User login
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that showed a high degree of specificity in identifying such lesions in the disease.
“There is a lack of consensus as to what defines a structural lesion on MRI of the sacroiliac joint [SIJ] typical of axial spondyloarthritis. Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies. The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19.
Making a definitive diagnosis of axSpA can be difficult because MRI can show a variety of SIJ abnormalities in healthy people as well as those with axSpA, said Dr. Maksymowych, chief medical officer of CARE Arthritis and professor in rheumatology at the University of Alberta in Edmonton, said in an interview prior to his presentation at the e-congress. “People who evaluate MRI scans are looking for clues as to what types of lesions they can be confident are indicative of axSpA.”
That started a process by the ASAS MRI group to evaluate scans from the landmark ASAS Classification Cohort study (Ann Rheum Dis. 2019;78:1550-8). “But,” said Dr. Maksymowych, “the MRI scans from that study were never evaluated.” So that work was handed off to the working group, whose 25 members included 7 expert image readers who evaluated the MRI scans.
The group adopted a standardized approach for evaluating MRIs of the SIJ in 148 cases, dividing each SIJ into quadrants and then evaluating consecutive MRI slices. The readers first documented whether they observed a definite structural lesion on the scan, which they then used as an external reference standard. They then analyzed which lesion, and in how many SIJ quadrants or slices, best reflected this external standard.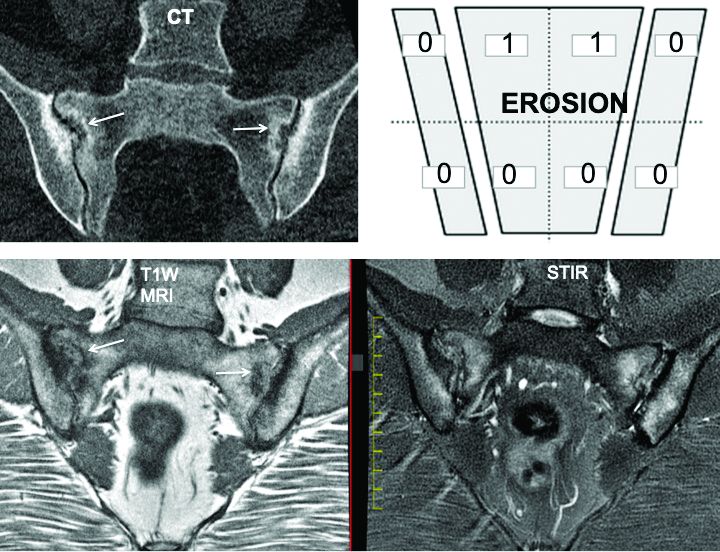
The investigators defined an erosion as “a defect in subchondral bone associated with full-thickness loss of a dark appearance of the subchondral cortex at its expected location, with loss of signal on a T1-weighted, non–fat-suppressed sequence, compared with the normal bright appearance of adjacent bone marrow.” They defined a fat lesion or fat metaplasia as a “bright signal seen on a T1-weighted, non–fat-suppressed sequence that is brighter than normal bone marrow which meets the following requirements: It is homogeneously bright, located in a typical anatomical area (specifically subchondral bone), and has a sharply defined border along its nonarticular border with normal bone marrow.”
An erosion in one quadrant isn’t sufficient to define a scan as positive for a definite structural lesion, said Dr. Maksymowych; but an erosion in three quadrants or in two or more consecutive slices meets the group’s designation of a definite structural lesion. “This showed over a 95% specificity for being associated with a definite structural lesion as defined by a majority of the seven experts,” he said.
The group also determined that a fat lesion typical of axSpA has a homogeneous white appearance on T1-weighted scans with a sharply defined border. The group also determined that such a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant is strongly indicative of axSpA.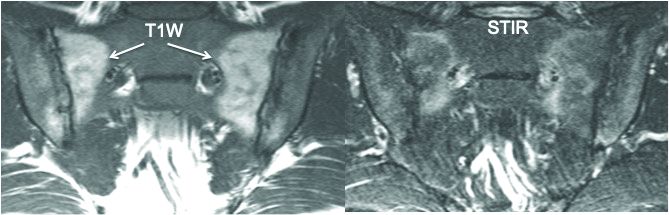
“So we now have definitions for two structural lesions, erosion and fat lesions, that reflect what a majority of experts consider to be a definite structural lesion according to at least 95% specificity,” he said. Sensitivity values were 90% for erosion in three quadrants and 83% for erosions in two or more consecutive slices. and 59% for a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant.
The second part of the analysis evaluated the predictive capacity of these lesion definitions for a rheumatologic diagnosis of axSpA at 4.4 years of follow-up. “These lesions predicted SpA with over 95% positive predictive value,” he said. “In other words, if you see them at baseline they’re going to predict SpA with high certainty at follow-up after 4.4 years.”
Three aspects of this study design are unique, Dr. Maksymowych noted. First is the high number of expert MRI readers who evaluated the scans. “There aren’t really too many studies I can think of that used more than two or three expert MRI readers,” he said.
Second is the way in which the study “very precisely and in a very standardized way” applied all the consensus-based ASAS definitions of structural SIJ lesions. “In the past, a variety of ways were used to define these lesions,” he said. “A good example would be the different ways in which erosions have been defined.”
The third novel aspect of the study is that the expert readers’ assessment of what constitutes a definite structural lesion was used as an external reference standard. For example, the study calculated sensitivity and specificity for numbers of SIJ quadrants and consecutive slices with erosion, sclerosis, and fat lesions where a majority of readers agreed on the presence of a structural lesion typical of axSpA with high confidence (3 or greater on a scale of 1-4). “The reason this was put in place is because we recognize sometimes lesions are very subtle and you can’t be certain that they’re reflecting SpA,” he said.
The investigators disclosed relationships with AbbVie, Amgen, Astellas, AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Celgene, Eli Lilly, Galapagos, Janssen, Merck, Novo Nordisk, Novartis, Orion, Pfizer, Regeneron, Roche, Sandoz, Sanofi, and UCB.
Maksymowych WP et al. Ann Rheum Dis, 2020;79[suppl 1]:53. Abstract OP0079.
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that showed a high degree of specificity in identifying such lesions in the disease.
“There is a lack of consensus as to what defines a structural lesion on MRI of the sacroiliac joint [SIJ] typical of axial spondyloarthritis. Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies. The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19.
Making a definitive diagnosis of axSpA can be difficult because MRI can show a variety of SIJ abnormalities in healthy people as well as those with axSpA, said Dr. Maksymowych, chief medical officer of CARE Arthritis and professor in rheumatology at the University of Alberta in Edmonton, said in an interview prior to his presentation at the e-congress. “People who evaluate MRI scans are looking for clues as to what types of lesions they can be confident are indicative of axSpA.”
That started a process by the ASAS MRI group to evaluate scans from the landmark ASAS Classification Cohort study (Ann Rheum Dis. 2019;78:1550-8). “But,” said Dr. Maksymowych, “the MRI scans from that study were never evaluated.” So that work was handed off to the working group, whose 25 members included 7 expert image readers who evaluated the MRI scans.
The group adopted a standardized approach for evaluating MRIs of the SIJ in 148 cases, dividing each SIJ into quadrants and then evaluating consecutive MRI slices. The readers first documented whether they observed a definite structural lesion on the scan, which they then used as an external reference standard. They then analyzed which lesion, and in how many SIJ quadrants or slices, best reflected this external standard.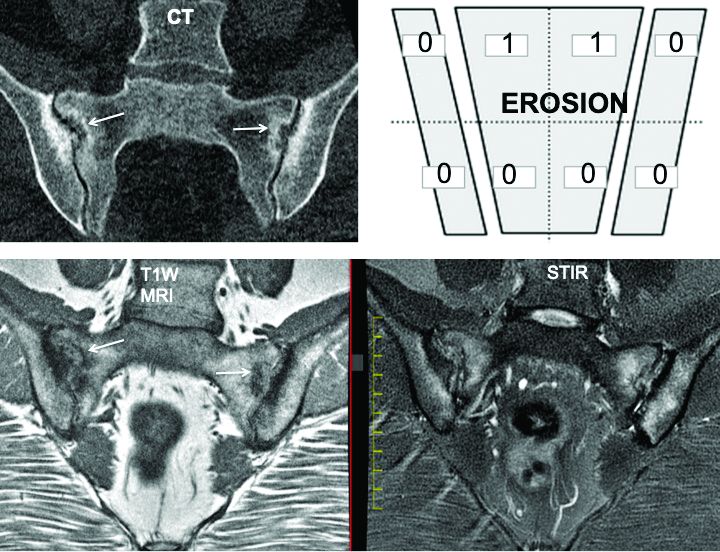
The investigators defined an erosion as “a defect in subchondral bone associated with full-thickness loss of a dark appearance of the subchondral cortex at its expected location, with loss of signal on a T1-weighted, non–fat-suppressed sequence, compared with the normal bright appearance of adjacent bone marrow.” They defined a fat lesion or fat metaplasia as a “bright signal seen on a T1-weighted, non–fat-suppressed sequence that is brighter than normal bone marrow which meets the following requirements: It is homogeneously bright, located in a typical anatomical area (specifically subchondral bone), and has a sharply defined border along its nonarticular border with normal bone marrow.”
An erosion in one quadrant isn’t sufficient to define a scan as positive for a definite structural lesion, said Dr. Maksymowych; but an erosion in three quadrants or in two or more consecutive slices meets the group’s designation of a definite structural lesion. “This showed over a 95% specificity for being associated with a definite structural lesion as defined by a majority of the seven experts,” he said.
The group also determined that a fat lesion typical of axSpA has a homogeneous white appearance on T1-weighted scans with a sharply defined border. The group also determined that such a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant is strongly indicative of axSpA.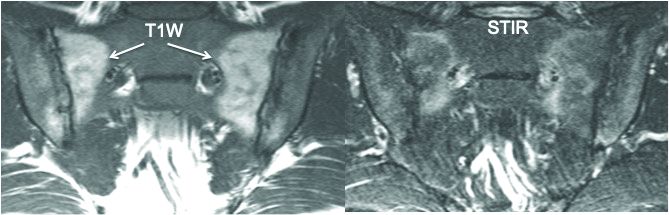
“So we now have definitions for two structural lesions, erosion and fat lesions, that reflect what a majority of experts consider to be a definite structural lesion according to at least 95% specificity,” he said. Sensitivity values were 90% for erosion in three quadrants and 83% for erosions in two or more consecutive slices. and 59% for a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant.
The second part of the analysis evaluated the predictive capacity of these lesion definitions for a rheumatologic diagnosis of axSpA at 4.4 years of follow-up. “These lesions predicted SpA with over 95% positive predictive value,” he said. “In other words, if you see them at baseline they’re going to predict SpA with high certainty at follow-up after 4.4 years.”
Three aspects of this study design are unique, Dr. Maksymowych noted. First is the high number of expert MRI readers who evaluated the scans. “There aren’t really too many studies I can think of that used more than two or three expert MRI readers,” he said.
Second is the way in which the study “very precisely and in a very standardized way” applied all the consensus-based ASAS definitions of structural SIJ lesions. “In the past, a variety of ways were used to define these lesions,” he said. “A good example would be the different ways in which erosions have been defined.”
The third novel aspect of the study is that the expert readers’ assessment of what constitutes a definite structural lesion was used as an external reference standard. For example, the study calculated sensitivity and specificity for numbers of SIJ quadrants and consecutive slices with erosion, sclerosis, and fat lesions where a majority of readers agreed on the presence of a structural lesion typical of axSpA with high confidence (3 or greater on a scale of 1-4). “The reason this was put in place is because we recognize sometimes lesions are very subtle and you can’t be certain that they’re reflecting SpA,” he said.
The investigators disclosed relationships with AbbVie, Amgen, Astellas, AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Celgene, Eli Lilly, Galapagos, Janssen, Merck, Novo Nordisk, Novartis, Orion, Pfizer, Regeneron, Roche, Sandoz, Sanofi, and UCB.
Maksymowych WP et al. Ann Rheum Dis, 2020;79[suppl 1]:53. Abstract OP0079.
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that showed a high degree of specificity in identifying such lesions in the disease.
“There is a lack of consensus as to what defines a structural lesion on MRI of the sacroiliac joint [SIJ] typical of axial spondyloarthritis. Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies. The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19.
Making a definitive diagnosis of axSpA can be difficult because MRI can show a variety of SIJ abnormalities in healthy people as well as those with axSpA, said Dr. Maksymowych, chief medical officer of CARE Arthritis and professor in rheumatology at the University of Alberta in Edmonton, said in an interview prior to his presentation at the e-congress. “People who evaluate MRI scans are looking for clues as to what types of lesions they can be confident are indicative of axSpA.”
That started a process by the ASAS MRI group to evaluate scans from the landmark ASAS Classification Cohort study (Ann Rheum Dis. 2019;78:1550-8). “But,” said Dr. Maksymowych, “the MRI scans from that study were never evaluated.” So that work was handed off to the working group, whose 25 members included 7 expert image readers who evaluated the MRI scans.
The group adopted a standardized approach for evaluating MRIs of the SIJ in 148 cases, dividing each SIJ into quadrants and then evaluating consecutive MRI slices. The readers first documented whether they observed a definite structural lesion on the scan, which they then used as an external reference standard. They then analyzed which lesion, and in how many SIJ quadrants or slices, best reflected this external standard.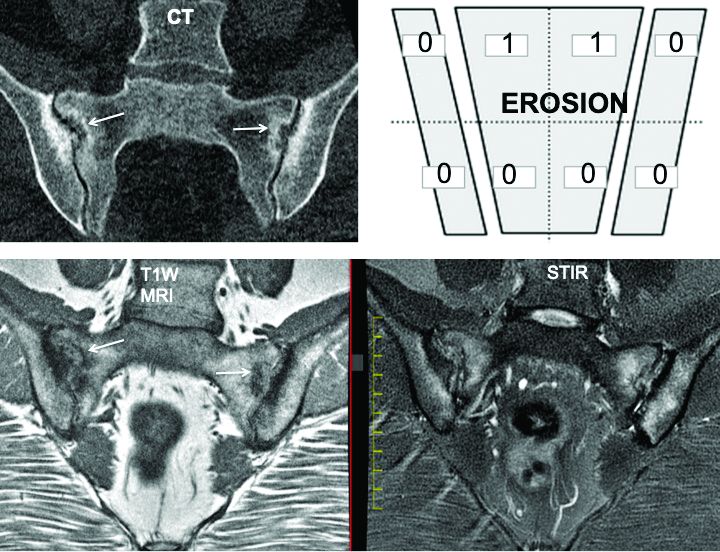
The investigators defined an erosion as “a defect in subchondral bone associated with full-thickness loss of a dark appearance of the subchondral cortex at its expected location, with loss of signal on a T1-weighted, non–fat-suppressed sequence, compared with the normal bright appearance of adjacent bone marrow.” They defined a fat lesion or fat metaplasia as a “bright signal seen on a T1-weighted, non–fat-suppressed sequence that is brighter than normal bone marrow which meets the following requirements: It is homogeneously bright, located in a typical anatomical area (specifically subchondral bone), and has a sharply defined border along its nonarticular border with normal bone marrow.”
An erosion in one quadrant isn’t sufficient to define a scan as positive for a definite structural lesion, said Dr. Maksymowych; but an erosion in three quadrants or in two or more consecutive slices meets the group’s designation of a definite structural lesion. “This showed over a 95% specificity for being associated with a definite structural lesion as defined by a majority of the seven experts,” he said.
The group also determined that a fat lesion typical of axSpA has a homogeneous white appearance on T1-weighted scans with a sharply defined border. The group also determined that such a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant is strongly indicative of axSpA.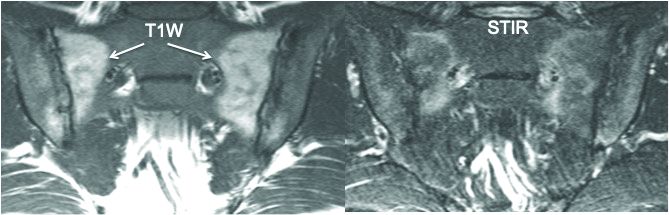
“So we now have definitions for two structural lesions, erosion and fat lesions, that reflect what a majority of experts consider to be a definite structural lesion according to at least 95% specificity,” he said. Sensitivity values were 90% for erosion in three quadrants and 83% for erosions in two or more consecutive slices. and 59% for a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant.
The second part of the analysis evaluated the predictive capacity of these lesion definitions for a rheumatologic diagnosis of axSpA at 4.4 years of follow-up. “These lesions predicted SpA with over 95% positive predictive value,” he said. “In other words, if you see them at baseline they’re going to predict SpA with high certainty at follow-up after 4.4 years.”
Three aspects of this study design are unique, Dr. Maksymowych noted. First is the high number of expert MRI readers who evaluated the scans. “There aren’t really too many studies I can think of that used more than two or three expert MRI readers,” he said.
Second is the way in which the study “very precisely and in a very standardized way” applied all the consensus-based ASAS definitions of structural SIJ lesions. “In the past, a variety of ways were used to define these lesions,” he said. “A good example would be the different ways in which erosions have been defined.”
The third novel aspect of the study is that the expert readers’ assessment of what constitutes a definite structural lesion was used as an external reference standard. For example, the study calculated sensitivity and specificity for numbers of SIJ quadrants and consecutive slices with erosion, sclerosis, and fat lesions where a majority of readers agreed on the presence of a structural lesion typical of axSpA with high confidence (3 or greater on a scale of 1-4). “The reason this was put in place is because we recognize sometimes lesions are very subtle and you can’t be certain that they’re reflecting SpA,” he said.
The investigators disclosed relationships with AbbVie, Amgen, Astellas, AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Celgene, Eli Lilly, Galapagos, Janssen, Merck, Novo Nordisk, Novartis, Orion, Pfizer, Regeneron, Roche, Sandoz, Sanofi, and UCB.
Maksymowych WP et al. Ann Rheum Dis, 2020;79[suppl 1]:53. Abstract OP0079.
FROM EULAR 2020 E-CONGRESS

