User login
A 67-year-old woman presented with multiple painful nodules that had developed on her scalp, face, and neck over the course of 1 year. She also had a few nodules on her trunk and hip. There was no associated bleeding, ulceration, or drainage from the lesions. She had no systemic symptoms. The patient reported that she’d had a similar lesion on her frontal scalp about 15 years earlier, and it was excised completely. (She was not aware of the diagnosis.) She indicated that her mother and son had similar lesions in the past.
Her medical history was remarkable for diabetes and hypertension, which were well controlled on metformin and lisinopril, respectively. The patient had cancer of the left breast that was treated with mastectomy and chemotherapy 3 years prior.
On physical examination, the patient had multiple firm, rubbery, tender nodules with tan or pink hue, measuring 1 to 1.5 cm. The nodules were located on the left side of her chin and right preauricular area (FIGURE 1), as well as the right sides of her neck and hip. Most of the nodules were solitary; the preauricular area had 2 clustered pink lesions. The largest nodule was located on the patient’s chin and had overlying telangiectasias.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Cylindroma
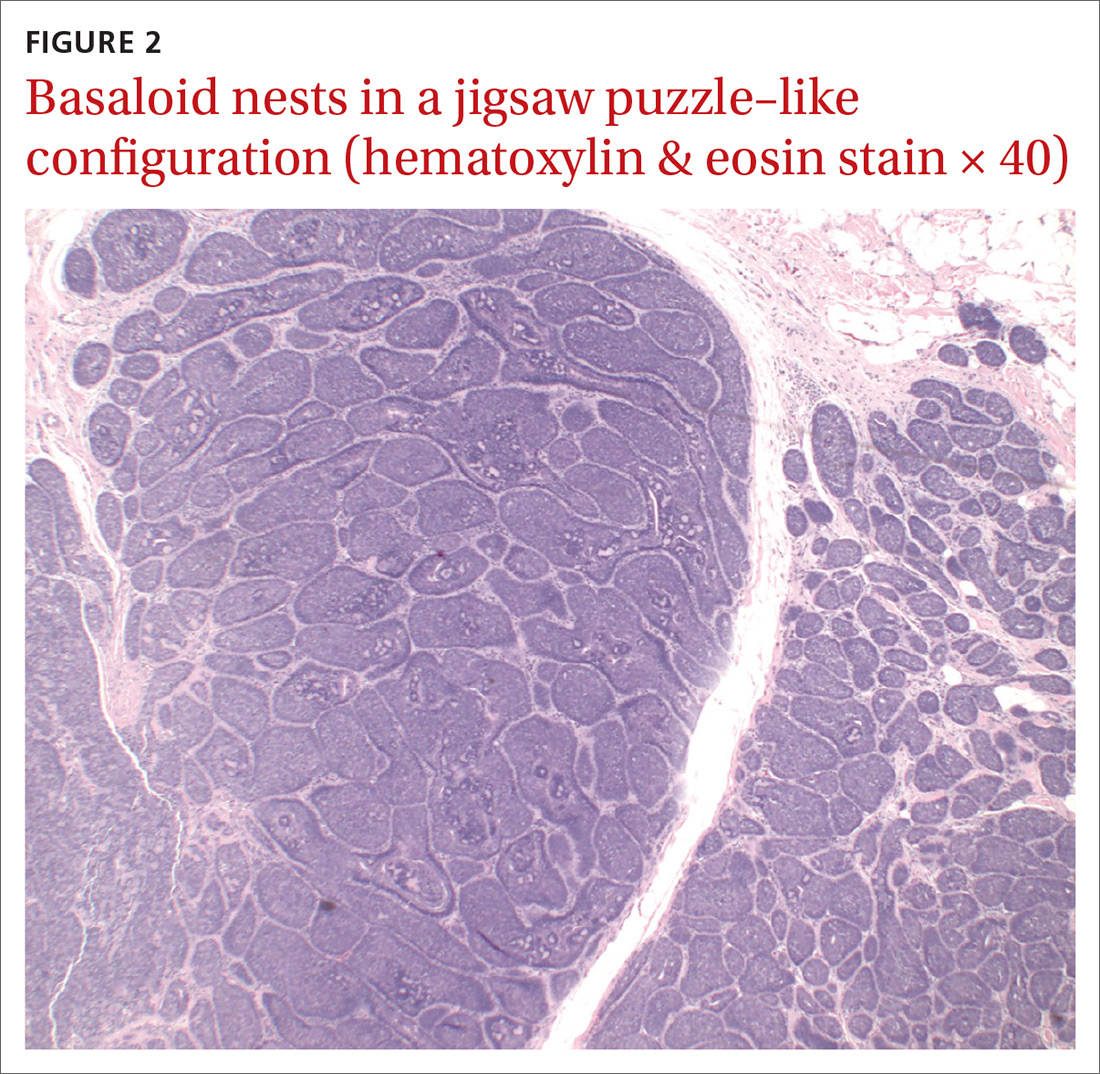
Definitive diagnosis was made by shave biopsy of the left hip lesion. Histopathology demonstrated various-sized discrete aggregates of basaloid cell nests in a jigsaw puzzle–like configuration (FIGURE 2), surrounded by rims of homogenous eosinophilic material. Histologic findings were consistent with cylindroma.1
Rare with a female predominance. Solitary cylindromas occur sporadically and usually affect middle-aged and elderly patients. Incidence is rare, but there is a female predominance of 6 to 9:1.2 Clinical appearance shows a slow-growing, firm mass that can range from a few millimeters to a few centimeters in diameter. The masses can have a pink or blue hue and usually are nontender unless there is nerve impingement.2
If multiple tumors are present or the patient has a family history of similar lesions, the disorder is likely inherited in an autosomal dominant pattern (with variable expression), which can be associated with Brooke-Spiegler syndrome. This syndrome is related to a mutation of the cylindromatosis gene on chromosome 16. This is a tumor suppressor gene, inactivation of which can lead to uninhibited action of NF-
Rarely, cylindromas can undergo malignant transformation; signs include ulceration, bleeding, rapid growth, or color change.2 In these cases, appropriate imaging such as computed tomography, magnetic resonance imaging, or positron emission tomography should be sought as there have been case reports of cylindroma extension to bone, as well as metastases to sites including the lymph nodes, thyroid, liver, lungs, bones, and meninges.4
Lipomas and pilar cysts comprise the differential
Lipomas are soft, painless, flesh-colored masses that typically appear on the trunk and arms but are uncommon on the face. Telangiectasias are not seen.
Continue to: Pilar cysts
Pilar cysts can mimic cylindromas in clinical presentation. Derived from the root sheath of hair follicles, they typically appear on the scalp but rarely on the face. Pilar cysts are slow growing, firm, and whitish in color5; several cysts can appear at a time.
Pilomatricomas are firm skin masses—usually < 3 cm in size—that can vary in color. There may be an extrusion of calcified material within the nodules, which does not occur in cylindromas.
Sebaceous adenomas are yellowish papules, usually < 1 cm in size, that appear on the head and neck area.6
Making the diagnosis. The clinical appearance of cylindromas and their location will point to the diagnosis, as will a family history of similar lesions. Ultimately, the diagnosis is confirmed by biopsy.
Treatment mainstay includes excision
Complete excision of all lesions is key due to the possibility of malignant transformation and metastasis. Options for removal include electrodesiccation, curettage, cryosurgery,3 high-dose radiation, and the use of a CO2 laser.2 For multiple large tumors, or ones in cosmetically sensitive areas, consider referral to Dermatology or Plastic Surgery. Further imaging should be sought to rule out extension to bone or metastasis. Patients with multiple cylindromas and Brooke-Spiegler syndrome need lifelong follow-up to monitor for recurrence and malignant transformation.3,7,8
Continue to: Our patient...
Our patient underwent complete excision of the left hip lesion. Other trunk lesions were excised serially. The patient was referred to a surgeon specializing in Mohs micrographic surgery for excision of the facial lesions. The patient and her family members were referred for genetic testing.
CORRESPONDENCE
Zeeshan Afzal, MD, McAllen Family Medicine Residency Program, University of Texas Rio Grande Valley, 205 E Toronto Ave, McAllen, TX 78503; Drzeeshanafzal@gmail.com
1. Elder D, Elenitsas R, Jaworsky CH, et al. Tumors of the epidermal appendages. Lever’s Histopathology of the Skin. 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1999:775-777.
2. Singh DD, Naujoks C, Depprich R, et al. Cylindroma of head and neck: Review of the literature and report of two rare cases. J Craniomaxillofac Surg. 2013;41:516-521.
3. Sicinska J, Rakowska A, Czuwara-Ladykowska J, et al. Cylindroma transforming into basal cell carcinoma in a patient with Brooke-Spiegler syndrome. J Dermatol Case Rep. 2007;1:4-9.
4. Jordão C, de Magalhães TC, Cuzzi T, et al. Cylindroma: an update. Int J Dermatol. 2015;54:275-278.
5. Stone M. Cysts. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:1920.
6. McCalmont T, Pincus L. Adnexal neoplasms. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:1938-1942.
7. Gerretsen AL, Van der Putte SC, Deenstra W, et al. Cutaneous cylindroma with malignant transformation. Cancer. 1993;72:1618-1623.
8. Manicketh I, Singh R, Ghosh PK. Eccrine cylindroma of the face and scalp. Indian Dermatol Online J. 2016;7:203-205.
A 67-year-old woman presented with multiple painful nodules that had developed on her scalp, face, and neck over the course of 1 year. She also had a few nodules on her trunk and hip. There was no associated bleeding, ulceration, or drainage from the lesions. She had no systemic symptoms. The patient reported that she’d had a similar lesion on her frontal scalp about 15 years earlier, and it was excised completely. (She was not aware of the diagnosis.) She indicated that her mother and son had similar lesions in the past.
Her medical history was remarkable for diabetes and hypertension, which were well controlled on metformin and lisinopril, respectively. The patient had cancer of the left breast that was treated with mastectomy and chemotherapy 3 years prior.
On physical examination, the patient had multiple firm, rubbery, tender nodules with tan or pink hue, measuring 1 to 1.5 cm. The nodules were located on the left side of her chin and right preauricular area (FIGURE 1), as well as the right sides of her neck and hip. Most of the nodules were solitary; the preauricular area had 2 clustered pink lesions. The largest nodule was located on the patient’s chin and had overlying telangiectasias.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Cylindroma
Definitive diagnosis was made by shave biopsy of the left hip lesion. Histopathology demonstrated various-sized discrete aggregates of basaloid cell nests in a jigsaw puzzle–like configuration (FIGURE 2), surrounded by rims of homogenous eosinophilic material. Histologic findings were consistent with cylindroma.1
Rare with a female predominance. Solitary cylindromas occur sporadically and usually affect middle-aged and elderly patients. Incidence is rare, but there is a female predominance of 6 to 9:1.2 Clinical appearance shows a slow-growing, firm mass that can range from a few millimeters to a few centimeters in diameter. The masses can have a pink or blue hue and usually are nontender unless there is nerve impingement.2
If multiple tumors are present or the patient has a family history of similar lesions, the disorder is likely inherited in an autosomal dominant pattern (with variable expression), which can be associated with Brooke-Spiegler syndrome. This syndrome is related to a mutation of the cylindromatosis gene on chromosome 16. This is a tumor suppressor gene, inactivation of which can lead to uninhibited action of NF-
Rarely, cylindromas can undergo malignant transformation; signs include ulceration, bleeding, rapid growth, or color change.2 In these cases, appropriate imaging such as computed tomography, magnetic resonance imaging, or positron emission tomography should be sought as there have been case reports of cylindroma extension to bone, as well as metastases to sites including the lymph nodes, thyroid, liver, lungs, bones, and meninges.4
Lipomas and pilar cysts comprise the differential
Lipomas are soft, painless, flesh-colored masses that typically appear on the trunk and arms but are uncommon on the face. Telangiectasias are not seen.
Continue to: Pilar cysts
Pilar cysts can mimic cylindromas in clinical presentation. Derived from the root sheath of hair follicles, they typically appear on the scalp but rarely on the face. Pilar cysts are slow growing, firm, and whitish in color5; several cysts can appear at a time.
Pilomatricomas are firm skin masses—usually < 3 cm in size—that can vary in color. There may be an extrusion of calcified material within the nodules, which does not occur in cylindromas.
Sebaceous adenomas are yellowish papules, usually < 1 cm in size, that appear on the head and neck area.6
Making the diagnosis. The clinical appearance of cylindromas and their location will point to the diagnosis, as will a family history of similar lesions. Ultimately, the diagnosis is confirmed by biopsy.
Treatment mainstay includes excision
Complete excision of all lesions is key due to the possibility of malignant transformation and metastasis. Options for removal include electrodesiccation, curettage, cryosurgery,3 high-dose radiation, and the use of a CO2 laser.2 For multiple large tumors, or ones in cosmetically sensitive areas, consider referral to Dermatology or Plastic Surgery. Further imaging should be sought to rule out extension to bone or metastasis. Patients with multiple cylindromas and Brooke-Spiegler syndrome need lifelong follow-up to monitor for recurrence and malignant transformation.3,7,8
Continue to: Our patient...
Our patient underwent complete excision of the left hip lesion. Other trunk lesions were excised serially. The patient was referred to a surgeon specializing in Mohs micrographic surgery for excision of the facial lesions. The patient and her family members were referred for genetic testing.
CORRESPONDENCE
Zeeshan Afzal, MD, McAllen Family Medicine Residency Program, University of Texas Rio Grande Valley, 205 E Toronto Ave, McAllen, TX 78503; Drzeeshanafzal@gmail.com
A 67-year-old woman presented with multiple painful nodules that had developed on her scalp, face, and neck over the course of 1 year. She also had a few nodules on her trunk and hip. There was no associated bleeding, ulceration, or drainage from the lesions. She had no systemic symptoms. The patient reported that she’d had a similar lesion on her frontal scalp about 15 years earlier, and it was excised completely. (She was not aware of the diagnosis.) She indicated that her mother and son had similar lesions in the past.
Her medical history was remarkable for diabetes and hypertension, which were well controlled on metformin and lisinopril, respectively. The patient had cancer of the left breast that was treated with mastectomy and chemotherapy 3 years prior.
On physical examination, the patient had multiple firm, rubbery, tender nodules with tan or pink hue, measuring 1 to 1.5 cm. The nodules were located on the left side of her chin and right preauricular area (FIGURE 1), as well as the right sides of her neck and hip. Most of the nodules were solitary; the preauricular area had 2 clustered pink lesions. The largest nodule was located on the patient’s chin and had overlying telangiectasias.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Cylindroma
Definitive diagnosis was made by shave biopsy of the left hip lesion. Histopathology demonstrated various-sized discrete aggregates of basaloid cell nests in a jigsaw puzzle–like configuration (FIGURE 2), surrounded by rims of homogenous eosinophilic material. Histologic findings were consistent with cylindroma.1
Rare with a female predominance. Solitary cylindromas occur sporadically and usually affect middle-aged and elderly patients. Incidence is rare, but there is a female predominance of 6 to 9:1.2 Clinical appearance shows a slow-growing, firm mass that can range from a few millimeters to a few centimeters in diameter. The masses can have a pink or blue hue and usually are nontender unless there is nerve impingement.2
If multiple tumors are present or the patient has a family history of similar lesions, the disorder is likely inherited in an autosomal dominant pattern (with variable expression), which can be associated with Brooke-Spiegler syndrome. This syndrome is related to a mutation of the cylindromatosis gene on chromosome 16. This is a tumor suppressor gene, inactivation of which can lead to uninhibited action of NF-
Rarely, cylindromas can undergo malignant transformation; signs include ulceration, bleeding, rapid growth, or color change.2 In these cases, appropriate imaging such as computed tomography, magnetic resonance imaging, or positron emission tomography should be sought as there have been case reports of cylindroma extension to bone, as well as metastases to sites including the lymph nodes, thyroid, liver, lungs, bones, and meninges.4
Lipomas and pilar cysts comprise the differential
Lipomas are soft, painless, flesh-colored masses that typically appear on the trunk and arms but are uncommon on the face. Telangiectasias are not seen.
Continue to: Pilar cysts
Pilar cysts can mimic cylindromas in clinical presentation. Derived from the root sheath of hair follicles, they typically appear on the scalp but rarely on the face. Pilar cysts are slow growing, firm, and whitish in color5; several cysts can appear at a time.
Pilomatricomas are firm skin masses—usually < 3 cm in size—that can vary in color. There may be an extrusion of calcified material within the nodules, which does not occur in cylindromas.
Sebaceous adenomas are yellowish papules, usually < 1 cm in size, that appear on the head and neck area.6
Making the diagnosis. The clinical appearance of cylindromas and their location will point to the diagnosis, as will a family history of similar lesions. Ultimately, the diagnosis is confirmed by biopsy.
Treatment mainstay includes excision
Complete excision of all lesions is key due to the possibility of malignant transformation and metastasis. Options for removal include electrodesiccation, curettage, cryosurgery,3 high-dose radiation, and the use of a CO2 laser.2 For multiple large tumors, or ones in cosmetically sensitive areas, consider referral to Dermatology or Plastic Surgery. Further imaging should be sought to rule out extension to bone or metastasis. Patients with multiple cylindromas and Brooke-Spiegler syndrome need lifelong follow-up to monitor for recurrence and malignant transformation.3,7,8
Continue to: Our patient...
Our patient underwent complete excision of the left hip lesion. Other trunk lesions were excised serially. The patient was referred to a surgeon specializing in Mohs micrographic surgery for excision of the facial lesions. The patient and her family members were referred for genetic testing.
CORRESPONDENCE
Zeeshan Afzal, MD, McAllen Family Medicine Residency Program, University of Texas Rio Grande Valley, 205 E Toronto Ave, McAllen, TX 78503; Drzeeshanafzal@gmail.com
1. Elder D, Elenitsas R, Jaworsky CH, et al. Tumors of the epidermal appendages. Lever’s Histopathology of the Skin. 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1999:775-777.
2. Singh DD, Naujoks C, Depprich R, et al. Cylindroma of head and neck: Review of the literature and report of two rare cases. J Craniomaxillofac Surg. 2013;41:516-521.
3. Sicinska J, Rakowska A, Czuwara-Ladykowska J, et al. Cylindroma transforming into basal cell carcinoma in a patient with Brooke-Spiegler syndrome. J Dermatol Case Rep. 2007;1:4-9.
4. Jordão C, de Magalhães TC, Cuzzi T, et al. Cylindroma: an update. Int J Dermatol. 2015;54:275-278.
5. Stone M. Cysts. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:1920.
6. McCalmont T, Pincus L. Adnexal neoplasms. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:1938-1942.
7. Gerretsen AL, Van der Putte SC, Deenstra W, et al. Cutaneous cylindroma with malignant transformation. Cancer. 1993;72:1618-1623.
8. Manicketh I, Singh R, Ghosh PK. Eccrine cylindroma of the face and scalp. Indian Dermatol Online J. 2016;7:203-205.
1. Elder D, Elenitsas R, Jaworsky CH, et al. Tumors of the epidermal appendages. Lever’s Histopathology of the Skin. 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1999:775-777.
2. Singh DD, Naujoks C, Depprich R, et al. Cylindroma of head and neck: Review of the literature and report of two rare cases. J Craniomaxillofac Surg. 2013;41:516-521.
3. Sicinska J, Rakowska A, Czuwara-Ladykowska J, et al. Cylindroma transforming into basal cell carcinoma in a patient with Brooke-Spiegler syndrome. J Dermatol Case Rep. 2007;1:4-9.
4. Jordão C, de Magalhães TC, Cuzzi T, et al. Cylindroma: an update. Int J Dermatol. 2015;54:275-278.
5. Stone M. Cysts. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:1920.
6. McCalmont T, Pincus L. Adnexal neoplasms. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:1938-1942.
7. Gerretsen AL, Van der Putte SC, Deenstra W, et al. Cutaneous cylindroma with malignant transformation. Cancer. 1993;72:1618-1623.
8. Manicketh I, Singh R, Ghosh PK. Eccrine cylindroma of the face and scalp. Indian Dermatol Online J. 2016;7:203-205.