User login
One of the most eagerly awaited results from an SHM compensation and productivity survey is the amount of financial support provided by hospitals or other organizations to HM groups (note that we’ve carefully avoided the dreaded “S” word). SHM has been asking this question since at least 2003, when the median annual support per hospitalist FTE was reported at $60,000. By 2007, that number had grown by 62% to $97,375. But the 2007 findings that might have caused the greatest uproar were that fully 37% of responding HM group leaders did not know their program’s annual expenses, and 35% did not know their program’s revenues.
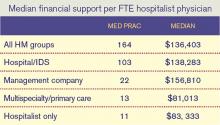
Fast-forward to today. The median annual financial support per FTE reported in the 2011 SHM/MGMA State of Hospital Medicine report is $136,403, a whopping 39% increase over the 2010 median of $98,253.
What caused this big increase in HM’s financial support requirement? Did costs go up that dramatically in just one year? Well, the median compensation for adult medicine hospitalists (the vast majority of hospitalists in the data set) went up by a mere 2.6% during the same period. The amount of support staffing reported by HM groups did not change appreciably. And since labor accounts for the vast majority of virtually every HM practice’s costs, it’s unlikely that the increase in financial support per FTE was caused by a dramatic increase in program costs.
Perhaps program revenues went down significantly, then. It’s true that the median professional fee collections per FTE for adult hospitalists declined between the 2010 and 2011 reports, but only by about 3.3%—probably a result of gearing up for healthcare reform, increases in indigent care and bad debt due to the weak economy, and similar revenue pressures. So it doesn’t appear that declining revenues can explain the big jump in financial support per FTE, either.
I’d like to think that one of the reasons financial support per FTE has increased so much is that we are getting better at how we ask the question. Early on, we simply asked, “If your group receives OTHER INCOME (besides collections for direct patient care), indicate source and amount of payments.” In recent years, the question has been fine-tuned to ask about “financial support over and above professional fee revenues from one or more hospitals or integrated delivery systems (or other sources),” and the survey guide has given even more detailed instructions. But in truth, the question was worded almost identically in 2010 and 2011.
All of this leads me to the unavoidable speculation that HM groups (and/or the hospitals they work for) probably are becoming more sophisticated about how they account for the costs of their hospitalist programs, and that HM group leaders are becoming more knowledgeable about their own programs’ costs and revenues (and, yes, the amount of financial support they receive). We haven’t asked respondents recently whether they know their practice’s costs and revenues, but maybe next time we should. I’ll bet the results will differ a lot from 2007.
—Leslie Flores, MHA, SHM senior advisor
One of the most eagerly awaited results from an SHM compensation and productivity survey is the amount of financial support provided by hospitals or other organizations to HM groups (note that we’ve carefully avoided the dreaded “S” word). SHM has been asking this question since at least 2003, when the median annual support per hospitalist FTE was reported at $60,000. By 2007, that number had grown by 62% to $97,375. But the 2007 findings that might have caused the greatest uproar were that fully 37% of responding HM group leaders did not know their program’s annual expenses, and 35% did not know their program’s revenues.
Fast-forward to today. The median annual financial support per FTE reported in the 2011 SHM/MGMA State of Hospital Medicine report is $136,403, a whopping 39% increase over the 2010 median of $98,253.
What caused this big increase in HM’s financial support requirement? Did costs go up that dramatically in just one year? Well, the median compensation for adult medicine hospitalists (the vast majority of hospitalists in the data set) went up by a mere 2.6% during the same period. The amount of support staffing reported by HM groups did not change appreciably. And since labor accounts for the vast majority of virtually every HM practice’s costs, it’s unlikely that the increase in financial support per FTE was caused by a dramatic increase in program costs.
Perhaps program revenues went down significantly, then. It’s true that the median professional fee collections per FTE for adult hospitalists declined between the 2010 and 2011 reports, but only by about 3.3%—probably a result of gearing up for healthcare reform, increases in indigent care and bad debt due to the weak economy, and similar revenue pressures. So it doesn’t appear that declining revenues can explain the big jump in financial support per FTE, either.
I’d like to think that one of the reasons financial support per FTE has increased so much is that we are getting better at how we ask the question. Early on, we simply asked, “If your group receives OTHER INCOME (besides collections for direct patient care), indicate source and amount of payments.” In recent years, the question has been fine-tuned to ask about “financial support over and above professional fee revenues from one or more hospitals or integrated delivery systems (or other sources),” and the survey guide has given even more detailed instructions. But in truth, the question was worded almost identically in 2010 and 2011.
All of this leads me to the unavoidable speculation that HM groups (and/or the hospitals they work for) probably are becoming more sophisticated about how they account for the costs of their hospitalist programs, and that HM group leaders are becoming more knowledgeable about their own programs’ costs and revenues (and, yes, the amount of financial support they receive). We haven’t asked respondents recently whether they know their practice’s costs and revenues, but maybe next time we should. I’ll bet the results will differ a lot from 2007.
—Leslie Flores, MHA, SHM senior advisor
One of the most eagerly awaited results from an SHM compensation and productivity survey is the amount of financial support provided by hospitals or other organizations to HM groups (note that we’ve carefully avoided the dreaded “S” word). SHM has been asking this question since at least 2003, when the median annual support per hospitalist FTE was reported at $60,000. By 2007, that number had grown by 62% to $97,375. But the 2007 findings that might have caused the greatest uproar were that fully 37% of responding HM group leaders did not know their program’s annual expenses, and 35% did not know their program’s revenues.
Fast-forward to today. The median annual financial support per FTE reported in the 2011 SHM/MGMA State of Hospital Medicine report is $136,403, a whopping 39% increase over the 2010 median of $98,253.
What caused this big increase in HM’s financial support requirement? Did costs go up that dramatically in just one year? Well, the median compensation for adult medicine hospitalists (the vast majority of hospitalists in the data set) went up by a mere 2.6% during the same period. The amount of support staffing reported by HM groups did not change appreciably. And since labor accounts for the vast majority of virtually every HM practice’s costs, it’s unlikely that the increase in financial support per FTE was caused by a dramatic increase in program costs.
Perhaps program revenues went down significantly, then. It’s true that the median professional fee collections per FTE for adult hospitalists declined between the 2010 and 2011 reports, but only by about 3.3%—probably a result of gearing up for healthcare reform, increases in indigent care and bad debt due to the weak economy, and similar revenue pressures. So it doesn’t appear that declining revenues can explain the big jump in financial support per FTE, either.
I’d like to think that one of the reasons financial support per FTE has increased so much is that we are getting better at how we ask the question. Early on, we simply asked, “If your group receives OTHER INCOME (besides collections for direct patient care), indicate source and amount of payments.” In recent years, the question has been fine-tuned to ask about “financial support over and above professional fee revenues from one or more hospitals or integrated delivery systems (or other sources),” and the survey guide has given even more detailed instructions. But in truth, the question was worded almost identically in 2010 and 2011.
All of this leads me to the unavoidable speculation that HM groups (and/or the hospitals they work for) probably are becoming more sophisticated about how they account for the costs of their hospitalist programs, and that HM group leaders are becoming more knowledgeable about their own programs’ costs and revenues (and, yes, the amount of financial support they receive). We haven’t asked respondents recently whether they know their practice’s costs and revenues, but maybe next time we should. I’ll bet the results will differ a lot from 2007.
—Leslie Flores, MHA, SHM senior advisor