User login
It's hard to imagine a busy urban hospital without its chorus of beepers.[1] This statement, the first sentence of an article published in 1988, rings (or beeps or buzzes) true to any resident physician today. At that time, pagers had replaced overhead paging, and provided a rapid method to contact physicians who were often scattered throughout the hospital. Still, it was an imperfect solution as the ubiquitous pager constantly interrupted patient care and other tasks, failed to prioritize information, and added to an already stressful working environment. Notably, interns were paged on average once per hour, and occasionally 5 or more times per hour, a frequency that was felt to be detrimental to patient care and to the working environment of resident physicians.[1]
Little has changed. Despite the instant, multidirectional communication platforms available today, alphanumeric paging remains a mainstay of communication between physicians and other members of the care team. Importantly, paging contributes to communication errors (eg, by failing to convey urgency, having incomplete information, or being missed entirely by coverage gaps),[2, 3] and interrupts resident workflow, thereby negatively affecting work efficiency and educational activities, and adding to perceived workload.[4, 5]
In this era of duty hour restrictions, there has been concern that residents experience increased workload due to having fewer hours to do the same amount of work.[6, 7] As such, the Accreditation Council of Graduate Medical Education emphasizes the quality of those hours, with a focus on several aspects of the resident working environment as key to improved educational and patient safety outcomes.[8, 9, 10]
Geographic localization of physicians to patient care units has been proposed as a means to improve communication and agreement on plans of care,[11, 12] and also to reduce resident workload by decreasing inefficiencies attributable to traveling throughout the hospital.[13] O'Leary, et al. (2009) found that when physicians were localized to 1 hospital unit, there was greater agreement between physicians and nurses on various aspects of care, such as planned tests and anticipated length of stay. In addition, members of the patient care team were better able to identify one another, and there was a perceived increase in face‐to‐face communication, and a perceived decrease in text paging.[11]
In consideration of these factors, in July 2011, at New YorkPresbyterian Hospital/Weill Cornell (NYPH/WC), an 800‐bed tertiary care teaching hospital in New York, New York, we geographically localized 2 internal medicine resident teams, and partially localized 2 additional teams. We investigated whether interns on teams that were geographically localized received fewer pages than interns on teams that were not localized. This study was reviewed by the institutional review board of Weill Cornell Medical College and met the requirements for exemption.
METHODS
We conducted a retrospective analysis of the number of pages received by interns during the day (7:00 am to 7:00 pm) on 5 general internal medicine teams during a 1‐month ward rotation between October 17, 2011 and November 13, 2011 at NYPH/WC. The general medicine teams were composed of 1 attending, 1 resident, and 2 interns each. Two teams were geographically localized to a 32‐bed unit (geographic localization model [GLM]). Two teams were partially localized to a 26‐bed unit, which included a respiratory care step‐down unit (partial localization model [PLM]). A fifth and final team admitted patients irrespective of their assigned bed location (standard model [SM]). Both the GLM and the PLM occasionally carried patients on other units to allow for overall census management and patient throughput. The total number of pages received by each intern over the study period was collected by retrospective analysis of electronic paging logs. Night pages (7 pm7 am) were excluded because of night float coverage. Weekend pages were excluded because data were inaccurate due to coverage for days off.
The daily number of admissions and daily census per team were recorded by physician assistants, who also assigned new patients to appropriate teams according to an admissions algorithm (see Supporting Figure 1 in the online version of this article). The percent of geographically localized patients on each team was estimated from the percentage of localized patients on the day of discharge averaged over the study period. For the SM team, percent localization was defined as the number of patients on the patient care unit that contained the team's work area.
Standard multivariate linear regression techniques were used to analyze the relationship between the number of pages received per intern and the type of team, controlling for the potential effect of total census and number of admissions. The regression model was used to determine adjusted marginal point estimates and 95% confidence intervals (CIs) for the average number of pages per intern per hour for each type of team. All statistical analyses were conducted using Stata version 12 (StataCorp, College Station, TX).
RESULTS
Over the 28‐day study period, a total of 6652 pages were received by 10 interns on 5 general internal medicine teams from 7 am to 7 pm Monday through Friday. The average daily census, average daily admissions, and percent of patients localized to patient care units for the individual teams are shown in Table 1. In univariate analysis, the mean daily pages per intern were not significantly different between the 2 teams within the GLM, nor between the 2 teams in the PLM, allowing them to be combined in multivariate analysis (data not shown). The number of pages received per intern per hour, adjusted for team census and number of admissions, was 2.2 (95% CI: 2.02.4) in the GLM, 2.8 (95% CI: 2.6‐3.0) in the PLM, and 3.9 (95% CI: 3.6‐4.2) in the SM (Table 1). All of these differences were statistically significant (P<0.001).
| Standard Model* | Partial Localization Model | Geographically Localized Model | |
|---|---|---|---|
| |||
| Percent of patients localized | 37% | 45% | 85% |
| Team census, mean (range per day) | 16.1 (1320) | 15.9 (1120) | 15.6 (1119) |
| Team admissions, mean (range per day) | 2.7 (15) | 2.9 (06) | 3.5 (07) |
| Pages per hour per intern, unadjusted, mean (95% CI) | 3.9 (3.6‐4.1) | 2.8 (2.6‐3.0) | 2.2 (2.02.4) |
| Pages per hour per intern, adjusted for census and admissions, mean (95% CI) | 3.9 (3.6‐4.2) | 2.8 (2.6‐3.0) | 2.2 (2.02.4) |
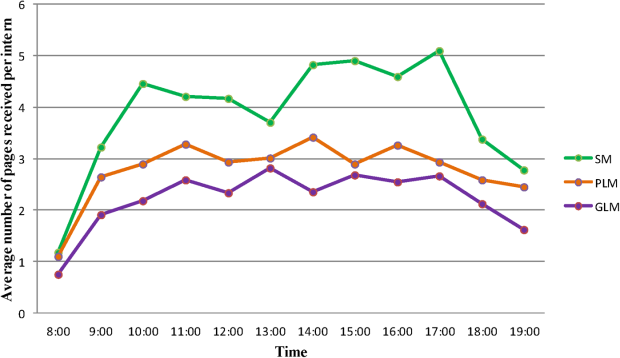
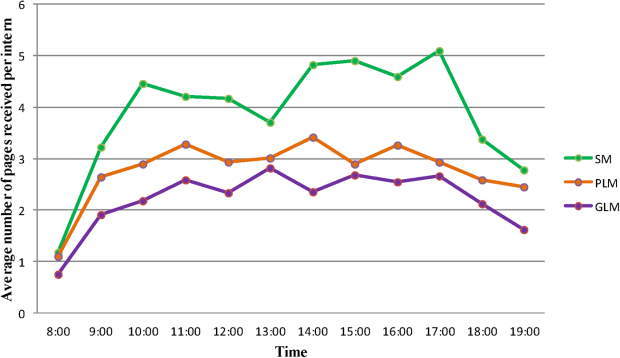
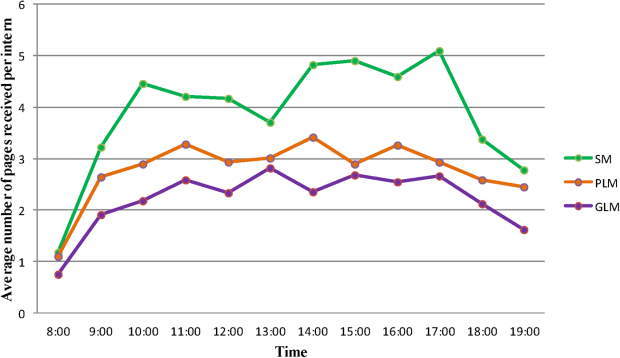
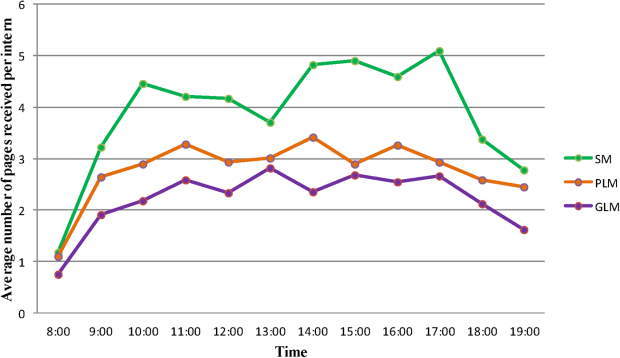
Figure 1 shows the pattern of daytime paging for each model. The GLM and PLM had a similar pattern, with an initial ramp up in the first 2 hours of the day, holding steady until approximately 4 pm, and then decrease until 7 pm. The SM had a steeper initial rise, and then continued to increase slowly until a peak at 4 pm.
DISCUSSION
This study corroborates that of Singh et al. (2012), who found that geographic localization led to significantly fewer pages.[14] Our results strengthen the evidence by demonstrating that even modest differences between the percent of patients localized to a care unit led to a significant decrease in the number of pages, indicating a dose‐response effect. The paging frequency we measured is higher than described in Singh et al. (1.4 pages per hour for localized teams), yet our average census appears to be 4 patients higher, which may account for some of that difference. We also show that interns on teams whose patients are more widely scattered throughout the hospital may experience upward of 5 pages per hour, an interruption by pager every 12 minutes, all day long.
A pager interruption is not solely limited to a disruption by noxious sound or vibration. The page recipient must then read the page and respond accordingly, which may involve a phone call, placing an order, walking to another location, or other work tasks. Although some of these interruptions must be handled immediately, such as a clinically deteriorating patient, many are not urgent, and could wait until the physician's current task or thought process is complete. There is also the potentially risky assumption on the part of the sender that the message has been received and will be acted upon. Furthermore, frequent paging is a common interruption to physician workflow; interruptions contribute to increased perceived physician workload[4, 5] and are likely detrimental to patient safety.[15, 16]
The most common metrics used to measure resident workload are patient census and number of admissions,[13] but these metrics have provided a mixed and likely incomplete picture. Recent research suggests that other factors, such as work efficiency (including interruptions, time spent obtaining test results, and time in transit) and work intensity (such as the acuity and complexity of patients), contribute significantly to actual and perceived resident workload.[13]
Our analysis was a single‐site, retrospective study, which occurred over 1 month and was limited to internal medicine teams. Additionally, geographic localization logically should lead to increased face‐to‐face interruptions, which we were unable to measure with this project, but direct communication is more efficient and less prone to error, which would likely lead to fewer overall interruptions. Although we anticipate that our findings are applicable to geographically localized patient care units in other hospitals, further investigation is warranted.
The paging chorus has only grown louder over the last 25 years, with likely downstream effects on patient safety and resident education. To mitigate these effects, it is incumbent upon us to approach our training and patient care environments with a critical and creative lens, and to explore opportunities to decrease interruptions and streamline our communication systems.
Acknowledgements
The authors acknowledge the assistance with data analysis of Arthur Evans, MD, MPH, and review of the manuscript by Brendan Reilly, MD.
Disclosures: Dr. Fanucchi and Ms. Unterbrink have no conflicts of interest to disclose. Dr. Logio reports receiving royalties from McGraw‐Hill for Core Concepts in Patient Safety online modules.
- , . The sounds of the hospital. Paging patterns in three teaching hospitals. N Engl J Med. 1988;319(24):1585–1589.
- , , . Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194.
- , , . Alphanumeric paging: a potential source of problems in patient care and communication. J Surg Educ. 2011;68(6):447–451.
- , , , , . Hospital doctors' workflow interruptions and activities: an observation study. BMJ Qual Saf. 2011;20(6):491–497.
- , , , , . The association of workflow interruptions and hospital doctors' workload: a prospective observational study. BMJ Qual Saf. 2012;21(5):399–407.
- , . Resident workload—let's treat the disease, not just the symptom. Comment on: Effect of the 2011 vs 2003 duty hour regulation‐compliant models on sleep duration, trainee education, and continuity of patient care among internal medicine house staff. JAMA Intern Med. 2013;173(8):655–656.
- , , , et al. Effect of the 2011 vs 2003 duty hour regulation‐compliant models on sleep duration, trainee education, and continuity of patient care among internal medicine house staff: a randomized trial. JAMA Intern Med. 2013;173(8):649–655.
- , . The ACGME 2011 Duty Hour Standards: Enhancing Quality of Care, Supervision, and Resident Professional Development. Chicago, IL: Accreditation Council for Graduate Medical Education; 2011.
- , , , . Institute of Medicine Resident Duty Hours: Enhancing Sleep, Supervision, and Safety. Washington, DC: National Academies Press; 2009.
- , , , , , . Perspective: beyond counting hours: the importance of supervision, professionalism, transitions of care, and workload in residency training. Acad Med. 2012;87(7):883–888.
- , , , et al. Impact of localizing physicians to hospital units on nurse‐physician communication and agreement on the plan of care. J Gen Intern Med. 2009;24(11):1223–1227.
- , , , et al. Unit‐based care teams and the frequency and quality of physician‐nurse communications. Arch Pediatr Adolesc Med. 2011;165(5):424–428.
- , , , et al. Service census caps and unit‐based admissions: resident workload, conference attendance, duty hour compliance, and patient safety. Mayo Clin Proc. 2012;87(4):320–327.
- , , , et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551–556.
- . The science of interruption. BMJ Qual Saf. 2012;21(5):357–360.
- , , , et al. The impact of interruptions on clinical task completion. Qual Saf Health Care. 2010;19(4):284–289.
It's hard to imagine a busy urban hospital without its chorus of beepers.[1] This statement, the first sentence of an article published in 1988, rings (or beeps or buzzes) true to any resident physician today. At that time, pagers had replaced overhead paging, and provided a rapid method to contact physicians who were often scattered throughout the hospital. Still, it was an imperfect solution as the ubiquitous pager constantly interrupted patient care and other tasks, failed to prioritize information, and added to an already stressful working environment. Notably, interns were paged on average once per hour, and occasionally 5 or more times per hour, a frequency that was felt to be detrimental to patient care and to the working environment of resident physicians.[1]
Little has changed. Despite the instant, multidirectional communication platforms available today, alphanumeric paging remains a mainstay of communication between physicians and other members of the care team. Importantly, paging contributes to communication errors (eg, by failing to convey urgency, having incomplete information, or being missed entirely by coverage gaps),[2, 3] and interrupts resident workflow, thereby negatively affecting work efficiency and educational activities, and adding to perceived workload.[4, 5]
In this era of duty hour restrictions, there has been concern that residents experience increased workload due to having fewer hours to do the same amount of work.[6, 7] As such, the Accreditation Council of Graduate Medical Education emphasizes the quality of those hours, with a focus on several aspects of the resident working environment as key to improved educational and patient safety outcomes.[8, 9, 10]
Geographic localization of physicians to patient care units has been proposed as a means to improve communication and agreement on plans of care,[11, 12] and also to reduce resident workload by decreasing inefficiencies attributable to traveling throughout the hospital.[13] O'Leary, et al. (2009) found that when physicians were localized to 1 hospital unit, there was greater agreement between physicians and nurses on various aspects of care, such as planned tests and anticipated length of stay. In addition, members of the patient care team were better able to identify one another, and there was a perceived increase in face‐to‐face communication, and a perceived decrease in text paging.[11]
In consideration of these factors, in July 2011, at New YorkPresbyterian Hospital/Weill Cornell (NYPH/WC), an 800‐bed tertiary care teaching hospital in New York, New York, we geographically localized 2 internal medicine resident teams, and partially localized 2 additional teams. We investigated whether interns on teams that were geographically localized received fewer pages than interns on teams that were not localized. This study was reviewed by the institutional review board of Weill Cornell Medical College and met the requirements for exemption.
METHODS
We conducted a retrospective analysis of the number of pages received by interns during the day (7:00 am to 7:00 pm) on 5 general internal medicine teams during a 1‐month ward rotation between October 17, 2011 and November 13, 2011 at NYPH/WC. The general medicine teams were composed of 1 attending, 1 resident, and 2 interns each. Two teams were geographically localized to a 32‐bed unit (geographic localization model [GLM]). Two teams were partially localized to a 26‐bed unit, which included a respiratory care step‐down unit (partial localization model [PLM]). A fifth and final team admitted patients irrespective of their assigned bed location (standard model [SM]). Both the GLM and the PLM occasionally carried patients on other units to allow for overall census management and patient throughput. The total number of pages received by each intern over the study period was collected by retrospective analysis of electronic paging logs. Night pages (7 pm7 am) were excluded because of night float coverage. Weekend pages were excluded because data were inaccurate due to coverage for days off.
The daily number of admissions and daily census per team were recorded by physician assistants, who also assigned new patients to appropriate teams according to an admissions algorithm (see Supporting Figure 1 in the online version of this article). The percent of geographically localized patients on each team was estimated from the percentage of localized patients on the day of discharge averaged over the study period. For the SM team, percent localization was defined as the number of patients on the patient care unit that contained the team's work area.
Standard multivariate linear regression techniques were used to analyze the relationship between the number of pages received per intern and the type of team, controlling for the potential effect of total census and number of admissions. The regression model was used to determine adjusted marginal point estimates and 95% confidence intervals (CIs) for the average number of pages per intern per hour for each type of team. All statistical analyses were conducted using Stata version 12 (StataCorp, College Station, TX).
RESULTS
Over the 28‐day study period, a total of 6652 pages were received by 10 interns on 5 general internal medicine teams from 7 am to 7 pm Monday through Friday. The average daily census, average daily admissions, and percent of patients localized to patient care units for the individual teams are shown in Table 1. In univariate analysis, the mean daily pages per intern were not significantly different between the 2 teams within the GLM, nor between the 2 teams in the PLM, allowing them to be combined in multivariate analysis (data not shown). The number of pages received per intern per hour, adjusted for team census and number of admissions, was 2.2 (95% CI: 2.02.4) in the GLM, 2.8 (95% CI: 2.6‐3.0) in the PLM, and 3.9 (95% CI: 3.6‐4.2) in the SM (Table 1). All of these differences were statistically significant (P<0.001).
| Standard Model* | Partial Localization Model | Geographically Localized Model | |
|---|---|---|---|
| |||
| Percent of patients localized | 37% | 45% | 85% |
| Team census, mean (range per day) | 16.1 (1320) | 15.9 (1120) | 15.6 (1119) |
| Team admissions, mean (range per day) | 2.7 (15) | 2.9 (06) | 3.5 (07) |
| Pages per hour per intern, unadjusted, mean (95% CI) | 3.9 (3.6‐4.1) | 2.8 (2.6‐3.0) | 2.2 (2.02.4) |
| Pages per hour per intern, adjusted for census and admissions, mean (95% CI) | 3.9 (3.6‐4.2) | 2.8 (2.6‐3.0) | 2.2 (2.02.4) |
Figure 1 shows the pattern of daytime paging for each model. The GLM and PLM had a similar pattern, with an initial ramp up in the first 2 hours of the day, holding steady until approximately 4 pm, and then decrease until 7 pm. The SM had a steeper initial rise, and then continued to increase slowly until a peak at 4 pm.
DISCUSSION
This study corroborates that of Singh et al. (2012), who found that geographic localization led to significantly fewer pages.[14] Our results strengthen the evidence by demonstrating that even modest differences between the percent of patients localized to a care unit led to a significant decrease in the number of pages, indicating a dose‐response effect. The paging frequency we measured is higher than described in Singh et al. (1.4 pages per hour for localized teams), yet our average census appears to be 4 patients higher, which may account for some of that difference. We also show that interns on teams whose patients are more widely scattered throughout the hospital may experience upward of 5 pages per hour, an interruption by pager every 12 minutes, all day long.
A pager interruption is not solely limited to a disruption by noxious sound or vibration. The page recipient must then read the page and respond accordingly, which may involve a phone call, placing an order, walking to another location, or other work tasks. Although some of these interruptions must be handled immediately, such as a clinically deteriorating patient, many are not urgent, and could wait until the physician's current task or thought process is complete. There is also the potentially risky assumption on the part of the sender that the message has been received and will be acted upon. Furthermore, frequent paging is a common interruption to physician workflow; interruptions contribute to increased perceived physician workload[4, 5] and are likely detrimental to patient safety.[15, 16]
The most common metrics used to measure resident workload are patient census and number of admissions,[13] but these metrics have provided a mixed and likely incomplete picture. Recent research suggests that other factors, such as work efficiency (including interruptions, time spent obtaining test results, and time in transit) and work intensity (such as the acuity and complexity of patients), contribute significantly to actual and perceived resident workload.[13]
Our analysis was a single‐site, retrospective study, which occurred over 1 month and was limited to internal medicine teams. Additionally, geographic localization logically should lead to increased face‐to‐face interruptions, which we were unable to measure with this project, but direct communication is more efficient and less prone to error, which would likely lead to fewer overall interruptions. Although we anticipate that our findings are applicable to geographically localized patient care units in other hospitals, further investigation is warranted.
The paging chorus has only grown louder over the last 25 years, with likely downstream effects on patient safety and resident education. To mitigate these effects, it is incumbent upon us to approach our training and patient care environments with a critical and creative lens, and to explore opportunities to decrease interruptions and streamline our communication systems.
Acknowledgements
The authors acknowledge the assistance with data analysis of Arthur Evans, MD, MPH, and review of the manuscript by Brendan Reilly, MD.
Disclosures: Dr. Fanucchi and Ms. Unterbrink have no conflicts of interest to disclose. Dr. Logio reports receiving royalties from McGraw‐Hill for Core Concepts in Patient Safety online modules.
It's hard to imagine a busy urban hospital without its chorus of beepers.[1] This statement, the first sentence of an article published in 1988, rings (or beeps or buzzes) true to any resident physician today. At that time, pagers had replaced overhead paging, and provided a rapid method to contact physicians who were often scattered throughout the hospital. Still, it was an imperfect solution as the ubiquitous pager constantly interrupted patient care and other tasks, failed to prioritize information, and added to an already stressful working environment. Notably, interns were paged on average once per hour, and occasionally 5 or more times per hour, a frequency that was felt to be detrimental to patient care and to the working environment of resident physicians.[1]
Little has changed. Despite the instant, multidirectional communication platforms available today, alphanumeric paging remains a mainstay of communication between physicians and other members of the care team. Importantly, paging contributes to communication errors (eg, by failing to convey urgency, having incomplete information, or being missed entirely by coverage gaps),[2, 3] and interrupts resident workflow, thereby negatively affecting work efficiency and educational activities, and adding to perceived workload.[4, 5]
In this era of duty hour restrictions, there has been concern that residents experience increased workload due to having fewer hours to do the same amount of work.[6, 7] As such, the Accreditation Council of Graduate Medical Education emphasizes the quality of those hours, with a focus on several aspects of the resident working environment as key to improved educational and patient safety outcomes.[8, 9, 10]
Geographic localization of physicians to patient care units has been proposed as a means to improve communication and agreement on plans of care,[11, 12] and also to reduce resident workload by decreasing inefficiencies attributable to traveling throughout the hospital.[13] O'Leary, et al. (2009) found that when physicians were localized to 1 hospital unit, there was greater agreement between physicians and nurses on various aspects of care, such as planned tests and anticipated length of stay. In addition, members of the patient care team were better able to identify one another, and there was a perceived increase in face‐to‐face communication, and a perceived decrease in text paging.[11]
In consideration of these factors, in July 2011, at New YorkPresbyterian Hospital/Weill Cornell (NYPH/WC), an 800‐bed tertiary care teaching hospital in New York, New York, we geographically localized 2 internal medicine resident teams, and partially localized 2 additional teams. We investigated whether interns on teams that were geographically localized received fewer pages than interns on teams that were not localized. This study was reviewed by the institutional review board of Weill Cornell Medical College and met the requirements for exemption.
METHODS
We conducted a retrospective analysis of the number of pages received by interns during the day (7:00 am to 7:00 pm) on 5 general internal medicine teams during a 1‐month ward rotation between October 17, 2011 and November 13, 2011 at NYPH/WC. The general medicine teams were composed of 1 attending, 1 resident, and 2 interns each. Two teams were geographically localized to a 32‐bed unit (geographic localization model [GLM]). Two teams were partially localized to a 26‐bed unit, which included a respiratory care step‐down unit (partial localization model [PLM]). A fifth and final team admitted patients irrespective of their assigned bed location (standard model [SM]). Both the GLM and the PLM occasionally carried patients on other units to allow for overall census management and patient throughput. The total number of pages received by each intern over the study period was collected by retrospective analysis of electronic paging logs. Night pages (7 pm7 am) were excluded because of night float coverage. Weekend pages were excluded because data were inaccurate due to coverage for days off.
The daily number of admissions and daily census per team were recorded by physician assistants, who also assigned new patients to appropriate teams according to an admissions algorithm (see Supporting Figure 1 in the online version of this article). The percent of geographically localized patients on each team was estimated from the percentage of localized patients on the day of discharge averaged over the study period. For the SM team, percent localization was defined as the number of patients on the patient care unit that contained the team's work area.
Standard multivariate linear regression techniques were used to analyze the relationship between the number of pages received per intern and the type of team, controlling for the potential effect of total census and number of admissions. The regression model was used to determine adjusted marginal point estimates and 95% confidence intervals (CIs) for the average number of pages per intern per hour for each type of team. All statistical analyses were conducted using Stata version 12 (StataCorp, College Station, TX).
RESULTS
Over the 28‐day study period, a total of 6652 pages were received by 10 interns on 5 general internal medicine teams from 7 am to 7 pm Monday through Friday. The average daily census, average daily admissions, and percent of patients localized to patient care units for the individual teams are shown in Table 1. In univariate analysis, the mean daily pages per intern were not significantly different between the 2 teams within the GLM, nor between the 2 teams in the PLM, allowing them to be combined in multivariate analysis (data not shown). The number of pages received per intern per hour, adjusted for team census and number of admissions, was 2.2 (95% CI: 2.02.4) in the GLM, 2.8 (95% CI: 2.6‐3.0) in the PLM, and 3.9 (95% CI: 3.6‐4.2) in the SM (Table 1). All of these differences were statistically significant (P<0.001).
| Standard Model* | Partial Localization Model | Geographically Localized Model | |
|---|---|---|---|
| |||
| Percent of patients localized | 37% | 45% | 85% |
| Team census, mean (range per day) | 16.1 (1320) | 15.9 (1120) | 15.6 (1119) |
| Team admissions, mean (range per day) | 2.7 (15) | 2.9 (06) | 3.5 (07) |
| Pages per hour per intern, unadjusted, mean (95% CI) | 3.9 (3.6‐4.1) | 2.8 (2.6‐3.0) | 2.2 (2.02.4) |
| Pages per hour per intern, adjusted for census and admissions, mean (95% CI) | 3.9 (3.6‐4.2) | 2.8 (2.6‐3.0) | 2.2 (2.02.4) |
Figure 1 shows the pattern of daytime paging for each model. The GLM and PLM had a similar pattern, with an initial ramp up in the first 2 hours of the day, holding steady until approximately 4 pm, and then decrease until 7 pm. The SM had a steeper initial rise, and then continued to increase slowly until a peak at 4 pm.
DISCUSSION
This study corroborates that of Singh et al. (2012), who found that geographic localization led to significantly fewer pages.[14] Our results strengthen the evidence by demonstrating that even modest differences between the percent of patients localized to a care unit led to a significant decrease in the number of pages, indicating a dose‐response effect. The paging frequency we measured is higher than described in Singh et al. (1.4 pages per hour for localized teams), yet our average census appears to be 4 patients higher, which may account for some of that difference. We also show that interns on teams whose patients are more widely scattered throughout the hospital may experience upward of 5 pages per hour, an interruption by pager every 12 minutes, all day long.
A pager interruption is not solely limited to a disruption by noxious sound or vibration. The page recipient must then read the page and respond accordingly, which may involve a phone call, placing an order, walking to another location, or other work tasks. Although some of these interruptions must be handled immediately, such as a clinically deteriorating patient, many are not urgent, and could wait until the physician's current task or thought process is complete. There is also the potentially risky assumption on the part of the sender that the message has been received and will be acted upon. Furthermore, frequent paging is a common interruption to physician workflow; interruptions contribute to increased perceived physician workload[4, 5] and are likely detrimental to patient safety.[15, 16]
The most common metrics used to measure resident workload are patient census and number of admissions,[13] but these metrics have provided a mixed and likely incomplete picture. Recent research suggests that other factors, such as work efficiency (including interruptions, time spent obtaining test results, and time in transit) and work intensity (such as the acuity and complexity of patients), contribute significantly to actual and perceived resident workload.[13]
Our analysis was a single‐site, retrospective study, which occurred over 1 month and was limited to internal medicine teams. Additionally, geographic localization logically should lead to increased face‐to‐face interruptions, which we were unable to measure with this project, but direct communication is more efficient and less prone to error, which would likely lead to fewer overall interruptions. Although we anticipate that our findings are applicable to geographically localized patient care units in other hospitals, further investigation is warranted.
The paging chorus has only grown louder over the last 25 years, with likely downstream effects on patient safety and resident education. To mitigate these effects, it is incumbent upon us to approach our training and patient care environments with a critical and creative lens, and to explore opportunities to decrease interruptions and streamline our communication systems.
Acknowledgements
The authors acknowledge the assistance with data analysis of Arthur Evans, MD, MPH, and review of the manuscript by Brendan Reilly, MD.
Disclosures: Dr. Fanucchi and Ms. Unterbrink have no conflicts of interest to disclose. Dr. Logio reports receiving royalties from McGraw‐Hill for Core Concepts in Patient Safety online modules.
- , . The sounds of the hospital. Paging patterns in three teaching hospitals. N Engl J Med. 1988;319(24):1585–1589.
- , , . Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194.
- , , . Alphanumeric paging: a potential source of problems in patient care and communication. J Surg Educ. 2011;68(6):447–451.
- , , , , . Hospital doctors' workflow interruptions and activities: an observation study. BMJ Qual Saf. 2011;20(6):491–497.
- , , , , . The association of workflow interruptions and hospital doctors' workload: a prospective observational study. BMJ Qual Saf. 2012;21(5):399–407.
- , . Resident workload—let's treat the disease, not just the symptom. Comment on: Effect of the 2011 vs 2003 duty hour regulation‐compliant models on sleep duration, trainee education, and continuity of patient care among internal medicine house staff. JAMA Intern Med. 2013;173(8):655–656.
- , , , et al. Effect of the 2011 vs 2003 duty hour regulation‐compliant models on sleep duration, trainee education, and continuity of patient care among internal medicine house staff: a randomized trial. JAMA Intern Med. 2013;173(8):649–655.
- , . The ACGME 2011 Duty Hour Standards: Enhancing Quality of Care, Supervision, and Resident Professional Development. Chicago, IL: Accreditation Council for Graduate Medical Education; 2011.
- , , , . Institute of Medicine Resident Duty Hours: Enhancing Sleep, Supervision, and Safety. Washington, DC: National Academies Press; 2009.
- , , , , , . Perspective: beyond counting hours: the importance of supervision, professionalism, transitions of care, and workload in residency training. Acad Med. 2012;87(7):883–888.
- , , , et al. Impact of localizing physicians to hospital units on nurse‐physician communication and agreement on the plan of care. J Gen Intern Med. 2009;24(11):1223–1227.
- , , , et al. Unit‐based care teams and the frequency and quality of physician‐nurse communications. Arch Pediatr Adolesc Med. 2011;165(5):424–428.
- , , , et al. Service census caps and unit‐based admissions: resident workload, conference attendance, duty hour compliance, and patient safety. Mayo Clin Proc. 2012;87(4):320–327.
- , , , et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551–556.
- . The science of interruption. BMJ Qual Saf. 2012;21(5):357–360.
- , , , et al. The impact of interruptions on clinical task completion. Qual Saf Health Care. 2010;19(4):284–289.
- , . The sounds of the hospital. Paging patterns in three teaching hospitals. N Engl J Med. 1988;319(24):1585–1589.
- , , . Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194.
- , , . Alphanumeric paging: a potential source of problems in patient care and communication. J Surg Educ. 2011;68(6):447–451.
- , , , , . Hospital doctors' workflow interruptions and activities: an observation study. BMJ Qual Saf. 2011;20(6):491–497.
- , , , , . The association of workflow interruptions and hospital doctors' workload: a prospective observational study. BMJ Qual Saf. 2012;21(5):399–407.
- , . Resident workload—let's treat the disease, not just the symptom. Comment on: Effect of the 2011 vs 2003 duty hour regulation‐compliant models on sleep duration, trainee education, and continuity of patient care among internal medicine house staff. JAMA Intern Med. 2013;173(8):655–656.
- , , , et al. Effect of the 2011 vs 2003 duty hour regulation‐compliant models on sleep duration, trainee education, and continuity of patient care among internal medicine house staff: a randomized trial. JAMA Intern Med. 2013;173(8):649–655.
- , . The ACGME 2011 Duty Hour Standards: Enhancing Quality of Care, Supervision, and Resident Professional Development. Chicago, IL: Accreditation Council for Graduate Medical Education; 2011.
- , , , . Institute of Medicine Resident Duty Hours: Enhancing Sleep, Supervision, and Safety. Washington, DC: National Academies Press; 2009.
- , , , , , . Perspective: beyond counting hours: the importance of supervision, professionalism, transitions of care, and workload in residency training. Acad Med. 2012;87(7):883–888.
- , , , et al. Impact of localizing physicians to hospital units on nurse‐physician communication and agreement on the plan of care. J Gen Intern Med. 2009;24(11):1223–1227.
- , , , et al. Unit‐based care teams and the frequency and quality of physician‐nurse communications. Arch Pediatr Adolesc Med. 2011;165(5):424–428.
- , , , et al. Service census caps and unit‐based admissions: resident workload, conference attendance, duty hour compliance, and patient safety. Mayo Clin Proc. 2012;87(4):320–327.
- , , , et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551–556.
- . The science of interruption. BMJ Qual Saf. 2012;21(5):357–360.
- , , , et al. The impact of interruptions on clinical task completion. Qual Saf Health Care. 2010;19(4):284–289.