User login
Chronic pain is more prevalent in the US than diabetes mellitus, cancer, and cardiovascular disease combined, impacting about 100 million adults.1 The annual cost of all that pain in the US is between $560 and $635 billion.1
The high prevalence of chronic pain among active duty service members and veterans remains a pressing concern given its negative impact on military readiness, health care utilization, productivity, quality of life, and chronic disability rates.2 Pain was found to be the leading complaint of service members returning from Operations Iraqi Freedom and Enduring Freedomand 44% of veterans returning from deployment suffered with chronic pain.3,4
Chronic pain often occurs in the presence of comorbidities. In one study for example, 45% of primary care patients with chronic pain (N = 250) screened positive for ≥ 1 of the 5 types of common anxiety disorders, and those with anxiety disorder had higher pain scores.5 Another study involving almost 6000 participants found that anxiety disorders were present in 35% of people with chronic pain compared with 18% in the general population.6
In addition, military members are prone to depression with a rate of major depressive disorder that is 5% higher than that of civilians.7 Depression often is underdiagnosed and undertreated. According to a National Center for Health Statistics, only 35% of those with symptoms of severe depression in the US saw a mental health provider in the previous year.8 Comorbid depression, anxiety, and chronic pain are strongly associated with more severe pain, greater disability, and poorer health-related quality of life.9
As a result, there was a call for system-level interventions to increase access to, and continuity of, mental health care services for active duty service members and veterans.1 It has been recommended that depression and anxiety screenings take place in primary and secondary care clinics.10 Standardized referral processes also are needed to enhance mental health diagnosis and referral techniques.11 Although various screening tools are available that have excellent reliability and construct validity (eg, General Anxiety Disorder-7 [GAD-7], Patient Health Questionnaire-9 [PHQ-9]), they are underutilized.12 I have witnessed a noticeable gap between clinical practice guidelines and current practice associated with chronic pain and screening for anxiety and depression within the Pain Management Clinic at Navy Medical Center of Camp Lejeune (NMCCL) in North Carolina.
Methods
The premise of this performance improvement (PI) project was to reduce missed opportunities of screening for anxiety and depression, and to examine the impact of the standardized use of the GAD-7 and PHQ-9 on the rate of mental health care referrals. The Theory of Unpleasant Symptoms was chosen as the underpinning of the project because it suggests that symptoms often cluster, and that the occurrence of multiple symptoms makes each of those, as well as other symptoms, worse.13 The PI model used the find, organize, clarify, understand, select (FOCUS), and plan, do, check, act (PDCA) models.14 The facility institutional review board ruled that this performance improvement project did not qualify as human research.
Inclusion and exclusion criteria
Patients were included if they were active duty service members aged 18 to 56 years at the initial patient encounter. Veterans and dependents were not part of the sample because of the high clinic volume. Patients who received mental health care services within the previous 90 days were excluded.
Registered nurses, licensed practical nurses, US Navy corpsman, medical assistants, and nurse aides were educated on the purpose of the GAD-7 and PHQ-9 and were instructed to have patients complete them upon every new patient encounter. A retrospective chart review was conducted over a 6-week time frame to collect and analyze de-identified demographic data including age, gender, prior deployment (yes or no), and branch of service. The review also examined whether the patient had received mental health care services, whether the screening instruments were completed, and whether a mental health referral was made. The clinic providers were asked to consider mental health care referrals for patients who scored ≥ 10 on either the GAD-7 or PHQ-9. The frequency of the use of the instruments and the number of mental health referrals made was calculated during the 3-week period before and after the standardized use of the instruments. The author conducted audits of the new patient charts at the end of each work day to assess whether the GAD-7 and PHQ-9 were completed.
Results
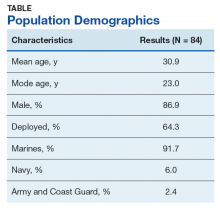
There were 117 new patient encounters during the 6-week project period. Thirty-three patients were excluded from the sample, leaving a remaining sample of 84. Thirty-two patients were included in the sample prior to the standardized use of the instruments, and 52 were included afterward (Table).
Prior to the standardized use of the screening tools, the GAD-7 was used during 75% of patient visits for pain and the PHQ-9 was used during 25%, reinforcing the premise of unpredictable utilization of the screening tools. Three mental health referrals were made during the 3-week period prior to the standardized use of the anxiety and depression instruments (3/32, 10%). After the standardized implementation of the GAD-7 and PHQ-9 tools, both instruments were used 98% of the time, and mental health referrals were made for 12 of 52 patients (23.1%). Eleven of the referrals were made based upon the trigger score of 10 on either the GAD-7 or PHQ-9. One referral was made for a patient with a score of 9 on the PHQ-9 because the provider determined a need for pain-related psychological services.
It was important to provide a link to mental health care because, as one study found, patients with a specific anxiety diagnosis are much more likely than those diagnosed with a not otherwise specified anxiety disorder to receive mental health care services (60% to 67% vs 37%).11 Similarly, patients diagnosed in specialty mental health care settings are more likely to receive mental health services than are those diagnosed in primary care.11 By the same token, experts estimate that 50% of those with severe depression symptoms are not properly diagnosed or treated in primary care.15
Strengths and Limitations
Utilization of the screening tools has led to further dialogue between patients and providers that anecdotally revealed suicidal ideation in some patients. Future studies could incorporate a qualitative component to include clinician and patient perceptions of mental health care services.
The study was limited by the lack of follow-up data to determine the effect of mental health care services on pain, function, or military readiness. Also, it is unclear whether education alone impacted the referral rate.
The author shared the outcomes of this PI project with fellow professionals at NMCCL. As a team, we explored ways for military to link with mental health care within their commands. The process of using these instruments is easily transferable to other clinics with no extraordinary cost.
Conclusion
The economic burden of major depressive disorder in the US has risen 21.5% from 2005 to 2010.16 Unfortunately, only 35% of those with symptoms of severe depression had contact with a mental health professional in the past year.8 Avoiding missing opportunities to screen for mental health conditions can decrease the disease burden. The GAD-7 and PHQ-9 are relatively cost free and are deemed reliable and valid for screening for, and determining the severity of, symptoms of anxiety and depression.12 The evidence suggests that screening for, and early recognition of, mental illness, are critical parts of evidence-based practice and provide the most cost-effective care.16
This PI project demonstrated that the standardized use of the GAD-7 and PHQ-9 during patient visits for pain did improve adherence to guidelines and resulted in a significant increase in the rate of mental health referrals from 10% to 23.1%. This information is valuable because a score of ≥ 10 on either screening instrument is considered the optimal cutoff for diagnosing and determining severity of anxiety and depression symptoms.12 The US Department of Veterans Affairs (VA) and the US Department of Defense (DoD) have jointly developed clinical practice guidelines, which recommend that interventions, such as behavioral therapies or first-line pharmacologic treatment, be offered to patients with mild to moderate symptoms of depression.17 The VA/DoD guidelines for low back pain suggest screening for mental health disorders.2 For these reasons, the standardized use of the screening instruments remains in place within the pain management clinic at NMCCL.
1. Board on Health Sciences Policy. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. The National Academies Press: Washington, DC; 2011.
2. US Department of Defense, US Department of Veterans Affairs. VA/DoD clinical practice guidelines for diagnosis and treatment of low back pain. https://www.healthquality.va.gov/guidelines/Pain/lbp/VADoDLBPCPG092917.pdf. Published October 21, 2016. Accessed September 26, 2019.
3. Gironda RJ, Clark ME, Massengale JP, Walker RL. Pain among veterans of Operations Enduring Freedom and Iraqi Freedom. Pain Med. 2006;7(4):339-343.
4. Arlotta CJ. New recommendations for pain management among active duty service military and veterans. Forbes. February 13, 2015. https://www.forbes.com/sites/cjarlotta/2015/02/13/managing-chronic-pain-in-the-active-military-and-veteran-populations/#7d7dd7d93fc3. Accessed September 26, 2019.
5. Kroenke K, Outcalt S, Krebs E, et al. Association between anxiety, health-related quality of life and functional impairment in primry care patients with chronic pain. Gen Hosp Psychiatry. 2013;35(4):359-365.
6. McWilliams LA, Cox BJ, Enns MW. Mood and anxiety disorders associated with chronic pain: an examination in a nationally representative sample. Pain. 2003;106(1-2):127-133.
7. Lazar SG. The mental health needs of active duty service members and veterans. Psychodynamic Psychiatry. 2014;42(3):459-478.
8. Pratt LA, Brody DJ. Depression in the U.S. household population, 2009-2012. NCHS Data Brief No. 172. https://www.cdc.gov/nchs/data/databriefs/db172.pdf. Published December 2014. Accessed September 26, 2019.
9. Bair MJ, Wu J, Damush TM, Sutherland JM, Kroenke K. Association of depression and anxiety alone and in combination with chronic musculoskeletal pain in primary care patients. Psychosom Med. 2008;70(8):890-897.
10. National Institute for Clinical Health and Care Excellence. Common mental health problems: identification and pathways to care. https://www.nice.org.uk/guidance/CG123/chapter/1-Guidance#step-1-identification-and-assessment. Published May 2011. Accessed September 26, 2019.
11. Barrera TL, Mott JM, Hundt NE, et al. Diagnostic specificity and mental health service utilization among veterans with newly diagnosed anxiety disorders. Gen Hosp Psychiatry. 2014;36(2):192-198.
12. Kroenke K, Spitzer RL, Williams JBW, Lowe B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345-359.
13. Smith MJ, Liehr PR. The Theory of Unpleasant Symptoms. Middle Range Theory for Nursing. New York, NY: Springer Publishing Company, 2014:165-195.
14. Substance Abuse and Mental Health Services Administration, Health Resources and Services Administration. FOCUS PDCA: plan-do-check-act. https://www.integration.samhsa.gov/pbhci-learning-community/Cross-site_TA_slides_-_FOCUSPDCA_Final.pdf. Published September 19, 2017. Accessed September 26, 2019.
15. Bridges KW, Goldberg DP. Somatic presentation of DSM III psychiatric disorders in primary care. J Psychosom Res. 1985;29(6):563-569.
16. Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. 2015;76(2):155-162.
17. US Department of Defense, US Department of Veterans Affairs. VA/DoD clinical practice guidelines. Management of major depressive disorder (MDD) https://www.healthquality.va.gov/guidelines/MH/mdd/. Updated October 12, 2017. Accessed September 26, 2019.
Chronic pain is more prevalent in the US than diabetes mellitus, cancer, and cardiovascular disease combined, impacting about 100 million adults.1 The annual cost of all that pain in the US is between $560 and $635 billion.1
The high prevalence of chronic pain among active duty service members and veterans remains a pressing concern given its negative impact on military readiness, health care utilization, productivity, quality of life, and chronic disability rates.2 Pain was found to be the leading complaint of service members returning from Operations Iraqi Freedom and Enduring Freedomand 44% of veterans returning from deployment suffered with chronic pain.3,4
Chronic pain often occurs in the presence of comorbidities. In one study for example, 45% of primary care patients with chronic pain (N = 250) screened positive for ≥ 1 of the 5 types of common anxiety disorders, and those with anxiety disorder had higher pain scores.5 Another study involving almost 6000 participants found that anxiety disorders were present in 35% of people with chronic pain compared with 18% in the general population.6
In addition, military members are prone to depression with a rate of major depressive disorder that is 5% higher than that of civilians.7 Depression often is underdiagnosed and undertreated. According to a National Center for Health Statistics, only 35% of those with symptoms of severe depression in the US saw a mental health provider in the previous year.8 Comorbid depression, anxiety, and chronic pain are strongly associated with more severe pain, greater disability, and poorer health-related quality of life.9
As a result, there was a call for system-level interventions to increase access to, and continuity of, mental health care services for active duty service members and veterans.1 It has been recommended that depression and anxiety screenings take place in primary and secondary care clinics.10 Standardized referral processes also are needed to enhance mental health diagnosis and referral techniques.11 Although various screening tools are available that have excellent reliability and construct validity (eg, General Anxiety Disorder-7 [GAD-7], Patient Health Questionnaire-9 [PHQ-9]), they are underutilized.12 I have witnessed a noticeable gap between clinical practice guidelines and current practice associated with chronic pain and screening for anxiety and depression within the Pain Management Clinic at Navy Medical Center of Camp Lejeune (NMCCL) in North Carolina.
Methods
The premise of this performance improvement (PI) project was to reduce missed opportunities of screening for anxiety and depression, and to examine the impact of the standardized use of the GAD-7 and PHQ-9 on the rate of mental health care referrals. The Theory of Unpleasant Symptoms was chosen as the underpinning of the project because it suggests that symptoms often cluster, and that the occurrence of multiple symptoms makes each of those, as well as other symptoms, worse.13 The PI model used the find, organize, clarify, understand, select (FOCUS), and plan, do, check, act (PDCA) models.14 The facility institutional review board ruled that this performance improvement project did not qualify as human research.
Inclusion and exclusion criteria
Patients were included if they were active duty service members aged 18 to 56 years at the initial patient encounter. Veterans and dependents were not part of the sample because of the high clinic volume. Patients who received mental health care services within the previous 90 days were excluded.
Registered nurses, licensed practical nurses, US Navy corpsman, medical assistants, and nurse aides were educated on the purpose of the GAD-7 and PHQ-9 and were instructed to have patients complete them upon every new patient encounter. A retrospective chart review was conducted over a 6-week time frame to collect and analyze de-identified demographic data including age, gender, prior deployment (yes or no), and branch of service. The review also examined whether the patient had received mental health care services, whether the screening instruments were completed, and whether a mental health referral was made. The clinic providers were asked to consider mental health care referrals for patients who scored ≥ 10 on either the GAD-7 or PHQ-9. The frequency of the use of the instruments and the number of mental health referrals made was calculated during the 3-week period before and after the standardized use of the instruments. The author conducted audits of the new patient charts at the end of each work day to assess whether the GAD-7 and PHQ-9 were completed.
Results
There were 117 new patient encounters during the 6-week project period. Thirty-three patients were excluded from the sample, leaving a remaining sample of 84. Thirty-two patients were included in the sample prior to the standardized use of the instruments, and 52 were included afterward (Table).
Prior to the standardized use of the screening tools, the GAD-7 was used during 75% of patient visits for pain and the PHQ-9 was used during 25%, reinforcing the premise of unpredictable utilization of the screening tools. Three mental health referrals were made during the 3-week period prior to the standardized use of the anxiety and depression instruments (3/32, 10%). After the standardized implementation of the GAD-7 and PHQ-9 tools, both instruments were used 98% of the time, and mental health referrals were made for 12 of 52 patients (23.1%). Eleven of the referrals were made based upon the trigger score of 10 on either the GAD-7 or PHQ-9. One referral was made for a patient with a score of 9 on the PHQ-9 because the provider determined a need for pain-related psychological services.
It was important to provide a link to mental health care because, as one study found, patients with a specific anxiety diagnosis are much more likely than those diagnosed with a not otherwise specified anxiety disorder to receive mental health care services (60% to 67% vs 37%).11 Similarly, patients diagnosed in specialty mental health care settings are more likely to receive mental health services than are those diagnosed in primary care.11 By the same token, experts estimate that 50% of those with severe depression symptoms are not properly diagnosed or treated in primary care.15
Strengths and Limitations
Utilization of the screening tools has led to further dialogue between patients and providers that anecdotally revealed suicidal ideation in some patients. Future studies could incorporate a qualitative component to include clinician and patient perceptions of mental health care services.
The study was limited by the lack of follow-up data to determine the effect of mental health care services on pain, function, or military readiness. Also, it is unclear whether education alone impacted the referral rate.
The author shared the outcomes of this PI project with fellow professionals at NMCCL. As a team, we explored ways for military to link with mental health care within their commands. The process of using these instruments is easily transferable to other clinics with no extraordinary cost.
Conclusion
The economic burden of major depressive disorder in the US has risen 21.5% from 2005 to 2010.16 Unfortunately, only 35% of those with symptoms of severe depression had contact with a mental health professional in the past year.8 Avoiding missing opportunities to screen for mental health conditions can decrease the disease burden. The GAD-7 and PHQ-9 are relatively cost free and are deemed reliable and valid for screening for, and determining the severity of, symptoms of anxiety and depression.12 The evidence suggests that screening for, and early recognition of, mental illness, are critical parts of evidence-based practice and provide the most cost-effective care.16
This PI project demonstrated that the standardized use of the GAD-7 and PHQ-9 during patient visits for pain did improve adherence to guidelines and resulted in a significant increase in the rate of mental health referrals from 10% to 23.1%. This information is valuable because a score of ≥ 10 on either screening instrument is considered the optimal cutoff for diagnosing and determining severity of anxiety and depression symptoms.12 The US Department of Veterans Affairs (VA) and the US Department of Defense (DoD) have jointly developed clinical practice guidelines, which recommend that interventions, such as behavioral therapies or first-line pharmacologic treatment, be offered to patients with mild to moderate symptoms of depression.17 The VA/DoD guidelines for low back pain suggest screening for mental health disorders.2 For these reasons, the standardized use of the screening instruments remains in place within the pain management clinic at NMCCL.
Chronic pain is more prevalent in the US than diabetes mellitus, cancer, and cardiovascular disease combined, impacting about 100 million adults.1 The annual cost of all that pain in the US is between $560 and $635 billion.1
The high prevalence of chronic pain among active duty service members and veterans remains a pressing concern given its negative impact on military readiness, health care utilization, productivity, quality of life, and chronic disability rates.2 Pain was found to be the leading complaint of service members returning from Operations Iraqi Freedom and Enduring Freedomand 44% of veterans returning from deployment suffered with chronic pain.3,4
Chronic pain often occurs in the presence of comorbidities. In one study for example, 45% of primary care patients with chronic pain (N = 250) screened positive for ≥ 1 of the 5 types of common anxiety disorders, and those with anxiety disorder had higher pain scores.5 Another study involving almost 6000 participants found that anxiety disorders were present in 35% of people with chronic pain compared with 18% in the general population.6
In addition, military members are prone to depression with a rate of major depressive disorder that is 5% higher than that of civilians.7 Depression often is underdiagnosed and undertreated. According to a National Center for Health Statistics, only 35% of those with symptoms of severe depression in the US saw a mental health provider in the previous year.8 Comorbid depression, anxiety, and chronic pain are strongly associated with more severe pain, greater disability, and poorer health-related quality of life.9
As a result, there was a call for system-level interventions to increase access to, and continuity of, mental health care services for active duty service members and veterans.1 It has been recommended that depression and anxiety screenings take place in primary and secondary care clinics.10 Standardized referral processes also are needed to enhance mental health diagnosis and referral techniques.11 Although various screening tools are available that have excellent reliability and construct validity (eg, General Anxiety Disorder-7 [GAD-7], Patient Health Questionnaire-9 [PHQ-9]), they are underutilized.12 I have witnessed a noticeable gap between clinical practice guidelines and current practice associated with chronic pain and screening for anxiety and depression within the Pain Management Clinic at Navy Medical Center of Camp Lejeune (NMCCL) in North Carolina.
Methods
The premise of this performance improvement (PI) project was to reduce missed opportunities of screening for anxiety and depression, and to examine the impact of the standardized use of the GAD-7 and PHQ-9 on the rate of mental health care referrals. The Theory of Unpleasant Symptoms was chosen as the underpinning of the project because it suggests that symptoms often cluster, and that the occurrence of multiple symptoms makes each of those, as well as other symptoms, worse.13 The PI model used the find, organize, clarify, understand, select (FOCUS), and plan, do, check, act (PDCA) models.14 The facility institutional review board ruled that this performance improvement project did not qualify as human research.
Inclusion and exclusion criteria
Patients were included if they were active duty service members aged 18 to 56 years at the initial patient encounter. Veterans and dependents were not part of the sample because of the high clinic volume. Patients who received mental health care services within the previous 90 days were excluded.
Registered nurses, licensed practical nurses, US Navy corpsman, medical assistants, and nurse aides were educated on the purpose of the GAD-7 and PHQ-9 and were instructed to have patients complete them upon every new patient encounter. A retrospective chart review was conducted over a 6-week time frame to collect and analyze de-identified demographic data including age, gender, prior deployment (yes or no), and branch of service. The review also examined whether the patient had received mental health care services, whether the screening instruments were completed, and whether a mental health referral was made. The clinic providers were asked to consider mental health care referrals for patients who scored ≥ 10 on either the GAD-7 or PHQ-9. The frequency of the use of the instruments and the number of mental health referrals made was calculated during the 3-week period before and after the standardized use of the instruments. The author conducted audits of the new patient charts at the end of each work day to assess whether the GAD-7 and PHQ-9 were completed.
Results
There were 117 new patient encounters during the 6-week project period. Thirty-three patients were excluded from the sample, leaving a remaining sample of 84. Thirty-two patients were included in the sample prior to the standardized use of the instruments, and 52 were included afterward (Table).
Prior to the standardized use of the screening tools, the GAD-7 was used during 75% of patient visits for pain and the PHQ-9 was used during 25%, reinforcing the premise of unpredictable utilization of the screening tools. Three mental health referrals were made during the 3-week period prior to the standardized use of the anxiety and depression instruments (3/32, 10%). After the standardized implementation of the GAD-7 and PHQ-9 tools, both instruments were used 98% of the time, and mental health referrals were made for 12 of 52 patients (23.1%). Eleven of the referrals were made based upon the trigger score of 10 on either the GAD-7 or PHQ-9. One referral was made for a patient with a score of 9 on the PHQ-9 because the provider determined a need for pain-related psychological services.
It was important to provide a link to mental health care because, as one study found, patients with a specific anxiety diagnosis are much more likely than those diagnosed with a not otherwise specified anxiety disorder to receive mental health care services (60% to 67% vs 37%).11 Similarly, patients diagnosed in specialty mental health care settings are more likely to receive mental health services than are those diagnosed in primary care.11 By the same token, experts estimate that 50% of those with severe depression symptoms are not properly diagnosed or treated in primary care.15
Strengths and Limitations
Utilization of the screening tools has led to further dialogue between patients and providers that anecdotally revealed suicidal ideation in some patients. Future studies could incorporate a qualitative component to include clinician and patient perceptions of mental health care services.
The study was limited by the lack of follow-up data to determine the effect of mental health care services on pain, function, or military readiness. Also, it is unclear whether education alone impacted the referral rate.
The author shared the outcomes of this PI project with fellow professionals at NMCCL. As a team, we explored ways for military to link with mental health care within their commands. The process of using these instruments is easily transferable to other clinics with no extraordinary cost.
Conclusion
The economic burden of major depressive disorder in the US has risen 21.5% from 2005 to 2010.16 Unfortunately, only 35% of those with symptoms of severe depression had contact with a mental health professional in the past year.8 Avoiding missing opportunities to screen for mental health conditions can decrease the disease burden. The GAD-7 and PHQ-9 are relatively cost free and are deemed reliable and valid for screening for, and determining the severity of, symptoms of anxiety and depression.12 The evidence suggests that screening for, and early recognition of, mental illness, are critical parts of evidence-based practice and provide the most cost-effective care.16
This PI project demonstrated that the standardized use of the GAD-7 and PHQ-9 during patient visits for pain did improve adherence to guidelines and resulted in a significant increase in the rate of mental health referrals from 10% to 23.1%. This information is valuable because a score of ≥ 10 on either screening instrument is considered the optimal cutoff for diagnosing and determining severity of anxiety and depression symptoms.12 The US Department of Veterans Affairs (VA) and the US Department of Defense (DoD) have jointly developed clinical practice guidelines, which recommend that interventions, such as behavioral therapies or first-line pharmacologic treatment, be offered to patients with mild to moderate symptoms of depression.17 The VA/DoD guidelines for low back pain suggest screening for mental health disorders.2 For these reasons, the standardized use of the screening instruments remains in place within the pain management clinic at NMCCL.
1. Board on Health Sciences Policy. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. The National Academies Press: Washington, DC; 2011.
2. US Department of Defense, US Department of Veterans Affairs. VA/DoD clinical practice guidelines for diagnosis and treatment of low back pain. https://www.healthquality.va.gov/guidelines/Pain/lbp/VADoDLBPCPG092917.pdf. Published October 21, 2016. Accessed September 26, 2019.
3. Gironda RJ, Clark ME, Massengale JP, Walker RL. Pain among veterans of Operations Enduring Freedom and Iraqi Freedom. Pain Med. 2006;7(4):339-343.
4. Arlotta CJ. New recommendations for pain management among active duty service military and veterans. Forbes. February 13, 2015. https://www.forbes.com/sites/cjarlotta/2015/02/13/managing-chronic-pain-in-the-active-military-and-veteran-populations/#7d7dd7d93fc3. Accessed September 26, 2019.
5. Kroenke K, Outcalt S, Krebs E, et al. Association between anxiety, health-related quality of life and functional impairment in primry care patients with chronic pain. Gen Hosp Psychiatry. 2013;35(4):359-365.
6. McWilliams LA, Cox BJ, Enns MW. Mood and anxiety disorders associated with chronic pain: an examination in a nationally representative sample. Pain. 2003;106(1-2):127-133.
7. Lazar SG. The mental health needs of active duty service members and veterans. Psychodynamic Psychiatry. 2014;42(3):459-478.
8. Pratt LA, Brody DJ. Depression in the U.S. household population, 2009-2012. NCHS Data Brief No. 172. https://www.cdc.gov/nchs/data/databriefs/db172.pdf. Published December 2014. Accessed September 26, 2019.
9. Bair MJ, Wu J, Damush TM, Sutherland JM, Kroenke K. Association of depression and anxiety alone and in combination with chronic musculoskeletal pain in primary care patients. Psychosom Med. 2008;70(8):890-897.
10. National Institute for Clinical Health and Care Excellence. Common mental health problems: identification and pathways to care. https://www.nice.org.uk/guidance/CG123/chapter/1-Guidance#step-1-identification-and-assessment. Published May 2011. Accessed September 26, 2019.
11. Barrera TL, Mott JM, Hundt NE, et al. Diagnostic specificity and mental health service utilization among veterans with newly diagnosed anxiety disorders. Gen Hosp Psychiatry. 2014;36(2):192-198.
12. Kroenke K, Spitzer RL, Williams JBW, Lowe B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345-359.
13. Smith MJ, Liehr PR. The Theory of Unpleasant Symptoms. Middle Range Theory for Nursing. New York, NY: Springer Publishing Company, 2014:165-195.
14. Substance Abuse and Mental Health Services Administration, Health Resources and Services Administration. FOCUS PDCA: plan-do-check-act. https://www.integration.samhsa.gov/pbhci-learning-community/Cross-site_TA_slides_-_FOCUSPDCA_Final.pdf. Published September 19, 2017. Accessed September 26, 2019.
15. Bridges KW, Goldberg DP. Somatic presentation of DSM III psychiatric disorders in primary care. J Psychosom Res. 1985;29(6):563-569.
16. Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. 2015;76(2):155-162.
17. US Department of Defense, US Department of Veterans Affairs. VA/DoD clinical practice guidelines. Management of major depressive disorder (MDD) https://www.healthquality.va.gov/guidelines/MH/mdd/. Updated October 12, 2017. Accessed September 26, 2019.
1. Board on Health Sciences Policy. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. The National Academies Press: Washington, DC; 2011.
2. US Department of Defense, US Department of Veterans Affairs. VA/DoD clinical practice guidelines for diagnosis and treatment of low back pain. https://www.healthquality.va.gov/guidelines/Pain/lbp/VADoDLBPCPG092917.pdf. Published October 21, 2016. Accessed September 26, 2019.
3. Gironda RJ, Clark ME, Massengale JP, Walker RL. Pain among veterans of Operations Enduring Freedom and Iraqi Freedom. Pain Med. 2006;7(4):339-343.
4. Arlotta CJ. New recommendations for pain management among active duty service military and veterans. Forbes. February 13, 2015. https://www.forbes.com/sites/cjarlotta/2015/02/13/managing-chronic-pain-in-the-active-military-and-veteran-populations/#7d7dd7d93fc3. Accessed September 26, 2019.
5. Kroenke K, Outcalt S, Krebs E, et al. Association between anxiety, health-related quality of life and functional impairment in primry care patients with chronic pain. Gen Hosp Psychiatry. 2013;35(4):359-365.
6. McWilliams LA, Cox BJ, Enns MW. Mood and anxiety disorders associated with chronic pain: an examination in a nationally representative sample. Pain. 2003;106(1-2):127-133.
7. Lazar SG. The mental health needs of active duty service members and veterans. Psychodynamic Psychiatry. 2014;42(3):459-478.
8. Pratt LA, Brody DJ. Depression in the U.S. household population, 2009-2012. NCHS Data Brief No. 172. https://www.cdc.gov/nchs/data/databriefs/db172.pdf. Published December 2014. Accessed September 26, 2019.
9. Bair MJ, Wu J, Damush TM, Sutherland JM, Kroenke K. Association of depression and anxiety alone and in combination with chronic musculoskeletal pain in primary care patients. Psychosom Med. 2008;70(8):890-897.
10. National Institute for Clinical Health and Care Excellence. Common mental health problems: identification and pathways to care. https://www.nice.org.uk/guidance/CG123/chapter/1-Guidance#step-1-identification-and-assessment. Published May 2011. Accessed September 26, 2019.
11. Barrera TL, Mott JM, Hundt NE, et al. Diagnostic specificity and mental health service utilization among veterans with newly diagnosed anxiety disorders. Gen Hosp Psychiatry. 2014;36(2):192-198.
12. Kroenke K, Spitzer RL, Williams JBW, Lowe B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345-359.
13. Smith MJ, Liehr PR. The Theory of Unpleasant Symptoms. Middle Range Theory for Nursing. New York, NY: Springer Publishing Company, 2014:165-195.
14. Substance Abuse and Mental Health Services Administration, Health Resources and Services Administration. FOCUS PDCA: plan-do-check-act. https://www.integration.samhsa.gov/pbhci-learning-community/Cross-site_TA_slides_-_FOCUSPDCA_Final.pdf. Published September 19, 2017. Accessed September 26, 2019.
15. Bridges KW, Goldberg DP. Somatic presentation of DSM III psychiatric disorders in primary care. J Psychosom Res. 1985;29(6):563-569.
16. Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. 2015;76(2):155-162.
17. US Department of Defense, US Department of Veterans Affairs. VA/DoD clinical practice guidelines. Management of major depressive disorder (MDD) https://www.healthquality.va.gov/guidelines/MH/mdd/. Updated October 12, 2017. Accessed September 26, 2019.