User login
ANSWER
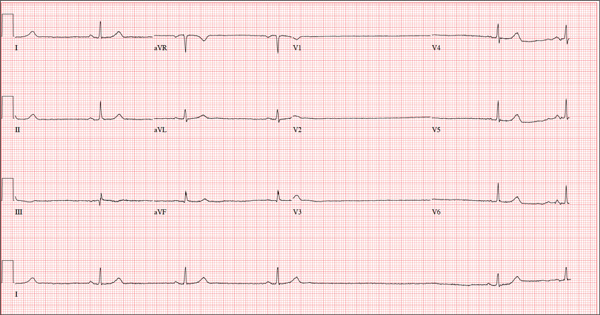
The ECG shows marked sinus bradycardia with a four-second pause consistent with sinus arrest. This may be due to conduction disease within the sinus node and may be exacerbated by use of β-blockers or calcium-channel blockers, or by hypothyroidism.
The patient’s episodes of near-syncope coincided with sinus arrest on telemetry monitoring. She underwent implantation of a dual-chamber permanent pacemaker and resumed all previous activities without issue.
ANSWER
The ECG shows marked sinus bradycardia with a four-second pause consistent with sinus arrest. This may be due to conduction disease within the sinus node and may be exacerbated by use of β-blockers or calcium-channel blockers, or by hypothyroidism.
The patient’s episodes of near-syncope coincided with sinus arrest on telemetry monitoring. She underwent implantation of a dual-chamber permanent pacemaker and resumed all previous activities without issue.
ANSWER
The ECG shows marked sinus bradycardia with a four-second pause consistent with sinus arrest. This may be due to conduction disease within the sinus node and may be exacerbated by use of β-blockers or calcium-channel blockers, or by hypothyroidism.
The patient’s episodes of near-syncope coincided with sinus arrest on telemetry monitoring. She underwent implantation of a dual-chamber permanent pacemaker and resumed all previous activities without issue.
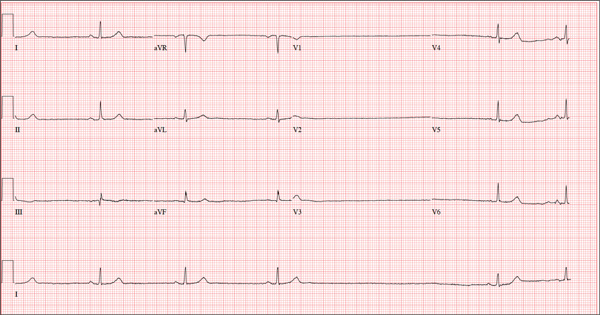
A 74-year-old woman is transferred from a skilled nursing facility (SNF) for evaluation following three episodes of near-syncope in the past week. Each episode occurred while the patient was “at rest,” sitting at a table playing cards with her fellow residents. The most recent episode, witnessed by a nurse’s aide, occurred this morning. The aide called the nursing supervisor to explain that the patient had been engaged in conversation and then slumped over in her chair for approximately three to four minutes. When her companions shook her, she promptly woke up and continued playing cards as if nothing had happened. Upon questioning, the patient denied experiencing shortness of breath, palpitations, or chest pain. Her statement that “this has never happened before” was promptly corrected by her companions. The patient’s medical history is positive for hypertension, hypothyroidism, cholecystitis, and diverticulitis. There is a remote history of pneumonia. Surgical history is positive for cholecystectomy, hysterectomy, and multiple colonoscopies. The patient’s regular medications include amlodipine, atorvastatin, levothyroxine, and baby aspirin. She is allergic to sulfa. A widow for 11 years, the patient has resided in the SNF for three years and has two sons who visit weekly. She is quite active, serving as chairwoman for many of the facility’s events. She has never smoked but says she “enjoys” a nightly glass of brandy before bed. Review of systems is positive for loose stools and occasional blood secondary to her diverticulitis. She denies palpitations, arrhythmias, tachycardia, or other cardiac symptoms. She wears corrective lenses and hearing aids. Vital signs include a blood pressure of 148/98 mm Hg; pulse, 50 beats/min; respiratory rate, 14 breaths/min; and temperature, 98.8°F. Her weight is 146.3 lb and her height, 58 in. Physical examination reveals a keenly alert, oriented (x 3), and well-nourished woman. Her hearing is intact with her hearing aids in place. There are no indications of carotid bruit, jugular venous distention, or thyromegaly. The lungs are clear in all fields. The cardiac exam is remarkable for a rate of 50 beats/min; the rhythm is regular. There is a grade II/VI systolic murmur over the left sternal border. The abdominal exam reveals well-healed surgical scars. Her abdomen is nontender, and there are no palpable masses. Peripheral pulses are strong and regular in all extremities, and there are minimal signs of osteoarthritis in her hands and fingers. The neurologic exam is intact and unremarkable. As you leave the patient’s room, you ask your new technician to obtain a 12-lead ECG. Shortly thereafter, the tech opens the exam room door, shouting for help. By the time you enter the room, the patient is lying comfortably on the exam table, wondering what is wrong. The tech hands you the ECG, which shows a ventricular rate of 29 beats/min; PR interval, 176 ms; QRS duration, 76 ms; QT/QTc interval, 474/329 ms; P axis, 30°; R axis, 42°; and T axis, 20°. What is your interpretation of this ECG?