User login
Using magnets to improve health is sometimes hawked in dubious classified ads and “infomercials.” However, a legitimate use of magnetism—repetitive transcranial magnetic stimulation (rTMS)—is showing promise in treating severe depression (Box) 1-4 and other psychiatric disorders.
Patients or their families are likely to ask psychiatrists about rTMS as more becomes known about this investigational technology. Drawing from our experience and the evidence, we offer an update on whether rTMS may be an alternative for treating depression and address issues that must be resolved before it could be used in clinical practice.
WHAT IS RTMS?
rTMS consists of a series of magnetic pulses produced by a stimulator, which can be adjusted for:
- coil type and placement
- stimulation site, intensity, frequency, and number
- amount of time between stimulations
- treatment duration.
In 1985, Barker and colleagues developed single-pulse transcranial magnetic stimulation to examine motor cortex function.1 The single-pulse mechanism they discovered was subsequently adapted to deliver repetitive pulses and is referred to as repetitive transcranial magnetic stimulation (rTMS).
How rTMS works. Transcranial magnetic stimulation uses an electromagnetic coil applied to the head to produce an intense, localized, fluctuating magnetic field that passes unimpeded into a small area of the brain, inducing an electrical current. This results in neuronal depolarization in a localized area under the coil, and possibly distal effects as well.2 During the neurophysiological studies, it was discovered that subjects also experienced a change in mood.
Antidepressant effects. Similar physiologic effects induced by rTMS, electroconvulsive therapy (ECT), and antidepressants on the endocrine system, sleep parameters, and biochemical measures suggest antidepressant properties.3 In 1993, the first published study examining rTMS in psychiatric patients reported reduced depressive symptoms in two subjects.4 Since then, several clinical trials have examined rTMS’ antidepressive effects. In 2001, Canada’s Health Ministry approved rTMS for treating major depression. In the United States, rTMS remains investigational and is FDA-approved only for clinical trials.
Coil type and placement. Initial studies involved stimulation—typically low-frequency—over the vertex, but most subsequent rTMS trials in depression have stimulated the left dorsolateral prefrontal cortex. Neuroimaging studies have shown prefrontal functioning abnormalities in depressed subjects, and it is hypothesized that stimulating this area (plus possible distal effects) may produce an antidepressant effect.5
Various configurations have been used, but circular and figure-eight-shaped coils are most common. These flat coils are made of tightly wound ferromagnetic material such as copper, enclosed in a heavy plastic cover. With the figure-eight coil, the intersection of the two loops produces the strongest magnetic field.
Stimulation site. Stimulation intensity depends on the individual’s motor threshold, and the site can be determined visually or electrophysiologically.
- With the visual method, the motor threshold over the left primary motor cortex site for the first dorsal interosseous muscle (FDI) or the abductor pollius brevis (APB) is determined by iteration. This involves placing the coil at a progression of sites and increasing stimulation intensity until reliable (in 5 of 10 stimulations) contractions are seen in the right FDI or APB.
- Similarly, the electrophysiologic method uses 5 of 10 motorevoked potentials of 50 microvolts to locate the site.
The only small trial that compared visual and electrophysiologic site determination showed similar results with both methods.6 The most common stimulation site is the left dorsolateral prefrontal cortex, 5 cm anterior and parasagittal to the FDI or APB motor cortex. Alternately, frameless stereotactic systems or the international 10-20 proportional system used in EEG labs have been recommended to target sites more accurately.
Stimulus intensity. Each individual’s motor threshold determines stimulus intensity. Using functional MRI studies, researchers from the Medical University of South Carolina concluded that higher stimulation intensity relative to the motor threshold may have a more robust effect, as the magnetic field declines with distance from the coil.7 However, intensities >120% of the motor threshold are generally avoided because of possible increased seizure risk.9
Frequency of stimulation. Most researchers apply frequencies of 1 to 20 Hz over the left dorsolateral prefrontal cortex, but also use lower frequencies (<1 Hz) over the right dorsolateral prefrontal cortex. Using higher frequencies in major depression is attractive in theory because of:
- the reported association of decreased regional cerebral blood flow with hypometabolism in the left dorsolateral prefrontal cortex
- higher-frequency stimulation’s ability to produce temporary excitation and neuronal depolarization.
Number of stimulations. The number of stimulations is determined by frequency (Hz) and stimulation train duration (for example, 10 Hz for 5 seconds equals 50 stimulations). A typical treatment session incorporates 10 to 30 stimulation trains several seconds apart (the inter-train interval). Thus, a typical session delivers 1,000 to 1,200 stimulations. In studies of unmedicated depressed patients, the total number of stimulations has varied from 8,000 to 32,000 per treatment course.
Duration between two stimulation trains. Chen et al have demonstrated that shorter (<1 second) inter-train intervals increase seizure risk with higher frequencies (such as 20 Hz) and intensities (>100% of motor threshold) of stimulation.9 Based on their studies with healthy volunteers, they recommended several “safe” ranges (such as 5 seconds at 110% of motor threshold). Most trials use 30- to 60-second inter-train intervals.
Most treatments continue 2 to 4 weeks, Monday through Friday, although more frequent treatments are being studied.
EFFICACY FOR DEPRESSION
Most studies of rTMS in depression have compared real rTMS to a sham control or electroconvulsive therapy (ECT).
In earlier studies, the sham procedure typically involved tilting the coil away from the skull. This method has been questioned, however, because of evidence of neuronal depolarization.10
More recent sham coils mimic the real coils’ sound and sensation, without magnetic stimulation.
Despite these methodologic problems and some mixed results, depressed patients receiving rTMS show more favorable results than those receiving sham rTMS.11,12 Several meta-analyses have attempted to quantify rTMS’ efficacy for depression:
- Holtzheimer et al concluded that rTMS was statistically superior to sham rTMS, but the clinical significance of these findings was modest in a population of mostly outpatients with less-severe depression.13
- Burt et al found a statistically strong antidepressant effect, but its magnitude varied and few of the studies yielded a substantial clinical response or remission. The team also noted that rTMS’ long-term efficacy or adverse effects are unknown.14
- Kozel et al concluded that left prefrontal rTMS rendered a significant antidepressant effect with measurable clinical improvement.15
- Gershon et al16 supported an antidepressant effect for rTMS when compared with sham rTMS or ECT.
Ongoing rTMS research includes subjects with many types of mild to severe psychiatric illnesses, including major depression, obsessive-compulsive disorder, and psychosis. Typically, patients referred for experimental approaches have not responded to or tolerated available treatments. Exclusion criteria used by most rTMS studies are listed in the Table.
Table
Medical conditions that preclude use of rTMS
| Serious medical conditions History of seizures Increased intracranial pressure Serious head trauma |
| Myocardial infarction within the past 6 months |
| Pregnancy or childbearing potential (unless reliable contraception is being used) |
| Intracranial metallic implants |
| Pacemakers or other implanted devices |
rTMS vs. ECT. Four randomized, controlled trials have compared rTMS with ECT for treating severely ill, often medication-resistant patients.17-20 Although their methodologies differed, all four studies concluded that rTMS and ECT offer similar efficacy, except that rTMS may be less effective for treating psychotic depression.
One study found ECT more effective than rTMS for psychotic depression, although the patients who received ECT were also treated with antipsychotics and/or antidepressants.17 Our study,19 which did not use these agents, has not corroborated this observation. Preliminary data also indicate comparable relapse rates following acute ECT and rTMS when subjects are followed on maintenance medication.21
ADVERSE EFFECTS
The potential adverse effects of new treatments must always be considered. Thus far, rTMS appears to produce minimal, relatively benign complications, including:
- mild discomfort at the stimulation site
- localized muscle twitching during stimulation
- mild post-treatment headaches—believed caused by muscle contractions—which usually respond to aspirin or acetaminophen
- treatment stimulation-related seizures (rarely).8
The rTMS device makes a loud clicking noise, and subjects wear protective ear plugs during treatment.
Patient experience. The first rTMS session—during which the patient’s motor threshold is determined—can last up to 45 minutes. Subsequent sessions are usually 15 to 20 minutes. Patients are typically apprehensive before the first session but become more relaxed with experience and tolerate the treatments easily.
During the procedure, many patients describe a tapping sensation on the forehead, and some experience slight muscle twitching around the eye or corner of the mouth. As the coil warms, the skin it touches sometimes flushes pink, although this does not seem to bother our patients. They can return to their daily routines immediately after a session.
rTMS for major depression. In our experience, rTMS may help patients with major depression. For example, one patient diagnosed with a major depressive episode with psychotic features was referred to our study comparing rTMS with ECT.19 Her depression had lasted several months, with partial response to ECT treatments. She signed informed consent and was randomly assigned to receive rTMS treatment.
At study admission, the patient’s Hamilton Depression Rating Scale (HDRS) score was 48, indicating moderate to severe depression. Following 10 rTMS sessions, her HDRS score had dropped to 2, with remission of symptoms. No follow-up results were documented.
Cognitive effects. Whereas mood disorders are associated with medication-independent neuropsychological deficits, most studies have found no adverse cognitive effects with rTMS.22 Indeed, some of our rTMS patients have improved in certain cognitive tests, although this may be explained by test-retest effects or better attention and concentration associated with mood improvement.
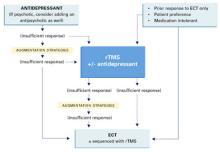
Figure Potential roles for rTMS in treating major depression
Solid lines represent current standards of practice. Dotted lines represent hypothetical roles for rTMS.
Source: Adapted and reprinted with permission from Dowd et al. Is repetitive transcranial magnetic stimulation an alternative to ECTfor the treatment of depression? Contemp Psychiatry 2002;1:1-10.
POTENTIAL ROLE FOR rTMS
Today’s standard treatment of major depressive episodes begins with an antidepressant (plus an antipsychotic, if necessary) and proceeds to augmentation strategies if response is insufficient. rTMS may one day become an augmentation or monotherapy option for patients who do not respond sufficiently to standard treatments (Figure).
ECT treatment may be initiated if a patient has had a prior good response to ECT, is intolerant to medication, or prefers ECT. In that case, rTMS may be used as an alternate initial treatment or with ECT. Thus, rTMS may be used:
- to augment antidepressants
- as an alternative to antidepressants or ECT
- or sequentially with ECT.
Before that can happen, however, optimal treatment parameters need to be clarified by larger, well-designed, controlled studies comparing rTMS to a valid sham treatment, antidepressants, and ECT.
Related resources
- International Society for Transcranial Stimulation. www.ists.unibe.ch/
- Repetitive Transcranial Magnetic Stimulation Research Clinic at Yale-New Haven Psychiatric Hospital.
Disclosure
The authors report that they have no proprietary interest in the technology discussed in this article.
1. Barker A, Jalinous R, Freeston I. Non-invasive magnetic stimulation of human motor cortex. Lancet 1985;1:1106-7.
2. Lisanby SH, Datto CJ, Szuba MP. ECT and rTMS: past, present, and future. Depress Anxiety 2000;12:115-17.
3. Post A, Keck PE, Jr. Transcranial magnetic stimulation as a therapeutic tool in psychiatry: what do we know about the neurobiological mechanisms? J Psychiatr Res 2001;35:193-215.
4. Holfich G, Kasper S, Hufnagel A, et al. Application of transcranial magnetic stimulation in treatment of drug resistant major depression—a report of two cases. Human Psychopharmacol 1993;8:361-5.
5. George MS, Nahas Z, Speer AM, et al. Transcranial magnetic stimulation—a new method for investigating the neuroanatomy of depression. In: Ebert D, Ebmeier K (eds). New models for depression. New York: Karger, 1998;94-122.
6. Pridmore A, Americo Fernandes Filho J, Nahas Z, et al. Motor threshold in transcranial magnetic stimulation: a comparison of a neurophysiological method and a visualization of movement method. J ECT 1998;14(1):25-7.
7. Kozel FA, Nahas Z, deBrux C, et al. How coil-cortex distance relates to age, motor threshold, and antidepressant response to repetitive transcranial magnetic stimulation. J Neuropsychiatry Clin Neurosci 2000;13:376-84.
8. Wassermann EM. Risk and safety of repetitive transcranial magnetic stimulation: report and suggested guidelines from the International Workshop on the Safety of Repetitive Transcranial Magnetic Stimulation, 1996. Electroencephalogr Clin Neurophysiol 1998;108:1-16.
9. Chen R, Gerloff C, Classen J, et al. Safety of different inter-train intervals for repetitive transcranial magnetic stimulation and recommendations for safe ranges of stimulation parameters. Electroencephalogr Clin Neurophysiol 1997;105:415-21.
10. Loo CK, Taylor JL, Gandevia SC, et al. Transcranial magnetic stimulation in controlled treatment studies: Are some “sham” forms active? Biol Psychiatry. 2000;47:325-31.
11. George MS, Nahas Z, Molloy M, et al. A controlled trial of daily left prefrontal cortex TMS for treating depression. Biol Psychiatry 2000;48:962-70.
12. Berman RM, Narasimhan M, Sanacora G, et al. A randomized clinical trial of repetitive transcranial magnetic stimulation in the treatment of major depression. Biol Psychiatry 2000;47:332-7.
13. Holtzheimer PE, Russo J, Avery D. A meta-analysis of repetitive transcranial magnetic stimulation in the treatment of depression. Psychopharmacol Bull 2001;35:149-69.
14. Burt T, Lisanby SH, Sackeim HA. Neuropsychiatric applications of transcranial magnetic stimulation: a meta-analysis. Int J Neuropsychopharmacol 2002;5:73-103.
15. Kozel FE, George MS. Meta-analysis of left prefrontal repetitive transcranial magnetic stimulation (rTMS) to treat depression. J Psychiatr Pract 2002;8:270-5.
16. Gershon AA, Dannon PN, Grunhaus L. Transcranial magnetic stimulation in the treatment of depression. Am JPsychiatry 2003;160(5):835-45.
17. Grunhaus L, Dannon PN, Schreiber S, et al. Repetitive transcranial magnetic stimulation is as effective as electroconvulsive therapy in the treatment of nondelusional major depressive disorder: an open study. Biol Psychiatry 2000;47:314-24.
18. Pridmore S, Bruno R, Turnier-Shea Y, et al. Comparison of unlimited numbers of rapid transcranial magnetic stimulation and ECT treatment sessions in major depression episodes. Int J Neuropsychopharmacol 2000;3:129-34.
19. Janicak PG, Dowd SM, Martis B, et al. Repetitive transcranial magnetic stimulation versus electroconvulsive therapy for major depression: preliminary results of a randomized trial. Biol Psychiatry 2002;51:659-67
20. Grunhaus L, Schreiber S, Dolberg OT, et al. A randomized controlled comparison of electroconvulsive therapy and repetitive transcranial magnetic stimulation in severe and resistant nonpsychotic major depression. Biol Psychiatry 2003;53:324-31.
21. Dannon PH, Dolberg OT, Schreiber S, Grunhaus L. Three and six month outcome following courses of either ECT or rTMS in a population of severely depressed individuals—preliminary report. Biol Psychiatry 2002;15:687-90.
22. Martis B, Alam D, Dowd SM, et al. Neurocognitive effects of repetitive transcranial magnetic stimulation in severe major depression. Clin Neurophysiology (in press).
Using magnets to improve health is sometimes hawked in dubious classified ads and “infomercials.” However, a legitimate use of magnetism—repetitive transcranial magnetic stimulation (rTMS)—is showing promise in treating severe depression (Box) 1-4 and other psychiatric disorders.
Patients or their families are likely to ask psychiatrists about rTMS as more becomes known about this investigational technology. Drawing from our experience and the evidence, we offer an update on whether rTMS may be an alternative for treating depression and address issues that must be resolved before it could be used in clinical practice.
WHAT IS RTMS?
rTMS consists of a series of magnetic pulses produced by a stimulator, which can be adjusted for:
- coil type and placement
- stimulation site, intensity, frequency, and number
- amount of time between stimulations
- treatment duration.
In 1985, Barker and colleagues developed single-pulse transcranial magnetic stimulation to examine motor cortex function.1 The single-pulse mechanism they discovered was subsequently adapted to deliver repetitive pulses and is referred to as repetitive transcranial magnetic stimulation (rTMS).
How rTMS works. Transcranial magnetic stimulation uses an electromagnetic coil applied to the head to produce an intense, localized, fluctuating magnetic field that passes unimpeded into a small area of the brain, inducing an electrical current. This results in neuronal depolarization in a localized area under the coil, and possibly distal effects as well.2 During the neurophysiological studies, it was discovered that subjects also experienced a change in mood.
Antidepressant effects. Similar physiologic effects induced by rTMS, electroconvulsive therapy (ECT), and antidepressants on the endocrine system, sleep parameters, and biochemical measures suggest antidepressant properties.3 In 1993, the first published study examining rTMS in psychiatric patients reported reduced depressive symptoms in two subjects.4 Since then, several clinical trials have examined rTMS’ antidepressive effects. In 2001, Canada’s Health Ministry approved rTMS for treating major depression. In the United States, rTMS remains investigational and is FDA-approved only for clinical trials.
Coil type and placement. Initial studies involved stimulation—typically low-frequency—over the vertex, but most subsequent rTMS trials in depression have stimulated the left dorsolateral prefrontal cortex. Neuroimaging studies have shown prefrontal functioning abnormalities in depressed subjects, and it is hypothesized that stimulating this area (plus possible distal effects) may produce an antidepressant effect.5
Various configurations have been used, but circular and figure-eight-shaped coils are most common. These flat coils are made of tightly wound ferromagnetic material such as copper, enclosed in a heavy plastic cover. With the figure-eight coil, the intersection of the two loops produces the strongest magnetic field.
Stimulation site. Stimulation intensity depends on the individual’s motor threshold, and the site can be determined visually or electrophysiologically.
- With the visual method, the motor threshold over the left primary motor cortex site for the first dorsal interosseous muscle (FDI) or the abductor pollius brevis (APB) is determined by iteration. This involves placing the coil at a progression of sites and increasing stimulation intensity until reliable (in 5 of 10 stimulations) contractions are seen in the right FDI or APB.
- Similarly, the electrophysiologic method uses 5 of 10 motorevoked potentials of 50 microvolts to locate the site.
The only small trial that compared visual and electrophysiologic site determination showed similar results with both methods.6 The most common stimulation site is the left dorsolateral prefrontal cortex, 5 cm anterior and parasagittal to the FDI or APB motor cortex. Alternately, frameless stereotactic systems or the international 10-20 proportional system used in EEG labs have been recommended to target sites more accurately.
Stimulus intensity. Each individual’s motor threshold determines stimulus intensity. Using functional MRI studies, researchers from the Medical University of South Carolina concluded that higher stimulation intensity relative to the motor threshold may have a more robust effect, as the magnetic field declines with distance from the coil.7 However, intensities >120% of the motor threshold are generally avoided because of possible increased seizure risk.9
Frequency of stimulation. Most researchers apply frequencies of 1 to 20 Hz over the left dorsolateral prefrontal cortex, but also use lower frequencies (<1 Hz) over the right dorsolateral prefrontal cortex. Using higher frequencies in major depression is attractive in theory because of:
- the reported association of decreased regional cerebral blood flow with hypometabolism in the left dorsolateral prefrontal cortex
- higher-frequency stimulation’s ability to produce temporary excitation and neuronal depolarization.
Number of stimulations. The number of stimulations is determined by frequency (Hz) and stimulation train duration (for example, 10 Hz for 5 seconds equals 50 stimulations). A typical treatment session incorporates 10 to 30 stimulation trains several seconds apart (the inter-train interval). Thus, a typical session delivers 1,000 to 1,200 stimulations. In studies of unmedicated depressed patients, the total number of stimulations has varied from 8,000 to 32,000 per treatment course.
Duration between two stimulation trains. Chen et al have demonstrated that shorter (<1 second) inter-train intervals increase seizure risk with higher frequencies (such as 20 Hz) and intensities (>100% of motor threshold) of stimulation.9 Based on their studies with healthy volunteers, they recommended several “safe” ranges (such as 5 seconds at 110% of motor threshold). Most trials use 30- to 60-second inter-train intervals.
Most treatments continue 2 to 4 weeks, Monday through Friday, although more frequent treatments are being studied.
EFFICACY FOR DEPRESSION
Most studies of rTMS in depression have compared real rTMS to a sham control or electroconvulsive therapy (ECT).
In earlier studies, the sham procedure typically involved tilting the coil away from the skull. This method has been questioned, however, because of evidence of neuronal depolarization.10
More recent sham coils mimic the real coils’ sound and sensation, without magnetic stimulation.
Despite these methodologic problems and some mixed results, depressed patients receiving rTMS show more favorable results than those receiving sham rTMS.11,12 Several meta-analyses have attempted to quantify rTMS’ efficacy for depression:
- Holtzheimer et al concluded that rTMS was statistically superior to sham rTMS, but the clinical significance of these findings was modest in a population of mostly outpatients with less-severe depression.13
- Burt et al found a statistically strong antidepressant effect, but its magnitude varied and few of the studies yielded a substantial clinical response or remission. The team also noted that rTMS’ long-term efficacy or adverse effects are unknown.14
- Kozel et al concluded that left prefrontal rTMS rendered a significant antidepressant effect with measurable clinical improvement.15
- Gershon et al16 supported an antidepressant effect for rTMS when compared with sham rTMS or ECT.
Ongoing rTMS research includes subjects with many types of mild to severe psychiatric illnesses, including major depression, obsessive-compulsive disorder, and psychosis. Typically, patients referred for experimental approaches have not responded to or tolerated available treatments. Exclusion criteria used by most rTMS studies are listed in the Table.
Table
Medical conditions that preclude use of rTMS
| Serious medical conditions History of seizures Increased intracranial pressure Serious head trauma |
| Myocardial infarction within the past 6 months |
| Pregnancy or childbearing potential (unless reliable contraception is being used) |
| Intracranial metallic implants |
| Pacemakers or other implanted devices |
rTMS vs. ECT. Four randomized, controlled trials have compared rTMS with ECT for treating severely ill, often medication-resistant patients.17-20 Although their methodologies differed, all four studies concluded that rTMS and ECT offer similar efficacy, except that rTMS may be less effective for treating psychotic depression.
One study found ECT more effective than rTMS for psychotic depression, although the patients who received ECT were also treated with antipsychotics and/or antidepressants.17 Our study,19 which did not use these agents, has not corroborated this observation. Preliminary data also indicate comparable relapse rates following acute ECT and rTMS when subjects are followed on maintenance medication.21
ADVERSE EFFECTS
The potential adverse effects of new treatments must always be considered. Thus far, rTMS appears to produce minimal, relatively benign complications, including:
- mild discomfort at the stimulation site
- localized muscle twitching during stimulation
- mild post-treatment headaches—believed caused by muscle contractions—which usually respond to aspirin or acetaminophen
- treatment stimulation-related seizures (rarely).8
The rTMS device makes a loud clicking noise, and subjects wear protective ear plugs during treatment.
Patient experience. The first rTMS session—during which the patient’s motor threshold is determined—can last up to 45 minutes. Subsequent sessions are usually 15 to 20 minutes. Patients are typically apprehensive before the first session but become more relaxed with experience and tolerate the treatments easily.
During the procedure, many patients describe a tapping sensation on the forehead, and some experience slight muscle twitching around the eye or corner of the mouth. As the coil warms, the skin it touches sometimes flushes pink, although this does not seem to bother our patients. They can return to their daily routines immediately after a session.
rTMS for major depression. In our experience, rTMS may help patients with major depression. For example, one patient diagnosed with a major depressive episode with psychotic features was referred to our study comparing rTMS with ECT.19 Her depression had lasted several months, with partial response to ECT treatments. She signed informed consent and was randomly assigned to receive rTMS treatment.
At study admission, the patient’s Hamilton Depression Rating Scale (HDRS) score was 48, indicating moderate to severe depression. Following 10 rTMS sessions, her HDRS score had dropped to 2, with remission of symptoms. No follow-up results were documented.
Cognitive effects. Whereas mood disorders are associated with medication-independent neuropsychological deficits, most studies have found no adverse cognitive effects with rTMS.22 Indeed, some of our rTMS patients have improved in certain cognitive tests, although this may be explained by test-retest effects or better attention and concentration associated with mood improvement.
Figure Potential roles for rTMS in treating major depression
Solid lines represent current standards of practice. Dotted lines represent hypothetical roles for rTMS.
Source: Adapted and reprinted with permission from Dowd et al. Is repetitive transcranial magnetic stimulation an alternative to ECTfor the treatment of depression? Contemp Psychiatry 2002;1:1-10.
POTENTIAL ROLE FOR rTMS
Today’s standard treatment of major depressive episodes begins with an antidepressant (plus an antipsychotic, if necessary) and proceeds to augmentation strategies if response is insufficient. rTMS may one day become an augmentation or monotherapy option for patients who do not respond sufficiently to standard treatments (Figure).
ECT treatment may be initiated if a patient has had a prior good response to ECT, is intolerant to medication, or prefers ECT. In that case, rTMS may be used as an alternate initial treatment or with ECT. Thus, rTMS may be used:
- to augment antidepressants
- as an alternative to antidepressants or ECT
- or sequentially with ECT.
Before that can happen, however, optimal treatment parameters need to be clarified by larger, well-designed, controlled studies comparing rTMS to a valid sham treatment, antidepressants, and ECT.
Related resources
- International Society for Transcranial Stimulation. www.ists.unibe.ch/
- Repetitive Transcranial Magnetic Stimulation Research Clinic at Yale-New Haven Psychiatric Hospital.
Disclosure
The authors report that they have no proprietary interest in the technology discussed in this article.
Using magnets to improve health is sometimes hawked in dubious classified ads and “infomercials.” However, a legitimate use of magnetism—repetitive transcranial magnetic stimulation (rTMS)—is showing promise in treating severe depression (Box) 1-4 and other psychiatric disorders.
Patients or their families are likely to ask psychiatrists about rTMS as more becomes known about this investigational technology. Drawing from our experience and the evidence, we offer an update on whether rTMS may be an alternative for treating depression and address issues that must be resolved before it could be used in clinical practice.
WHAT IS RTMS?
rTMS consists of a series of magnetic pulses produced by a stimulator, which can be adjusted for:
- coil type and placement
- stimulation site, intensity, frequency, and number
- amount of time between stimulations
- treatment duration.
In 1985, Barker and colleagues developed single-pulse transcranial magnetic stimulation to examine motor cortex function.1 The single-pulse mechanism they discovered was subsequently adapted to deliver repetitive pulses and is referred to as repetitive transcranial magnetic stimulation (rTMS).
How rTMS works. Transcranial magnetic stimulation uses an electromagnetic coil applied to the head to produce an intense, localized, fluctuating magnetic field that passes unimpeded into a small area of the brain, inducing an electrical current. This results in neuronal depolarization in a localized area under the coil, and possibly distal effects as well.2 During the neurophysiological studies, it was discovered that subjects also experienced a change in mood.
Antidepressant effects. Similar physiologic effects induced by rTMS, electroconvulsive therapy (ECT), and antidepressants on the endocrine system, sleep parameters, and biochemical measures suggest antidepressant properties.3 In 1993, the first published study examining rTMS in psychiatric patients reported reduced depressive symptoms in two subjects.4 Since then, several clinical trials have examined rTMS’ antidepressive effects. In 2001, Canada’s Health Ministry approved rTMS for treating major depression. In the United States, rTMS remains investigational and is FDA-approved only for clinical trials.
Coil type and placement. Initial studies involved stimulation—typically low-frequency—over the vertex, but most subsequent rTMS trials in depression have stimulated the left dorsolateral prefrontal cortex. Neuroimaging studies have shown prefrontal functioning abnormalities in depressed subjects, and it is hypothesized that stimulating this area (plus possible distal effects) may produce an antidepressant effect.5
Various configurations have been used, but circular and figure-eight-shaped coils are most common. These flat coils are made of tightly wound ferromagnetic material such as copper, enclosed in a heavy plastic cover. With the figure-eight coil, the intersection of the two loops produces the strongest magnetic field.
Stimulation site. Stimulation intensity depends on the individual’s motor threshold, and the site can be determined visually or electrophysiologically.
- With the visual method, the motor threshold over the left primary motor cortex site for the first dorsal interosseous muscle (FDI) or the abductor pollius brevis (APB) is determined by iteration. This involves placing the coil at a progression of sites and increasing stimulation intensity until reliable (in 5 of 10 stimulations) contractions are seen in the right FDI or APB.
- Similarly, the electrophysiologic method uses 5 of 10 motorevoked potentials of 50 microvolts to locate the site.
The only small trial that compared visual and electrophysiologic site determination showed similar results with both methods.6 The most common stimulation site is the left dorsolateral prefrontal cortex, 5 cm anterior and parasagittal to the FDI or APB motor cortex. Alternately, frameless stereotactic systems or the international 10-20 proportional system used in EEG labs have been recommended to target sites more accurately.
Stimulus intensity. Each individual’s motor threshold determines stimulus intensity. Using functional MRI studies, researchers from the Medical University of South Carolina concluded that higher stimulation intensity relative to the motor threshold may have a more robust effect, as the magnetic field declines with distance from the coil.7 However, intensities >120% of the motor threshold are generally avoided because of possible increased seizure risk.9
Frequency of stimulation. Most researchers apply frequencies of 1 to 20 Hz over the left dorsolateral prefrontal cortex, but also use lower frequencies (<1 Hz) over the right dorsolateral prefrontal cortex. Using higher frequencies in major depression is attractive in theory because of:
- the reported association of decreased regional cerebral blood flow with hypometabolism in the left dorsolateral prefrontal cortex
- higher-frequency stimulation’s ability to produce temporary excitation and neuronal depolarization.
Number of stimulations. The number of stimulations is determined by frequency (Hz) and stimulation train duration (for example, 10 Hz for 5 seconds equals 50 stimulations). A typical treatment session incorporates 10 to 30 stimulation trains several seconds apart (the inter-train interval). Thus, a typical session delivers 1,000 to 1,200 stimulations. In studies of unmedicated depressed patients, the total number of stimulations has varied from 8,000 to 32,000 per treatment course.
Duration between two stimulation trains. Chen et al have demonstrated that shorter (<1 second) inter-train intervals increase seizure risk with higher frequencies (such as 20 Hz) and intensities (>100% of motor threshold) of stimulation.9 Based on their studies with healthy volunteers, they recommended several “safe” ranges (such as 5 seconds at 110% of motor threshold). Most trials use 30- to 60-second inter-train intervals.
Most treatments continue 2 to 4 weeks, Monday through Friday, although more frequent treatments are being studied.
EFFICACY FOR DEPRESSION
Most studies of rTMS in depression have compared real rTMS to a sham control or electroconvulsive therapy (ECT).
In earlier studies, the sham procedure typically involved tilting the coil away from the skull. This method has been questioned, however, because of evidence of neuronal depolarization.10
More recent sham coils mimic the real coils’ sound and sensation, without magnetic stimulation.
Despite these methodologic problems and some mixed results, depressed patients receiving rTMS show more favorable results than those receiving sham rTMS.11,12 Several meta-analyses have attempted to quantify rTMS’ efficacy for depression:
- Holtzheimer et al concluded that rTMS was statistically superior to sham rTMS, but the clinical significance of these findings was modest in a population of mostly outpatients with less-severe depression.13
- Burt et al found a statistically strong antidepressant effect, but its magnitude varied and few of the studies yielded a substantial clinical response or remission. The team also noted that rTMS’ long-term efficacy or adverse effects are unknown.14
- Kozel et al concluded that left prefrontal rTMS rendered a significant antidepressant effect with measurable clinical improvement.15
- Gershon et al16 supported an antidepressant effect for rTMS when compared with sham rTMS or ECT.
Ongoing rTMS research includes subjects with many types of mild to severe psychiatric illnesses, including major depression, obsessive-compulsive disorder, and psychosis. Typically, patients referred for experimental approaches have not responded to or tolerated available treatments. Exclusion criteria used by most rTMS studies are listed in the Table.
Table
Medical conditions that preclude use of rTMS
| Serious medical conditions History of seizures Increased intracranial pressure Serious head trauma |
| Myocardial infarction within the past 6 months |
| Pregnancy or childbearing potential (unless reliable contraception is being used) |
| Intracranial metallic implants |
| Pacemakers or other implanted devices |
rTMS vs. ECT. Four randomized, controlled trials have compared rTMS with ECT for treating severely ill, often medication-resistant patients.17-20 Although their methodologies differed, all four studies concluded that rTMS and ECT offer similar efficacy, except that rTMS may be less effective for treating psychotic depression.
One study found ECT more effective than rTMS for psychotic depression, although the patients who received ECT were also treated with antipsychotics and/or antidepressants.17 Our study,19 which did not use these agents, has not corroborated this observation. Preliminary data also indicate comparable relapse rates following acute ECT and rTMS when subjects are followed on maintenance medication.21
ADVERSE EFFECTS
The potential adverse effects of new treatments must always be considered. Thus far, rTMS appears to produce minimal, relatively benign complications, including:
- mild discomfort at the stimulation site
- localized muscle twitching during stimulation
- mild post-treatment headaches—believed caused by muscle contractions—which usually respond to aspirin or acetaminophen
- treatment stimulation-related seizures (rarely).8
The rTMS device makes a loud clicking noise, and subjects wear protective ear plugs during treatment.
Patient experience. The first rTMS session—during which the patient’s motor threshold is determined—can last up to 45 minutes. Subsequent sessions are usually 15 to 20 minutes. Patients are typically apprehensive before the first session but become more relaxed with experience and tolerate the treatments easily.
During the procedure, many patients describe a tapping sensation on the forehead, and some experience slight muscle twitching around the eye or corner of the mouth. As the coil warms, the skin it touches sometimes flushes pink, although this does not seem to bother our patients. They can return to their daily routines immediately after a session.
rTMS for major depression. In our experience, rTMS may help patients with major depression. For example, one patient diagnosed with a major depressive episode with psychotic features was referred to our study comparing rTMS with ECT.19 Her depression had lasted several months, with partial response to ECT treatments. She signed informed consent and was randomly assigned to receive rTMS treatment.
At study admission, the patient’s Hamilton Depression Rating Scale (HDRS) score was 48, indicating moderate to severe depression. Following 10 rTMS sessions, her HDRS score had dropped to 2, with remission of symptoms. No follow-up results were documented.
Cognitive effects. Whereas mood disorders are associated with medication-independent neuropsychological deficits, most studies have found no adverse cognitive effects with rTMS.22 Indeed, some of our rTMS patients have improved in certain cognitive tests, although this may be explained by test-retest effects or better attention and concentration associated with mood improvement.
Figure Potential roles for rTMS in treating major depression
Solid lines represent current standards of practice. Dotted lines represent hypothetical roles for rTMS.
Source: Adapted and reprinted with permission from Dowd et al. Is repetitive transcranial magnetic stimulation an alternative to ECTfor the treatment of depression? Contemp Psychiatry 2002;1:1-10.
POTENTIAL ROLE FOR rTMS
Today’s standard treatment of major depressive episodes begins with an antidepressant (plus an antipsychotic, if necessary) and proceeds to augmentation strategies if response is insufficient. rTMS may one day become an augmentation or monotherapy option for patients who do not respond sufficiently to standard treatments (Figure).
ECT treatment may be initiated if a patient has had a prior good response to ECT, is intolerant to medication, or prefers ECT. In that case, rTMS may be used as an alternate initial treatment or with ECT. Thus, rTMS may be used:
- to augment antidepressants
- as an alternative to antidepressants or ECT
- or sequentially with ECT.
Before that can happen, however, optimal treatment parameters need to be clarified by larger, well-designed, controlled studies comparing rTMS to a valid sham treatment, antidepressants, and ECT.
Related resources
- International Society for Transcranial Stimulation. www.ists.unibe.ch/
- Repetitive Transcranial Magnetic Stimulation Research Clinic at Yale-New Haven Psychiatric Hospital.
Disclosure
The authors report that they have no proprietary interest in the technology discussed in this article.
1. Barker A, Jalinous R, Freeston I. Non-invasive magnetic stimulation of human motor cortex. Lancet 1985;1:1106-7.
2. Lisanby SH, Datto CJ, Szuba MP. ECT and rTMS: past, present, and future. Depress Anxiety 2000;12:115-17.
3. Post A, Keck PE, Jr. Transcranial magnetic stimulation as a therapeutic tool in psychiatry: what do we know about the neurobiological mechanisms? J Psychiatr Res 2001;35:193-215.
4. Holfich G, Kasper S, Hufnagel A, et al. Application of transcranial magnetic stimulation in treatment of drug resistant major depression—a report of two cases. Human Psychopharmacol 1993;8:361-5.
5. George MS, Nahas Z, Speer AM, et al. Transcranial magnetic stimulation—a new method for investigating the neuroanatomy of depression. In: Ebert D, Ebmeier K (eds). New models for depression. New York: Karger, 1998;94-122.
6. Pridmore A, Americo Fernandes Filho J, Nahas Z, et al. Motor threshold in transcranial magnetic stimulation: a comparison of a neurophysiological method and a visualization of movement method. J ECT 1998;14(1):25-7.
7. Kozel FA, Nahas Z, deBrux C, et al. How coil-cortex distance relates to age, motor threshold, and antidepressant response to repetitive transcranial magnetic stimulation. J Neuropsychiatry Clin Neurosci 2000;13:376-84.
8. Wassermann EM. Risk and safety of repetitive transcranial magnetic stimulation: report and suggested guidelines from the International Workshop on the Safety of Repetitive Transcranial Magnetic Stimulation, 1996. Electroencephalogr Clin Neurophysiol 1998;108:1-16.
9. Chen R, Gerloff C, Classen J, et al. Safety of different inter-train intervals for repetitive transcranial magnetic stimulation and recommendations for safe ranges of stimulation parameters. Electroencephalogr Clin Neurophysiol 1997;105:415-21.
10. Loo CK, Taylor JL, Gandevia SC, et al. Transcranial magnetic stimulation in controlled treatment studies: Are some “sham” forms active? Biol Psychiatry. 2000;47:325-31.
11. George MS, Nahas Z, Molloy M, et al. A controlled trial of daily left prefrontal cortex TMS for treating depression. Biol Psychiatry 2000;48:962-70.
12. Berman RM, Narasimhan M, Sanacora G, et al. A randomized clinical trial of repetitive transcranial magnetic stimulation in the treatment of major depression. Biol Psychiatry 2000;47:332-7.
13. Holtzheimer PE, Russo J, Avery D. A meta-analysis of repetitive transcranial magnetic stimulation in the treatment of depression. Psychopharmacol Bull 2001;35:149-69.
14. Burt T, Lisanby SH, Sackeim HA. Neuropsychiatric applications of transcranial magnetic stimulation: a meta-analysis. Int J Neuropsychopharmacol 2002;5:73-103.
15. Kozel FE, George MS. Meta-analysis of left prefrontal repetitive transcranial magnetic stimulation (rTMS) to treat depression. J Psychiatr Pract 2002;8:270-5.
16. Gershon AA, Dannon PN, Grunhaus L. Transcranial magnetic stimulation in the treatment of depression. Am JPsychiatry 2003;160(5):835-45.
17. Grunhaus L, Dannon PN, Schreiber S, et al. Repetitive transcranial magnetic stimulation is as effective as electroconvulsive therapy in the treatment of nondelusional major depressive disorder: an open study. Biol Psychiatry 2000;47:314-24.
18. Pridmore S, Bruno R, Turnier-Shea Y, et al. Comparison of unlimited numbers of rapid transcranial magnetic stimulation and ECT treatment sessions in major depression episodes. Int J Neuropsychopharmacol 2000;3:129-34.
19. Janicak PG, Dowd SM, Martis B, et al. Repetitive transcranial magnetic stimulation versus electroconvulsive therapy for major depression: preliminary results of a randomized trial. Biol Psychiatry 2002;51:659-67
20. Grunhaus L, Schreiber S, Dolberg OT, et al. A randomized controlled comparison of electroconvulsive therapy and repetitive transcranial magnetic stimulation in severe and resistant nonpsychotic major depression. Biol Psychiatry 2003;53:324-31.
21. Dannon PH, Dolberg OT, Schreiber S, Grunhaus L. Three and six month outcome following courses of either ECT or rTMS in a population of severely depressed individuals—preliminary report. Biol Psychiatry 2002;15:687-90.
22. Martis B, Alam D, Dowd SM, et al. Neurocognitive effects of repetitive transcranial magnetic stimulation in severe major depression. Clin Neurophysiology (in press).
1. Barker A, Jalinous R, Freeston I. Non-invasive magnetic stimulation of human motor cortex. Lancet 1985;1:1106-7.
2. Lisanby SH, Datto CJ, Szuba MP. ECT and rTMS: past, present, and future. Depress Anxiety 2000;12:115-17.
3. Post A, Keck PE, Jr. Transcranial magnetic stimulation as a therapeutic tool in psychiatry: what do we know about the neurobiological mechanisms? J Psychiatr Res 2001;35:193-215.
4. Holfich G, Kasper S, Hufnagel A, et al. Application of transcranial magnetic stimulation in treatment of drug resistant major depression—a report of two cases. Human Psychopharmacol 1993;8:361-5.
5. George MS, Nahas Z, Speer AM, et al. Transcranial magnetic stimulation—a new method for investigating the neuroanatomy of depression. In: Ebert D, Ebmeier K (eds). New models for depression. New York: Karger, 1998;94-122.
6. Pridmore A, Americo Fernandes Filho J, Nahas Z, et al. Motor threshold in transcranial magnetic stimulation: a comparison of a neurophysiological method and a visualization of movement method. J ECT 1998;14(1):25-7.
7. Kozel FA, Nahas Z, deBrux C, et al. How coil-cortex distance relates to age, motor threshold, and antidepressant response to repetitive transcranial magnetic stimulation. J Neuropsychiatry Clin Neurosci 2000;13:376-84.
8. Wassermann EM. Risk and safety of repetitive transcranial magnetic stimulation: report and suggested guidelines from the International Workshop on the Safety of Repetitive Transcranial Magnetic Stimulation, 1996. Electroencephalogr Clin Neurophysiol 1998;108:1-16.
9. Chen R, Gerloff C, Classen J, et al. Safety of different inter-train intervals for repetitive transcranial magnetic stimulation and recommendations for safe ranges of stimulation parameters. Electroencephalogr Clin Neurophysiol 1997;105:415-21.
10. Loo CK, Taylor JL, Gandevia SC, et al. Transcranial magnetic stimulation in controlled treatment studies: Are some “sham” forms active? Biol Psychiatry. 2000;47:325-31.
11. George MS, Nahas Z, Molloy M, et al. A controlled trial of daily left prefrontal cortex TMS for treating depression. Biol Psychiatry 2000;48:962-70.
12. Berman RM, Narasimhan M, Sanacora G, et al. A randomized clinical trial of repetitive transcranial magnetic stimulation in the treatment of major depression. Biol Psychiatry 2000;47:332-7.
13. Holtzheimer PE, Russo J, Avery D. A meta-analysis of repetitive transcranial magnetic stimulation in the treatment of depression. Psychopharmacol Bull 2001;35:149-69.
14. Burt T, Lisanby SH, Sackeim HA. Neuropsychiatric applications of transcranial magnetic stimulation: a meta-analysis. Int J Neuropsychopharmacol 2002;5:73-103.
15. Kozel FE, George MS. Meta-analysis of left prefrontal repetitive transcranial magnetic stimulation (rTMS) to treat depression. J Psychiatr Pract 2002;8:270-5.
16. Gershon AA, Dannon PN, Grunhaus L. Transcranial magnetic stimulation in the treatment of depression. Am JPsychiatry 2003;160(5):835-45.
17. Grunhaus L, Dannon PN, Schreiber S, et al. Repetitive transcranial magnetic stimulation is as effective as electroconvulsive therapy in the treatment of nondelusional major depressive disorder: an open study. Biol Psychiatry 2000;47:314-24.
18. Pridmore S, Bruno R, Turnier-Shea Y, et al. Comparison of unlimited numbers of rapid transcranial magnetic stimulation and ECT treatment sessions in major depression episodes. Int J Neuropsychopharmacol 2000;3:129-34.
19. Janicak PG, Dowd SM, Martis B, et al. Repetitive transcranial magnetic stimulation versus electroconvulsive therapy for major depression: preliminary results of a randomized trial. Biol Psychiatry 2002;51:659-67
20. Grunhaus L, Schreiber S, Dolberg OT, et al. A randomized controlled comparison of electroconvulsive therapy and repetitive transcranial magnetic stimulation in severe and resistant nonpsychotic major depression. Biol Psychiatry 2003;53:324-31.
21. Dannon PH, Dolberg OT, Schreiber S, Grunhaus L. Three and six month outcome following courses of either ECT or rTMS in a population of severely depressed individuals—preliminary report. Biol Psychiatry 2002;15:687-90.
22. Martis B, Alam D, Dowd SM, et al. Neurocognitive effects of repetitive transcranial magnetic stimulation in severe major depression. Clin Neurophysiology (in press).