User login
Postcesarean pain relief better on nonopioid regimen
LAS VEGAS – Women who had cesarean delivery and received a nonopioid pain control regimen at hospital discharge had lower pain scores by 4 weeks post partum than those who also received opioids, according to study results shared during a fellows session at the meeting presented by the Society for Maternal-Fetal Medicine.
At 2-4 weeks post partum, the mean pain score on a visual analog scale (VAS) was 12/100 mm for women on the nonopioid regimen, compared with 16/100 mm for women who received opioids, using an intention-to-treat analysis. The median pain score for those in the nonopioid arm was 0, compared with 6 for those in the opioid arm.
The findings surprised Jenifer Dinis, MD, a maternal-fetal medicine fellow at the University of Texas, Houston, and her collaborators, because they had hypothesized merely that the two groups would have similar pain scores 2-4 weeks after delivery.
Although women in the nonopioid arm were able to obtain a rescue hydrocodone prescription through the study, and some women obtained opioids from their private physician, they still used less than half as much opioid medication as women in the opioid arm (21 versus 43 morphine milligram equivalents, P less than .01).
However, women in the nonopioid arm did not use significantly more ibuprofen or acetaminophen, and there was no difference in patient satisfaction with the outpatient postpartum analgesic regimen between study arms. Somnolence was more common in the opioid arm (P = .03); no other medication side effects were significantly more common in one group than the other.
Overall, 22 of 76 (29%) women in the nonopioid arm took any opioids after discharge, compared with 59/81 (73%) in the opioid arm (P less than .01).
After cesarean delivery, the 170 participating women had an inpatient pain control regimen determined by their primary ob.gyn., Dr. Dinis said in her presentation. Patients were randomized 1:1 to their outpatient analgesia regimens on postoperative day 2 or 3, with appropriate prescriptions placed in patient charts. Participants received either a nonopioid regimen with prescriptions for 60 ibuprofen tablets (600 mg) and 60 acetaminophen tablets (325 mg), or to an opioid regimen that included ibuprofen plus hydrocodone/acetaminophen 5 (325 mg) 1-2 tablets every 4 hours.
Pain scores were assessed between 2 and 4 weeks after delivery, either at an in-person appointment or by means of a phone call and a provided email link.
The single-site study was designed as a parallel-group equivalence trial, to show noninferiority of one pain control regimen over the other. Women between the ages of 18 and 50 years were included if they had a cesarean delivery; both English- and Spanish-speaking women were enrolled.
Allowing for attrition and crossover, Dr. Dinis and her colleagues enrolled 85 patients per study arm to achieve sufficient statistical power to detect the difference needed. The investigators planned both an intention-to-treat and a per-protocol analysis in their registered clinical trial.
Postpartum pain assessments were not obtained for 12 patients in the nonopioid group, and 9 in the opioid group, leaving 73 and 76 patients in each group for the per-protocol analysis, respectively.
At baseline, patients were a mean 28 years old, and a little over a quarter (28%) were nulliparous. Participants were overall about half African American and 34%-40% Hispanic. Over half (62%-72%) received Medicaid; most women (62%-75%) had body mass indices of 30 kg/m2 or more.
The mean gestational age at delivery was a little more than 36 weeks, with about half of deliveries being the participant’s first cesarean delivery. About 90% of women had a Pfannenstiel skin incision, with a low transverse uterine incision.
Patients were aware of their allocation, and the study results aren’t applicable to women with opioid or benzodiazepine use disorder, she noted. However, the study was pragmatic, included all types of cesarean deliveries, and was adequately powered to detect “the smallest clinically significant difference.”
Dr. Dinis reported no outside sources of funding and no conflicts of interest.
SOURCE: Dinis J et al. Am J Obstet Gynecol. 2019 Jan;220(1):S34, Abstract 42.
LAS VEGAS – Women who had cesarean delivery and received a nonopioid pain control regimen at hospital discharge had lower pain scores by 4 weeks post partum than those who also received opioids, according to study results shared during a fellows session at the meeting presented by the Society for Maternal-Fetal Medicine.
At 2-4 weeks post partum, the mean pain score on a visual analog scale (VAS) was 12/100 mm for women on the nonopioid regimen, compared with 16/100 mm for women who received opioids, using an intention-to-treat analysis. The median pain score for those in the nonopioid arm was 0, compared with 6 for those in the opioid arm.
The findings surprised Jenifer Dinis, MD, a maternal-fetal medicine fellow at the University of Texas, Houston, and her collaborators, because they had hypothesized merely that the two groups would have similar pain scores 2-4 weeks after delivery.
Although women in the nonopioid arm were able to obtain a rescue hydrocodone prescription through the study, and some women obtained opioids from their private physician, they still used less than half as much opioid medication as women in the opioid arm (21 versus 43 morphine milligram equivalents, P less than .01).
However, women in the nonopioid arm did not use significantly more ibuprofen or acetaminophen, and there was no difference in patient satisfaction with the outpatient postpartum analgesic regimen between study arms. Somnolence was more common in the opioid arm (P = .03); no other medication side effects were significantly more common in one group than the other.
Overall, 22 of 76 (29%) women in the nonopioid arm took any opioids after discharge, compared with 59/81 (73%) in the opioid arm (P less than .01).
After cesarean delivery, the 170 participating women had an inpatient pain control regimen determined by their primary ob.gyn., Dr. Dinis said in her presentation. Patients were randomized 1:1 to their outpatient analgesia regimens on postoperative day 2 or 3, with appropriate prescriptions placed in patient charts. Participants received either a nonopioid regimen with prescriptions for 60 ibuprofen tablets (600 mg) and 60 acetaminophen tablets (325 mg), or to an opioid regimen that included ibuprofen plus hydrocodone/acetaminophen 5 (325 mg) 1-2 tablets every 4 hours.
Pain scores were assessed between 2 and 4 weeks after delivery, either at an in-person appointment or by means of a phone call and a provided email link.
The single-site study was designed as a parallel-group equivalence trial, to show noninferiority of one pain control regimen over the other. Women between the ages of 18 and 50 years were included if they had a cesarean delivery; both English- and Spanish-speaking women were enrolled.
Allowing for attrition and crossover, Dr. Dinis and her colleagues enrolled 85 patients per study arm to achieve sufficient statistical power to detect the difference needed. The investigators planned both an intention-to-treat and a per-protocol analysis in their registered clinical trial.
Postpartum pain assessments were not obtained for 12 patients in the nonopioid group, and 9 in the opioid group, leaving 73 and 76 patients in each group for the per-protocol analysis, respectively.
At baseline, patients were a mean 28 years old, and a little over a quarter (28%) were nulliparous. Participants were overall about half African American and 34%-40% Hispanic. Over half (62%-72%) received Medicaid; most women (62%-75%) had body mass indices of 30 kg/m2 or more.
The mean gestational age at delivery was a little more than 36 weeks, with about half of deliveries being the participant’s first cesarean delivery. About 90% of women had a Pfannenstiel skin incision, with a low transverse uterine incision.
Patients were aware of their allocation, and the study results aren’t applicable to women with opioid or benzodiazepine use disorder, she noted. However, the study was pragmatic, included all types of cesarean deliveries, and was adequately powered to detect “the smallest clinically significant difference.”
Dr. Dinis reported no outside sources of funding and no conflicts of interest.
SOURCE: Dinis J et al. Am J Obstet Gynecol. 2019 Jan;220(1):S34, Abstract 42.
LAS VEGAS – Women who had cesarean delivery and received a nonopioid pain control regimen at hospital discharge had lower pain scores by 4 weeks post partum than those who also received opioids, according to study results shared during a fellows session at the meeting presented by the Society for Maternal-Fetal Medicine.
At 2-4 weeks post partum, the mean pain score on a visual analog scale (VAS) was 12/100 mm for women on the nonopioid regimen, compared with 16/100 mm for women who received opioids, using an intention-to-treat analysis. The median pain score for those in the nonopioid arm was 0, compared with 6 for those in the opioid arm.
The findings surprised Jenifer Dinis, MD, a maternal-fetal medicine fellow at the University of Texas, Houston, and her collaborators, because they had hypothesized merely that the two groups would have similar pain scores 2-4 weeks after delivery.
Although women in the nonopioid arm were able to obtain a rescue hydrocodone prescription through the study, and some women obtained opioids from their private physician, they still used less than half as much opioid medication as women in the opioid arm (21 versus 43 morphine milligram equivalents, P less than .01).
However, women in the nonopioid arm did not use significantly more ibuprofen or acetaminophen, and there was no difference in patient satisfaction with the outpatient postpartum analgesic regimen between study arms. Somnolence was more common in the opioid arm (P = .03); no other medication side effects were significantly more common in one group than the other.
Overall, 22 of 76 (29%) women in the nonopioid arm took any opioids after discharge, compared with 59/81 (73%) in the opioid arm (P less than .01).
After cesarean delivery, the 170 participating women had an inpatient pain control regimen determined by their primary ob.gyn., Dr. Dinis said in her presentation. Patients were randomized 1:1 to their outpatient analgesia regimens on postoperative day 2 or 3, with appropriate prescriptions placed in patient charts. Participants received either a nonopioid regimen with prescriptions for 60 ibuprofen tablets (600 mg) and 60 acetaminophen tablets (325 mg), or to an opioid regimen that included ibuprofen plus hydrocodone/acetaminophen 5 (325 mg) 1-2 tablets every 4 hours.
Pain scores were assessed between 2 and 4 weeks after delivery, either at an in-person appointment or by means of a phone call and a provided email link.
The single-site study was designed as a parallel-group equivalence trial, to show noninferiority of one pain control regimen over the other. Women between the ages of 18 and 50 years were included if they had a cesarean delivery; both English- and Spanish-speaking women were enrolled.
Allowing for attrition and crossover, Dr. Dinis and her colleagues enrolled 85 patients per study arm to achieve sufficient statistical power to detect the difference needed. The investigators planned both an intention-to-treat and a per-protocol analysis in their registered clinical trial.
Postpartum pain assessments were not obtained for 12 patients in the nonopioid group, and 9 in the opioid group, leaving 73 and 76 patients in each group for the per-protocol analysis, respectively.
At baseline, patients were a mean 28 years old, and a little over a quarter (28%) were nulliparous. Participants were overall about half African American and 34%-40% Hispanic. Over half (62%-72%) received Medicaid; most women (62%-75%) had body mass indices of 30 kg/m2 or more.
The mean gestational age at delivery was a little more than 36 weeks, with about half of deliveries being the participant’s first cesarean delivery. About 90% of women had a Pfannenstiel skin incision, with a low transverse uterine incision.
Patients were aware of their allocation, and the study results aren’t applicable to women with opioid or benzodiazepine use disorder, she noted. However, the study was pragmatic, included all types of cesarean deliveries, and was adequately powered to detect “the smallest clinically significant difference.”
Dr. Dinis reported no outside sources of funding and no conflicts of interest.
SOURCE: Dinis J et al. Am J Obstet Gynecol. 2019 Jan;220(1):S34, Abstract 42.
REPORTING FROM THE PREGNANCY MEETING
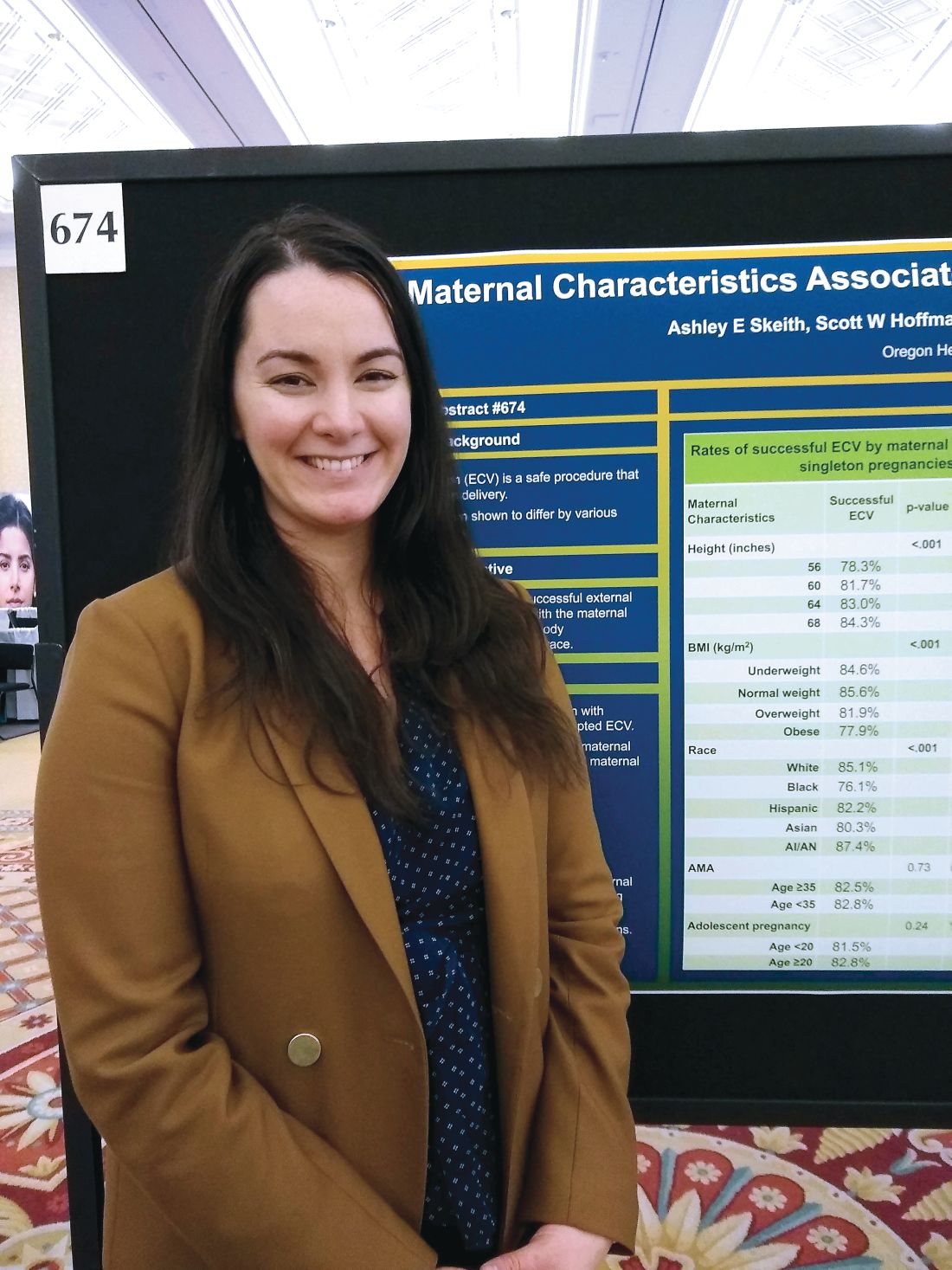
Successful external cephalic version more likely in taller, leaner women
LAS VEGAS – according to data shared in a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Race/ethnicity also had an impact on the likelihood that external cephalic version (ECV) would be successful.
In an interview, first author Ashley E. Skeith, a medical student at Oregon Health and Sciences University, Portland, said that various characteristics of a pregnancy may affect the success of ECV, but it wasn’t known which maternal characteristics might be associated with greater success of the maneuver.
She and her collaborators found that rates of success were high overall, but that 84% of women 68 inches or taller had successful ECVs, compared with 78% of women less than 60 inches tall. Rates were 82% and 83% for women 60-64 inches and 64-68 inches tall, respectively (adjusted odds ratio, 1.03; P less than .001).
The retrospective cohort study used data from 18,896 women who had singleton, breech, term gestations for whom ECV was attempted. Variables extracted from the medical record included maternal age, height, race, and prepregnancy body mass index (BMI).
For analysis, maternal BMI was grouped into four categories: underweight (BMI, less than 18.5 kg/m2), normal weight (BMI, 18.5-24.9 kg/m2), overweight (BMI, 25-29 kg/m2), and obese (BMI, greater than 30 kg/m2).
Women who were normal weight had the highest likelihood of a successful ECV, at 86%, followed by underweight women at 85%. Women who were overweight and obese had lower success rates, at 82% and 78%, respectively (aOR, 0.86; P less than .001).
Compared with white women, black women had an aOR of 0.60 for successful ECV (P less than .001). The aOR for successful ECV for Asian women was 0.71; for Hispanic women, the aOR was 0.82. American Indian and Alaska Native women were slightly more likely to have successful ECV than white women, but the difference was not significant after statistical adjustment.
Neither advanced maternal age (greater than 35 years) nor adolescent pregnancy were associated with decreased likelihood of successful ECV.
Potential confounders included maternal education level and insurance status, how much weight was gained during pregnancy, whether an epidural was administered, and whether the mother had diabetes. Multivariable regression analysis adjusted for these variables, said Ms. Skeith.
“External cephalic version is a safe procedure that reduces risk of cesarean delivery,” wrote Ms. Skeith and her colleagues. “Though fetal positioning and analgesia have been considered in the prediction of ECV success, [these] data [suggest] that maternal stature and race/ethnicity could be incorporated into potential prediction tools.”
Ms. Skeith reported no outside sources of funding or conflicts of interest.
SOURCE: Skeith AE et al. Am J Obstet Gynecol. 2019 Jan;220(1):S445-7, Abstract 674.
LAS VEGAS – according to data shared in a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Race/ethnicity also had an impact on the likelihood that external cephalic version (ECV) would be successful.
In an interview, first author Ashley E. Skeith, a medical student at Oregon Health and Sciences University, Portland, said that various characteristics of a pregnancy may affect the success of ECV, but it wasn’t known which maternal characteristics might be associated with greater success of the maneuver.
She and her collaborators found that rates of success were high overall, but that 84% of women 68 inches or taller had successful ECVs, compared with 78% of women less than 60 inches tall. Rates were 82% and 83% for women 60-64 inches and 64-68 inches tall, respectively (adjusted odds ratio, 1.03; P less than .001).
The retrospective cohort study used data from 18,896 women who had singleton, breech, term gestations for whom ECV was attempted. Variables extracted from the medical record included maternal age, height, race, and prepregnancy body mass index (BMI).
For analysis, maternal BMI was grouped into four categories: underweight (BMI, less than 18.5 kg/m2), normal weight (BMI, 18.5-24.9 kg/m2), overweight (BMI, 25-29 kg/m2), and obese (BMI, greater than 30 kg/m2).
Women who were normal weight had the highest likelihood of a successful ECV, at 86%, followed by underweight women at 85%. Women who were overweight and obese had lower success rates, at 82% and 78%, respectively (aOR, 0.86; P less than .001).
Compared with white women, black women had an aOR of 0.60 for successful ECV (P less than .001). The aOR for successful ECV for Asian women was 0.71; for Hispanic women, the aOR was 0.82. American Indian and Alaska Native women were slightly more likely to have successful ECV than white women, but the difference was not significant after statistical adjustment.
Neither advanced maternal age (greater than 35 years) nor adolescent pregnancy were associated with decreased likelihood of successful ECV.
Potential confounders included maternal education level and insurance status, how much weight was gained during pregnancy, whether an epidural was administered, and whether the mother had diabetes. Multivariable regression analysis adjusted for these variables, said Ms. Skeith.
“External cephalic version is a safe procedure that reduces risk of cesarean delivery,” wrote Ms. Skeith and her colleagues. “Though fetal positioning and analgesia have been considered in the prediction of ECV success, [these] data [suggest] that maternal stature and race/ethnicity could be incorporated into potential prediction tools.”
Ms. Skeith reported no outside sources of funding or conflicts of interest.
SOURCE: Skeith AE et al. Am J Obstet Gynecol. 2019 Jan;220(1):S445-7, Abstract 674.
LAS VEGAS – according to data shared in a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Race/ethnicity also had an impact on the likelihood that external cephalic version (ECV) would be successful.
In an interview, first author Ashley E. Skeith, a medical student at Oregon Health and Sciences University, Portland, said that various characteristics of a pregnancy may affect the success of ECV, but it wasn’t known which maternal characteristics might be associated with greater success of the maneuver.
She and her collaborators found that rates of success were high overall, but that 84% of women 68 inches or taller had successful ECVs, compared with 78% of women less than 60 inches tall. Rates were 82% and 83% for women 60-64 inches and 64-68 inches tall, respectively (adjusted odds ratio, 1.03; P less than .001).
The retrospective cohort study used data from 18,896 women who had singleton, breech, term gestations for whom ECV was attempted. Variables extracted from the medical record included maternal age, height, race, and prepregnancy body mass index (BMI).
For analysis, maternal BMI was grouped into four categories: underweight (BMI, less than 18.5 kg/m2), normal weight (BMI, 18.5-24.9 kg/m2), overweight (BMI, 25-29 kg/m2), and obese (BMI, greater than 30 kg/m2).
Women who were normal weight had the highest likelihood of a successful ECV, at 86%, followed by underweight women at 85%. Women who were overweight and obese had lower success rates, at 82% and 78%, respectively (aOR, 0.86; P less than .001).
Compared with white women, black women had an aOR of 0.60 for successful ECV (P less than .001). The aOR for successful ECV for Asian women was 0.71; for Hispanic women, the aOR was 0.82. American Indian and Alaska Native women were slightly more likely to have successful ECV than white women, but the difference was not significant after statistical adjustment.
Neither advanced maternal age (greater than 35 years) nor adolescent pregnancy were associated with decreased likelihood of successful ECV.
Potential confounders included maternal education level and insurance status, how much weight was gained during pregnancy, whether an epidural was administered, and whether the mother had diabetes. Multivariable regression analysis adjusted for these variables, said Ms. Skeith.
“External cephalic version is a safe procedure that reduces risk of cesarean delivery,” wrote Ms. Skeith and her colleagues. “Though fetal positioning and analgesia have been considered in the prediction of ECV success, [these] data [suggest] that maternal stature and race/ethnicity could be incorporated into potential prediction tools.”
Ms. Skeith reported no outside sources of funding or conflicts of interest.
SOURCE: Skeith AE et al. Am J Obstet Gynecol. 2019 Jan;220(1):S445-7, Abstract 674.
REPORTING FROM THE PREGNANCY MEETING
Knotless, absorbable sutures best staples for postcesarean skin closure
LAS VEGAS – compared with staples, in a single-site, retrospective study.
For women whose skin incisions were closed with knotless sutures, mean surgical time was 38 minutes; for women who received a staple closure, mean surgical time was 44 minutes (P less than .001). Also, fewer women whose incisions were closed with knotless sutures experienced surgical bleeding greater than 1,000 mL, compared with those who received staples (0.3% vs. 3.0%; P less than .001).
Two previous randomized, controlled trials comparing knotless sutures with staples for skin closure after cesarean delivery were small and had methodological limitations, Inna Bleicher, MD, said in an interview during a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Dr. Bleicher and her colleagues reviewed records from 2,173 elective cesarean deliveries over a period of 4 years. Absorbable, antibacterial, knotless sutures were used for closure for 1,172 women, while staples were used for the remaining 1,001 women.
Over the study period, Dr. Bleicher noted that there was a gradual transition from the use of staples to absorbable, knotless sutures, which also were increasingly used for the hysterotomy closure. She added that, in conversation with peers at Bnai-Zion Medical Center, Haifa, Israel, where she practices as an ob.gyn, she’s found that physicians find the sutures easy and quick to use, because the sutures are double ended, allowing the possibility for two operators to work together in wound closure.
The study’s primary outcome measure was the rate of postoperative infection, defined as postoperative white blood count greater than 18,000 per microliter and antimicrobial treatment. Secondary outcome measures included C-reactive protein levels, hospital readmission for infection related to the delivery, duration of surgery, and surgical blood loss estimated at 1,000 mL or more.
A higher proportion of women in the staple closure group than the knotless suture group required postsurgical antibiotic treatment (11% vs. 10%), but this difference didn’t reach statistical significance (P = .243).
There were no significant differences in the groups in terms of maternal age (about 32 years), or gestational age at delivery (about 39 weeks).
“Our results suggest that cesarean scar skin closure with antibacterial knotless sutures did not increase, and may even reduce, the rates of postoperative infection, morbidity, surgical blood loss, and may shorten operation time,” wrote Dr. Bleicher and her colleagues.
Dr. Bleicher reported no outside sources of funding and no conflicts of interest.
SOURCE: Bleicher I et al. Am J Obstet Gynecol. 2019 Jan. 220;1:S622, Abstract 966.
LAS VEGAS – compared with staples, in a single-site, retrospective study.
For women whose skin incisions were closed with knotless sutures, mean surgical time was 38 minutes; for women who received a staple closure, mean surgical time was 44 minutes (P less than .001). Also, fewer women whose incisions were closed with knotless sutures experienced surgical bleeding greater than 1,000 mL, compared with those who received staples (0.3% vs. 3.0%; P less than .001).
Two previous randomized, controlled trials comparing knotless sutures with staples for skin closure after cesarean delivery were small and had methodological limitations, Inna Bleicher, MD, said in an interview during a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Dr. Bleicher and her colleagues reviewed records from 2,173 elective cesarean deliveries over a period of 4 years. Absorbable, antibacterial, knotless sutures were used for closure for 1,172 women, while staples were used for the remaining 1,001 women.
Over the study period, Dr. Bleicher noted that there was a gradual transition from the use of staples to absorbable, knotless sutures, which also were increasingly used for the hysterotomy closure. She added that, in conversation with peers at Bnai-Zion Medical Center, Haifa, Israel, where she practices as an ob.gyn, she’s found that physicians find the sutures easy and quick to use, because the sutures are double ended, allowing the possibility for two operators to work together in wound closure.
The study’s primary outcome measure was the rate of postoperative infection, defined as postoperative white blood count greater than 18,000 per microliter and antimicrobial treatment. Secondary outcome measures included C-reactive protein levels, hospital readmission for infection related to the delivery, duration of surgery, and surgical blood loss estimated at 1,000 mL or more.
A higher proportion of women in the staple closure group than the knotless suture group required postsurgical antibiotic treatment (11% vs. 10%), but this difference didn’t reach statistical significance (P = .243).
There were no significant differences in the groups in terms of maternal age (about 32 years), or gestational age at delivery (about 39 weeks).
“Our results suggest that cesarean scar skin closure with antibacterial knotless sutures did not increase, and may even reduce, the rates of postoperative infection, morbidity, surgical blood loss, and may shorten operation time,” wrote Dr. Bleicher and her colleagues.
Dr. Bleicher reported no outside sources of funding and no conflicts of interest.
SOURCE: Bleicher I et al. Am J Obstet Gynecol. 2019 Jan. 220;1:S622, Abstract 966.
LAS VEGAS – compared with staples, in a single-site, retrospective study.
For women whose skin incisions were closed with knotless sutures, mean surgical time was 38 minutes; for women who received a staple closure, mean surgical time was 44 minutes (P less than .001). Also, fewer women whose incisions were closed with knotless sutures experienced surgical bleeding greater than 1,000 mL, compared with those who received staples (0.3% vs. 3.0%; P less than .001).
Two previous randomized, controlled trials comparing knotless sutures with staples for skin closure after cesarean delivery were small and had methodological limitations, Inna Bleicher, MD, said in an interview during a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Dr. Bleicher and her colleagues reviewed records from 2,173 elective cesarean deliveries over a period of 4 years. Absorbable, antibacterial, knotless sutures were used for closure for 1,172 women, while staples were used for the remaining 1,001 women.
Over the study period, Dr. Bleicher noted that there was a gradual transition from the use of staples to absorbable, knotless sutures, which also were increasingly used for the hysterotomy closure. She added that, in conversation with peers at Bnai-Zion Medical Center, Haifa, Israel, where she practices as an ob.gyn, she’s found that physicians find the sutures easy and quick to use, because the sutures are double ended, allowing the possibility for two operators to work together in wound closure.
The study’s primary outcome measure was the rate of postoperative infection, defined as postoperative white blood count greater than 18,000 per microliter and antimicrobial treatment. Secondary outcome measures included C-reactive protein levels, hospital readmission for infection related to the delivery, duration of surgery, and surgical blood loss estimated at 1,000 mL or more.
A higher proportion of women in the staple closure group than the knotless suture group required postsurgical antibiotic treatment (11% vs. 10%), but this difference didn’t reach statistical significance (P = .243).
There were no significant differences in the groups in terms of maternal age (about 32 years), or gestational age at delivery (about 39 weeks).
“Our results suggest that cesarean scar skin closure with antibacterial knotless sutures did not increase, and may even reduce, the rates of postoperative infection, morbidity, surgical blood loss, and may shorten operation time,” wrote Dr. Bleicher and her colleagues.
Dr. Bleicher reported no outside sources of funding and no conflicts of interest.
SOURCE: Bleicher I et al. Am J Obstet Gynecol. 2019 Jan. 220;1:S622, Abstract 966.
REPORTING FROM THE PREGNANCY MEETING
Tight intrapartum glucose control doesn’t improve neonatal outcomes
LAS VEGAS – There was no difference in first neonatal glucose level or glucose levels within the first 24 hours of life when women with gestational diabetes received strict, rather than liberalized, glucose management in labor.
In a study of 76 women with gestational diabetes mellitus (GDM), the mean first blood glucose level was 53 mg/dL for neonates born to the 38 mothers who received tight glucose control during labor; for those born to the 38 women who received liberalized control, mean first glucose level was 56 mg/dL (interquartile ranges, 22-85 mg/dL and 27-126 mg/dL, respectively; P = .56).
Secondary outcomes tracked in the study included the proportion of neonates whose glucose levels were low (defined as less than 40 mg/dL) at birth. This figure was identical in both groups, at 24%.
These findings ran counter to the hypothesis that Maureen Hamel, MD, and her colleagues at Brown University, Providence, R.I., had formulated – that neonates whose mothers had tight intrapartum glucose control would have lower rates of neonatal hypoglycemia than those born to women with liberalized intrapartum control.
Although the differences did not reach statistical significance, numerically more infants in the tight-control group required any intervention for hypoglycemia (45% vs. 32%; P = .35) or intravenous intervention for hypoglycemia (11% vs 0%; P = .35). Neonatal ICU admission was required for 13% of the tight-control neonates versus 3% of the liberalized-control group (P = .20).
“A protocol aimed at tight maternal glucose management in labor, compared to liberalized management, for women with GDM, did not result in a lower rate of neonatal hypoglycemia and was associated with mean neonatal glucose closer to hypoglycemia [40 mg/dL] in the first 24 hours of life,” said Dr. Hamel, discussing the findings of her award-winning abstract at the meeting presented by the Society for Maternal-Fetal Medicine.
Women were included if they were at least 18 years old with a singleton pregnancy and a diagnosis of gestational diabetes. Participants received care through a specialized program for pregnant women with diabetes; they were considered to have GDM if they had at least two abnormal values from a 100-g, 3-hour glucose tolerance test (GTT) or had a blood glucose reading of at least 200 mg/dL from a 1-hour 50-g GTT. About two-thirds of women required medical management of GDM; about 80% received labor induction at 39 weeks’ gestation.
At 36 weeks’ gestation, participants were block-randomized 1:1 to receive tight or liberalized intrapartum blood glucose control, with allocation unknown to both providers and patients until participants were admitted for delivery. Neonatal providers were blinded as to allocation throughout the admission. “In the tight glucose control group, point-of-care glucose was assessed hourly,” said Dr. Hamel. “Goal glucose levels were 70-100 [mg/dL], and treatment was initiated for a single maternal glucose greater than 100 and less than 60 [mg/dL].”
Those in the liberalized group had blood sugar checked every 4 hours in the absence of symptoms, with a goal blood glucose range of 70-120 mg/dL and treatment initiated for blood glucose over 120 or less than 60 mg/dL.
The increase in older women giving birth partly underlies the increase in GDM, said Dr. Hamel. By 35 years of age, about 15% of women will develop GDM, compared with under 6% for women giving birth between 20 and 24 years of age.
Neonatal hypoglycemia, with associated risks for neonatal ICU admission, seizures, and neurologic injury, is more common in women with GDM, said Dr. Hamel, a maternal-fetal medicine fellow.
There’s wide institutional and geographic variation in intrapartum maternal glucose management, said Dr. Hamel. Even within her own institution, blood sugar might be checked just once in labor, every 2 hours, or every hour, and the threshold for treatment might be set at a maternal blood glucose level over 100, 120, or even 200 mg/dL.
The study benefited from the fact that there was standardized antepartum GDM management in place and that 100% of outcome data were available. Also, the a priori sample size to detect significant between-group differences was obtained, and neonatal providers were blinded as to maternal glucose control strategy. Replication of the study should be both easy and feasible, said Dr. Hamel.
However, only very short-term outcomes were tracked, and the study was not powered to detect differences in such less-frequent neonatal outcomes as neonatal ICU admission.
“There is no benefit to tight maternal glucose control in labor among women with GDM,” concluded Dr. Hamel. “Our findings support glucose assessment every 4 hours, with intervention for blood glucose levels less than 60 or higher than 120 [mg/dL].”
Dr. Hamel reported no outside sources of funding and no conflicts of interest.
SOURCE: Hamel M et al. Am J Obstet Gynecol. 2019 Jan. 220;1:S36, Abstract 44.
LAS VEGAS – There was no difference in first neonatal glucose level or glucose levels within the first 24 hours of life when women with gestational diabetes received strict, rather than liberalized, glucose management in labor.
In a study of 76 women with gestational diabetes mellitus (GDM), the mean first blood glucose level was 53 mg/dL for neonates born to the 38 mothers who received tight glucose control during labor; for those born to the 38 women who received liberalized control, mean first glucose level was 56 mg/dL (interquartile ranges, 22-85 mg/dL and 27-126 mg/dL, respectively; P = .56).
Secondary outcomes tracked in the study included the proportion of neonates whose glucose levels were low (defined as less than 40 mg/dL) at birth. This figure was identical in both groups, at 24%.
These findings ran counter to the hypothesis that Maureen Hamel, MD, and her colleagues at Brown University, Providence, R.I., had formulated – that neonates whose mothers had tight intrapartum glucose control would have lower rates of neonatal hypoglycemia than those born to women with liberalized intrapartum control.
Although the differences did not reach statistical significance, numerically more infants in the tight-control group required any intervention for hypoglycemia (45% vs. 32%; P = .35) or intravenous intervention for hypoglycemia (11% vs 0%; P = .35). Neonatal ICU admission was required for 13% of the tight-control neonates versus 3% of the liberalized-control group (P = .20).
“A protocol aimed at tight maternal glucose management in labor, compared to liberalized management, for women with GDM, did not result in a lower rate of neonatal hypoglycemia and was associated with mean neonatal glucose closer to hypoglycemia [40 mg/dL] in the first 24 hours of life,” said Dr. Hamel, discussing the findings of her award-winning abstract at the meeting presented by the Society for Maternal-Fetal Medicine.
Women were included if they were at least 18 years old with a singleton pregnancy and a diagnosis of gestational diabetes. Participants received care through a specialized program for pregnant women with diabetes; they were considered to have GDM if they had at least two abnormal values from a 100-g, 3-hour glucose tolerance test (GTT) or had a blood glucose reading of at least 200 mg/dL from a 1-hour 50-g GTT. About two-thirds of women required medical management of GDM; about 80% received labor induction at 39 weeks’ gestation.
At 36 weeks’ gestation, participants were block-randomized 1:1 to receive tight or liberalized intrapartum blood glucose control, with allocation unknown to both providers and patients until participants were admitted for delivery. Neonatal providers were blinded as to allocation throughout the admission. “In the tight glucose control group, point-of-care glucose was assessed hourly,” said Dr. Hamel. “Goal glucose levels were 70-100 [mg/dL], and treatment was initiated for a single maternal glucose greater than 100 and less than 60 [mg/dL].”
Those in the liberalized group had blood sugar checked every 4 hours in the absence of symptoms, with a goal blood glucose range of 70-120 mg/dL and treatment initiated for blood glucose over 120 or less than 60 mg/dL.
The increase in older women giving birth partly underlies the increase in GDM, said Dr. Hamel. By 35 years of age, about 15% of women will develop GDM, compared with under 6% for women giving birth between 20 and 24 years of age.
Neonatal hypoglycemia, with associated risks for neonatal ICU admission, seizures, and neurologic injury, is more common in women with GDM, said Dr. Hamel, a maternal-fetal medicine fellow.
There’s wide institutional and geographic variation in intrapartum maternal glucose management, said Dr. Hamel. Even within her own institution, blood sugar might be checked just once in labor, every 2 hours, or every hour, and the threshold for treatment might be set at a maternal blood glucose level over 100, 120, or even 200 mg/dL.
The study benefited from the fact that there was standardized antepartum GDM management in place and that 100% of outcome data were available. Also, the a priori sample size to detect significant between-group differences was obtained, and neonatal providers were blinded as to maternal glucose control strategy. Replication of the study should be both easy and feasible, said Dr. Hamel.
However, only very short-term outcomes were tracked, and the study was not powered to detect differences in such less-frequent neonatal outcomes as neonatal ICU admission.
“There is no benefit to tight maternal glucose control in labor among women with GDM,” concluded Dr. Hamel. “Our findings support glucose assessment every 4 hours, with intervention for blood glucose levels less than 60 or higher than 120 [mg/dL].”
Dr. Hamel reported no outside sources of funding and no conflicts of interest.
SOURCE: Hamel M et al. Am J Obstet Gynecol. 2019 Jan. 220;1:S36, Abstract 44.
LAS VEGAS – There was no difference in first neonatal glucose level or glucose levels within the first 24 hours of life when women with gestational diabetes received strict, rather than liberalized, glucose management in labor.
In a study of 76 women with gestational diabetes mellitus (GDM), the mean first blood glucose level was 53 mg/dL for neonates born to the 38 mothers who received tight glucose control during labor; for those born to the 38 women who received liberalized control, mean first glucose level was 56 mg/dL (interquartile ranges, 22-85 mg/dL and 27-126 mg/dL, respectively; P = .56).
Secondary outcomes tracked in the study included the proportion of neonates whose glucose levels were low (defined as less than 40 mg/dL) at birth. This figure was identical in both groups, at 24%.
These findings ran counter to the hypothesis that Maureen Hamel, MD, and her colleagues at Brown University, Providence, R.I., had formulated – that neonates whose mothers had tight intrapartum glucose control would have lower rates of neonatal hypoglycemia than those born to women with liberalized intrapartum control.
Although the differences did not reach statistical significance, numerically more infants in the tight-control group required any intervention for hypoglycemia (45% vs. 32%; P = .35) or intravenous intervention for hypoglycemia (11% vs 0%; P = .35). Neonatal ICU admission was required for 13% of the tight-control neonates versus 3% of the liberalized-control group (P = .20).
“A protocol aimed at tight maternal glucose management in labor, compared to liberalized management, for women with GDM, did not result in a lower rate of neonatal hypoglycemia and was associated with mean neonatal glucose closer to hypoglycemia [40 mg/dL] in the first 24 hours of life,” said Dr. Hamel, discussing the findings of her award-winning abstract at the meeting presented by the Society for Maternal-Fetal Medicine.
Women were included if they were at least 18 years old with a singleton pregnancy and a diagnosis of gestational diabetes. Participants received care through a specialized program for pregnant women with diabetes; they were considered to have GDM if they had at least two abnormal values from a 100-g, 3-hour glucose tolerance test (GTT) or had a blood glucose reading of at least 200 mg/dL from a 1-hour 50-g GTT. About two-thirds of women required medical management of GDM; about 80% received labor induction at 39 weeks’ gestation.
At 36 weeks’ gestation, participants were block-randomized 1:1 to receive tight or liberalized intrapartum blood glucose control, with allocation unknown to both providers and patients until participants were admitted for delivery. Neonatal providers were blinded as to allocation throughout the admission. “In the tight glucose control group, point-of-care glucose was assessed hourly,” said Dr. Hamel. “Goal glucose levels were 70-100 [mg/dL], and treatment was initiated for a single maternal glucose greater than 100 and less than 60 [mg/dL].”
Those in the liberalized group had blood sugar checked every 4 hours in the absence of symptoms, with a goal blood glucose range of 70-120 mg/dL and treatment initiated for blood glucose over 120 or less than 60 mg/dL.
The increase in older women giving birth partly underlies the increase in GDM, said Dr. Hamel. By 35 years of age, about 15% of women will develop GDM, compared with under 6% for women giving birth between 20 and 24 years of age.
Neonatal hypoglycemia, with associated risks for neonatal ICU admission, seizures, and neurologic injury, is more common in women with GDM, said Dr. Hamel, a maternal-fetal medicine fellow.
There’s wide institutional and geographic variation in intrapartum maternal glucose management, said Dr. Hamel. Even within her own institution, blood sugar might be checked just once in labor, every 2 hours, or every hour, and the threshold for treatment might be set at a maternal blood glucose level over 100, 120, or even 200 mg/dL.
The study benefited from the fact that there was standardized antepartum GDM management in place and that 100% of outcome data were available. Also, the a priori sample size to detect significant between-group differences was obtained, and neonatal providers were blinded as to maternal glucose control strategy. Replication of the study should be both easy and feasible, said Dr. Hamel.
However, only very short-term outcomes were tracked, and the study was not powered to detect differences in such less-frequent neonatal outcomes as neonatal ICU admission.
“There is no benefit to tight maternal glucose control in labor among women with GDM,” concluded Dr. Hamel. “Our findings support glucose assessment every 4 hours, with intervention for blood glucose levels less than 60 or higher than 120 [mg/dL].”
Dr. Hamel reported no outside sources of funding and no conflicts of interest.
SOURCE: Hamel M et al. Am J Obstet Gynecol. 2019 Jan. 220;1:S36, Abstract 44.
REPORTING FROM THE PREGNANCY MEETING
Texting improves postpregnancy hypertension monitoring in black women
LAS VEGAS – Adi Hirshberg, MD, reported at the Pregnancy Meeting.
The text messaging system increased the compliance rate to 93%, compared with just 30% of those asked to return to the office after hospital discharge. Just as importantly, it completely erased racial disparity in compliance rates, compared with white women, with more than 90% of both groups complying, said Dr. Hirshberg of the University of Pennsylvania, Philadelphia.
“Our study shows that text-based monitoring eliminated the observed racial disparity in postpregnancy hypertension care,” she said at the meeting sponsored by the Society for Maternal-Fetal Medicine. “Using texts as a standard of care would have likely led to medication initiation or adjustment for an additional 20% or more women who missed an office visit. This is an innovative way to equally engage all women in the postpregnancy period.”
Dr. Hirshberg presented a preplanned subanalysis of the Remote Surveillance of Hypertension (TextBP) trial, published last year (BMJ Qual Saf. 2018;27:871-7). The publication gave overall data; this analysis broke results down by race.
TextBP equally randomized 206 postpartum women with pregnancy-induced hypertension to the usual practice of office-based BP monitoring, or to 2 weeks of text-based surveillance using a home BP cuff. It was open to all women with pregnancy-related hypertension who delivered in the Hospital of the University of Pennsylvania. Hypertension classes included gestational hypertension, preeclampsia, chronic hypertension with superimposed preeclampsia, and HELLP syndrome before or during the delivery admission. Women were randomized to usual care or to an office-based BP check within the first postpartum week.
The texting platform was developed through Way to Health, a web-based platform within the institution, with secure technological infrastructure. A starting introductory text message was sent by the Way to Health platform to the phone number provided on day of discharge.
Patients received reminders to text message their blood pressure twice daily for 2 weeks post partum, starting on the day after discharge. If the patient reported a systolic BP of more than 160 mm Hg or diastolic more than 110 mm Hg, the clinician received an alert.
The overall results showed that significantly more women in the texting group reported their blood pressure (92% vs. 44%), compared with the controls. Almost everyone in the texting group (84%) met the established criteria for BP measurement.
Dr. Hirshberg and her colleagues wanted to zero in on black women, to discover if the text reminders could help boost their compliance. This is important for a couple of reasons, she said. For one thing, black women face a higher baseline risk of hypertensive disorders and cardiovascular disease, both in general and during and after pregnancy. Second, “for every 100 black women who require postpartum hypertension surveillance, only about a third are likely to attended an office visit after discharge,” leaving them vulnerable to potentially preventable complications of hypertension.
Even in the original analysis, return rates for postpregnancy BP checks were low in both groups and, in fact, seemed to be declining over several years. In 2012, 56% of nonblack and 33% of black women returned for their checks. By 2014, that number had declined to 34% and 20%. The numbers parallel the increasing disparity in U.S. maternal death rate between black women and nonblack women. From 1989 to 2013, the death rate for black mothers doubled, jumping from 20 to 40 deaths per 100,000 live births. During the same period, the death rate for nonblack mothers increased from about 8 to about 11 per 10,000. Dr. Hirshberg said.
In the subanalysis, the primary outcomes were the percentage of patients in whom a blood pressure was obtained in the first 10 days following discharge. In the control office visit group, about 33% of black women had a measurement, compared with 70% of nonblack women – a significant difference. Text messaging, however, completely eliminated the disparity. In the texting group, 91% of nonblack women and 93% of black women had a BP measurement.
There were no hypertension readmissions in the texting arm; there were four in the office-visit arm, three of which occurred in black women.
“This suggests that the traditional office-based follow-up may have resulted in missed opportunities to start an antihypertensive in about 10 of the 55 women who missed their office visit,” Dr. Hirshberg said, adding that “these kinds of early interventions can reduce maternal morbidity and mortality and increase overall health in all.”
She reported no relevant financial disclosures.
SOURCE: Hirshberg A et al. Am J Obstet Gynecol. 2019 Jan;220(1):S6, Abstract 7.
LAS VEGAS – Adi Hirshberg, MD, reported at the Pregnancy Meeting.
The text messaging system increased the compliance rate to 93%, compared with just 30% of those asked to return to the office after hospital discharge. Just as importantly, it completely erased racial disparity in compliance rates, compared with white women, with more than 90% of both groups complying, said Dr. Hirshberg of the University of Pennsylvania, Philadelphia.
“Our study shows that text-based monitoring eliminated the observed racial disparity in postpregnancy hypertension care,” she said at the meeting sponsored by the Society for Maternal-Fetal Medicine. “Using texts as a standard of care would have likely led to medication initiation or adjustment for an additional 20% or more women who missed an office visit. This is an innovative way to equally engage all women in the postpregnancy period.”
Dr. Hirshberg presented a preplanned subanalysis of the Remote Surveillance of Hypertension (TextBP) trial, published last year (BMJ Qual Saf. 2018;27:871-7). The publication gave overall data; this analysis broke results down by race.
TextBP equally randomized 206 postpartum women with pregnancy-induced hypertension to the usual practice of office-based BP monitoring, or to 2 weeks of text-based surveillance using a home BP cuff. It was open to all women with pregnancy-related hypertension who delivered in the Hospital of the University of Pennsylvania. Hypertension classes included gestational hypertension, preeclampsia, chronic hypertension with superimposed preeclampsia, and HELLP syndrome before or during the delivery admission. Women were randomized to usual care or to an office-based BP check within the first postpartum week.
The texting platform was developed through Way to Health, a web-based platform within the institution, with secure technological infrastructure. A starting introductory text message was sent by the Way to Health platform to the phone number provided on day of discharge.
Patients received reminders to text message their blood pressure twice daily for 2 weeks post partum, starting on the day after discharge. If the patient reported a systolic BP of more than 160 mm Hg or diastolic more than 110 mm Hg, the clinician received an alert.
The overall results showed that significantly more women in the texting group reported their blood pressure (92% vs. 44%), compared with the controls. Almost everyone in the texting group (84%) met the established criteria for BP measurement.
Dr. Hirshberg and her colleagues wanted to zero in on black women, to discover if the text reminders could help boost their compliance. This is important for a couple of reasons, she said. For one thing, black women face a higher baseline risk of hypertensive disorders and cardiovascular disease, both in general and during and after pregnancy. Second, “for every 100 black women who require postpartum hypertension surveillance, only about a third are likely to attended an office visit after discharge,” leaving them vulnerable to potentially preventable complications of hypertension.
Even in the original analysis, return rates for postpregnancy BP checks were low in both groups and, in fact, seemed to be declining over several years. In 2012, 56% of nonblack and 33% of black women returned for their checks. By 2014, that number had declined to 34% and 20%. The numbers parallel the increasing disparity in U.S. maternal death rate between black women and nonblack women. From 1989 to 2013, the death rate for black mothers doubled, jumping from 20 to 40 deaths per 100,000 live births. During the same period, the death rate for nonblack mothers increased from about 8 to about 11 per 10,000. Dr. Hirshberg said.
In the subanalysis, the primary outcomes were the percentage of patients in whom a blood pressure was obtained in the first 10 days following discharge. In the control office visit group, about 33% of black women had a measurement, compared with 70% of nonblack women – a significant difference. Text messaging, however, completely eliminated the disparity. In the texting group, 91% of nonblack women and 93% of black women had a BP measurement.
There were no hypertension readmissions in the texting arm; there were four in the office-visit arm, three of which occurred in black women.
“This suggests that the traditional office-based follow-up may have resulted in missed opportunities to start an antihypertensive in about 10 of the 55 women who missed their office visit,” Dr. Hirshberg said, adding that “these kinds of early interventions can reduce maternal morbidity and mortality and increase overall health in all.”
She reported no relevant financial disclosures.
SOURCE: Hirshberg A et al. Am J Obstet Gynecol. 2019 Jan;220(1):S6, Abstract 7.
LAS VEGAS – Adi Hirshberg, MD, reported at the Pregnancy Meeting.
The text messaging system increased the compliance rate to 93%, compared with just 30% of those asked to return to the office after hospital discharge. Just as importantly, it completely erased racial disparity in compliance rates, compared with white women, with more than 90% of both groups complying, said Dr. Hirshberg of the University of Pennsylvania, Philadelphia.
“Our study shows that text-based monitoring eliminated the observed racial disparity in postpregnancy hypertension care,” she said at the meeting sponsored by the Society for Maternal-Fetal Medicine. “Using texts as a standard of care would have likely led to medication initiation or adjustment for an additional 20% or more women who missed an office visit. This is an innovative way to equally engage all women in the postpregnancy period.”
Dr. Hirshberg presented a preplanned subanalysis of the Remote Surveillance of Hypertension (TextBP) trial, published last year (BMJ Qual Saf. 2018;27:871-7). The publication gave overall data; this analysis broke results down by race.
TextBP equally randomized 206 postpartum women with pregnancy-induced hypertension to the usual practice of office-based BP monitoring, or to 2 weeks of text-based surveillance using a home BP cuff. It was open to all women with pregnancy-related hypertension who delivered in the Hospital of the University of Pennsylvania. Hypertension classes included gestational hypertension, preeclampsia, chronic hypertension with superimposed preeclampsia, and HELLP syndrome before or during the delivery admission. Women were randomized to usual care or to an office-based BP check within the first postpartum week.
The texting platform was developed through Way to Health, a web-based platform within the institution, with secure technological infrastructure. A starting introductory text message was sent by the Way to Health platform to the phone number provided on day of discharge.
Patients received reminders to text message their blood pressure twice daily for 2 weeks post partum, starting on the day after discharge. If the patient reported a systolic BP of more than 160 mm Hg or diastolic more than 110 mm Hg, the clinician received an alert.
The overall results showed that significantly more women in the texting group reported their blood pressure (92% vs. 44%), compared with the controls. Almost everyone in the texting group (84%) met the established criteria for BP measurement.
Dr. Hirshberg and her colleagues wanted to zero in on black women, to discover if the text reminders could help boost their compliance. This is important for a couple of reasons, she said. For one thing, black women face a higher baseline risk of hypertensive disorders and cardiovascular disease, both in general and during and after pregnancy. Second, “for every 100 black women who require postpartum hypertension surveillance, only about a third are likely to attended an office visit after discharge,” leaving them vulnerable to potentially preventable complications of hypertension.
Even in the original analysis, return rates for postpregnancy BP checks were low in both groups and, in fact, seemed to be declining over several years. In 2012, 56% of nonblack and 33% of black women returned for their checks. By 2014, that number had declined to 34% and 20%. The numbers parallel the increasing disparity in U.S. maternal death rate between black women and nonblack women. From 1989 to 2013, the death rate for black mothers doubled, jumping from 20 to 40 deaths per 100,000 live births. During the same period, the death rate for nonblack mothers increased from about 8 to about 11 per 10,000. Dr. Hirshberg said.
In the subanalysis, the primary outcomes were the percentage of patients in whom a blood pressure was obtained in the first 10 days following discharge. In the control office visit group, about 33% of black women had a measurement, compared with 70% of nonblack women – a significant difference. Text messaging, however, completely eliminated the disparity. In the texting group, 91% of nonblack women and 93% of black women had a BP measurement.
There were no hypertension readmissions in the texting arm; there were four in the office-visit arm, three of which occurred in black women.
“This suggests that the traditional office-based follow-up may have resulted in missed opportunities to start an antihypertensive in about 10 of the 55 women who missed their office visit,” Dr. Hirshberg said, adding that “these kinds of early interventions can reduce maternal morbidity and mortality and increase overall health in all.”
She reported no relevant financial disclosures.
SOURCE: Hirshberg A et al. Am J Obstet Gynecol. 2019 Jan;220(1):S6, Abstract 7.
REPORTING FROM THE PREGNANCY MEETING
Delayed cord clamping didn’t drop maternal hemoglobin in term cesarean deliveries
LAS VEGAS – according to a recent study.
The change in maternal hemoglobin from preoperative level to postoperative day 1, the study’s primary outcome measure, was not significantly different whether the umbilical cord was clamped within 15 seconds of delivery or clamping was delayed for 1 minute.
For the 56 women who received immediate cord clamping, hemoglobin dropped a mean 1.78 g/dL; for the 57 women who received delayed cord clamping, the drop was 1.85 g/dL (P = .69). Mean estimated blood loss for the delayed clamping group was numerically higher at 884 mL, compared with 830 mL for the immediate clamping group, but this was not a statistically significant difference (P = .13)
However, the practice did result in significantly greater neonatal hemoglobin measured at 24-72 hours post delivery. Hemoglobin data were available for 90 infants, or about 80% of participants. For the 44 infants in the immediate clamping group, mean hemoglobin was 16.4 g/dL; for the delayed clamping group, the figure was 18.1 g/dL (P less than .01).
Although delayed cord clamping has clear benefits to the neonate, whether the practice adversely affects women undergoing cesarean was not clear, said Stephanie Purisch, MD, who discussed the findings of the two-site, randomized, clinical trial during a fellows research session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“Maternal outcomes have not been a focus of research” in the cord clamping literature, said Dr. Purisch, from Columbia University, New York. A 2013 Cochrane review found that delayed cord clamping did not change postpartum hemoglobin levels or increase blood loss or the need for transfusion. However, she said, the review included only healthy women who expected a vaginal delivery, so cesarean deliveries were undersampled in the data.
Of the 3,911 deliveries included in all prior randomized, controlled trials of delayed cord clamping, just 87, or 2.2%, were cesarean deliveries, she said. In cesarean deliveries, mean blood loss is double that of vaginal deliveries. Delayed clamping could further increase bleeding because the hysterotomy closure is delayed, said Dr. Purisch, so the question of safety in cesarean deliveries is clinically important.
Faced with this knowledge gap, Dr. Purisch and her colleagues constructed a prospective, randomized, controlled trial of delayed cord clamping in cesarean delivery at term, with the hypothesis that maternal blood loss would be increased by the practice.
Patients were eligible if they had singleton gestations with cesarean deliveries scheduled at 37 weeks’ gestation or more. Patients with known placentation problems, significant maternal or known fetal anemia, maternal bleeding disorders, and preeclampsia were excluded. The study also did not include pregnancies with known fetal anomalies or intrauterine growth retardation, or those in which cord blood banking was planned or the mother would refuse blood products.
In an intention-to-treat analysis, Dr. Purisch and her colleagues randomly assigned participants 1:1 to immediate cord clamping, defined as clamping the cord by 15 seconds after delivery, or delayed cord clamping, in which the umbilical cord was clamped 1 minute after delivery.
Oxytocin was routinely administered to each group on delivery, and there was no umbilical cord milking in either group. For the delayed-clamping group, the infant was kept at the level of the placenta and tended by the pediatric team during the minute before clamping. Dr. Purisch explained that cord clamping was performed before 60 seconds in the intervention group if needed for neonatal resuscitation.
Participants were similar in the two study arms, with a median gestational age of 39.1 weeks at delivery. Most women (60%-64%) had one prior cesarean delivery, with about a quarter having two or more prior cesarean deliveries. Preoperative maternal hemoglobin was 11.6-12.0 g/dL. About 41% of participants were Hispanic, and the median prepregnancy body mass index for participants was about 27 kg/m2.
Looking at secondary outcome measures, there was no difference in rates of postpartum hemorrhage or uterotonic administration between the two groups (P = .99 for both). Hemoglobin levels at postoperative day 1 were numerically higher for the delayed cord clamping group, but the difference wasn’t significant (10.2 vs. 9.8 g/dL; P = .18). Just two women, both in the immediate cord clamping group, required blood transfusions.
Additional neonatal secondary outcome measures included birth weight, Apgar scores at 1 and 5 minutes, the need for phototherapy for jaundice, and umbilical cord artery pH. There were no between-group differences except that umbilical cord artery pH was slightly lower in the delayed group (7.2 vs. 7.3; P = .04).
“Delayed cord clamping is not associated with increased maternal blood loss … but it does achieve higher neonatal hemoglobin levels at 24-72 hours of life,” said Dr. Purisch. “These results provide support for the application of current [American College of Obstetricians and Gynecologists] recommendations to women planned for cesarean delivery.”
The study was funded by the Columbia Maternal-Fetal Medicine Fellow Research Fund. Dr. Purisch reported no conflicts of interest.
SOURCE: Purisch, S. et al. Am J Obstet Gynecol. 2019 Jan;220(1):S37-38, Abstract 47.
LAS VEGAS – according to a recent study.
The change in maternal hemoglobin from preoperative level to postoperative day 1, the study’s primary outcome measure, was not significantly different whether the umbilical cord was clamped within 15 seconds of delivery or clamping was delayed for 1 minute.
For the 56 women who received immediate cord clamping, hemoglobin dropped a mean 1.78 g/dL; for the 57 women who received delayed cord clamping, the drop was 1.85 g/dL (P = .69). Mean estimated blood loss for the delayed clamping group was numerically higher at 884 mL, compared with 830 mL for the immediate clamping group, but this was not a statistically significant difference (P = .13)
However, the practice did result in significantly greater neonatal hemoglobin measured at 24-72 hours post delivery. Hemoglobin data were available for 90 infants, or about 80% of participants. For the 44 infants in the immediate clamping group, mean hemoglobin was 16.4 g/dL; for the delayed clamping group, the figure was 18.1 g/dL (P less than .01).
Although delayed cord clamping has clear benefits to the neonate, whether the practice adversely affects women undergoing cesarean was not clear, said Stephanie Purisch, MD, who discussed the findings of the two-site, randomized, clinical trial during a fellows research session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“Maternal outcomes have not been a focus of research” in the cord clamping literature, said Dr. Purisch, from Columbia University, New York. A 2013 Cochrane review found that delayed cord clamping did not change postpartum hemoglobin levels or increase blood loss or the need for transfusion. However, she said, the review included only healthy women who expected a vaginal delivery, so cesarean deliveries were undersampled in the data.
Of the 3,911 deliveries included in all prior randomized, controlled trials of delayed cord clamping, just 87, or 2.2%, were cesarean deliveries, she said. In cesarean deliveries, mean blood loss is double that of vaginal deliveries. Delayed clamping could further increase bleeding because the hysterotomy closure is delayed, said Dr. Purisch, so the question of safety in cesarean deliveries is clinically important.
Faced with this knowledge gap, Dr. Purisch and her colleagues constructed a prospective, randomized, controlled trial of delayed cord clamping in cesarean delivery at term, with the hypothesis that maternal blood loss would be increased by the practice.
Patients were eligible if they had singleton gestations with cesarean deliveries scheduled at 37 weeks’ gestation or more. Patients with known placentation problems, significant maternal or known fetal anemia, maternal bleeding disorders, and preeclampsia were excluded. The study also did not include pregnancies with known fetal anomalies or intrauterine growth retardation, or those in which cord blood banking was planned or the mother would refuse blood products.
In an intention-to-treat analysis, Dr. Purisch and her colleagues randomly assigned participants 1:1 to immediate cord clamping, defined as clamping the cord by 15 seconds after delivery, or delayed cord clamping, in which the umbilical cord was clamped 1 minute after delivery.
Oxytocin was routinely administered to each group on delivery, and there was no umbilical cord milking in either group. For the delayed-clamping group, the infant was kept at the level of the placenta and tended by the pediatric team during the minute before clamping. Dr. Purisch explained that cord clamping was performed before 60 seconds in the intervention group if needed for neonatal resuscitation.
Participants were similar in the two study arms, with a median gestational age of 39.1 weeks at delivery. Most women (60%-64%) had one prior cesarean delivery, with about a quarter having two or more prior cesarean deliveries. Preoperative maternal hemoglobin was 11.6-12.0 g/dL. About 41% of participants were Hispanic, and the median prepregnancy body mass index for participants was about 27 kg/m2.
Looking at secondary outcome measures, there was no difference in rates of postpartum hemorrhage or uterotonic administration between the two groups (P = .99 for both). Hemoglobin levels at postoperative day 1 were numerically higher for the delayed cord clamping group, but the difference wasn’t significant (10.2 vs. 9.8 g/dL; P = .18). Just two women, both in the immediate cord clamping group, required blood transfusions.
Additional neonatal secondary outcome measures included birth weight, Apgar scores at 1 and 5 minutes, the need for phototherapy for jaundice, and umbilical cord artery pH. There were no between-group differences except that umbilical cord artery pH was slightly lower in the delayed group (7.2 vs. 7.3; P = .04).
“Delayed cord clamping is not associated with increased maternal blood loss … but it does achieve higher neonatal hemoglobin levels at 24-72 hours of life,” said Dr. Purisch. “These results provide support for the application of current [American College of Obstetricians and Gynecologists] recommendations to women planned for cesarean delivery.”
The study was funded by the Columbia Maternal-Fetal Medicine Fellow Research Fund. Dr. Purisch reported no conflicts of interest.
SOURCE: Purisch, S. et al. Am J Obstet Gynecol. 2019 Jan;220(1):S37-38, Abstract 47.
LAS VEGAS – according to a recent study.
The change in maternal hemoglobin from preoperative level to postoperative day 1, the study’s primary outcome measure, was not significantly different whether the umbilical cord was clamped within 15 seconds of delivery or clamping was delayed for 1 minute.
For the 56 women who received immediate cord clamping, hemoglobin dropped a mean 1.78 g/dL; for the 57 women who received delayed cord clamping, the drop was 1.85 g/dL (P = .69). Mean estimated blood loss for the delayed clamping group was numerically higher at 884 mL, compared with 830 mL for the immediate clamping group, but this was not a statistically significant difference (P = .13)
However, the practice did result in significantly greater neonatal hemoglobin measured at 24-72 hours post delivery. Hemoglobin data were available for 90 infants, or about 80% of participants. For the 44 infants in the immediate clamping group, mean hemoglobin was 16.4 g/dL; for the delayed clamping group, the figure was 18.1 g/dL (P less than .01).
Although delayed cord clamping has clear benefits to the neonate, whether the practice adversely affects women undergoing cesarean was not clear, said Stephanie Purisch, MD, who discussed the findings of the two-site, randomized, clinical trial during a fellows research session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“Maternal outcomes have not been a focus of research” in the cord clamping literature, said Dr. Purisch, from Columbia University, New York. A 2013 Cochrane review found that delayed cord clamping did not change postpartum hemoglobin levels or increase blood loss or the need for transfusion. However, she said, the review included only healthy women who expected a vaginal delivery, so cesarean deliveries were undersampled in the data.
Of the 3,911 deliveries included in all prior randomized, controlled trials of delayed cord clamping, just 87, or 2.2%, were cesarean deliveries, she said. In cesarean deliveries, mean blood loss is double that of vaginal deliveries. Delayed clamping could further increase bleeding because the hysterotomy closure is delayed, said Dr. Purisch, so the question of safety in cesarean deliveries is clinically important.
Faced with this knowledge gap, Dr. Purisch and her colleagues constructed a prospective, randomized, controlled trial of delayed cord clamping in cesarean delivery at term, with the hypothesis that maternal blood loss would be increased by the practice.
Patients were eligible if they had singleton gestations with cesarean deliveries scheduled at 37 weeks’ gestation or more. Patients with known placentation problems, significant maternal or known fetal anemia, maternal bleeding disorders, and preeclampsia were excluded. The study also did not include pregnancies with known fetal anomalies or intrauterine growth retardation, or those in which cord blood banking was planned or the mother would refuse blood products.
In an intention-to-treat analysis, Dr. Purisch and her colleagues randomly assigned participants 1:1 to immediate cord clamping, defined as clamping the cord by 15 seconds after delivery, or delayed cord clamping, in which the umbilical cord was clamped 1 minute after delivery.
Oxytocin was routinely administered to each group on delivery, and there was no umbilical cord milking in either group. For the delayed-clamping group, the infant was kept at the level of the placenta and tended by the pediatric team during the minute before clamping. Dr. Purisch explained that cord clamping was performed before 60 seconds in the intervention group if needed for neonatal resuscitation.
Participants were similar in the two study arms, with a median gestational age of 39.1 weeks at delivery. Most women (60%-64%) had one prior cesarean delivery, with about a quarter having two or more prior cesarean deliveries. Preoperative maternal hemoglobin was 11.6-12.0 g/dL. About 41% of participants were Hispanic, and the median prepregnancy body mass index for participants was about 27 kg/m2.
Looking at secondary outcome measures, there was no difference in rates of postpartum hemorrhage or uterotonic administration between the two groups (P = .99 for both). Hemoglobin levels at postoperative day 1 were numerically higher for the delayed cord clamping group, but the difference wasn’t significant (10.2 vs. 9.8 g/dL; P = .18). Just two women, both in the immediate cord clamping group, required blood transfusions.
Additional neonatal secondary outcome measures included birth weight, Apgar scores at 1 and 5 minutes, the need for phototherapy for jaundice, and umbilical cord artery pH. There were no between-group differences except that umbilical cord artery pH was slightly lower in the delayed group (7.2 vs. 7.3; P = .04).
“Delayed cord clamping is not associated with increased maternal blood loss … but it does achieve higher neonatal hemoglobin levels at 24-72 hours of life,” said Dr. Purisch. “These results provide support for the application of current [American College of Obstetricians and Gynecologists] recommendations to women planned for cesarean delivery.”
The study was funded by the Columbia Maternal-Fetal Medicine Fellow Research Fund. Dr. Purisch reported no conflicts of interest.
SOURCE: Purisch, S. et al. Am J Obstet Gynecol. 2019 Jan;220(1):S37-38, Abstract 47.
REPORTING FROM THE PREGNANCY MEETING
Dental device borrowed from sports world no help in pushing
LAS VEGAS –
In a randomized, controlled trial of 346 nulliparous women, the device, adapted from a design used in athletics, made no difference in the duration of the second stage of labor overall or in passive descent or active pushing time. The findings were presented on behalf of first author Eric Bergh, MD, by Patricia Rekawek, MD, at a fellows abstract session at the meeting sponsored by the Society for Maternal-Fetal Medicine. Dr. Rekawek and Dr. Bergh are maternal-fetal medicine fellows at the Icahn School of Medicine at Mount Sinai, New York.
The dental support device (DSD) was actually used by 128 (74%) of the patients who were randomized to DSD usage. Of these patients, two thirds (n = 85) used the device for all second stage contractions. About one quarter (27%; n = 35) used it less than half the time, and a small minority (6%; n = 8) used it more than half the time but not for all pushing, noted Dr. Rekawek.
Most women (61%) who used the device agreed or strongly agreed that it was helpful. Most also found it comfortable (67%), and would use it again in a future delivery (61%). Having a custom-fit DSD, or spending more time practicing before labor, might help with efficacy in shortening the second stage of labor and merits study, the investigators said.
Reducing time spent in the second stage of labor could benefit both mother and neonate because “a prolonged second stage of labor is associated with multiple maternal and neonatal complications,” including increased risk for chorioamnionitis, neonatal sepsis, low umbilical artery pH, shoulder dystocia, and third- and fourth-degree lacerations, said Dr. Rekawek.
In athletics, a DSD “raises the vertical dimension of the deep bite and increases the size of the oropharynx” by introducing a 3-mm bite plate between the upper and lower rear molars. The DSD mouthpiece integrates the bite plates with a retainer-like band that wraps around the front incisors; speaking and drinking are possible with the DSD in place, said Dr. Rekawek.
She added that athletic evidence suggests that the DSD can lead to increased oxygenation, less head and neck tension, less muscle fatigue, and improved exercise capacity in some sports.
If these benefits translated to the maternal Valsalva maneuver during the second stage of labor, the increased isometric endurance could increase uterine pressure and optimize the expulsive effect of pushing, explained Dr. Rekawek. However, mixed results were seen in previous work that had women using a DSD during the second stage of labor.
The current study was powered to detect a difference of 20% in the duration of the second stage of labor for nulliparous women who were randomized either to use or not use a DSD while pushing. Women and their caregivers learned their random allocation by opening a sealed envelope at the beginning of the second stage of labor.
The study included nulliparous women who were carrying a singleton pregnancy of at least 37 weeks’ gestation and without known fetal anomalies. Enrollment occurred before the second stage of labor, and 173 women participated in each arm of the study.
For those who were assigned to use the DSD, the second stage of labor lasted a median 84 minutes, whereas the median for the control group was 92 minutes (P = .11) in an intention-to-treat analysis. Passive descent and active pushing lasted a median 14 and 50 minutes, respectively, for the DSD group, compared with 13 and 55 minutes for the control group (P = .22 and P = .29, respectively).
Another analysis of the primary outcome measure used Kaplan-Meier curves to compare the curves of the women who remained pregnant in each group across the period of the second stage of labor. There was no significant difference between the groups when the data were examined in this manner (log rank P = .18).
Secondary maternal outcomes included the mode of delivery. Most women (83%-85%) in each group had a normal spontaneous vaginal delivery, with no differences in any mode of delivery (P = .93). Neonatal outcomes also were similar between groups, with no significant differences in sex, birth weight, arterial pH, and neonatal intensive care unit admissions.
The investigators tracked whether patients were admitted in spontaneous labor, for labor induction with active membranes, or with premature rupture of membranes. Also, they looked at the degree of cervical dilation at admission, whether oxytocin or epidural anesthesia were used in labor, and anesthetic administered during the second stage of labor. There were no differences between groups in these variables.
Dr. Rekawek noted that the study benefited from a large sample size and a prospective, randomized design. Blinding lasted only until pushing began. Also, although all patients were taught how to use the device, they didn’t have an opportunity to practice.
Dr. Rekawek presented on behalf of Dr. Bergh because he became a new father the day before the presentation. His wife, said Dr. Rekawek, didn’t use a dental support device.
The authors reported that they have no relevant financial disclosures.
SOURCE: Bergh E et al. Am J Obstet Gynecol. 2019 Jan;220(1):S39, Abstract 49.
LAS VEGAS –
In a randomized, controlled trial of 346 nulliparous women, the device, adapted from a design used in athletics, made no difference in the duration of the second stage of labor overall or in passive descent or active pushing time. The findings were presented on behalf of first author Eric Bergh, MD, by Patricia Rekawek, MD, at a fellows abstract session at the meeting sponsored by the Society for Maternal-Fetal Medicine. Dr. Rekawek and Dr. Bergh are maternal-fetal medicine fellows at the Icahn School of Medicine at Mount Sinai, New York.
The dental support device (DSD) was actually used by 128 (74%) of the patients who were randomized to DSD usage. Of these patients, two thirds (n = 85) used the device for all second stage contractions. About one quarter (27%; n = 35) used it less than half the time, and a small minority (6%; n = 8) used it more than half the time but not for all pushing, noted Dr. Rekawek.
Most women (61%) who used the device agreed or strongly agreed that it was helpful. Most also found it comfortable (67%), and would use it again in a future delivery (61%). Having a custom-fit DSD, or spending more time practicing before labor, might help with efficacy in shortening the second stage of labor and merits study, the investigators said.
Reducing time spent in the second stage of labor could benefit both mother and neonate because “a prolonged second stage of labor is associated with multiple maternal and neonatal complications,” including increased risk for chorioamnionitis, neonatal sepsis, low umbilical artery pH, shoulder dystocia, and third- and fourth-degree lacerations, said Dr. Rekawek.
In athletics, a DSD “raises the vertical dimension of the deep bite and increases the size of the oropharynx” by introducing a 3-mm bite plate between the upper and lower rear molars. The DSD mouthpiece integrates the bite plates with a retainer-like band that wraps around the front incisors; speaking and drinking are possible with the DSD in place, said Dr. Rekawek.
She added that athletic evidence suggests that the DSD can lead to increased oxygenation, less head and neck tension, less muscle fatigue, and improved exercise capacity in some sports.
If these benefits translated to the maternal Valsalva maneuver during the second stage of labor, the increased isometric endurance could increase uterine pressure and optimize the expulsive effect of pushing, explained Dr. Rekawek. However, mixed results were seen in previous work that had women using a DSD during the second stage of labor.
The current study was powered to detect a difference of 20% in the duration of the second stage of labor for nulliparous women who were randomized either to use or not use a DSD while pushing. Women and their caregivers learned their random allocation by opening a sealed envelope at the beginning of the second stage of labor.
The study included nulliparous women who were carrying a singleton pregnancy of at least 37 weeks’ gestation and without known fetal anomalies. Enrollment occurred before the second stage of labor, and 173 women participated in each arm of the study.
For those who were assigned to use the DSD, the second stage of labor lasted a median 84 minutes, whereas the median for the control group was 92 minutes (P = .11) in an intention-to-treat analysis. Passive descent and active pushing lasted a median 14 and 50 minutes, respectively, for the DSD group, compared with 13 and 55 minutes for the control group (P = .22 and P = .29, respectively).
Another analysis of the primary outcome measure used Kaplan-Meier curves to compare the curves of the women who remained pregnant in each group across the period of the second stage of labor. There was no significant difference between the groups when the data were examined in this manner (log rank P = .18).
Secondary maternal outcomes included the mode of delivery. Most women (83%-85%) in each group had a normal spontaneous vaginal delivery, with no differences in any mode of delivery (P = .93). Neonatal outcomes also were similar between groups, with no significant differences in sex, birth weight, arterial pH, and neonatal intensive care unit admissions.
The investigators tracked whether patients were admitted in spontaneous labor, for labor induction with active membranes, or with premature rupture of membranes. Also, they looked at the degree of cervical dilation at admission, whether oxytocin or epidural anesthesia were used in labor, and anesthetic administered during the second stage of labor. There were no differences between groups in these variables.
Dr. Rekawek noted that the study benefited from a large sample size and a prospective, randomized design. Blinding lasted only until pushing began. Also, although all patients were taught how to use the device, they didn’t have an opportunity to practice.
Dr. Rekawek presented on behalf of Dr. Bergh because he became a new father the day before the presentation. His wife, said Dr. Rekawek, didn’t use a dental support device.
The authors reported that they have no relevant financial disclosures.
SOURCE: Bergh E et al. Am J Obstet Gynecol. 2019 Jan;220(1):S39, Abstract 49.
LAS VEGAS –
In a randomized, controlled trial of 346 nulliparous women, the device, adapted from a design used in athletics, made no difference in the duration of the second stage of labor overall or in passive descent or active pushing time. The findings were presented on behalf of first author Eric Bergh, MD, by Patricia Rekawek, MD, at a fellows abstract session at the meeting sponsored by the Society for Maternal-Fetal Medicine. Dr. Rekawek and Dr. Bergh are maternal-fetal medicine fellows at the Icahn School of Medicine at Mount Sinai, New York.
The dental support device (DSD) was actually used by 128 (74%) of the patients who were randomized to DSD usage. Of these patients, two thirds (n = 85) used the device for all second stage contractions. About one quarter (27%; n = 35) used it less than half the time, and a small minority (6%; n = 8) used it more than half the time but not for all pushing, noted Dr. Rekawek.
Most women (61%) who used the device agreed or strongly agreed that it was helpful. Most also found it comfortable (67%), and would use it again in a future delivery (61%). Having a custom-fit DSD, or spending more time practicing before labor, might help with efficacy in shortening the second stage of labor and merits study, the investigators said.
Reducing time spent in the second stage of labor could benefit both mother and neonate because “a prolonged second stage of labor is associated with multiple maternal and neonatal complications,” including increased risk for chorioamnionitis, neonatal sepsis, low umbilical artery pH, shoulder dystocia, and third- and fourth-degree lacerations, said Dr. Rekawek.
In athletics, a DSD “raises the vertical dimension of the deep bite and increases the size of the oropharynx” by introducing a 3-mm bite plate between the upper and lower rear molars. The DSD mouthpiece integrates the bite plates with a retainer-like band that wraps around the front incisors; speaking and drinking are possible with the DSD in place, said Dr. Rekawek.
She added that athletic evidence suggests that the DSD can lead to increased oxygenation, less head and neck tension, less muscle fatigue, and improved exercise capacity in some sports.
If these benefits translated to the maternal Valsalva maneuver during the second stage of labor, the increased isometric endurance could increase uterine pressure and optimize the expulsive effect of pushing, explained Dr. Rekawek. However, mixed results were seen in previous work that had women using a DSD during the second stage of labor.
The current study was powered to detect a difference of 20% in the duration of the second stage of labor for nulliparous women who were randomized either to use or not use a DSD while pushing. Women and their caregivers learned their random allocation by opening a sealed envelope at the beginning of the second stage of labor.
The study included nulliparous women who were carrying a singleton pregnancy of at least 37 weeks’ gestation and without known fetal anomalies. Enrollment occurred before the second stage of labor, and 173 women participated in each arm of the study.
For those who were assigned to use the DSD, the second stage of labor lasted a median 84 minutes, whereas the median for the control group was 92 minutes (P = .11) in an intention-to-treat analysis. Passive descent and active pushing lasted a median 14 and 50 minutes, respectively, for the DSD group, compared with 13 and 55 minutes for the control group (P = .22 and P = .29, respectively).
Another analysis of the primary outcome measure used Kaplan-Meier curves to compare the curves of the women who remained pregnant in each group across the period of the second stage of labor. There was no significant difference between the groups when the data were examined in this manner (log rank P = .18).
Secondary maternal outcomes included the mode of delivery. Most women (83%-85%) in each group had a normal spontaneous vaginal delivery, with no differences in any mode of delivery (P = .93). Neonatal outcomes also were similar between groups, with no significant differences in sex, birth weight, arterial pH, and neonatal intensive care unit admissions.
The investigators tracked whether patients were admitted in spontaneous labor, for labor induction with active membranes, or with premature rupture of membranes. Also, they looked at the degree of cervical dilation at admission, whether oxytocin or epidural anesthesia were used in labor, and anesthetic administered during the second stage of labor. There were no differences between groups in these variables.
Dr. Rekawek noted that the study benefited from a large sample size and a prospective, randomized design. Blinding lasted only until pushing began. Also, although all patients were taught how to use the device, they didn’t have an opportunity to practice.
Dr. Rekawek presented on behalf of Dr. Bergh because he became a new father the day before the presentation. His wife, said Dr. Rekawek, didn’t use a dental support device.
The authors reported that they have no relevant financial disclosures.
SOURCE: Bergh E et al. Am J Obstet Gynecol. 2019 Jan;220(1):S39, Abstract 49.
REPORTING FROM THE PREGNANCY MEETING
Sildenafil associated with persistent pulmonary hypertension in neonates with early IUGR
LAS VEGAS – Increased rates of persistent neonatal pulmonary hypertension in neonates put the brakes on STRIDER, an international placebo-controlled study looking at sildenafil as a treatment for early-onset intrauterine growth restriction (IUGR).
The study’s independent data safety monitoring board halted STRIDER (Sildenafil Therapy in Dismal Prognosis Early-Onset Fetal Growth Restriction) last July, after an interim safety analysis identified possible fetal harm and no signal of benefit over placebo, Dr. Anouk Pels reported at the annual meeting of the Society for Maternal-Fetal Medicine. The late-breaking presentation at the meeting revealed the first outcome data details.
The board had “serious concerns that sildenafil may cause harm to newborn children. … Given the results , it is extremely unlikely that any benefit could be shown on the primary endpoint if the trial is continued to its completion,” said Dr. Pels of the University of Amsterdam. “Our recommendation is not to use sildenafil for this indication in pregnant women.”
Although the link remains as-yet unproven, pulmonary hypertension among sildenafil-exposed neonates is biologically plausible, she said. It could have been a symptomatic rebound response to the discontinuation of constant intrauterine sildenafil exposure – or it could have been a hint of something more profound. Like the genital vasculature, pulmonary vasculature is a target of the drug. Intrauterine exposure to sildenafil could theoretically alter its development.
“It’s possible that sildenafil may be causing structural changes in the pulmonary vasculature of fetuses. This needs to be explored further, and we will do so by performing additional analyses on autopsy data and placental histology.”
STRIDER involved 261 pregnant women diagnosed with severe early-onset fetal growth restriction. They were randomized to sildenafil 25 mg or placebo three times daily until delivery or 32 weeks’ gestation. A safety analysis was conducted after every 50 patients were enrolled. The preplanned interim analysis was conducted after half of the cohort had been enrolled and received at least one dose of the study medication.
The primary outcome was a composite measure of neonatal mortality or major neonatal morbidity at hospital discharge.
Gestational age at baseline was about 24.6 weeks, and the estimated fetal weight by ultrasound, 465 g. About 45% of pregnancies had evidence of a notching in the uterine artery. In about 42%, the pulsatility index of the umbilical artery was above the 95th percentile; the pulsatility index of the middle cerebral artery was below the 5% percentile in about 70% of cases.
About a quarter of the women had a diagnosis of pregnancy-induced hypertension, and another quarter, preeclampsia. Women used the study medication for a mean of 22 days.
There were no significant between-group differences in maternal outcomes. Median gestational age at delivery was 28 weeks in both groups. About 10% in each group experienced new-onset pregnancy-induced hypertension; About a quarter of each group developed new-onset preeclampsia or HELLP (hemolysis, elevated liver enzymes, low platelet count). There were no between-group differences in the number of maternal antihypertensives prescribed.
The primary combined outcome of neonatal mortality or major neonatal morbidity occurred in 66 of the sildenafil-exposed neonates and 58 of the placebo-exposed infants (61% vs. 54%) – not a significant difference. Fetal death occurred in 23 and 29 pregnancies, respectively (21% and 27%); neonatal death occurred in 21 and 11, respectively (19% and 10%). Overall, fetal/neonatal mortality was similar between the sildenafil and placebo groups (41% and 37%, respectively).
Of the 64 sildenafil-exposed neonates who survived to hospital discharge, 22 exhibited clinically relevant morbidity. Of the 67 in the placebo-treated group who survived to hospital discharge, 18 had clinically relevant morbidity. Overall, 42 in the sildenafil group and 49 of the placebo group survived to hospital discharge without relevant morbidity.
There were a number of secondary outcomes, none exhibiting any significant between-group differences. These included the median weights of those who experienced intrauterine death (425 g and 350 g), median live birth weight (725 g and 783 g), intraventricular hemorrhage of grade II or IV (3% and 2%), periventricular hemorrhage grade II or higher (0%, both groups), necrotizing enterocolitis grade II or higher (7% and 8%), and at least one culture-proven or clinical infection (41% and 33%).
The significantly higher rates of pulmonary hypertension in the sildenafil-exposed neonates was the showstopper. Almost half of the 21 who died had proven pulmonary hypertension (10), as did 6 of the 64 who survived – an excess of 16 cases. Of proven cases, 11 were persistent pulmonary hypertension. There were also two cases of sepsis-associated pulmonary hypertension and four cases of bronchopulmonary dysplasia associated with the disorder. In the placebo-exposed group, pulmonary hypertension occurred in 3 of the 11 deaths and 1 of the 67 who survived. Of proven cases, two were persistent pulmonary hypertension. There was no sepsis-associated pulmonary hypertension, but there were three cases of bronchopulmonary dysplasia associated with the disorder. Some children had both persistent pulmonary hypertension and bronchopulmonary dysplasia.
“While there was no difference in the primary outcomes or in overall mortality, there were more cases of pulmonary hypertension in the sildenafil group,” Dr. Pels said. “We can speculate on the cause, whether it was related to sildenafil and why, or whether it was simply chance. This is the reason we need to conduct more in-depth analyses of these data.”
Funding came from federal health agencies and universities in the countries where STRIDER was conducted, including New Zealand, Australia, the United Kingdom, Ireland, and the Netherlands. Dr. Pels had no relevant financial disclosures.
SOURCE: Pels A et al. The Pregnancy Meeting, Late-Breaker 2.
LAS VEGAS – Increased rates of persistent neonatal pulmonary hypertension in neonates put the brakes on STRIDER, an international placebo-controlled study looking at sildenafil as a treatment for early-onset intrauterine growth restriction (IUGR).
The study’s independent data safety monitoring board halted STRIDER (Sildenafil Therapy in Dismal Prognosis Early-Onset Fetal Growth Restriction) last July, after an interim safety analysis identified possible fetal harm and no signal of benefit over placebo, Dr. Anouk Pels reported at the annual meeting of the Society for Maternal-Fetal Medicine. The late-breaking presentation at the meeting revealed the first outcome data details.
The board had “serious concerns that sildenafil may cause harm to newborn children. … Given the results , it is extremely unlikely that any benefit could be shown on the primary endpoint if the trial is continued to its completion,” said Dr. Pels of the University of Amsterdam. “Our recommendation is not to use sildenafil for this indication in pregnant women.”
Although the link remains as-yet unproven, pulmonary hypertension among sildenafil-exposed neonates is biologically plausible, she said. It could have been a symptomatic rebound response to the discontinuation of constant intrauterine sildenafil exposure – or it could have been a hint of something more profound. Like the genital vasculature, pulmonary vasculature is a target of the drug. Intrauterine exposure to sildenafil could theoretically alter its development.
“It’s possible that sildenafil may be causing structural changes in the pulmonary vasculature of fetuses. This needs to be explored further, and we will do so by performing additional analyses on autopsy data and placental histology.”
STRIDER involved 261 pregnant women diagnosed with severe early-onset fetal growth restriction. They were randomized to sildenafil 25 mg or placebo three times daily until delivery or 32 weeks’ gestation. A safety analysis was conducted after every 50 patients were enrolled. The preplanned interim analysis was conducted after half of the cohort had been enrolled and received at least one dose of the study medication.
The primary outcome was a composite measure of neonatal mortality or major neonatal morbidity at hospital discharge.
Gestational age at baseline was about 24.6 weeks, and the estimated fetal weight by ultrasound, 465 g. About 45% of pregnancies had evidence of a notching in the uterine artery. In about 42%, the pulsatility index of the umbilical artery was above the 95th percentile; the pulsatility index of the middle cerebral artery was below the 5% percentile in about 70% of cases.
About a quarter of the women had a diagnosis of pregnancy-induced hypertension, and another quarter, preeclampsia. Women used the study medication for a mean of 22 days.
There were no significant between-group differences in maternal outcomes. Median gestational age at delivery was 28 weeks in both groups. About 10% in each group experienced new-onset pregnancy-induced hypertension; About a quarter of each group developed new-onset preeclampsia or HELLP (hemolysis, elevated liver enzymes, low platelet count). There were no between-group differences in the number of maternal antihypertensives prescribed.
The primary combined outcome of neonatal mortality or major neonatal morbidity occurred in 66 of the sildenafil-exposed neonates and 58 of the placebo-exposed infants (61% vs. 54%) – not a significant difference. Fetal death occurred in 23 and 29 pregnancies, respectively (21% and 27%); neonatal death occurred in 21 and 11, respectively (19% and 10%). Overall, fetal/neonatal mortality was similar between the sildenafil and placebo groups (41% and 37%, respectively).
Of the 64 sildenafil-exposed neonates who survived to hospital discharge, 22 exhibited clinically relevant morbidity. Of the 67 in the placebo-treated group who survived to hospital discharge, 18 had clinically relevant morbidity. Overall, 42 in the sildenafil group and 49 of the placebo group survived to hospital discharge without relevant morbidity.
There were a number of secondary outcomes, none exhibiting any significant between-group differences. These included the median weights of those who experienced intrauterine death (425 g and 350 g), median live birth weight (725 g and 783 g), intraventricular hemorrhage of grade II or IV (3% and 2%), periventricular hemorrhage grade II or higher (0%, both groups), necrotizing enterocolitis grade II or higher (7% and 8%), and at least one culture-proven or clinical infection (41% and 33%).
The significantly higher rates of pulmonary hypertension in the sildenafil-exposed neonates was the showstopper. Almost half of the 21 who died had proven pulmonary hypertension (10), as did 6 of the 64 who survived – an excess of 16 cases. Of proven cases, 11 were persistent pulmonary hypertension. There were also two cases of sepsis-associated pulmonary hypertension and four cases of bronchopulmonary dysplasia associated with the disorder. In the placebo-exposed group, pulmonary hypertension occurred in 3 of the 11 deaths and 1 of the 67 who survived. Of proven cases, two were persistent pulmonary hypertension. There was no sepsis-associated pulmonary hypertension, but there were three cases of bronchopulmonary dysplasia associated with the disorder. Some children had both persistent pulmonary hypertension and bronchopulmonary dysplasia.
“While there was no difference in the primary outcomes or in overall mortality, there were more cases of pulmonary hypertension in the sildenafil group,” Dr. Pels said. “We can speculate on the cause, whether it was related to sildenafil and why, or whether it was simply chance. This is the reason we need to conduct more in-depth analyses of these data.”
Funding came from federal health agencies and universities in the countries where STRIDER was conducted, including New Zealand, Australia, the United Kingdom, Ireland, and the Netherlands. Dr. Pels had no relevant financial disclosures.
SOURCE: Pels A et al. The Pregnancy Meeting, Late-Breaker 2.
LAS VEGAS – Increased rates of persistent neonatal pulmonary hypertension in neonates put the brakes on STRIDER, an international placebo-controlled study looking at sildenafil as a treatment for early-onset intrauterine growth restriction (IUGR).
The study’s independent data safety monitoring board halted STRIDER (Sildenafil Therapy in Dismal Prognosis Early-Onset Fetal Growth Restriction) last July, after an interim safety analysis identified possible fetal harm and no signal of benefit over placebo, Dr. Anouk Pels reported at the annual meeting of the Society for Maternal-Fetal Medicine. The late-breaking presentation at the meeting revealed the first outcome data details.
The board had “serious concerns that sildenafil may cause harm to newborn children. … Given the results , it is extremely unlikely that any benefit could be shown on the primary endpoint if the trial is continued to its completion,” said Dr. Pels of the University of Amsterdam. “Our recommendation is not to use sildenafil for this indication in pregnant women.”
Although the link remains as-yet unproven, pulmonary hypertension among sildenafil-exposed neonates is biologically plausible, she said. It could have been a symptomatic rebound response to the discontinuation of constant intrauterine sildenafil exposure – or it could have been a hint of something more profound. Like the genital vasculature, pulmonary vasculature is a target of the drug. Intrauterine exposure to sildenafil could theoretically alter its development.
“It’s possible that sildenafil may be causing structural changes in the pulmonary vasculature of fetuses. This needs to be explored further, and we will do so by performing additional analyses on autopsy data and placental histology.”
STRIDER involved 261 pregnant women diagnosed with severe early-onset fetal growth restriction. They were randomized to sildenafil 25 mg or placebo three times daily until delivery or 32 weeks’ gestation. A safety analysis was conducted after every 50 patients were enrolled. The preplanned interim analysis was conducted after half of the cohort had been enrolled and received at least one dose of the study medication.
The primary outcome was a composite measure of neonatal mortality or major neonatal morbidity at hospital discharge.
Gestational age at baseline was about 24.6 weeks, and the estimated fetal weight by ultrasound, 465 g. About 45% of pregnancies had evidence of a notching in the uterine artery. In about 42%, the pulsatility index of the umbilical artery was above the 95th percentile; the pulsatility index of the middle cerebral artery was below the 5% percentile in about 70% of cases.
About a quarter of the women had a diagnosis of pregnancy-induced hypertension, and another quarter, preeclampsia. Women used the study medication for a mean of 22 days.
There were no significant between-group differences in maternal outcomes. Median gestational age at delivery was 28 weeks in both groups. About 10% in each group experienced new-onset pregnancy-induced hypertension; About a quarter of each group developed new-onset preeclampsia or HELLP (hemolysis, elevated liver enzymes, low platelet count). There were no between-group differences in the number of maternal antihypertensives prescribed.
The primary combined outcome of neonatal mortality or major neonatal morbidity occurred in 66 of the sildenafil-exposed neonates and 58 of the placebo-exposed infants (61% vs. 54%) – not a significant difference. Fetal death occurred in 23 and 29 pregnancies, respectively (21% and 27%); neonatal death occurred in 21 and 11, respectively (19% and 10%). Overall, fetal/neonatal mortality was similar between the sildenafil and placebo groups (41% and 37%, respectively).
Of the 64 sildenafil-exposed neonates who survived to hospital discharge, 22 exhibited clinically relevant morbidity. Of the 67 in the placebo-treated group who survived to hospital discharge, 18 had clinically relevant morbidity. Overall, 42 in the sildenafil group and 49 of the placebo group survived to hospital discharge without relevant morbidity.
There were a number of secondary outcomes, none exhibiting any significant between-group differences. These included the median weights of those who experienced intrauterine death (425 g and 350 g), median live birth weight (725 g and 783 g), intraventricular hemorrhage of grade II or IV (3% and 2%), periventricular hemorrhage grade II or higher (0%, both groups), necrotizing enterocolitis grade II or higher (7% and 8%), and at least one culture-proven or clinical infection (41% and 33%).
The significantly higher rates of pulmonary hypertension in the sildenafil-exposed neonates was the showstopper. Almost half of the 21 who died had proven pulmonary hypertension (10), as did 6 of the 64 who survived – an excess of 16 cases. Of proven cases, 11 were persistent pulmonary hypertension. There were also two cases of sepsis-associated pulmonary hypertension and four cases of bronchopulmonary dysplasia associated with the disorder. In the placebo-exposed group, pulmonary hypertension occurred in 3 of the 11 deaths and 1 of the 67 who survived. Of proven cases, two were persistent pulmonary hypertension. There was no sepsis-associated pulmonary hypertension, but there were three cases of bronchopulmonary dysplasia associated with the disorder. Some children had both persistent pulmonary hypertension and bronchopulmonary dysplasia.
“While there was no difference in the primary outcomes or in overall mortality, there were more cases of pulmonary hypertension in the sildenafil group,” Dr. Pels said. “We can speculate on the cause, whether it was related to sildenafil and why, or whether it was simply chance. This is the reason we need to conduct more in-depth analyses of these data.”
Funding came from federal health agencies and universities in the countries where STRIDER was conducted, including New Zealand, Australia, the United Kingdom, Ireland, and the Netherlands. Dr. Pels had no relevant financial disclosures.
SOURCE: Pels A et al. The Pregnancy Meeting, Late-Breaker 2.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point:
Major finding: There were 16 cases of persistent pulmonary hypertension in the treated group and four in the placebo group.
Study details: The randomized study involved 261 pregnant women treated with sildenafil for early-onset intrauterine growth restriction.
Disclosures: Funding agencies and universities in the countries involved in the trial contributed to funding. Dr. Pels had no relevant financial disclosures.
Source: Pels A et al. The Pregnancy Meeting, Late-Breaker 2.
One postdelivery antibiotic dose nearly halves infection in operative delivery
LAS VEGAS – A randomized controlled trial comparing a single postdelivery intravenous dose of antibiotic after operative delivery found that antibiotics nearly halved the risk for maternal infection.
For women who received a single dose of amoxicillin-clavulanic acid, the risk ratio was 0.58 for suspected or confirmed infection, compared with those who received an intravenous dose of saline solution (95% confidence interval, 0.49-0.69, P less than .001). Culture-confirmed systemic infections were similarly reduced by a risk ratio (RR) of 0.44 (95% CI, 0.22-0.89; P =.018).
Superficial and deep incisional infections were also significantly less likely in the women who had received antibiotics (RRs 0.53 and 0.46, respectively; P less than .001 for both). Although sepsis occurred in numerically fewer women who received antibiotics, the numbers were, overall, small and not statistically significant.
By 6 weeks after delivery, patients receiving antibiotics were less likely to have outpatient or home visits for perineal problems or concerns as well (P less than .001).
“This trial shows clear benefit of a single dose of prophylactic antibiotic after operative vaginal birth, and this should be introduced into routine practice,” said Marian Knight, MBChB, DPhil.
Dr. Knight presented findings of the randomized trial, dubbed ANODE, at a late-breaking abstract session of the meeting, which was sponsored by the Society for Maternal-Fetal Medicine. Dr. Knight, professor of maternal and child population health at the University of Oxford (England), explained that ANODE aimed to determine whether a single dose of prophylactic amoxicillin-clavulanic acid was clinically effective in preventing confirmed or suspected maternal infection after operative vaginal birth.
The study tips the scales in favor of the anti-infective properties of the single antibiotic dose after operative delivery, and comes at a time when unacceptable levels of maternal morbidity and mortality coexist with pressing worries about antibiotic resistance, Dr. Knight said.
The multicenter randomized, blinded, placebo-controlled trial was conducted at 27 sites in the United Kingdom between March 2016 and June 2018.
Women at the study sites who underwent operative delivery, whether by forceps or vacuum extraction, received either a single dose of intravenous amoxicillin-clavulanic acid (1 gm/200 mg), or a placebo dose of saline solution. Antibiotics were given in the window of 0 to 6 hours post-delivery.
The primary outcome measure was confirmed or suspected maternal infection within 6 weeks of delivery. Women were positive for infection if they were prescribed antibiotics for perineal wound infections, if they experienced endometrial or uterine infections, if they had urinary tract infections with “systemic features, or if they had other systemic infections. Other criteria for infection were culture-confirmed systemic infection, or endometritis by criteria established by the Centers for Disease Control and Prevention.
Dr. Knight and her colleagues used an intention-to-treat analysis that looked at the primary outcome as a risk ratio, with a 95% CI. Secondary outcomes, also presented as risk ratios, were considered with a 99% CI.
A total of 3,427 women were randomized. In all, 1,715 women in the active arm and 1,705 in the placebo arm were included in the outcomes analyses. Women were interviewed by telephone, they completed questionnaires, and they received a questionnaire by mail or completed one online. Slightly more than 1,500 women in each arm completed the phone interview, and nearly 1,300 in each arm completed the initial questionnaire.
The mean age was 30 years, and most of the participants (84%-87%) were white. Most were of normal weight, with a median body mass index at the initial prenatal visit of 25 kg/m2.
Though women with multiple pregnancies were included in the study, just 11 in the active arm and 9 in the placebo arm delivered twins. There were no triplets. Most women (76%-78%) were primiparous, and just 7%-8% of women had prior cesarean delivery.
The mode of operative delivery for most of the participants (63%-67%) was forceps, with all but 10 of the remaining women receiving vacuum extraction (the remaining 10 had spontaneous vaginal deliveries).
The reasons for instrumental delivery were approximately evenly divided between failure of labor to progress and fetal compromise.
Nearly 90% of the women – more than 1,500 in each study arm – received episiotomies, a figure that Dr. Knight said she found surprising. She noted that mediolateral incisions are the standard of care in the United Kingdom. Still, 29%-33% of the women experienced a tear, with most being second-degree tears. Third- and fourth-degree tears occurred in two women overall. Almost all of the women (99%) had their wounds sutured.
Three serious adverse events were reported. One woman in the placebo arm required intensive care unit admission for severe sepsis, and another placebo participant required a transfusion after postpartum hemorrhage. One patient who received antibiotic had immediate diffuse itching and a swollen throat. However, antibiotic side effects were reported in only 2 of the 1,715 active arm participants, Dr. Knight said.
The competing concerns of maternal safety and antibiotic stewardship are weighed against a global backdrop of high maternal infection rates, Dr. Knight said. Sepsis causes 11% of global maternal deaths, a rate that drops to about 5% in higher-income nations. However, she pointed out, that figure rises to about 13% in the United States.
“For every woman that dies from pregnancy-related infection, a further 70 have severe infection and survive,” she said.
Known risk factors for infection include operative vaginal delivery and cesarean deliveries. For cesareans performed after the onset of labor, the adjusted odds ratio reaches 6.7 for severe infection, Dr. Knight said (PLoS Med. 2014;11:e1001672). A systematic review estimated that the rate for any infection following cesarean delivery approaches one in four women, she said (Cochrane Database Syst Rev. 2014 Oct 28;[10]:CD007482).
The same systematic review found that prophylactic antibiotics reduced incidence of wound infection, endometritis, and serious maternal wound infection after cesarean delivery (RR 0.40, 0.38, and 0.31, respectively).
For operative vaginal deliveries, however, a Cochrane review found one study of 393 women. Although no women given antibiotics developed endometritis compared with seven cases of endometritis in the no-antibiotics group for a RR of .07, the 95% confidence interval in the Cochrane analysis included zero, so the findings weren’t statistically significant. Hospital length of stay didn’t differ between the two groups (Cochrane Database Syst Rev. 2014 Oct 13;[10]:CD004455).
Citing this review, the United Kingdom’s Royal College of Gynecologists had concluded that evidence was insufficient to support routine antibiotic prophylaxis in operative deliveries. The American College of Obstetricians and Gynecologists make no mention of antibiotic prophylaxis or postdelivery infection in its guidelines for operative delivery, Dr. Knight said.
Since confirmed or suspected infection was still seen in 11% of women who received antibiotics, further analysis “is needed to investigate whether early administration, prenatal administration, or repeated administration is more likely to be effective,” she said. Women in the ANODE trial received their dose at a median of 3 hours after delivery.
“Until these analyses are completed, there is no indication for administration of more than a single dose of prophylactic antibiotic, or for predelivery administration,” she said.
Dr. Knight reported that ANODE was funded by the U.K.’s National Institute for Health Research. She reported that she had no conflicts of interest.
SOURCE: Knight M et al. Am J Obstet Gynecol. 2019 Jan;220;1:S685. Abstract LB 3.
LAS VEGAS – A randomized controlled trial comparing a single postdelivery intravenous dose of antibiotic after operative delivery found that antibiotics nearly halved the risk for maternal infection.
For women who received a single dose of amoxicillin-clavulanic acid, the risk ratio was 0.58 for suspected or confirmed infection, compared with those who received an intravenous dose of saline solution (95% confidence interval, 0.49-0.69, P less than .001). Culture-confirmed systemic infections were similarly reduced by a risk ratio (RR) of 0.44 (95% CI, 0.22-0.89; P =.018).
Superficial and deep incisional infections were also significantly less likely in the women who had received antibiotics (RRs 0.53 and 0.46, respectively; P less than .001 for both). Although sepsis occurred in numerically fewer women who received antibiotics, the numbers were, overall, small and not statistically significant.
By 6 weeks after delivery, patients receiving antibiotics were less likely to have outpatient or home visits for perineal problems or concerns as well (P less than .001).
“This trial shows clear benefit of a single dose of prophylactic antibiotic after operative vaginal birth, and this should be introduced into routine practice,” said Marian Knight, MBChB, DPhil.
Dr. Knight presented findings of the randomized trial, dubbed ANODE, at a late-breaking abstract session of the meeting, which was sponsored by the Society for Maternal-Fetal Medicine. Dr. Knight, professor of maternal and child population health at the University of Oxford (England), explained that ANODE aimed to determine whether a single dose of prophylactic amoxicillin-clavulanic acid was clinically effective in preventing confirmed or suspected maternal infection after operative vaginal birth.
The study tips the scales in favor of the anti-infective properties of the single antibiotic dose after operative delivery, and comes at a time when unacceptable levels of maternal morbidity and mortality coexist with pressing worries about antibiotic resistance, Dr. Knight said.
The multicenter randomized, blinded, placebo-controlled trial was conducted at 27 sites in the United Kingdom between March 2016 and June 2018.
Women at the study sites who underwent operative delivery, whether by forceps or vacuum extraction, received either a single dose of intravenous amoxicillin-clavulanic acid (1 gm/200 mg), or a placebo dose of saline solution. Antibiotics were given in the window of 0 to 6 hours post-delivery.
The primary outcome measure was confirmed or suspected maternal infection within 6 weeks of delivery. Women were positive for infection if they were prescribed antibiotics for perineal wound infections, if they experienced endometrial or uterine infections, if they had urinary tract infections with “systemic features, or if they had other systemic infections. Other criteria for infection were culture-confirmed systemic infection, or endometritis by criteria established by the Centers for Disease Control and Prevention.
Dr. Knight and her colleagues used an intention-to-treat analysis that looked at the primary outcome as a risk ratio, with a 95% CI. Secondary outcomes, also presented as risk ratios, were considered with a 99% CI.
A total of 3,427 women were randomized. In all, 1,715 women in the active arm and 1,705 in the placebo arm were included in the outcomes analyses. Women were interviewed by telephone, they completed questionnaires, and they received a questionnaire by mail or completed one online. Slightly more than 1,500 women in each arm completed the phone interview, and nearly 1,300 in each arm completed the initial questionnaire.
The mean age was 30 years, and most of the participants (84%-87%) were white. Most were of normal weight, with a median body mass index at the initial prenatal visit of 25 kg/m2.
Though women with multiple pregnancies were included in the study, just 11 in the active arm and 9 in the placebo arm delivered twins. There were no triplets. Most women (76%-78%) were primiparous, and just 7%-8% of women had prior cesarean delivery.
The mode of operative delivery for most of the participants (63%-67%) was forceps, with all but 10 of the remaining women receiving vacuum extraction (the remaining 10 had spontaneous vaginal deliveries).
The reasons for instrumental delivery were approximately evenly divided between failure of labor to progress and fetal compromise.
Nearly 90% of the women – more than 1,500 in each study arm – received episiotomies, a figure that Dr. Knight said she found surprising. She noted that mediolateral incisions are the standard of care in the United Kingdom. Still, 29%-33% of the women experienced a tear, with most being second-degree tears. Third- and fourth-degree tears occurred in two women overall. Almost all of the women (99%) had their wounds sutured.
Three serious adverse events were reported. One woman in the placebo arm required intensive care unit admission for severe sepsis, and another placebo participant required a transfusion after postpartum hemorrhage. One patient who received antibiotic had immediate diffuse itching and a swollen throat. However, antibiotic side effects were reported in only 2 of the 1,715 active arm participants, Dr. Knight said.
The competing concerns of maternal safety and antibiotic stewardship are weighed against a global backdrop of high maternal infection rates, Dr. Knight said. Sepsis causes 11% of global maternal deaths, a rate that drops to about 5% in higher-income nations. However, she pointed out, that figure rises to about 13% in the United States.
“For every woman that dies from pregnancy-related infection, a further 70 have severe infection and survive,” she said.
Known risk factors for infection include operative vaginal delivery and cesarean deliveries. For cesareans performed after the onset of labor, the adjusted odds ratio reaches 6.7 for severe infection, Dr. Knight said (PLoS Med. 2014;11:e1001672). A systematic review estimated that the rate for any infection following cesarean delivery approaches one in four women, she said (Cochrane Database Syst Rev. 2014 Oct 28;[10]:CD007482).
The same systematic review found that prophylactic antibiotics reduced incidence of wound infection, endometritis, and serious maternal wound infection after cesarean delivery (RR 0.40, 0.38, and 0.31, respectively).
For operative vaginal deliveries, however, a Cochrane review found one study of 393 women. Although no women given antibiotics developed endometritis compared with seven cases of endometritis in the no-antibiotics group for a RR of .07, the 95% confidence interval in the Cochrane analysis included zero, so the findings weren’t statistically significant. Hospital length of stay didn’t differ between the two groups (Cochrane Database Syst Rev. 2014 Oct 13;[10]:CD004455).
Citing this review, the United Kingdom’s Royal College of Gynecologists had concluded that evidence was insufficient to support routine antibiotic prophylaxis in operative deliveries. The American College of Obstetricians and Gynecologists make no mention of antibiotic prophylaxis or postdelivery infection in its guidelines for operative delivery, Dr. Knight said.
Since confirmed or suspected infection was still seen in 11% of women who received antibiotics, further analysis “is needed to investigate whether early administration, prenatal administration, or repeated administration is more likely to be effective,” she said. Women in the ANODE trial received their dose at a median of 3 hours after delivery.
“Until these analyses are completed, there is no indication for administration of more than a single dose of prophylactic antibiotic, or for predelivery administration,” she said.
Dr. Knight reported that ANODE was funded by the U.K.’s National Institute for Health Research. She reported that she had no conflicts of interest.
SOURCE: Knight M et al. Am J Obstet Gynecol. 2019 Jan;220;1:S685. Abstract LB 3.
LAS VEGAS – A randomized controlled trial comparing a single postdelivery intravenous dose of antibiotic after operative delivery found that antibiotics nearly halved the risk for maternal infection.
For women who received a single dose of amoxicillin-clavulanic acid, the risk ratio was 0.58 for suspected or confirmed infection, compared with those who received an intravenous dose of saline solution (95% confidence interval, 0.49-0.69, P less than .001). Culture-confirmed systemic infections were similarly reduced by a risk ratio (RR) of 0.44 (95% CI, 0.22-0.89; P =.018).
Superficial and deep incisional infections were also significantly less likely in the women who had received antibiotics (RRs 0.53 and 0.46, respectively; P less than .001 for both). Although sepsis occurred in numerically fewer women who received antibiotics, the numbers were, overall, small and not statistically significant.
By 6 weeks after delivery, patients receiving antibiotics were less likely to have outpatient or home visits for perineal problems or concerns as well (P less than .001).
“This trial shows clear benefit of a single dose of prophylactic antibiotic after operative vaginal birth, and this should be introduced into routine practice,” said Marian Knight, MBChB, DPhil.
Dr. Knight presented findings of the randomized trial, dubbed ANODE, at a late-breaking abstract session of the meeting, which was sponsored by the Society for Maternal-Fetal Medicine. Dr. Knight, professor of maternal and child population health at the University of Oxford (England), explained that ANODE aimed to determine whether a single dose of prophylactic amoxicillin-clavulanic acid was clinically effective in preventing confirmed or suspected maternal infection after operative vaginal birth.
The study tips the scales in favor of the anti-infective properties of the single antibiotic dose after operative delivery, and comes at a time when unacceptable levels of maternal morbidity and mortality coexist with pressing worries about antibiotic resistance, Dr. Knight said.
The multicenter randomized, blinded, placebo-controlled trial was conducted at 27 sites in the United Kingdom between March 2016 and June 2018.
Women at the study sites who underwent operative delivery, whether by forceps or vacuum extraction, received either a single dose of intravenous amoxicillin-clavulanic acid (1 gm/200 mg), or a placebo dose of saline solution. Antibiotics were given in the window of 0 to 6 hours post-delivery.
The primary outcome measure was confirmed or suspected maternal infection within 6 weeks of delivery. Women were positive for infection if they were prescribed antibiotics for perineal wound infections, if they experienced endometrial or uterine infections, if they had urinary tract infections with “systemic features, or if they had other systemic infections. Other criteria for infection were culture-confirmed systemic infection, or endometritis by criteria established by the Centers for Disease Control and Prevention.
Dr. Knight and her colleagues used an intention-to-treat analysis that looked at the primary outcome as a risk ratio, with a 95% CI. Secondary outcomes, also presented as risk ratios, were considered with a 99% CI.
A total of 3,427 women were randomized. In all, 1,715 women in the active arm and 1,705 in the placebo arm were included in the outcomes analyses. Women were interviewed by telephone, they completed questionnaires, and they received a questionnaire by mail or completed one online. Slightly more than 1,500 women in each arm completed the phone interview, and nearly 1,300 in each arm completed the initial questionnaire.
The mean age was 30 years, and most of the participants (84%-87%) were white. Most were of normal weight, with a median body mass index at the initial prenatal visit of 25 kg/m2.
Though women with multiple pregnancies were included in the study, just 11 in the active arm and 9 in the placebo arm delivered twins. There were no triplets. Most women (76%-78%) were primiparous, and just 7%-8% of women had prior cesarean delivery.
The mode of operative delivery for most of the participants (63%-67%) was forceps, with all but 10 of the remaining women receiving vacuum extraction (the remaining 10 had spontaneous vaginal deliveries).
The reasons for instrumental delivery were approximately evenly divided between failure of labor to progress and fetal compromise.
Nearly 90% of the women – more than 1,500 in each study arm – received episiotomies, a figure that Dr. Knight said she found surprising. She noted that mediolateral incisions are the standard of care in the United Kingdom. Still, 29%-33% of the women experienced a tear, with most being second-degree tears. Third- and fourth-degree tears occurred in two women overall. Almost all of the women (99%) had their wounds sutured.
Three serious adverse events were reported. One woman in the placebo arm required intensive care unit admission for severe sepsis, and another placebo participant required a transfusion after postpartum hemorrhage. One patient who received antibiotic had immediate diffuse itching and a swollen throat. However, antibiotic side effects were reported in only 2 of the 1,715 active arm participants, Dr. Knight said.
The competing concerns of maternal safety and antibiotic stewardship are weighed against a global backdrop of high maternal infection rates, Dr. Knight said. Sepsis causes 11% of global maternal deaths, a rate that drops to about 5% in higher-income nations. However, she pointed out, that figure rises to about 13% in the United States.
“For every woman that dies from pregnancy-related infection, a further 70 have severe infection and survive,” she said.
Known risk factors for infection include operative vaginal delivery and cesarean deliveries. For cesareans performed after the onset of labor, the adjusted odds ratio reaches 6.7 for severe infection, Dr. Knight said (PLoS Med. 2014;11:e1001672). A systematic review estimated that the rate for any infection following cesarean delivery approaches one in four women, she said (Cochrane Database Syst Rev. 2014 Oct 28;[10]:CD007482).
The same systematic review found that prophylactic antibiotics reduced incidence of wound infection, endometritis, and serious maternal wound infection after cesarean delivery (RR 0.40, 0.38, and 0.31, respectively).
For operative vaginal deliveries, however, a Cochrane review found one study of 393 women. Although no women given antibiotics developed endometritis compared with seven cases of endometritis in the no-antibiotics group for a RR of .07, the 95% confidence interval in the Cochrane analysis included zero, so the findings weren’t statistically significant. Hospital length of stay didn’t differ between the two groups (Cochrane Database Syst Rev. 2014 Oct 13;[10]:CD004455).
Citing this review, the United Kingdom’s Royal College of Gynecologists had concluded that evidence was insufficient to support routine antibiotic prophylaxis in operative deliveries. The American College of Obstetricians and Gynecologists make no mention of antibiotic prophylaxis or postdelivery infection in its guidelines for operative delivery, Dr. Knight said.
Since confirmed or suspected infection was still seen in 11% of women who received antibiotics, further analysis “is needed to investigate whether early administration, prenatal administration, or repeated administration is more likely to be effective,” she said. Women in the ANODE trial received their dose at a median of 3 hours after delivery.
“Until these analyses are completed, there is no indication for administration of more than a single dose of prophylactic antibiotic, or for predelivery administration,” she said.
Dr. Knight reported that ANODE was funded by the U.K.’s National Institute for Health Research. She reported that she had no conflicts of interest.
SOURCE: Knight M et al. Am J Obstet Gynecol. 2019 Jan;220;1:S685. Abstract LB 3.
REPORTING FROM THE PREGNANCY MEETING
Umbilical cord milking tied to severe IVH in very premature neonates
Delayed cord clamping and cutting is safer
LAS VEGAS – Umbilical cord milking can cause severe intraventricular hemorrhage (IVH) in very premature neonates and should not be performed on these cerebrovascularly fragile premature babies.
Just six of these procedures would be needed to cause a case of severe IVH in neonates born at 23-27 weeks’ gestation, Michael W. Varner, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“Centers practicing umbilical cord milking should consider discontinuing this practice in infants 23-27 weeks’ gestation,” said Dr. Varner of the University of Utah, Salt Lake City.
The damage to the brains of very young preemies appears to be a direct result of the fluid overload caused by milking, he said. “From a mechanistic perspective, we can intuit that these findings are consistent with cord milking. This causes increasing venous return to the right atrium where it enters the foramen ovale and aorta. These very premature babies have more pulmonary vasoconstriction, which shunts more blood toward the brain. This results in fluctuations in flow in an immature brain with fragile germinal matrices and perhaps further compromised by chorioamnionitis inflammation, resulting in IVH.”
Premature Infants Receiving Milking or Delayed Cord Clamping (PREMOD2) was a noninferiority trial of umbilical cord milking compared to delayed cord clamping and cutting in preterm infants. Conducted at 11 sites in the United States and Europe, the study was halted prematurely when the data safety monitoring board determined that cord milking increased the risk of IVH in younger preemies and was no better than delayed cutting in the older preemies. The analysis presented at the meeting is the first public discussion of the data details.
The trial involved 474 premature neonates. They were randomized to placental transfusion via a 60-second delay in cord clamping and cutting or to umbilical cord milking, which involved grasping the cord and manually pushing the cord blood toward the infant four times before clamping. All participating sites received a video demonstrating the proper procedure. The cohort also was divided by gestational age: 23-27 weeks and 28-31 weeks.
The primary endpoint was a combination of severe IVH (grade 3 or higher) and neonatal death. Overall, the primary endpoint occurred in 29 of those randomized to cord milking (12%) and 20 randomized to delayed clamping (8%) – a significant difference.
This finding was largely driven by the treatment differences in the 23-27 week group, Dr. Varner said. Severe IVH occurred in 20 (22%) of those randomized to cord milking and five (6%) of those randomized to delayed clamping – a highly statistically significant difference with a P value of 0.0019.
In the 28-31 week group, there were no cases of severe IVH in the cord milking group, and three cases in the delayed clamping group; the difference was not statistically significant.
Overall, deaths were similar between the cord milking and cord clamping groups (17 and 15, respectively). Most of these deaths occurred in the younger group (14 in the cord milking group and 13 in the clamping group). There were five deaths in the older group: three in the cord milking group and two in the clamping group. None of these differences were statistically significant.
After seeing these data in a preplanned interim safety analysis, the Data Safety Monitoring Board stopped the study, saying that the intervention appeared dangerous for the younger babies, and no better than the delayed cutting and clamping for the older group, Dr. Varner said.
Since the trial was halted, investigators have been dissecting the data to identify any other intracranial hemorrhage risks particular to the infants. They found no significant differences in maternal characteristics at baseline, and – other than age and randomization– nothing significantly different between the infant groups. Severe persistent IVH occurred in almost 70% of the infants born at 23 weeks’ gestation but in only 7% in the delayed cord clamping group. The risks declined rapidly with increasing gestational age, although they were at all times greater than the risk of IVH in the cord clamping group.
“Looking at the data by gestational age, it’s clear that the majority of the severe IVH occurrences were in the 23 weekers, and also occurred in the first 7 days of life,” Dr. Varner said.
The cohort will be followed for at least another year, he added, as investigators track neurodevelopmental outcomes.
Investigators are particularly interested in differences in motor and language skills, as well as general cognitive development.
The study was sponsored by theEunice Kennedy Shriver National Institute of Child Health and Development. Neither Dr. Varner nor any of the coauthors had any financial declarations.
SOURCE: Katheria AC et al. The Pregnancy Meeting, late breaking abstract 1.
Delayed cord clamping and cutting is safer
Delayed cord clamping and cutting is safer
LAS VEGAS – Umbilical cord milking can cause severe intraventricular hemorrhage (IVH) in very premature neonates and should not be performed on these cerebrovascularly fragile premature babies.
Just six of these procedures would be needed to cause a case of severe IVH in neonates born at 23-27 weeks’ gestation, Michael W. Varner, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“Centers practicing umbilical cord milking should consider discontinuing this practice in infants 23-27 weeks’ gestation,” said Dr. Varner of the University of Utah, Salt Lake City.
The damage to the brains of very young preemies appears to be a direct result of the fluid overload caused by milking, he said. “From a mechanistic perspective, we can intuit that these findings are consistent with cord milking. This causes increasing venous return to the right atrium where it enters the foramen ovale and aorta. These very premature babies have more pulmonary vasoconstriction, which shunts more blood toward the brain. This results in fluctuations in flow in an immature brain with fragile germinal matrices and perhaps further compromised by chorioamnionitis inflammation, resulting in IVH.”
Premature Infants Receiving Milking or Delayed Cord Clamping (PREMOD2) was a noninferiority trial of umbilical cord milking compared to delayed cord clamping and cutting in preterm infants. Conducted at 11 sites in the United States and Europe, the study was halted prematurely when the data safety monitoring board determined that cord milking increased the risk of IVH in younger preemies and was no better than delayed cutting in the older preemies. The analysis presented at the meeting is the first public discussion of the data details.
The trial involved 474 premature neonates. They were randomized to placental transfusion via a 60-second delay in cord clamping and cutting or to umbilical cord milking, which involved grasping the cord and manually pushing the cord blood toward the infant four times before clamping. All participating sites received a video demonstrating the proper procedure. The cohort also was divided by gestational age: 23-27 weeks and 28-31 weeks.
The primary endpoint was a combination of severe IVH (grade 3 or higher) and neonatal death. Overall, the primary endpoint occurred in 29 of those randomized to cord milking (12%) and 20 randomized to delayed clamping (8%) – a significant difference.
This finding was largely driven by the treatment differences in the 23-27 week group, Dr. Varner said. Severe IVH occurred in 20 (22%) of those randomized to cord milking and five (6%) of those randomized to delayed clamping – a highly statistically significant difference with a P value of 0.0019.
In the 28-31 week group, there were no cases of severe IVH in the cord milking group, and three cases in the delayed clamping group; the difference was not statistically significant.
Overall, deaths were similar between the cord milking and cord clamping groups (17 and 15, respectively). Most of these deaths occurred in the younger group (14 in the cord milking group and 13 in the clamping group). There were five deaths in the older group: three in the cord milking group and two in the clamping group. None of these differences were statistically significant.
After seeing these data in a preplanned interim safety analysis, the Data Safety Monitoring Board stopped the study, saying that the intervention appeared dangerous for the younger babies, and no better than the delayed cutting and clamping for the older group, Dr. Varner said.
Since the trial was halted, investigators have been dissecting the data to identify any other intracranial hemorrhage risks particular to the infants. They found no significant differences in maternal characteristics at baseline, and – other than age and randomization– nothing significantly different between the infant groups. Severe persistent IVH occurred in almost 70% of the infants born at 23 weeks’ gestation but in only 7% in the delayed cord clamping group. The risks declined rapidly with increasing gestational age, although they were at all times greater than the risk of IVH in the cord clamping group.
“Looking at the data by gestational age, it’s clear that the majority of the severe IVH occurrences were in the 23 weekers, and also occurred in the first 7 days of life,” Dr. Varner said.
The cohort will be followed for at least another year, he added, as investigators track neurodevelopmental outcomes.
Investigators are particularly interested in differences in motor and language skills, as well as general cognitive development.
The study was sponsored by theEunice Kennedy Shriver National Institute of Child Health and Development. Neither Dr. Varner nor any of the coauthors had any financial declarations.
SOURCE: Katheria AC et al. The Pregnancy Meeting, late breaking abstract 1.
LAS VEGAS – Umbilical cord milking can cause severe intraventricular hemorrhage (IVH) in very premature neonates and should not be performed on these cerebrovascularly fragile premature babies.
Just six of these procedures would be needed to cause a case of severe IVH in neonates born at 23-27 weeks’ gestation, Michael W. Varner, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“Centers practicing umbilical cord milking should consider discontinuing this practice in infants 23-27 weeks’ gestation,” said Dr. Varner of the University of Utah, Salt Lake City.
The damage to the brains of very young preemies appears to be a direct result of the fluid overload caused by milking, he said. “From a mechanistic perspective, we can intuit that these findings are consistent with cord milking. This causes increasing venous return to the right atrium where it enters the foramen ovale and aorta. These very premature babies have more pulmonary vasoconstriction, which shunts more blood toward the brain. This results in fluctuations in flow in an immature brain with fragile germinal matrices and perhaps further compromised by chorioamnionitis inflammation, resulting in IVH.”
Premature Infants Receiving Milking or Delayed Cord Clamping (PREMOD2) was a noninferiority trial of umbilical cord milking compared to delayed cord clamping and cutting in preterm infants. Conducted at 11 sites in the United States and Europe, the study was halted prematurely when the data safety monitoring board determined that cord milking increased the risk of IVH in younger preemies and was no better than delayed cutting in the older preemies. The analysis presented at the meeting is the first public discussion of the data details.
The trial involved 474 premature neonates. They were randomized to placental transfusion via a 60-second delay in cord clamping and cutting or to umbilical cord milking, which involved grasping the cord and manually pushing the cord blood toward the infant four times before clamping. All participating sites received a video demonstrating the proper procedure. The cohort also was divided by gestational age: 23-27 weeks and 28-31 weeks.
The primary endpoint was a combination of severe IVH (grade 3 or higher) and neonatal death. Overall, the primary endpoint occurred in 29 of those randomized to cord milking (12%) and 20 randomized to delayed clamping (8%) – a significant difference.
This finding was largely driven by the treatment differences in the 23-27 week group, Dr. Varner said. Severe IVH occurred in 20 (22%) of those randomized to cord milking and five (6%) of those randomized to delayed clamping – a highly statistically significant difference with a P value of 0.0019.
In the 28-31 week group, there were no cases of severe IVH in the cord milking group, and three cases in the delayed clamping group; the difference was not statistically significant.
Overall, deaths were similar between the cord milking and cord clamping groups (17 and 15, respectively). Most of these deaths occurred in the younger group (14 in the cord milking group and 13 in the clamping group). There were five deaths in the older group: three in the cord milking group and two in the clamping group. None of these differences were statistically significant.
After seeing these data in a preplanned interim safety analysis, the Data Safety Monitoring Board stopped the study, saying that the intervention appeared dangerous for the younger babies, and no better than the delayed cutting and clamping for the older group, Dr. Varner said.
Since the trial was halted, investigators have been dissecting the data to identify any other intracranial hemorrhage risks particular to the infants. They found no significant differences in maternal characteristics at baseline, and – other than age and randomization– nothing significantly different between the infant groups. Severe persistent IVH occurred in almost 70% of the infants born at 23 weeks’ gestation but in only 7% in the delayed cord clamping group. The risks declined rapidly with increasing gestational age, although they were at all times greater than the risk of IVH in the cord clamping group.
“Looking at the data by gestational age, it’s clear that the majority of the severe IVH occurrences were in the 23 weekers, and also occurred in the first 7 days of life,” Dr. Varner said.
The cohort will be followed for at least another year, he added, as investigators track neurodevelopmental outcomes.
Investigators are particularly interested in differences in motor and language skills, as well as general cognitive development.
The study was sponsored by theEunice Kennedy Shriver National Institute of Child Health and Development. Neither Dr. Varner nor any of the coauthors had any financial declarations.
SOURCE: Katheria AC et al. The Pregnancy Meeting, late breaking abstract 1.
REPORTING FROM THE PREGNANCY MEETING