User login
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record. However, there are instances when the majority of the encounter constitutes counseling/coordination of care (C/CC). Physicians might only document a brief history and exam, or nothing at all. Utilizing time-based billing principles allows a physician to disregard the “key component” requirements and select a visit level reflective of this effort.
For example, a 64-year-old female is hospitalized with newly diagnosed diabetes and requires extensive counseling regarding disease management, lifestyle modification, and medication regime, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient and leaves the room to coordinate the patient’s ongoing care (25 minutes). The hospitalist then asks a resident to assist with the remaining counseling efforts (20 minutes). Code 99232 (inpatient visit, 25 minutes total visit time) would be appropriate to report.
Counseling, Coordination of Care
Time may be used as the determining factor for the visit level, if more than 50% of the total visit time involves C/CC.1 Time is not used for visit-level selection if C/CC is minimal or absent from the patient encounter. Total visit time is acknowledged as the physician’s face-to-face (i.e. bedside) time combined with time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the individual case with other involved healthcare providers.
Time associated with activities performed outside of the patient’s unit/floor is not considered when calculating total visit time. Time associated with teaching students/interns also is excluded; only the attending physician’s time counts.
When the requirements have been met, the physician selects the visit level that corresponds with the documented total visit time (see Table 1). In the scenario above, the visit level is chosen based on the attending physician’s documented time (25 minutes). The resident’s time cannot be included.
Documentation Requirements
Physicians must document the interaction during the patient encounter: history and exam, if updated or performed; discussion points; and patient response, if applicable. The medical record entry must contain both the C/CC time and the total visit time.2 “Total visit time=35 minutes; >50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payor may prefer one documentation style over another. It is always best to ask about the payor’s policy and review local documentation standards to ensure compliance.
Family Discussions
Physicians are always involved in family discussions. It is appropriate to count this as C/CC time. In the event that the family discussion takes place without the patient present, only count this as C/CC time if:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision-makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.4
The medical record should reflect these criteria. Do not consider the time if the discussion takes place in an area outside of the patient’s unit/floor, or if the time is spent counseling family members through their grieving process.
It is not uncommon for the family discussion to take place later in the day, after the physician has made earlier rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient evaluation (i.e. history update and physical) and management service (i.e. care plan review/revision), this second encounter might be regarded as a prolonged care service.
Prolonged Care
Prolonged care codes exist for both outpatient and inpatient services. A hospitalists’ focus involves the inpatient code series:
99356: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, first hour; and
99357: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, each additional 30 minutes.
Code 99356 is reported during the first hour of prolonged services, after the initial 30 minutes is reached; code 99357 is reported for each additional 30 minutes of prolonged care beyond the first hour, after the first 15 minutes of each additional segment. Both are “add on” codes and cannot be reported alone on a claim form; a “primary” code must be reported. Similarly, 99357 cannot be reported without 99356, and 99356 must be reported with one of the following inpatient service (primary) codes: 99218-99220, 99221-99223, 99231-99233, 99251-99255, 99304-99310. Only one unit of 99356 may be reported per patient per physician group per day, whereas multiple units of 99357 may be reported in a single day.
The CPT definition of prolonged care varies from that of the Centers for Medicare & Medicaid Services (CMS). Since 2009, CPT recognizes the total duration spent by a physician on a given date, even if the time spent by the physician on that date is not continuous; the time involves both face-to-face time and unit/floor time.5 CMS only attributes direct face-to-face time between the physician and the patient toward prolonged care billing. Time spent reviewing charts or discussion of a patient with house medical staff, waiting for test results, waiting for changes in the patient’s condition, waiting for end of a therapy session, or waiting for use of facilities cannot be billed as prolonged services.5 This is in direct opposition to its policy for C/CC services, and makes prolonged care services inefficient.
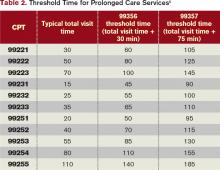
Medicare also identifies “threshold” time (see Table 2). The total physician visit time must exceed the time requirements associated with the “primary” codes by a 30-minute threshold (e.g. 99221+99356=30 minutes+30 minutes=60 minutes threshold time). The physician must document the total face-to-face time spent in separate notes throughout the day or, more realistically, in one cumulative note.
When two providers from the same group and same specialty perform services on the same date (e.g. physician A saw the patient during morning rounds, and physician B spoke with the patient/family in the afternoon), only one physician can report the cumulative service.6 As always, query payors for coverage, because some non-Medicare insurers do not recognize these codes.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare National Coverage Determinations Manual: Chapter 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011:7-21.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.5. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record. However, there are instances when the majority of the encounter constitutes counseling/coordination of care (C/CC). Physicians might only document a brief history and exam, or nothing at all. Utilizing time-based billing principles allows a physician to disregard the “key component” requirements and select a visit level reflective of this effort.
For example, a 64-year-old female is hospitalized with newly diagnosed diabetes and requires extensive counseling regarding disease management, lifestyle modification, and medication regime, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient and leaves the room to coordinate the patient’s ongoing care (25 minutes). The hospitalist then asks a resident to assist with the remaining counseling efforts (20 minutes). Code 99232 (inpatient visit, 25 minutes total visit time) would be appropriate to report.
Counseling, Coordination of Care
Time may be used as the determining factor for the visit level, if more than 50% of the total visit time involves C/CC.1 Time is not used for visit-level selection if C/CC is minimal or absent from the patient encounter. Total visit time is acknowledged as the physician’s face-to-face (i.e. bedside) time combined with time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the individual case with other involved healthcare providers.
Time associated with activities performed outside of the patient’s unit/floor is not considered when calculating total visit time. Time associated with teaching students/interns also is excluded; only the attending physician’s time counts.
When the requirements have been met, the physician selects the visit level that corresponds with the documented total visit time (see Table 1). In the scenario above, the visit level is chosen based on the attending physician’s documented time (25 minutes). The resident’s time cannot be included.
Documentation Requirements
Physicians must document the interaction during the patient encounter: history and exam, if updated or performed; discussion points; and patient response, if applicable. The medical record entry must contain both the C/CC time and the total visit time.2 “Total visit time=35 minutes; >50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payor may prefer one documentation style over another. It is always best to ask about the payor’s policy and review local documentation standards to ensure compliance.
Family Discussions
Physicians are always involved in family discussions. It is appropriate to count this as C/CC time. In the event that the family discussion takes place without the patient present, only count this as C/CC time if:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision-makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.4
The medical record should reflect these criteria. Do not consider the time if the discussion takes place in an area outside of the patient’s unit/floor, or if the time is spent counseling family members through their grieving process.
It is not uncommon for the family discussion to take place later in the day, after the physician has made earlier rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient evaluation (i.e. history update and physical) and management service (i.e. care plan review/revision), this second encounter might be regarded as a prolonged care service.
Prolonged Care
Prolonged care codes exist for both outpatient and inpatient services. A hospitalists’ focus involves the inpatient code series:
99356: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, first hour; and
99357: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, each additional 30 minutes.
Code 99356 is reported during the first hour of prolonged services, after the initial 30 minutes is reached; code 99357 is reported for each additional 30 minutes of prolonged care beyond the first hour, after the first 15 minutes of each additional segment. Both are “add on” codes and cannot be reported alone on a claim form; a “primary” code must be reported. Similarly, 99357 cannot be reported without 99356, and 99356 must be reported with one of the following inpatient service (primary) codes: 99218-99220, 99221-99223, 99231-99233, 99251-99255, 99304-99310. Only one unit of 99356 may be reported per patient per physician group per day, whereas multiple units of 99357 may be reported in a single day.
The CPT definition of prolonged care varies from that of the Centers for Medicare & Medicaid Services (CMS). Since 2009, CPT recognizes the total duration spent by a physician on a given date, even if the time spent by the physician on that date is not continuous; the time involves both face-to-face time and unit/floor time.5 CMS only attributes direct face-to-face time between the physician and the patient toward prolonged care billing. Time spent reviewing charts or discussion of a patient with house medical staff, waiting for test results, waiting for changes in the patient’s condition, waiting for end of a therapy session, or waiting for use of facilities cannot be billed as prolonged services.5 This is in direct opposition to its policy for C/CC services, and makes prolonged care services inefficient.
Medicare also identifies “threshold” time (see Table 2). The total physician visit time must exceed the time requirements associated with the “primary” codes by a 30-minute threshold (e.g. 99221+99356=30 minutes+30 minutes=60 minutes threshold time). The physician must document the total face-to-face time spent in separate notes throughout the day or, more realistically, in one cumulative note.
When two providers from the same group and same specialty perform services on the same date (e.g. physician A saw the patient during morning rounds, and physician B spoke with the patient/family in the afternoon), only one physician can report the cumulative service.6 As always, query payors for coverage, because some non-Medicare insurers do not recognize these codes.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare National Coverage Determinations Manual: Chapter 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011:7-21.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.5. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record. However, there are instances when the majority of the encounter constitutes counseling/coordination of care (C/CC). Physicians might only document a brief history and exam, or nothing at all. Utilizing time-based billing principles allows a physician to disregard the “key component” requirements and select a visit level reflective of this effort.
For example, a 64-year-old female is hospitalized with newly diagnosed diabetes and requires extensive counseling regarding disease management, lifestyle modification, and medication regime, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient and leaves the room to coordinate the patient’s ongoing care (25 minutes). The hospitalist then asks a resident to assist with the remaining counseling efforts (20 minutes). Code 99232 (inpatient visit, 25 minutes total visit time) would be appropriate to report.
Counseling, Coordination of Care
Time may be used as the determining factor for the visit level, if more than 50% of the total visit time involves C/CC.1 Time is not used for visit-level selection if C/CC is minimal or absent from the patient encounter. Total visit time is acknowledged as the physician’s face-to-face (i.e. bedside) time combined with time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the individual case with other involved healthcare providers.
Time associated with activities performed outside of the patient’s unit/floor is not considered when calculating total visit time. Time associated with teaching students/interns also is excluded; only the attending physician’s time counts.
When the requirements have been met, the physician selects the visit level that corresponds with the documented total visit time (see Table 1). In the scenario above, the visit level is chosen based on the attending physician’s documented time (25 minutes). The resident’s time cannot be included.
Documentation Requirements
Physicians must document the interaction during the patient encounter: history and exam, if updated or performed; discussion points; and patient response, if applicable. The medical record entry must contain both the C/CC time and the total visit time.2 “Total visit time=35 minutes; >50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payor may prefer one documentation style over another. It is always best to ask about the payor’s policy and review local documentation standards to ensure compliance.
Family Discussions
Physicians are always involved in family discussions. It is appropriate to count this as C/CC time. In the event that the family discussion takes place without the patient present, only count this as C/CC time if:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision-makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.4
The medical record should reflect these criteria. Do not consider the time if the discussion takes place in an area outside of the patient’s unit/floor, or if the time is spent counseling family members through their grieving process.
It is not uncommon for the family discussion to take place later in the day, after the physician has made earlier rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient evaluation (i.e. history update and physical) and management service (i.e. care plan review/revision), this second encounter might be regarded as a prolonged care service.
Prolonged Care
Prolonged care codes exist for both outpatient and inpatient services. A hospitalists’ focus involves the inpatient code series:
99356: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, first hour; and
99357: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, each additional 30 minutes.
Code 99356 is reported during the first hour of prolonged services, after the initial 30 minutes is reached; code 99357 is reported for each additional 30 minutes of prolonged care beyond the first hour, after the first 15 minutes of each additional segment. Both are “add on” codes and cannot be reported alone on a claim form; a “primary” code must be reported. Similarly, 99357 cannot be reported without 99356, and 99356 must be reported with one of the following inpatient service (primary) codes: 99218-99220, 99221-99223, 99231-99233, 99251-99255, 99304-99310. Only one unit of 99356 may be reported per patient per physician group per day, whereas multiple units of 99357 may be reported in a single day.
The CPT definition of prolonged care varies from that of the Centers for Medicare & Medicaid Services (CMS). Since 2009, CPT recognizes the total duration spent by a physician on a given date, even if the time spent by the physician on that date is not continuous; the time involves both face-to-face time and unit/floor time.5 CMS only attributes direct face-to-face time between the physician and the patient toward prolonged care billing. Time spent reviewing charts or discussion of a patient with house medical staff, waiting for test results, waiting for changes in the patient’s condition, waiting for end of a therapy session, or waiting for use of facilities cannot be billed as prolonged services.5 This is in direct opposition to its policy for C/CC services, and makes prolonged care services inefficient.
Medicare also identifies “threshold” time (see Table 2). The total physician visit time must exceed the time requirements associated with the “primary” codes by a 30-minute threshold (e.g. 99221+99356=30 minutes+30 minutes=60 minutes threshold time). The physician must document the total face-to-face time spent in separate notes throughout the day or, more realistically, in one cumulative note.
When two providers from the same group and same specialty perform services on the same date (e.g. physician A saw the patient during morning rounds, and physician B spoke with the patient/family in the afternoon), only one physician can report the cumulative service.6 As always, query payors for coverage, because some non-Medicare insurers do not recognize these codes.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare National Coverage Determinations Manual: Chapter 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011:7-21.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.5. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.