User login
Know the general work-up and contraindications
Case
A 56-year-old female comes to the hospitalist service for presumed sepsis with acute renal insufficiency. She has a history of steadily progressive Parkinson’s disease. Vital signs show a temperature of 104° F; heart rate,135; BP, 100/70; respiratory rate, 20; oxygen saturation, 100% on room air. She is rigid on exam with creatine kinase, 2450 IU/L, and serum creatinine, 2.2. History reveals the patient’s levodopa was increased to 1,200 mg/day recently, then stopped by the family after she became paranoid. A diagnosis of neuroleptic malignant syndrome (NMS) is made.
Background
Electroconvulsive therapy (ECT) has been the gold standard for treatment of refractory psychiatric disease for decades. While it has proven beneficial for both medical and psychiatric disorders, it remains surrounded in controversy. Additionally, there is a significant degree of discomfort among nonpsychiatric providers on when to consider ECT, as well as how to evaluate the patient and manage their comorbidities before and during the procedure1.
Hospitalists should be familiar with the relative contraindications and general work-up for ECT, which can expedite both psychiatric and anesthesia evaluations and minimize adverse outcomes.
While the mechanism of action still is not known, ECT exerts a variety of effects in the brain and periphery. The dominant theory is that ECT increases neurotransmitter activity throughout the brain. Studies have shown increased GABA transmission, normalized glutamate transmission, and resetting of the hypothalamic-pituitary axis, as well as activation of downstream signal transduction pathways leading to increased synaptic connectivity in the brain. Many of ECT’s results may be caused by combinations of the above mechanisms2.
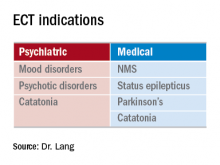
ECT principally is indicated for refractory mood and psychotic disorders. These include schizophrenia, bipolar disorder, and major depression. ECT-responsive patients typically have failed multiple appropriate medication trials and often have prolonged hospitalizations. What is less known are the medical indications for this procedure. Examples include Parkinson’s disease (especially with on/off phenomenon), status epilepticus, and neuroleptic malignant syndrome. Additionally, ECT has been shown to be beneficial for slow-to-resolve delirium and catatonia (regardless of etiology).
A psychiatrist also may take into consideration factors such as past response to ECT or the level of urgency to the patient’s presentation. A general work-up includes basic comprehensive metabolic panel, complete blood count, chest x-ray, EKG, and other testing based on history, physical, and past medical history.
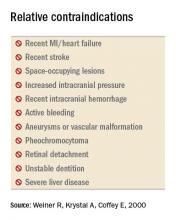
While there are no absolute contraindications to ECT, several relative contraindications exist. These include recent MI or stroke (generally within the last 30 days), increased intracranial pressure, active bleeding (especially from the central nervous system), retinal detachment, and unstable dentition. Apart from making sure the technique is medically indicated, an ECT consultant also evaluates the medical comorbidities. The patient may require treatment, such as removal of unstable dentition prior to the procedure, if clinical urgency does not preclude a delay.
Select patients require more detailed consultation prior to the onset of anesthesia. Examples would include patients with pseudocholinesterase deficiency, myasthenia gravis, or pregnancy. Pregnancy often is considered a contraindication, but ECT has no notable effect on labor & delivery, fetal injury, or development. It would be a preferred modality over medications, especially in unstable mothers during the first trimester. ECT exerts little effect on the fetus, as the amount of current that actually gets to the fetus is negligible6.
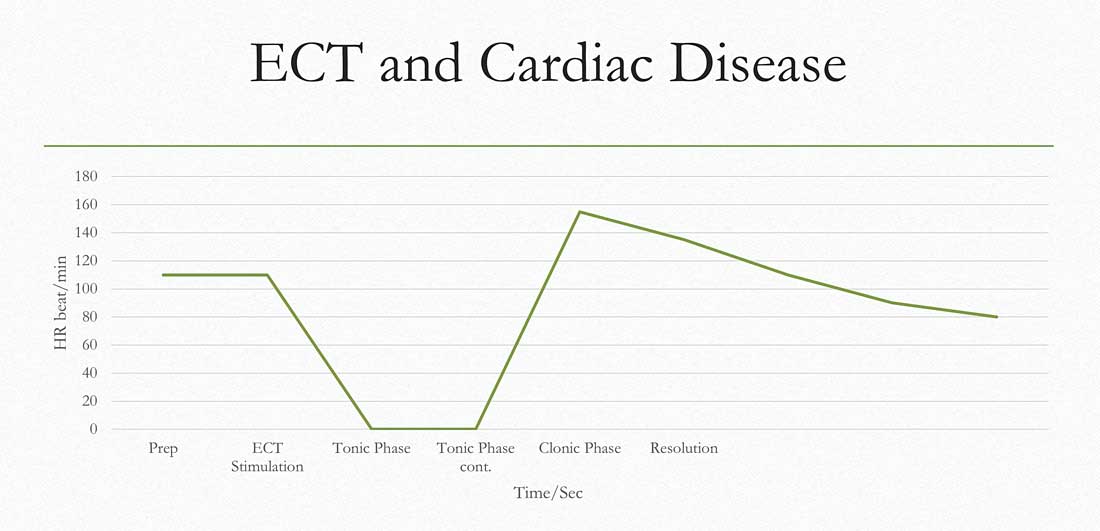
Outside the central nervous system, ECT exerts the most influence over the cardiovascular system. During the tonic phase of a seizure, increased vagal tone can depress the heart rate to asystole in some patients (see chart below). This may last for 3-4 seconds until the clonic phase occurs (with a noradrenergic surge), whereupon the heart rate can accelerate to the 140s. Unless unstable cardiac disease is present, patients typically tolerate this extremely well without any adverse sequela7. Studies involving patients who have severe aortic stenosis and pacemakers/defibrillators show overall excellent tolerability8,9.
Medications can have an impact on the onset, quality, and duration of seizures. Thus, a careful medication review is needed. A consultant will look first for medications such as benzodiazepines or anticonvulsants that would raise the seizure threshold. Ideally, the medications would be stopped, but if not feasible, they can be held the night before (or the day before in the case of such long half-life agents as diazepam) to minimize their impact.
As for anticonvulsants, the doses can be reduced, along with modest increases in energy settings to facilitate seizure. If used for mood stabilization only, one could consider stopping them completely, but this is usually not required (it is not recommended to stop them if used for epilepsy). Lithium can lead to prolonged neuromuscular blockade, prolonged seizures, or postictal delirium. However, discontinuation of lithium also has a risk-benefit consideration, so usually, doses are reduced and/or decreased doses of neuromuscular blockade are employed. Theophylline can induce extended seizures or status epilepticus so it is usually held prior to ECT.
Back to the case
Given the patient’s severe Parkinson’s disease and concurrent NMS, ECT was initiated. By the second treatment, fever and tachycardia resolved. By the sixth treatment, all NMS symptoms and associated paranoia had completely resolved and her Parkinson’s disease rating scale score went from 142 to 42. Her levodopa dose was reduced from 1,200 to 300 mg/day. She remained stable for years afterward.
Bottom line
ECT is both effective and well tolerated in patients who have received appropriate medical evaluation.
Dr. Lang is clinical associate professor in the departments of psychiatry and internal medicine and director of the electroconvulsive therapy and transcranial magnetic stimulation programs at East Carolina University, Greenville, N.C.
Key points
- ECT is indicated for psychotic and depressive disorders, with high efficacy and rapid response.
- ECT also has proven benefits for NMS, catatonia, delirium, status epilepticus, and Parkinson’s disease.
- Evaluation and focused treatment of relative contraindications maximizes both safety and tolerability of ECT.
References
1. Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
2. Baghai T et al. Electroconvulsive therapy and its different indications. Dialogues Clin Neurosci. Mar 2008;10(1):105-17.
3. Ozer F et al. Electroconvulsive therapy in drug-induced psychiatric states and neuroleptic malignant syndrome. J ECT. 2005 Jun;21(2):125-7.
4. Taylor S. Electroconvulsive therapy: A review of history, patient selection, technique, and medication management. South Med J. 2007 May;100(5):494-8.
5. The Practice of Electroconvulsive Therapy, 2nd edition. A Task Force Report of the American Psychiatric Association. 2001. pp. 84-85.
6. Miller LJ. Use of electroconvulsive therapy during pregnancy. Hosp Community Psychiatry. 1994 May;45(5):444-50.
7. Miller R et al. ECT: Physiologic Effects. Miller’s Anesthesia. 7th Edition. 2009.
8. Mueller PS et al. The Safety of electroconvulsive therapy in patients with severe aortic stenosis. Mayo Clin Proc. 2007 Nov;82(11):1360-3.
9. Dolenc TJ et al. Electroconvulsive therapy in patients with cardiac pacemakers & implantable cardioverter defibrillators. Pacing Clin Electrophysiol. 2004 Sep;27(9):1257-63.
Suggested readings
The practice of electroconvulsive therapy: Recommendations for treatment, training, and privileging (A Task Force Report of the American Psychiatric Association), 2nd Edition. APA Publishing. 2001.
Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
Rosenquist P et al. Charting the course of electroconvulsive therapy: Where have we been and where are we headed? J Psychosoc Nurs Ment Health Serv. 2016 Dec 1;54(12):39-43.
QUIZ
1. All of the following are indications for ECT except?
A. Schizophrenia.
B. Panic attacks.
C. Bipolar mania.
D. Catatonia.
Answer: B. Panic attacks. ECT is not effective for anxiety disorders including panic, generalized anxiety, PTSD, or OCD.
2. The most commonly accepted mechanism of action for ECT is?
A. Reduction in glutamate levels.
B. Altering signal transduction pathways.
C. Increased neurotransmitter activity.
D. Increased cerebral blood flow.
Answer: C. Increased neurotransmitter activity. There are data to support all, but neurotransmitter flow is most accepted thus far.
3. Which of the following is a common side effect of ECT?
A. Bronchospasm.
B. Diarrhea.
C. Delirium.
D. Visual changes.
Answer: C. Delirium. The rest are rare or not noted.
4. Which of the following is a relative contraindication for ECT?
A. Pregnancy.
B. Epilepsy.
C. Advanced age.
D. Increased intracranial pressure.
Answer: D. Increased intracranial pressure.
Know the general work-up and contraindications
Know the general work-up and contraindications
Case
A 56-year-old female comes to the hospitalist service for presumed sepsis with acute renal insufficiency. She has a history of steadily progressive Parkinson’s disease. Vital signs show a temperature of 104° F; heart rate,135; BP, 100/70; respiratory rate, 20; oxygen saturation, 100% on room air. She is rigid on exam with creatine kinase, 2450 IU/L, and serum creatinine, 2.2. History reveals the patient’s levodopa was increased to 1,200 mg/day recently, then stopped by the family after she became paranoid. A diagnosis of neuroleptic malignant syndrome (NMS) is made.
Background
Electroconvulsive therapy (ECT) has been the gold standard for treatment of refractory psychiatric disease for decades. While it has proven beneficial for both medical and psychiatric disorders, it remains surrounded in controversy. Additionally, there is a significant degree of discomfort among nonpsychiatric providers on when to consider ECT, as well as how to evaluate the patient and manage their comorbidities before and during the procedure1.
Hospitalists should be familiar with the relative contraindications and general work-up for ECT, which can expedite both psychiatric and anesthesia evaluations and minimize adverse outcomes.
While the mechanism of action still is not known, ECT exerts a variety of effects in the brain and periphery. The dominant theory is that ECT increases neurotransmitter activity throughout the brain. Studies have shown increased GABA transmission, normalized glutamate transmission, and resetting of the hypothalamic-pituitary axis, as well as activation of downstream signal transduction pathways leading to increased synaptic connectivity in the brain. Many of ECT’s results may be caused by combinations of the above mechanisms2.
ECT principally is indicated for refractory mood and psychotic disorders. These include schizophrenia, bipolar disorder, and major depression. ECT-responsive patients typically have failed multiple appropriate medication trials and often have prolonged hospitalizations. What is less known are the medical indications for this procedure. Examples include Parkinson’s disease (especially with on/off phenomenon), status epilepticus, and neuroleptic malignant syndrome. Additionally, ECT has been shown to be beneficial for slow-to-resolve delirium and catatonia (regardless of etiology).
A psychiatrist also may take into consideration factors such as past response to ECT or the level of urgency to the patient’s presentation. A general work-up includes basic comprehensive metabolic panel, complete blood count, chest x-ray, EKG, and other testing based on history, physical, and past medical history.
While there are no absolute contraindications to ECT, several relative contraindications exist. These include recent MI or stroke (generally within the last 30 days), increased intracranial pressure, active bleeding (especially from the central nervous system), retinal detachment, and unstable dentition. Apart from making sure the technique is medically indicated, an ECT consultant also evaluates the medical comorbidities. The patient may require treatment, such as removal of unstable dentition prior to the procedure, if clinical urgency does not preclude a delay.
Select patients require more detailed consultation prior to the onset of anesthesia. Examples would include patients with pseudocholinesterase deficiency, myasthenia gravis, or pregnancy. Pregnancy often is considered a contraindication, but ECT has no notable effect on labor & delivery, fetal injury, or development. It would be a preferred modality over medications, especially in unstable mothers during the first trimester. ECT exerts little effect on the fetus, as the amount of current that actually gets to the fetus is negligible6.
Outside the central nervous system, ECT exerts the most influence over the cardiovascular system. During the tonic phase of a seizure, increased vagal tone can depress the heart rate to asystole in some patients (see chart below). This may last for 3-4 seconds until the clonic phase occurs (with a noradrenergic surge), whereupon the heart rate can accelerate to the 140s. Unless unstable cardiac disease is present, patients typically tolerate this extremely well without any adverse sequela7. Studies involving patients who have severe aortic stenosis and pacemakers/defibrillators show overall excellent tolerability8,9.
Medications can have an impact on the onset, quality, and duration of seizures. Thus, a careful medication review is needed. A consultant will look first for medications such as benzodiazepines or anticonvulsants that would raise the seizure threshold. Ideally, the medications would be stopped, but if not feasible, they can be held the night before (or the day before in the case of such long half-life agents as diazepam) to minimize their impact.
As for anticonvulsants, the doses can be reduced, along with modest increases in energy settings to facilitate seizure. If used for mood stabilization only, one could consider stopping them completely, but this is usually not required (it is not recommended to stop them if used for epilepsy). Lithium can lead to prolonged neuromuscular blockade, prolonged seizures, or postictal delirium. However, discontinuation of lithium also has a risk-benefit consideration, so usually, doses are reduced and/or decreased doses of neuromuscular blockade are employed. Theophylline can induce extended seizures or status epilepticus so it is usually held prior to ECT.
Back to the case
Given the patient’s severe Parkinson’s disease and concurrent NMS, ECT was initiated. By the second treatment, fever and tachycardia resolved. By the sixth treatment, all NMS symptoms and associated paranoia had completely resolved and her Parkinson’s disease rating scale score went from 142 to 42. Her levodopa dose was reduced from 1,200 to 300 mg/day. She remained stable for years afterward.
Bottom line
ECT is both effective and well tolerated in patients who have received appropriate medical evaluation.
Dr. Lang is clinical associate professor in the departments of psychiatry and internal medicine and director of the electroconvulsive therapy and transcranial magnetic stimulation programs at East Carolina University, Greenville, N.C.
Key points
- ECT is indicated for psychotic and depressive disorders, with high efficacy and rapid response.
- ECT also has proven benefits for NMS, catatonia, delirium, status epilepticus, and Parkinson’s disease.
- Evaluation and focused treatment of relative contraindications maximizes both safety and tolerability of ECT.
References
1. Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
2. Baghai T et al. Electroconvulsive therapy and its different indications. Dialogues Clin Neurosci. Mar 2008;10(1):105-17.
3. Ozer F et al. Electroconvulsive therapy in drug-induced psychiatric states and neuroleptic malignant syndrome. J ECT. 2005 Jun;21(2):125-7.
4. Taylor S. Electroconvulsive therapy: A review of history, patient selection, technique, and medication management. South Med J. 2007 May;100(5):494-8.
5. The Practice of Electroconvulsive Therapy, 2nd edition. A Task Force Report of the American Psychiatric Association. 2001. pp. 84-85.
6. Miller LJ. Use of electroconvulsive therapy during pregnancy. Hosp Community Psychiatry. 1994 May;45(5):444-50.
7. Miller R et al. ECT: Physiologic Effects. Miller’s Anesthesia. 7th Edition. 2009.
8. Mueller PS et al. The Safety of electroconvulsive therapy in patients with severe aortic stenosis. Mayo Clin Proc. 2007 Nov;82(11):1360-3.
9. Dolenc TJ et al. Electroconvulsive therapy in patients with cardiac pacemakers & implantable cardioverter defibrillators. Pacing Clin Electrophysiol. 2004 Sep;27(9):1257-63.
Suggested readings
The practice of electroconvulsive therapy: Recommendations for treatment, training, and privileging (A Task Force Report of the American Psychiatric Association), 2nd Edition. APA Publishing. 2001.
Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
Rosenquist P et al. Charting the course of electroconvulsive therapy: Where have we been and where are we headed? J Psychosoc Nurs Ment Health Serv. 2016 Dec 1;54(12):39-43.
QUIZ
1. All of the following are indications for ECT except?
A. Schizophrenia.
B. Panic attacks.
C. Bipolar mania.
D. Catatonia.
Answer: B. Panic attacks. ECT is not effective for anxiety disorders including panic, generalized anxiety, PTSD, or OCD.
2. The most commonly accepted mechanism of action for ECT is?
A. Reduction in glutamate levels.
B. Altering signal transduction pathways.
C. Increased neurotransmitter activity.
D. Increased cerebral blood flow.
Answer: C. Increased neurotransmitter activity. There are data to support all, but neurotransmitter flow is most accepted thus far.
3. Which of the following is a common side effect of ECT?
A. Bronchospasm.
B. Diarrhea.
C. Delirium.
D. Visual changes.
Answer: C. Delirium. The rest are rare or not noted.
4. Which of the following is a relative contraindication for ECT?
A. Pregnancy.
B. Epilepsy.
C. Advanced age.
D. Increased intracranial pressure.
Answer: D. Increased intracranial pressure.
Case
A 56-year-old female comes to the hospitalist service for presumed sepsis with acute renal insufficiency. She has a history of steadily progressive Parkinson’s disease. Vital signs show a temperature of 104° F; heart rate,135; BP, 100/70; respiratory rate, 20; oxygen saturation, 100% on room air. She is rigid on exam with creatine kinase, 2450 IU/L, and serum creatinine, 2.2. History reveals the patient’s levodopa was increased to 1,200 mg/day recently, then stopped by the family after she became paranoid. A diagnosis of neuroleptic malignant syndrome (NMS) is made.
Background
Electroconvulsive therapy (ECT) has been the gold standard for treatment of refractory psychiatric disease for decades. While it has proven beneficial for both medical and psychiatric disorders, it remains surrounded in controversy. Additionally, there is a significant degree of discomfort among nonpsychiatric providers on when to consider ECT, as well as how to evaluate the patient and manage their comorbidities before and during the procedure1.
Hospitalists should be familiar with the relative contraindications and general work-up for ECT, which can expedite both psychiatric and anesthesia evaluations and minimize adverse outcomes.
While the mechanism of action still is not known, ECT exerts a variety of effects in the brain and periphery. The dominant theory is that ECT increases neurotransmitter activity throughout the brain. Studies have shown increased GABA transmission, normalized glutamate transmission, and resetting of the hypothalamic-pituitary axis, as well as activation of downstream signal transduction pathways leading to increased synaptic connectivity in the brain. Many of ECT’s results may be caused by combinations of the above mechanisms2.
ECT principally is indicated for refractory mood and psychotic disorders. These include schizophrenia, bipolar disorder, and major depression. ECT-responsive patients typically have failed multiple appropriate medication trials and often have prolonged hospitalizations. What is less known are the medical indications for this procedure. Examples include Parkinson’s disease (especially with on/off phenomenon), status epilepticus, and neuroleptic malignant syndrome. Additionally, ECT has been shown to be beneficial for slow-to-resolve delirium and catatonia (regardless of etiology).
A psychiatrist also may take into consideration factors such as past response to ECT or the level of urgency to the patient’s presentation. A general work-up includes basic comprehensive metabolic panel, complete blood count, chest x-ray, EKG, and other testing based on history, physical, and past medical history.
While there are no absolute contraindications to ECT, several relative contraindications exist. These include recent MI or stroke (generally within the last 30 days), increased intracranial pressure, active bleeding (especially from the central nervous system), retinal detachment, and unstable dentition. Apart from making sure the technique is medically indicated, an ECT consultant also evaluates the medical comorbidities. The patient may require treatment, such as removal of unstable dentition prior to the procedure, if clinical urgency does not preclude a delay.
Select patients require more detailed consultation prior to the onset of anesthesia. Examples would include patients with pseudocholinesterase deficiency, myasthenia gravis, or pregnancy. Pregnancy often is considered a contraindication, but ECT has no notable effect on labor & delivery, fetal injury, or development. It would be a preferred modality over medications, especially in unstable mothers during the first trimester. ECT exerts little effect on the fetus, as the amount of current that actually gets to the fetus is negligible6.
Outside the central nervous system, ECT exerts the most influence over the cardiovascular system. During the tonic phase of a seizure, increased vagal tone can depress the heart rate to asystole in some patients (see chart below). This may last for 3-4 seconds until the clonic phase occurs (with a noradrenergic surge), whereupon the heart rate can accelerate to the 140s. Unless unstable cardiac disease is present, patients typically tolerate this extremely well without any adverse sequela7. Studies involving patients who have severe aortic stenosis and pacemakers/defibrillators show overall excellent tolerability8,9.
Medications can have an impact on the onset, quality, and duration of seizures. Thus, a careful medication review is needed. A consultant will look first for medications such as benzodiazepines or anticonvulsants that would raise the seizure threshold. Ideally, the medications would be stopped, but if not feasible, they can be held the night before (or the day before in the case of such long half-life agents as diazepam) to minimize their impact.
As for anticonvulsants, the doses can be reduced, along with modest increases in energy settings to facilitate seizure. If used for mood stabilization only, one could consider stopping them completely, but this is usually not required (it is not recommended to stop them if used for epilepsy). Lithium can lead to prolonged neuromuscular blockade, prolonged seizures, or postictal delirium. However, discontinuation of lithium also has a risk-benefit consideration, so usually, doses are reduced and/or decreased doses of neuromuscular blockade are employed. Theophylline can induce extended seizures or status epilepticus so it is usually held prior to ECT.
Back to the case
Given the patient’s severe Parkinson’s disease and concurrent NMS, ECT was initiated. By the second treatment, fever and tachycardia resolved. By the sixth treatment, all NMS symptoms and associated paranoia had completely resolved and her Parkinson’s disease rating scale score went from 142 to 42. Her levodopa dose was reduced from 1,200 to 300 mg/day. She remained stable for years afterward.
Bottom line
ECT is both effective and well tolerated in patients who have received appropriate medical evaluation.
Dr. Lang is clinical associate professor in the departments of psychiatry and internal medicine and director of the electroconvulsive therapy and transcranial magnetic stimulation programs at East Carolina University, Greenville, N.C.
Key points
- ECT is indicated for psychotic and depressive disorders, with high efficacy and rapid response.
- ECT also has proven benefits for NMS, catatonia, delirium, status epilepticus, and Parkinson’s disease.
- Evaluation and focused treatment of relative contraindications maximizes both safety and tolerability of ECT.
References
1. Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
2. Baghai T et al. Electroconvulsive therapy and its different indications. Dialogues Clin Neurosci. Mar 2008;10(1):105-17.
3. Ozer F et al. Electroconvulsive therapy in drug-induced psychiatric states and neuroleptic malignant syndrome. J ECT. 2005 Jun;21(2):125-7.
4. Taylor S. Electroconvulsive therapy: A review of history, patient selection, technique, and medication management. South Med J. 2007 May;100(5):494-8.
5. The Practice of Electroconvulsive Therapy, 2nd edition. A Task Force Report of the American Psychiatric Association. 2001. pp. 84-85.
6. Miller LJ. Use of electroconvulsive therapy during pregnancy. Hosp Community Psychiatry. 1994 May;45(5):444-50.
7. Miller R et al. ECT: Physiologic Effects. Miller’s Anesthesia. 7th Edition. 2009.
8. Mueller PS et al. The Safety of electroconvulsive therapy in patients with severe aortic stenosis. Mayo Clin Proc. 2007 Nov;82(11):1360-3.
9. Dolenc TJ et al. Electroconvulsive therapy in patients with cardiac pacemakers & implantable cardioverter defibrillators. Pacing Clin Electrophysiol. 2004 Sep;27(9):1257-63.
Suggested readings
The practice of electroconvulsive therapy: Recommendations for treatment, training, and privileging (A Task Force Report of the American Psychiatric Association), 2nd Edition. APA Publishing. 2001.
Weiner R et al. “Electroconvulsive therapy in the medical & neurologic patient” in A Stoudemire, BS Fogel & D Greenberg (eds) Psychiatric Care of the Medical Patient, 2nd ed., New York, Oxford Univ Press. 2000:419-28. (Second edition is out of print.)
Rosenquist P et al. Charting the course of electroconvulsive therapy: Where have we been and where are we headed? J Psychosoc Nurs Ment Health Serv. 2016 Dec 1;54(12):39-43.
QUIZ
1. All of the following are indications for ECT except?
A. Schizophrenia.
B. Panic attacks.
C. Bipolar mania.
D. Catatonia.
Answer: B. Panic attacks. ECT is not effective for anxiety disorders including panic, generalized anxiety, PTSD, or OCD.
2. The most commonly accepted mechanism of action for ECT is?
A. Reduction in glutamate levels.
B. Altering signal transduction pathways.
C. Increased neurotransmitter activity.
D. Increased cerebral blood flow.
Answer: C. Increased neurotransmitter activity. There are data to support all, but neurotransmitter flow is most accepted thus far.
3. Which of the following is a common side effect of ECT?
A. Bronchospasm.
B. Diarrhea.
C. Delirium.
D. Visual changes.
Answer: C. Delirium. The rest are rare or not noted.
4. Which of the following is a relative contraindication for ECT?
A. Pregnancy.
B. Epilepsy.
C. Advanced age.
D. Increased intracranial pressure.
Answer: D. Increased intracranial pressure.