User login
Hospitalists often encounter patients who are or could become critically ill. The increased efforts while caring for these patients are best captured through critical-care service codes 99291 and 99292.
Although these codes yield higher reimbursement ($204.15 and $102.45, respectively, per national Medicare average payment), they are reported only under certain circumstances. The physician’s documentation must include enough detail to support critical-care claims: the patient’s condition, the nature of the physician’s care, and the time spent rendering care. Documentation of any other pertinent information is strongly encouraged because these services often come under payer scrutiny.
Condition and Care
A patient’s condition must meet the established criteria before the service qualifies as critical care. More specifically, the patient must have a critical illness or injury that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition.
The physician’s personal attention (i.e., care involving one critically ill patient at a time) is essential for rendering the highly complex decisions necessary to prevent the patient’s decline if left untreated. Given the seriousness of the patient’s condition, the physician is expected to focus only on the patient for whom critical-care time is reported.
Duration
Critical care is a time-based service. It constitutes the physician’s time spent providing direct care at the bedside and gathering and reviewing data on the patient’s unit or floor.
If the physician is not immediately available to the patient, the time associated with indirect care (e.g., reviewing data, calling the family from the office) is not counted in the overall critical-care service.
The physician keeps tracks of his/her total critical-care time throughout the day. A new period of critical-care time begins each calendar day. There is no prohibition against reporting multiple hours or days of critical care, as long as the patient’s condition prompts the service and documentation supports it.
Code 99291 represents the first “hour” of critical care, which physicians may report after accumulating the first 30 minutes of care. Alternately, physician management of the patient involving less than 30 minutes of critical-care time on a given day must be reported with the appropriate evaluation and management (E/M) code:
- Initial inpatient service (99221-99223);
- Subsequent hospital care (99231-99233); or
- Inpatient consultation (99251-99255).
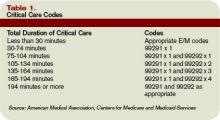
Once the physician achieves 75 minutes of critical-care time, he/she reports 99292 for the additional “30 minutes” of care beyond the first hour. Never report 99292 alone on the claim form. Code 99292 is considered an “add-on” code, which means it must be reported in addition to a primary code. Code 99291 is always the primary code (reported once per physician/group per day) for critical-care services. Code 99292 can be reported in multiple units per physician/group per day according to the number of minutes spent after the initial hour (see Table 1, p. 30).
Service Inclusions
Critical care involves highly complex decision making to manage the patient’s condition. This includes the physician’s performance and/or interpretation of labs, diagnostic studies, and procedures inherent in critical care.
Therefore, do not report the following services when billing 99291-99292:
- Cardiac output measurements (93561, 93562);
- Chest X-rays (71010, 71015, 71020);
- Pulse oximetry (94760, 94761, 94762); and
- Blood gases (multiple codes).
Further, don’t report interpretation of data stored in computers:
- Electrocardiograms, blood pressures, hematologic data (99090);
- Gastric intubation (43752, 91105);
- Temporary transcutaneous pacing (92953);
- Ventilation management (94002-94004, 94660, 94662); and
- Vascular access procedures (36000, 36410, 36415, 36591, 36600).
Any other service or procedure provided by the physician can be billed in addition to 99291-99292.
Be sure not to add separately billable procedure time into the physician’s total critical-care time. A notation in the medical record should reflect this (e.g., time spent inserting a central line is not included in today’s critical-care time).
Location
Because a patient can become seriously ill in any setting, physicians often provide critical-care services in emergency departments (EDs) and on standard medical-surgical floors before the patient is transferred to the intensive care unit (ICU).
Bed location alone does not determine critical-care reporting. Patients assigned to an ICU might be critically ill or injured and meet the “condition” requirements for 99291-99292.
However, the care provided may not meet the remaining requirements. According to the American Medical Association’s Current Procedural Terminology 2008 (Professional Edition) and the Medicare Claims Processing Manual, payment can be made for critical-care services provided in any location as long as the care provided meets the definition of critical care. Services for a patient who is not critically ill and unstable but who happens to be receiving care in a critical-care, intensive-care, or other specialized-care unit are reported using subsequent hospital care codes 99231-99233 or hospital consultation codes 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Hospitalists often encounter patients who are or could become critically ill. The increased efforts while caring for these patients are best captured through critical-care service codes 99291 and 99292.
Although these codes yield higher reimbursement ($204.15 and $102.45, respectively, per national Medicare average payment), they are reported only under certain circumstances. The physician’s documentation must include enough detail to support critical-care claims: the patient’s condition, the nature of the physician’s care, and the time spent rendering care. Documentation of any other pertinent information is strongly encouraged because these services often come under payer scrutiny.
Condition and Care
A patient’s condition must meet the established criteria before the service qualifies as critical care. More specifically, the patient must have a critical illness or injury that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition.
The physician’s personal attention (i.e., care involving one critically ill patient at a time) is essential for rendering the highly complex decisions necessary to prevent the patient’s decline if left untreated. Given the seriousness of the patient’s condition, the physician is expected to focus only on the patient for whom critical-care time is reported.
Duration
Critical care is a time-based service. It constitutes the physician’s time spent providing direct care at the bedside and gathering and reviewing data on the patient’s unit or floor.
If the physician is not immediately available to the patient, the time associated with indirect care (e.g., reviewing data, calling the family from the office) is not counted in the overall critical-care service.
The physician keeps tracks of his/her total critical-care time throughout the day. A new period of critical-care time begins each calendar day. There is no prohibition against reporting multiple hours or days of critical care, as long as the patient’s condition prompts the service and documentation supports it.
Code 99291 represents the first “hour” of critical care, which physicians may report after accumulating the first 30 minutes of care. Alternately, physician management of the patient involving less than 30 minutes of critical-care time on a given day must be reported with the appropriate evaluation and management (E/M) code:
- Initial inpatient service (99221-99223);
- Subsequent hospital care (99231-99233); or
- Inpatient consultation (99251-99255).
Once the physician achieves 75 minutes of critical-care time, he/she reports 99292 for the additional “30 minutes” of care beyond the first hour. Never report 99292 alone on the claim form. Code 99292 is considered an “add-on” code, which means it must be reported in addition to a primary code. Code 99291 is always the primary code (reported once per physician/group per day) for critical-care services. Code 99292 can be reported in multiple units per physician/group per day according to the number of minutes spent after the initial hour (see Table 1, p. 30).
Service Inclusions
Critical care involves highly complex decision making to manage the patient’s condition. This includes the physician’s performance and/or interpretation of labs, diagnostic studies, and procedures inherent in critical care.
Therefore, do not report the following services when billing 99291-99292:
- Cardiac output measurements (93561, 93562);
- Chest X-rays (71010, 71015, 71020);
- Pulse oximetry (94760, 94761, 94762); and
- Blood gases (multiple codes).
Further, don’t report interpretation of data stored in computers:
- Electrocardiograms, blood pressures, hematologic data (99090);
- Gastric intubation (43752, 91105);
- Temporary transcutaneous pacing (92953);
- Ventilation management (94002-94004, 94660, 94662); and
- Vascular access procedures (36000, 36410, 36415, 36591, 36600).
Any other service or procedure provided by the physician can be billed in addition to 99291-99292.
Be sure not to add separately billable procedure time into the physician’s total critical-care time. A notation in the medical record should reflect this (e.g., time spent inserting a central line is not included in today’s critical-care time).
Location
Because a patient can become seriously ill in any setting, physicians often provide critical-care services in emergency departments (EDs) and on standard medical-surgical floors before the patient is transferred to the intensive care unit (ICU).
Bed location alone does not determine critical-care reporting. Patients assigned to an ICU might be critically ill or injured and meet the “condition” requirements for 99291-99292.
However, the care provided may not meet the remaining requirements. According to the American Medical Association’s Current Procedural Terminology 2008 (Professional Edition) and the Medicare Claims Processing Manual, payment can be made for critical-care services provided in any location as long as the care provided meets the definition of critical care. Services for a patient who is not critically ill and unstable but who happens to be receiving care in a critical-care, intensive-care, or other specialized-care unit are reported using subsequent hospital care codes 99231-99233 or hospital consultation codes 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Hospitalists often encounter patients who are or could become critically ill. The increased efforts while caring for these patients are best captured through critical-care service codes 99291 and 99292.
Although these codes yield higher reimbursement ($204.15 and $102.45, respectively, per national Medicare average payment), they are reported only under certain circumstances. The physician’s documentation must include enough detail to support critical-care claims: the patient’s condition, the nature of the physician’s care, and the time spent rendering care. Documentation of any other pertinent information is strongly encouraged because these services often come under payer scrutiny.
Condition and Care
A patient’s condition must meet the established criteria before the service qualifies as critical care. More specifically, the patient must have a critical illness or injury that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition.
The physician’s personal attention (i.e., care involving one critically ill patient at a time) is essential for rendering the highly complex decisions necessary to prevent the patient’s decline if left untreated. Given the seriousness of the patient’s condition, the physician is expected to focus only on the patient for whom critical-care time is reported.
Duration
Critical care is a time-based service. It constitutes the physician’s time spent providing direct care at the bedside and gathering and reviewing data on the patient’s unit or floor.
If the physician is not immediately available to the patient, the time associated with indirect care (e.g., reviewing data, calling the family from the office) is not counted in the overall critical-care service.
The physician keeps tracks of his/her total critical-care time throughout the day. A new period of critical-care time begins each calendar day. There is no prohibition against reporting multiple hours or days of critical care, as long as the patient’s condition prompts the service and documentation supports it.
Code 99291 represents the first “hour” of critical care, which physicians may report after accumulating the first 30 minutes of care. Alternately, physician management of the patient involving less than 30 minutes of critical-care time on a given day must be reported with the appropriate evaluation and management (E/M) code:
- Initial inpatient service (99221-99223);
- Subsequent hospital care (99231-99233); or
- Inpatient consultation (99251-99255).
Once the physician achieves 75 minutes of critical-care time, he/she reports 99292 for the additional “30 minutes” of care beyond the first hour. Never report 99292 alone on the claim form. Code 99292 is considered an “add-on” code, which means it must be reported in addition to a primary code. Code 99291 is always the primary code (reported once per physician/group per day) for critical-care services. Code 99292 can be reported in multiple units per physician/group per day according to the number of minutes spent after the initial hour (see Table 1, p. 30).
Service Inclusions
Critical care involves highly complex decision making to manage the patient’s condition. This includes the physician’s performance and/or interpretation of labs, diagnostic studies, and procedures inherent in critical care.
Therefore, do not report the following services when billing 99291-99292:
- Cardiac output measurements (93561, 93562);
- Chest X-rays (71010, 71015, 71020);
- Pulse oximetry (94760, 94761, 94762); and
- Blood gases (multiple codes).
Further, don’t report interpretation of data stored in computers:
- Electrocardiograms, blood pressures, hematologic data (99090);
- Gastric intubation (43752, 91105);
- Temporary transcutaneous pacing (92953);
- Ventilation management (94002-94004, 94660, 94662); and
- Vascular access procedures (36000, 36410, 36415, 36591, 36600).
Any other service or procedure provided by the physician can be billed in addition to 99291-99292.
Be sure not to add separately billable procedure time into the physician’s total critical-care time. A notation in the medical record should reflect this (e.g., time spent inserting a central line is not included in today’s critical-care time).
Location
Because a patient can become seriously ill in any setting, physicians often provide critical-care services in emergency departments (EDs) and on standard medical-surgical floors before the patient is transferred to the intensive care unit (ICU).
Bed location alone does not determine critical-care reporting. Patients assigned to an ICU might be critically ill or injured and meet the “condition” requirements for 99291-99292.
However, the care provided may not meet the remaining requirements. According to the American Medical Association’s Current Procedural Terminology 2008 (Professional Edition) and the Medicare Claims Processing Manual, payment can be made for critical-care services provided in any location as long as the care provided meets the definition of critical care. Services for a patient who is not critically ill and unstable but who happens to be receiving care in a critical-care, intensive-care, or other specialized-care unit are reported using subsequent hospital care codes 99231-99233 or hospital consultation codes 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.