User login
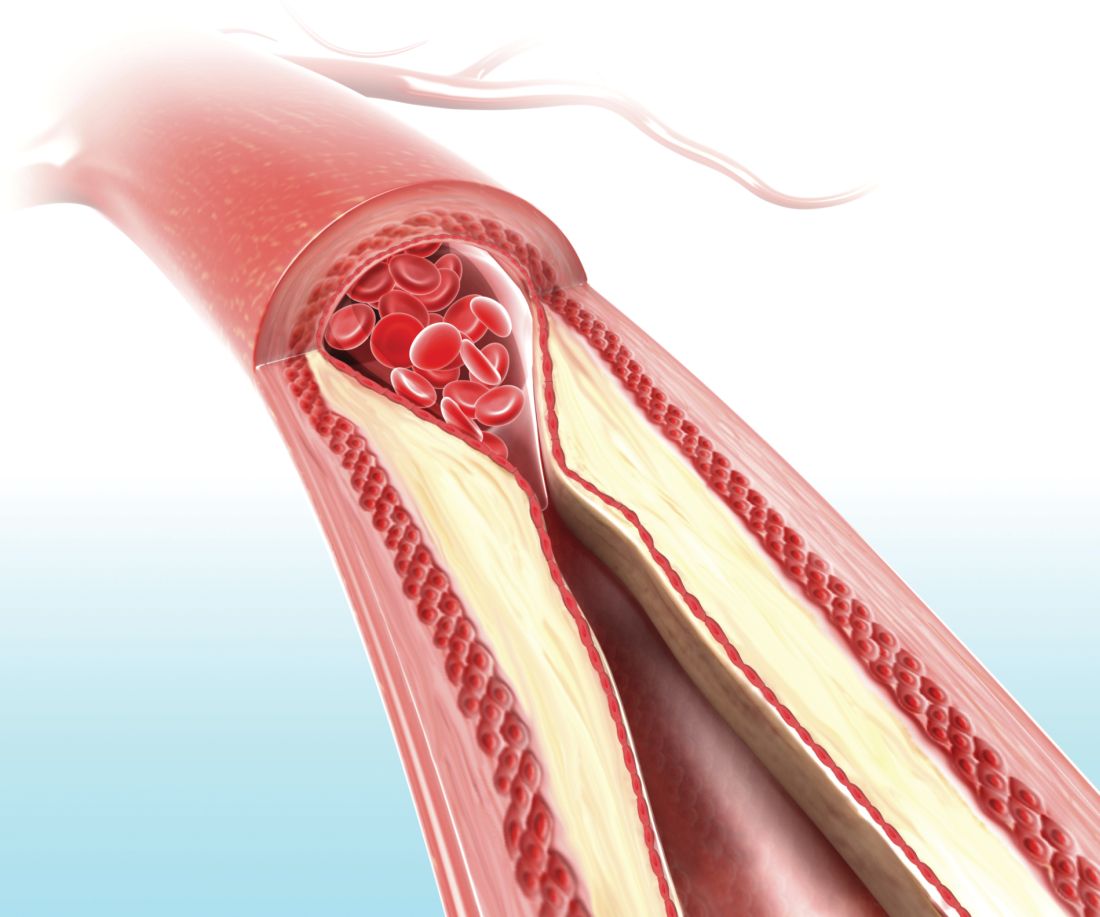
A pictorial representation of carotid ultrasound coupled with a follow-up phone call from a nurse led to reduced cardiovascular disease risk at 1-year follow-up, according to a randomized, controlled study of northern Sweden residents at risk of cardiovascular disease.
“Our study supports further attempts to solve the major problem of prevention failure because of low adherence, despite effective, cost-effective, and evidence-based medications and methods for a healthier lifestyle,” wrote lead author Ulf Näslund, of Umeå (Sweden) University, and his coauthors. The study was published online in the Lancet.
In this trial of 3,532 individuals who were aged 40-60 years with one or more conventional cardiovascular risk factors, the intervention group (1,749) received pictorial information of atherosclerosis as an add-on to normal care. Their primary care physician received the same information, and these participants also received a follow-up phone call from a nurse 2-4 weeks later. The other participants (1,783) received standard care but neither the presentation nor the phone call.
Both the Framingham risk score (FRS) and European Systematic Coronary Risk Evaluation (SCORE) were both used to assess outcomes; at 1-year follow-up, the intervention group had an FRS that decreased from baseline (–0.58; 95% confidence interval, –0.86 to –0.30), compared with an increase in the control group (0.35; 95% CI, 0.08-0.63). SCORE values increased twice as much in the control group (0.27; 95% CI, 0.23-0.30), compared with the intervention group (0.13; 95% CI, 0.09-0.18). The authors also observed no differential responses for education level, surmising that “this type of risk communication might contribute to reduction of the social gap in health.”
The authors shared their study’s limitations, including notable differences between dropouts and participants at 1-year follow-up with regard to metabolic risk factors and such fast-developing imaging technologies as CT and MRI out-dating ultrasound findings. They also acknowledged that more research needs to be undertaken to prove that these outcomes are genuine.
This study was funded by Västerbotten County Council, the Swedish Research Council, the Heart and Lung Foundation, and the Swedish Society of Medicine. No conflicts of interest were reported.
SOURCE: Näslund U et al. Lancet. 2018 Dec 3. doi: 10.1016/S0140-6736(18)32818-6.
Though improving adherence and outcomes has long eluded clinicians and researchers, this study by Näslund and colleagues provides optimism that cardiovascular risk can be mitigated through educational and motivational factors, according to Richard Kones, MD, of the Cardiometabolic Research Institute in Houston; Umme Rumana, MBBS, of the University of Texas at Houston and the New York Institute of Technology in Old Westbury; and Alberto Morales-Salinas, MD, of the Cardiocentro Ernesto Che Guevara in Villa Clara, Cuba.
The three authors underlined the struggles that low- and middle-income countries go through in terms of “poor adherence and uneven availability and access” for those with high cardiovascular risk; even richer countries like the United States still suffer through a high percentage of hospital admissions that stem from nonadherence to medication. As such, the work of Näslund and colleagues displays the potential of image-based information plus follow-up reinforcement in a manner not often utilized.
“The strengths of the study include size, detail, and the pragmatic, randomized, controlled trial design,” they noted, adding that few other analyses in this area are even comparable. At the same time, lack of resources — including access to transportation and medication — may limit the effectiveness of motivation, especially since the United States differs in prices and health disparities as compared to the study’s Swedish populace.
Coronary heart disease remains one of the world’s leading causes of deaths, and higher adherence will likely lead to “drastic improvements in cardiovascular outcomes.” Yet the three authors state that more research needs to be done to quantify the exact impact of adherence in regard to medication, physical activity, or any reliever of cardiovascular risk: “Whether the results are sustainable and will reduce subsequent major adverse cardiac and cerebrovascular events requires longer follow-up.”
These comments are adapted from an accompanying editorial (Lancet. 2018 Dec 3. doi: 10.1016/S0140-6736[18]33079-4 ). The authors declared no conflict of interest.
Though improving adherence and outcomes has long eluded clinicians and researchers, this study by Näslund and colleagues provides optimism that cardiovascular risk can be mitigated through educational and motivational factors, according to Richard Kones, MD, of the Cardiometabolic Research Institute in Houston; Umme Rumana, MBBS, of the University of Texas at Houston and the New York Institute of Technology in Old Westbury; and Alberto Morales-Salinas, MD, of the Cardiocentro Ernesto Che Guevara in Villa Clara, Cuba.
The three authors underlined the struggles that low- and middle-income countries go through in terms of “poor adherence and uneven availability and access” for those with high cardiovascular risk; even richer countries like the United States still suffer through a high percentage of hospital admissions that stem from nonadherence to medication. As such, the work of Näslund and colleagues displays the potential of image-based information plus follow-up reinforcement in a manner not often utilized.
“The strengths of the study include size, detail, and the pragmatic, randomized, controlled trial design,” they noted, adding that few other analyses in this area are even comparable. At the same time, lack of resources — including access to transportation and medication — may limit the effectiveness of motivation, especially since the United States differs in prices and health disparities as compared to the study’s Swedish populace.
Coronary heart disease remains one of the world’s leading causes of deaths, and higher adherence will likely lead to “drastic improvements in cardiovascular outcomes.” Yet the three authors state that more research needs to be done to quantify the exact impact of adherence in regard to medication, physical activity, or any reliever of cardiovascular risk: “Whether the results are sustainable and will reduce subsequent major adverse cardiac and cerebrovascular events requires longer follow-up.”
These comments are adapted from an accompanying editorial (Lancet. 2018 Dec 3. doi: 10.1016/S0140-6736[18]33079-4 ). The authors declared no conflict of interest.
Though improving adherence and outcomes has long eluded clinicians and researchers, this study by Näslund and colleagues provides optimism that cardiovascular risk can be mitigated through educational and motivational factors, according to Richard Kones, MD, of the Cardiometabolic Research Institute in Houston; Umme Rumana, MBBS, of the University of Texas at Houston and the New York Institute of Technology in Old Westbury; and Alberto Morales-Salinas, MD, of the Cardiocentro Ernesto Che Guevara in Villa Clara, Cuba.
The three authors underlined the struggles that low- and middle-income countries go through in terms of “poor adherence and uneven availability and access” for those with high cardiovascular risk; even richer countries like the United States still suffer through a high percentage of hospital admissions that stem from nonadherence to medication. As such, the work of Näslund and colleagues displays the potential of image-based information plus follow-up reinforcement in a manner not often utilized.
“The strengths of the study include size, detail, and the pragmatic, randomized, controlled trial design,” they noted, adding that few other analyses in this area are even comparable. At the same time, lack of resources — including access to transportation and medication — may limit the effectiveness of motivation, especially since the United States differs in prices and health disparities as compared to the study’s Swedish populace.
Coronary heart disease remains one of the world’s leading causes of deaths, and higher adherence will likely lead to “drastic improvements in cardiovascular outcomes.” Yet the three authors state that more research needs to be done to quantify the exact impact of adherence in regard to medication, physical activity, or any reliever of cardiovascular risk: “Whether the results are sustainable and will reduce subsequent major adverse cardiac and cerebrovascular events requires longer follow-up.”
These comments are adapted from an accompanying editorial (Lancet. 2018 Dec 3. doi: 10.1016/S0140-6736[18]33079-4 ). The authors declared no conflict of interest.
A pictorial representation of carotid ultrasound coupled with a follow-up phone call from a nurse led to reduced cardiovascular disease risk at 1-year follow-up, according to a randomized, controlled study of northern Sweden residents at risk of cardiovascular disease.
“Our study supports further attempts to solve the major problem of prevention failure because of low adherence, despite effective, cost-effective, and evidence-based medications and methods for a healthier lifestyle,” wrote lead author Ulf Näslund, of Umeå (Sweden) University, and his coauthors. The study was published online in the Lancet.
In this trial of 3,532 individuals who were aged 40-60 years with one or more conventional cardiovascular risk factors, the intervention group (1,749) received pictorial information of atherosclerosis as an add-on to normal care. Their primary care physician received the same information, and these participants also received a follow-up phone call from a nurse 2-4 weeks later. The other participants (1,783) received standard care but neither the presentation nor the phone call.
Both the Framingham risk score (FRS) and European Systematic Coronary Risk Evaluation (SCORE) were both used to assess outcomes; at 1-year follow-up, the intervention group had an FRS that decreased from baseline (–0.58; 95% confidence interval, –0.86 to –0.30), compared with an increase in the control group (0.35; 95% CI, 0.08-0.63). SCORE values increased twice as much in the control group (0.27; 95% CI, 0.23-0.30), compared with the intervention group (0.13; 95% CI, 0.09-0.18). The authors also observed no differential responses for education level, surmising that “this type of risk communication might contribute to reduction of the social gap in health.”
The authors shared their study’s limitations, including notable differences between dropouts and participants at 1-year follow-up with regard to metabolic risk factors and such fast-developing imaging technologies as CT and MRI out-dating ultrasound findings. They also acknowledged that more research needs to be undertaken to prove that these outcomes are genuine.
This study was funded by Västerbotten County Council, the Swedish Research Council, the Heart and Lung Foundation, and the Swedish Society of Medicine. No conflicts of interest were reported.
SOURCE: Näslund U et al. Lancet. 2018 Dec 3. doi: 10.1016/S0140-6736(18)32818-6.
A pictorial representation of carotid ultrasound coupled with a follow-up phone call from a nurse led to reduced cardiovascular disease risk at 1-year follow-up, according to a randomized, controlled study of northern Sweden residents at risk of cardiovascular disease.
“Our study supports further attempts to solve the major problem of prevention failure because of low adherence, despite effective, cost-effective, and evidence-based medications and methods for a healthier lifestyle,” wrote lead author Ulf Näslund, of Umeå (Sweden) University, and his coauthors. The study was published online in the Lancet.
In this trial of 3,532 individuals who were aged 40-60 years with one or more conventional cardiovascular risk factors, the intervention group (1,749) received pictorial information of atherosclerosis as an add-on to normal care. Their primary care physician received the same information, and these participants also received a follow-up phone call from a nurse 2-4 weeks later. The other participants (1,783) received standard care but neither the presentation nor the phone call.
Both the Framingham risk score (FRS) and European Systematic Coronary Risk Evaluation (SCORE) were both used to assess outcomes; at 1-year follow-up, the intervention group had an FRS that decreased from baseline (–0.58; 95% confidence interval, –0.86 to –0.30), compared with an increase in the control group (0.35; 95% CI, 0.08-0.63). SCORE values increased twice as much in the control group (0.27; 95% CI, 0.23-0.30), compared with the intervention group (0.13; 95% CI, 0.09-0.18). The authors also observed no differential responses for education level, surmising that “this type of risk communication might contribute to reduction of the social gap in health.”
The authors shared their study’s limitations, including notable differences between dropouts and participants at 1-year follow-up with regard to metabolic risk factors and such fast-developing imaging technologies as CT and MRI out-dating ultrasound findings. They also acknowledged that more research needs to be undertaken to prove that these outcomes are genuine.
This study was funded by Västerbotten County Council, the Swedish Research Council, the Heart and Lung Foundation, and the Swedish Society of Medicine. No conflicts of interest were reported.
SOURCE: Näslund U et al. Lancet. 2018 Dec 3. doi: 10.1016/S0140-6736(18)32818-6.
FROM THE LANCET
Key clinical point: Patients who received a pictorial representation of atherosclerosis, plus a nurse-led follow-up phone call, saw reduced cardiovascular disease risk after 1 year.
Major finding: At 1-year follow-up, the intervention group had a Framingham risk score that decreased from baseline (–0.58; 95% confidence interval, –0.86 to –0.30) while the control group saw an increase (0.35; 95% CI, 0.08-0.63).
Study details: A randomized controlled trial of 3,532 participants in a cardiovascular disease prevention program in northern Sweden.
Disclosures: This study was funded by Västerbotten County Council, the Swedish Research Council, the Heart and Lung Foundation, and the Swedish Society of Medicine. No conflicts of interest were reported.
Source: Näslund U et al. Lancet. 2018 Dec 3. doi: 10.1016/S0140-6736(18)32818-6.