User login
In January 2004, the Mercy Inpatient Medicine Service embarked on a quality-based incentive program, or “pay-for-performance.” This was spurred on by Blue Cross of Massachusetts, which contracted with all hospitals in the state to receive a substantial financial bonus for agreed-upon quality indicators.
Prior to the start date, representatives from Mercy Medical Center negotiated with Blue Cross, arriving at the following quality indicators and targets for all hospital patients for the period of January to December 2004:
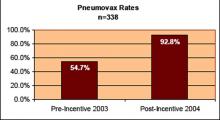
- For pneumonia patients, 45% rate of pneumococcal vaccine screening and administration;
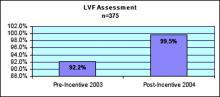
- For heart failure patients, 85% rate of documentation of ejection fraction; and
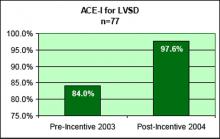
- For heart failure patients with ejection fraction <40%, prescription of an ACE-inhibitor (or documentation of a contraindication) upon discharge.
The Mercy Inpatient Medicine Service, which consisted of 10 full-time hospitalists in 2004, cared for approximately 75% of all medical inpatients at the hospital. We created a quality-based incentive program for this hospital medicine group that mirrored the incentives mentioned above for the entire hospital. We postulated that superior performance by the hospitalists would “raise the bar” for the remainder of the patients, some of whom were cared for by a separate hospital medicine group and some by traditional PCPs.
Mechanics of the Pay for Performance Program
The quality-based bonus was structured so that it would be paid out at 6-month intervals in equal parts to all full-time hospitalists. The magnitude of the bonus was set in excess of 7.5% of the hospitalists’ base salary, an amount that we felt would be large enough to influence behavior change.
From the outset of the bonus period (2004), as medical director of the group, I convened a weekly meeting with hospitalists and representatives from the Quality Improvement department, nursing, and case management. The meeting was being held amid the backdrop of a renewed institutional emphasis on all the JCAHO Core Measures and other quality/patient safety initiatives. The purpose of the meeting was to review hospital performance on all JCAHO Core Measures.
A nurse from the Quality Improvement department reviewed all charts of pneumonia and heart failure patients. For cases where pneumovax was not screened/administered, ejection fraction not assessed, and ACE-I not given, a hospitalist would review the chart and provide feedback to the physician-of-record regarding the nature of the problem. Further, I provided regular feedback to the hospital medicine group regarding their performance on the 3 indicators.
Results
The results in Figures 1–3 are for the hospitalist group, with results for the hospital as a whole slightly lower, but still in excess of the targets agreed upon with Blue Cross.
Summary
Mercy’s experience in 2004 is among the first hospitalist pay-for-performance programs reported. This quality-based incentive resulted in marked improvement in 3 quality indicators, resulting in the hospital’s attainment of the bonus paid by Blue Cross. The hospitalists were satisfied with the incentive program, because they felt appropriately rewarded for high-quality care. It is interesting to note that less-aggressive measures had been undertaken in the past to improve these indicators, but with little success. In 2004, with financial rewards at stake, more robust processes—such as a weekly meeting, ongoing chart review, and direct feedback to physicians—were put in place to ensure quality improvement.
Win Whitcomb, MD, cofounded the Society of Hospital Medicine with John Nelson, MD, in 1996. He is director of Performance Improvement at Mercy Medical Center, Springfield, MA, and can be reached at wfwhit@comcast.net.
In January 2004, the Mercy Inpatient Medicine Service embarked on a quality-based incentive program, or “pay-for-performance.” This was spurred on by Blue Cross of Massachusetts, which contracted with all hospitals in the state to receive a substantial financial bonus for agreed-upon quality indicators.
Prior to the start date, representatives from Mercy Medical Center negotiated with Blue Cross, arriving at the following quality indicators and targets for all hospital patients for the period of January to December 2004:
- For pneumonia patients, 45% rate of pneumococcal vaccine screening and administration;
- For heart failure patients, 85% rate of documentation of ejection fraction; and
- For heart failure patients with ejection fraction <40%, prescription of an ACE-inhibitor (or documentation of a contraindication) upon discharge.
The Mercy Inpatient Medicine Service, which consisted of 10 full-time hospitalists in 2004, cared for approximately 75% of all medical inpatients at the hospital. We created a quality-based incentive program for this hospital medicine group that mirrored the incentives mentioned above for the entire hospital. We postulated that superior performance by the hospitalists would “raise the bar” for the remainder of the patients, some of whom were cared for by a separate hospital medicine group and some by traditional PCPs.
Mechanics of the Pay for Performance Program
The quality-based bonus was structured so that it would be paid out at 6-month intervals in equal parts to all full-time hospitalists. The magnitude of the bonus was set in excess of 7.5% of the hospitalists’ base salary, an amount that we felt would be large enough to influence behavior change.
From the outset of the bonus period (2004), as medical director of the group, I convened a weekly meeting with hospitalists and representatives from the Quality Improvement department, nursing, and case management. The meeting was being held amid the backdrop of a renewed institutional emphasis on all the JCAHO Core Measures and other quality/patient safety initiatives. The purpose of the meeting was to review hospital performance on all JCAHO Core Measures.
A nurse from the Quality Improvement department reviewed all charts of pneumonia and heart failure patients. For cases where pneumovax was not screened/administered, ejection fraction not assessed, and ACE-I not given, a hospitalist would review the chart and provide feedback to the physician-of-record regarding the nature of the problem. Further, I provided regular feedback to the hospital medicine group regarding their performance on the 3 indicators.
Results
The results in Figures 1–3 are for the hospitalist group, with results for the hospital as a whole slightly lower, but still in excess of the targets agreed upon with Blue Cross.
Summary
Mercy’s experience in 2004 is among the first hospitalist pay-for-performance programs reported. This quality-based incentive resulted in marked improvement in 3 quality indicators, resulting in the hospital’s attainment of the bonus paid by Blue Cross. The hospitalists were satisfied with the incentive program, because they felt appropriately rewarded for high-quality care. It is interesting to note that less-aggressive measures had been undertaken in the past to improve these indicators, but with little success. In 2004, with financial rewards at stake, more robust processes—such as a weekly meeting, ongoing chart review, and direct feedback to physicians—were put in place to ensure quality improvement.
Win Whitcomb, MD, cofounded the Society of Hospital Medicine with John Nelson, MD, in 1996. He is director of Performance Improvement at Mercy Medical Center, Springfield, MA, and can be reached at wfwhit@comcast.net.
In January 2004, the Mercy Inpatient Medicine Service embarked on a quality-based incentive program, or “pay-for-performance.” This was spurred on by Blue Cross of Massachusetts, which contracted with all hospitals in the state to receive a substantial financial bonus for agreed-upon quality indicators.
Prior to the start date, representatives from Mercy Medical Center negotiated with Blue Cross, arriving at the following quality indicators and targets for all hospital patients for the period of January to December 2004:
- For pneumonia patients, 45% rate of pneumococcal vaccine screening and administration;
- For heart failure patients, 85% rate of documentation of ejection fraction; and
- For heart failure patients with ejection fraction <40%, prescription of an ACE-inhibitor (or documentation of a contraindication) upon discharge.
The Mercy Inpatient Medicine Service, which consisted of 10 full-time hospitalists in 2004, cared for approximately 75% of all medical inpatients at the hospital. We created a quality-based incentive program for this hospital medicine group that mirrored the incentives mentioned above for the entire hospital. We postulated that superior performance by the hospitalists would “raise the bar” for the remainder of the patients, some of whom were cared for by a separate hospital medicine group and some by traditional PCPs.
Mechanics of the Pay for Performance Program
The quality-based bonus was structured so that it would be paid out at 6-month intervals in equal parts to all full-time hospitalists. The magnitude of the bonus was set in excess of 7.5% of the hospitalists’ base salary, an amount that we felt would be large enough to influence behavior change.
From the outset of the bonus period (2004), as medical director of the group, I convened a weekly meeting with hospitalists and representatives from the Quality Improvement department, nursing, and case management. The meeting was being held amid the backdrop of a renewed institutional emphasis on all the JCAHO Core Measures and other quality/patient safety initiatives. The purpose of the meeting was to review hospital performance on all JCAHO Core Measures.
A nurse from the Quality Improvement department reviewed all charts of pneumonia and heart failure patients. For cases where pneumovax was not screened/administered, ejection fraction not assessed, and ACE-I not given, a hospitalist would review the chart and provide feedback to the physician-of-record regarding the nature of the problem. Further, I provided regular feedback to the hospital medicine group regarding their performance on the 3 indicators.
Results
The results in Figures 1–3 are for the hospitalist group, with results for the hospital as a whole slightly lower, but still in excess of the targets agreed upon with Blue Cross.
Summary
Mercy’s experience in 2004 is among the first hospitalist pay-for-performance programs reported. This quality-based incentive resulted in marked improvement in 3 quality indicators, resulting in the hospital’s attainment of the bonus paid by Blue Cross. The hospitalists were satisfied with the incentive program, because they felt appropriately rewarded for high-quality care. It is interesting to note that less-aggressive measures had been undertaken in the past to improve these indicators, but with little success. In 2004, with financial rewards at stake, more robust processes—such as a weekly meeting, ongoing chart review, and direct feedback to physicians—were put in place to ensure quality improvement.
Win Whitcomb, MD, cofounded the Society of Hospital Medicine with John Nelson, MD, in 1996. He is director of Performance Improvement at Mercy Medical Center, Springfield, MA, and can be reached at wfwhit@comcast.net.