User login
Social phobia was accorded official psychiatric diagnostic status in the United States less than 20 years ago, but has been described in the medical literature for centuries. Hippocrates described such a patient: “He dare not come in company for fear he should be misused, disgraced, overshoot himself in gestures or speeches or be sick; he thinks every man observes him.”1
This observation was made more than 2,000 years ago. Yet social anxiety disorder (SAD) was left largely unstudied until the mid-1980s.2 An estimated 20 million people in the U.S. suffer from this disorder.
What causes some people to break into a cold sweat at the thought of the most casual encounter with a checkout clerk, a coworker, or an acquaintance? Limited evidence points to underlying biological abnormalities in SAD, but there have been no conclusive findings.
Two main subtypes of SAD exist (Box 1). Roughly 25% of sufferers have discrete or nongeneralized SAD, that is, circumscribed social fears limited to one or two situations, such as speaking in public or performing before an audience. The remaining 75% suffer from generalized SAD, the more severe subtype in which all or nearly all interpersonal interactions are difficult.
Generalized SAD often begins early in life, with a mean onset at about age 15, but 35% of the time SAD occurs in individuals before age 10.3 This subtype appears to run in families, while the nongeneralized subtype does not, suggesting that a genetic inheritance is possible. From an etiological perspective, the possible effects of parenting styles of socially anxious parents, or acquisition of social anxiety conditioned by experiencing extreme embarrassment, may also contribute to the development of SAD in some people. Approximately twice as many females as males are affected, and almost all are affected before age 25.3,4 When social fears interfere with social, occupational, or family life, the affected individual is not suffering from normal "shyness," but rather a treatable anxiety disorder.
–Toastmasters slogan
Generalized
- Most social interactions
- Early onset
- Social skills deficit
- High comorbidity
- Lower achievement
- Remission rare
Nongeneralized
- Limited fears
- Later onset
- Social skills normal
- Less comorbidity
- Less Impairment
- Remits often
The National Comorbidity Survey (NCS) estimated lifetime prevalence of SAD at 13.3% and 12-month prevalence at 7.6%, making it the third most common psychiatric disorder, following only major depression and alcohol abuse/dependence.5 Despite this high rate, SAD remains woefully underdiagnosed.
Anyone who has had to speak in public, play a musical instrument at a recital, or perform in some way under the watchful expectation of an audience has experienced anxiety as he or she anticipates the "big moment” (Box 2). Once the performance is under way, the anxiety usually lessens to a more manageable level for most people. In fact, nearly one in three Americans will admit to moderate or great fear of speaking in public.
Mr. L, a 40-year-old eighth-grade teacher, consulted a psychiatrist because he was scheduled to be evaluated by a state education accreditation committee while teaching class. Though he had always passed these before, he had been worried sick for weeks and was experiencing panic attacks each time he thought about the accreditation visit.
He lived with his mother, had never dated, and had few friends. He was extremely inhibited outside the classroom, brought cash to stores to avoid being observed while writing a check or signing credit card slips, and avoided social gatherings outside of his church, which he attended with his mother and tolerated with distress.
Further history revealed that he had quit medical school during his third year because he had so much difficulty presenting cases to the attending on ward rounds that he chose to leave the profession in order to avoid feeling sick each morning and afternoon.
Enough people encounter the fear of public speaking to support the weekly Toastmasters meetings in most U.S. cities. Many people overcome their social anxiety about public speaking or performing with continued practice. However, those with nongeneralized SAD, who are among the most severely affected, may remain so fearful of speaking or performing under scrutiny that they avoid it at any cost—even if it means passing up a job or promotion or even choosing to change professions.
The majority (75%) of those with SAD—representing approximately 15 million individuals in the U.S.—suffer from generalized SAD, a much more severe, potentially disabling subtype. These unfortunate individuals fear and avoid most or all social interactions outside their home except those with family or close friends. When they encounter or even anticipate entering feared social situations, individuals with generalized SAD experience severe anxiety. Blushing, tremulousness, and sweating can be noticed by others, and thus are particularly distressing to those with SAD.
Recovery without treatment is rare. The typically early age at onset of generalized SAD3,4 imposes greater limitations on development of social competence than on those who develop more discrete fear of public speaking or performing later in life—after socialization skills have already developed.
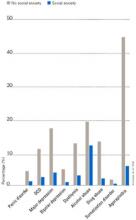
Individuals with SAD frequently suffer from comorbid psychiatric disorders, mostly depression and/or other anxiety disorders.6Figure 1 shows that individuals with SAD are at significantly increased risk for depression, other anxiety disorders, and alcohol and drug abuse. Since generalized SAD usually appears at an earlier age than other anxiety disorders, it represents a risk factor for subsequent depression. The level of functional impairment caused by SAD is similar to that caused by major depression7 (Figure 2).
As more comorbid psychiatric disorders accrue, impairment and increased risk for additional disorders may occur. Further, the risk of suicide is increased in those with comorbid SAD vs. those with SAD only. The findings suggest that if social anxiety were detected and treated effectively at an early age, it might be possible to prevent other psychiatric disorders—particularly depression—as well as the predictable morbidity and mortality that accompanies untreated SAD. Given the estimated $44 billion annual cost of anxiety disorders in the U.S.,8 research targeted at testing this hypothesis would appear to be a good investment.
Figure 1 HOW PREVALENT IS LIFETIME COMORBIDITY IN SAD?
- Inherent avoidance of scrutiny, (e.g., evaluation)
- Uncertain diagnostic threshold
- Acceptance of pathological shyness as ‘just my personality’
- Lack of understanding by professionals, family, friends
- Coping strategies that mask disability
- Comorbid psychiatric disorders that mask SAD
Figure 2 QUALITY OF LIFE IN PATIENTS WITH SOCIAL ANXIETY DISORDER
Seeing the unseen: making the diagnosis quickly
Although SAD is extremely common, a variety of factors may contribute to the low rate of recognition of the disorder (Box 3). Because of their intense discomfort toward scrutiny by authority figures such as their physician, individuals with SAD may not be willing to discuss their fears. Studies estimating the prevalence in primary care suggest that these individuals visit their referring physicians at about the same rate as the general population.6,9-11 Affected individuals are unlikely to seek psychiatric treatment unless they have a comorbid depression or anxiety.6,7
Table 1
DIFFERENTIAL DIAGNOSIS FOR SOCIAL ANXIETY DISORDER
| Condition | Diagnostic features |
|---|---|
| Posttraumatic stress disorder | Temporally follows traumatic event; cues related to trauma, not exclusively to social situations |
| Panic disorder | Unexpected panic attacks, not exclusively socially mediated anxiety |
| Agoraphobia | Fearful avoidance of situations in which panic attacks may occur, not limited to social situations |
| Major depression or atypical depression | Social withdrawal temporally related to mood disturbance, not to fear of humiliation or embarrassment; atypical depression with rejection sensitivity associated with other symptoms (e.g., hypersomnia, hyperphagia, anergy, mood reactivity) |
| Generalized anxiety disorder | Focus of worry not limited to social situations; social discomfort or avoidance not a key feature |
| Body dysmorphic disorder | Avoidance of social activity focused on concern over perceived ugliness |
| Avoidant personality disorder | Often present in generalized social anxiety disorder; may represent more severe end of social anxiety disorder spectrum; social activity desired but avoided |
| Schizotypal/schizoid personality disorders | Avoidance of social situations is preferred by individual and is not due to fear of embarrassment or humiliation |
| Normal shyness | Minimal or no interference with social, occupational, or family functioning |
| Adapted from Lydiard RB. Social anxiety disorder: comorbidity and its implications. J Clin Psychiatry.2001;62(suppl 1):17-23. | |
SAD can be difficult to tease apart from other coexisting conditions. Individuals who present for treatment of other anxiety disorders, depression, or substance abuse disorders should be considered at risk for current but undetected SAD. Many of the symptoms overlap (Table 1). The key diagnostic feature, which leads to the diagnosis of SAD, is that the fear and avoidance specifically are related to being in or anticipating a feared social situation (Box 4).
Social
- Attending parties, weddings etc.
- Conversing in a group
- Speaking on the telephone
- Interacting with authority figure (e.g., teacher or boss)
- Making eye contact
- Ordering in a restaurant
Performance
- Public speaking
- Eating in public
- Writing a check
- Using a public toilet
- Taking a test
- Trying on clothes in a store
- Speaking up at a meeting
Many clinicians mistake social anxiety for panic disorder, since panic attacks in people with SAD are often cued by social situations. There can be up to a 40% overlap of SAD with panic disorder.4 Without probing carefully into the focus on fear and avoidance, SAD can be easily overlooked. Individuals with panic disorder experience unexpected attacks and are terrified at the prospect of additional attacks, while those with SAD experience attacks linked to social situations and fear scrutiny and embarrassment more than the attacks themselves.
SAD and major depression frequently coexist,4,11,12 challenging clinicians to distinguish social reticence and withdrawal accompanying depression from the fearful avoidance that typifies SAD. SAD usually precedes depression. Asking if the patient experienced social anxiety prior to the onset of depression can help identify SAD with comorbid depression.
Alcohol-related disorders are twice as likely to occur in those affected by SAD as in those not affected. The risk for females increases more than it does for males.2-4 SAD most often precedes alcohol abuse. Studies show that about 30% of patients receiving treatment for alcohol abuse/dependence have SAD. If it remains undetected, the risk of rapid relapse is high. That’s because patients are highly unlikely to participate in psychosocial treatments that help sustain post-treatment abstinence, such as the Alcoholics Anonymous 12-step program. A recent study found that both social anxiety and alcohol abuse disorders improve when SAD in alcoholics is treated.13
A substantially higher percentage of adults with SAD, especially women, have histories of prior childhood sexual and/or physical abuse than the general population.14 Recent studies both in women following rape and in combat veterans with posttraumatic stress disorder (PTSD) suggest that those with perceived life-threatening events are at higher risk for developing secondary SAD than are individuals who experience less severe trauma.15,16 We do not yet know if secondary SAD in trauma victims is different in character or response to treatment.
Individuals with certain medical conditions can develop symptoms resembling SAD. These include stuttering, benign essential tremor,17 Parkinson’s disease, disfiguring burn injuries, and possibly irritable bowel syndrome. Such patients are technically excluded from being diagnosed with SAD, though they would meet criteria if the diagnostic rules were suspended. A limited body of literature and clinical experience suggests that symptoms secondary to physical conditions may respond to the same treatment as SAD in medically healthy persons. A treatment trial for selected patients with SAD symptoms associated with medical conditions may provide significant benefits. Clearly more research is needed in this area.
- “Being embarrassed or looking stupid are among my worst fears.”
- “Fear of embarrassment causes me to avoid doing things or speaking to people.”
- “I avoid activities in which I am the center of attention.”
Connor et al, Depress Anxiety 2001;14:137
A recently developed self-rating scale, the Social Phobia Inventory (SPIN), assesses the spectrum of cognitive, behavioral, and physiological symptoms associated with SAD.18 Three of the 17 SPIN items have been found to identify generalized SAD with a high degree of sensitivity (Box 5).
The 3 main goals of SAD treatment are
- Acute reduction and control of pathological anxiety and related phobic avoidance;
- Adequate treatment of depression or other comorbid conditions;
- Long-term management of the social phobia.
Significant advances in treatment have emerged over the past 2 decades. We now know that cognitive behavioral therapy (CBT), medication, and their combination are efficacious.
Social situations involving speaking or performance are usually predictable, and nongeneralized SAD is thus amenable to use of a beta-blocker or benzodiazepine (Box 6). Beta-blockers are often adequate for control of tremor and increased heart rate. Some patients may also benefit more from judicious use of a benzodiazepine prior to the event.
In contrast, generalized SAD is less predictable, and continual treatment is recommended. Ideally, a medication regimen would be easily tolerated long-term, and would have antidepressant effects and a broad spectrum of efficacy against commonly coexisting disorders. Because of the significant risk for depression in individuals with SAD, first-line antidepressant treatment is preferred when possible over other medications.
The selective serotonin reuptake inhibitors (SSRIs) are now considered the first-line pharmacological treatment for social phobia. Paroxetine was the first to receive FDA approval for generalized SAD.19 Large multicenter studies supporting the efficacy of two other SSRIs—sertraline and fluvoxamine—have been reported.12 The SSRIs also appear to work against the other psychiatric disorders with which SAD commonly co-occurs, such as panic disorder, major depression, generalized anxiety disorder, and PTSD.
The empirical database is very limited, but it appears that SSRI treatment for a significant percentage of patients with SAD may require higher doses (up to twice the amount) than are usually needed for depression.10 Approximately 50% to 65% of patients with generalized SAD respond to any given SSRI. In our experience, failure to respond to one SSRI does not preclude response to a second SSRI.
The irreversible monoamine oxidase (MAO) inhibitor phenelzine was the first antidepressant shown to be useful for SAD. Tranylcypromine is less well studied, but also appears to be effective. The significant side effects (weight gain, orthostatic hypotension, insomnia) and inconvenience of administration have reduced use of these agents.
Nongeneralized
- PRN treatment
- Beta-blockers
- Benzodiazepines
Generalized
- Continuous treatment
- Broad-spectrum antidepressants
- Benzodiazepines
- MAOIs
- Antiepileptic agents
The tricyclic antidepressants are probably not effective, with the exception of clomipramine (also a potent inhibitor of serotonin reuptake).12 Clomipramine, while an effective anxiolytic and antidepressant, causes prohibitive side effects in many patients (e.g., sexual dysfunction and weight gain).
Key elements for individual or group setting
- Cognitive “restructuring”
- Social skills enhancement
The newer antidepressants venlafaxine and nefazodone are less well studied than the SSRIs, but show promise as potential broad-spectrum agents. Bupropion, a novel antidepressant, and the azapirone anxiolytic buspirone do not appear to work against SAD.
The main role of the benzodiazepines in SAD treatment is adjunctive to antidepressants or in some patients intolerant of, or unresponsive to, other treatments. Clonazepam, alprazolam, and probably others are effective for SAD, but they may not effectively treat or prevent depression or other commonly associated disorders.
The anticonvulsant gabapentin has been shown in one controlled study to be effective in treating SAD.20 This agent may be particularly useful for complicated patients such as those with a history of alcohol-related disorders, bipolar-spectrum disorder, or intolerance to SSRIs.
In parallel with the development of effective psychopharmacological treatments, several types of behavioral and cognitive behavioral treatments have been investigated, including imaginal flooding, graduated exposure, social skills training, cognitive-behavior approaches, and combined cognitive restructuring and graduated exposure.21 These treatments involve similar elements targeted at the cognitive distortions and avoidance behaviors, which represent core features of SAD (Box 7).
Many clinicians believe that combined pharmacotherapy and CBT treatment are superior to either modality alone for treating SAD. The little empirical information available indicates that acute treatment differences between drug alone and drug in combination with CBT are not impressive. However, there appears to be a lower rate of relapse following CBT than after medication discontinuation.
Despite our ability to treat this disorder, only a small fraction of sufferers get treatment. If untreated, the risk of comorbidity is extremely high. Routine screening for SAD, especially in younger individuals, could provide for early detection and treatment. Psychiatrists can play an important role in early detection and treatment by educating consumers, teachers, school nurses, psychologists, and pediatricians.
Related resources
- Lydiard, R.B. Social anxiety disorder comorbidity and its implications J. Clin. Psychiatry. 2001;62(suppl):17-23.
- American Psychiatric Association, http://www.psych.org
- American Psychological Association, http://www.apa.org
- National Institute for Mental Health: Anxiety Disorders, http://www.nimh.nih.gov/anxiety/
- Anxiety Disorders Associations of America, http://www.adaa.org/
Drug brand names
- Alprazolam • Xanax
- Atenolol • Tenormin
- Bupropion • Wellbutrin
- Buspirone • Buspar
- Clomipramine • Anafranil
- Clonazepam • Klonopin
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Gabapentin • Neurontin
- Lorazepam • Ativan
- Nefazodone • Serzone
- Paroxetine • Paxil
- Phenelzine • Nardil
- Propranolol • Inderal
- Sertraline • Zoloft
- Tranylcypromine • Parnate
- Venlafaxine • Effexor
Disclosure
The author reports that he has received grant/research support and has served as a consultant to and on the speaker's bureau of Bristol-Myers Squibb Co., GlaxoSmithKline, Pfizer Inc., Eli Lilly and Co., Parke-Davis, and Solvay Pharmaceuticals. He also has received grant/research support and served as a consultant for Forest Pharmaceuticals, Wyeth-Ayerst Pharmaceuticals, and Roche; received grant/research support from Sanofi-Synthelabo; and has served as consultant for Dupont Pharmaceuticals and AstraZeneca.
1. Burton R. The Anatomy of Melancholy, vol. 1, 11th ed. London, England. Thomas Tegg, Cheapside; 1845.
2. Liebowitz MR, Gorman JM, Fyer AJ, Klein DF. Social phobia: review of a neglected anxiety disorder. Arch Gen Psychiatry. 1985;42:729-736.
3. Magee WJ, Eaton WW, Wittchen HU, et al. Agoraphobia, simple phobia, and social phobia in the National Comorbidity Survey. Arch Gen Psychiatry. 1996;53:159-168.
4. Schneier FR, Johnson J, et al. Social phobia: comorbidity and morbidity in an epidemiologic sample. Arch Gen Psychiatry. 1992;49:282-288.
5. Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8-19.
6. Goldenberg IM, et al. The infrequency of “pure culture” diagnosis among the anxiety disorders. J Clin Psychiatry. 1996;57:528-533.
7. Wittchen HU, Beloch E. The impact of social phobia on quality of life. Int Clin Psychopharmacol. 1996;11(suppl):15-23.
8. Greenberg PE, Sisitsky T, Kessler RC, et al. The economic burden of anxiety disorders in the 1990s. J Clin Psychiatry. 1999;60:427-435.
9. Weiller E, Bisserbe JC, Boyer P, et al. Social phobia in general health care. Br J Psychiatry. 1996;168:169-174.
10. Katzelnick DJ, Greist JH. Social anxiety disorder: an unrecognized problem in primary care. J Clin Psychiatry. 2001;62:11.-
11. Davidson J. Social anxiety disorder under scrutiny. Depress Anxiety. 2000;11:93-98.
12. Lydiard RB. Social anxiety disorder: treatment role of the SSRIs. In Montgomery SA, den Boer JA (eds). SSRIs in Depression and Anxiety Perspectives in Psychiatry ,vol 8. NY: Wiley, Chichester, 129-150, 2001.
13. Randall CL, et al. Paroxetine improves both social anxiety and alcohol use in dually-diagnosed patients at the American College of Neuropsychopharmacology. San Juan, Puerto Rico. Dec 10-15, 2000.
14. Stein MB, Walker JR, Anderson G, et al. Childhood physical and sexual abuse in patients with anxiety disorders and in a community sample. Am J Psychiatry. 1996;153:275-277.
15. Boudreaux E, Kilpatrick DG, Resnick HS, et al. Criminal victimization, posttraumatic stress disorder, and comorbid psychopathology among a community sample of women. J Trauma Stress. 1998;11:665-678.
16. Orsillo SM, Heimberg RG, Juster HR, Garrett J. Social phobia and PTSD in Vietnam veterans. J Trauma Stress. 1996;9:235-252.
17. George MS, Lydiard RB. Social phobia secondary to physical disability: a review of benign essential tremor (BET) and stuttering. Psychosomatics. 1994;35:520-523.
18. Connor KM, et al. Mini-SPIN: A brief screening assessment for generalized social anxiety disorder. Depress Anxiety. 2001;14:137-140.
19. Stein MB, Liebowitz MR, Lydiard RB, et al. Paroxetine treatment of generalized social phobia (social anxiety disorder): a randomized controlled trial. JAMA. 1998;280:708-713.
20. Pande AC, Davidson JR, Jefferson JW, et al. Treatment of social phobia with gabapentin: a placebo-controlled study. J Clin Psychopharmacol. 1999;19:341-348.
21. Heimberg RG. Specific issues in the cognitive behavioral treatment of social phobia. J Clin Psychiatry. 1993;54(suppl 12):36-45.
Social phobia was accorded official psychiatric diagnostic status in the United States less than 20 years ago, but has been described in the medical literature for centuries. Hippocrates described such a patient: “He dare not come in company for fear he should be misused, disgraced, overshoot himself in gestures or speeches or be sick; he thinks every man observes him.”1
This observation was made more than 2,000 years ago. Yet social anxiety disorder (SAD) was left largely unstudied until the mid-1980s.2 An estimated 20 million people in the U.S. suffer from this disorder.
What causes some people to break into a cold sweat at the thought of the most casual encounter with a checkout clerk, a coworker, or an acquaintance? Limited evidence points to underlying biological abnormalities in SAD, but there have been no conclusive findings.
Two main subtypes of SAD exist (Box 1). Roughly 25% of sufferers have discrete or nongeneralized SAD, that is, circumscribed social fears limited to one or two situations, such as speaking in public or performing before an audience. The remaining 75% suffer from generalized SAD, the more severe subtype in which all or nearly all interpersonal interactions are difficult.
Generalized SAD often begins early in life, with a mean onset at about age 15, but 35% of the time SAD occurs in individuals before age 10.3 This subtype appears to run in families, while the nongeneralized subtype does not, suggesting that a genetic inheritance is possible. From an etiological perspective, the possible effects of parenting styles of socially anxious parents, or acquisition of social anxiety conditioned by experiencing extreme embarrassment, may also contribute to the development of SAD in some people. Approximately twice as many females as males are affected, and almost all are affected before age 25.3,4 When social fears interfere with social, occupational, or family life, the affected individual is not suffering from normal "shyness," but rather a treatable anxiety disorder.
–Toastmasters slogan
Generalized
- Most social interactions
- Early onset
- Social skills deficit
- High comorbidity
- Lower achievement
- Remission rare
Nongeneralized
- Limited fears
- Later onset
- Social skills normal
- Less comorbidity
- Less Impairment
- Remits often
The National Comorbidity Survey (NCS) estimated lifetime prevalence of SAD at 13.3% and 12-month prevalence at 7.6%, making it the third most common psychiatric disorder, following only major depression and alcohol abuse/dependence.5 Despite this high rate, SAD remains woefully underdiagnosed.
Anyone who has had to speak in public, play a musical instrument at a recital, or perform in some way under the watchful expectation of an audience has experienced anxiety as he or she anticipates the "big moment” (Box 2). Once the performance is under way, the anxiety usually lessens to a more manageable level for most people. In fact, nearly one in three Americans will admit to moderate or great fear of speaking in public.
Mr. L, a 40-year-old eighth-grade teacher, consulted a psychiatrist because he was scheduled to be evaluated by a state education accreditation committee while teaching class. Though he had always passed these before, he had been worried sick for weeks and was experiencing panic attacks each time he thought about the accreditation visit.
He lived with his mother, had never dated, and had few friends. He was extremely inhibited outside the classroom, brought cash to stores to avoid being observed while writing a check or signing credit card slips, and avoided social gatherings outside of his church, which he attended with his mother and tolerated with distress.
Further history revealed that he had quit medical school during his third year because he had so much difficulty presenting cases to the attending on ward rounds that he chose to leave the profession in order to avoid feeling sick each morning and afternoon.
Enough people encounter the fear of public speaking to support the weekly Toastmasters meetings in most U.S. cities. Many people overcome their social anxiety about public speaking or performing with continued practice. However, those with nongeneralized SAD, who are among the most severely affected, may remain so fearful of speaking or performing under scrutiny that they avoid it at any cost—even if it means passing up a job or promotion or even choosing to change professions.
The majority (75%) of those with SAD—representing approximately 15 million individuals in the U.S.—suffer from generalized SAD, a much more severe, potentially disabling subtype. These unfortunate individuals fear and avoid most or all social interactions outside their home except those with family or close friends. When they encounter or even anticipate entering feared social situations, individuals with generalized SAD experience severe anxiety. Blushing, tremulousness, and sweating can be noticed by others, and thus are particularly distressing to those with SAD.
Recovery without treatment is rare. The typically early age at onset of generalized SAD3,4 imposes greater limitations on development of social competence than on those who develop more discrete fear of public speaking or performing later in life—after socialization skills have already developed.
Individuals with SAD frequently suffer from comorbid psychiatric disorders, mostly depression and/or other anxiety disorders.6Figure 1 shows that individuals with SAD are at significantly increased risk for depression, other anxiety disorders, and alcohol and drug abuse. Since generalized SAD usually appears at an earlier age than other anxiety disorders, it represents a risk factor for subsequent depression. The level of functional impairment caused by SAD is similar to that caused by major depression7 (Figure 2).
As more comorbid psychiatric disorders accrue, impairment and increased risk for additional disorders may occur. Further, the risk of suicide is increased in those with comorbid SAD vs. those with SAD only. The findings suggest that if social anxiety were detected and treated effectively at an early age, it might be possible to prevent other psychiatric disorders—particularly depression—as well as the predictable morbidity and mortality that accompanies untreated SAD. Given the estimated $44 billion annual cost of anxiety disorders in the U.S.,8 research targeted at testing this hypothesis would appear to be a good investment.
Figure 1 HOW PREVALENT IS LIFETIME COMORBIDITY IN SAD?
- Inherent avoidance of scrutiny, (e.g., evaluation)
- Uncertain diagnostic threshold
- Acceptance of pathological shyness as ‘just my personality’
- Lack of understanding by professionals, family, friends
- Coping strategies that mask disability
- Comorbid psychiatric disorders that mask SAD
Figure 2 QUALITY OF LIFE IN PATIENTS WITH SOCIAL ANXIETY DISORDER
Seeing the unseen: making the diagnosis quickly
Although SAD is extremely common, a variety of factors may contribute to the low rate of recognition of the disorder (Box 3). Because of their intense discomfort toward scrutiny by authority figures such as their physician, individuals with SAD may not be willing to discuss their fears. Studies estimating the prevalence in primary care suggest that these individuals visit their referring physicians at about the same rate as the general population.6,9-11 Affected individuals are unlikely to seek psychiatric treatment unless they have a comorbid depression or anxiety.6,7
Table 1
DIFFERENTIAL DIAGNOSIS FOR SOCIAL ANXIETY DISORDER
| Condition | Diagnostic features |
|---|---|
| Posttraumatic stress disorder | Temporally follows traumatic event; cues related to trauma, not exclusively to social situations |
| Panic disorder | Unexpected panic attacks, not exclusively socially mediated anxiety |
| Agoraphobia | Fearful avoidance of situations in which panic attacks may occur, not limited to social situations |
| Major depression or atypical depression | Social withdrawal temporally related to mood disturbance, not to fear of humiliation or embarrassment; atypical depression with rejection sensitivity associated with other symptoms (e.g., hypersomnia, hyperphagia, anergy, mood reactivity) |
| Generalized anxiety disorder | Focus of worry not limited to social situations; social discomfort or avoidance not a key feature |
| Body dysmorphic disorder | Avoidance of social activity focused on concern over perceived ugliness |
| Avoidant personality disorder | Often present in generalized social anxiety disorder; may represent more severe end of social anxiety disorder spectrum; social activity desired but avoided |
| Schizotypal/schizoid personality disorders | Avoidance of social situations is preferred by individual and is not due to fear of embarrassment or humiliation |
| Normal shyness | Minimal or no interference with social, occupational, or family functioning |
| Adapted from Lydiard RB. Social anxiety disorder: comorbidity and its implications. J Clin Psychiatry.2001;62(suppl 1):17-23. | |
SAD can be difficult to tease apart from other coexisting conditions. Individuals who present for treatment of other anxiety disorders, depression, or substance abuse disorders should be considered at risk for current but undetected SAD. Many of the symptoms overlap (Table 1). The key diagnostic feature, which leads to the diagnosis of SAD, is that the fear and avoidance specifically are related to being in or anticipating a feared social situation (Box 4).
Social
- Attending parties, weddings etc.
- Conversing in a group
- Speaking on the telephone
- Interacting with authority figure (e.g., teacher or boss)
- Making eye contact
- Ordering in a restaurant
Performance
- Public speaking
- Eating in public
- Writing a check
- Using a public toilet
- Taking a test
- Trying on clothes in a store
- Speaking up at a meeting
Many clinicians mistake social anxiety for panic disorder, since panic attacks in people with SAD are often cued by social situations. There can be up to a 40% overlap of SAD with panic disorder.4 Without probing carefully into the focus on fear and avoidance, SAD can be easily overlooked. Individuals with panic disorder experience unexpected attacks and are terrified at the prospect of additional attacks, while those with SAD experience attacks linked to social situations and fear scrutiny and embarrassment more than the attacks themselves.
SAD and major depression frequently coexist,4,11,12 challenging clinicians to distinguish social reticence and withdrawal accompanying depression from the fearful avoidance that typifies SAD. SAD usually precedes depression. Asking if the patient experienced social anxiety prior to the onset of depression can help identify SAD with comorbid depression.
Alcohol-related disorders are twice as likely to occur in those affected by SAD as in those not affected. The risk for females increases more than it does for males.2-4 SAD most often precedes alcohol abuse. Studies show that about 30% of patients receiving treatment for alcohol abuse/dependence have SAD. If it remains undetected, the risk of rapid relapse is high. That’s because patients are highly unlikely to participate in psychosocial treatments that help sustain post-treatment abstinence, such as the Alcoholics Anonymous 12-step program. A recent study found that both social anxiety and alcohol abuse disorders improve when SAD in alcoholics is treated.13
A substantially higher percentage of adults with SAD, especially women, have histories of prior childhood sexual and/or physical abuse than the general population.14 Recent studies both in women following rape and in combat veterans with posttraumatic stress disorder (PTSD) suggest that those with perceived life-threatening events are at higher risk for developing secondary SAD than are individuals who experience less severe trauma.15,16 We do not yet know if secondary SAD in trauma victims is different in character or response to treatment.
Individuals with certain medical conditions can develop symptoms resembling SAD. These include stuttering, benign essential tremor,17 Parkinson’s disease, disfiguring burn injuries, and possibly irritable bowel syndrome. Such patients are technically excluded from being diagnosed with SAD, though they would meet criteria if the diagnostic rules were suspended. A limited body of literature and clinical experience suggests that symptoms secondary to physical conditions may respond to the same treatment as SAD in medically healthy persons. A treatment trial for selected patients with SAD symptoms associated with medical conditions may provide significant benefits. Clearly more research is needed in this area.
- “Being embarrassed or looking stupid are among my worst fears.”
- “Fear of embarrassment causes me to avoid doing things or speaking to people.”
- “I avoid activities in which I am the center of attention.”
Connor et al, Depress Anxiety 2001;14:137
A recently developed self-rating scale, the Social Phobia Inventory (SPIN), assesses the spectrum of cognitive, behavioral, and physiological symptoms associated with SAD.18 Three of the 17 SPIN items have been found to identify generalized SAD with a high degree of sensitivity (Box 5).
The 3 main goals of SAD treatment are
- Acute reduction and control of pathological anxiety and related phobic avoidance;
- Adequate treatment of depression or other comorbid conditions;
- Long-term management of the social phobia.
Significant advances in treatment have emerged over the past 2 decades. We now know that cognitive behavioral therapy (CBT), medication, and their combination are efficacious.
Social situations involving speaking or performance are usually predictable, and nongeneralized SAD is thus amenable to use of a beta-blocker or benzodiazepine (Box 6). Beta-blockers are often adequate for control of tremor and increased heart rate. Some patients may also benefit more from judicious use of a benzodiazepine prior to the event.
In contrast, generalized SAD is less predictable, and continual treatment is recommended. Ideally, a medication regimen would be easily tolerated long-term, and would have antidepressant effects and a broad spectrum of efficacy against commonly coexisting disorders. Because of the significant risk for depression in individuals with SAD, first-line antidepressant treatment is preferred when possible over other medications.
The selective serotonin reuptake inhibitors (SSRIs) are now considered the first-line pharmacological treatment for social phobia. Paroxetine was the first to receive FDA approval for generalized SAD.19 Large multicenter studies supporting the efficacy of two other SSRIs—sertraline and fluvoxamine—have been reported.12 The SSRIs also appear to work against the other psychiatric disorders with which SAD commonly co-occurs, such as panic disorder, major depression, generalized anxiety disorder, and PTSD.
The empirical database is very limited, but it appears that SSRI treatment for a significant percentage of patients with SAD may require higher doses (up to twice the amount) than are usually needed for depression.10 Approximately 50% to 65% of patients with generalized SAD respond to any given SSRI. In our experience, failure to respond to one SSRI does not preclude response to a second SSRI.
The irreversible monoamine oxidase (MAO) inhibitor phenelzine was the first antidepressant shown to be useful for SAD. Tranylcypromine is less well studied, but also appears to be effective. The significant side effects (weight gain, orthostatic hypotension, insomnia) and inconvenience of administration have reduced use of these agents.
Nongeneralized
- PRN treatment
- Beta-blockers
- Benzodiazepines
Generalized
- Continuous treatment
- Broad-spectrum antidepressants
- Benzodiazepines
- MAOIs
- Antiepileptic agents
The tricyclic antidepressants are probably not effective, with the exception of clomipramine (also a potent inhibitor of serotonin reuptake).12 Clomipramine, while an effective anxiolytic and antidepressant, causes prohibitive side effects in many patients (e.g., sexual dysfunction and weight gain).
Key elements for individual or group setting
- Cognitive “restructuring”
- Social skills enhancement
The newer antidepressants venlafaxine and nefazodone are less well studied than the SSRIs, but show promise as potential broad-spectrum agents. Bupropion, a novel antidepressant, and the azapirone anxiolytic buspirone do not appear to work against SAD.
The main role of the benzodiazepines in SAD treatment is adjunctive to antidepressants or in some patients intolerant of, or unresponsive to, other treatments. Clonazepam, alprazolam, and probably others are effective for SAD, but they may not effectively treat or prevent depression or other commonly associated disorders.
The anticonvulsant gabapentin has been shown in one controlled study to be effective in treating SAD.20 This agent may be particularly useful for complicated patients such as those with a history of alcohol-related disorders, bipolar-spectrum disorder, or intolerance to SSRIs.
In parallel with the development of effective psychopharmacological treatments, several types of behavioral and cognitive behavioral treatments have been investigated, including imaginal flooding, graduated exposure, social skills training, cognitive-behavior approaches, and combined cognitive restructuring and graduated exposure.21 These treatments involve similar elements targeted at the cognitive distortions and avoidance behaviors, which represent core features of SAD (Box 7).
Many clinicians believe that combined pharmacotherapy and CBT treatment are superior to either modality alone for treating SAD. The little empirical information available indicates that acute treatment differences between drug alone and drug in combination with CBT are not impressive. However, there appears to be a lower rate of relapse following CBT than after medication discontinuation.
Despite our ability to treat this disorder, only a small fraction of sufferers get treatment. If untreated, the risk of comorbidity is extremely high. Routine screening for SAD, especially in younger individuals, could provide for early detection and treatment. Psychiatrists can play an important role in early detection and treatment by educating consumers, teachers, school nurses, psychologists, and pediatricians.
Related resources
- Lydiard, R.B. Social anxiety disorder comorbidity and its implications J. Clin. Psychiatry. 2001;62(suppl):17-23.
- American Psychiatric Association, http://www.psych.org
- American Psychological Association, http://www.apa.org
- National Institute for Mental Health: Anxiety Disorders, http://www.nimh.nih.gov/anxiety/
- Anxiety Disorders Associations of America, http://www.adaa.org/
Drug brand names
- Alprazolam • Xanax
- Atenolol • Tenormin
- Bupropion • Wellbutrin
- Buspirone • Buspar
- Clomipramine • Anafranil
- Clonazepam • Klonopin
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Gabapentin • Neurontin
- Lorazepam • Ativan
- Nefazodone • Serzone
- Paroxetine • Paxil
- Phenelzine • Nardil
- Propranolol • Inderal
- Sertraline • Zoloft
- Tranylcypromine • Parnate
- Venlafaxine • Effexor
Disclosure
The author reports that he has received grant/research support and has served as a consultant to and on the speaker's bureau of Bristol-Myers Squibb Co., GlaxoSmithKline, Pfizer Inc., Eli Lilly and Co., Parke-Davis, and Solvay Pharmaceuticals. He also has received grant/research support and served as a consultant for Forest Pharmaceuticals, Wyeth-Ayerst Pharmaceuticals, and Roche; received grant/research support from Sanofi-Synthelabo; and has served as consultant for Dupont Pharmaceuticals and AstraZeneca.
Social phobia was accorded official psychiatric diagnostic status in the United States less than 20 years ago, but has been described in the medical literature for centuries. Hippocrates described such a patient: “He dare not come in company for fear he should be misused, disgraced, overshoot himself in gestures or speeches or be sick; he thinks every man observes him.”1
This observation was made more than 2,000 years ago. Yet social anxiety disorder (SAD) was left largely unstudied until the mid-1980s.2 An estimated 20 million people in the U.S. suffer from this disorder.
What causes some people to break into a cold sweat at the thought of the most casual encounter with a checkout clerk, a coworker, or an acquaintance? Limited evidence points to underlying biological abnormalities in SAD, but there have been no conclusive findings.
Two main subtypes of SAD exist (Box 1). Roughly 25% of sufferers have discrete or nongeneralized SAD, that is, circumscribed social fears limited to one or two situations, such as speaking in public or performing before an audience. The remaining 75% suffer from generalized SAD, the more severe subtype in which all or nearly all interpersonal interactions are difficult.
Generalized SAD often begins early in life, with a mean onset at about age 15, but 35% of the time SAD occurs in individuals before age 10.3 This subtype appears to run in families, while the nongeneralized subtype does not, suggesting that a genetic inheritance is possible. From an etiological perspective, the possible effects of parenting styles of socially anxious parents, or acquisition of social anxiety conditioned by experiencing extreme embarrassment, may also contribute to the development of SAD in some people. Approximately twice as many females as males are affected, and almost all are affected before age 25.3,4 When social fears interfere with social, occupational, or family life, the affected individual is not suffering from normal "shyness," but rather a treatable anxiety disorder.
–Toastmasters slogan
Generalized
- Most social interactions
- Early onset
- Social skills deficit
- High comorbidity
- Lower achievement
- Remission rare
Nongeneralized
- Limited fears
- Later onset
- Social skills normal
- Less comorbidity
- Less Impairment
- Remits often
The National Comorbidity Survey (NCS) estimated lifetime prevalence of SAD at 13.3% and 12-month prevalence at 7.6%, making it the third most common psychiatric disorder, following only major depression and alcohol abuse/dependence.5 Despite this high rate, SAD remains woefully underdiagnosed.
Anyone who has had to speak in public, play a musical instrument at a recital, or perform in some way under the watchful expectation of an audience has experienced anxiety as he or she anticipates the "big moment” (Box 2). Once the performance is under way, the anxiety usually lessens to a more manageable level for most people. In fact, nearly one in three Americans will admit to moderate or great fear of speaking in public.
Mr. L, a 40-year-old eighth-grade teacher, consulted a psychiatrist because he was scheduled to be evaluated by a state education accreditation committee while teaching class. Though he had always passed these before, he had been worried sick for weeks and was experiencing panic attacks each time he thought about the accreditation visit.
He lived with his mother, had never dated, and had few friends. He was extremely inhibited outside the classroom, brought cash to stores to avoid being observed while writing a check or signing credit card slips, and avoided social gatherings outside of his church, which he attended with his mother and tolerated with distress.
Further history revealed that he had quit medical school during his third year because he had so much difficulty presenting cases to the attending on ward rounds that he chose to leave the profession in order to avoid feeling sick each morning and afternoon.
Enough people encounter the fear of public speaking to support the weekly Toastmasters meetings in most U.S. cities. Many people overcome their social anxiety about public speaking or performing with continued practice. However, those with nongeneralized SAD, who are among the most severely affected, may remain so fearful of speaking or performing under scrutiny that they avoid it at any cost—even if it means passing up a job or promotion or even choosing to change professions.
The majority (75%) of those with SAD—representing approximately 15 million individuals in the U.S.—suffer from generalized SAD, a much more severe, potentially disabling subtype. These unfortunate individuals fear and avoid most or all social interactions outside their home except those with family or close friends. When they encounter or even anticipate entering feared social situations, individuals with generalized SAD experience severe anxiety. Blushing, tremulousness, and sweating can be noticed by others, and thus are particularly distressing to those with SAD.
Recovery without treatment is rare. The typically early age at onset of generalized SAD3,4 imposes greater limitations on development of social competence than on those who develop more discrete fear of public speaking or performing later in life—after socialization skills have already developed.
Individuals with SAD frequently suffer from comorbid psychiatric disorders, mostly depression and/or other anxiety disorders.6Figure 1 shows that individuals with SAD are at significantly increased risk for depression, other anxiety disorders, and alcohol and drug abuse. Since generalized SAD usually appears at an earlier age than other anxiety disorders, it represents a risk factor for subsequent depression. The level of functional impairment caused by SAD is similar to that caused by major depression7 (Figure 2).
As more comorbid psychiatric disorders accrue, impairment and increased risk for additional disorders may occur. Further, the risk of suicide is increased in those with comorbid SAD vs. those with SAD only. The findings suggest that if social anxiety were detected and treated effectively at an early age, it might be possible to prevent other psychiatric disorders—particularly depression—as well as the predictable morbidity and mortality that accompanies untreated SAD. Given the estimated $44 billion annual cost of anxiety disorders in the U.S.,8 research targeted at testing this hypothesis would appear to be a good investment.
Figure 1 HOW PREVALENT IS LIFETIME COMORBIDITY IN SAD?
- Inherent avoidance of scrutiny, (e.g., evaluation)
- Uncertain diagnostic threshold
- Acceptance of pathological shyness as ‘just my personality’
- Lack of understanding by professionals, family, friends
- Coping strategies that mask disability
- Comorbid psychiatric disorders that mask SAD
Figure 2 QUALITY OF LIFE IN PATIENTS WITH SOCIAL ANXIETY DISORDER
Seeing the unseen: making the diagnosis quickly
Although SAD is extremely common, a variety of factors may contribute to the low rate of recognition of the disorder (Box 3). Because of their intense discomfort toward scrutiny by authority figures such as their physician, individuals with SAD may not be willing to discuss their fears. Studies estimating the prevalence in primary care suggest that these individuals visit their referring physicians at about the same rate as the general population.6,9-11 Affected individuals are unlikely to seek psychiatric treatment unless they have a comorbid depression or anxiety.6,7
Table 1
DIFFERENTIAL DIAGNOSIS FOR SOCIAL ANXIETY DISORDER
| Condition | Diagnostic features |
|---|---|
| Posttraumatic stress disorder | Temporally follows traumatic event; cues related to trauma, not exclusively to social situations |
| Panic disorder | Unexpected panic attacks, not exclusively socially mediated anxiety |
| Agoraphobia | Fearful avoidance of situations in which panic attacks may occur, not limited to social situations |
| Major depression or atypical depression | Social withdrawal temporally related to mood disturbance, not to fear of humiliation or embarrassment; atypical depression with rejection sensitivity associated with other symptoms (e.g., hypersomnia, hyperphagia, anergy, mood reactivity) |
| Generalized anxiety disorder | Focus of worry not limited to social situations; social discomfort or avoidance not a key feature |
| Body dysmorphic disorder | Avoidance of social activity focused on concern over perceived ugliness |
| Avoidant personality disorder | Often present in generalized social anxiety disorder; may represent more severe end of social anxiety disorder spectrum; social activity desired but avoided |
| Schizotypal/schizoid personality disorders | Avoidance of social situations is preferred by individual and is not due to fear of embarrassment or humiliation |
| Normal shyness | Minimal or no interference with social, occupational, or family functioning |
| Adapted from Lydiard RB. Social anxiety disorder: comorbidity and its implications. J Clin Psychiatry.2001;62(suppl 1):17-23. | |
SAD can be difficult to tease apart from other coexisting conditions. Individuals who present for treatment of other anxiety disorders, depression, or substance abuse disorders should be considered at risk for current but undetected SAD. Many of the symptoms overlap (Table 1). The key diagnostic feature, which leads to the diagnosis of SAD, is that the fear and avoidance specifically are related to being in or anticipating a feared social situation (Box 4).
Social
- Attending parties, weddings etc.
- Conversing in a group
- Speaking on the telephone
- Interacting with authority figure (e.g., teacher or boss)
- Making eye contact
- Ordering in a restaurant
Performance
- Public speaking
- Eating in public
- Writing a check
- Using a public toilet
- Taking a test
- Trying on clothes in a store
- Speaking up at a meeting
Many clinicians mistake social anxiety for panic disorder, since panic attacks in people with SAD are often cued by social situations. There can be up to a 40% overlap of SAD with panic disorder.4 Without probing carefully into the focus on fear and avoidance, SAD can be easily overlooked. Individuals with panic disorder experience unexpected attacks and are terrified at the prospect of additional attacks, while those with SAD experience attacks linked to social situations and fear scrutiny and embarrassment more than the attacks themselves.
SAD and major depression frequently coexist,4,11,12 challenging clinicians to distinguish social reticence and withdrawal accompanying depression from the fearful avoidance that typifies SAD. SAD usually precedes depression. Asking if the patient experienced social anxiety prior to the onset of depression can help identify SAD with comorbid depression.
Alcohol-related disorders are twice as likely to occur in those affected by SAD as in those not affected. The risk for females increases more than it does for males.2-4 SAD most often precedes alcohol abuse. Studies show that about 30% of patients receiving treatment for alcohol abuse/dependence have SAD. If it remains undetected, the risk of rapid relapse is high. That’s because patients are highly unlikely to participate in psychosocial treatments that help sustain post-treatment abstinence, such as the Alcoholics Anonymous 12-step program. A recent study found that both social anxiety and alcohol abuse disorders improve when SAD in alcoholics is treated.13
A substantially higher percentage of adults with SAD, especially women, have histories of prior childhood sexual and/or physical abuse than the general population.14 Recent studies both in women following rape and in combat veterans with posttraumatic stress disorder (PTSD) suggest that those with perceived life-threatening events are at higher risk for developing secondary SAD than are individuals who experience less severe trauma.15,16 We do not yet know if secondary SAD in trauma victims is different in character or response to treatment.
Individuals with certain medical conditions can develop symptoms resembling SAD. These include stuttering, benign essential tremor,17 Parkinson’s disease, disfiguring burn injuries, and possibly irritable bowel syndrome. Such patients are technically excluded from being diagnosed with SAD, though they would meet criteria if the diagnostic rules were suspended. A limited body of literature and clinical experience suggests that symptoms secondary to physical conditions may respond to the same treatment as SAD in medically healthy persons. A treatment trial for selected patients with SAD symptoms associated with medical conditions may provide significant benefits. Clearly more research is needed in this area.
- “Being embarrassed or looking stupid are among my worst fears.”
- “Fear of embarrassment causes me to avoid doing things or speaking to people.”
- “I avoid activities in which I am the center of attention.”
Connor et al, Depress Anxiety 2001;14:137
A recently developed self-rating scale, the Social Phobia Inventory (SPIN), assesses the spectrum of cognitive, behavioral, and physiological symptoms associated with SAD.18 Three of the 17 SPIN items have been found to identify generalized SAD with a high degree of sensitivity (Box 5).
The 3 main goals of SAD treatment are
- Acute reduction and control of pathological anxiety and related phobic avoidance;
- Adequate treatment of depression or other comorbid conditions;
- Long-term management of the social phobia.
Significant advances in treatment have emerged over the past 2 decades. We now know that cognitive behavioral therapy (CBT), medication, and their combination are efficacious.
Social situations involving speaking or performance are usually predictable, and nongeneralized SAD is thus amenable to use of a beta-blocker or benzodiazepine (Box 6). Beta-blockers are often adequate for control of tremor and increased heart rate. Some patients may also benefit more from judicious use of a benzodiazepine prior to the event.
In contrast, generalized SAD is less predictable, and continual treatment is recommended. Ideally, a medication regimen would be easily tolerated long-term, and would have antidepressant effects and a broad spectrum of efficacy against commonly coexisting disorders. Because of the significant risk for depression in individuals with SAD, first-line antidepressant treatment is preferred when possible over other medications.
The selective serotonin reuptake inhibitors (SSRIs) are now considered the first-line pharmacological treatment for social phobia. Paroxetine was the first to receive FDA approval for generalized SAD.19 Large multicenter studies supporting the efficacy of two other SSRIs—sertraline and fluvoxamine—have been reported.12 The SSRIs also appear to work against the other psychiatric disorders with which SAD commonly co-occurs, such as panic disorder, major depression, generalized anxiety disorder, and PTSD.
The empirical database is very limited, but it appears that SSRI treatment for a significant percentage of patients with SAD may require higher doses (up to twice the amount) than are usually needed for depression.10 Approximately 50% to 65% of patients with generalized SAD respond to any given SSRI. In our experience, failure to respond to one SSRI does not preclude response to a second SSRI.
The irreversible monoamine oxidase (MAO) inhibitor phenelzine was the first antidepressant shown to be useful for SAD. Tranylcypromine is less well studied, but also appears to be effective. The significant side effects (weight gain, orthostatic hypotension, insomnia) and inconvenience of administration have reduced use of these agents.
Nongeneralized
- PRN treatment
- Beta-blockers
- Benzodiazepines
Generalized
- Continuous treatment
- Broad-spectrum antidepressants
- Benzodiazepines
- MAOIs
- Antiepileptic agents
The tricyclic antidepressants are probably not effective, with the exception of clomipramine (also a potent inhibitor of serotonin reuptake).12 Clomipramine, while an effective anxiolytic and antidepressant, causes prohibitive side effects in many patients (e.g., sexual dysfunction and weight gain).
Key elements for individual or group setting
- Cognitive “restructuring”
- Social skills enhancement
The newer antidepressants venlafaxine and nefazodone are less well studied than the SSRIs, but show promise as potential broad-spectrum agents. Bupropion, a novel antidepressant, and the azapirone anxiolytic buspirone do not appear to work against SAD.
The main role of the benzodiazepines in SAD treatment is adjunctive to antidepressants or in some patients intolerant of, or unresponsive to, other treatments. Clonazepam, alprazolam, and probably others are effective for SAD, but they may not effectively treat or prevent depression or other commonly associated disorders.
The anticonvulsant gabapentin has been shown in one controlled study to be effective in treating SAD.20 This agent may be particularly useful for complicated patients such as those with a history of alcohol-related disorders, bipolar-spectrum disorder, or intolerance to SSRIs.
In parallel with the development of effective psychopharmacological treatments, several types of behavioral and cognitive behavioral treatments have been investigated, including imaginal flooding, graduated exposure, social skills training, cognitive-behavior approaches, and combined cognitive restructuring and graduated exposure.21 These treatments involve similar elements targeted at the cognitive distortions and avoidance behaviors, which represent core features of SAD (Box 7).
Many clinicians believe that combined pharmacotherapy and CBT treatment are superior to either modality alone for treating SAD. The little empirical information available indicates that acute treatment differences between drug alone and drug in combination with CBT are not impressive. However, there appears to be a lower rate of relapse following CBT than after medication discontinuation.
Despite our ability to treat this disorder, only a small fraction of sufferers get treatment. If untreated, the risk of comorbidity is extremely high. Routine screening for SAD, especially in younger individuals, could provide for early detection and treatment. Psychiatrists can play an important role in early detection and treatment by educating consumers, teachers, school nurses, psychologists, and pediatricians.
Related resources
- Lydiard, R.B. Social anxiety disorder comorbidity and its implications J. Clin. Psychiatry. 2001;62(suppl):17-23.
- American Psychiatric Association, http://www.psych.org
- American Psychological Association, http://www.apa.org
- National Institute for Mental Health: Anxiety Disorders, http://www.nimh.nih.gov/anxiety/
- Anxiety Disorders Associations of America, http://www.adaa.org/
Drug brand names
- Alprazolam • Xanax
- Atenolol • Tenormin
- Bupropion • Wellbutrin
- Buspirone • Buspar
- Clomipramine • Anafranil
- Clonazepam • Klonopin
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Gabapentin • Neurontin
- Lorazepam • Ativan
- Nefazodone • Serzone
- Paroxetine • Paxil
- Phenelzine • Nardil
- Propranolol • Inderal
- Sertraline • Zoloft
- Tranylcypromine • Parnate
- Venlafaxine • Effexor
Disclosure
The author reports that he has received grant/research support and has served as a consultant to and on the speaker's bureau of Bristol-Myers Squibb Co., GlaxoSmithKline, Pfizer Inc., Eli Lilly and Co., Parke-Davis, and Solvay Pharmaceuticals. He also has received grant/research support and served as a consultant for Forest Pharmaceuticals, Wyeth-Ayerst Pharmaceuticals, and Roche; received grant/research support from Sanofi-Synthelabo; and has served as consultant for Dupont Pharmaceuticals and AstraZeneca.
1. Burton R. The Anatomy of Melancholy, vol. 1, 11th ed. London, England. Thomas Tegg, Cheapside; 1845.
2. Liebowitz MR, Gorman JM, Fyer AJ, Klein DF. Social phobia: review of a neglected anxiety disorder. Arch Gen Psychiatry. 1985;42:729-736.
3. Magee WJ, Eaton WW, Wittchen HU, et al. Agoraphobia, simple phobia, and social phobia in the National Comorbidity Survey. Arch Gen Psychiatry. 1996;53:159-168.
4. Schneier FR, Johnson J, et al. Social phobia: comorbidity and morbidity in an epidemiologic sample. Arch Gen Psychiatry. 1992;49:282-288.
5. Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8-19.
6. Goldenberg IM, et al. The infrequency of “pure culture” diagnosis among the anxiety disorders. J Clin Psychiatry. 1996;57:528-533.
7. Wittchen HU, Beloch E. The impact of social phobia on quality of life. Int Clin Psychopharmacol. 1996;11(suppl):15-23.
8. Greenberg PE, Sisitsky T, Kessler RC, et al. The economic burden of anxiety disorders in the 1990s. J Clin Psychiatry. 1999;60:427-435.
9. Weiller E, Bisserbe JC, Boyer P, et al. Social phobia in general health care. Br J Psychiatry. 1996;168:169-174.
10. Katzelnick DJ, Greist JH. Social anxiety disorder: an unrecognized problem in primary care. J Clin Psychiatry. 2001;62:11.-
11. Davidson J. Social anxiety disorder under scrutiny. Depress Anxiety. 2000;11:93-98.
12. Lydiard RB. Social anxiety disorder: treatment role of the SSRIs. In Montgomery SA, den Boer JA (eds). SSRIs in Depression and Anxiety Perspectives in Psychiatry ,vol 8. NY: Wiley, Chichester, 129-150, 2001.
13. Randall CL, et al. Paroxetine improves both social anxiety and alcohol use in dually-diagnosed patients at the American College of Neuropsychopharmacology. San Juan, Puerto Rico. Dec 10-15, 2000.
14. Stein MB, Walker JR, Anderson G, et al. Childhood physical and sexual abuse in patients with anxiety disorders and in a community sample. Am J Psychiatry. 1996;153:275-277.
15. Boudreaux E, Kilpatrick DG, Resnick HS, et al. Criminal victimization, posttraumatic stress disorder, and comorbid psychopathology among a community sample of women. J Trauma Stress. 1998;11:665-678.
16. Orsillo SM, Heimberg RG, Juster HR, Garrett J. Social phobia and PTSD in Vietnam veterans. J Trauma Stress. 1996;9:235-252.
17. George MS, Lydiard RB. Social phobia secondary to physical disability: a review of benign essential tremor (BET) and stuttering. Psychosomatics. 1994;35:520-523.
18. Connor KM, et al. Mini-SPIN: A brief screening assessment for generalized social anxiety disorder. Depress Anxiety. 2001;14:137-140.
19. Stein MB, Liebowitz MR, Lydiard RB, et al. Paroxetine treatment of generalized social phobia (social anxiety disorder): a randomized controlled trial. JAMA. 1998;280:708-713.
20. Pande AC, Davidson JR, Jefferson JW, et al. Treatment of social phobia with gabapentin: a placebo-controlled study. J Clin Psychopharmacol. 1999;19:341-348.
21. Heimberg RG. Specific issues in the cognitive behavioral treatment of social phobia. J Clin Psychiatry. 1993;54(suppl 12):36-45.
1. Burton R. The Anatomy of Melancholy, vol. 1, 11th ed. London, England. Thomas Tegg, Cheapside; 1845.
2. Liebowitz MR, Gorman JM, Fyer AJ, Klein DF. Social phobia: review of a neglected anxiety disorder. Arch Gen Psychiatry. 1985;42:729-736.
3. Magee WJ, Eaton WW, Wittchen HU, et al. Agoraphobia, simple phobia, and social phobia in the National Comorbidity Survey. Arch Gen Psychiatry. 1996;53:159-168.
4. Schneier FR, Johnson J, et al. Social phobia: comorbidity and morbidity in an epidemiologic sample. Arch Gen Psychiatry. 1992;49:282-288.
5. Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8-19.
6. Goldenberg IM, et al. The infrequency of “pure culture” diagnosis among the anxiety disorders. J Clin Psychiatry. 1996;57:528-533.
7. Wittchen HU, Beloch E. The impact of social phobia on quality of life. Int Clin Psychopharmacol. 1996;11(suppl):15-23.
8. Greenberg PE, Sisitsky T, Kessler RC, et al. The economic burden of anxiety disorders in the 1990s. J Clin Psychiatry. 1999;60:427-435.
9. Weiller E, Bisserbe JC, Boyer P, et al. Social phobia in general health care. Br J Psychiatry. 1996;168:169-174.
10. Katzelnick DJ, Greist JH. Social anxiety disorder: an unrecognized problem in primary care. J Clin Psychiatry. 2001;62:11.-
11. Davidson J. Social anxiety disorder under scrutiny. Depress Anxiety. 2000;11:93-98.
12. Lydiard RB. Social anxiety disorder: treatment role of the SSRIs. In Montgomery SA, den Boer JA (eds). SSRIs in Depression and Anxiety Perspectives in Psychiatry ,vol 8. NY: Wiley, Chichester, 129-150, 2001.
13. Randall CL, et al. Paroxetine improves both social anxiety and alcohol use in dually-diagnosed patients at the American College of Neuropsychopharmacology. San Juan, Puerto Rico. Dec 10-15, 2000.
14. Stein MB, Walker JR, Anderson G, et al. Childhood physical and sexual abuse in patients with anxiety disorders and in a community sample. Am J Psychiatry. 1996;153:275-277.
15. Boudreaux E, Kilpatrick DG, Resnick HS, et al. Criminal victimization, posttraumatic stress disorder, and comorbid psychopathology among a community sample of women. J Trauma Stress. 1998;11:665-678.
16. Orsillo SM, Heimberg RG, Juster HR, Garrett J. Social phobia and PTSD in Vietnam veterans. J Trauma Stress. 1996;9:235-252.
17. George MS, Lydiard RB. Social phobia secondary to physical disability: a review of benign essential tremor (BET) and stuttering. Psychosomatics. 1994;35:520-523.
18. Connor KM, et al. Mini-SPIN: A brief screening assessment for generalized social anxiety disorder. Depress Anxiety. 2001;14:137-140.
19. Stein MB, Liebowitz MR, Lydiard RB, et al. Paroxetine treatment of generalized social phobia (social anxiety disorder): a randomized controlled trial. JAMA. 1998;280:708-713.
20. Pande AC, Davidson JR, Jefferson JW, et al. Treatment of social phobia with gabapentin: a placebo-controlled study. J Clin Psychopharmacol. 1999;19:341-348.
21. Heimberg RG. Specific issues in the cognitive behavioral treatment of social phobia. J Clin Psychiatry. 1993;54(suppl 12):36-45.