Leader rounding for high reliability includes regularly scheduled, structured visits, with interdisciplinary teams to discuss high reliability, safety, and improvement efforts. The specific aim of these particular rounds is for senior leaders to be visible where teams are located and learn from staff (especially those on the frontlines of care) about day-to-day challenges that may contribute to patient harm.12,13 Leader rounding for high reliability is also an important approach to improving leadership visibility across the organization, demonstrating a commitment to high reliability, and building trust and relationships with staff through open and honest dialogue. It is also an important approach to increasing leadership understanding of operational, clinical, nonclinical, patient experience issues, and concern related to safety.11 This opportunity enables leaders to provide and receive real-time feedback from staff.9,11 This experience also gives leaders an opportunity to reinforce the VHA’s 3 pillars, 5 principles, and 7 values related to high reliability (Figure 2)14 as well as to recognize behaviors that support a culture of safety.15
In preparation for implementing a leader rounding for high reliability process at the VABHS, we conducted an extensive literature review for peer-reviewed publications published between January 2015 and September 2022 regarding how other organizations implemented leader rounding. This search found a dearth of evidence as it specifically relates to leader rounding for high reliability. This motivated us to create a process for developing and implementing leader rounding for high reliability in pursuit of improving patient safety. With this objective in mind, we created and piloted a process in the fall of 2023. The first 3 months were focused on the medical center director rounding with other members of the executive leadership team to assess the feasibility and acceptability of the process. In December 2023, members of the executive leadership team began conducting leader rounding for high reliability separately. The following steps are based on the lessons we have gleaned from evolving evidence, our experiences, and developing and implementing an approach to leader rounding for high reliability.
ESTABLISH A PROCESS
Leader rounding for high reliability is performed by health care organization executive leadership, directors, managers, and supervisors. When properly conducted, increased levels of teamwork and more effective bidirectional communication take place, resulting in a united team motivated to improve patient safety.16,17 Important early steps for implementing leader rounding for high reliability include establishing a process and getting leadership buy-in. Purposeful attention to planning is critical as is understanding the organizational factors that might deter success. Establishing a process should consider facilitators and barriers to implementation, which can include high vs low leadership turnover, structured vs unstructured rounding, and time for rounding vs competing demands.18,19 We have learned that effective planning is important for ensuring that leadership teams are well prepared and ambitious about leader rounding for high reliability.
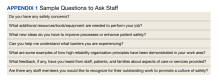
Leader rounding for high reliability involves brief 10-to-15-minute interactions with interdisciplinary teams, including frontline staff. For health care organizations beginning to implement this approach, having scripts or checklists accessible might be of help. If possible, the rounds should be scheduled in advance. This helps to avoid rounding in areas at their busiest times. When possible, leader rounding for high reliability should occur as planned. Canceling rounds sends the message that leader rounding for high reliability and the valuable interactions they support are a low priority. When conflicts arise, another leader should be sent to participate. Developing a list of questions in advance helps to underscore key messages to be shared as well as reinforce principles, practices, behaviors, and attitudes related to high reliability (Appendix 1).11
Finally, closing the loop is critical to the leader rounding process and to improve bidirectional communication. Closed-loop communication, following up on and/or closing out an area of discussion, not only promotes a shared understanding of information but has been found to improve patient safety.19 Effective leader rounding for high reliability includes summarizing issues and opportunities, deciding on a date for resolution for open action items, and identifying who is responsible for taking action. Senior leaders are not responsible for resolving all issues. If a team or manager of a work area can solve any issues identified, this should be encouraged and supported so accountability is maintained at the most appropriate level of the organization.
Instrumental to leader rounding for high reliability is establishing a cadence for when leaders will visit work areas.14 The most critical strategy, especially in times of change, is consistency in rounding.11 At the start of implementation, we decided on a biweekly cadence. Initially leaders visited areas of the organization within their respective reporting structure. Once this was established, leaders periodically round in areas outside their scope of responsibility. This affords leaders the opportunity to observe other areas of the organization. As noted, it is important for leaders to be flexible with the rounding process especially in areas where direct patient care is being provided.