User login
ORLANDO – Good data suggest that marijuana has legitimate medical indications, but smoking the drug is not the appropriate method of delivery, and clinicians without experience with marijuana should consider its many liabilities before issuing a prescription, according to an expert who said he is not antimarijuana and has prescribed this therapy himself.
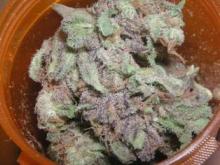
“Dried cannabis is not a medication in any traditional sense of the word. That does not mean cannabinoids have no legitimate indication as therapeutic agents, but smoking anything for your health is something of an oxymoron,” Dr. Douglas L. Gourlay of the departments of anesthesiology and psychiatry at the University of Toronto said at the Pain Care for Primary Care meeting.
Cannabis, distinct from cannabinoids, is defined as the dried leaves of the marijuana plant. According to Dr. Gourlay, who spoke at the meeting, which was cosponsored by the Journal of Family Practice, the plant has more than 400 compounds, including more than 60 cannabinoids, which are chemicals that act on cannabinoid receptors, primarily in the central nervous system. For physicians wishing to deliver cannabinoids for a medical indication, the problem posed by cannabis is quality control.
“You are being asked to prescribe something for which you have no practical means of titrating the dose,” Dr. Gourlay said. Even ignoring the potential risks of exposing the lungs to a variety of oxidized chemicals with no known therapeutic benefit, the absence of quality control will be problematic if the patient or family members subsequently claim iatrogenic harm.
For recreational use of cannabis, the focus has been on the concentration of tetrahydrocannabinol (THC), which is the cannabinoid most closely associated with euphoric effects. However, the potential medical benefits of marijuana, such as relief of glaucoma symptoms, reduction of chemotherapy-induced nausea, or control of neuropathic pain, are not necessarily related to THC. Well-designed clinical studies aimed at determining which other cannabinoids and at which doses are most relevant for medical use have yet to be performed, Dr. Gourlay said.
For the clinician, legalization of medical marijuana in the absence of reliable data on best practice creates some potential risks. According to Dr. Gourlay, patients who harm themselves or others in an accident attributed to impaired judgment from medical marijuana might pursue legal action against the prescribing physician. The relative absence of standards regarding marijuana use would complicate the defense.
“Unless you can competently discuss the pros and cons of herbal cannabis, including indications and contraindications that are relevant to informed consent, you would be wise to consider carefully any decision to prescribe,” Dr. Gourlay suggested.
The problem for many clinicians, according to Dr. Gourlay, is that patients often are already using marijuana and employ a variety of strategies to induce the physician to provide a prescription to legitimize this activity. He outlined several familiar traps that he urged physicians to avoid. These include claims by patients that a prescription would protect them from legal problems for a drug they will be using in any event or that clinicians can provide a dosing regimen that can be the basis for a plan to eventually taper use.
“Once you start down this road, it will be very difficult to change course,” said Dr. Gourlay, noting that even a discussion of marijuana should be well documented so that there are no misinterpretations regarding instructions about use or avoiding use. In situations in which patients are insistent about their need for marijuana, “consider having a third party in the room,” he suggested.
In areas where cannabinoids are available in well-defined concentrations for oral delivery, a stronger case can be made for medicinal applications, but clinical studies still remain limited, Dr. Gourlay said. He said he hopes trials will eventually be conducted to gauge the benefit-to-risk ratio for specific indications.
“I am not anticannabinoids, but I have never prescribed cannabis to smoke,” Dr. Gourlay reported. Even though recent legislation now permits recreational use of marijuana in several states, Dr. Gourlay urged clinicians to employ a conservative approach to clinical use until more data clarify both the drug’s benefits and safety.
The Journal of Family Practice and this news organization are owned by the same company.
The meeting was held by the American Pain Society and Global Academy for Medical Education. Global Academy and this news organization are owned the same company.
This post has been updated 8/5/2015.
ORLANDO – Good data suggest that marijuana has legitimate medical indications, but smoking the drug is not the appropriate method of delivery, and clinicians without experience with marijuana should consider its many liabilities before issuing a prescription, according to an expert who said he is not antimarijuana and has prescribed this therapy himself.
“Dried cannabis is not a medication in any traditional sense of the word. That does not mean cannabinoids have no legitimate indication as therapeutic agents, but smoking anything for your health is something of an oxymoron,” Dr. Douglas L. Gourlay of the departments of anesthesiology and psychiatry at the University of Toronto said at the Pain Care for Primary Care meeting.
Cannabis, distinct from cannabinoids, is defined as the dried leaves of the marijuana plant. According to Dr. Gourlay, who spoke at the meeting, which was cosponsored by the Journal of Family Practice, the plant has more than 400 compounds, including more than 60 cannabinoids, which are chemicals that act on cannabinoid receptors, primarily in the central nervous system. For physicians wishing to deliver cannabinoids for a medical indication, the problem posed by cannabis is quality control.
“You are being asked to prescribe something for which you have no practical means of titrating the dose,” Dr. Gourlay said. Even ignoring the potential risks of exposing the lungs to a variety of oxidized chemicals with no known therapeutic benefit, the absence of quality control will be problematic if the patient or family members subsequently claim iatrogenic harm.
For recreational use of cannabis, the focus has been on the concentration of tetrahydrocannabinol (THC), which is the cannabinoid most closely associated with euphoric effects. However, the potential medical benefits of marijuana, such as relief of glaucoma symptoms, reduction of chemotherapy-induced nausea, or control of neuropathic pain, are not necessarily related to THC. Well-designed clinical studies aimed at determining which other cannabinoids and at which doses are most relevant for medical use have yet to be performed, Dr. Gourlay said.
For the clinician, legalization of medical marijuana in the absence of reliable data on best practice creates some potential risks. According to Dr. Gourlay, patients who harm themselves or others in an accident attributed to impaired judgment from medical marijuana might pursue legal action against the prescribing physician. The relative absence of standards regarding marijuana use would complicate the defense.
“Unless you can competently discuss the pros and cons of herbal cannabis, including indications and contraindications that are relevant to informed consent, you would be wise to consider carefully any decision to prescribe,” Dr. Gourlay suggested.
The problem for many clinicians, according to Dr. Gourlay, is that patients often are already using marijuana and employ a variety of strategies to induce the physician to provide a prescription to legitimize this activity. He outlined several familiar traps that he urged physicians to avoid. These include claims by patients that a prescription would protect them from legal problems for a drug they will be using in any event or that clinicians can provide a dosing regimen that can be the basis for a plan to eventually taper use.
“Once you start down this road, it will be very difficult to change course,” said Dr. Gourlay, noting that even a discussion of marijuana should be well documented so that there are no misinterpretations regarding instructions about use or avoiding use. In situations in which patients are insistent about their need for marijuana, “consider having a third party in the room,” he suggested.
In areas where cannabinoids are available in well-defined concentrations for oral delivery, a stronger case can be made for medicinal applications, but clinical studies still remain limited, Dr. Gourlay said. He said he hopes trials will eventually be conducted to gauge the benefit-to-risk ratio for specific indications.
“I am not anticannabinoids, but I have never prescribed cannabis to smoke,” Dr. Gourlay reported. Even though recent legislation now permits recreational use of marijuana in several states, Dr. Gourlay urged clinicians to employ a conservative approach to clinical use until more data clarify both the drug’s benefits and safety.
The Journal of Family Practice and this news organization are owned by the same company.
The meeting was held by the American Pain Society and Global Academy for Medical Education. Global Academy and this news organization are owned the same company.
This post has been updated 8/5/2015.
ORLANDO – Good data suggest that marijuana has legitimate medical indications, but smoking the drug is not the appropriate method of delivery, and clinicians without experience with marijuana should consider its many liabilities before issuing a prescription, according to an expert who said he is not antimarijuana and has prescribed this therapy himself.
“Dried cannabis is not a medication in any traditional sense of the word. That does not mean cannabinoids have no legitimate indication as therapeutic agents, but smoking anything for your health is something of an oxymoron,” Dr. Douglas L. Gourlay of the departments of anesthesiology and psychiatry at the University of Toronto said at the Pain Care for Primary Care meeting.
Cannabis, distinct from cannabinoids, is defined as the dried leaves of the marijuana plant. According to Dr. Gourlay, who spoke at the meeting, which was cosponsored by the Journal of Family Practice, the plant has more than 400 compounds, including more than 60 cannabinoids, which are chemicals that act on cannabinoid receptors, primarily in the central nervous system. For physicians wishing to deliver cannabinoids for a medical indication, the problem posed by cannabis is quality control.
“You are being asked to prescribe something for which you have no practical means of titrating the dose,” Dr. Gourlay said. Even ignoring the potential risks of exposing the lungs to a variety of oxidized chemicals with no known therapeutic benefit, the absence of quality control will be problematic if the patient or family members subsequently claim iatrogenic harm.
For recreational use of cannabis, the focus has been on the concentration of tetrahydrocannabinol (THC), which is the cannabinoid most closely associated with euphoric effects. However, the potential medical benefits of marijuana, such as relief of glaucoma symptoms, reduction of chemotherapy-induced nausea, or control of neuropathic pain, are not necessarily related to THC. Well-designed clinical studies aimed at determining which other cannabinoids and at which doses are most relevant for medical use have yet to be performed, Dr. Gourlay said.
For the clinician, legalization of medical marijuana in the absence of reliable data on best practice creates some potential risks. According to Dr. Gourlay, patients who harm themselves or others in an accident attributed to impaired judgment from medical marijuana might pursue legal action against the prescribing physician. The relative absence of standards regarding marijuana use would complicate the defense.
“Unless you can competently discuss the pros and cons of herbal cannabis, including indications and contraindications that are relevant to informed consent, you would be wise to consider carefully any decision to prescribe,” Dr. Gourlay suggested.
The problem for many clinicians, according to Dr. Gourlay, is that patients often are already using marijuana and employ a variety of strategies to induce the physician to provide a prescription to legitimize this activity. He outlined several familiar traps that he urged physicians to avoid. These include claims by patients that a prescription would protect them from legal problems for a drug they will be using in any event or that clinicians can provide a dosing regimen that can be the basis for a plan to eventually taper use.
“Once you start down this road, it will be very difficult to change course,” said Dr. Gourlay, noting that even a discussion of marijuana should be well documented so that there are no misinterpretations regarding instructions about use or avoiding use. In situations in which patients are insistent about their need for marijuana, “consider having a third party in the room,” he suggested.
In areas where cannabinoids are available in well-defined concentrations for oral delivery, a stronger case can be made for medicinal applications, but clinical studies still remain limited, Dr. Gourlay said. He said he hopes trials will eventually be conducted to gauge the benefit-to-risk ratio for specific indications.
“I am not anticannabinoids, but I have never prescribed cannabis to smoke,” Dr. Gourlay reported. Even though recent legislation now permits recreational use of marijuana in several states, Dr. Gourlay urged clinicians to employ a conservative approach to clinical use until more data clarify both the drug’s benefits and safety.
The Journal of Family Practice and this news organization are owned by the same company.
The meeting was held by the American Pain Society and Global Academy for Medical Education. Global Academy and this news organization are owned the same company.
This post has been updated 8/5/2015.
EXPERT ANALYSIS AT THE PAIN CARE FOR PRIMARY CARE MEETING