User login
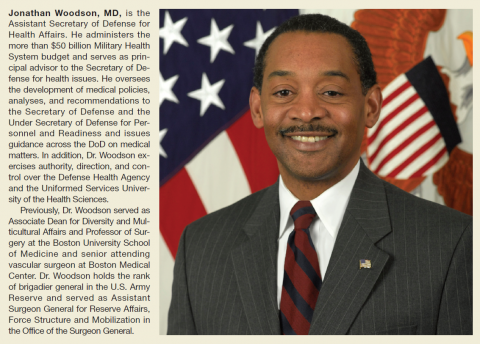
Assistant Secretary of Defense for Health Affairs Dr. Jonathan Woodson sits atop a massively complex health care system. With an annual budget of > $50 billion and 133,000 military and civilian health care providers, allied health professionals, and health administrators spread around the globe, the Military Health System (MHS) is exceedingly complex. Keeping the system running is challenging enough, but Woodson is focused on transforming it into a more nimble, efficient, proactive and cost-effective health care system.
Federal Practitioner recently talked with Dr. Woodson about the challenges of transforming the MHS. We also discussed the Defense Health Agency and how global health threats like Ebola fit in to the MHS mission. The following is condensed and edited, but the complete interview can be heard here: Jonathan Woodson on Military Health Readiness.
The Military Health System Mission
Assistant Secretary of Defense for Health Affairs Jonathan Woodson. The Department of Defense has a unique mission. So yes, we do deliver health care; but we deliver health care on a global basis. And in fact, we are the ones who are asked anytime there is a crisis to set up health care systems in austere places as a key enabler to those who would go in harm’s way and defend our nation.
That is a sober undertaking, and we undertake it with the full understanding that in today’s world, the American leadership and the American public expect us to not only deliver the standard of care, but really go above the standard of care and advance care anywhere in the world....If you look at the experience of the last 12 plus years of war, and you look at what has been accomplished in terms of combat casualty care, we have advanced that strategy for care.
At the beginning of the war, it was clear that we were operating from a traditional platform but a number of experts recognized that what we needed to develop was a system that could drive change based upon data. The Joint Trauma System was born, which analyzed the outcomes of just about every case that was treated. But more importantly, [it] mined the data and rapidly changed the strategies for care as we found optimal ways of delivering care.
This included everything from our strategy for evacuation and the development of critical care air medical transplant units that provided prompt evacuation from the battlefield and echelons of care so those service members would receive very sophisticated advanced care, to strategies for employing new drugs, new techniques, new training strategies for medics and bringing critical care skills closer to the point of injury. Across a wide swath of strategies for delivering care, the system has been constantly improved.
And now we see from the data that despite the fact that we’re taking care of more severely injured individuals, the fatality rates have dropped. An individual who makes it to a role 3 facility—whatever the injury severity—has a 98% chance of surviving.
This has culminated most recently in terms of this transfer of knowledge with us signing a partnership agreement with the American College of Surgeons, which will allow us to further interact with the civilian communities in terms of trying to define optimal ways for caring for injured patients. This will be good not only for us, but it will be good for the civilian communities as well.
Research and Sharing Advances
Dr. Woodson. We have outlined 6 strategic lines of effort to help modernize the military health system, and they include modernizing our management with an enterprise focus, defining our 21st century capabilities that are necessary to make us better, stronger, and more relevant for the future. [We are also] looking at the medical force structure, particularly since today we have to ensure that we understand and employ subspecialists in the right way.
In addition, we are looking at defining and investing in strategic partners. Our strategic partners are like the American College of Surgeons but represent a wide range of potential academic and research institutions that can collaborate with us to ensure that we achieve results in our research portfolio, particularly against the priorities that are very important to military medicine.
The other areas that we need to concentrate on is reforming TRICARE and defining our requirements and competencies in global health engagement. The issue is investing in and defining our strategic partners, which is what I think is going to make us extraordinarily strong, because realistically we need to approach this as the whole-of-society investment in our national defense. Our strategic partners, of course, include our other federal partners, such as the Veterans Administration.
Continuity of Care
Dr. Woodson. We are committed to serving the needs of servicemen and women who might be injured or become ill as a result of their service for decades to come. That is, we understand that they may, in fact, require care for decades. And as a result, we, of course, have several ways of ensuring that they do receive that care. We have a defined sort of insurance benefit called TRICARE; a vehicle that allows separating servicemen and women who qualify to receive care in the civilian sector.
But beyond that, we have strengthened our partnership and our collaboration with the Veterans Administration to break down barriers so that we can transition servicemen and women more effectively and easily. [For] things like transferring critical medical information, we’ve developed an integrative mental health strategy so that we have common evidence-based strategies for mental health care.
We’ve recently concluded an agreement to reform the way the 2 departments reimburse each other so that the whole issue of billing doesn’t become an encumbrance to delivery of care. We’ve agreed to a common credentialing system so that our providers can more easily serve in either system, which leads to more effective, efficient care and use of our human resources.
Across many lines—the ones I’ve mentioned, and many others—we are ensuring that we can care for the servicemen and women who might become ill or injured and require care going on into the decades to ensure that they have high-quality lives and they’re kept healthy.
The Global Response to Ebola
Dr. Woodson. We have subject matter experts that have worked in infectious diseases for some time. You know, the United States Army Institute of Infectious Diseases is a well-recognized, longstanding organization that has helped produce vaccines and strategies to care for infectious diseases and has contributed very substantially to the biosecurity not only of this nation, but of the world.
We’ve got really the indomitable spirit of the average serviceman and woman who, when given a complex job, know how to meet the mission. And so we have superb leaders, and we have become a key enabler.
When the U.S. shows up, then other countries rally. It provides a platform in which other countries can now commit to the effort. And that’s probably as important as anything else, because this needs to be a worldwide effort to stem this epidemic that is occurring in West Africa.
The Defense Health Agency
The Defense Health Agency has as its mission to put in effect common clinical and business processes to achieve those economies of scale and allow us to use our dollars and other resources more wisely. The Defense Health Agency was charged with initially standing up 10 shared services to include facilities planning, medical logistics, health information technology, managing the TRICARE health plan, pharmacy programs, the Public Health System, acquisitions, budget and resources, management systems, medical education and training, and medical research and development.
As such, we’ve achieved great results over the first year, saving about $248 million. But more importantly, we set the foundation for 21st century systems that will allow us to manage the Military Health System much more effectively, such as establishing a foundation for a common cost accounting system and the development of an enterprise performance management system.
The Military Health System added what we call the Quadruple Aim, which is providing better outcomes, better patient care experience, managing costs, and meeting our readiness mission. We have also established a solid strategic plan and framework in which to ensure that we will meet that end. We’ve had tremendous progress over the first year.
I just want to remind you and everyone of what a heavy lift this was. This is a major reorganization where thousands of people have been reassigned and reorganized to produce a more effective management system. This was no easy lift, but it has been tremendously successful to date.
You don’t necessarily flip the switch and everything is mature and working optimally overnight. The intent was to ensure that it was fully operational and capable by 1 October 2015. What we have seen to date is that it’s ahead of schedule, and that’s good news.
It represents major transformational change. Many people have to be moved. We had to build a new leadership team that, in fact, was heavily invested and contributed to by the uniformed services, the Army, Navy, and Air Force. So they’re deeply invested in the leadership and the governance of the Defense Health Agency.
The Military’s Health Care Challenges
Dr. Woodson. Our central guiding principle is the Quadruple Aim. And at the center, as I mentioned before, is this issue of readiness; and readiness is about ensuring that we have a healthy force to do the nation’s bidding in terms of defense. Not only do we have a healthy force, but we keep them healthy. So we commit to looking at environmental concerns wherever they are deployed. Of course, we provide force protection measures such as vaccines and medicines to prevent infectious diseases, such as malaria if they’re working in a part of the world where that’s endemic.
This is all part of the responsibilities of the military health system. But also, the second part of the readiness responsibility is ensuring that we have a ready medical force. A group of superbly trained providers from the embedded combat medic up to the super subspecialist neurosurgeon, nurses of all specialties and varieties, and other allied health professionals that can create a robust Military Health System and provide above the standard of care anywhere in the world where our sailors, marines, airmen, and soldiers may be operating.
We also have to deal with the issue of chronic problems, health problems that afflict our society. We have started initiatives to address obesity and fitness across a broad spectrum. As a strategy for the military health system, we’re moving from the system of health care, which is just providing treatment after an established disease has occurred, to one of health, which is looking at the whole paradigm of wellness and preventing disease from occurring. It is about reaching into that white space where people learn, work, and play to ensure that they can make healthy choices....We’re deeply invested in the health of the beneficiaries that we serve across a broad spectrum, and we’re deeply invested in the issue of prevention, not only the treatment of disease.
The issue that I would want everyone to understand is that health care and health care delivery in the 21st century is very complex. It’s about not only the actual technology, advances in medical science, but it’s also about addressing where medical science hits human systems and how do you make the system work so that you achieve the best outcomes? And in that mix are the issues of cost and ensuring that you have the ability to deliver that care wherever it’s needed. We’ve mapped out with the leadership of the Military Health System, the surgeons general, and all of their leaders a pathway forward that, in fact, will ensure that the Military Health System will be strong, better, and relevant going into the 21st century and will continue to be a key enabler for the national security, national defense, and the national military strategies.
As a designated Combat Support Agency, the Defense Health Agency is also responsible for meeting the medical needs of the combatant commanders. Central to this role is to ensure our service members are medically ready to perform their mission, and our military medical personnel are ready to perform their mission—“Medically Ready Force…Ready Medical Force.”
Assistant Secretary of Defense for Health Affairs Dr. Jonathan Woodson sits atop a massively complex health care system. With an annual budget of > $50 billion and 133,000 military and civilian health care providers, allied health professionals, and health administrators spread around the globe, the Military Health System (MHS) is exceedingly complex. Keeping the system running is challenging enough, but Woodson is focused on transforming it into a more nimble, efficient, proactive and cost-effective health care system.
Federal Practitioner recently talked with Dr. Woodson about the challenges of transforming the MHS. We also discussed the Defense Health Agency and how global health threats like Ebola fit in to the MHS mission. The following is condensed and edited, but the complete interview can be heard here: Jonathan Woodson on Military Health Readiness.
The Military Health System Mission
Assistant Secretary of Defense for Health Affairs Jonathan Woodson. The Department of Defense has a unique mission. So yes, we do deliver health care; but we deliver health care on a global basis. And in fact, we are the ones who are asked anytime there is a crisis to set up health care systems in austere places as a key enabler to those who would go in harm’s way and defend our nation.
That is a sober undertaking, and we undertake it with the full understanding that in today’s world, the American leadership and the American public expect us to not only deliver the standard of care, but really go above the standard of care and advance care anywhere in the world....If you look at the experience of the last 12 plus years of war, and you look at what has been accomplished in terms of combat casualty care, we have advanced that strategy for care.
At the beginning of the war, it was clear that we were operating from a traditional platform but a number of experts recognized that what we needed to develop was a system that could drive change based upon data. The Joint Trauma System was born, which analyzed the outcomes of just about every case that was treated. But more importantly, [it] mined the data and rapidly changed the strategies for care as we found optimal ways of delivering care.
This included everything from our strategy for evacuation and the development of critical care air medical transplant units that provided prompt evacuation from the battlefield and echelons of care so those service members would receive very sophisticated advanced care, to strategies for employing new drugs, new techniques, new training strategies for medics and bringing critical care skills closer to the point of injury. Across a wide swath of strategies for delivering care, the system has been constantly improved.
And now we see from the data that despite the fact that we’re taking care of more severely injured individuals, the fatality rates have dropped. An individual who makes it to a role 3 facility—whatever the injury severity—has a 98% chance of surviving.
This has culminated most recently in terms of this transfer of knowledge with us signing a partnership agreement with the American College of Surgeons, which will allow us to further interact with the civilian communities in terms of trying to define optimal ways for caring for injured patients. This will be good not only for us, but it will be good for the civilian communities as well.
Research and Sharing Advances
Dr. Woodson. We have outlined 6 strategic lines of effort to help modernize the military health system, and they include modernizing our management with an enterprise focus, defining our 21st century capabilities that are necessary to make us better, stronger, and more relevant for the future. [We are also] looking at the medical force structure, particularly since today we have to ensure that we understand and employ subspecialists in the right way.
In addition, we are looking at defining and investing in strategic partners. Our strategic partners are like the American College of Surgeons but represent a wide range of potential academic and research institutions that can collaborate with us to ensure that we achieve results in our research portfolio, particularly against the priorities that are very important to military medicine.
The other areas that we need to concentrate on is reforming TRICARE and defining our requirements and competencies in global health engagement. The issue is investing in and defining our strategic partners, which is what I think is going to make us extraordinarily strong, because realistically we need to approach this as the whole-of-society investment in our national defense. Our strategic partners, of course, include our other federal partners, such as the Veterans Administration.
Continuity of Care
Dr. Woodson. We are committed to serving the needs of servicemen and women who might be injured or become ill as a result of their service for decades to come. That is, we understand that they may, in fact, require care for decades. And as a result, we, of course, have several ways of ensuring that they do receive that care. We have a defined sort of insurance benefit called TRICARE; a vehicle that allows separating servicemen and women who qualify to receive care in the civilian sector.
But beyond that, we have strengthened our partnership and our collaboration with the Veterans Administration to break down barriers so that we can transition servicemen and women more effectively and easily. [For] things like transferring critical medical information, we’ve developed an integrative mental health strategy so that we have common evidence-based strategies for mental health care.
We’ve recently concluded an agreement to reform the way the 2 departments reimburse each other so that the whole issue of billing doesn’t become an encumbrance to delivery of care. We’ve agreed to a common credentialing system so that our providers can more easily serve in either system, which leads to more effective, efficient care and use of our human resources.
Across many lines—the ones I’ve mentioned, and many others—we are ensuring that we can care for the servicemen and women who might become ill or injured and require care going on into the decades to ensure that they have high-quality lives and they’re kept healthy.
The Global Response to Ebola
Dr. Woodson. We have subject matter experts that have worked in infectious diseases for some time. You know, the United States Army Institute of Infectious Diseases is a well-recognized, longstanding organization that has helped produce vaccines and strategies to care for infectious diseases and has contributed very substantially to the biosecurity not only of this nation, but of the world.
We’ve got really the indomitable spirit of the average serviceman and woman who, when given a complex job, know how to meet the mission. And so we have superb leaders, and we have become a key enabler.
When the U.S. shows up, then other countries rally. It provides a platform in which other countries can now commit to the effort. And that’s probably as important as anything else, because this needs to be a worldwide effort to stem this epidemic that is occurring in West Africa.
The Defense Health Agency
The Defense Health Agency has as its mission to put in effect common clinical and business processes to achieve those economies of scale and allow us to use our dollars and other resources more wisely. The Defense Health Agency was charged with initially standing up 10 shared services to include facilities planning, medical logistics, health information technology, managing the TRICARE health plan, pharmacy programs, the Public Health System, acquisitions, budget and resources, management systems, medical education and training, and medical research and development.
As such, we’ve achieved great results over the first year, saving about $248 million. But more importantly, we set the foundation for 21st century systems that will allow us to manage the Military Health System much more effectively, such as establishing a foundation for a common cost accounting system and the development of an enterprise performance management system.
The Military Health System added what we call the Quadruple Aim, which is providing better outcomes, better patient care experience, managing costs, and meeting our readiness mission. We have also established a solid strategic plan and framework in which to ensure that we will meet that end. We’ve had tremendous progress over the first year.
I just want to remind you and everyone of what a heavy lift this was. This is a major reorganization where thousands of people have been reassigned and reorganized to produce a more effective management system. This was no easy lift, but it has been tremendously successful to date.
You don’t necessarily flip the switch and everything is mature and working optimally overnight. The intent was to ensure that it was fully operational and capable by 1 October 2015. What we have seen to date is that it’s ahead of schedule, and that’s good news.
It represents major transformational change. Many people have to be moved. We had to build a new leadership team that, in fact, was heavily invested and contributed to by the uniformed services, the Army, Navy, and Air Force. So they’re deeply invested in the leadership and the governance of the Defense Health Agency.
The Military’s Health Care Challenges
Dr. Woodson. Our central guiding principle is the Quadruple Aim. And at the center, as I mentioned before, is this issue of readiness; and readiness is about ensuring that we have a healthy force to do the nation’s bidding in terms of defense. Not only do we have a healthy force, but we keep them healthy. So we commit to looking at environmental concerns wherever they are deployed. Of course, we provide force protection measures such as vaccines and medicines to prevent infectious diseases, such as malaria if they’re working in a part of the world where that’s endemic.
This is all part of the responsibilities of the military health system. But also, the second part of the readiness responsibility is ensuring that we have a ready medical force. A group of superbly trained providers from the embedded combat medic up to the super subspecialist neurosurgeon, nurses of all specialties and varieties, and other allied health professionals that can create a robust Military Health System and provide above the standard of care anywhere in the world where our sailors, marines, airmen, and soldiers may be operating.
We also have to deal with the issue of chronic problems, health problems that afflict our society. We have started initiatives to address obesity and fitness across a broad spectrum. As a strategy for the military health system, we’re moving from the system of health care, which is just providing treatment after an established disease has occurred, to one of health, which is looking at the whole paradigm of wellness and preventing disease from occurring. It is about reaching into that white space where people learn, work, and play to ensure that they can make healthy choices....We’re deeply invested in the health of the beneficiaries that we serve across a broad spectrum, and we’re deeply invested in the issue of prevention, not only the treatment of disease.
The issue that I would want everyone to understand is that health care and health care delivery in the 21st century is very complex. It’s about not only the actual technology, advances in medical science, but it’s also about addressing where medical science hits human systems and how do you make the system work so that you achieve the best outcomes? And in that mix are the issues of cost and ensuring that you have the ability to deliver that care wherever it’s needed. We’ve mapped out with the leadership of the Military Health System, the surgeons general, and all of their leaders a pathway forward that, in fact, will ensure that the Military Health System will be strong, better, and relevant going into the 21st century and will continue to be a key enabler for the national security, national defense, and the national military strategies.
As a designated Combat Support Agency, the Defense Health Agency is also responsible for meeting the medical needs of the combatant commanders. Central to this role is to ensure our service members are medically ready to perform their mission, and our military medical personnel are ready to perform their mission—“Medically Ready Force…Ready Medical Force.”
Assistant Secretary of Defense for Health Affairs Dr. Jonathan Woodson sits atop a massively complex health care system. With an annual budget of > $50 billion and 133,000 military and civilian health care providers, allied health professionals, and health administrators spread around the globe, the Military Health System (MHS) is exceedingly complex. Keeping the system running is challenging enough, but Woodson is focused on transforming it into a more nimble, efficient, proactive and cost-effective health care system.
Federal Practitioner recently talked with Dr. Woodson about the challenges of transforming the MHS. We also discussed the Defense Health Agency and how global health threats like Ebola fit in to the MHS mission. The following is condensed and edited, but the complete interview can be heard here: Jonathan Woodson on Military Health Readiness.
The Military Health System Mission
Assistant Secretary of Defense for Health Affairs Jonathan Woodson. The Department of Defense has a unique mission. So yes, we do deliver health care; but we deliver health care on a global basis. And in fact, we are the ones who are asked anytime there is a crisis to set up health care systems in austere places as a key enabler to those who would go in harm’s way and defend our nation.
That is a sober undertaking, and we undertake it with the full understanding that in today’s world, the American leadership and the American public expect us to not only deliver the standard of care, but really go above the standard of care and advance care anywhere in the world....If you look at the experience of the last 12 plus years of war, and you look at what has been accomplished in terms of combat casualty care, we have advanced that strategy for care.
At the beginning of the war, it was clear that we were operating from a traditional platform but a number of experts recognized that what we needed to develop was a system that could drive change based upon data. The Joint Trauma System was born, which analyzed the outcomes of just about every case that was treated. But more importantly, [it] mined the data and rapidly changed the strategies for care as we found optimal ways of delivering care.
This included everything from our strategy for evacuation and the development of critical care air medical transplant units that provided prompt evacuation from the battlefield and echelons of care so those service members would receive very sophisticated advanced care, to strategies for employing new drugs, new techniques, new training strategies for medics and bringing critical care skills closer to the point of injury. Across a wide swath of strategies for delivering care, the system has been constantly improved.
And now we see from the data that despite the fact that we’re taking care of more severely injured individuals, the fatality rates have dropped. An individual who makes it to a role 3 facility—whatever the injury severity—has a 98% chance of surviving.
This has culminated most recently in terms of this transfer of knowledge with us signing a partnership agreement with the American College of Surgeons, which will allow us to further interact with the civilian communities in terms of trying to define optimal ways for caring for injured patients. This will be good not only for us, but it will be good for the civilian communities as well.
Research and Sharing Advances
Dr. Woodson. We have outlined 6 strategic lines of effort to help modernize the military health system, and they include modernizing our management with an enterprise focus, defining our 21st century capabilities that are necessary to make us better, stronger, and more relevant for the future. [We are also] looking at the medical force structure, particularly since today we have to ensure that we understand and employ subspecialists in the right way.
In addition, we are looking at defining and investing in strategic partners. Our strategic partners are like the American College of Surgeons but represent a wide range of potential academic and research institutions that can collaborate with us to ensure that we achieve results in our research portfolio, particularly against the priorities that are very important to military medicine.
The other areas that we need to concentrate on is reforming TRICARE and defining our requirements and competencies in global health engagement. The issue is investing in and defining our strategic partners, which is what I think is going to make us extraordinarily strong, because realistically we need to approach this as the whole-of-society investment in our national defense. Our strategic partners, of course, include our other federal partners, such as the Veterans Administration.
Continuity of Care
Dr. Woodson. We are committed to serving the needs of servicemen and women who might be injured or become ill as a result of their service for decades to come. That is, we understand that they may, in fact, require care for decades. And as a result, we, of course, have several ways of ensuring that they do receive that care. We have a defined sort of insurance benefit called TRICARE; a vehicle that allows separating servicemen and women who qualify to receive care in the civilian sector.
But beyond that, we have strengthened our partnership and our collaboration with the Veterans Administration to break down barriers so that we can transition servicemen and women more effectively and easily. [For] things like transferring critical medical information, we’ve developed an integrative mental health strategy so that we have common evidence-based strategies for mental health care.
We’ve recently concluded an agreement to reform the way the 2 departments reimburse each other so that the whole issue of billing doesn’t become an encumbrance to delivery of care. We’ve agreed to a common credentialing system so that our providers can more easily serve in either system, which leads to more effective, efficient care and use of our human resources.
Across many lines—the ones I’ve mentioned, and many others—we are ensuring that we can care for the servicemen and women who might become ill or injured and require care going on into the decades to ensure that they have high-quality lives and they’re kept healthy.
The Global Response to Ebola
Dr. Woodson. We have subject matter experts that have worked in infectious diseases for some time. You know, the United States Army Institute of Infectious Diseases is a well-recognized, longstanding organization that has helped produce vaccines and strategies to care for infectious diseases and has contributed very substantially to the biosecurity not only of this nation, but of the world.
We’ve got really the indomitable spirit of the average serviceman and woman who, when given a complex job, know how to meet the mission. And so we have superb leaders, and we have become a key enabler.
When the U.S. shows up, then other countries rally. It provides a platform in which other countries can now commit to the effort. And that’s probably as important as anything else, because this needs to be a worldwide effort to stem this epidemic that is occurring in West Africa.
The Defense Health Agency
The Defense Health Agency has as its mission to put in effect common clinical and business processes to achieve those economies of scale and allow us to use our dollars and other resources more wisely. The Defense Health Agency was charged with initially standing up 10 shared services to include facilities planning, medical logistics, health information technology, managing the TRICARE health plan, pharmacy programs, the Public Health System, acquisitions, budget and resources, management systems, medical education and training, and medical research and development.
As such, we’ve achieved great results over the first year, saving about $248 million. But more importantly, we set the foundation for 21st century systems that will allow us to manage the Military Health System much more effectively, such as establishing a foundation for a common cost accounting system and the development of an enterprise performance management system.
The Military Health System added what we call the Quadruple Aim, which is providing better outcomes, better patient care experience, managing costs, and meeting our readiness mission. We have also established a solid strategic plan and framework in which to ensure that we will meet that end. We’ve had tremendous progress over the first year.
I just want to remind you and everyone of what a heavy lift this was. This is a major reorganization where thousands of people have been reassigned and reorganized to produce a more effective management system. This was no easy lift, but it has been tremendously successful to date.
You don’t necessarily flip the switch and everything is mature and working optimally overnight. The intent was to ensure that it was fully operational and capable by 1 October 2015. What we have seen to date is that it’s ahead of schedule, and that’s good news.
It represents major transformational change. Many people have to be moved. We had to build a new leadership team that, in fact, was heavily invested and contributed to by the uniformed services, the Army, Navy, and Air Force. So they’re deeply invested in the leadership and the governance of the Defense Health Agency.
The Military’s Health Care Challenges
Dr. Woodson. Our central guiding principle is the Quadruple Aim. And at the center, as I mentioned before, is this issue of readiness; and readiness is about ensuring that we have a healthy force to do the nation’s bidding in terms of defense. Not only do we have a healthy force, but we keep them healthy. So we commit to looking at environmental concerns wherever they are deployed. Of course, we provide force protection measures such as vaccines and medicines to prevent infectious diseases, such as malaria if they’re working in a part of the world where that’s endemic.
This is all part of the responsibilities of the military health system. But also, the second part of the readiness responsibility is ensuring that we have a ready medical force. A group of superbly trained providers from the embedded combat medic up to the super subspecialist neurosurgeon, nurses of all specialties and varieties, and other allied health professionals that can create a robust Military Health System and provide above the standard of care anywhere in the world where our sailors, marines, airmen, and soldiers may be operating.
We also have to deal with the issue of chronic problems, health problems that afflict our society. We have started initiatives to address obesity and fitness across a broad spectrum. As a strategy for the military health system, we’re moving from the system of health care, which is just providing treatment after an established disease has occurred, to one of health, which is looking at the whole paradigm of wellness and preventing disease from occurring. It is about reaching into that white space where people learn, work, and play to ensure that they can make healthy choices....We’re deeply invested in the health of the beneficiaries that we serve across a broad spectrum, and we’re deeply invested in the issue of prevention, not only the treatment of disease.
The issue that I would want everyone to understand is that health care and health care delivery in the 21st century is very complex. It’s about not only the actual technology, advances in medical science, but it’s also about addressing where medical science hits human systems and how do you make the system work so that you achieve the best outcomes? And in that mix are the issues of cost and ensuring that you have the ability to deliver that care wherever it’s needed. We’ve mapped out with the leadership of the Military Health System, the surgeons general, and all of their leaders a pathway forward that, in fact, will ensure that the Military Health System will be strong, better, and relevant going into the 21st century and will continue to be a key enabler for the national security, national defense, and the national military strategies.
As a designated Combat Support Agency, the Defense Health Agency is also responsible for meeting the medical needs of the combatant commanders. Central to this role is to ensure our service members are medically ready to perform their mission, and our military medical personnel are ready to perform their mission—“Medically Ready Force…Ready Medical Force.”