User login
LAS VEGAS – according to data shared in a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
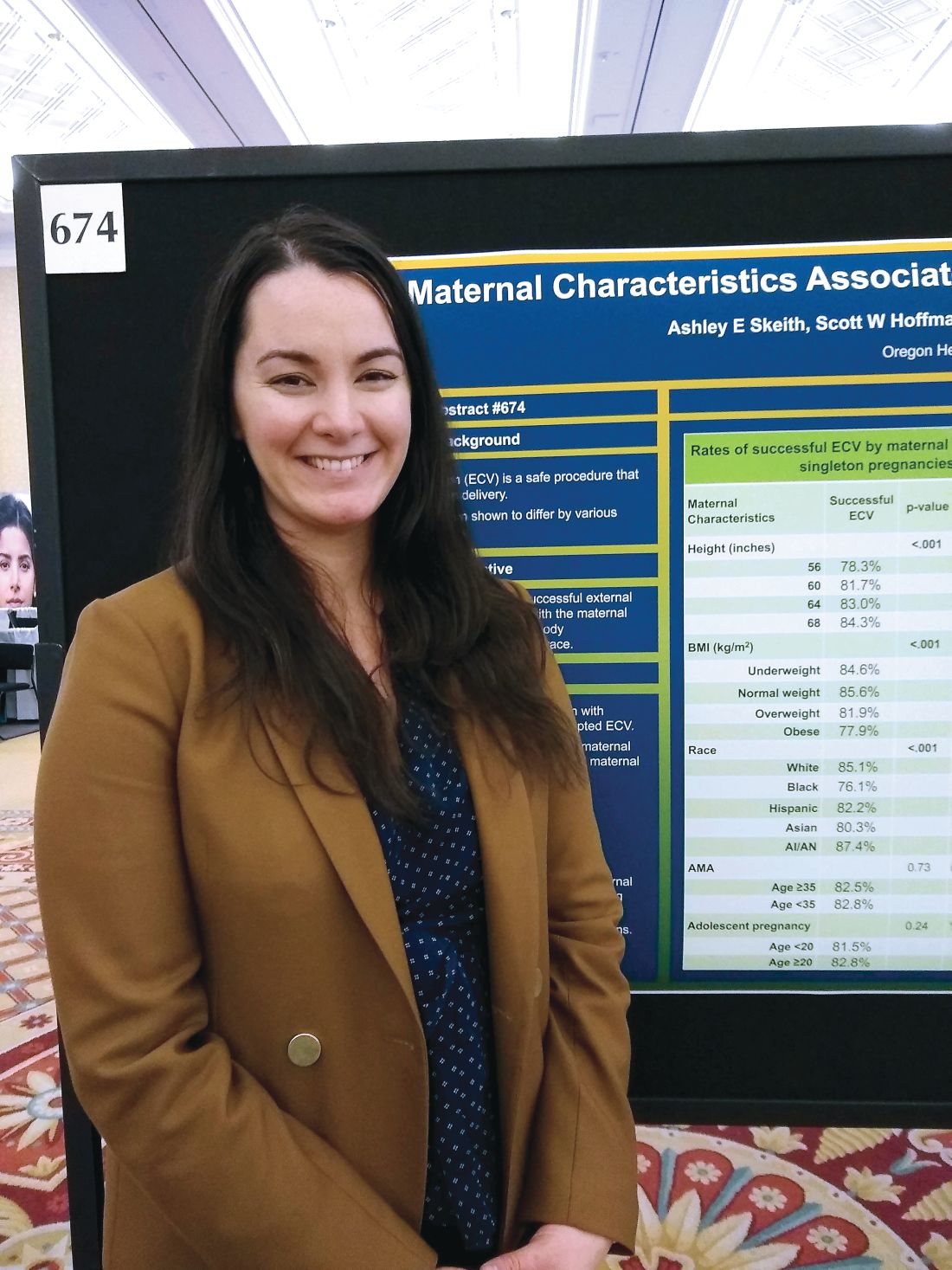
Race/ethnicity also had an impact on the likelihood that external cephalic version (ECV) would be successful.
In an interview, first author Ashley E. Skeith, a medical student at Oregon Health and Sciences University, Portland, said that various characteristics of a pregnancy may affect the success of ECV, but it wasn’t known which maternal characteristics might be associated with greater success of the maneuver.
She and her collaborators found that rates of success were high overall, but that 84% of women 68 inches or taller had successful ECVs, compared with 78% of women less than 60 inches tall. Rates were 82% and 83% for women 60-64 inches and 64-68 inches tall, respectively (adjusted odds ratio, 1.03; P less than .001).
The retrospective cohort study used data from 18,896 women who had singleton, breech, term gestations for whom ECV was attempted. Variables extracted from the medical record included maternal age, height, race, and prepregnancy body mass index (BMI).
For analysis, maternal BMI was grouped into four categories: underweight (BMI, less than 18.5 kg/m2), normal weight (BMI, 18.5-24.9 kg/m2), overweight (BMI, 25-29 kg/m2), and obese (BMI, greater than 30 kg/m2).
Women who were normal weight had the highest likelihood of a successful ECV, at 86%, followed by underweight women at 85%. Women who were overweight and obese had lower success rates, at 82% and 78%, respectively (aOR, 0.86; P less than .001).
Compared with white women, black women had an aOR of 0.60 for successful ECV (P less than .001). The aOR for successful ECV for Asian women was 0.71; for Hispanic women, the aOR was 0.82. American Indian and Alaska Native women were slightly more likely to have successful ECV than white women, but the difference was not significant after statistical adjustment.
Neither advanced maternal age (greater than 35 years) nor adolescent pregnancy were associated with decreased likelihood of successful ECV.
Potential confounders included maternal education level and insurance status, how much weight was gained during pregnancy, whether an epidural was administered, and whether the mother had diabetes. Multivariable regression analysis adjusted for these variables, said Ms. Skeith.
“External cephalic version is a safe procedure that reduces risk of cesarean delivery,” wrote Ms. Skeith and her colleagues. “Though fetal positioning and analgesia have been considered in the prediction of ECV success, [these] data [suggest] that maternal stature and race/ethnicity could be incorporated into potential prediction tools.”
Ms. Skeith reported no outside sources of funding or conflicts of interest.
SOURCE: Skeith AE et al. Am J Obstet Gynecol. 2019 Jan;220(1):S445-7, Abstract 674.
LAS VEGAS – according to data shared in a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Race/ethnicity also had an impact on the likelihood that external cephalic version (ECV) would be successful.
In an interview, first author Ashley E. Skeith, a medical student at Oregon Health and Sciences University, Portland, said that various characteristics of a pregnancy may affect the success of ECV, but it wasn’t known which maternal characteristics might be associated with greater success of the maneuver.
She and her collaborators found that rates of success were high overall, but that 84% of women 68 inches or taller had successful ECVs, compared with 78% of women less than 60 inches tall. Rates were 82% and 83% for women 60-64 inches and 64-68 inches tall, respectively (adjusted odds ratio, 1.03; P less than .001).
The retrospective cohort study used data from 18,896 women who had singleton, breech, term gestations for whom ECV was attempted. Variables extracted from the medical record included maternal age, height, race, and prepregnancy body mass index (BMI).
For analysis, maternal BMI was grouped into four categories: underweight (BMI, less than 18.5 kg/m2), normal weight (BMI, 18.5-24.9 kg/m2), overweight (BMI, 25-29 kg/m2), and obese (BMI, greater than 30 kg/m2).
Women who were normal weight had the highest likelihood of a successful ECV, at 86%, followed by underweight women at 85%. Women who were overweight and obese had lower success rates, at 82% and 78%, respectively (aOR, 0.86; P less than .001).
Compared with white women, black women had an aOR of 0.60 for successful ECV (P less than .001). The aOR for successful ECV for Asian women was 0.71; for Hispanic women, the aOR was 0.82. American Indian and Alaska Native women were slightly more likely to have successful ECV than white women, but the difference was not significant after statistical adjustment.
Neither advanced maternal age (greater than 35 years) nor adolescent pregnancy were associated with decreased likelihood of successful ECV.
Potential confounders included maternal education level and insurance status, how much weight was gained during pregnancy, whether an epidural was administered, and whether the mother had diabetes. Multivariable regression analysis adjusted for these variables, said Ms. Skeith.
“External cephalic version is a safe procedure that reduces risk of cesarean delivery,” wrote Ms. Skeith and her colleagues. “Though fetal positioning and analgesia have been considered in the prediction of ECV success, [these] data [suggest] that maternal stature and race/ethnicity could be incorporated into potential prediction tools.”
Ms. Skeith reported no outside sources of funding or conflicts of interest.
SOURCE: Skeith AE et al. Am J Obstet Gynecol. 2019 Jan;220(1):S445-7, Abstract 674.
LAS VEGAS – according to data shared in a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Race/ethnicity also had an impact on the likelihood that external cephalic version (ECV) would be successful.
In an interview, first author Ashley E. Skeith, a medical student at Oregon Health and Sciences University, Portland, said that various characteristics of a pregnancy may affect the success of ECV, but it wasn’t known which maternal characteristics might be associated with greater success of the maneuver.
She and her collaborators found that rates of success were high overall, but that 84% of women 68 inches or taller had successful ECVs, compared with 78% of women less than 60 inches tall. Rates were 82% and 83% for women 60-64 inches and 64-68 inches tall, respectively (adjusted odds ratio, 1.03; P less than .001).
The retrospective cohort study used data from 18,896 women who had singleton, breech, term gestations for whom ECV was attempted. Variables extracted from the medical record included maternal age, height, race, and prepregnancy body mass index (BMI).
For analysis, maternal BMI was grouped into four categories: underweight (BMI, less than 18.5 kg/m2), normal weight (BMI, 18.5-24.9 kg/m2), overweight (BMI, 25-29 kg/m2), and obese (BMI, greater than 30 kg/m2).
Women who were normal weight had the highest likelihood of a successful ECV, at 86%, followed by underweight women at 85%. Women who were overweight and obese had lower success rates, at 82% and 78%, respectively (aOR, 0.86; P less than .001).
Compared with white women, black women had an aOR of 0.60 for successful ECV (P less than .001). The aOR for successful ECV for Asian women was 0.71; for Hispanic women, the aOR was 0.82. American Indian and Alaska Native women were slightly more likely to have successful ECV than white women, but the difference was not significant after statistical adjustment.
Neither advanced maternal age (greater than 35 years) nor adolescent pregnancy were associated with decreased likelihood of successful ECV.
Potential confounders included maternal education level and insurance status, how much weight was gained during pregnancy, whether an epidural was administered, and whether the mother had diabetes. Multivariable regression analysis adjusted for these variables, said Ms. Skeith.
“External cephalic version is a safe procedure that reduces risk of cesarean delivery,” wrote Ms. Skeith and her colleagues. “Though fetal positioning and analgesia have been considered in the prediction of ECV success, [these] data [suggest] that maternal stature and race/ethnicity could be incorporated into potential prediction tools.”
Ms. Skeith reported no outside sources of funding or conflicts of interest.
SOURCE: Skeith AE et al. Am J Obstet Gynecol. 2019 Jan;220(1):S445-7, Abstract 674.
REPORTING FROM THE PREGNANCY MEETING