More than 65% of all physicians who train in the U.S. rotate through a VA hospital at some point during their training. In 2015 alone, more than 43,000 residents received some or all of their clinical training through VA. 1 Of the approximately 120 VAMCs that hold academic affiliations
with medical schools and residency training programs, several hold affiliations with multiple institutions, including VA Boston Healthcare System (VABHS) in Massachusetts. The West Roxbury campus is the home of VA Boston’s acute care hospital, where residents and fellows from Boston Medical Center (BMC), Beth Israel Deaconess Medical Center (BIDMC), and Brigham and Women’s Hospital (BWH) train together. These are 3 of the largest medical training programs in Boston, though each provides a unique training experience for residents due to differences in patient population, faculty expertise, and hospital network affiliations (Table 1).
This diversity brings differences in cultural norms, institutional preferences, and educational expectations. Furthermore, residents from different programs who work together at VA Boston are often meeting one another for the first time, as opportunities for interinstitutional collaboration among these 3 training programs do not exist outside of VA. This training environment presents both an opportunity
and a challenge for medical educators: offering the best possible learning experience for physiciansin-training from multiple programs while providing the best possible care for U.S. veterans.
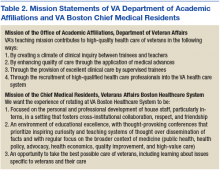
To guide educators charged with meeting this challenge, the VA Office of Academic Affiliations put forth a mission statement describing its overarching teaching mission (Table 2). 2
This mission statement describes an institutional approach to medical education, but it lacks guidance on how to provide an outstanding learning experience for trainees in specific specialties at each of the different VA sites. The VA graduate medical education experience provides an opportunity to care for veterans with a diversity of unique medical and social conditions that are often not represented at trainees’ home institutions. A more detailed mission statement is needed to guide local educators in harnessing issues specific to the care of the veteran in improving both patient care and trainees’ experience.To address this gap, chief medical residents from the 3 affiliate residency training programs came together to develop a shared mission statement for what we envision as the educational experience for all medical trainees rotating through VABHS (Table 2). In this article, we describe the development of a mission statement for graduate medical education in internal medicine at VABHS and provides examples of how our mission statement guided educational programming.
Methods
Whereas the affiliated institutions assign generic competency-based learning objectives to rotations at VABHS, no specific overarching educational objectives for residents have been defined previously. The directors of the internal medicine residency programs at each of the VABHS affiliate institutions grant their respective VA-based chief medical residents the autonomy to deliver graduate medical education at VA as they see fit, in collaboration with their colleagues from the other affiliated institutions and the VA director of medical resident education. This autonomy and flexibility allowed each of the chief medical residents to articulate an individual vision for VA graduate medical education based on their affiliate program’s goals, values, and mission.