women who wished to reduce or eliminate opioids while pregnant.
In related work, naltrexone showed promise for MAT in pregnancy, with rapid fetal clearance and no neonatal abstinence syndrome (NAS) seen in women who were adherent to naltrexone.
Presenting early experiences from an obstetric clinic dedicated to care of women with opioid use disorder (OUD), Craig Towers, MD, said that the clinic began seeing patients in November, 2016. “Eastern Tennessee has a high rate of opioid use disorder,” so the clinic at the University of Tennessee, Knoxville, fills an unmet need, he said, speaking during a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Women who enroll at the clinic are offered MAT; those who are stable on MAT and adherent to prenatal care also are offered the choice to taper from MAT and detoxify, said Dr. Towers, professor in the division of maternal-fetal medicine in the department of obstetrics and gynecology at the University of Tennessee – Knoxville.
The prospective observational cohort study found that, of a total of 367 compliant patients, 286 (78%) chose opioid tapering/detoxification, and of these, 152 (53%) did detoxify fully. Of these patients, 126 (83%) were taking no opioids at delivery, and their infants experienced no NAS.
At the time of delivery, 26 patients (17%) were taking opioids at delivery; 18 were back on MAT, and 8 were using illicit opioids. A total of 116 patients chose to continue MAT, whether they stayed on the regimen or converted back to stable MAT doses after beginning to taper.
Another option offered women at the OUD-dedicated obstetric clinic is the use of the Bridge device, a percutaneous nerve field stimulator, for OUD. Dr. Tower said that, in early use in 14 patients, the Bridge was successful in helping women transition off opioids completely in 10 (71%) patients.
About the larger study, Dr. Towers said, “This is the first study to prospectively report outcome data on a designated OUD clinic that offers detoxification during pregnancy.
“With a structured program that includes behavioral health and offers the option of detoxification, fetal risks are negligible, relapse rates by delivery are low, and NAS rates are greatly decreased,” wrote Dr. Towers and colleagues in the abstract accompanying the study.
In a related poster presentation, Dr. Towers reported outcomes for a subset of pregnant women with OUD who received naltrexone as MAT. Previously, said Dr. Towers, retrospective work showed no significant harm using naltrexone, which is one of the three approved options for MAT to manage OUD, along with buprenorphine and methadone. Naltrexone has the advantage of helping reduce cravings.
Of the 108 patients, 82 (76%) remained on naltrexone until delivery; in these pregnancies, there were no cases of NAS. However, among the 26 pregnancies in which women stopped taking naltrexone before delivery, there were 6 (23%) NAS cases.
Fifty-one patients were started on naltrexone before 24 weeks’ gestation, and of those patients, no changes were seen with fetal monitoring. There were no instances of spontaneous abortion or intrauterine demise in any participants.
The investigators tracked gestational age at the point of full detoxification and gestational age at the point naltrexone was started. Additionally, fetal response to naltrexone and maternal and neonatal outcomes were recorded.
“This is the first prospective study and largest to date on the use of naltrexone in pregnancy,” Dr. Towers and his colleagues wrote in the poster accompanying the presentation. “These data demonstrate that naltrexone MAT is a viable option for managing OUD in pregnancy.”
Dr. Towers reported no conflicts of interest and no outside sources of funding.
LAS VEGAS – A prospective study of pregnant women with opioid use disorder showed good success with tapering or discontinuation of medication-assisted treatment (MAT) for women who wished to reduce or eliminate opioids while pregnant.
In related work, naltrexone showed promise for MAT in pregnancy, with rapid fetal clearance and no neonatal abstinence syndrome (NAS) seen in women who were adherent to naltrexone.
Presenting early experiences from an obstetric clinic dedicated to care of women with opioid use disorder (OUD), Craig Towers, MD, said that the clinic began seeing patients in November, 2016. “Eastern Tennessee has a high rate of opioid use disorder,” so the clinic at the University of Tennessee, Knoxville, fills an unmet need, he said, speaking during a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Women who enroll at the clinic are offered MAT; those who are stable on MAT and adherent to prenatal care also are offered the choice to taper from MAT and detoxify, said Dr. Towers, professor in the division of maternal-fetal medicine in the department of obstetrics and gynecology at the University of Tennessee – Knoxville.
The prospective observational cohort study found that, of a total of 367 compliant patients, 286 (78%) chose opioid tapering/detoxification, and of these, 152 (53%) did detoxify fully. Of these patients, 126 (83%) were taking no opioids at delivery, and their infants experienced no NAS.
At the time of delivery, 26 patients (17%) were taking opioids at delivery; 18 were back on MAT, and 8 were using illicit opioids. A total of 116 patients chose to continue MAT, whether they stayed on the regimen or converted back to stable MAT doses after beginning to taper.
Another option offered women at the OUD-dedicated obstetric clinic is the use of the Bridge device, a percutaneous nerve field stimulator, for OUD. Dr. Tower said that, in early use in 14 patients, the Bridge was successful in helping women transition off opioids completely in 10 (71%) patients.
About the larger study, Dr. Towers said, “This is the first study to prospectively report outcome data on a designated OUD clinic that offers detoxification during pregnancy.
“With a structured program that includes behavioral health and offers the option of detoxification, fetal risks are negligible, relapse rates by delivery are low, and NAS rates are greatly decreased,” wrote Dr. Towers and colleagues in the abstract accompanying the study.
In a related poster presentation, Dr. Towers reported outcomes for a subset of pregnant women with OUD who received naltrexone as MAT. Previously, said Dr. Towers, retrospective work showed no significant harm using naltrexone, which is one of the three approved options for MAT to manage OUD, along with buprenorphine and methadone. Naltrexone has the advantage of helping reduce cravings.
Of the 108 patients, 82 (76%) remained on naltrexone until delivery; in these pregnancies, there were no cases of NAS. However, among the 26 pregnancies in which women stopped taking naltrexone before delivery, there were 6 (23%) NAS cases.
Fifty-one patients were started on naltrexone before 24 weeks’ gestation, and of those patients, no changes were seen with fetal monitoring. There were no instances of spontaneous abortion or intrauterine demise in any participants.
The investigators tracked gestational age at the point of full detoxification and gestational age at the point naltrexone was started. Additionally, fetal response to naltrexone and maternal and neonatal outcomes were recorded.
“This is the first prospective study and largest to date on the use of naltrexone in pregnancy,” Dr. Towers and his colleagues wrote in the poster accompanying the presentation. “These data demonstrate that naltrexone MAT is a viable option for managing OUD in pregnancy.”
Dr. Towers reported no conflicts of interest and no outside sources of funding.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Over two-thirds of MAT-adherent patients chose detoxification.
Major finding:
Study details: Prospective single-center cohort study of 367 pregnant women with opioid use disorder.
Disclosures: Dr. Towers reported no outside sources of funding and no relevant conflicts of interest.
Source: Towers C. et al. SMFM 2019, Posters 141 & 142.