User login
THE CASE
An 84-year old woman came to the emergency department (ED) with sharp back pain on her left side that she’d had for 4 days. The pain radiated to her posterior hips when standing. She said her whole body felt achy and she was experiencing weakness in both legs.
The patient had a history of hypertension, coronary artery disease, and aortic stenosis; she’d received a bioprosthetic aortic valve 7 years ago. She was not immunocompromised or receiving steroids but was taking docusate, oxybutynin, carvedilol, amlodipine, atorvastatin, furosemide, rivaroxaban, and a multivitamin. Her physical exam, vital signs, and complete blood count (CBC) were normal. An x-ray of the lumbar spine showed degenerative joint/disc disease and spondylosis at L4-L5 and L5-S1. The patient was sent home with oxycodone/acetaminophen 5 mg/325 mg every 6 hours as needed for pain and told to follow up with her family physician (FP).
Six days later, the patient went to see her FP and told her that her symptoms hadn’t improved. She was afebrile and her blood pressure was 150/80 mm Hg. Her muscle strength was 4/5 with hip flexion bilaterally; the rest of her strength was 5/5. There was no lumbar paraspinal tenderness and she had a negative straight leg raise test. No other neurologic deficits were noted. The FP prescribed physical therapy at home with a licensed therapist, which consisted of stretching exercises and active, dynamic exercise to improve the patient’s range of motion. She also ordered outpatient lumbar magnetic resonance imaging (MRI).
THE DIAGNOSIS
Approximately 3 weeks later, the patient’s MRI revealed osteomyelitis/discitis at the L3-L4 level and severe tricompartmental stenosis from L2-L3 through L4-L5. A day after receiving the results—and about a month after having first gone to the ED—the patient was admitted to the hospital. She was afebrile and her blood pressure was 148/75 mm Hg. Her physical exam revealed no leukocytosis or neurologic deficits, but did show a systolic murmur from her aortic valve.
She had an erythrocyte sedimentation rate (ESR) of 77 mm/hr (normal range for women, <30 mm/hr) and her C-reactive protein (CRP) level was 5.88 mg/dL (<.50 mg/dL indicates average risk for cardiovascular disease). A transesophageal echocardiogram was performed and there was no sign of vegetation or thrombi. However, blood cultures were positive for Streptococcus salivarius—a bacterium found on human dental plaque—which we determined was the cause of the osteomyelitis.
To the best of our knowledge, there have been no other case reports that described S. salivarius as having caused osteomyelitis without concurrent endocarditis.
DISCUSSION
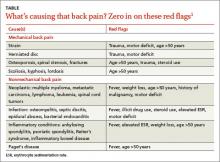
Back pain is a common and costly issue among primary care patients. More than two-thirds of adults suffer from low back pain at some point, primarily without underlying malignancy or neurologic deficits.1,2 Acute low back pain is often mechanical (97%); however, other causes, including infection, may be to blame (TABLE).1 Most acute back pain will improve with conservative treatment and patients need only reassurance of a favorable prognosis, but 20% of patients may develop chronic back pain.2
The diagnostic approach to low back pain varies widely.3 Some data indicate that early imaging of back pain can lead to unneeded follow-up testing, radiation exposure, unnecessary surgery, patient “labeling,” and increased health care costs, all of which suggest that routine imaging shouldn’t be pursued in acute low back pain.4
Red flags for acute low back pain that warrant imaging include age >50 years, fever, weight loss, elevated ESR, history of malignancy, trauma, motor deficits, steroid or illicit drug use, and litigation.1 If not already done, it’s also important to order a CBC, ESR, and CRP for patients with any of these red flags.
Imaging studies are important, but clinical correlation is crucial because imaging can reveal disk abnormalities even in healthy, asymptomatic patients.5 Computed tomography scans or MRI is indicated for patients with neurologic deficits or nerve root tension signs, but only if a patient is a potential candidate for surgery or epidural steroid injection.6,7 If you suspect an infection (such as spondylodiscitis or osteomyelitis), diagnosing the condition quickly is key.
Our patient had 2 red flags (age >50 years and elevated ESR) that helped us reach an unlikely diagnosis of lumbar osteomyelitis with S. salivarius as the cause. Degenerative spinal disease seen on x-ray may have delayed our patient’s diagnosis. If our patient had had an ESR or CRP test earlier, or if further imaging had been conducted sooner (given her proximal muscle weakness), the correct diagnosis would have been made more quickly and appropriate treatment provided sooner.
Our patient
The patient was started on a 6-week course of intravenous ceftriaxone 2g/d, which she continued to receive at home via a peripherally inserted central catheter. The patient was instructed at discharge (on Day 8) to follow up with her FP, which she did 12 days later. At that visit, her back pain was improved and her ESR and CRP levels were within normal ranges.
THE TAKEAWAY
When evaluating a patient who presents with low back pain, perform a focused history and be on the lookout for “red flags” that warrant further imaging and testing. Routine imaging is not recommended for patients with nonspecific low back pain, but imaging may be indicated for patients with neurologic deficits or nerve root tension signs.
A patient with low back pain caused by osteomyelitis may present with fever, elevated ESR, and/or motor deficits. Identifying the bacteria underlying the infection will help guide selection of appropriate antibiotics.
1. Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001;344:363-370.
2. Deyo RA, Phillips WR. Low back pain. A primary care challenge. Spine (Phila Pa 1976). 1996;21:2826-2832.
3. Cherkin DC, Deyo RA, Wheeler K, et al. Physician variation in diagnostic testing for low back pain. Who you see is what you get. Arthritis Rheum. 1994;37:15-22.
4. Srinivas SV, Deyo RA, Berger ZD. Application of “less is more” to low back pain. Arch Intern Med. 2012;172:1016-1020.
5. Jensen MC, Brant-Zawadzki MN, Obuchowski N, et al. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69-73.
6. Wipf JE, Deyo RA. Low back pain. Med Clin North Am. 1995;79:231-246.
7. Chou R, Qaseem A, Snow V, et al; Clinical Efficacy Assessment Committee of the American College of Physicians; American College of Physicians; American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-493.
THE CASE
An 84-year old woman came to the emergency department (ED) with sharp back pain on her left side that she’d had for 4 days. The pain radiated to her posterior hips when standing. She said her whole body felt achy and she was experiencing weakness in both legs.
The patient had a history of hypertension, coronary artery disease, and aortic stenosis; she’d received a bioprosthetic aortic valve 7 years ago. She was not immunocompromised or receiving steroids but was taking docusate, oxybutynin, carvedilol, amlodipine, atorvastatin, furosemide, rivaroxaban, and a multivitamin. Her physical exam, vital signs, and complete blood count (CBC) were normal. An x-ray of the lumbar spine showed degenerative joint/disc disease and spondylosis at L4-L5 and L5-S1. The patient was sent home with oxycodone/acetaminophen 5 mg/325 mg every 6 hours as needed for pain and told to follow up with her family physician (FP).
Six days later, the patient went to see her FP and told her that her symptoms hadn’t improved. She was afebrile and her blood pressure was 150/80 mm Hg. Her muscle strength was 4/5 with hip flexion bilaterally; the rest of her strength was 5/5. There was no lumbar paraspinal tenderness and she had a negative straight leg raise test. No other neurologic deficits were noted. The FP prescribed physical therapy at home with a licensed therapist, which consisted of stretching exercises and active, dynamic exercise to improve the patient’s range of motion. She also ordered outpatient lumbar magnetic resonance imaging (MRI).
THE DIAGNOSIS
Approximately 3 weeks later, the patient’s MRI revealed osteomyelitis/discitis at the L3-L4 level and severe tricompartmental stenosis from L2-L3 through L4-L5. A day after receiving the results—and about a month after having first gone to the ED—the patient was admitted to the hospital. She was afebrile and her blood pressure was 148/75 mm Hg. Her physical exam revealed no leukocytosis or neurologic deficits, but did show a systolic murmur from her aortic valve.
She had an erythrocyte sedimentation rate (ESR) of 77 mm/hr (normal range for women, <30 mm/hr) and her C-reactive protein (CRP) level was 5.88 mg/dL (<.50 mg/dL indicates average risk for cardiovascular disease). A transesophageal echocardiogram was performed and there was no sign of vegetation or thrombi. However, blood cultures were positive for Streptococcus salivarius—a bacterium found on human dental plaque—which we determined was the cause of the osteomyelitis.
To the best of our knowledge, there have been no other case reports that described S. salivarius as having caused osteomyelitis without concurrent endocarditis.
DISCUSSION
Back pain is a common and costly issue among primary care patients. More than two-thirds of adults suffer from low back pain at some point, primarily without underlying malignancy or neurologic deficits.1,2 Acute low back pain is often mechanical (97%); however, other causes, including infection, may be to blame (TABLE).1 Most acute back pain will improve with conservative treatment and patients need only reassurance of a favorable prognosis, but 20% of patients may develop chronic back pain.2
The diagnostic approach to low back pain varies widely.3 Some data indicate that early imaging of back pain can lead to unneeded follow-up testing, radiation exposure, unnecessary surgery, patient “labeling,” and increased health care costs, all of which suggest that routine imaging shouldn’t be pursued in acute low back pain.4
Red flags for acute low back pain that warrant imaging include age >50 years, fever, weight loss, elevated ESR, history of malignancy, trauma, motor deficits, steroid or illicit drug use, and litigation.1 If not already done, it’s also important to order a CBC, ESR, and CRP for patients with any of these red flags.
Imaging studies are important, but clinical correlation is crucial because imaging can reveal disk abnormalities even in healthy, asymptomatic patients.5 Computed tomography scans or MRI is indicated for patients with neurologic deficits or nerve root tension signs, but only if a patient is a potential candidate for surgery or epidural steroid injection.6,7 If you suspect an infection (such as spondylodiscitis or osteomyelitis), diagnosing the condition quickly is key.
Our patient had 2 red flags (age >50 years and elevated ESR) that helped us reach an unlikely diagnosis of lumbar osteomyelitis with S. salivarius as the cause. Degenerative spinal disease seen on x-ray may have delayed our patient’s diagnosis. If our patient had had an ESR or CRP test earlier, or if further imaging had been conducted sooner (given her proximal muscle weakness), the correct diagnosis would have been made more quickly and appropriate treatment provided sooner.
Our patient
The patient was started on a 6-week course of intravenous ceftriaxone 2g/d, which she continued to receive at home via a peripherally inserted central catheter. The patient was instructed at discharge (on Day 8) to follow up with her FP, which she did 12 days later. At that visit, her back pain was improved and her ESR and CRP levels were within normal ranges.
THE TAKEAWAY
When evaluating a patient who presents with low back pain, perform a focused history and be on the lookout for “red flags” that warrant further imaging and testing. Routine imaging is not recommended for patients with nonspecific low back pain, but imaging may be indicated for patients with neurologic deficits or nerve root tension signs.
A patient with low back pain caused by osteomyelitis may present with fever, elevated ESR, and/or motor deficits. Identifying the bacteria underlying the infection will help guide selection of appropriate antibiotics.
THE CASE
An 84-year old woman came to the emergency department (ED) with sharp back pain on her left side that she’d had for 4 days. The pain radiated to her posterior hips when standing. She said her whole body felt achy and she was experiencing weakness in both legs.
The patient had a history of hypertension, coronary artery disease, and aortic stenosis; she’d received a bioprosthetic aortic valve 7 years ago. She was not immunocompromised or receiving steroids but was taking docusate, oxybutynin, carvedilol, amlodipine, atorvastatin, furosemide, rivaroxaban, and a multivitamin. Her physical exam, vital signs, and complete blood count (CBC) were normal. An x-ray of the lumbar spine showed degenerative joint/disc disease and spondylosis at L4-L5 and L5-S1. The patient was sent home with oxycodone/acetaminophen 5 mg/325 mg every 6 hours as needed for pain and told to follow up with her family physician (FP).
Six days later, the patient went to see her FP and told her that her symptoms hadn’t improved. She was afebrile and her blood pressure was 150/80 mm Hg. Her muscle strength was 4/5 with hip flexion bilaterally; the rest of her strength was 5/5. There was no lumbar paraspinal tenderness and she had a negative straight leg raise test. No other neurologic deficits were noted. The FP prescribed physical therapy at home with a licensed therapist, which consisted of stretching exercises and active, dynamic exercise to improve the patient’s range of motion. She also ordered outpatient lumbar magnetic resonance imaging (MRI).
THE DIAGNOSIS
Approximately 3 weeks later, the patient’s MRI revealed osteomyelitis/discitis at the L3-L4 level and severe tricompartmental stenosis from L2-L3 through L4-L5. A day after receiving the results—and about a month after having first gone to the ED—the patient was admitted to the hospital. She was afebrile and her blood pressure was 148/75 mm Hg. Her physical exam revealed no leukocytosis or neurologic deficits, but did show a systolic murmur from her aortic valve.
She had an erythrocyte sedimentation rate (ESR) of 77 mm/hr (normal range for women, <30 mm/hr) and her C-reactive protein (CRP) level was 5.88 mg/dL (<.50 mg/dL indicates average risk for cardiovascular disease). A transesophageal echocardiogram was performed and there was no sign of vegetation or thrombi. However, blood cultures were positive for Streptococcus salivarius—a bacterium found on human dental plaque—which we determined was the cause of the osteomyelitis.
To the best of our knowledge, there have been no other case reports that described S. salivarius as having caused osteomyelitis without concurrent endocarditis.
DISCUSSION
Back pain is a common and costly issue among primary care patients. More than two-thirds of adults suffer from low back pain at some point, primarily without underlying malignancy or neurologic deficits.1,2 Acute low back pain is often mechanical (97%); however, other causes, including infection, may be to blame (TABLE).1 Most acute back pain will improve with conservative treatment and patients need only reassurance of a favorable prognosis, but 20% of patients may develop chronic back pain.2
The diagnostic approach to low back pain varies widely.3 Some data indicate that early imaging of back pain can lead to unneeded follow-up testing, radiation exposure, unnecessary surgery, patient “labeling,” and increased health care costs, all of which suggest that routine imaging shouldn’t be pursued in acute low back pain.4
Red flags for acute low back pain that warrant imaging include age >50 years, fever, weight loss, elevated ESR, history of malignancy, trauma, motor deficits, steroid or illicit drug use, and litigation.1 If not already done, it’s also important to order a CBC, ESR, and CRP for patients with any of these red flags.
Imaging studies are important, but clinical correlation is crucial because imaging can reveal disk abnormalities even in healthy, asymptomatic patients.5 Computed tomography scans or MRI is indicated for patients with neurologic deficits or nerve root tension signs, but only if a patient is a potential candidate for surgery or epidural steroid injection.6,7 If you suspect an infection (such as spondylodiscitis or osteomyelitis), diagnosing the condition quickly is key.
Our patient had 2 red flags (age >50 years and elevated ESR) that helped us reach an unlikely diagnosis of lumbar osteomyelitis with S. salivarius as the cause. Degenerative spinal disease seen on x-ray may have delayed our patient’s diagnosis. If our patient had had an ESR or CRP test earlier, or if further imaging had been conducted sooner (given her proximal muscle weakness), the correct diagnosis would have been made more quickly and appropriate treatment provided sooner.
Our patient
The patient was started on a 6-week course of intravenous ceftriaxone 2g/d, which she continued to receive at home via a peripherally inserted central catheter. The patient was instructed at discharge (on Day 8) to follow up with her FP, which she did 12 days later. At that visit, her back pain was improved and her ESR and CRP levels were within normal ranges.
THE TAKEAWAY
When evaluating a patient who presents with low back pain, perform a focused history and be on the lookout for “red flags” that warrant further imaging and testing. Routine imaging is not recommended for patients with nonspecific low back pain, but imaging may be indicated for patients with neurologic deficits or nerve root tension signs.
A patient with low back pain caused by osteomyelitis may present with fever, elevated ESR, and/or motor deficits. Identifying the bacteria underlying the infection will help guide selection of appropriate antibiotics.
1. Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001;344:363-370.
2. Deyo RA, Phillips WR. Low back pain. A primary care challenge. Spine (Phila Pa 1976). 1996;21:2826-2832.
3. Cherkin DC, Deyo RA, Wheeler K, et al. Physician variation in diagnostic testing for low back pain. Who you see is what you get. Arthritis Rheum. 1994;37:15-22.
4. Srinivas SV, Deyo RA, Berger ZD. Application of “less is more” to low back pain. Arch Intern Med. 2012;172:1016-1020.
5. Jensen MC, Brant-Zawadzki MN, Obuchowski N, et al. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69-73.
6. Wipf JE, Deyo RA. Low back pain. Med Clin North Am. 1995;79:231-246.
7. Chou R, Qaseem A, Snow V, et al; Clinical Efficacy Assessment Committee of the American College of Physicians; American College of Physicians; American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-493.
1. Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001;344:363-370.
2. Deyo RA, Phillips WR. Low back pain. A primary care challenge. Spine (Phila Pa 1976). 1996;21:2826-2832.
3. Cherkin DC, Deyo RA, Wheeler K, et al. Physician variation in diagnostic testing for low back pain. Who you see is what you get. Arthritis Rheum. 1994;37:15-22.
4. Srinivas SV, Deyo RA, Berger ZD. Application of “less is more” to low back pain. Arch Intern Med. 2012;172:1016-1020.
5. Jensen MC, Brant-Zawadzki MN, Obuchowski N, et al. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69-73.
6. Wipf JE, Deyo RA. Low back pain. Med Clin North Am. 1995;79:231-246.
7. Chou R, Qaseem A, Snow V, et al; Clinical Efficacy Assessment Committee of the American College of Physicians; American College of Physicians; American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-493.