User login
Osteoid osteoma of the talar neck is an unusual clinical condition that is often overlooked on initial assessment of patients with ankle pain. Here, we present a case report of an adolescent male with talar neck osteoid osteoma who reported persistent pain after an injury. We discuss the differential diagnosis of persistent anterior ankle pain and assess the treatment options for osteoid osteoma of the talar neck. The patient’s guardian provided written informed consent for print and electronic publication of this case report.
Case Report
A 13-year-old boy presented to our clinic 3 months after a right ankle sprain. He had visited the emergency department at the time of injury; radiographs of the ankle were reported negative for fractures, dislocations, or bone pathologies. He was treated conservatively with elastic support, icing, rest, elevation, and weight-bearing as tolerated. Upon presentation to our office, his pain involved the entire ankle joint. He had not put weight on it since the injury. On examination, he had a significant limp, anteromedial swelling, and tenderness over the ankle joint anteromedially. His neurologic and vascular examinations were normal.
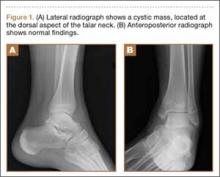
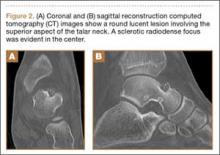
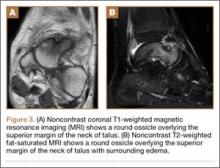
His plain radiographs showed a cystic mass, located at the dorsal aspect of the talar neck (Figures 1A, 1B). Computed tomography (CT) showed a round lucent lesion involving the superior aspect of the talar neck, measuring 9 mm by 6 mm. A sclerotic radiodense focus was evident in the center (Figures 2A, 2B). Noncontrast multiplanar, multisequence magnetic resonance imaging (MRI) showed abnormal edema throughout the talus and a 9-mm rounded ossicle overlying the superior margin of the neck of the talus (Figures 3A, 3B).
Differential Diagnosis
The differential diagnosis for anterior ankle pain includes ankle sprain, monoarticular arthritis, anterior ankle impingement, and talar neck fractures. Other related findings include the presence of a talar ridge and a talar beak.
Ankle sprains are very common injuries. The mainstay treatment consists of ice, resting, elevation, and elastic or semirigid support, and patients usually recover over the course of a few weeks. These sprains are typically injuries of the lateral or medial ligaments of the ankle. Extension of a ligament tear across the anterior capsule can explain persistent anterior ankle pain. The presence of a bony lesion on plain radiographs, however, makes the diagnosis of an ankle sprain, with or without extension into the anterior capsule, less likely.
Monoarticular arthritis, which may present in the ankle and has a wide differential diagnosis, usually involves the whole joint.
Anterior ankle impingement typically occurs in athletes who participate in sports that involve kicking. It can be a bony or soft-tissue impingent. Clinically, patients present with pain and loss of motion, specifically dorsiflexion.
Talar neck fractures are usually the result of high-energy trauma. Stress fractures of the neck of the talus are uncommon and are associated with a recent sudden increase in physical activity, such as running, dancing, or military training. Radiographs, CT scans, and MRI help define the fracture line.
The talar ridge is the site of capsular and ligamentous attachment on the superior aspect of the talar neck and may become hypertrophic in athletes. A hypertrophic talar ridge is asymptomatic and is not considered a pathologic finding on radiographs.
The talar beak, a flaring of the anterosuperior aspect of the talar head, is an indirect sign of tarsal coalition. When symptomatic, patients complain of subtalar symptoms, typically pain and limitation of motion. It usually does not present acutely.
Treatment
We offered the patient surgical excision, and his guardian consented to left ankle arthroscopy. We performed synovectomy using a combination of 3.5-mm shaver and radiofrequency probe. We identified the mass: round, soft, and located at the superior-medial aspect of the talar neck. We removed it in piecemeal fashion using manual arthroscopic instruments, and cauterized its base using the radiofrequency probe. We allowed the patient weight-bearing as tolerated starting the day after surgery.
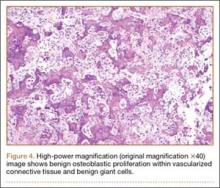
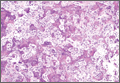
We submitted the specimen for pathologic evaluation (Figure 4). It consisted of multiple pieces of tan/brown tissue. Histologic examination showed benign osteoblastic proliferation composed of anastomosing bony trabeculae with variable mineralization, lined by plump osteoblasts, within vascularized connective tissue; benign giant cells were present, consistent with a nidus of an osteoid osteoma.
On the first postoperative visit, the patient was pain-free and bearing weight with crutches. He was gradually weaned from his crutches and returned to full weight-bearing over the next 4 weeks. At 12-month follow-up, he was symptom-free with good range of motion and full return to previous level of activity.
Discussion
Osteoid osteoma is a small, benign, well-circumscribed osteoblastic cortical lesion, typically identified in long bones or, less frequently, in the subperiosteal region.1 It often affects adolescents. Osteoid osteoma has been described in the talus in a few case series2-7 and is associated with a typical nidus that can be identified on CT scans. It does not present acutely, however. The typical presentation for osteoid osteoma is bone pain at night that responds to nonsteroidal anti-inflammatory drugs. However, this presentation is not universal and is frequently missed.2
Juxta-articular osteoid osteomas in the ankle and foot can be difficult to diagnose. The most common site is the talus.3 The majority of patients link their pain to a remote ankle injury. The time delay to diagnosis is on average 2.5 years, but it can be as long as 10 years.4-6 A CT scan is the best method to identify the nidus; MRI can be misleading if it shows only marrow edema but not a nidus.4,5,7 In our patient, an injury was documented, and the patient denied prior symptoms. We cannot explain how an injury would trigger the formation of an osteoid osteoma or cause a previously asymptomatic osteoid osteoma to become symptomatic.
Medical treatment with nonsteroidal anti-inflammatory drugs has been used but is reported to take 2 to 4 years for resolution of symptoms; many patients may consider the treatment time frame too long when other alternatives are available.8 These include open resection, arthroscopic resection, and image-guided ablation. Open surgical techniques include en bloc resection and curettage. Bone grafting or internal fixation may be performed as needed. Arthroscopic excision of juxta-articular osteoid osteomas offers the advantages of good visualization and avoidance of soft-tissue dissection, and allows for complete excision of the lesion as well as synovectomy.6,9,10 Arthroscopic excision also allows for quicker rehabilitation. Image-guided ablation, such as radionuclide-guided excision, CT-guided thermal ablation, and laser photocoagulation, may be even less invasive but do not allow for direct visualization, complete resection, and biopsy.11
Conclusion
Osteoid osteoma is a small, benign, well-circumscribed osteoblastic cortical lesion, typically identified in long bones or, less frequently, in the subperiosteal region.1 It often affects adolescents. Osteoid osteoma has been described in the talus in multiple case series and is associated with a typical nidus that can be identified on CT scans. Usually, it does not present acutely. The typical presentation for osteoid osteoma is bone pain at night that responds to nonsteroidal anti-inflammatory drugs. This presentation is not universal, however, and is frequently missed, especially when the pain is associated with a prior injury.2 Arthroscopic exploration of the ankle with resection of subperiosteal osteoid osteoma and the associated synovitis using thermal ablation of the base with radiofrequency offers lasting cure with minimal morbidity.
1. Edeiken J, DePalma AF, Hodes PJ. Osteoid osteoma. Clin Orthop Relat Res. 1966;49:201-206.
2. El Rayes MA, El Kordy S. Osteoid osteoma of the talus. Foot. 2003;13(3):166–168.
3. Capanna R, Van Horn JR, Ayala A, Picci P, Bettelli G. Osteoid osteoma and osteoblastoma of the talus. A report of 40 cases. Skeletal Radiol. 1986;15(5):360-364.
4. Chuang SY, Wang SJ, Au MK, Huang GS. Osteoid osteoma in talar neck: a report of two cases. Foot Ankle Int. 1998;19(1):44-47.
5. Snow SW, Sobel M, DiCarlo EF, Thompson FM, Deland JT. Chronic ankle pain caused by osteoid osteoma of the neck of the talus. Foot Ankle Int. 1997;18(2):98-101.
6. Yercan HS, Okcu G, Őzalp T, Ősiç U. Arthroscopic removal of the osteoid osteoma on the neck of the talus. Knee Surg Sports Traumatol Arthrosc. 2004;12(3):246-249.
7. Mazlout O, Saudan M, Ladeb MF, Garcia JF, Bianchi S. Osteoid osteoma of the talar neck: a diagnostic challenge. Eur J Radiol Extra. 2004;49(2):67-70.
8. Kneisl JS, Simon MA. Medical management compared with operative treatment for osteoid-osteoma. J Bone Joint Surg Am. 1992;74(2):179-185.
9. Bojanić I, Orlić D, Ivković A. Arthroscopic removal of a juxtaarticular osteoid osteoma of the talar neck. J Foot Ankle Surg. 2003;42(6):359-362.
10. Tüzüner S, Aydin AT. Arthroscopic removal of an osteoid osteoma at talar neck. Arthroscopy. 1998;14(4):405-409.
11. Amendola A, Vellet D, Willits K. Osteoid osteoma of the neck of the talus: percutaneous, computed tomography-guided technique for complete excision. Foot Ankle Int. 1994;15(8):429-432.
Osteoid osteoma of the talar neck is an unusual clinical condition that is often overlooked on initial assessment of patients with ankle pain. Here, we present a case report of an adolescent male with talar neck osteoid osteoma who reported persistent pain after an injury. We discuss the differential diagnosis of persistent anterior ankle pain and assess the treatment options for osteoid osteoma of the talar neck. The patient’s guardian provided written informed consent for print and electronic publication of this case report.
Case Report
A 13-year-old boy presented to our clinic 3 months after a right ankle sprain. He had visited the emergency department at the time of injury; radiographs of the ankle were reported negative for fractures, dislocations, or bone pathologies. He was treated conservatively with elastic support, icing, rest, elevation, and weight-bearing as tolerated. Upon presentation to our office, his pain involved the entire ankle joint. He had not put weight on it since the injury. On examination, he had a significant limp, anteromedial swelling, and tenderness over the ankle joint anteromedially. His neurologic and vascular examinations were normal.
His plain radiographs showed a cystic mass, located at the dorsal aspect of the talar neck (Figures 1A, 1B). Computed tomography (CT) showed a round lucent lesion involving the superior aspect of the talar neck, measuring 9 mm by 6 mm. A sclerotic radiodense focus was evident in the center (Figures 2A, 2B). Noncontrast multiplanar, multisequence magnetic resonance imaging (MRI) showed abnormal edema throughout the talus and a 9-mm rounded ossicle overlying the superior margin of the neck of the talus (Figures 3A, 3B).
Differential Diagnosis
The differential diagnosis for anterior ankle pain includes ankle sprain, monoarticular arthritis, anterior ankle impingement, and talar neck fractures. Other related findings include the presence of a talar ridge and a talar beak.
Ankle sprains are very common injuries. The mainstay treatment consists of ice, resting, elevation, and elastic or semirigid support, and patients usually recover over the course of a few weeks. These sprains are typically injuries of the lateral or medial ligaments of the ankle. Extension of a ligament tear across the anterior capsule can explain persistent anterior ankle pain. The presence of a bony lesion on plain radiographs, however, makes the diagnosis of an ankle sprain, with or without extension into the anterior capsule, less likely.
Monoarticular arthritis, which may present in the ankle and has a wide differential diagnosis, usually involves the whole joint.
Anterior ankle impingement typically occurs in athletes who participate in sports that involve kicking. It can be a bony or soft-tissue impingent. Clinically, patients present with pain and loss of motion, specifically dorsiflexion.
Talar neck fractures are usually the result of high-energy trauma. Stress fractures of the neck of the talus are uncommon and are associated with a recent sudden increase in physical activity, such as running, dancing, or military training. Radiographs, CT scans, and MRI help define the fracture line.
The talar ridge is the site of capsular and ligamentous attachment on the superior aspect of the talar neck and may become hypertrophic in athletes. A hypertrophic talar ridge is asymptomatic and is not considered a pathologic finding on radiographs.
The talar beak, a flaring of the anterosuperior aspect of the talar head, is an indirect sign of tarsal coalition. When symptomatic, patients complain of subtalar symptoms, typically pain and limitation of motion. It usually does not present acutely.
Treatment
We offered the patient surgical excision, and his guardian consented to left ankle arthroscopy. We performed synovectomy using a combination of 3.5-mm shaver and radiofrequency probe. We identified the mass: round, soft, and located at the superior-medial aspect of the talar neck. We removed it in piecemeal fashion using manual arthroscopic instruments, and cauterized its base using the radiofrequency probe. We allowed the patient weight-bearing as tolerated starting the day after surgery.
We submitted the specimen for pathologic evaluation (Figure 4). It consisted of multiple pieces of tan/brown tissue. Histologic examination showed benign osteoblastic proliferation composed of anastomosing bony trabeculae with variable mineralization, lined by plump osteoblasts, within vascularized connective tissue; benign giant cells were present, consistent with a nidus of an osteoid osteoma.
On the first postoperative visit, the patient was pain-free and bearing weight with crutches. He was gradually weaned from his crutches and returned to full weight-bearing over the next 4 weeks. At 12-month follow-up, he was symptom-free with good range of motion and full return to previous level of activity.
Discussion
Osteoid osteoma is a small, benign, well-circumscribed osteoblastic cortical lesion, typically identified in long bones or, less frequently, in the subperiosteal region.1 It often affects adolescents. Osteoid osteoma has been described in the talus in a few case series2-7 and is associated with a typical nidus that can be identified on CT scans. It does not present acutely, however. The typical presentation for osteoid osteoma is bone pain at night that responds to nonsteroidal anti-inflammatory drugs. However, this presentation is not universal and is frequently missed.2
Juxta-articular osteoid osteomas in the ankle and foot can be difficult to diagnose. The most common site is the talus.3 The majority of patients link their pain to a remote ankle injury. The time delay to diagnosis is on average 2.5 years, but it can be as long as 10 years.4-6 A CT scan is the best method to identify the nidus; MRI can be misleading if it shows only marrow edema but not a nidus.4,5,7 In our patient, an injury was documented, and the patient denied prior symptoms. We cannot explain how an injury would trigger the formation of an osteoid osteoma or cause a previously asymptomatic osteoid osteoma to become symptomatic.
Medical treatment with nonsteroidal anti-inflammatory drugs has been used but is reported to take 2 to 4 years for resolution of symptoms; many patients may consider the treatment time frame too long when other alternatives are available.8 These include open resection, arthroscopic resection, and image-guided ablation. Open surgical techniques include en bloc resection and curettage. Bone grafting or internal fixation may be performed as needed. Arthroscopic excision of juxta-articular osteoid osteomas offers the advantages of good visualization and avoidance of soft-tissue dissection, and allows for complete excision of the lesion as well as synovectomy.6,9,10 Arthroscopic excision also allows for quicker rehabilitation. Image-guided ablation, such as radionuclide-guided excision, CT-guided thermal ablation, and laser photocoagulation, may be even less invasive but do not allow for direct visualization, complete resection, and biopsy.11
Conclusion
Osteoid osteoma is a small, benign, well-circumscribed osteoblastic cortical lesion, typically identified in long bones or, less frequently, in the subperiosteal region.1 It often affects adolescents. Osteoid osteoma has been described in the talus in multiple case series and is associated with a typical nidus that can be identified on CT scans. Usually, it does not present acutely. The typical presentation for osteoid osteoma is bone pain at night that responds to nonsteroidal anti-inflammatory drugs. This presentation is not universal, however, and is frequently missed, especially when the pain is associated with a prior injury.2 Arthroscopic exploration of the ankle with resection of subperiosteal osteoid osteoma and the associated synovitis using thermal ablation of the base with radiofrequency offers lasting cure with minimal morbidity.
Osteoid osteoma of the talar neck is an unusual clinical condition that is often overlooked on initial assessment of patients with ankle pain. Here, we present a case report of an adolescent male with talar neck osteoid osteoma who reported persistent pain after an injury. We discuss the differential diagnosis of persistent anterior ankle pain and assess the treatment options for osteoid osteoma of the talar neck. The patient’s guardian provided written informed consent for print and electronic publication of this case report.
Case Report
A 13-year-old boy presented to our clinic 3 months after a right ankle sprain. He had visited the emergency department at the time of injury; radiographs of the ankle were reported negative for fractures, dislocations, or bone pathologies. He was treated conservatively with elastic support, icing, rest, elevation, and weight-bearing as tolerated. Upon presentation to our office, his pain involved the entire ankle joint. He had not put weight on it since the injury. On examination, he had a significant limp, anteromedial swelling, and tenderness over the ankle joint anteromedially. His neurologic and vascular examinations were normal.
His plain radiographs showed a cystic mass, located at the dorsal aspect of the talar neck (Figures 1A, 1B). Computed tomography (CT) showed a round lucent lesion involving the superior aspect of the talar neck, measuring 9 mm by 6 mm. A sclerotic radiodense focus was evident in the center (Figures 2A, 2B). Noncontrast multiplanar, multisequence magnetic resonance imaging (MRI) showed abnormal edema throughout the talus and a 9-mm rounded ossicle overlying the superior margin of the neck of the talus (Figures 3A, 3B).
Differential Diagnosis
The differential diagnosis for anterior ankle pain includes ankle sprain, monoarticular arthritis, anterior ankle impingement, and talar neck fractures. Other related findings include the presence of a talar ridge and a talar beak.
Ankle sprains are very common injuries. The mainstay treatment consists of ice, resting, elevation, and elastic or semirigid support, and patients usually recover over the course of a few weeks. These sprains are typically injuries of the lateral or medial ligaments of the ankle. Extension of a ligament tear across the anterior capsule can explain persistent anterior ankle pain. The presence of a bony lesion on plain radiographs, however, makes the diagnosis of an ankle sprain, with or without extension into the anterior capsule, less likely.
Monoarticular arthritis, which may present in the ankle and has a wide differential diagnosis, usually involves the whole joint.
Anterior ankle impingement typically occurs in athletes who participate in sports that involve kicking. It can be a bony or soft-tissue impingent. Clinically, patients present with pain and loss of motion, specifically dorsiflexion.
Talar neck fractures are usually the result of high-energy trauma. Stress fractures of the neck of the talus are uncommon and are associated with a recent sudden increase in physical activity, such as running, dancing, or military training. Radiographs, CT scans, and MRI help define the fracture line.
The talar ridge is the site of capsular and ligamentous attachment on the superior aspect of the talar neck and may become hypertrophic in athletes. A hypertrophic talar ridge is asymptomatic and is not considered a pathologic finding on radiographs.
The talar beak, a flaring of the anterosuperior aspect of the talar head, is an indirect sign of tarsal coalition. When symptomatic, patients complain of subtalar symptoms, typically pain and limitation of motion. It usually does not present acutely.
Treatment
We offered the patient surgical excision, and his guardian consented to left ankle arthroscopy. We performed synovectomy using a combination of 3.5-mm shaver and radiofrequency probe. We identified the mass: round, soft, and located at the superior-medial aspect of the talar neck. We removed it in piecemeal fashion using manual arthroscopic instruments, and cauterized its base using the radiofrequency probe. We allowed the patient weight-bearing as tolerated starting the day after surgery.
We submitted the specimen for pathologic evaluation (Figure 4). It consisted of multiple pieces of tan/brown tissue. Histologic examination showed benign osteoblastic proliferation composed of anastomosing bony trabeculae with variable mineralization, lined by plump osteoblasts, within vascularized connective tissue; benign giant cells were present, consistent with a nidus of an osteoid osteoma.
On the first postoperative visit, the patient was pain-free and bearing weight with crutches. He was gradually weaned from his crutches and returned to full weight-bearing over the next 4 weeks. At 12-month follow-up, he was symptom-free with good range of motion and full return to previous level of activity.
Discussion
Osteoid osteoma is a small, benign, well-circumscribed osteoblastic cortical lesion, typically identified in long bones or, less frequently, in the subperiosteal region.1 It often affects adolescents. Osteoid osteoma has been described in the talus in a few case series2-7 and is associated with a typical nidus that can be identified on CT scans. It does not present acutely, however. The typical presentation for osteoid osteoma is bone pain at night that responds to nonsteroidal anti-inflammatory drugs. However, this presentation is not universal and is frequently missed.2
Juxta-articular osteoid osteomas in the ankle and foot can be difficult to diagnose. The most common site is the talus.3 The majority of patients link their pain to a remote ankle injury. The time delay to diagnosis is on average 2.5 years, but it can be as long as 10 years.4-6 A CT scan is the best method to identify the nidus; MRI can be misleading if it shows only marrow edema but not a nidus.4,5,7 In our patient, an injury was documented, and the patient denied prior symptoms. We cannot explain how an injury would trigger the formation of an osteoid osteoma or cause a previously asymptomatic osteoid osteoma to become symptomatic.
Medical treatment with nonsteroidal anti-inflammatory drugs has been used but is reported to take 2 to 4 years for resolution of symptoms; many patients may consider the treatment time frame too long when other alternatives are available.8 These include open resection, arthroscopic resection, and image-guided ablation. Open surgical techniques include en bloc resection and curettage. Bone grafting or internal fixation may be performed as needed. Arthroscopic excision of juxta-articular osteoid osteomas offers the advantages of good visualization and avoidance of soft-tissue dissection, and allows for complete excision of the lesion as well as synovectomy.6,9,10 Arthroscopic excision also allows for quicker rehabilitation. Image-guided ablation, such as radionuclide-guided excision, CT-guided thermal ablation, and laser photocoagulation, may be even less invasive but do not allow for direct visualization, complete resection, and biopsy.11
Conclusion
Osteoid osteoma is a small, benign, well-circumscribed osteoblastic cortical lesion, typically identified in long bones or, less frequently, in the subperiosteal region.1 It often affects adolescents. Osteoid osteoma has been described in the talus in multiple case series and is associated with a typical nidus that can be identified on CT scans. Usually, it does not present acutely. The typical presentation for osteoid osteoma is bone pain at night that responds to nonsteroidal anti-inflammatory drugs. This presentation is not universal, however, and is frequently missed, especially when the pain is associated with a prior injury.2 Arthroscopic exploration of the ankle with resection of subperiosteal osteoid osteoma and the associated synovitis using thermal ablation of the base with radiofrequency offers lasting cure with minimal morbidity.
1. Edeiken J, DePalma AF, Hodes PJ. Osteoid osteoma. Clin Orthop Relat Res. 1966;49:201-206.
2. El Rayes MA, El Kordy S. Osteoid osteoma of the talus. Foot. 2003;13(3):166–168.
3. Capanna R, Van Horn JR, Ayala A, Picci P, Bettelli G. Osteoid osteoma and osteoblastoma of the talus. A report of 40 cases. Skeletal Radiol. 1986;15(5):360-364.
4. Chuang SY, Wang SJ, Au MK, Huang GS. Osteoid osteoma in talar neck: a report of two cases. Foot Ankle Int. 1998;19(1):44-47.
5. Snow SW, Sobel M, DiCarlo EF, Thompson FM, Deland JT. Chronic ankle pain caused by osteoid osteoma of the neck of the talus. Foot Ankle Int. 1997;18(2):98-101.
6. Yercan HS, Okcu G, Őzalp T, Ősiç U. Arthroscopic removal of the osteoid osteoma on the neck of the talus. Knee Surg Sports Traumatol Arthrosc. 2004;12(3):246-249.
7. Mazlout O, Saudan M, Ladeb MF, Garcia JF, Bianchi S. Osteoid osteoma of the talar neck: a diagnostic challenge. Eur J Radiol Extra. 2004;49(2):67-70.
8. Kneisl JS, Simon MA. Medical management compared with operative treatment for osteoid-osteoma. J Bone Joint Surg Am. 1992;74(2):179-185.
9. Bojanić I, Orlić D, Ivković A. Arthroscopic removal of a juxtaarticular osteoid osteoma of the talar neck. J Foot Ankle Surg. 2003;42(6):359-362.
10. Tüzüner S, Aydin AT. Arthroscopic removal of an osteoid osteoma at talar neck. Arthroscopy. 1998;14(4):405-409.
11. Amendola A, Vellet D, Willits K. Osteoid osteoma of the neck of the talus: percutaneous, computed tomography-guided technique for complete excision. Foot Ankle Int. 1994;15(8):429-432.
1. Edeiken J, DePalma AF, Hodes PJ. Osteoid osteoma. Clin Orthop Relat Res. 1966;49:201-206.
2. El Rayes MA, El Kordy S. Osteoid osteoma of the talus. Foot. 2003;13(3):166–168.
3. Capanna R, Van Horn JR, Ayala A, Picci P, Bettelli G. Osteoid osteoma and osteoblastoma of the talus. A report of 40 cases. Skeletal Radiol. 1986;15(5):360-364.
4. Chuang SY, Wang SJ, Au MK, Huang GS. Osteoid osteoma in talar neck: a report of two cases. Foot Ankle Int. 1998;19(1):44-47.
5. Snow SW, Sobel M, DiCarlo EF, Thompson FM, Deland JT. Chronic ankle pain caused by osteoid osteoma of the neck of the talus. Foot Ankle Int. 1997;18(2):98-101.
6. Yercan HS, Okcu G, Őzalp T, Ősiç U. Arthroscopic removal of the osteoid osteoma on the neck of the talus. Knee Surg Sports Traumatol Arthrosc. 2004;12(3):246-249.
7. Mazlout O, Saudan M, Ladeb MF, Garcia JF, Bianchi S. Osteoid osteoma of the talar neck: a diagnostic challenge. Eur J Radiol Extra. 2004;49(2):67-70.
8. Kneisl JS, Simon MA. Medical management compared with operative treatment for osteoid-osteoma. J Bone Joint Surg Am. 1992;74(2):179-185.
9. Bojanić I, Orlić D, Ivković A. Arthroscopic removal of a juxtaarticular osteoid osteoma of the talar neck. J Foot Ankle Surg. 2003;42(6):359-362.
10. Tüzüner S, Aydin AT. Arthroscopic removal of an osteoid osteoma at talar neck. Arthroscopy. 1998;14(4):405-409.
11. Amendola A, Vellet D, Willits K. Osteoid osteoma of the neck of the talus: percutaneous, computed tomography-guided technique for complete excision. Foot Ankle Int. 1994;15(8):429-432.