User login
Patients who arrive in the emergency department (ED) following a cerebrovascular event—stroke or transient ischemic attack—present a number of challenges to the hospitalist. In addition to the varied clinical presentations characteristic of stroke itself, many patients with stroke exhibit a number of cardiovascular risk factors, as well as one or more comorbidities (such as diabetes mellitus). In addition, these patients may be receiving multiple medications.
The risk factors for ischemic stroke are broadly consistent with those for other forms of atherothrombotic cardiovascular disease. Strong evidence from recent observational and interventional studies indicates, however, that patients who experience a stroke or an acute myocardial infarction are likely to experience a recurrent event of the same type.1,2 Therefore, it is appropriate for the clinician to select preventive therapy specifically directed at stroke prevention.
The prevention of secondary stroke is an element of acute care, but it straddles the boundaries among acute care, rehabilitation, and primary care. It is, therefore, an arena that fully engages the skills of the hospitalist. Goals of the hospital physician include the following:
- Minimize the risks of medical complications;
- Ensure an effective continuum of care, with smooth transitions among ED treatment, inpatient care, and long-term management in the community setting; and
- Maintain/improve the quality and consistency of care vis-à-vis adherence to established guidelines for secondary stroke prevention.
Assessment and Risk Evaluation
Initial assessment of patients with suspected stroke or transient ischemic attack seeks to eliminate other possible causes of current or recent neurologic deficit and to confirm the basic nature of the event (ischemic or hemorrhagic). Evidence-based guidelines from the American Stroke Association should be followed in the diagnosis and assessment of these patients in the ED.3
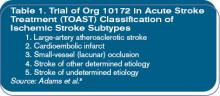
The sophistication of risk evaluation for primary and secondary stroke generally lags behind the evaluation used for cardiac events—a disparity noted by a number of stroke researchers who have called for more extensive epidemiologic studies in support of an adequate risk assessment structure.4-7 The use of the Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification structure for ischemic stroke has provided a better footing for such studies; a similar framework is used to guide treatment pathways for secondary prevention8 (See Table 1, p. 33.)
Recent studies generally support hypertension, cigarette smoking, and atrial fibrillation as strong risk factors for first ischemic stroke; however, few studies have been devoted specifically to analysis of secondary stroke risk factors.5,9 One recent study demonstrated that levels of C-reactive protein are strongly predictive of second events after stroke, with the risk in the highest quintile of C-reactive protein (>1.41 mg/mL) more than eight-fold greater than that in the lowest quintile (£0.12 mg/mL).10
Manage Risk Factors
Several of the risk factors for primary and secondary stroke, including advancing age, male gender, and black and Hispanic racial/ethnic background, are important prognostic determinants. Other important risk factors that are modifiable, at least in theory, include hypertension, smoking, dyslipidemia, obesity, excessive alcohol use, physical inactivity, and impaired glucose tolerance.11
In addition to assessing and managing physical parameters, the clinician should review the patient’s history with regard to contact with the healthcare system. Consider the quality of the patient’s relationship with a primary care provider in light of post-stroke outpatient management. If no such provider exists—or if other concerns are expressed—it may be necessary to help the patient and/or the family in this regard. If evidence reveals that the patient has had problems with medication compliance or regular follow-up, it may be necessary to provide counseling and other support to the patient and family.
Treatment Decision Making
Approach treatment decisions following stroke or transient ischemic attack in a collaborative, multidisciplinary fashion. The hospitalist should facilitate appropriate consultation and evaluation—not only by neurologists and the medical stroke team but also by physical and/or occupational therapists, speech pathologists, and nutritionists/dieticians as needed. Clarify the roles of the hospital physician, especially in managing the patient through the care continuum systematically, as well as in relation to a specific patient.
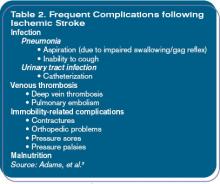
Patients with stroke are susceptible to a range of potential complications during hospitalization and beyond—many of which are exacerbated by neurological damage and motor impairment. (See Table 2, p. 34.) These complications are significant contributors to poststroke morbidity and mortality; pulmonary embolism alone accounts for 10% of deaths after stroke, and sepsis secondary to urinary tract infection develops in about 5% of patients with stroke.3
Treatment Approaches
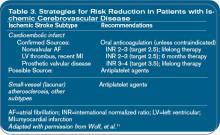
The general approach to secondary stroke prevention should be based on the type of primary stroke that has occurred and should be refined according to specific stroke features and the findings obtained through additional diagnostic workup. (See Table 3, p. 36.)
The nonpharmacologic approach of managing lifestyle-related factors, such as quitting smoking, curbing alcohol consumption, and increasing physical exercise, remains an important element of preventive therapy; patients and their support teams should be encouraged to take an active role in making recommended changes.
As can be seen in Table 3, prevention of secondary events following stroke resulting from a confirmed cardioembolic source is based on anticoagulant (warfarin) therapy. For strokes resulting from carotid atherosclerosis, surgical repair (carotid endarterectomy) is of demonstrated benefit in patients with at least 70% stenosis and should be considered in patients with stenosis greater than 50%. Surgical complication rates can, however, negate any advantage of endarterectomy.11,12
The cornerstone of medical therapy for preventing recurrence after any noncardioembolic ischemic stroke is treatment with antiplatelet (platelet antiaggregation) agents, including aspirin, the thienopyridine derivative clopidogrel, or a combination of aspirin and extended-release dipyridamole.
Studies of aspirin generally suggest that low daily doses provide efficacy comparable or equivalent to that of higher doses, along with a reduced risk for serious adverse events. An example is the Dutch Transient Ischemic Attack (TIA) Trial Study, which randomly assigned 3,131 patients who had experienced a recent stroke or transient ischemic attack to dosages of 30 mg/day or 283 mg/day of aspirin. After a mean follow-up period of 2.6 years, no significant between-group differences were noted with regard to the incidence of the composite outcome measure of vascular death, nonfatal stroke, or nonfatal acute myocardial infarction (14.7% and 15.2%, respectively). However, 24% fewer major bleeding complications and 41% fewer minor bleeding complications were reported with the low dose compared with the higher dose.13
Similarly, the United Kingdom TIA study randomly assigned 2,435 patients with recent transient ischemic attack or minor ischemic stroke to placebo or to aspirin at 1,200 mg/day or 300 mg/day. After a mean follow-up of four years, the aspirin groups were virtually identical with regard to the composite vascular death, nonfatal stroke, or nonfatal acute myocardial infarction endpoint; relative risk reduction for combined aspirin groups versus placebo was 15%. The 1,200 mg/day aspirin group, however, reported a higher rate of upper gastrointestinal symptoms and bleeding episodes.14
Additional support for the efficacy of low-dose aspirin was provided by the Swedish Aspirin Low-Dose Trial (SALT), which randomly assigned 1,360 patients to 75 mg/day of aspirin or a placebo. In aspirin-treated subjects, an 18% reduction versus placebo was observed in the primary endpoint of stroke or death (P=0.02). In addition, aspirin reduced the incidence of a composite secondary outcome (stroke, or two or more transient ischemic attacks within a week, necessitating a change in therapy) by 20% versus placebo (P=0.03).15
The first evaluation of clopidogrel after stroke or transient ischemic attack was the Clopidogrel versus Aspirin in Patients at Risk of Recurrent Ischaemic Events (CAPRIE) study. A total of 19,185 patients with recent stroke/transient ischemic attack, recent myocardial infarction, or peripheral arterial disease were randomly assigned to receive aspirin at 325 mg/day or clopidogrel at 75mg/day; 6,431 patients were in the cerebrovascular disease (stroke/transient ischemic attack) cohort. At follow-up (mean: 1.91 years), a statistically significant benefit was seen for clopidogrel over aspirin in the composite endpoint of ischemic stroke, acute myocardial infarction, or vascular death among all patients (annual incidence rates for composite outcome: clopidogrel, 5.32%; aspirin, 5.83%; absolute risk reduction 0.51%; relative risk reduction 8.7%; P=0.043). The CAPRIE cohort data does show that much of the difference favoring clopidogrel over aspirin was derived from the peripheral artery disease group (relative risk reduction 3.8%; P=0.0028). In the stroke/transient ischemic attack cohort, comparative risk reduction for the composite endpoint was reduced and not statistically significant (relative risk reduction 7.3%; P=0.26).16
The Management of Atherosclerosis with Clopidogrel in High-Risk Patients (MATCH) study was an evaluation of clopidogrel versus clopidogrel plus aspirin in the prevention of secondary stroke. Seven thousand five hundred ninety-nine patients with a history of stroke or transient ischemic attack and other vascular risk factors were randomly assigned to clopidogrel alone or clopidogrel plus aspirin. After a mean follow-up of 18 months, the clopidogrel plus aspirin combination group demonstrated only an insignificant benefit in the composite outcome of rehospitalization for an ischemic event, ischemic stroke, acute myocardial infarction, or vascular death (clopidogrel plus aspirin 15.70%; clopidogrel monotherapy 16.73%; relative risk reduction 6.4%; P=0.244).13 In addition, the clopidogrel plus aspirin combination produced an increased absolute incidence of life-threatening bleeding episodes versus clopidogrel alone (2.6% versus 1.3%) that was greater than the absolute reduction in efficacy outcome events. Therefore, the combination of clopidogrel plus aspirin is not recommended for secondary event prevention after stroke or transient ischemic attack.17,18
In the recently reported Clopidogrel for High Risk and Ischemic Stabilization, Management, and Avoidance (CHARISMA) study, patients with documented coronary disease, cerebrovascular disease, or peripheral artery disease were administered either clopidogrel (75 mg/day) plus aspirin (75–162 mg/day) or aspirin alone.19 The study also included patients with multiple atherosclerotic risk factors but without documented arterial disease.
There was no significant difference between treatment arms regarding the primary composite endpoint of myocardial infarction, stroke, or cardiovascular death. Prespecified subgroup analyses showed a 1% absolute decrease in the incidence of the primary endpoint in patients with documented vascular disease (P=0.046) and an increase of 1.1% in the asymptomatic patients with multiple vascular risk factors (P=0.20) among those patients randomized to combination therapy. Severe bleeding (defined as fatal bleeding, intracranial hemorrhage, or bleeding causing hemodynamic compromise) occurred in 1.7% of patients in the combination therapy arm and 1.3% in the aspirin arm (P=0.09). Moderate bleeding, defined as that necessitating transfusion but not meeting the criteria for severe bleeding, occurred in 2.1% of patients in the combination therapy arm and 1.3% in the aspirin arm (P<0.001). The investigators concluded that clopidogrel plus aspirin provided no significant advantage over aspirin alone in reducing incidence of the primary combined endpoint.
Extended-release dipyridamole in combination with aspirin was evaluated in the European Stroke Prevention Study-2 (ESPS-2). The combination was compared with aspirin alone and with dipyridamole alone, as well as with placebo, in 6,602 patients with a history of stroke or transient ischemic attack. Extended-release dipyridamole and aspirin monotherapy showed similar efficacy in reducing the risk of stroke (relative risk reduction versus placebo: aspirin 18%, P=0.013; extended-release dipyridamole 16%, P=0.039). The extended-release dipyridamole plus aspirin combination, however, showed evidence of additive benefit; the relative risk reduction for stroke with extended-release dipyridamole plus aspirin was 23% versus aspirin alone (P=0.006) and 25% versus extended-release dipyridamole alone (P=0.002). Compared with placebo, the extended-release dipyridamole plus aspirin combination was associated with relative risk reductions of 37% (P<0.001) for stroke and 24% (P<0.001) for stroke or death. This combination reduced the relative risk of stroke over aspirin alone by 23%.20
Despite the apparent additive benefit derived from extended-release dipyridamole plus aspirin, no evidence was found for an increase in adverse outcomes. Adverse gastrointestinal events in the combination therapy group were comparable with those noted with aspirin monotherapy, with an increased incidence of headache.20
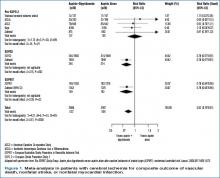
As in ESPS-2, the European/Australian Stroke Prevention in Reversible Ischemia Trial (ESPRIT) investigated the combination of aspirin and dipyridamole (principally extended-release dipyridamole). Using a primary combined endpoint of vascular death, nonfatal stroke, nonfatal myocardial infarction, and major bleeding complications, ESPRIT confirmed aspirin plus dipyridamole to be superior to aspirin monotherapy in reducing these complications.21 An overall risk ratio of 0.82 for the composite endpoint (P=0.0003) was determined in a meta-analysis of the trials comparing aspirin alone to aspirin plus dipyridamole.21 (See Figure 1, p. 39.)
An in-progress prospective secondary stroke prevention study, the Prospective Regimen for Effectively Avoiding Second Strokes (PRoFESS) study, which consists of 15,500 patients with a recent history of ischemic stroke, will provide the first head-to-head comparison of clopidogrel monotherapy with the extended-release dipyridamole plus aspirin combination. The two antiplatelet regimens will be evaluated through a 2 x 2 design in the presence and in the absence of the antihypertensive telmisartan, with results expected in 2007. PRoFESS findings should help to clarify the comparative efficacy of clopidogrel versus extended-release dipyridamole plus aspirin with regard to the primary endpoint (time to first stroke recurrence) and a vascular events composite endpoint.
Antiplatelet Treatment Guidelines
The American Academy of Neurology guidelines recommend the use of aspirin within 48 hours of stroke symptom onset (except when tissue plasminogen activator treatment has been used or is anticipated) to reduce mortality and prevent early stroke recurrence.22 A more extensive set of evidence-based guidelines for antiplatelet and antithrombotic use following ischemic stroke, including recommendations for secondary event prevention, was developed in 2004 by the American College of Chest Physicians (ACCP).23 The primary recommendation (Grade 1A) is to provide treatment with an antiplatelet agent (i.e., aspirin at 50 to 325 mg/day, extended-release dipyridamole at 200 mg plus aspirin at 25 mg twice daily, or clopidogrel at 75 mg/day) following noncardioembolic stroke. The ACCP has also suggested that extended-release dipyridamole plus aspirin (Grade 2A) or clopidogrel (Grade 2B) may be preferable to aspirin monotherapy. This suggestion does include the caveat that this “places a relatively high value on a small absolute risk reduction in stroke rates, and a relatively low value on minimizing drug expenditures.”23
Discharge Planning
When the post-stroke patient is prepared for discharge, place the highest priority on ensuring an effective continuum of care. Comprehensively review all medications, including those prescribed for prevention of secondary events, with the patient and family or caregivers. Explain the purpose of each medication, along with the consequences of poor compliance or discontinuation; reinforce the need for lifelong therapy for stroke prevention and amelioration of stroke risk factors at every opportunity.
A key step in establishing the continuum of care is to gain buy-in from the primary care provider for continuing medical therapy and follow-up. If appropriate, cite current guidelines from the American Academy of Neurology, the American College of Chest Physicians, and the American Stroke Association. Occupational or physical therapy, if indicated, should be planned before discharge and coordinated with the primary care provider for continued follow-up. This evaluation may also result in a recommendation for inpatient rehabilitation or, in the interim, a skilled nursing facility placement.
Given the improvement that many patients realize over the short term, staged discharge to a skilled nursing facility may be followed after a short interval by a stay at an inpatient rehabilitation facility. Coordination of this staged approach must be carefully implemented, as it is easy for this to fall through the cracks during transitions of care.
Conclusion: Stroke Centers and Systems of Care
Managing patients with stroke is in many ways an ideal fit for the hospitalist model. From symptom onset, the patient with stroke challenges traditional approaches to care in multiple ways: variable presentation involving multiple neurologic symptoms, frequent systemic comorbidities and risk factors, highly variable disease course and sequelae, and the need for active and coordinated management throughout the continuum of care. The hospital physician should seek to improve the value of care by ensuring and facilitating consistent management according to established guidelines and by managing the transitions between phases of treatment.
SHM provides numerous valuable tools to the hospital physician for use in improving the care of patients with stroke, including diagnostic and assessment instruments and guidelines, algorithms and pathways for management of patients with stroke, sample standing orders from leading institutions, and resources that can be provided to patients and their families. All are available or downloadable from the SHM Web site, at www.hospitalmedicine.org/AM/Template.cfm?Section=Quality_Improvement_Resource_ Rooms&Template=/ CM/HTMLDisplay.cfm&ContentID=6566. Even (or perhaps especially) in the absence of higher-level systems dedicated to the care of patients with stroke, the hospital physician can serve as a critical linchpin in the optimization of patient outcomes following stroke. TH
Dr. Likosky is executive director, Evergreen Neuroscience Institute, Kirkland, Wash., as well as a hospitalist and neurohospitalist.
References
- Gebel JM Jr. Secondary stroke prevention with antiplatelet therapy with emphasis on the cardiac patient: a neurologist’s view. J Am Coll Cardiol. 2005 Sep 6;46(5):752-755.
- Vickrey BG, Rector TS, Wickstrom SL, et al. Occurrence of secondary ischemic events among persons with atherosclerotic vascular disease. Stroke. 2002 Apr;33(4):901-906.
- Adams HP Jr, Adams RJ, Brott T, et al. Guidelines for the early management of patients with ischemic stroke: A scientific statement from the Stroke Council of the American Stroke Association. Stroke. 2003 Apr;34(4):1056-1083.
- Leira EC, Chang KC, Davis PH, et al. Can we predict early recurrence in acute stroke? Cerebrovasc Dis. 2004;18(2):139-144.
- Pinto A, Tuttolomondo A, Di Raimondo D, et al. Cerebrovascular risk factors and clinical classification of strokes. Semin Vasc Med. 2004 Aug;4(3):287-303.
- Rothwell PM. Incidence, risk factors and prognosis of stroke and TIA: the need for high-quality, large-scale epidemiological studies and meta-analyses. Cerebrovasc Dis. 2003;16(Suppl 3):2-10.
- Schulz UG, Rothwell PM. Differences in vascular risk factors between etiological subtypes of ischemic stroke: importance of population-based studies. Stroke. 2003 Aug;34(8):2050-2059; Epub 2003 Jun 26.
- Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993 Jan;24(1):35-41.
- Sacco RL, Benjamin EJ, Broderick JP, et al. American Heart Association Prevention Conference. IV. Prevention and rehabilitation of stroke. Risk factors. Stroke. 1997;28:1507-1517.
- Arenillas JF, Alvarez-Sabin J, Molina CA, et al. C-reactive protein predicts further ischemic events in first-ever transient ischemic attack or stroke patients with intracranial large-artery occlusive disease. Stroke. 2003 Oct;34(10):2463-2468.
- Wolf PA, Clagett GP, Easton JD, et al. Preventing ischemic stroke in patients with prior stroke and transient ischemic attack: a statement for healthcare professionals from the Stroke Council of the American Heart Association. Stroke. 1999;30:1991-1994.
- Chaturvedi S, Bruno A, Feasby T, et al. Carotid endarterectomy—an evidence-based review: report of the Therapeutics and Technology Assessment Sub-committee of the American Academy of Neurology. Neurology. 2005 Sep 27;65(6):794-801.
- The Dutch TIA Trial Study Group. A comparison of two doses of aspirin (30 mg vs. 283 mg a day) in patients after a transient ischemic attack or minor ischemic stroke. N Engl J Med. 1991;325:1261-1266.
- Farrell B, Godwin J, Richards S, et al. The United Kingdom transient ischaemic attack (UK-TIA) aspirin trial: final results. J Neurol Neurosurg Psychiatry. 1991 Dec;54(12):1044-1054.
- The SALT Collaborative Group. Swedish Aspirin Low-Dose Trial (SALT) of 75 mg aspirin as secondary prophylaxis after cerebrovascular ischaemic events. Lancet. 1991 Nov 30;338(8779):1345-1349.
- CAPRIE Steering Committee. A randomised, blinded trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet. 1996 Nov 16;348(9038):1329-1339.
- Diener HC, Bogousslavsky J, Brass LM, et al. Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial. Lancet. 2004;364:331-337.
- Hankey GJ, Eikelboom JW. Adding aspirin to clopidogrel after TIA and ischemic stroke: benefits do not match risks. Neurology. 2005 Apr 12;64(7):1117-1121.
- Bhatt DL, Fox KA, Hacke W, et al; CHARISMA Investigators. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med. 2006 Apr 20;354(16):1706-1717.
- Diener HC, Cunha L, Forbes C, et al. European Stroke Prevention Study. 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci. 1996 Nov;143(1-2):1-13.
- Halkes PH, van Gijn J, Kappelle LJ, et al. (ESPRIT Study Group). Aspirin plus dipyridamole versus aspirin alone after cerebral ischaemia of arterial origin (ESPRIT): randomised controlled trial. Lancet. 2006 May 20;367(9523):1665-1673.
- Coull BM, Williams LS, Goldstein LB, et al. Anticoagulants and antiplatelet agents in acute ischemic stroke: report of the Joint Stroke Guideline Development Committee of the American Academy of Neurology and the American Stroke Association (a division of the American Heart Association). Neurology. 2002 Jul 9;59(1):13-22.
- Albers GW, Amarenco P, Easton JD, et al. Antithrombotic and thrombolytic therapy for ischemic stroke: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004 Sep;126(3 Suppl):483S-512S.
Patients who arrive in the emergency department (ED) following a cerebrovascular event—stroke or transient ischemic attack—present a number of challenges to the hospitalist. In addition to the varied clinical presentations characteristic of stroke itself, many patients with stroke exhibit a number of cardiovascular risk factors, as well as one or more comorbidities (such as diabetes mellitus). In addition, these patients may be receiving multiple medications.
The risk factors for ischemic stroke are broadly consistent with those for other forms of atherothrombotic cardiovascular disease. Strong evidence from recent observational and interventional studies indicates, however, that patients who experience a stroke or an acute myocardial infarction are likely to experience a recurrent event of the same type.1,2 Therefore, it is appropriate for the clinician to select preventive therapy specifically directed at stroke prevention.
The prevention of secondary stroke is an element of acute care, but it straddles the boundaries among acute care, rehabilitation, and primary care. It is, therefore, an arena that fully engages the skills of the hospitalist. Goals of the hospital physician include the following:
- Minimize the risks of medical complications;
- Ensure an effective continuum of care, with smooth transitions among ED treatment, inpatient care, and long-term management in the community setting; and
- Maintain/improve the quality and consistency of care vis-à-vis adherence to established guidelines for secondary stroke prevention.
Assessment and Risk Evaluation
Initial assessment of patients with suspected stroke or transient ischemic attack seeks to eliminate other possible causes of current or recent neurologic deficit and to confirm the basic nature of the event (ischemic or hemorrhagic). Evidence-based guidelines from the American Stroke Association should be followed in the diagnosis and assessment of these patients in the ED.3
The sophistication of risk evaluation for primary and secondary stroke generally lags behind the evaluation used for cardiac events—a disparity noted by a number of stroke researchers who have called for more extensive epidemiologic studies in support of an adequate risk assessment structure.4-7 The use of the Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification structure for ischemic stroke has provided a better footing for such studies; a similar framework is used to guide treatment pathways for secondary prevention8 (See Table 1, p. 33.)
Recent studies generally support hypertension, cigarette smoking, and atrial fibrillation as strong risk factors for first ischemic stroke; however, few studies have been devoted specifically to analysis of secondary stroke risk factors.5,9 One recent study demonstrated that levels of C-reactive protein are strongly predictive of second events after stroke, with the risk in the highest quintile of C-reactive protein (>1.41 mg/mL) more than eight-fold greater than that in the lowest quintile (£0.12 mg/mL).10
Manage Risk Factors
Several of the risk factors for primary and secondary stroke, including advancing age, male gender, and black and Hispanic racial/ethnic background, are important prognostic determinants. Other important risk factors that are modifiable, at least in theory, include hypertension, smoking, dyslipidemia, obesity, excessive alcohol use, physical inactivity, and impaired glucose tolerance.11
In addition to assessing and managing physical parameters, the clinician should review the patient’s history with regard to contact with the healthcare system. Consider the quality of the patient’s relationship with a primary care provider in light of post-stroke outpatient management. If no such provider exists—or if other concerns are expressed—it may be necessary to help the patient and/or the family in this regard. If evidence reveals that the patient has had problems with medication compliance or regular follow-up, it may be necessary to provide counseling and other support to the patient and family.
Treatment Decision Making
Approach treatment decisions following stroke or transient ischemic attack in a collaborative, multidisciplinary fashion. The hospitalist should facilitate appropriate consultation and evaluation—not only by neurologists and the medical stroke team but also by physical and/or occupational therapists, speech pathologists, and nutritionists/dieticians as needed. Clarify the roles of the hospital physician, especially in managing the patient through the care continuum systematically, as well as in relation to a specific patient.
Patients with stroke are susceptible to a range of potential complications during hospitalization and beyond—many of which are exacerbated by neurological damage and motor impairment. (See Table 2, p. 34.) These complications are significant contributors to poststroke morbidity and mortality; pulmonary embolism alone accounts for 10% of deaths after stroke, and sepsis secondary to urinary tract infection develops in about 5% of patients with stroke.3
Treatment Approaches
The general approach to secondary stroke prevention should be based on the type of primary stroke that has occurred and should be refined according to specific stroke features and the findings obtained through additional diagnostic workup. (See Table 3, p. 36.)
The nonpharmacologic approach of managing lifestyle-related factors, such as quitting smoking, curbing alcohol consumption, and increasing physical exercise, remains an important element of preventive therapy; patients and their support teams should be encouraged to take an active role in making recommended changes.
As can be seen in Table 3, prevention of secondary events following stroke resulting from a confirmed cardioembolic source is based on anticoagulant (warfarin) therapy. For strokes resulting from carotid atherosclerosis, surgical repair (carotid endarterectomy) is of demonstrated benefit in patients with at least 70% stenosis and should be considered in patients with stenosis greater than 50%. Surgical complication rates can, however, negate any advantage of endarterectomy.11,12
The cornerstone of medical therapy for preventing recurrence after any noncardioembolic ischemic stroke is treatment with antiplatelet (platelet antiaggregation) agents, including aspirin, the thienopyridine derivative clopidogrel, or a combination of aspirin and extended-release dipyridamole.
Studies of aspirin generally suggest that low daily doses provide efficacy comparable or equivalent to that of higher doses, along with a reduced risk for serious adverse events. An example is the Dutch Transient Ischemic Attack (TIA) Trial Study, which randomly assigned 3,131 patients who had experienced a recent stroke or transient ischemic attack to dosages of 30 mg/day or 283 mg/day of aspirin. After a mean follow-up period of 2.6 years, no significant between-group differences were noted with regard to the incidence of the composite outcome measure of vascular death, nonfatal stroke, or nonfatal acute myocardial infarction (14.7% and 15.2%, respectively). However, 24% fewer major bleeding complications and 41% fewer minor bleeding complications were reported with the low dose compared with the higher dose.13
Similarly, the United Kingdom TIA study randomly assigned 2,435 patients with recent transient ischemic attack or minor ischemic stroke to placebo or to aspirin at 1,200 mg/day or 300 mg/day. After a mean follow-up of four years, the aspirin groups were virtually identical with regard to the composite vascular death, nonfatal stroke, or nonfatal acute myocardial infarction endpoint; relative risk reduction for combined aspirin groups versus placebo was 15%. The 1,200 mg/day aspirin group, however, reported a higher rate of upper gastrointestinal symptoms and bleeding episodes.14
Additional support for the efficacy of low-dose aspirin was provided by the Swedish Aspirin Low-Dose Trial (SALT), which randomly assigned 1,360 patients to 75 mg/day of aspirin or a placebo. In aspirin-treated subjects, an 18% reduction versus placebo was observed in the primary endpoint of stroke or death (P=0.02). In addition, aspirin reduced the incidence of a composite secondary outcome (stroke, or two or more transient ischemic attacks within a week, necessitating a change in therapy) by 20% versus placebo (P=0.03).15
The first evaluation of clopidogrel after stroke or transient ischemic attack was the Clopidogrel versus Aspirin in Patients at Risk of Recurrent Ischaemic Events (CAPRIE) study. A total of 19,185 patients with recent stroke/transient ischemic attack, recent myocardial infarction, or peripheral arterial disease were randomly assigned to receive aspirin at 325 mg/day or clopidogrel at 75mg/day; 6,431 patients were in the cerebrovascular disease (stroke/transient ischemic attack) cohort. At follow-up (mean: 1.91 years), a statistically significant benefit was seen for clopidogrel over aspirin in the composite endpoint of ischemic stroke, acute myocardial infarction, or vascular death among all patients (annual incidence rates for composite outcome: clopidogrel, 5.32%; aspirin, 5.83%; absolute risk reduction 0.51%; relative risk reduction 8.7%; P=0.043). The CAPRIE cohort data does show that much of the difference favoring clopidogrel over aspirin was derived from the peripheral artery disease group (relative risk reduction 3.8%; P=0.0028). In the stroke/transient ischemic attack cohort, comparative risk reduction for the composite endpoint was reduced and not statistically significant (relative risk reduction 7.3%; P=0.26).16
The Management of Atherosclerosis with Clopidogrel in High-Risk Patients (MATCH) study was an evaluation of clopidogrel versus clopidogrel plus aspirin in the prevention of secondary stroke. Seven thousand five hundred ninety-nine patients with a history of stroke or transient ischemic attack and other vascular risk factors were randomly assigned to clopidogrel alone or clopidogrel plus aspirin. After a mean follow-up of 18 months, the clopidogrel plus aspirin combination group demonstrated only an insignificant benefit in the composite outcome of rehospitalization for an ischemic event, ischemic stroke, acute myocardial infarction, or vascular death (clopidogrel plus aspirin 15.70%; clopidogrel monotherapy 16.73%; relative risk reduction 6.4%; P=0.244).13 In addition, the clopidogrel plus aspirin combination produced an increased absolute incidence of life-threatening bleeding episodes versus clopidogrel alone (2.6% versus 1.3%) that was greater than the absolute reduction in efficacy outcome events. Therefore, the combination of clopidogrel plus aspirin is not recommended for secondary event prevention after stroke or transient ischemic attack.17,18
In the recently reported Clopidogrel for High Risk and Ischemic Stabilization, Management, and Avoidance (CHARISMA) study, patients with documented coronary disease, cerebrovascular disease, or peripheral artery disease were administered either clopidogrel (75 mg/day) plus aspirin (75–162 mg/day) or aspirin alone.19 The study also included patients with multiple atherosclerotic risk factors but without documented arterial disease.
There was no significant difference between treatment arms regarding the primary composite endpoint of myocardial infarction, stroke, or cardiovascular death. Prespecified subgroup analyses showed a 1% absolute decrease in the incidence of the primary endpoint in patients with documented vascular disease (P=0.046) and an increase of 1.1% in the asymptomatic patients with multiple vascular risk factors (P=0.20) among those patients randomized to combination therapy. Severe bleeding (defined as fatal bleeding, intracranial hemorrhage, or bleeding causing hemodynamic compromise) occurred in 1.7% of patients in the combination therapy arm and 1.3% in the aspirin arm (P=0.09). Moderate bleeding, defined as that necessitating transfusion but not meeting the criteria for severe bleeding, occurred in 2.1% of patients in the combination therapy arm and 1.3% in the aspirin arm (P<0.001). The investigators concluded that clopidogrel plus aspirin provided no significant advantage over aspirin alone in reducing incidence of the primary combined endpoint.
Extended-release dipyridamole in combination with aspirin was evaluated in the European Stroke Prevention Study-2 (ESPS-2). The combination was compared with aspirin alone and with dipyridamole alone, as well as with placebo, in 6,602 patients with a history of stroke or transient ischemic attack. Extended-release dipyridamole and aspirin monotherapy showed similar efficacy in reducing the risk of stroke (relative risk reduction versus placebo: aspirin 18%, P=0.013; extended-release dipyridamole 16%, P=0.039). The extended-release dipyridamole plus aspirin combination, however, showed evidence of additive benefit; the relative risk reduction for stroke with extended-release dipyridamole plus aspirin was 23% versus aspirin alone (P=0.006) and 25% versus extended-release dipyridamole alone (P=0.002). Compared with placebo, the extended-release dipyridamole plus aspirin combination was associated with relative risk reductions of 37% (P<0.001) for stroke and 24% (P<0.001) for stroke or death. This combination reduced the relative risk of stroke over aspirin alone by 23%.20
Despite the apparent additive benefit derived from extended-release dipyridamole plus aspirin, no evidence was found for an increase in adverse outcomes. Adverse gastrointestinal events in the combination therapy group were comparable with those noted with aspirin monotherapy, with an increased incidence of headache.20
As in ESPS-2, the European/Australian Stroke Prevention in Reversible Ischemia Trial (ESPRIT) investigated the combination of aspirin and dipyridamole (principally extended-release dipyridamole). Using a primary combined endpoint of vascular death, nonfatal stroke, nonfatal myocardial infarction, and major bleeding complications, ESPRIT confirmed aspirin plus dipyridamole to be superior to aspirin monotherapy in reducing these complications.21 An overall risk ratio of 0.82 for the composite endpoint (P=0.0003) was determined in a meta-analysis of the trials comparing aspirin alone to aspirin plus dipyridamole.21 (See Figure 1, p. 39.)
An in-progress prospective secondary stroke prevention study, the Prospective Regimen for Effectively Avoiding Second Strokes (PRoFESS) study, which consists of 15,500 patients with a recent history of ischemic stroke, will provide the first head-to-head comparison of clopidogrel monotherapy with the extended-release dipyridamole plus aspirin combination. The two antiplatelet regimens will be evaluated through a 2 x 2 design in the presence and in the absence of the antihypertensive telmisartan, with results expected in 2007. PRoFESS findings should help to clarify the comparative efficacy of clopidogrel versus extended-release dipyridamole plus aspirin with regard to the primary endpoint (time to first stroke recurrence) and a vascular events composite endpoint.
Antiplatelet Treatment Guidelines
The American Academy of Neurology guidelines recommend the use of aspirin within 48 hours of stroke symptom onset (except when tissue plasminogen activator treatment has been used or is anticipated) to reduce mortality and prevent early stroke recurrence.22 A more extensive set of evidence-based guidelines for antiplatelet and antithrombotic use following ischemic stroke, including recommendations for secondary event prevention, was developed in 2004 by the American College of Chest Physicians (ACCP).23 The primary recommendation (Grade 1A) is to provide treatment with an antiplatelet agent (i.e., aspirin at 50 to 325 mg/day, extended-release dipyridamole at 200 mg plus aspirin at 25 mg twice daily, or clopidogrel at 75 mg/day) following noncardioembolic stroke. The ACCP has also suggested that extended-release dipyridamole plus aspirin (Grade 2A) or clopidogrel (Grade 2B) may be preferable to aspirin monotherapy. This suggestion does include the caveat that this “places a relatively high value on a small absolute risk reduction in stroke rates, and a relatively low value on minimizing drug expenditures.”23
Discharge Planning
When the post-stroke patient is prepared for discharge, place the highest priority on ensuring an effective continuum of care. Comprehensively review all medications, including those prescribed for prevention of secondary events, with the patient and family or caregivers. Explain the purpose of each medication, along with the consequences of poor compliance or discontinuation; reinforce the need for lifelong therapy for stroke prevention and amelioration of stroke risk factors at every opportunity.
A key step in establishing the continuum of care is to gain buy-in from the primary care provider for continuing medical therapy and follow-up. If appropriate, cite current guidelines from the American Academy of Neurology, the American College of Chest Physicians, and the American Stroke Association. Occupational or physical therapy, if indicated, should be planned before discharge and coordinated with the primary care provider for continued follow-up. This evaluation may also result in a recommendation for inpatient rehabilitation or, in the interim, a skilled nursing facility placement.
Given the improvement that many patients realize over the short term, staged discharge to a skilled nursing facility may be followed after a short interval by a stay at an inpatient rehabilitation facility. Coordination of this staged approach must be carefully implemented, as it is easy for this to fall through the cracks during transitions of care.
Conclusion: Stroke Centers and Systems of Care
Managing patients with stroke is in many ways an ideal fit for the hospitalist model. From symptom onset, the patient with stroke challenges traditional approaches to care in multiple ways: variable presentation involving multiple neurologic symptoms, frequent systemic comorbidities and risk factors, highly variable disease course and sequelae, and the need for active and coordinated management throughout the continuum of care. The hospital physician should seek to improve the value of care by ensuring and facilitating consistent management according to established guidelines and by managing the transitions between phases of treatment.
SHM provides numerous valuable tools to the hospital physician for use in improving the care of patients with stroke, including diagnostic and assessment instruments and guidelines, algorithms and pathways for management of patients with stroke, sample standing orders from leading institutions, and resources that can be provided to patients and their families. All are available or downloadable from the SHM Web site, at www.hospitalmedicine.org/AM/Template.cfm?Section=Quality_Improvement_Resource_ Rooms&Template=/ CM/HTMLDisplay.cfm&ContentID=6566. Even (or perhaps especially) in the absence of higher-level systems dedicated to the care of patients with stroke, the hospital physician can serve as a critical linchpin in the optimization of patient outcomes following stroke. TH
Dr. Likosky is executive director, Evergreen Neuroscience Institute, Kirkland, Wash., as well as a hospitalist and neurohospitalist.
References
- Gebel JM Jr. Secondary stroke prevention with antiplatelet therapy with emphasis on the cardiac patient: a neurologist’s view. J Am Coll Cardiol. 2005 Sep 6;46(5):752-755.
- Vickrey BG, Rector TS, Wickstrom SL, et al. Occurrence of secondary ischemic events among persons with atherosclerotic vascular disease. Stroke. 2002 Apr;33(4):901-906.
- Adams HP Jr, Adams RJ, Brott T, et al. Guidelines for the early management of patients with ischemic stroke: A scientific statement from the Stroke Council of the American Stroke Association. Stroke. 2003 Apr;34(4):1056-1083.
- Leira EC, Chang KC, Davis PH, et al. Can we predict early recurrence in acute stroke? Cerebrovasc Dis. 2004;18(2):139-144.
- Pinto A, Tuttolomondo A, Di Raimondo D, et al. Cerebrovascular risk factors and clinical classification of strokes. Semin Vasc Med. 2004 Aug;4(3):287-303.
- Rothwell PM. Incidence, risk factors and prognosis of stroke and TIA: the need for high-quality, large-scale epidemiological studies and meta-analyses. Cerebrovasc Dis. 2003;16(Suppl 3):2-10.
- Schulz UG, Rothwell PM. Differences in vascular risk factors between etiological subtypes of ischemic stroke: importance of population-based studies. Stroke. 2003 Aug;34(8):2050-2059; Epub 2003 Jun 26.
- Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993 Jan;24(1):35-41.
- Sacco RL, Benjamin EJ, Broderick JP, et al. American Heart Association Prevention Conference. IV. Prevention and rehabilitation of stroke. Risk factors. Stroke. 1997;28:1507-1517.
- Arenillas JF, Alvarez-Sabin J, Molina CA, et al. C-reactive protein predicts further ischemic events in first-ever transient ischemic attack or stroke patients with intracranial large-artery occlusive disease. Stroke. 2003 Oct;34(10):2463-2468.
- Wolf PA, Clagett GP, Easton JD, et al. Preventing ischemic stroke in patients with prior stroke and transient ischemic attack: a statement for healthcare professionals from the Stroke Council of the American Heart Association. Stroke. 1999;30:1991-1994.
- Chaturvedi S, Bruno A, Feasby T, et al. Carotid endarterectomy—an evidence-based review: report of the Therapeutics and Technology Assessment Sub-committee of the American Academy of Neurology. Neurology. 2005 Sep 27;65(6):794-801.
- The Dutch TIA Trial Study Group. A comparison of two doses of aspirin (30 mg vs. 283 mg a day) in patients after a transient ischemic attack or minor ischemic stroke. N Engl J Med. 1991;325:1261-1266.
- Farrell B, Godwin J, Richards S, et al. The United Kingdom transient ischaemic attack (UK-TIA) aspirin trial: final results. J Neurol Neurosurg Psychiatry. 1991 Dec;54(12):1044-1054.
- The SALT Collaborative Group. Swedish Aspirin Low-Dose Trial (SALT) of 75 mg aspirin as secondary prophylaxis after cerebrovascular ischaemic events. Lancet. 1991 Nov 30;338(8779):1345-1349.
- CAPRIE Steering Committee. A randomised, blinded trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet. 1996 Nov 16;348(9038):1329-1339.
- Diener HC, Bogousslavsky J, Brass LM, et al. Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial. Lancet. 2004;364:331-337.
- Hankey GJ, Eikelboom JW. Adding aspirin to clopidogrel after TIA and ischemic stroke: benefits do not match risks. Neurology. 2005 Apr 12;64(7):1117-1121.
- Bhatt DL, Fox KA, Hacke W, et al; CHARISMA Investigators. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med. 2006 Apr 20;354(16):1706-1717.
- Diener HC, Cunha L, Forbes C, et al. European Stroke Prevention Study. 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci. 1996 Nov;143(1-2):1-13.
- Halkes PH, van Gijn J, Kappelle LJ, et al. (ESPRIT Study Group). Aspirin plus dipyridamole versus aspirin alone after cerebral ischaemia of arterial origin (ESPRIT): randomised controlled trial. Lancet. 2006 May 20;367(9523):1665-1673.
- Coull BM, Williams LS, Goldstein LB, et al. Anticoagulants and antiplatelet agents in acute ischemic stroke: report of the Joint Stroke Guideline Development Committee of the American Academy of Neurology and the American Stroke Association (a division of the American Heart Association). Neurology. 2002 Jul 9;59(1):13-22.
- Albers GW, Amarenco P, Easton JD, et al. Antithrombotic and thrombolytic therapy for ischemic stroke: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004 Sep;126(3 Suppl):483S-512S.
Patients who arrive in the emergency department (ED) following a cerebrovascular event—stroke or transient ischemic attack—present a number of challenges to the hospitalist. In addition to the varied clinical presentations characteristic of stroke itself, many patients with stroke exhibit a number of cardiovascular risk factors, as well as one or more comorbidities (such as diabetes mellitus). In addition, these patients may be receiving multiple medications.
The risk factors for ischemic stroke are broadly consistent with those for other forms of atherothrombotic cardiovascular disease. Strong evidence from recent observational and interventional studies indicates, however, that patients who experience a stroke or an acute myocardial infarction are likely to experience a recurrent event of the same type.1,2 Therefore, it is appropriate for the clinician to select preventive therapy specifically directed at stroke prevention.
The prevention of secondary stroke is an element of acute care, but it straddles the boundaries among acute care, rehabilitation, and primary care. It is, therefore, an arena that fully engages the skills of the hospitalist. Goals of the hospital physician include the following:
- Minimize the risks of medical complications;
- Ensure an effective continuum of care, with smooth transitions among ED treatment, inpatient care, and long-term management in the community setting; and
- Maintain/improve the quality and consistency of care vis-à-vis adherence to established guidelines for secondary stroke prevention.
Assessment and Risk Evaluation
Initial assessment of patients with suspected stroke or transient ischemic attack seeks to eliminate other possible causes of current or recent neurologic deficit and to confirm the basic nature of the event (ischemic or hemorrhagic). Evidence-based guidelines from the American Stroke Association should be followed in the diagnosis and assessment of these patients in the ED.3
The sophistication of risk evaluation for primary and secondary stroke generally lags behind the evaluation used for cardiac events—a disparity noted by a number of stroke researchers who have called for more extensive epidemiologic studies in support of an adequate risk assessment structure.4-7 The use of the Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification structure for ischemic stroke has provided a better footing for such studies; a similar framework is used to guide treatment pathways for secondary prevention8 (See Table 1, p. 33.)
Recent studies generally support hypertension, cigarette smoking, and atrial fibrillation as strong risk factors for first ischemic stroke; however, few studies have been devoted specifically to analysis of secondary stroke risk factors.5,9 One recent study demonstrated that levels of C-reactive protein are strongly predictive of second events after stroke, with the risk in the highest quintile of C-reactive protein (>1.41 mg/mL) more than eight-fold greater than that in the lowest quintile (£0.12 mg/mL).10
Manage Risk Factors
Several of the risk factors for primary and secondary stroke, including advancing age, male gender, and black and Hispanic racial/ethnic background, are important prognostic determinants. Other important risk factors that are modifiable, at least in theory, include hypertension, smoking, dyslipidemia, obesity, excessive alcohol use, physical inactivity, and impaired glucose tolerance.11
In addition to assessing and managing physical parameters, the clinician should review the patient’s history with regard to contact with the healthcare system. Consider the quality of the patient’s relationship with a primary care provider in light of post-stroke outpatient management. If no such provider exists—or if other concerns are expressed—it may be necessary to help the patient and/or the family in this regard. If evidence reveals that the patient has had problems with medication compliance or regular follow-up, it may be necessary to provide counseling and other support to the patient and family.
Treatment Decision Making
Approach treatment decisions following stroke or transient ischemic attack in a collaborative, multidisciplinary fashion. The hospitalist should facilitate appropriate consultation and evaluation—not only by neurologists and the medical stroke team but also by physical and/or occupational therapists, speech pathologists, and nutritionists/dieticians as needed. Clarify the roles of the hospital physician, especially in managing the patient through the care continuum systematically, as well as in relation to a specific patient.
Patients with stroke are susceptible to a range of potential complications during hospitalization and beyond—many of which are exacerbated by neurological damage and motor impairment. (See Table 2, p. 34.) These complications are significant contributors to poststroke morbidity and mortality; pulmonary embolism alone accounts for 10% of deaths after stroke, and sepsis secondary to urinary tract infection develops in about 5% of patients with stroke.3
Treatment Approaches
The general approach to secondary stroke prevention should be based on the type of primary stroke that has occurred and should be refined according to specific stroke features and the findings obtained through additional diagnostic workup. (See Table 3, p. 36.)
The nonpharmacologic approach of managing lifestyle-related factors, such as quitting smoking, curbing alcohol consumption, and increasing physical exercise, remains an important element of preventive therapy; patients and their support teams should be encouraged to take an active role in making recommended changes.
As can be seen in Table 3, prevention of secondary events following stroke resulting from a confirmed cardioembolic source is based on anticoagulant (warfarin) therapy. For strokes resulting from carotid atherosclerosis, surgical repair (carotid endarterectomy) is of demonstrated benefit in patients with at least 70% stenosis and should be considered in patients with stenosis greater than 50%. Surgical complication rates can, however, negate any advantage of endarterectomy.11,12
The cornerstone of medical therapy for preventing recurrence after any noncardioembolic ischemic stroke is treatment with antiplatelet (platelet antiaggregation) agents, including aspirin, the thienopyridine derivative clopidogrel, or a combination of aspirin and extended-release dipyridamole.
Studies of aspirin generally suggest that low daily doses provide efficacy comparable or equivalent to that of higher doses, along with a reduced risk for serious adverse events. An example is the Dutch Transient Ischemic Attack (TIA) Trial Study, which randomly assigned 3,131 patients who had experienced a recent stroke or transient ischemic attack to dosages of 30 mg/day or 283 mg/day of aspirin. After a mean follow-up period of 2.6 years, no significant between-group differences were noted with regard to the incidence of the composite outcome measure of vascular death, nonfatal stroke, or nonfatal acute myocardial infarction (14.7% and 15.2%, respectively). However, 24% fewer major bleeding complications and 41% fewer minor bleeding complications were reported with the low dose compared with the higher dose.13
Similarly, the United Kingdom TIA study randomly assigned 2,435 patients with recent transient ischemic attack or minor ischemic stroke to placebo or to aspirin at 1,200 mg/day or 300 mg/day. After a mean follow-up of four years, the aspirin groups were virtually identical with regard to the composite vascular death, nonfatal stroke, or nonfatal acute myocardial infarction endpoint; relative risk reduction for combined aspirin groups versus placebo was 15%. The 1,200 mg/day aspirin group, however, reported a higher rate of upper gastrointestinal symptoms and bleeding episodes.14
Additional support for the efficacy of low-dose aspirin was provided by the Swedish Aspirin Low-Dose Trial (SALT), which randomly assigned 1,360 patients to 75 mg/day of aspirin or a placebo. In aspirin-treated subjects, an 18% reduction versus placebo was observed in the primary endpoint of stroke or death (P=0.02). In addition, aspirin reduced the incidence of a composite secondary outcome (stroke, or two or more transient ischemic attacks within a week, necessitating a change in therapy) by 20% versus placebo (P=0.03).15
The first evaluation of clopidogrel after stroke or transient ischemic attack was the Clopidogrel versus Aspirin in Patients at Risk of Recurrent Ischaemic Events (CAPRIE) study. A total of 19,185 patients with recent stroke/transient ischemic attack, recent myocardial infarction, or peripheral arterial disease were randomly assigned to receive aspirin at 325 mg/day or clopidogrel at 75mg/day; 6,431 patients were in the cerebrovascular disease (stroke/transient ischemic attack) cohort. At follow-up (mean: 1.91 years), a statistically significant benefit was seen for clopidogrel over aspirin in the composite endpoint of ischemic stroke, acute myocardial infarction, or vascular death among all patients (annual incidence rates for composite outcome: clopidogrel, 5.32%; aspirin, 5.83%; absolute risk reduction 0.51%; relative risk reduction 8.7%; P=0.043). The CAPRIE cohort data does show that much of the difference favoring clopidogrel over aspirin was derived from the peripheral artery disease group (relative risk reduction 3.8%; P=0.0028). In the stroke/transient ischemic attack cohort, comparative risk reduction for the composite endpoint was reduced and not statistically significant (relative risk reduction 7.3%; P=0.26).16
The Management of Atherosclerosis with Clopidogrel in High-Risk Patients (MATCH) study was an evaluation of clopidogrel versus clopidogrel plus aspirin in the prevention of secondary stroke. Seven thousand five hundred ninety-nine patients with a history of stroke or transient ischemic attack and other vascular risk factors were randomly assigned to clopidogrel alone or clopidogrel plus aspirin. After a mean follow-up of 18 months, the clopidogrel plus aspirin combination group demonstrated only an insignificant benefit in the composite outcome of rehospitalization for an ischemic event, ischemic stroke, acute myocardial infarction, or vascular death (clopidogrel plus aspirin 15.70%; clopidogrel monotherapy 16.73%; relative risk reduction 6.4%; P=0.244).13 In addition, the clopidogrel plus aspirin combination produced an increased absolute incidence of life-threatening bleeding episodes versus clopidogrel alone (2.6% versus 1.3%) that was greater than the absolute reduction in efficacy outcome events. Therefore, the combination of clopidogrel plus aspirin is not recommended for secondary event prevention after stroke or transient ischemic attack.17,18
In the recently reported Clopidogrel for High Risk and Ischemic Stabilization, Management, and Avoidance (CHARISMA) study, patients with documented coronary disease, cerebrovascular disease, or peripheral artery disease were administered either clopidogrel (75 mg/day) plus aspirin (75–162 mg/day) or aspirin alone.19 The study also included patients with multiple atherosclerotic risk factors but without documented arterial disease.
There was no significant difference between treatment arms regarding the primary composite endpoint of myocardial infarction, stroke, or cardiovascular death. Prespecified subgroup analyses showed a 1% absolute decrease in the incidence of the primary endpoint in patients with documented vascular disease (P=0.046) and an increase of 1.1% in the asymptomatic patients with multiple vascular risk factors (P=0.20) among those patients randomized to combination therapy. Severe bleeding (defined as fatal bleeding, intracranial hemorrhage, or bleeding causing hemodynamic compromise) occurred in 1.7% of patients in the combination therapy arm and 1.3% in the aspirin arm (P=0.09). Moderate bleeding, defined as that necessitating transfusion but not meeting the criteria for severe bleeding, occurred in 2.1% of patients in the combination therapy arm and 1.3% in the aspirin arm (P<0.001). The investigators concluded that clopidogrel plus aspirin provided no significant advantage over aspirin alone in reducing incidence of the primary combined endpoint.
Extended-release dipyridamole in combination with aspirin was evaluated in the European Stroke Prevention Study-2 (ESPS-2). The combination was compared with aspirin alone and with dipyridamole alone, as well as with placebo, in 6,602 patients with a history of stroke or transient ischemic attack. Extended-release dipyridamole and aspirin monotherapy showed similar efficacy in reducing the risk of stroke (relative risk reduction versus placebo: aspirin 18%, P=0.013; extended-release dipyridamole 16%, P=0.039). The extended-release dipyridamole plus aspirin combination, however, showed evidence of additive benefit; the relative risk reduction for stroke with extended-release dipyridamole plus aspirin was 23% versus aspirin alone (P=0.006) and 25% versus extended-release dipyridamole alone (P=0.002). Compared with placebo, the extended-release dipyridamole plus aspirin combination was associated with relative risk reductions of 37% (P<0.001) for stroke and 24% (P<0.001) for stroke or death. This combination reduced the relative risk of stroke over aspirin alone by 23%.20
Despite the apparent additive benefit derived from extended-release dipyridamole plus aspirin, no evidence was found for an increase in adverse outcomes. Adverse gastrointestinal events in the combination therapy group were comparable with those noted with aspirin monotherapy, with an increased incidence of headache.20
As in ESPS-2, the European/Australian Stroke Prevention in Reversible Ischemia Trial (ESPRIT) investigated the combination of aspirin and dipyridamole (principally extended-release dipyridamole). Using a primary combined endpoint of vascular death, nonfatal stroke, nonfatal myocardial infarction, and major bleeding complications, ESPRIT confirmed aspirin plus dipyridamole to be superior to aspirin monotherapy in reducing these complications.21 An overall risk ratio of 0.82 for the composite endpoint (P=0.0003) was determined in a meta-analysis of the trials comparing aspirin alone to aspirin plus dipyridamole.21 (See Figure 1, p. 39.)
An in-progress prospective secondary stroke prevention study, the Prospective Regimen for Effectively Avoiding Second Strokes (PRoFESS) study, which consists of 15,500 patients with a recent history of ischemic stroke, will provide the first head-to-head comparison of clopidogrel monotherapy with the extended-release dipyridamole plus aspirin combination. The two antiplatelet regimens will be evaluated through a 2 x 2 design in the presence and in the absence of the antihypertensive telmisartan, with results expected in 2007. PRoFESS findings should help to clarify the comparative efficacy of clopidogrel versus extended-release dipyridamole plus aspirin with regard to the primary endpoint (time to first stroke recurrence) and a vascular events composite endpoint.
Antiplatelet Treatment Guidelines
The American Academy of Neurology guidelines recommend the use of aspirin within 48 hours of stroke symptom onset (except when tissue plasminogen activator treatment has been used or is anticipated) to reduce mortality and prevent early stroke recurrence.22 A more extensive set of evidence-based guidelines for antiplatelet and antithrombotic use following ischemic stroke, including recommendations for secondary event prevention, was developed in 2004 by the American College of Chest Physicians (ACCP).23 The primary recommendation (Grade 1A) is to provide treatment with an antiplatelet agent (i.e., aspirin at 50 to 325 mg/day, extended-release dipyridamole at 200 mg plus aspirin at 25 mg twice daily, or clopidogrel at 75 mg/day) following noncardioembolic stroke. The ACCP has also suggested that extended-release dipyridamole plus aspirin (Grade 2A) or clopidogrel (Grade 2B) may be preferable to aspirin monotherapy. This suggestion does include the caveat that this “places a relatively high value on a small absolute risk reduction in stroke rates, and a relatively low value on minimizing drug expenditures.”23
Discharge Planning
When the post-stroke patient is prepared for discharge, place the highest priority on ensuring an effective continuum of care. Comprehensively review all medications, including those prescribed for prevention of secondary events, with the patient and family or caregivers. Explain the purpose of each medication, along with the consequences of poor compliance or discontinuation; reinforce the need for lifelong therapy for stroke prevention and amelioration of stroke risk factors at every opportunity.
A key step in establishing the continuum of care is to gain buy-in from the primary care provider for continuing medical therapy and follow-up. If appropriate, cite current guidelines from the American Academy of Neurology, the American College of Chest Physicians, and the American Stroke Association. Occupational or physical therapy, if indicated, should be planned before discharge and coordinated with the primary care provider for continued follow-up. This evaluation may also result in a recommendation for inpatient rehabilitation or, in the interim, a skilled nursing facility placement.
Given the improvement that many patients realize over the short term, staged discharge to a skilled nursing facility may be followed after a short interval by a stay at an inpatient rehabilitation facility. Coordination of this staged approach must be carefully implemented, as it is easy for this to fall through the cracks during transitions of care.
Conclusion: Stroke Centers and Systems of Care
Managing patients with stroke is in many ways an ideal fit for the hospitalist model. From symptom onset, the patient with stroke challenges traditional approaches to care in multiple ways: variable presentation involving multiple neurologic symptoms, frequent systemic comorbidities and risk factors, highly variable disease course and sequelae, and the need for active and coordinated management throughout the continuum of care. The hospital physician should seek to improve the value of care by ensuring and facilitating consistent management according to established guidelines and by managing the transitions between phases of treatment.
SHM provides numerous valuable tools to the hospital physician for use in improving the care of patients with stroke, including diagnostic and assessment instruments and guidelines, algorithms and pathways for management of patients with stroke, sample standing orders from leading institutions, and resources that can be provided to patients and their families. All are available or downloadable from the SHM Web site, at www.hospitalmedicine.org/AM/Template.cfm?Section=Quality_Improvement_Resource_ Rooms&Template=/ CM/HTMLDisplay.cfm&ContentID=6566. Even (or perhaps especially) in the absence of higher-level systems dedicated to the care of patients with stroke, the hospital physician can serve as a critical linchpin in the optimization of patient outcomes following stroke. TH
Dr. Likosky is executive director, Evergreen Neuroscience Institute, Kirkland, Wash., as well as a hospitalist and neurohospitalist.
References
- Gebel JM Jr. Secondary stroke prevention with antiplatelet therapy with emphasis on the cardiac patient: a neurologist’s view. J Am Coll Cardiol. 2005 Sep 6;46(5):752-755.
- Vickrey BG, Rector TS, Wickstrom SL, et al. Occurrence of secondary ischemic events among persons with atherosclerotic vascular disease. Stroke. 2002 Apr;33(4):901-906.
- Adams HP Jr, Adams RJ, Brott T, et al. Guidelines for the early management of patients with ischemic stroke: A scientific statement from the Stroke Council of the American Stroke Association. Stroke. 2003 Apr;34(4):1056-1083.
- Leira EC, Chang KC, Davis PH, et al. Can we predict early recurrence in acute stroke? Cerebrovasc Dis. 2004;18(2):139-144.
- Pinto A, Tuttolomondo A, Di Raimondo D, et al. Cerebrovascular risk factors and clinical classification of strokes. Semin Vasc Med. 2004 Aug;4(3):287-303.
- Rothwell PM. Incidence, risk factors and prognosis of stroke and TIA: the need for high-quality, large-scale epidemiological studies and meta-analyses. Cerebrovasc Dis. 2003;16(Suppl 3):2-10.
- Schulz UG, Rothwell PM. Differences in vascular risk factors between etiological subtypes of ischemic stroke: importance of population-based studies. Stroke. 2003 Aug;34(8):2050-2059; Epub 2003 Jun 26.
- Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993 Jan;24(1):35-41.
- Sacco RL, Benjamin EJ, Broderick JP, et al. American Heart Association Prevention Conference. IV. Prevention and rehabilitation of stroke. Risk factors. Stroke. 1997;28:1507-1517.
- Arenillas JF, Alvarez-Sabin J, Molina CA, et al. C-reactive protein predicts further ischemic events in first-ever transient ischemic attack or stroke patients with intracranial large-artery occlusive disease. Stroke. 2003 Oct;34(10):2463-2468.
- Wolf PA, Clagett GP, Easton JD, et al. Preventing ischemic stroke in patients with prior stroke and transient ischemic attack: a statement for healthcare professionals from the Stroke Council of the American Heart Association. Stroke. 1999;30:1991-1994.
- Chaturvedi S, Bruno A, Feasby T, et al. Carotid endarterectomy—an evidence-based review: report of the Therapeutics and Technology Assessment Sub-committee of the American Academy of Neurology. Neurology. 2005 Sep 27;65(6):794-801.
- The Dutch TIA Trial Study Group. A comparison of two doses of aspirin (30 mg vs. 283 mg a day) in patients after a transient ischemic attack or minor ischemic stroke. N Engl J Med. 1991;325:1261-1266.
- Farrell B, Godwin J, Richards S, et al. The United Kingdom transient ischaemic attack (UK-TIA) aspirin trial: final results. J Neurol Neurosurg Psychiatry. 1991 Dec;54(12):1044-1054.
- The SALT Collaborative Group. Swedish Aspirin Low-Dose Trial (SALT) of 75 mg aspirin as secondary prophylaxis after cerebrovascular ischaemic events. Lancet. 1991 Nov 30;338(8779):1345-1349.
- CAPRIE Steering Committee. A randomised, blinded trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet. 1996 Nov 16;348(9038):1329-1339.
- Diener HC, Bogousslavsky J, Brass LM, et al. Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial. Lancet. 2004;364:331-337.
- Hankey GJ, Eikelboom JW. Adding aspirin to clopidogrel after TIA and ischemic stroke: benefits do not match risks. Neurology. 2005 Apr 12;64(7):1117-1121.
- Bhatt DL, Fox KA, Hacke W, et al; CHARISMA Investigators. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med. 2006 Apr 20;354(16):1706-1717.
- Diener HC, Cunha L, Forbes C, et al. European Stroke Prevention Study. 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci. 1996 Nov;143(1-2):1-13.
- Halkes PH, van Gijn J, Kappelle LJ, et al. (ESPRIT Study Group). Aspirin plus dipyridamole versus aspirin alone after cerebral ischaemia of arterial origin (ESPRIT): randomised controlled trial. Lancet. 2006 May 20;367(9523):1665-1673.
- Coull BM, Williams LS, Goldstein LB, et al. Anticoagulants and antiplatelet agents in acute ischemic stroke: report of the Joint Stroke Guideline Development Committee of the American Academy of Neurology and the American Stroke Association (a division of the American Heart Association). Neurology. 2002 Jul 9;59(1):13-22.
- Albers GW, Amarenco P, Easton JD, et al. Antithrombotic and thrombolytic therapy for ischemic stroke: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004 Sep;126(3 Suppl):483S-512S.