User login
Stopping dual antiplatelet therapy (DAPT) (eg, clopidogrel plus aspirin) after 3 months is reasonable in patients with stable ischemic heart disease who have a second-generation drug-eluting stent and a high bleeding risk, with stable ischemic disease defined as at least 1 year free of acute coronary syndromes. However, these patients should continue lifelong aspirin monotherapy. Current guidelines suggest that in stable ischemic disease, the risk-benefit ratio may favor an even shorter duration of DAPT than the 6 months currently recommended.1
STABLE ISCHEMIC HEART DISEASE VS ACUTE CORONARY SYNDROME
Percutaneous coronary intervention for stable ischemic heart disease is indicated primarily in patients with angina that persists despite optimal antianginal therapy.
The prognostic implications of DAPT are different in stable ischemic disease than in acute coronary syndromes. The substrate treated by percutaneous intervention in stable ischemic disease is primarily fibrofatty plaque, as opposed to thrombus in acute coronary syndromes.
Percutaneous intervention significantly improves the prognosis in acute coronary syndromes, whereas its impact on overall survival in stable ischemic heart disease is not well documented. Given these differences, our discussion about DAPT in stable ischemic disease cannot be extrapolated to acute coronary syndromes.
BENEFITS OF DAPT
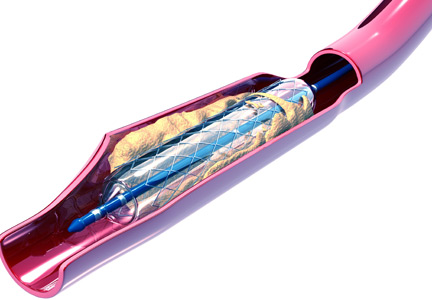
DAPT is mandatory early after drug-eluting stent placement, when the stent continuously releases medication, inhibiting tissue growth within the lumen of the stent.
Endothelialization of the stent normally occurs during the first 7 to 30 days after placement. During this period, the nonendothelialized stent poses a risk of thrombosis, a life-threatening, catastrophic condition with a mortality rate between 9% and 45%.1
THERAPY BEYOND 12 MONTHS
Although guidelines have traditionally recommended 12 months of DAPT, the optimal duration is still debated.
A duration beyond 12 months in patients with a history of myocardial infarction was shown to be reasonable in 2 large trials,2,3 while a 2016 review by Bittl et al4 suggested that therapy beyond 12 months in patients with a newer-generation drug-eluting stent could increase the incidence of major bleeding. A detailed discussion of DAPT longer than 12 months is beyond the scope of this article.
EVIDENCE FOR SHORTER DURATION
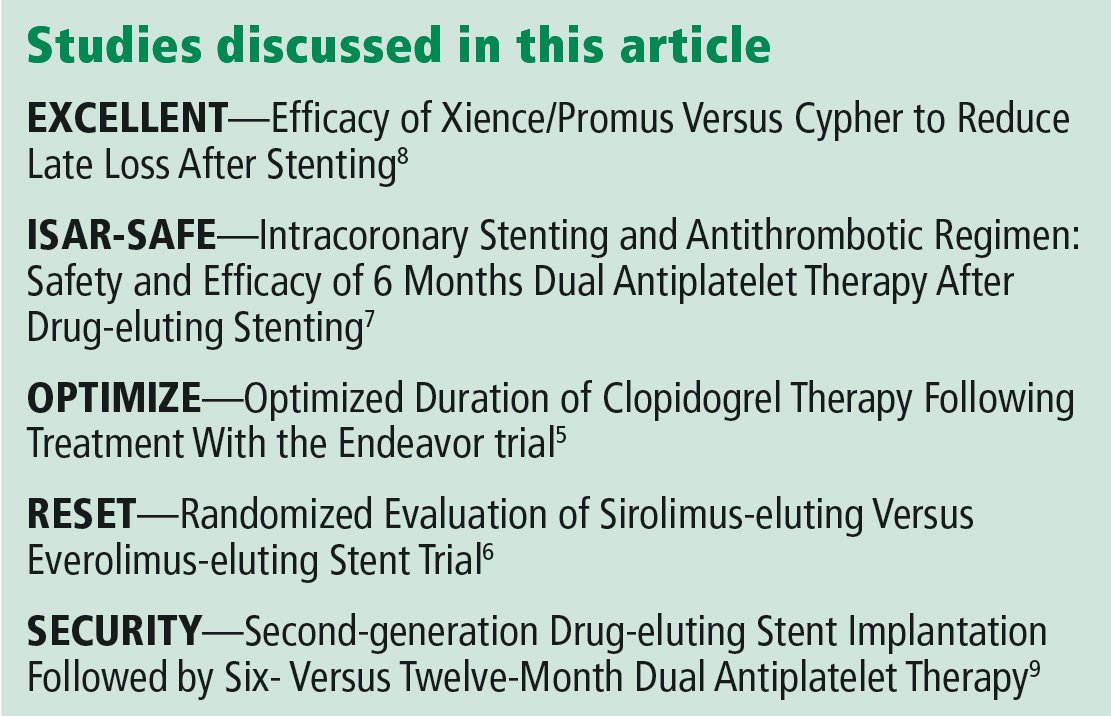
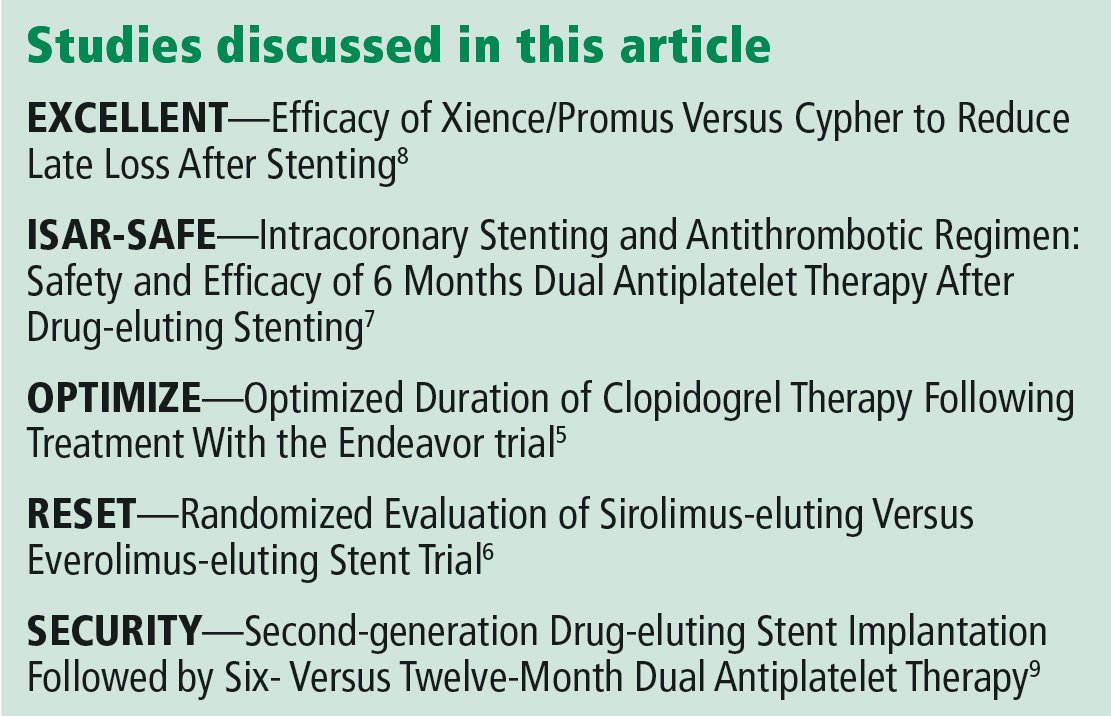
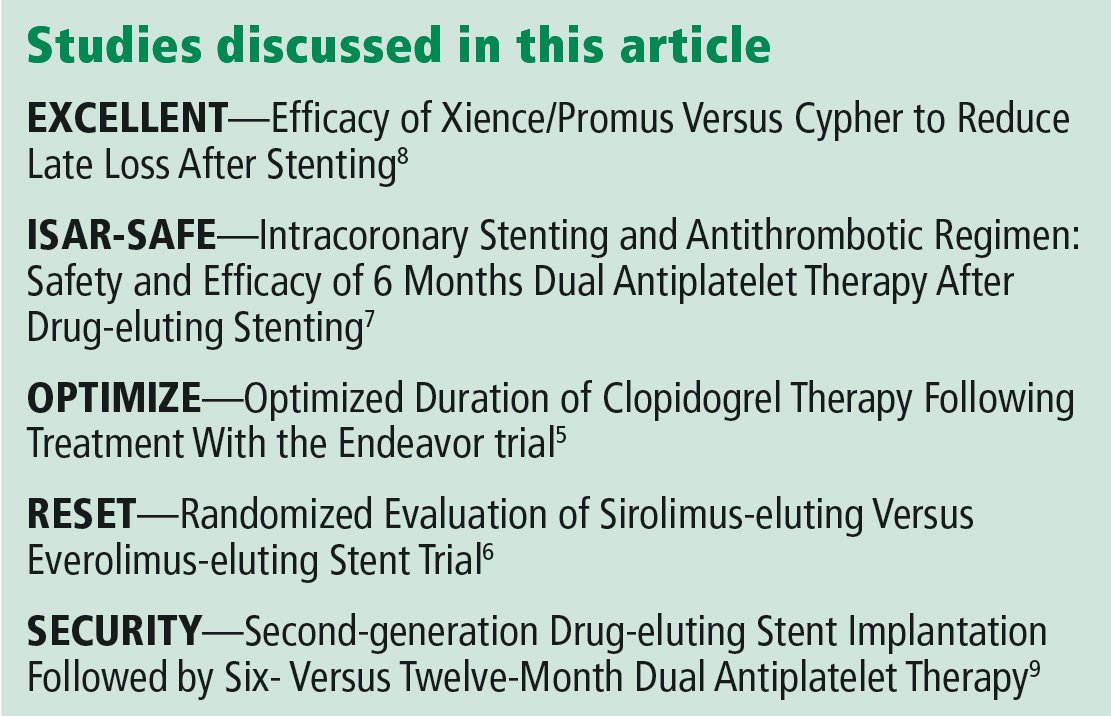
The results of 5 major trials support shorter duration of DAPT in stable ischemic disease.
The OPTIMIZE5 and RESET6 trials found that 3 months of DAPT was not inferior to 12 months in terms of ischemic and safety end points.
The ISAR-SAFE,7 EXCELLENT,8 and SECURITY9 trials also reported that 6 months of DAPT was not inferior to 12 months for the primary composite end point of death, stent thrombosis, myocardial infarction, stroke, or major bleeding.
However, these trials may have been underpowered to detect a difference in rates of stent thrombosis with shorter-duration DAPT.
CURRENT GUIDELINES
For patients at high bleeding risk, the current guidelines of the American College of Cardiology and American Heart Association, updated in 2016, suggest that it may be reasonable to discontinue DAPT 3 months after drug-eluting stent placement in patients with stable ischemic heart disease, and at 6 months in patients with acute coronary syndrome (class IIb recommendation, level of evidence C).1 These recommendations are based on results of randomized controlled trials showing no difference in the rate of stent thrombosis and composite ischemic events with a shorter duration than with 12 months of therapy.5–10
The evidence for DAPT in stable ischemic disease is based on clopidogrel, with only limited data on ticagrelor.1 To our knowledge, no study to date has evaluated DAPT in this setting for less than 3 months, and further study is needed to address shorter-duration approaches with current-generation drug-eluting stents Since 2017, all coronary stents implanted in the United States have been second-generation stents.
TOOLS TO HELP DECISION-MAKING
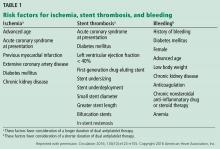
The decision to stop DAPT in a patient at high risk of bleeding requires a careful assessment of the risks and benefits. Risk factors for bleeding include advanced age, history of major bleeding, anticoagulation, chronic kidney disease (serum creatinine level ≥ 2 mg/dL), platelet count 100 × 109/L or lower, and history of stroke.11
- Age 75 or older: −2 points
- Ages 65 to 74: −1
- Age under 65: 0
- Diabetes mellitus: 1
- Myocardial infarction at presentation: 1
- History of percutaneous coronary intervention or myocardial infarction: 1
- Stent diameter less than 3 mm: 1
- Paclitaxel drug-eluting stent: 1
- Current smoker: 2
- Percutaneous coronary intervention with saphenous vein graft: 2
- Congestive heart failure or left ventricular ejection fraction less than 30%: 2.
A score of 2 or greater favors continuing DAPT, as it indicates higher ischemic risk. A score less than 2 favors discontinuing DAPT, as it indicates higher bleeding risk.1,2
IF BLEEDING RISK IS HIGH
Preventing and controlling bleeding associated with DAPT is important. The gastrointestinal tract is the most common site of bleeding.
Aspirin inhibits prostaglandin synthesis, leading to disruption of the protective mucous membrane. Therefore, a proton pump inhibitor should be started along with DAPT in patients at high risk of gastrointestinal bleeding.
If a patient’s bleeding risk significantly outweighs the risk of stent thrombosis, or if active hemorrhage makes a patient hemodynamically unstable, antiplatelet therapy must be stopped.1
FACING SURGERY
For patients with a drug-eluting stent who are on DAPT and are to undergo elective noncardiac surgery, 3 considerations must be kept in mind:
- The risk of stent thrombosis if DAPT needs to be interrupted
- The consequences of delaying the surgical procedure
- The risk and consequences of periprocedural and intraprocedural bleeding if DAPT is continued.
Because clinical evidence for bridging therapy with intravenous antiplatelet or anticoagulant agents is limited, it is difficult to make recommendations about stopping DAPT. However, once bleeding risk is stabilized, DAPT should be restarted as soon as possible.1
CURRENT RESEARCH
Several trials are under way to further evaluate ways to minimize bleeding risk and shorten the duration of DAPT.
A prospective multicenter trial is evaluating 3-month DAPT in patients at high bleeding risk who undergo placement of an everolimus-eluting stent.11 This study is expected to be completed in August 2019.
Another strategy for patients at high bleeding risk is use of a polymer-free drug-coated coronary stent. In a 2015 trial comparing a biolimus A9-coated stent vs a bare-metal stent, patients received DAPT for 1 month after stent placement. The drug-coated stent was found to be superior in terms of the primary safety end point (cardiac death, myocardial infarction, or stent thrombosis).12 This stent is not yet approved by the US Food and Drug Administration at the time of this writing.
Further study is needed to evaluate DAPT durations of less than 3 months and to establish the proper timing for safely discontinuing DAPT in difficult clinical scenarios.
WHEN STOPPING MAY BE REASONABLE
According to current guidelines, in patients at high bleeding risk with a second-generation or newer drug-eluting stent for stable ischemic heart disease, discontinuing DAPT 3 months after stent placement may be reasonable.1 The decision to stop DAPT in these patients requires a careful assessment of the risks and benefits and may be aided by a tool such as the DAPT risk score. However, these recommendations cannot be extrapolated to patients with an acute coronary syndrome within the past year, as they are at higher risk.
TAKE-HOME MESSAGES
- A cardiologist should be consulted before discontinuing DAPT in patients with a drug-eluting stent, especially if the stent was recently placed.
- The duration of therapy depends on the indication for stent placement (stable ischemic heart disease vs acute coronary syndrome) and on stent location.
- Based on the 2016 American College of Cardiology/American Heart Association guidelines,1 in patients at high bleeding risk with a second-generation drug-eluting stent, discontinuing DAPT is safe after 3 months in patients with stable ischemic heart disease, and after 6 months in patients with an acute coronary syndrome.
- When prescribing DAPT, available evidence favors clopidogrel in patients with stable ischemic heart disease who have a second-generation drug-eluting stent and are at high bleeding risk.
- In these patients, the risk-benefit ratio based on the DAPT score may be useful when considering stopping clopidogrel.
- Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2016; 134(10):e123–e155. doi:10.1161/CIR.0000000000000404 [correction in doi:10.1161/CIR.0000000000000452]
- Mauri L, Kereiakes DJ, Yeh RW, et al; DAPT Study Investigators. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med 2014; 371(23):2155–2166. doi:10.1056/NEJMoa1409312
- Bonaca MP, Bhatt DL, Cohen M, et al; PEGASUS-TIMI 54 Steering Committee and Investigators. Long-term use of ticagrelor in patients with prior myocardial infarction. N Engl J Med 2015; 372(19):1791–1800. doi:10.1056/NEJMoa1500857
- Bittl JA, Baber U, Bradley SM, Wijeysundera DN. Duration of dual antiplatelet therapy: a systematic review for the 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2016; 68(10):1116–1139. doi:10.1016/j.jacc.2016.03.512
- Feres F, Costa RA, Abizaid A, et al; OPTIMIZE Trial Investigators. Three vs twelve months of dual antiplatelet therapy after zotarolimus-eluting stents: the OPTIMIZE randomized trial. JAMA 2013; 310(23):2510–2522. doi:10.1001/jama.2013.282183
- Kubo T, Akasaka T, Kozuma K, et al. Comparison of neointimal coverage between everolimus-eluting stents and sirolimus-eluting stents: an optical coherence tomography substudy of RESET. EuroIntervention 2015. doi:10.4244/EIJV11I5A109
- Schulz-Schupke S, Byrne RA, ten Berg JM, et al; Intracoronary Stenting and Antithrombotic Regimen: Safety And EFficacy of 6 Months Dual Antiplatelet Therapy After Drug-Eluting Stenting (ISAR-SAFE) Trial Investigators. ISAR-SAFE: a randomized, double-blind, placebo-controlled trial of 6 vs 12 months of clopidogrel therapy after drug-eluting stenting. Eur Heart J 2015; 36(20):1252–1263. doi:10.1093/eurheartj/ehu523
- Gwon HC, Hahn JY, Park KW, et al. Six-month versus 12-month dual antiplatelet therapy after implantation of drug-eluting stents: the efficacy of Xience/Promus vs Cypher to reduce late loss after stenting (EXCELLENT) randomized, multicenter study. Circulation 2012; 125(3):505–513. doi:10.1161/CIRCULATIONAHA.111.059022
- Colombo A, Chieffo A, Frasheri A, et al. Second-generation drug-eluting stent implantation followed by 6- vs 12-month dual antiplatelet therapy: the SECURITY randomized clinical trial. J Am Coll Cardiol 2014; 64(20):2086–2097. doi:10.1016/j.jacc.2014.09.008
- Kim BK, Hong MK, Shin DH, et al; RESET Investigators. A new strategy for discontinuation of dual antiplatelet therapy: the RESET Trial (REal Safety and Efficacy of 3-month dual antiplatelet Therapy following Endeavor zotarolimus-eluting stent implantation). J Am Coll Cardiol 2012; 60(15):1340–1348. doi:10.1016/j.jacc.2012.06.043
- US National Library of Medicine. ClinicalTrials.gov. EVOLVE Short DAPT Study. https://clinicaltrials.gov/ct2/show/NCT02605447. Accessed December 3, 2018.
- Urban P, Meredith IT, Abizaid A, et al; LEADERS FREE Investigators. Polymer-free drug-coated coronary stents in patients at high bleeding risk. N Engl J Med 2015; 373(21):2038–2047. doi:10.1056/NEJMoa1503943
Stopping dual antiplatelet therapy (DAPT) (eg, clopidogrel plus aspirin) after 3 months is reasonable in patients with stable ischemic heart disease who have a second-generation drug-eluting stent and a high bleeding risk, with stable ischemic disease defined as at least 1 year free of acute coronary syndromes. However, these patients should continue lifelong aspirin monotherapy. Current guidelines suggest that in stable ischemic disease, the risk-benefit ratio may favor an even shorter duration of DAPT than the 6 months currently recommended.1
STABLE ISCHEMIC HEART DISEASE VS ACUTE CORONARY SYNDROME
Percutaneous coronary intervention for stable ischemic heart disease is indicated primarily in patients with angina that persists despite optimal antianginal therapy.
The prognostic implications of DAPT are different in stable ischemic disease than in acute coronary syndromes. The substrate treated by percutaneous intervention in stable ischemic disease is primarily fibrofatty plaque, as opposed to thrombus in acute coronary syndromes.
Percutaneous intervention significantly improves the prognosis in acute coronary syndromes, whereas its impact on overall survival in stable ischemic heart disease is not well documented. Given these differences, our discussion about DAPT in stable ischemic disease cannot be extrapolated to acute coronary syndromes.
BENEFITS OF DAPT
DAPT is mandatory early after drug-eluting stent placement, when the stent continuously releases medication, inhibiting tissue growth within the lumen of the stent.
Endothelialization of the stent normally occurs during the first 7 to 30 days after placement. During this period, the nonendothelialized stent poses a risk of thrombosis, a life-threatening, catastrophic condition with a mortality rate between 9% and 45%.1
THERAPY BEYOND 12 MONTHS
Although guidelines have traditionally recommended 12 months of DAPT, the optimal duration is still debated.
A duration beyond 12 months in patients with a history of myocardial infarction was shown to be reasonable in 2 large trials,2,3 while a 2016 review by Bittl et al4 suggested that therapy beyond 12 months in patients with a newer-generation drug-eluting stent could increase the incidence of major bleeding. A detailed discussion of DAPT longer than 12 months is beyond the scope of this article.
EVIDENCE FOR SHORTER DURATION
The results of 5 major trials support shorter duration of DAPT in stable ischemic disease.
The OPTIMIZE5 and RESET6 trials found that 3 months of DAPT was not inferior to 12 months in terms of ischemic and safety end points.
The ISAR-SAFE,7 EXCELLENT,8 and SECURITY9 trials also reported that 6 months of DAPT was not inferior to 12 months for the primary composite end point of death, stent thrombosis, myocardial infarction, stroke, or major bleeding.
However, these trials may have been underpowered to detect a difference in rates of stent thrombosis with shorter-duration DAPT.
CURRENT GUIDELINES
For patients at high bleeding risk, the current guidelines of the American College of Cardiology and American Heart Association, updated in 2016, suggest that it may be reasonable to discontinue DAPT 3 months after drug-eluting stent placement in patients with stable ischemic heart disease, and at 6 months in patients with acute coronary syndrome (class IIb recommendation, level of evidence C).1 These recommendations are based on results of randomized controlled trials showing no difference in the rate of stent thrombosis and composite ischemic events with a shorter duration than with 12 months of therapy.5–10
The evidence for DAPT in stable ischemic disease is based on clopidogrel, with only limited data on ticagrelor.1 To our knowledge, no study to date has evaluated DAPT in this setting for less than 3 months, and further study is needed to address shorter-duration approaches with current-generation drug-eluting stents Since 2017, all coronary stents implanted in the United States have been second-generation stents.
TOOLS TO HELP DECISION-MAKING
The decision to stop DAPT in a patient at high risk of bleeding requires a careful assessment of the risks and benefits. Risk factors for bleeding include advanced age, history of major bleeding, anticoagulation, chronic kidney disease (serum creatinine level ≥ 2 mg/dL), platelet count 100 × 109/L or lower, and history of stroke.11
- Age 75 or older: −2 points
- Ages 65 to 74: −1
- Age under 65: 0
- Diabetes mellitus: 1
- Myocardial infarction at presentation: 1
- History of percutaneous coronary intervention or myocardial infarction: 1
- Stent diameter less than 3 mm: 1
- Paclitaxel drug-eluting stent: 1
- Current smoker: 2
- Percutaneous coronary intervention with saphenous vein graft: 2
- Congestive heart failure or left ventricular ejection fraction less than 30%: 2.
A score of 2 or greater favors continuing DAPT, as it indicates higher ischemic risk. A score less than 2 favors discontinuing DAPT, as it indicates higher bleeding risk.1,2
IF BLEEDING RISK IS HIGH
Preventing and controlling bleeding associated with DAPT is important. The gastrointestinal tract is the most common site of bleeding.
Aspirin inhibits prostaglandin synthesis, leading to disruption of the protective mucous membrane. Therefore, a proton pump inhibitor should be started along with DAPT in patients at high risk of gastrointestinal bleeding.
If a patient’s bleeding risk significantly outweighs the risk of stent thrombosis, or if active hemorrhage makes a patient hemodynamically unstable, antiplatelet therapy must be stopped.1
FACING SURGERY
For patients with a drug-eluting stent who are on DAPT and are to undergo elective noncardiac surgery, 3 considerations must be kept in mind:
- The risk of stent thrombosis if DAPT needs to be interrupted
- The consequences of delaying the surgical procedure
- The risk and consequences of periprocedural and intraprocedural bleeding if DAPT is continued.
Because clinical evidence for bridging therapy with intravenous antiplatelet or anticoagulant agents is limited, it is difficult to make recommendations about stopping DAPT. However, once bleeding risk is stabilized, DAPT should be restarted as soon as possible.1
CURRENT RESEARCH
Several trials are under way to further evaluate ways to minimize bleeding risk and shorten the duration of DAPT.
A prospective multicenter trial is evaluating 3-month DAPT in patients at high bleeding risk who undergo placement of an everolimus-eluting stent.11 This study is expected to be completed in August 2019.
Another strategy for patients at high bleeding risk is use of a polymer-free drug-coated coronary stent. In a 2015 trial comparing a biolimus A9-coated stent vs a bare-metal stent, patients received DAPT for 1 month after stent placement. The drug-coated stent was found to be superior in terms of the primary safety end point (cardiac death, myocardial infarction, or stent thrombosis).12 This stent is not yet approved by the US Food and Drug Administration at the time of this writing.
Further study is needed to evaluate DAPT durations of less than 3 months and to establish the proper timing for safely discontinuing DAPT in difficult clinical scenarios.
WHEN STOPPING MAY BE REASONABLE
According to current guidelines, in patients at high bleeding risk with a second-generation or newer drug-eluting stent for stable ischemic heart disease, discontinuing DAPT 3 months after stent placement may be reasonable.1 The decision to stop DAPT in these patients requires a careful assessment of the risks and benefits and may be aided by a tool such as the DAPT risk score. However, these recommendations cannot be extrapolated to patients with an acute coronary syndrome within the past year, as they are at higher risk.
TAKE-HOME MESSAGES
- A cardiologist should be consulted before discontinuing DAPT in patients with a drug-eluting stent, especially if the stent was recently placed.
- The duration of therapy depends on the indication for stent placement (stable ischemic heart disease vs acute coronary syndrome) and on stent location.
- Based on the 2016 American College of Cardiology/American Heart Association guidelines,1 in patients at high bleeding risk with a second-generation drug-eluting stent, discontinuing DAPT is safe after 3 months in patients with stable ischemic heart disease, and after 6 months in patients with an acute coronary syndrome.
- When prescribing DAPT, available evidence favors clopidogrel in patients with stable ischemic heart disease who have a second-generation drug-eluting stent and are at high bleeding risk.
- In these patients, the risk-benefit ratio based on the DAPT score may be useful when considering stopping clopidogrel.
Stopping dual antiplatelet therapy (DAPT) (eg, clopidogrel plus aspirin) after 3 months is reasonable in patients with stable ischemic heart disease who have a second-generation drug-eluting stent and a high bleeding risk, with stable ischemic disease defined as at least 1 year free of acute coronary syndromes. However, these patients should continue lifelong aspirin monotherapy. Current guidelines suggest that in stable ischemic disease, the risk-benefit ratio may favor an even shorter duration of DAPT than the 6 months currently recommended.1
STABLE ISCHEMIC HEART DISEASE VS ACUTE CORONARY SYNDROME
Percutaneous coronary intervention for stable ischemic heart disease is indicated primarily in patients with angina that persists despite optimal antianginal therapy.
The prognostic implications of DAPT are different in stable ischemic disease than in acute coronary syndromes. The substrate treated by percutaneous intervention in stable ischemic disease is primarily fibrofatty plaque, as opposed to thrombus in acute coronary syndromes.
Percutaneous intervention significantly improves the prognosis in acute coronary syndromes, whereas its impact on overall survival in stable ischemic heart disease is not well documented. Given these differences, our discussion about DAPT in stable ischemic disease cannot be extrapolated to acute coronary syndromes.
BENEFITS OF DAPT
DAPT is mandatory early after drug-eluting stent placement, when the stent continuously releases medication, inhibiting tissue growth within the lumen of the stent.
Endothelialization of the stent normally occurs during the first 7 to 30 days after placement. During this period, the nonendothelialized stent poses a risk of thrombosis, a life-threatening, catastrophic condition with a mortality rate between 9% and 45%.1
THERAPY BEYOND 12 MONTHS
Although guidelines have traditionally recommended 12 months of DAPT, the optimal duration is still debated.
A duration beyond 12 months in patients with a history of myocardial infarction was shown to be reasonable in 2 large trials,2,3 while a 2016 review by Bittl et al4 suggested that therapy beyond 12 months in patients with a newer-generation drug-eluting stent could increase the incidence of major bleeding. A detailed discussion of DAPT longer than 12 months is beyond the scope of this article.
EVIDENCE FOR SHORTER DURATION
The results of 5 major trials support shorter duration of DAPT in stable ischemic disease.
The OPTIMIZE5 and RESET6 trials found that 3 months of DAPT was not inferior to 12 months in terms of ischemic and safety end points.
The ISAR-SAFE,7 EXCELLENT,8 and SECURITY9 trials also reported that 6 months of DAPT was not inferior to 12 months for the primary composite end point of death, stent thrombosis, myocardial infarction, stroke, or major bleeding.
However, these trials may have been underpowered to detect a difference in rates of stent thrombosis with shorter-duration DAPT.
CURRENT GUIDELINES
For patients at high bleeding risk, the current guidelines of the American College of Cardiology and American Heart Association, updated in 2016, suggest that it may be reasonable to discontinue DAPT 3 months after drug-eluting stent placement in patients with stable ischemic heart disease, and at 6 months in patients with acute coronary syndrome (class IIb recommendation, level of evidence C).1 These recommendations are based on results of randomized controlled trials showing no difference in the rate of stent thrombosis and composite ischemic events with a shorter duration than with 12 months of therapy.5–10
The evidence for DAPT in stable ischemic disease is based on clopidogrel, with only limited data on ticagrelor.1 To our knowledge, no study to date has evaluated DAPT in this setting for less than 3 months, and further study is needed to address shorter-duration approaches with current-generation drug-eluting stents Since 2017, all coronary stents implanted in the United States have been second-generation stents.
TOOLS TO HELP DECISION-MAKING
The decision to stop DAPT in a patient at high risk of bleeding requires a careful assessment of the risks and benefits. Risk factors for bleeding include advanced age, history of major bleeding, anticoagulation, chronic kidney disease (serum creatinine level ≥ 2 mg/dL), platelet count 100 × 109/L or lower, and history of stroke.11
- Age 75 or older: −2 points
- Ages 65 to 74: −1
- Age under 65: 0
- Diabetes mellitus: 1
- Myocardial infarction at presentation: 1
- History of percutaneous coronary intervention or myocardial infarction: 1
- Stent diameter less than 3 mm: 1
- Paclitaxel drug-eluting stent: 1
- Current smoker: 2
- Percutaneous coronary intervention with saphenous vein graft: 2
- Congestive heart failure or left ventricular ejection fraction less than 30%: 2.
A score of 2 or greater favors continuing DAPT, as it indicates higher ischemic risk. A score less than 2 favors discontinuing DAPT, as it indicates higher bleeding risk.1,2
IF BLEEDING RISK IS HIGH
Preventing and controlling bleeding associated with DAPT is important. The gastrointestinal tract is the most common site of bleeding.
Aspirin inhibits prostaglandin synthesis, leading to disruption of the protective mucous membrane. Therefore, a proton pump inhibitor should be started along with DAPT in patients at high risk of gastrointestinal bleeding.
If a patient’s bleeding risk significantly outweighs the risk of stent thrombosis, or if active hemorrhage makes a patient hemodynamically unstable, antiplatelet therapy must be stopped.1
FACING SURGERY
For patients with a drug-eluting stent who are on DAPT and are to undergo elective noncardiac surgery, 3 considerations must be kept in mind:
- The risk of stent thrombosis if DAPT needs to be interrupted
- The consequences of delaying the surgical procedure
- The risk and consequences of periprocedural and intraprocedural bleeding if DAPT is continued.
Because clinical evidence for bridging therapy with intravenous antiplatelet or anticoagulant agents is limited, it is difficult to make recommendations about stopping DAPT. However, once bleeding risk is stabilized, DAPT should be restarted as soon as possible.1
CURRENT RESEARCH
Several trials are under way to further evaluate ways to minimize bleeding risk and shorten the duration of DAPT.
A prospective multicenter trial is evaluating 3-month DAPT in patients at high bleeding risk who undergo placement of an everolimus-eluting stent.11 This study is expected to be completed in August 2019.
Another strategy for patients at high bleeding risk is use of a polymer-free drug-coated coronary stent. In a 2015 trial comparing a biolimus A9-coated stent vs a bare-metal stent, patients received DAPT for 1 month after stent placement. The drug-coated stent was found to be superior in terms of the primary safety end point (cardiac death, myocardial infarction, or stent thrombosis).12 This stent is not yet approved by the US Food and Drug Administration at the time of this writing.
Further study is needed to evaluate DAPT durations of less than 3 months and to establish the proper timing for safely discontinuing DAPT in difficult clinical scenarios.
WHEN STOPPING MAY BE REASONABLE
According to current guidelines, in patients at high bleeding risk with a second-generation or newer drug-eluting stent for stable ischemic heart disease, discontinuing DAPT 3 months after stent placement may be reasonable.1 The decision to stop DAPT in these patients requires a careful assessment of the risks and benefits and may be aided by a tool such as the DAPT risk score. However, these recommendations cannot be extrapolated to patients with an acute coronary syndrome within the past year, as they are at higher risk.
TAKE-HOME MESSAGES
- A cardiologist should be consulted before discontinuing DAPT in patients with a drug-eluting stent, especially if the stent was recently placed.
- The duration of therapy depends on the indication for stent placement (stable ischemic heart disease vs acute coronary syndrome) and on stent location.
- Based on the 2016 American College of Cardiology/American Heart Association guidelines,1 in patients at high bleeding risk with a second-generation drug-eluting stent, discontinuing DAPT is safe after 3 months in patients with stable ischemic heart disease, and after 6 months in patients with an acute coronary syndrome.
- When prescribing DAPT, available evidence favors clopidogrel in patients with stable ischemic heart disease who have a second-generation drug-eluting stent and are at high bleeding risk.
- In these patients, the risk-benefit ratio based on the DAPT score may be useful when considering stopping clopidogrel.
- Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2016; 134(10):e123–e155. doi:10.1161/CIR.0000000000000404 [correction in doi:10.1161/CIR.0000000000000452]
- Mauri L, Kereiakes DJ, Yeh RW, et al; DAPT Study Investigators. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med 2014; 371(23):2155–2166. doi:10.1056/NEJMoa1409312
- Bonaca MP, Bhatt DL, Cohen M, et al; PEGASUS-TIMI 54 Steering Committee and Investigators. Long-term use of ticagrelor in patients with prior myocardial infarction. N Engl J Med 2015; 372(19):1791–1800. doi:10.1056/NEJMoa1500857
- Bittl JA, Baber U, Bradley SM, Wijeysundera DN. Duration of dual antiplatelet therapy: a systematic review for the 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2016; 68(10):1116–1139. doi:10.1016/j.jacc.2016.03.512
- Feres F, Costa RA, Abizaid A, et al; OPTIMIZE Trial Investigators. Three vs twelve months of dual antiplatelet therapy after zotarolimus-eluting stents: the OPTIMIZE randomized trial. JAMA 2013; 310(23):2510–2522. doi:10.1001/jama.2013.282183
- Kubo T, Akasaka T, Kozuma K, et al. Comparison of neointimal coverage between everolimus-eluting stents and sirolimus-eluting stents: an optical coherence tomography substudy of RESET. EuroIntervention 2015. doi:10.4244/EIJV11I5A109
- Schulz-Schupke S, Byrne RA, ten Berg JM, et al; Intracoronary Stenting and Antithrombotic Regimen: Safety And EFficacy of 6 Months Dual Antiplatelet Therapy After Drug-Eluting Stenting (ISAR-SAFE) Trial Investigators. ISAR-SAFE: a randomized, double-blind, placebo-controlled trial of 6 vs 12 months of clopidogrel therapy after drug-eluting stenting. Eur Heart J 2015; 36(20):1252–1263. doi:10.1093/eurheartj/ehu523
- Gwon HC, Hahn JY, Park KW, et al. Six-month versus 12-month dual antiplatelet therapy after implantation of drug-eluting stents: the efficacy of Xience/Promus vs Cypher to reduce late loss after stenting (EXCELLENT) randomized, multicenter study. Circulation 2012; 125(3):505–513. doi:10.1161/CIRCULATIONAHA.111.059022
- Colombo A, Chieffo A, Frasheri A, et al. Second-generation drug-eluting stent implantation followed by 6- vs 12-month dual antiplatelet therapy: the SECURITY randomized clinical trial. J Am Coll Cardiol 2014; 64(20):2086–2097. doi:10.1016/j.jacc.2014.09.008
- Kim BK, Hong MK, Shin DH, et al; RESET Investigators. A new strategy for discontinuation of dual antiplatelet therapy: the RESET Trial (REal Safety and Efficacy of 3-month dual antiplatelet Therapy following Endeavor zotarolimus-eluting stent implantation). J Am Coll Cardiol 2012; 60(15):1340–1348. doi:10.1016/j.jacc.2012.06.043
- US National Library of Medicine. ClinicalTrials.gov. EVOLVE Short DAPT Study. https://clinicaltrials.gov/ct2/show/NCT02605447. Accessed December 3, 2018.
- Urban P, Meredith IT, Abizaid A, et al; LEADERS FREE Investigators. Polymer-free drug-coated coronary stents in patients at high bleeding risk. N Engl J Med 2015; 373(21):2038–2047. doi:10.1056/NEJMoa1503943
- Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2016; 134(10):e123–e155. doi:10.1161/CIR.0000000000000404 [correction in doi:10.1161/CIR.0000000000000452]
- Mauri L, Kereiakes DJ, Yeh RW, et al; DAPT Study Investigators. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med 2014; 371(23):2155–2166. doi:10.1056/NEJMoa1409312
- Bonaca MP, Bhatt DL, Cohen M, et al; PEGASUS-TIMI 54 Steering Committee and Investigators. Long-term use of ticagrelor in patients with prior myocardial infarction. N Engl J Med 2015; 372(19):1791–1800. doi:10.1056/NEJMoa1500857
- Bittl JA, Baber U, Bradley SM, Wijeysundera DN. Duration of dual antiplatelet therapy: a systematic review for the 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2016; 68(10):1116–1139. doi:10.1016/j.jacc.2016.03.512
- Feres F, Costa RA, Abizaid A, et al; OPTIMIZE Trial Investigators. Three vs twelve months of dual antiplatelet therapy after zotarolimus-eluting stents: the OPTIMIZE randomized trial. JAMA 2013; 310(23):2510–2522. doi:10.1001/jama.2013.282183
- Kubo T, Akasaka T, Kozuma K, et al. Comparison of neointimal coverage between everolimus-eluting stents and sirolimus-eluting stents: an optical coherence tomography substudy of RESET. EuroIntervention 2015. doi:10.4244/EIJV11I5A109
- Schulz-Schupke S, Byrne RA, ten Berg JM, et al; Intracoronary Stenting and Antithrombotic Regimen: Safety And EFficacy of 6 Months Dual Antiplatelet Therapy After Drug-Eluting Stenting (ISAR-SAFE) Trial Investigators. ISAR-SAFE: a randomized, double-blind, placebo-controlled trial of 6 vs 12 months of clopidogrel therapy after drug-eluting stenting. Eur Heart J 2015; 36(20):1252–1263. doi:10.1093/eurheartj/ehu523
- Gwon HC, Hahn JY, Park KW, et al. Six-month versus 12-month dual antiplatelet therapy after implantation of drug-eluting stents: the efficacy of Xience/Promus vs Cypher to reduce late loss after stenting (EXCELLENT) randomized, multicenter study. Circulation 2012; 125(3):505–513. doi:10.1161/CIRCULATIONAHA.111.059022
- Colombo A, Chieffo A, Frasheri A, et al. Second-generation drug-eluting stent implantation followed by 6- vs 12-month dual antiplatelet therapy: the SECURITY randomized clinical trial. J Am Coll Cardiol 2014; 64(20):2086–2097. doi:10.1016/j.jacc.2014.09.008
- Kim BK, Hong MK, Shin DH, et al; RESET Investigators. A new strategy for discontinuation of dual antiplatelet therapy: the RESET Trial (REal Safety and Efficacy of 3-month dual antiplatelet Therapy following Endeavor zotarolimus-eluting stent implantation). J Am Coll Cardiol 2012; 60(15):1340–1348. doi:10.1016/j.jacc.2012.06.043
- US National Library of Medicine. ClinicalTrials.gov. EVOLVE Short DAPT Study. https://clinicaltrials.gov/ct2/show/NCT02605447. Accessed December 3, 2018.
- Urban P, Meredith IT, Abizaid A, et al; LEADERS FREE Investigators. Polymer-free drug-coated coronary stents in patients at high bleeding risk. N Engl J Med 2015; 373(21):2038–2047. doi:10.1056/NEJMoa1503943