User login
HCV Hub
AbbVie
acid
addicted
addiction
adolescent
adult sites
Advocacy
advocacy
agitated states
AJO, postsurgical analgesic, knee, replacement, surgery
alcohol
amphetamine
androgen
antibody
apple cider vinegar
assistance
Assistance
association
at home
attorney
audit
ayurvedic
baby
ban
baricitinib
bed bugs
best
bible
bisexual
black
bleach
blog
bulimia nervosa
buy
cannabis
certificate
certification
certified
cervical cancer, concurrent chemoradiotherapy, intravoxel incoherent motion magnetic resonance imaging, MRI, IVIM, diffusion-weighted MRI, DWI
charlie sheen
cheap
cheapest
child
childhood
childlike
children
chronic fatigue syndrome
Cladribine Tablets
cocaine
cock
combination therapies, synergistic antitumor efficacy, pertuzumab, trastuzumab, ipilimumab, nivolumab, palbociclib, letrozole, lapatinib, docetaxel, trametinib, dabrafenib, carflzomib, lenalidomide
contagious
Cortical Lesions
cream
creams
crime
criminal
cure
dangerous
dangers
dasabuvir
Dasabuvir
dead
deadly
death
dementia
dependence
dependent
depression
dermatillomania
die
diet
direct-acting antivirals
Disability
Discount
discount
dog
drink
drug abuse
drug-induced
dying
eastern medicine
eat
ect
eczema
electroconvulsive therapy
electromagnetic therapy
electrotherapy
epa
epilepsy
erectile dysfunction
explosive disorder
fake
Fake-ovir
fatal
fatalities
fatality
fibromyalgia
financial
Financial
fish oil
food
foods
foundation
free
Gabriel Pardo
gaston
general hospital
genetic
geriatric
Giancarlo Comi
gilead
Gilead
glaucoma
Glenn S. Williams
Glenn Williams
Gloria Dalla Costa
gonorrhea
Greedy
greedy
guns
hallucinations
harvoni
Harvoni
herbal
herbs
heroin
herpes
Hidradenitis Suppurativa,
holistic
home
home remedies
home remedy
homeopathic
homeopathy
hydrocortisone
ice
image
images
job
kid
kids
kill
killer
laser
lawsuit
lawyer
ledipasvir
Ledipasvir
lesbian
lesions
lights
liver
lupus
marijuana
melancholic
memory loss
menopausal
mental retardation
military
milk
moisturizers
monoamine oxidase inhibitor drugs
MRI
MS
murder
national
natural
natural cure
natural cures
natural medications
natural medicine
natural medicines
natural remedies
natural remedy
natural treatment
natural treatments
naturally
Needy
needy
Neurology Reviews
neuropathic
nightclub massacre
nightclub shooting
nude
nudity
nutraceuticals
OASIS
oasis
off label
ombitasvir
Ombitasvir
ombitasvir/paritaprevir/ritonavir with dasabuvir
orlando shooting
overactive thyroid gland
overdose
overdosed
Paolo Preziosa
paritaprevir
Paritaprevir
pediatric
pedophile
photo
photos
picture
post partum
postnatal
pregnancy
pregnant
prenatal
prepartum
prison
program
Program
Protest
protest
psychedelics
pulse nightclub
puppy
purchase
purchasing
rape
recall
recreational drug
Rehabilitation
Retinal Measurements
retrograde ejaculation
risperdal
ritonavir
Ritonavir
ritonavir with dasabuvir
robin williams
sales
sasquatch
schizophrenia
seizure
seizures
sex
sexual
sexy
shock treatment
silver
sleep disorders
smoking
sociopath
sofosbuvir
Sofosbuvir
sovaldi
ssri
store
sue
suicidal
suicide
supplements
support
Support
Support Path
teen
teenage
teenagers
Telerehabilitation
testosterone
Th17
Th17:FoxP3+Treg cell ratio
Th22
toxic
toxin
tragedy
treatment resistant
V Pak
vagina
velpatasvir
Viekira Pa
Viekira Pak
viekira pak
violence
virgin
vitamin
VPak
weight loss
withdrawal
wrinkles
xxx
young adult
young adults
zoloft
financial
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
Gastrointestinal and liver diseases remain substantial public health burden
Diseases such as Clostridium difficile infection, inflammatory bowel disease, and liver cancer continue to cost billions and cause many thousands of deaths in the United States every year, investigators reported in the December issue of Gastroenterology.
“Gastrointestinal and liver diseases are a source of substantial burden and cost,” said Dr. Anne Peery and her associates at the University of North Carolina School of Medicine and the Gillings School of Public Health, both in Chapel Hill. The Affordable Care Act has extended health insurance to more than 16 million Americans, which is “expected to change the landscape of care for GI illnesses” and intensifies the need for their comprehensive study, the researchers added.
They analyzed health care visits, costs, and deaths from GI, pancreatic, and hepatic diseases for 2007 through 2012 by using surveillance data from the Centers for Disease Control and Prevention, the Agency for Healthcare Research and Quality, and the National Cancer Institute. Chronic hepatitis C virus infection was a leading disease burden, they found. Associated emergency department visits rose by 176% between 2006 and 2012, hospital admissions increased by 225% between 2003 and 2012, and in-hospital mortality approached 6%. These trends reflect the aging of baby boomers, who make up three-quarters of infected patients, the investigators noted. As a result, rates of new liver cancers also are rising, and end-stage liver disease is expected to keep increasing until 2030, they added (Gastroenterology. 2015 Aug 20. doi: 10.1053/j.gastro.2015.08.045). Aging boomers are increasingly seeking care for other age-related GI disorders, the investigators reported. Outpatient visits for hemorrhoids are rising, as are emergency department visits for constipation and lower-GI bleeding, and hospitalizations for acute diverticulitis and C. difficile infection. Gastrointestinal hemorrhage was the most common diagnosis at hospitalization, accounting for more than 500,000 discharges and costing almost $5 billion dollars in 2012 alone, the researchers said.
Despite better treatments, hospital admissions for Crohn’s disease and ulcerative colitis also rose from less than 60,000 in 1993 to about 100,000 in 2012, said Dr. Peery and her associates. “This is congruent with earlier trends using the National Hospital Discharge Survey. Emergency department visits [for inflammatory bowel disease] are also rising,” they added.
In contrast, cases and deaths from colorectal cancer continue to drop, partly because of intensified screening efforts, the investigators said. They called the trend “encouraging,” but noted that CRC still tops cancers of the pancreas, liver, and intrahepatic bile ducts as the leading GI cause of mortality in the United States. In 2012, more than 51,000 Americans died from CRC, and screening efforts captured only 58% of those between 50 and 75 years old. Boosting that percentage to 80% by 2018 http://nccrt.org/tools/80-percent-by-2018/ could prevent 280,000 CRC cases and 200,000 deaths within 20 years, Dr. Peery and her associates noted.
The National Institutes of Health helped fund the work. The investigators reported having no conflicts of interest.
Source: American Gastroenterological Association
In the excellent study by Peery and colleagues, statistics on health care utilization in the ambulatory and hospital settings, incidence and mortality from GI cancers, and mortality associated with other GI illnesses from 2007 to 2012 was collected using data from multiple complementary databases. This is the ideal methodology for this type of study because it quantifies utilization data from several complementary national databases. Of course, these data may be limited by systematic errors in ICD coding and costs are estimated using Medicare’s cost-to-charge ratio. Nevertheless, these data provide the best “snap shot” of trends in the burden of gastrointestinal and liver illness as of 2012.
What are the key points? First, the increase in the burden of GI and liver illness probably reflects the aging of the “baby boomer” population. Furthermore, since the Affordable Care Act is expanding access to health care, the burden on gastroenterologists is also likely to expand. Second, although we’re doing a good job with CRC screening, there is also room for improvement. While the incidence of CRC continues to decrease, only 58% of adults aged 50-75 years old had CRC screening in 2010. Third, HCV-associated hospitalizations have doubled from 2003 to 2012. Since HCV-associated cirrhosis is likely to increase until 2030, insurers and public health officials will have to carefully weigh the initial high cost of using new and highly effective regimens of direct-acting antiviral agents versus the downstream costs of managing these individuals after developing decompensated cirrhosis.
Dr. Philip S. Schoenfeld is professor of medicine and director, training program in GI epidemiology, division of gastroenterology, University of Michigan, Ann Arbor. He has no conflicts of interest.
In the excellent study by Peery and colleagues, statistics on health care utilization in the ambulatory and hospital settings, incidence and mortality from GI cancers, and mortality associated with other GI illnesses from 2007 to 2012 was collected using data from multiple complementary databases. This is the ideal methodology for this type of study because it quantifies utilization data from several complementary national databases. Of course, these data may be limited by systematic errors in ICD coding and costs are estimated using Medicare’s cost-to-charge ratio. Nevertheless, these data provide the best “snap shot” of trends in the burden of gastrointestinal and liver illness as of 2012.
What are the key points? First, the increase in the burden of GI and liver illness probably reflects the aging of the “baby boomer” population. Furthermore, since the Affordable Care Act is expanding access to health care, the burden on gastroenterologists is also likely to expand. Second, although we’re doing a good job with CRC screening, there is also room for improvement. While the incidence of CRC continues to decrease, only 58% of adults aged 50-75 years old had CRC screening in 2010. Third, HCV-associated hospitalizations have doubled from 2003 to 2012. Since HCV-associated cirrhosis is likely to increase until 2030, insurers and public health officials will have to carefully weigh the initial high cost of using new and highly effective regimens of direct-acting antiviral agents versus the downstream costs of managing these individuals after developing decompensated cirrhosis.
Dr. Philip S. Schoenfeld is professor of medicine and director, training program in GI epidemiology, division of gastroenterology, University of Michigan, Ann Arbor. He has no conflicts of interest.
In the excellent study by Peery and colleagues, statistics on health care utilization in the ambulatory and hospital settings, incidence and mortality from GI cancers, and mortality associated with other GI illnesses from 2007 to 2012 was collected using data from multiple complementary databases. This is the ideal methodology for this type of study because it quantifies utilization data from several complementary national databases. Of course, these data may be limited by systematic errors in ICD coding and costs are estimated using Medicare’s cost-to-charge ratio. Nevertheless, these data provide the best “snap shot” of trends in the burden of gastrointestinal and liver illness as of 2012.
What are the key points? First, the increase in the burden of GI and liver illness probably reflects the aging of the “baby boomer” population. Furthermore, since the Affordable Care Act is expanding access to health care, the burden on gastroenterologists is also likely to expand. Second, although we’re doing a good job with CRC screening, there is also room for improvement. While the incidence of CRC continues to decrease, only 58% of adults aged 50-75 years old had CRC screening in 2010. Third, HCV-associated hospitalizations have doubled from 2003 to 2012. Since HCV-associated cirrhosis is likely to increase until 2030, insurers and public health officials will have to carefully weigh the initial high cost of using new and highly effective regimens of direct-acting antiviral agents versus the downstream costs of managing these individuals after developing decompensated cirrhosis.
Dr. Philip S. Schoenfeld is professor of medicine and director, training program in GI epidemiology, division of gastroenterology, University of Michigan, Ann Arbor. He has no conflicts of interest.
Diseases such as Clostridium difficile infection, inflammatory bowel disease, and liver cancer continue to cost billions and cause many thousands of deaths in the United States every year, investigators reported in the December issue of Gastroenterology.
“Gastrointestinal and liver diseases are a source of substantial burden and cost,” said Dr. Anne Peery and her associates at the University of North Carolina School of Medicine and the Gillings School of Public Health, both in Chapel Hill. The Affordable Care Act has extended health insurance to more than 16 million Americans, which is “expected to change the landscape of care for GI illnesses” and intensifies the need for their comprehensive study, the researchers added.
They analyzed health care visits, costs, and deaths from GI, pancreatic, and hepatic diseases for 2007 through 2012 by using surveillance data from the Centers for Disease Control and Prevention, the Agency for Healthcare Research and Quality, and the National Cancer Institute. Chronic hepatitis C virus infection was a leading disease burden, they found. Associated emergency department visits rose by 176% between 2006 and 2012, hospital admissions increased by 225% between 2003 and 2012, and in-hospital mortality approached 6%. These trends reflect the aging of baby boomers, who make up three-quarters of infected patients, the investigators noted. As a result, rates of new liver cancers also are rising, and end-stage liver disease is expected to keep increasing until 2030, they added (Gastroenterology. 2015 Aug 20. doi: 10.1053/j.gastro.2015.08.045). Aging boomers are increasingly seeking care for other age-related GI disorders, the investigators reported. Outpatient visits for hemorrhoids are rising, as are emergency department visits for constipation and lower-GI bleeding, and hospitalizations for acute diverticulitis and C. difficile infection. Gastrointestinal hemorrhage was the most common diagnosis at hospitalization, accounting for more than 500,000 discharges and costing almost $5 billion dollars in 2012 alone, the researchers said.
Despite better treatments, hospital admissions for Crohn’s disease and ulcerative colitis also rose from less than 60,000 in 1993 to about 100,000 in 2012, said Dr. Peery and her associates. “This is congruent with earlier trends using the National Hospital Discharge Survey. Emergency department visits [for inflammatory bowel disease] are also rising,” they added.
In contrast, cases and deaths from colorectal cancer continue to drop, partly because of intensified screening efforts, the investigators said. They called the trend “encouraging,” but noted that CRC still tops cancers of the pancreas, liver, and intrahepatic bile ducts as the leading GI cause of mortality in the United States. In 2012, more than 51,000 Americans died from CRC, and screening efforts captured only 58% of those between 50 and 75 years old. Boosting that percentage to 80% by 2018 http://nccrt.org/tools/80-percent-by-2018/ could prevent 280,000 CRC cases and 200,000 deaths within 20 years, Dr. Peery and her associates noted.
The National Institutes of Health helped fund the work. The investigators reported having no conflicts of interest.
Source: American Gastroenterological Association
Diseases such as Clostridium difficile infection, inflammatory bowel disease, and liver cancer continue to cost billions and cause many thousands of deaths in the United States every year, investigators reported in the December issue of Gastroenterology.
“Gastrointestinal and liver diseases are a source of substantial burden and cost,” said Dr. Anne Peery and her associates at the University of North Carolina School of Medicine and the Gillings School of Public Health, both in Chapel Hill. The Affordable Care Act has extended health insurance to more than 16 million Americans, which is “expected to change the landscape of care for GI illnesses” and intensifies the need for their comprehensive study, the researchers added.
They analyzed health care visits, costs, and deaths from GI, pancreatic, and hepatic diseases for 2007 through 2012 by using surveillance data from the Centers for Disease Control and Prevention, the Agency for Healthcare Research and Quality, and the National Cancer Institute. Chronic hepatitis C virus infection was a leading disease burden, they found. Associated emergency department visits rose by 176% between 2006 and 2012, hospital admissions increased by 225% between 2003 and 2012, and in-hospital mortality approached 6%. These trends reflect the aging of baby boomers, who make up three-quarters of infected patients, the investigators noted. As a result, rates of new liver cancers also are rising, and end-stage liver disease is expected to keep increasing until 2030, they added (Gastroenterology. 2015 Aug 20. doi: 10.1053/j.gastro.2015.08.045). Aging boomers are increasingly seeking care for other age-related GI disorders, the investigators reported. Outpatient visits for hemorrhoids are rising, as are emergency department visits for constipation and lower-GI bleeding, and hospitalizations for acute diverticulitis and C. difficile infection. Gastrointestinal hemorrhage was the most common diagnosis at hospitalization, accounting for more than 500,000 discharges and costing almost $5 billion dollars in 2012 alone, the researchers said.
Despite better treatments, hospital admissions for Crohn’s disease and ulcerative colitis also rose from less than 60,000 in 1993 to about 100,000 in 2012, said Dr. Peery and her associates. “This is congruent with earlier trends using the National Hospital Discharge Survey. Emergency department visits [for inflammatory bowel disease] are also rising,” they added.
In contrast, cases and deaths from colorectal cancer continue to drop, partly because of intensified screening efforts, the investigators said. They called the trend “encouraging,” but noted that CRC still tops cancers of the pancreas, liver, and intrahepatic bile ducts as the leading GI cause of mortality in the United States. In 2012, more than 51,000 Americans died from CRC, and screening efforts captured only 58% of those between 50 and 75 years old. Boosting that percentage to 80% by 2018 http://nccrt.org/tools/80-percent-by-2018/ could prevent 280,000 CRC cases and 200,000 deaths within 20 years, Dr. Peery and her associates noted.
The National Institutes of Health helped fund the work. The investigators reported having no conflicts of interest.
Source: American Gastroenterological Association
FROM GASTROENTEROLOGY
Key clinical point: Gastrointestinal and liver diseases remain a major cause of health care utilization and associated costs in the United States.
Major finding: Hospital admissions and associated costs for Clostridium difficile infection, inflammatory bowel disease, and liver disease all rose substantially between 1993 and 2012.
Data source: Analysis of surveillance data from the Centers for Disease Control and Prevention, Agency for Healthcare Research and Quality, and National Cancer Institute.
Disclosures: The National Institutes of Health helped fund the work. The investigators reported having no conflicts of interest.
IDWeek: Despite better drugs, HCV deaths keep rising
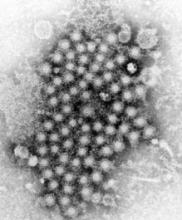
SAN DIEGO – Despite better therapies, deaths from hepatitis C virus (HCV) infection continue to rise, indicating poor penetrance of medications and care to patients who need them, Dr. Scott Holmberg said at an annual scientific meeting on infectious diseases.
“Deaths in chronic HCV–infected persons, even when grossly under-enumerated on death certificates, far outstrip deaths from 60 other infectious conditions reportable to CDC,” said Dr. Holmberg of the Centers for Disease Control and Prevention Division of Viral Hepatitis in Atlanta.
Drugs for chronic HCV infection have vastly improved in the past several years, yielding far better rates of sustained viral response (SVR) and high chances of cure after 8-24 weeks of treatment. To see if better antiviral therapies have affected HCV mortality rates, Dr. Holmberg and his associates studied ICD-9 data from Multiple Cause of Death records for all U.S. death certificates between 2003 and 2013. They divided deaths that were linked to HCV or 60 other nationally notifiable infectious diseases by U.S. Census numbers for the same year. They also examined data from the Chronic Hepatitis Cohort Study (Clin Infect Dis. 2014;58:1055-61), which includes patients presumed to have adequate access to HCV treatment.
Chronic HCV-related deaths climbed from about 12,000 annually in 2003 to more than 19,000 in 2013, said Dr. Holmberg. In contrast, deaths from the 60 other reportable infectious diseases dropped from about 25,000 annually to below 20,000 per year. Annual deaths tied to HIV infection ranked second behind HCV at about 8,800, followed by Staphylococcus aureus (including MRSA), hepatitis B virus, tuberculosis, and pneumococcal disease. “This does not include 4,444 adult influenza deaths, but does include 165 childhood influenza deaths in 2013,” Dr. Holmberg noted.
The analysis of the Chronic Hepatitis Cohort Study revealed a doubling in mortality from chronic HCV infection among patients who should have had adequate access to treatment, according to Dr. Holmberg. For every 100 person-years of observation, about 2.5 people died from consequences of chronic HCV infection in 2007, compared with about 5.5 in 2013, he said. “Hidden mortality from HCV is considerable,” he added. “Only 19% of HCV patients who died had their infection noted anywhere on their death certificates, despite the fact that more than 75% had premortem evidence of liver disease.”
Uptake of sofosbuvir-based regimens more than quintupled in the second quarter of 2015, compared with a year earlier, according to data from Gilead Sciences presented by Dr. Holmberg. But high drug costs have spurred state Medicaid programs and private payers to stipulate many preapproval requirements, he noted. Patients must be drug and alcohol free for at least 6 months, and in many states, must provide evidence of liver scarring from a recent biopsy or FibroScan, which is not always easy to access. “This is often a barrier,” Dr. Holmberg said. “For those in more rural areas, finding a specialist, as required by many state Medicaid offices, can be very difficult.”
And there are even more obstacles. Many clinicians still see HCV as a “benign condition,” and patients often have other urgent health, social, or financial problems, Dr. Holmberg said. The public, for its part, may not prioritize infectious diseases. “These patients lack a strong advocacy group,” he added. “Most are former injection drug users, and the public is often reluctant to help them.”
So what are the measurable results of these barriers? Among about 3.2 million individuals in the United States with chronic HCV infection, only half were ever tested for HCV, 38% received some sort of care related to their infection, 11% were treated, and 6% achieved SVR, Dr. Holmberg and his associates noted in a perspective piece (N Engl J Med. 2013;368:1859-861).
At the same time, the United States faces an emerging epidemic of new HCV infections in nonurban areas among young persons who inject drugs (MMWR. 64;453-8). “This is really a tale of two epidemics,” he added. “Control of the chronic and the acute outbreaks will require a multipronged approach, with interventions along a testing to cure continuum of care.”
Dr. Holmberg and his associates reported their findings at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers reported no funding sources and had no financial disclosures.
SAN DIEGO – Despite better therapies, deaths from hepatitis C virus (HCV) infection continue to rise, indicating poor penetrance of medications and care to patients who need them, Dr. Scott Holmberg said at an annual scientific meeting on infectious diseases.
“Deaths in chronic HCV–infected persons, even when grossly under-enumerated on death certificates, far outstrip deaths from 60 other infectious conditions reportable to CDC,” said Dr. Holmberg of the Centers for Disease Control and Prevention Division of Viral Hepatitis in Atlanta.
Drugs for chronic HCV infection have vastly improved in the past several years, yielding far better rates of sustained viral response (SVR) and high chances of cure after 8-24 weeks of treatment. To see if better antiviral therapies have affected HCV mortality rates, Dr. Holmberg and his associates studied ICD-9 data from Multiple Cause of Death records for all U.S. death certificates between 2003 and 2013. They divided deaths that were linked to HCV or 60 other nationally notifiable infectious diseases by U.S. Census numbers for the same year. They also examined data from the Chronic Hepatitis Cohort Study (Clin Infect Dis. 2014;58:1055-61), which includes patients presumed to have adequate access to HCV treatment.
Chronic HCV-related deaths climbed from about 12,000 annually in 2003 to more than 19,000 in 2013, said Dr. Holmberg. In contrast, deaths from the 60 other reportable infectious diseases dropped from about 25,000 annually to below 20,000 per year. Annual deaths tied to HIV infection ranked second behind HCV at about 8,800, followed by Staphylococcus aureus (including MRSA), hepatitis B virus, tuberculosis, and pneumococcal disease. “This does not include 4,444 adult influenza deaths, but does include 165 childhood influenza deaths in 2013,” Dr. Holmberg noted.
The analysis of the Chronic Hepatitis Cohort Study revealed a doubling in mortality from chronic HCV infection among patients who should have had adequate access to treatment, according to Dr. Holmberg. For every 100 person-years of observation, about 2.5 people died from consequences of chronic HCV infection in 2007, compared with about 5.5 in 2013, he said. “Hidden mortality from HCV is considerable,” he added. “Only 19% of HCV patients who died had their infection noted anywhere on their death certificates, despite the fact that more than 75% had premortem evidence of liver disease.”
Uptake of sofosbuvir-based regimens more than quintupled in the second quarter of 2015, compared with a year earlier, according to data from Gilead Sciences presented by Dr. Holmberg. But high drug costs have spurred state Medicaid programs and private payers to stipulate many preapproval requirements, he noted. Patients must be drug and alcohol free for at least 6 months, and in many states, must provide evidence of liver scarring from a recent biopsy or FibroScan, which is not always easy to access. “This is often a barrier,” Dr. Holmberg said. “For those in more rural areas, finding a specialist, as required by many state Medicaid offices, can be very difficult.”
And there are even more obstacles. Many clinicians still see HCV as a “benign condition,” and patients often have other urgent health, social, or financial problems, Dr. Holmberg said. The public, for its part, may not prioritize infectious diseases. “These patients lack a strong advocacy group,” he added. “Most are former injection drug users, and the public is often reluctant to help them.”
So what are the measurable results of these barriers? Among about 3.2 million individuals in the United States with chronic HCV infection, only half were ever tested for HCV, 38% received some sort of care related to their infection, 11% were treated, and 6% achieved SVR, Dr. Holmberg and his associates noted in a perspective piece (N Engl J Med. 2013;368:1859-861).
At the same time, the United States faces an emerging epidemic of new HCV infections in nonurban areas among young persons who inject drugs (MMWR. 64;453-8). “This is really a tale of two epidemics,” he added. “Control of the chronic and the acute outbreaks will require a multipronged approach, with interventions along a testing to cure continuum of care.”
Dr. Holmberg and his associates reported their findings at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers reported no funding sources and had no financial disclosures.
SAN DIEGO – Despite better therapies, deaths from hepatitis C virus (HCV) infection continue to rise, indicating poor penetrance of medications and care to patients who need them, Dr. Scott Holmberg said at an annual scientific meeting on infectious diseases.
“Deaths in chronic HCV–infected persons, even when grossly under-enumerated on death certificates, far outstrip deaths from 60 other infectious conditions reportable to CDC,” said Dr. Holmberg of the Centers for Disease Control and Prevention Division of Viral Hepatitis in Atlanta.
Drugs for chronic HCV infection have vastly improved in the past several years, yielding far better rates of sustained viral response (SVR) and high chances of cure after 8-24 weeks of treatment. To see if better antiviral therapies have affected HCV mortality rates, Dr. Holmberg and his associates studied ICD-9 data from Multiple Cause of Death records for all U.S. death certificates between 2003 and 2013. They divided deaths that were linked to HCV or 60 other nationally notifiable infectious diseases by U.S. Census numbers for the same year. They also examined data from the Chronic Hepatitis Cohort Study (Clin Infect Dis. 2014;58:1055-61), which includes patients presumed to have adequate access to HCV treatment.
Chronic HCV-related deaths climbed from about 12,000 annually in 2003 to more than 19,000 in 2013, said Dr. Holmberg. In contrast, deaths from the 60 other reportable infectious diseases dropped from about 25,000 annually to below 20,000 per year. Annual deaths tied to HIV infection ranked second behind HCV at about 8,800, followed by Staphylococcus aureus (including MRSA), hepatitis B virus, tuberculosis, and pneumococcal disease. “This does not include 4,444 adult influenza deaths, but does include 165 childhood influenza deaths in 2013,” Dr. Holmberg noted.
The analysis of the Chronic Hepatitis Cohort Study revealed a doubling in mortality from chronic HCV infection among patients who should have had adequate access to treatment, according to Dr. Holmberg. For every 100 person-years of observation, about 2.5 people died from consequences of chronic HCV infection in 2007, compared with about 5.5 in 2013, he said. “Hidden mortality from HCV is considerable,” he added. “Only 19% of HCV patients who died had their infection noted anywhere on their death certificates, despite the fact that more than 75% had premortem evidence of liver disease.”
Uptake of sofosbuvir-based regimens more than quintupled in the second quarter of 2015, compared with a year earlier, according to data from Gilead Sciences presented by Dr. Holmberg. But high drug costs have spurred state Medicaid programs and private payers to stipulate many preapproval requirements, he noted. Patients must be drug and alcohol free for at least 6 months, and in many states, must provide evidence of liver scarring from a recent biopsy or FibroScan, which is not always easy to access. “This is often a barrier,” Dr. Holmberg said. “For those in more rural areas, finding a specialist, as required by many state Medicaid offices, can be very difficult.”
And there are even more obstacles. Many clinicians still see HCV as a “benign condition,” and patients often have other urgent health, social, or financial problems, Dr. Holmberg said. The public, for its part, may not prioritize infectious diseases. “These patients lack a strong advocacy group,” he added. “Most are former injection drug users, and the public is often reluctant to help them.”
So what are the measurable results of these barriers? Among about 3.2 million individuals in the United States with chronic HCV infection, only half were ever tested for HCV, 38% received some sort of care related to their infection, 11% were treated, and 6% achieved SVR, Dr. Holmberg and his associates noted in a perspective piece (N Engl J Med. 2013;368:1859-861).
At the same time, the United States faces an emerging epidemic of new HCV infections in nonurban areas among young persons who inject drugs (MMWR. 64;453-8). “This is really a tale of two epidemics,” he added. “Control of the chronic and the acute outbreaks will require a multipronged approach, with interventions along a testing to cure continuum of care.”
Dr. Holmberg and his associates reported their findings at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers reported no funding sources and had no financial disclosures.
AT IDWEEK 2015
Key clinical point: Mortality from chronic hepatitis C virus infection continues to rise, despite significant improvements in antiviral therapies.
Major finding: Even with substantial underreporting, in 2013, deaths tied to chronic HCV infection exceeded mortality from 60 other reportable infectious diseases.
Data source: Analysis of 10 years of national death certificate data and 7 years of data from the Chronic Hepatitis Cohort Study.
Disclosures: The researchers reported no funding sources and made no financial disclosures.
High ALT/AST ratio linked to fatty liver risk in HCV
Individuals infected with the hepatitis C virus who have a higher ratio of alanine aminotransferase to aspartate aminotransferase may be at greater risk of developing nonalcoholic fatty liver disease and hepatosteatosis, new data suggest.
A community-based observational study in 1,354 Taiwanese individuals seropositive for hepatitis C virus – including 433 with nonalcoholic fatty liver disease – found a high alanine aminotransferase to aspartate aminotransferase ratio was significantly and independently associated with nonalcoholic fatty liver disease (OR, 1.90; 95% CI, 1.37 to 2.65; P less than .001) and high-degree nonalcoholic fatty liver disease (OR, 2.44; 95% CI, 1.58 to 3.77; P less than .001).
This effect was observed even after researchers accounted for potential confounders: age, body mass index, metabolic syndrome, cholesterol level, hepatitis B virus infection, and smoking.
The study found the ALT/AST ratio was significantly higher among patients with nonalcoholic fatty liver disease (1.2 ± 0.4 vs. 1.1 ± 0.4; P less than .001) – defined as hepatic steatosis by echogenic imaging – according to a paper published online Sept. 14 in BMJ Open.
Nonalcoholic fatty liver disease is a particular issue because not only can it progress to severe liver disease but it is also associated with a lower likelihood of achieving a sustained virologic response to antiviral therapy. In addition, the majority of cases of nonalcoholic fatty liver disease are silent and are discovered incidentally, the authors wrote.
“This is the first study to reveal a strong relationship between the ALT/AST ratio and NAFLD in patients with HCV, and the ALT/AST ratio was also an independent risk factor apart from the conventional risk factors for hepatosteatosis including the MetS [metabolic syndrome], LDL, TC, waist/hip ratio, and body mass index,” wrote Dr. Ming-Shyan Lin of Chang Gung Memorial Hospital, Taiwan, and coauthors.
While the AST/ALT ratio is a marker of liver cirrhosis and advanced liver disease, the ALT/AST ratio is also a marker for insulin resistance and metabolic syndrome.
Researchers also noted that individuals with hepatitis C infection and nonalcoholic fatty liver disease had a significantly higher incidence of metabolic syndrome, significantly higher fasting glucose, uric acid, and triglycerides, and a lower HDL than did those with low-degree nonalcoholic fatty liver disease.
“The prevalence of hepatosteatosis in chronic hepatitis C infection has been reported in up to 31%-72%, which is significantly higher than that in participants with other chronic liver disease such as hepatitis B or autoimmune hepatitis, suggesting a direct effect of HCV replication in the development of excess fat accumulation in the liver,” the authors wrote.
In this cohort, the prevalence of nonalcoholic fatty liver disease was 31.9%, and 19.6% of participants had moderate to severe hepatosteatosis (BMJ Open 2015, Sep 14. doi:10.1136/bmjopen-2015-008797).
Given the silent nature of nonalcoholic fatty liver disease, the authors suggested that the findings could help clinicians identify individuals with hepatosteatosis and implement interventions such as weight loss to reduce their risk of further progression.
No conflicts of interest were declared.
Individuals infected with the hepatitis C virus who have a higher ratio of alanine aminotransferase to aspartate aminotransferase may be at greater risk of developing nonalcoholic fatty liver disease and hepatosteatosis, new data suggest.
A community-based observational study in 1,354 Taiwanese individuals seropositive for hepatitis C virus – including 433 with nonalcoholic fatty liver disease – found a high alanine aminotransferase to aspartate aminotransferase ratio was significantly and independently associated with nonalcoholic fatty liver disease (OR, 1.90; 95% CI, 1.37 to 2.65; P less than .001) and high-degree nonalcoholic fatty liver disease (OR, 2.44; 95% CI, 1.58 to 3.77; P less than .001).
This effect was observed even after researchers accounted for potential confounders: age, body mass index, metabolic syndrome, cholesterol level, hepatitis B virus infection, and smoking.
The study found the ALT/AST ratio was significantly higher among patients with nonalcoholic fatty liver disease (1.2 ± 0.4 vs. 1.1 ± 0.4; P less than .001) – defined as hepatic steatosis by echogenic imaging – according to a paper published online Sept. 14 in BMJ Open.
Nonalcoholic fatty liver disease is a particular issue because not only can it progress to severe liver disease but it is also associated with a lower likelihood of achieving a sustained virologic response to antiviral therapy. In addition, the majority of cases of nonalcoholic fatty liver disease are silent and are discovered incidentally, the authors wrote.
“This is the first study to reveal a strong relationship between the ALT/AST ratio and NAFLD in patients with HCV, and the ALT/AST ratio was also an independent risk factor apart from the conventional risk factors for hepatosteatosis including the MetS [metabolic syndrome], LDL, TC, waist/hip ratio, and body mass index,” wrote Dr. Ming-Shyan Lin of Chang Gung Memorial Hospital, Taiwan, and coauthors.
While the AST/ALT ratio is a marker of liver cirrhosis and advanced liver disease, the ALT/AST ratio is also a marker for insulin resistance and metabolic syndrome.
Researchers also noted that individuals with hepatitis C infection and nonalcoholic fatty liver disease had a significantly higher incidence of metabolic syndrome, significantly higher fasting glucose, uric acid, and triglycerides, and a lower HDL than did those with low-degree nonalcoholic fatty liver disease.
“The prevalence of hepatosteatosis in chronic hepatitis C infection has been reported in up to 31%-72%, which is significantly higher than that in participants with other chronic liver disease such as hepatitis B or autoimmune hepatitis, suggesting a direct effect of HCV replication in the development of excess fat accumulation in the liver,” the authors wrote.
In this cohort, the prevalence of nonalcoholic fatty liver disease was 31.9%, and 19.6% of participants had moderate to severe hepatosteatosis (BMJ Open 2015, Sep 14. doi:10.1136/bmjopen-2015-008797).
Given the silent nature of nonalcoholic fatty liver disease, the authors suggested that the findings could help clinicians identify individuals with hepatosteatosis and implement interventions such as weight loss to reduce their risk of further progression.
No conflicts of interest were declared.
Individuals infected with the hepatitis C virus who have a higher ratio of alanine aminotransferase to aspartate aminotransferase may be at greater risk of developing nonalcoholic fatty liver disease and hepatosteatosis, new data suggest.
A community-based observational study in 1,354 Taiwanese individuals seropositive for hepatitis C virus – including 433 with nonalcoholic fatty liver disease – found a high alanine aminotransferase to aspartate aminotransferase ratio was significantly and independently associated with nonalcoholic fatty liver disease (OR, 1.90; 95% CI, 1.37 to 2.65; P less than .001) and high-degree nonalcoholic fatty liver disease (OR, 2.44; 95% CI, 1.58 to 3.77; P less than .001).
This effect was observed even after researchers accounted for potential confounders: age, body mass index, metabolic syndrome, cholesterol level, hepatitis B virus infection, and smoking.
The study found the ALT/AST ratio was significantly higher among patients with nonalcoholic fatty liver disease (1.2 ± 0.4 vs. 1.1 ± 0.4; P less than .001) – defined as hepatic steatosis by echogenic imaging – according to a paper published online Sept. 14 in BMJ Open.
Nonalcoholic fatty liver disease is a particular issue because not only can it progress to severe liver disease but it is also associated with a lower likelihood of achieving a sustained virologic response to antiviral therapy. In addition, the majority of cases of nonalcoholic fatty liver disease are silent and are discovered incidentally, the authors wrote.
“This is the first study to reveal a strong relationship between the ALT/AST ratio and NAFLD in patients with HCV, and the ALT/AST ratio was also an independent risk factor apart from the conventional risk factors for hepatosteatosis including the MetS [metabolic syndrome], LDL, TC, waist/hip ratio, and body mass index,” wrote Dr. Ming-Shyan Lin of Chang Gung Memorial Hospital, Taiwan, and coauthors.
While the AST/ALT ratio is a marker of liver cirrhosis and advanced liver disease, the ALT/AST ratio is also a marker for insulin resistance and metabolic syndrome.
Researchers also noted that individuals with hepatitis C infection and nonalcoholic fatty liver disease had a significantly higher incidence of metabolic syndrome, significantly higher fasting glucose, uric acid, and triglycerides, and a lower HDL than did those with low-degree nonalcoholic fatty liver disease.
“The prevalence of hepatosteatosis in chronic hepatitis C infection has been reported in up to 31%-72%, which is significantly higher than that in participants with other chronic liver disease such as hepatitis B or autoimmune hepatitis, suggesting a direct effect of HCV replication in the development of excess fat accumulation in the liver,” the authors wrote.
In this cohort, the prevalence of nonalcoholic fatty liver disease was 31.9%, and 19.6% of participants had moderate to severe hepatosteatosis (BMJ Open 2015, Sep 14. doi:10.1136/bmjopen-2015-008797).
Given the silent nature of nonalcoholic fatty liver disease, the authors suggested that the findings could help clinicians identify individuals with hepatosteatosis and implement interventions such as weight loss to reduce their risk of further progression.
No conflicts of interest were declared.
FROM BMJ OPEN
Key clinical point: A higher ratio of alanine aminotransferase to aspartate aminotransferase in individuals seropositive for hepatitis C virus may be associated with nonalcoholic fatty liver disease.
Major finding: A high ALT/AST ratio was significantly and independently associated with nonalcoholic fatty liver disease.
Data source: A community-based observational study in 1354 Taiwanese individuals seropositive for hepatitis C virus.
Disclosures: No conflicts of interest were declared.
Sofosbuvir reduces liver fibrosis in chronic hepatitis C
Antiviral treatment with sofosbuvir reduced liver fibrosis, as measured by three independent noninvasive predictors for liver fibrosis, and liver stiffness, in patients with chronic hepatitis C (CHC), according to new research published in the Digestive and Liver Disease (doi:10.1016/j.dld.2015.09.015).
“Despite the relatively small sample size, the effects on fibrosis parameters are impressive, implying clinically significant fibrosis regression and potential reduction of cirrhosis-associated mortality in successfully treated patients with CHC,” wrote Dr. Sebastian Bernuth of Cirrhosis Center Mainz (CCM), Johannes Gutenberg University Mainz, Germany, and colleagues.
CHC is a major cause of liver-associated mortality, and is responsible for approximately 25% of primary hepatocellular carcinomas and 25% of liver cirrhosis. Successful antiviral therapy with a sustained virological response (SVR) can reduce liver-related morbidity and mortality, including a decreased need for transplantation.
In 2014, the first NS5B RNA-polymerase inhibitor, sofosbuvir, was approved for use in conjunction with pegylated interferon-alpha (PEG-IFN) and/or ribavirin to treat hepatitis C infection, and yielded high SVR rates of around 90% after short-term therapy in genotype 1-3-infected patients.In this study, Dr. Benuth and his colleagues evaluated early changes in dynamic fibrosis-related parameters using the enhanced liver fibrosis (ELF) panel, combined with liver stiffness measurement (LSM), along with metabolic alterations in insulin resistance, and lipid and iron metabolism during sofosbuvir-based antiviral therapy.
A total of 32 patients were included in the analysis, and all received treatment with sofosbuvir, 19 in combination with PEG-IFN, 29 in combination with ribavirin, and four in combination with simeprevir.Patients experienced a biochemical and virological response within 4 weeks of starting treatment. At 12 weeks, the SVR was 93.8% and two patients experienced a relapse.There was a significant decrease from baseline to 12-week posttreatment follow-up in ELF (10.00 vs. 9.37; P = .007), and the median of the LSM (measured by Fibroscan) significantly decreased over the whole observation period, from 8 kPa (METAVIR F2) at baseline to 6.8 kPa (METAVIR F0-1) at 12 weeks (P = .016). This suggests a significant regression of liver fibrosis at 12 weeks, compared to baseline.The liver enzymes (ALT, AST, and gamma-GT) rapidly normalized under treatment, and total bilirubin also decreased from the baseline upper normal values (0.91 mg/dL) to 0.74 mg/dL (P = .034).“In conclusion, this is the first study implying significant and clinically relevant reduction in liver fibrosis measures by three independent noninvasive predictors for liver fibrosis assessment and liver stiffness measurement under highly effective antiviral regimens with sofosbuvir,” said the authors.
The study was supported by intramural funding of the University of Mainz (Inneruniversitäre Forschungsförderung Stufe I grant) to Dr. Tim Zimmermann, who has also received consultant/lecture fees and/or travel support from Abbvie, BMS, Gilead, Janssen-Cilag, Merck, and Roche. Dr. Martin F. Sprinzl received research funding from Gilead and lecture fees from Roche. All other authors have no conflicts of interest to declare in terms of this manuscript.
Antiviral treatment with sofosbuvir reduced liver fibrosis, as measured by three independent noninvasive predictors for liver fibrosis, and liver stiffness, in patients with chronic hepatitis C (CHC), according to new research published in the Digestive and Liver Disease (doi:10.1016/j.dld.2015.09.015).
“Despite the relatively small sample size, the effects on fibrosis parameters are impressive, implying clinically significant fibrosis regression and potential reduction of cirrhosis-associated mortality in successfully treated patients with CHC,” wrote Dr. Sebastian Bernuth of Cirrhosis Center Mainz (CCM), Johannes Gutenberg University Mainz, Germany, and colleagues.
CHC is a major cause of liver-associated mortality, and is responsible for approximately 25% of primary hepatocellular carcinomas and 25% of liver cirrhosis. Successful antiviral therapy with a sustained virological response (SVR) can reduce liver-related morbidity and mortality, including a decreased need for transplantation.
In 2014, the first NS5B RNA-polymerase inhibitor, sofosbuvir, was approved for use in conjunction with pegylated interferon-alpha (PEG-IFN) and/or ribavirin to treat hepatitis C infection, and yielded high SVR rates of around 90% after short-term therapy in genotype 1-3-infected patients.In this study, Dr. Benuth and his colleagues evaluated early changes in dynamic fibrosis-related parameters using the enhanced liver fibrosis (ELF) panel, combined with liver stiffness measurement (LSM), along with metabolic alterations in insulin resistance, and lipid and iron metabolism during sofosbuvir-based antiviral therapy.
A total of 32 patients were included in the analysis, and all received treatment with sofosbuvir, 19 in combination with PEG-IFN, 29 in combination with ribavirin, and four in combination with simeprevir.Patients experienced a biochemical and virological response within 4 weeks of starting treatment. At 12 weeks, the SVR was 93.8% and two patients experienced a relapse.There was a significant decrease from baseline to 12-week posttreatment follow-up in ELF (10.00 vs. 9.37; P = .007), and the median of the LSM (measured by Fibroscan) significantly decreased over the whole observation period, from 8 kPa (METAVIR F2) at baseline to 6.8 kPa (METAVIR F0-1) at 12 weeks (P = .016). This suggests a significant regression of liver fibrosis at 12 weeks, compared to baseline.The liver enzymes (ALT, AST, and gamma-GT) rapidly normalized under treatment, and total bilirubin also decreased from the baseline upper normal values (0.91 mg/dL) to 0.74 mg/dL (P = .034).“In conclusion, this is the first study implying significant and clinically relevant reduction in liver fibrosis measures by three independent noninvasive predictors for liver fibrosis assessment and liver stiffness measurement under highly effective antiviral regimens with sofosbuvir,” said the authors.
The study was supported by intramural funding of the University of Mainz (Inneruniversitäre Forschungsförderung Stufe I grant) to Dr. Tim Zimmermann, who has also received consultant/lecture fees and/or travel support from Abbvie, BMS, Gilead, Janssen-Cilag, Merck, and Roche. Dr. Martin F. Sprinzl received research funding from Gilead and lecture fees from Roche. All other authors have no conflicts of interest to declare in terms of this manuscript.
Antiviral treatment with sofosbuvir reduced liver fibrosis, as measured by three independent noninvasive predictors for liver fibrosis, and liver stiffness, in patients with chronic hepatitis C (CHC), according to new research published in the Digestive and Liver Disease (doi:10.1016/j.dld.2015.09.015).
“Despite the relatively small sample size, the effects on fibrosis parameters are impressive, implying clinically significant fibrosis regression and potential reduction of cirrhosis-associated mortality in successfully treated patients with CHC,” wrote Dr. Sebastian Bernuth of Cirrhosis Center Mainz (CCM), Johannes Gutenberg University Mainz, Germany, and colleagues.
CHC is a major cause of liver-associated mortality, and is responsible for approximately 25% of primary hepatocellular carcinomas and 25% of liver cirrhosis. Successful antiviral therapy with a sustained virological response (SVR) can reduce liver-related morbidity and mortality, including a decreased need for transplantation.
In 2014, the first NS5B RNA-polymerase inhibitor, sofosbuvir, was approved for use in conjunction with pegylated interferon-alpha (PEG-IFN) and/or ribavirin to treat hepatitis C infection, and yielded high SVR rates of around 90% after short-term therapy in genotype 1-3-infected patients.In this study, Dr. Benuth and his colleagues evaluated early changes in dynamic fibrosis-related parameters using the enhanced liver fibrosis (ELF) panel, combined with liver stiffness measurement (LSM), along with metabolic alterations in insulin resistance, and lipid and iron metabolism during sofosbuvir-based antiviral therapy.
A total of 32 patients were included in the analysis, and all received treatment with sofosbuvir, 19 in combination with PEG-IFN, 29 in combination with ribavirin, and four in combination with simeprevir.Patients experienced a biochemical and virological response within 4 weeks of starting treatment. At 12 weeks, the SVR was 93.8% and two patients experienced a relapse.There was a significant decrease from baseline to 12-week posttreatment follow-up in ELF (10.00 vs. 9.37; P = .007), and the median of the LSM (measured by Fibroscan) significantly decreased over the whole observation period, from 8 kPa (METAVIR F2) at baseline to 6.8 kPa (METAVIR F0-1) at 12 weeks (P = .016). This suggests a significant regression of liver fibrosis at 12 weeks, compared to baseline.The liver enzymes (ALT, AST, and gamma-GT) rapidly normalized under treatment, and total bilirubin also decreased from the baseline upper normal values (0.91 mg/dL) to 0.74 mg/dL (P = .034).“In conclusion, this is the first study implying significant and clinically relevant reduction in liver fibrosis measures by three independent noninvasive predictors for liver fibrosis assessment and liver stiffness measurement under highly effective antiviral regimens with sofosbuvir,” said the authors.
The study was supported by intramural funding of the University of Mainz (Inneruniversitäre Forschungsförderung Stufe I grant) to Dr. Tim Zimmermann, who has also received consultant/lecture fees and/or travel support from Abbvie, BMS, Gilead, Janssen-Cilag, Merck, and Roche. Dr. Martin F. Sprinzl received research funding from Gilead and lecture fees from Roche. All other authors have no conflicts of interest to declare in terms of this manuscript.
FROM DIGESTIVE AND LIVER DISEASE
Key clinical point: Treatment with sofosbuvir achieved clinically significant fibrosis regression and potential reduction of cirrhosis-associated mortality in patients with hepatitis C.
Major finding: There was a sustained virological response rate at 12-week follow-up (93.8%), and a significant decrease from baseline to 12-week posttreatment follow-up in enhanced liver fibrosis (ELF) scores (10.00 vs. 9.37; P = .007) and FibroScan (8.0 vs. 6.8 kPa; P = .016)
Data source: A total of 32 hepatitis C patients were treated prospectively with sofosbuvir and ELF scores and FibroScan measurements were taken at baseline, week 4, end of treatment, and 12 weeks thereafter.
Disclosures: The study was supported by intramural funding of the University of Mainz (Inneruniversitäre Forschungsförderung Stufe I grant) to Dr. Tim Zimmermann, who has also received consultant/lecture fees and/or travel support from Abbvie, BMS, Gilead, Janssen-Cilag, Merck, and Roche. Dr. Martin F. Sprinzl received research funding from Gilead and lecture fees from Roche. All other authors have no conflicts of interest to declare in terms of this manuscript.
Hepatitis C drove steep rises in cirrhosis, HCC, and related deaths
Cirrhosis nearly doubled among Veterans Affairs patients between 2001 and 2013, while cirrhosis-related mortality rose by about 50% and deaths from hepatocellular carcinoma almost tripled, investigators reported in the November issue of Gastroenterology.
Hepatitis C virus infection was “the overwhelming driver of these trends, with smaller contributions from alcoholic liver disease, nonalcoholic fatty liver disease, and other liver diseases,” said Dr. Lauren Beste of the University of Washington, Seattle, and her associates. Based on their data, the prevalence of cirrhosis in the United States will peak in 2021, they said. “In contrast, the incidence of HCC continues to increase, confirming worrisome predictions of rapid growth put forward by work (Gastroenterology. 2010;138[2]:513-21) conducted” in the early 2000s.
New HCV infections have dropped sharply in the United States since about 1990, but cases of HCV-related cirrhosis and HCC continue to rise as chronically infected patients age and their liver disease progresses. Although the burden of cirrhosis and HCC due to HCV infection is expected to peak in about the year 2020, the population-level effects of nonalcoholic fatty liver disease, alcoholic liver disease, and hepatitis B virus infection remained unclear, the investigators said. Therefore, they retrospectively studied underlying etiologies among a national cohort of almost 130,000 Veterans Affairs patients with cirrhosis and more than 21,000 patients with HCC between 2001 and 2013 (Gastroenterology 2015. doi: 10.1053/j.gastro.2015.07.056).
In 2013, the VA cared for more than 5.7 million patients, including about 1% with cirrhosis and 0.13% with HCC. Between 2001 and 2013, the prevalence of cirrhosis almost doubled, rising from 664 to 1,058 cases for every 100,000 patients. Deaths among cirrhotic patients also increased by about half, rising from 83 to 126 for every 100,000 patient-years. These liver-related deaths were mainly caused by HCC, whose incidence rose about 2.5 times from 17 to 45 per 100,000 patient-years, Dr. Beste and her associates reported.
Notably, deaths due to liver cancer rose threefold – from 13 to 37 per 100,000 patient-years between 2001 and 2013, “driven overwhelmingly by HCV with much smaller contributions from NAFLD and alcoholic liver disease,” said the researchers. By 2013, almost half of cirrhosis cases and related deaths occurred among HCV-infected patients, as did 67% of HCC cases and related deaths, they noted.
About 60% of patients with cirrhosis and HCV infection also had a longstanding history of alcohol use, the researchers noted. Addressing both factors, as well as diabetes, obesity, and other drivers of nonalcoholic fatty liver disease, could help ease the national burden of liver disease and liver-related mortality among U.S. veterans and other groups, they added. “The increasing burden of cirrhosis and HCC highlights the need for greater efforts to address their causes at a population level,” Dr. Beste and her associates wrote. “Health care systems will need to accommodate rising numbers of patients with cirrhosis and HCC.”
The Department of Veterans Affairs and the Veterans Health Administration funded the study. The investigators declared no competing interests.
Despite recent advances in hepatitis C virus treatment, many infected patients have preexisting liver fibrosis that puts them at risk for cirrhosis and hepatocellular carcinoma. Meanwhile, risk factors for nonalcoholic fatty liver disease (NAFLD) are increasingly prevalent. In this study, the investigators sought to understand the contribution of liver disease etiology to trends in adverse liver outcomes (the prevalence, incidence, and mortality of cirrhosis and HCC). They identified all VA health care users from 2001 to 2013 with diagnoses of cirrhosis (n = 129,998) or HCC (n = 21,326) and their liver disease etiology, and compared outcomes by calendar year.
 |
Dr. Barry Schlansky |
Over the study period, marked increases in cirrhosis prevalence (59%), cirrhosis mortality (52%), HCC incidence (164%), and HCC mortality (185%) were observed in this national VA cohort. The increasing prevalence of cirrhosis was mainly driven by increasing contributions from HCV or NAFLD liver disease, but rises in mortality from cirrhosis and both incidence and mortality from HCC were almost entirely due to HCV. Based on these trends, the researchers forecasted that the prevalence of cirrhosis will plateau and begin to decline in 2021 (2020 in the HCV subgroup), but rates of HCC will continue to surge.
Although these results differ from two recent analyses of the national cancer surveillance registry (SEER) that found decelerations in HCC incidence and mortality in recent years, the current study included methodologic features (stratification by liver disease etiology and absence of age standardization) that likely facilitated more accurate estimates of HCC incidence and mortality. The generalizability of VA data to the general population is always debated (the former is nearly exclusively men with a higher prevalence of HCV infection and other liver disease risk factors, all of whom have access to medical care), yet the researchers rightly note that the time trends in cirrhosis and HCC outcomes (rather than absolute numbers) are still applicable to the non-VA population, particularly men. This study highlights the dramatic rise in cirrhosis and HCC, and associated deaths from these conditions, over the last decade. In addition to aggressive treatment of the underlying cause of liver disease, meaningful reductions in the burden of advanced liver disease will require a renewed focus on measures to improve adherence with maintenance care for cirrhotic patients, especially liver cancer screening.
Dr. Barry Schlansky is assistant professor, division of gastroenterology and hepatology, department of medicine, Oregon Health and Science University, Portland. He has no conflicts of interest.
Despite recent advances in hepatitis C virus treatment, many infected patients have preexisting liver fibrosis that puts them at risk for cirrhosis and hepatocellular carcinoma. Meanwhile, risk factors for nonalcoholic fatty liver disease (NAFLD) are increasingly prevalent. In this study, the investigators sought to understand the contribution of liver disease etiology to trends in adverse liver outcomes (the prevalence, incidence, and mortality of cirrhosis and HCC). They identified all VA health care users from 2001 to 2013 with diagnoses of cirrhosis (n = 129,998) or HCC (n = 21,326) and their liver disease etiology, and compared outcomes by calendar year.
 |
Dr. Barry Schlansky |
Over the study period, marked increases in cirrhosis prevalence (59%), cirrhosis mortality (52%), HCC incidence (164%), and HCC mortality (185%) were observed in this national VA cohort. The increasing prevalence of cirrhosis was mainly driven by increasing contributions from HCV or NAFLD liver disease, but rises in mortality from cirrhosis and both incidence and mortality from HCC were almost entirely due to HCV. Based on these trends, the researchers forecasted that the prevalence of cirrhosis will plateau and begin to decline in 2021 (2020 in the HCV subgroup), but rates of HCC will continue to surge.
Although these results differ from two recent analyses of the national cancer surveillance registry (SEER) that found decelerations in HCC incidence and mortality in recent years, the current study included methodologic features (stratification by liver disease etiology and absence of age standardization) that likely facilitated more accurate estimates of HCC incidence and mortality. The generalizability of VA data to the general population is always debated (the former is nearly exclusively men with a higher prevalence of HCV infection and other liver disease risk factors, all of whom have access to medical care), yet the researchers rightly note that the time trends in cirrhosis and HCC outcomes (rather than absolute numbers) are still applicable to the non-VA population, particularly men. This study highlights the dramatic rise in cirrhosis and HCC, and associated deaths from these conditions, over the last decade. In addition to aggressive treatment of the underlying cause of liver disease, meaningful reductions in the burden of advanced liver disease will require a renewed focus on measures to improve adherence with maintenance care for cirrhotic patients, especially liver cancer screening.
Dr. Barry Schlansky is assistant professor, division of gastroenterology and hepatology, department of medicine, Oregon Health and Science University, Portland. He has no conflicts of interest.
Despite recent advances in hepatitis C virus treatment, many infected patients have preexisting liver fibrosis that puts them at risk for cirrhosis and hepatocellular carcinoma. Meanwhile, risk factors for nonalcoholic fatty liver disease (NAFLD) are increasingly prevalent. In this study, the investigators sought to understand the contribution of liver disease etiology to trends in adverse liver outcomes (the prevalence, incidence, and mortality of cirrhosis and HCC). They identified all VA health care users from 2001 to 2013 with diagnoses of cirrhosis (n = 129,998) or HCC (n = 21,326) and their liver disease etiology, and compared outcomes by calendar year.
 |
Dr. Barry Schlansky |
Over the study period, marked increases in cirrhosis prevalence (59%), cirrhosis mortality (52%), HCC incidence (164%), and HCC mortality (185%) were observed in this national VA cohort. The increasing prevalence of cirrhosis was mainly driven by increasing contributions from HCV or NAFLD liver disease, but rises in mortality from cirrhosis and both incidence and mortality from HCC were almost entirely due to HCV. Based on these trends, the researchers forecasted that the prevalence of cirrhosis will plateau and begin to decline in 2021 (2020 in the HCV subgroup), but rates of HCC will continue to surge.
Although these results differ from two recent analyses of the national cancer surveillance registry (SEER) that found decelerations in HCC incidence and mortality in recent years, the current study included methodologic features (stratification by liver disease etiology and absence of age standardization) that likely facilitated more accurate estimates of HCC incidence and mortality. The generalizability of VA data to the general population is always debated (the former is nearly exclusively men with a higher prevalence of HCV infection and other liver disease risk factors, all of whom have access to medical care), yet the researchers rightly note that the time trends in cirrhosis and HCC outcomes (rather than absolute numbers) are still applicable to the non-VA population, particularly men. This study highlights the dramatic rise in cirrhosis and HCC, and associated deaths from these conditions, over the last decade. In addition to aggressive treatment of the underlying cause of liver disease, meaningful reductions in the burden of advanced liver disease will require a renewed focus on measures to improve adherence with maintenance care for cirrhotic patients, especially liver cancer screening.
Dr. Barry Schlansky is assistant professor, division of gastroenterology and hepatology, department of medicine, Oregon Health and Science University, Portland. He has no conflicts of interest.
Cirrhosis nearly doubled among Veterans Affairs patients between 2001 and 2013, while cirrhosis-related mortality rose by about 50% and deaths from hepatocellular carcinoma almost tripled, investigators reported in the November issue of Gastroenterology.
Hepatitis C virus infection was “the overwhelming driver of these trends, with smaller contributions from alcoholic liver disease, nonalcoholic fatty liver disease, and other liver diseases,” said Dr. Lauren Beste of the University of Washington, Seattle, and her associates. Based on their data, the prevalence of cirrhosis in the United States will peak in 2021, they said. “In contrast, the incidence of HCC continues to increase, confirming worrisome predictions of rapid growth put forward by work (Gastroenterology. 2010;138[2]:513-21) conducted” in the early 2000s.
New HCV infections have dropped sharply in the United States since about 1990, but cases of HCV-related cirrhosis and HCC continue to rise as chronically infected patients age and their liver disease progresses. Although the burden of cirrhosis and HCC due to HCV infection is expected to peak in about the year 2020, the population-level effects of nonalcoholic fatty liver disease, alcoholic liver disease, and hepatitis B virus infection remained unclear, the investigators said. Therefore, they retrospectively studied underlying etiologies among a national cohort of almost 130,000 Veterans Affairs patients with cirrhosis and more than 21,000 patients with HCC between 2001 and 2013 (Gastroenterology 2015. doi: 10.1053/j.gastro.2015.07.056).
In 2013, the VA cared for more than 5.7 million patients, including about 1% with cirrhosis and 0.13% with HCC. Between 2001 and 2013, the prevalence of cirrhosis almost doubled, rising from 664 to 1,058 cases for every 100,000 patients. Deaths among cirrhotic patients also increased by about half, rising from 83 to 126 for every 100,000 patient-years. These liver-related deaths were mainly caused by HCC, whose incidence rose about 2.5 times from 17 to 45 per 100,000 patient-years, Dr. Beste and her associates reported.
Notably, deaths due to liver cancer rose threefold – from 13 to 37 per 100,000 patient-years between 2001 and 2013, “driven overwhelmingly by HCV with much smaller contributions from NAFLD and alcoholic liver disease,” said the researchers. By 2013, almost half of cirrhosis cases and related deaths occurred among HCV-infected patients, as did 67% of HCC cases and related deaths, they noted.
About 60% of patients with cirrhosis and HCV infection also had a longstanding history of alcohol use, the researchers noted. Addressing both factors, as well as diabetes, obesity, and other drivers of nonalcoholic fatty liver disease, could help ease the national burden of liver disease and liver-related mortality among U.S. veterans and other groups, they added. “The increasing burden of cirrhosis and HCC highlights the need for greater efforts to address their causes at a population level,” Dr. Beste and her associates wrote. “Health care systems will need to accommodate rising numbers of patients with cirrhosis and HCC.”
The Department of Veterans Affairs and the Veterans Health Administration funded the study. The investigators declared no competing interests.
Cirrhosis nearly doubled among Veterans Affairs patients between 2001 and 2013, while cirrhosis-related mortality rose by about 50% and deaths from hepatocellular carcinoma almost tripled, investigators reported in the November issue of Gastroenterology.
Hepatitis C virus infection was “the overwhelming driver of these trends, with smaller contributions from alcoholic liver disease, nonalcoholic fatty liver disease, and other liver diseases,” said Dr. Lauren Beste of the University of Washington, Seattle, and her associates. Based on their data, the prevalence of cirrhosis in the United States will peak in 2021, they said. “In contrast, the incidence of HCC continues to increase, confirming worrisome predictions of rapid growth put forward by work (Gastroenterology. 2010;138[2]:513-21) conducted” in the early 2000s.
New HCV infections have dropped sharply in the United States since about 1990, but cases of HCV-related cirrhosis and HCC continue to rise as chronically infected patients age and their liver disease progresses. Although the burden of cirrhosis and HCC due to HCV infection is expected to peak in about the year 2020, the population-level effects of nonalcoholic fatty liver disease, alcoholic liver disease, and hepatitis B virus infection remained unclear, the investigators said. Therefore, they retrospectively studied underlying etiologies among a national cohort of almost 130,000 Veterans Affairs patients with cirrhosis and more than 21,000 patients with HCC between 2001 and 2013 (Gastroenterology 2015. doi: 10.1053/j.gastro.2015.07.056).
In 2013, the VA cared for more than 5.7 million patients, including about 1% with cirrhosis and 0.13% with HCC. Between 2001 and 2013, the prevalence of cirrhosis almost doubled, rising from 664 to 1,058 cases for every 100,000 patients. Deaths among cirrhotic patients also increased by about half, rising from 83 to 126 for every 100,000 patient-years. These liver-related deaths were mainly caused by HCC, whose incidence rose about 2.5 times from 17 to 45 per 100,000 patient-years, Dr. Beste and her associates reported.
Notably, deaths due to liver cancer rose threefold – from 13 to 37 per 100,000 patient-years between 2001 and 2013, “driven overwhelmingly by HCV with much smaller contributions from NAFLD and alcoholic liver disease,” said the researchers. By 2013, almost half of cirrhosis cases and related deaths occurred among HCV-infected patients, as did 67% of HCC cases and related deaths, they noted.
About 60% of patients with cirrhosis and HCV infection also had a longstanding history of alcohol use, the researchers noted. Addressing both factors, as well as diabetes, obesity, and other drivers of nonalcoholic fatty liver disease, could help ease the national burden of liver disease and liver-related mortality among U.S. veterans and other groups, they added. “The increasing burden of cirrhosis and HCC highlights the need for greater efforts to address their causes at a population level,” Dr. Beste and her associates wrote. “Health care systems will need to accommodate rising numbers of patients with cirrhosis and HCC.”
The Department of Veterans Affairs and the Veterans Health Administration funded the study. The investigators declared no competing interests.
FROM GASTROENTEROLOGY
Key clinical point: Cirrhosis, hepatocellular carcinoma, and liver-related mortality rose substantially among Veterans Affairs patients over the past 12 years, mainly driven by HCV infection.
Major finding: The prevalence of cirrhosis nearly doubled between 2001 and 2013, while cirrhosis-related deaths rose by about 50% and the incidence of hepatocellular carcinoma almost tripled.
Data source: A retrospective cohort study of 129,998 Veterans Affairs patients with cirrhosis and 21,326 VA patients with HCC between 2001 and 2013.
Disclosures: The Department of Veterans Affairs and the Veterans Health Administration funded the study. The investigators declared no competing interests.
PCORI approves $83 million for HCV, rare disease research
The Patient-Centered Outcomes Research Institute (PCORI) board has approved $83 million in funding for research on hepatitis C virus and other diseases, the group announced Sept. 28.
Two of the 26 awards, totaling $29.5 million, will be used towards studies on caring for HCV patients, PCORI said in a statement.
The HCV awards were the result of a “targeted funding opportunity PCORI issued in response to input from the health care community, which identified HCV infection as a top health concern,” the statement said. PCORI is an independent, nonprofit organization based in Washington.
Studies will focus on comparing different antiviral medication regimens and improving treatment adherence in injection drug users.
“New oral medications for HCV offer significant improvements over previous therapies, but they were tested in specialized settings with carefully selected groups of patients,” PCORI said. The group hopes the grants will help close these research gaps and provide evidence of long-term efficacy, so patients and providers can make informed treatment decisions.
The HCV trials “will involve national advocacy organizations, major professional associations, payers, or other key patient and stakeholder groups in their research design and implementation,” PCORI said.
Read more at the PCORI website.
The Patient-Centered Outcomes Research Institute (PCORI) board has approved $83 million in funding for research on hepatitis C virus and other diseases, the group announced Sept. 28.
Two of the 26 awards, totaling $29.5 million, will be used towards studies on caring for HCV patients, PCORI said in a statement.
The HCV awards were the result of a “targeted funding opportunity PCORI issued in response to input from the health care community, which identified HCV infection as a top health concern,” the statement said. PCORI is an independent, nonprofit organization based in Washington.
Studies will focus on comparing different antiviral medication regimens and improving treatment adherence in injection drug users.
“New oral medications for HCV offer significant improvements over previous therapies, but they were tested in specialized settings with carefully selected groups of patients,” PCORI said. The group hopes the grants will help close these research gaps and provide evidence of long-term efficacy, so patients and providers can make informed treatment decisions.
The HCV trials “will involve national advocacy organizations, major professional associations, payers, or other key patient and stakeholder groups in their research design and implementation,” PCORI said.
Read more at the PCORI website.
The Patient-Centered Outcomes Research Institute (PCORI) board has approved $83 million in funding for research on hepatitis C virus and other diseases, the group announced Sept. 28.
Two of the 26 awards, totaling $29.5 million, will be used towards studies on caring for HCV patients, PCORI said in a statement.
The HCV awards were the result of a “targeted funding opportunity PCORI issued in response to input from the health care community, which identified HCV infection as a top health concern,” the statement said. PCORI is an independent, nonprofit organization based in Washington.
Studies will focus on comparing different antiviral medication regimens and improving treatment adherence in injection drug users.
“New oral medications for HCV offer significant improvements over previous therapies, but they were tested in specialized settings with carefully selected groups of patients,” PCORI said. The group hopes the grants will help close these research gaps and provide evidence of long-term efficacy, so patients and providers can make informed treatment decisions.
The HCV trials “will involve national advocacy organizations, major professional associations, payers, or other key patient and stakeholder groups in their research design and implementation,” PCORI said.
Read more at the PCORI website.
Sofosbuvir-velpatasvir combo effective in all HCV genotypes
A once-daily, fixed-dose combination of sofosbuvir (SOF) plus velpatasvir (VEL) had high success rates for the treatment of all six genotypes of hepatitis C virus, manufacturer Gilead Sciences reported.
In three of four phase III trials (ASTRAL-1, ASTRAL-2, and ASTRAL-3), 1,035 HCV patients were given the drug combination for 12 weeks. In the fourth trial (ASTRAL-4), 267 HCV patients with decompensated cirrhosis were randomized to receive either the SOF/VEL combination for 12 weeks with or without ribavirin or 24 weeks of just SOF/VEL. The primary efficacy endpoint for all studies was a sustained virological response at 12 weeks, the company said in a statement.
Results showed that 98% of patients in the first three trials achieved the efficacy endpoint. In the ASTRAL-4 study, 94% of patients in the SOF/VEL plus ribavirin group achieved sustained virological response at 12 weeks. The rates of success in patients receiving the SOF/VEL combination for 12 or 24 weeks were 83% and 86%, respectively. The most common adverse effects were fatigue, nausea, and headache.
The FDA has designated the SOF/VEL combination as “breakthrough therapy” status, granted to “investigational medicines that may offer major advances in treatment over existing options,” the statement said.
A once-daily, fixed-dose combination of sofosbuvir (SOF) plus velpatasvir (VEL) had high success rates for the treatment of all six genotypes of hepatitis C virus, manufacturer Gilead Sciences reported.
In three of four phase III trials (ASTRAL-1, ASTRAL-2, and ASTRAL-3), 1,035 HCV patients were given the drug combination for 12 weeks. In the fourth trial (ASTRAL-4), 267 HCV patients with decompensated cirrhosis were randomized to receive either the SOF/VEL combination for 12 weeks with or without ribavirin or 24 weeks of just SOF/VEL. The primary efficacy endpoint for all studies was a sustained virological response at 12 weeks, the company said in a statement.
Results showed that 98% of patients in the first three trials achieved the efficacy endpoint. In the ASTRAL-4 study, 94% of patients in the SOF/VEL plus ribavirin group achieved sustained virological response at 12 weeks. The rates of success in patients receiving the SOF/VEL combination for 12 or 24 weeks were 83% and 86%, respectively. The most common adverse effects were fatigue, nausea, and headache.
The FDA has designated the SOF/VEL combination as “breakthrough therapy” status, granted to “investigational medicines that may offer major advances in treatment over existing options,” the statement said.
A once-daily, fixed-dose combination of sofosbuvir (SOF) plus velpatasvir (VEL) had high success rates for the treatment of all six genotypes of hepatitis C virus, manufacturer Gilead Sciences reported.
In three of four phase III trials (ASTRAL-1, ASTRAL-2, and ASTRAL-3), 1,035 HCV patients were given the drug combination for 12 weeks. In the fourth trial (ASTRAL-4), 267 HCV patients with decompensated cirrhosis were randomized to receive either the SOF/VEL combination for 12 weeks with or without ribavirin or 24 weeks of just SOF/VEL. The primary efficacy endpoint for all studies was a sustained virological response at 12 weeks, the company said in a statement.
Results showed that 98% of patients in the first three trials achieved the efficacy endpoint. In the ASTRAL-4 study, 94% of patients in the SOF/VEL plus ribavirin group achieved sustained virological response at 12 weeks. The rates of success in patients receiving the SOF/VEL combination for 12 or 24 weeks were 83% and 86%, respectively. The most common adverse effects were fatigue, nausea, and headache.
The FDA has designated the SOF/VEL combination as “breakthrough therapy” status, granted to “investigational medicines that may offer major advances in treatment over existing options,” the statement said.
Smartphone app can pick up covert hepatic encephalopathy
Researchers have road-tested an app based on the Stroop test, which is designed to detect covert hepatic encephalopathy, with results suggesting it achieves results similar to those of a paper-based Stroop test.
The smartphone-based EncephalApp was tested in 167 patients with cirrhosis and 114 healthy age-matched controls, and showed significant correlation with individual paper/pen test and with crashes and illegal turns in driving simulation tests, as well as high test/retest reliability at 1 and 3 months.
The study also found that patients with prior overt hepatic encephalopathy had significantly worse response times with the EncephalApp compared to controls (Clin Gastroenterol Hepatol. 2015;13:1828-35).
“Although these [gold standard paper-pencil] measures are used to diagnose CHE [covert hepatic encephalopathy] in research studies, they have not found traction in clinical practice because of their copyrighted nature, need for psychological expertise, and time requirements,” wrote Dr. Jasmohan S. Bajaj of Virginia Commonwealth University and McGuire VA Hospital, both in Richmond, Va.
“Our results are in sync with the prior experience with the old Stroop App in that in similar prior HE [hepatic encephalopathy] studies, we found that the psychomotor function, i.e., the time required to complete tasks, was much more predictive than the errors committed (number of runs required) and the cognitive flexibility measures (OnTime-OffTime) in differentiating groups,” wrote Dr. Bajaj and colleagues.
The National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Advancing Translational Research and the McGuire Research Institute funded the study. There were no other conflicts of interest declared.
Researchers have road-tested an app based on the Stroop test, which is designed to detect covert hepatic encephalopathy, with results suggesting it achieves results similar to those of a paper-based Stroop test.
The smartphone-based EncephalApp was tested in 167 patients with cirrhosis and 114 healthy age-matched controls, and showed significant correlation with individual paper/pen test and with crashes and illegal turns in driving simulation tests, as well as high test/retest reliability at 1 and 3 months.
The study also found that patients with prior overt hepatic encephalopathy had significantly worse response times with the EncephalApp compared to controls (Clin Gastroenterol Hepatol. 2015;13:1828-35).
“Although these [gold standard paper-pencil] measures are used to diagnose CHE [covert hepatic encephalopathy] in research studies, they have not found traction in clinical practice because of their copyrighted nature, need for psychological expertise, and time requirements,” wrote Dr. Jasmohan S. Bajaj of Virginia Commonwealth University and McGuire VA Hospital, both in Richmond, Va.
“Our results are in sync with the prior experience with the old Stroop App in that in similar prior HE [hepatic encephalopathy] studies, we found that the psychomotor function, i.e., the time required to complete tasks, was much more predictive than the errors committed (number of runs required) and the cognitive flexibility measures (OnTime-OffTime) in differentiating groups,” wrote Dr. Bajaj and colleagues.
The National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Advancing Translational Research and the McGuire Research Institute funded the study. There were no other conflicts of interest declared.
Researchers have road-tested an app based on the Stroop test, which is designed to detect covert hepatic encephalopathy, with results suggesting it achieves results similar to those of a paper-based Stroop test.
The smartphone-based EncephalApp was tested in 167 patients with cirrhosis and 114 healthy age-matched controls, and showed significant correlation with individual paper/pen test and with crashes and illegal turns in driving simulation tests, as well as high test/retest reliability at 1 and 3 months.
The study also found that patients with prior overt hepatic encephalopathy had significantly worse response times with the EncephalApp compared to controls (Clin Gastroenterol Hepatol. 2015;13:1828-35).
“Although these [gold standard paper-pencil] measures are used to diagnose CHE [covert hepatic encephalopathy] in research studies, they have not found traction in clinical practice because of their copyrighted nature, need for psychological expertise, and time requirements,” wrote Dr. Jasmohan S. Bajaj of Virginia Commonwealth University and McGuire VA Hospital, both in Richmond, Va.
“Our results are in sync with the prior experience with the old Stroop App in that in similar prior HE [hepatic encephalopathy] studies, we found that the psychomotor function, i.e., the time required to complete tasks, was much more predictive than the errors committed (number of runs required) and the cognitive flexibility measures (OnTime-OffTime) in differentiating groups,” wrote Dr. Bajaj and colleagues.
The National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Advancing Translational Research and the McGuire Research Institute funded the study. There were no other conflicts of interest declared.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point:A smartphone-based app has achieved results in detecting covert hepatic encephalopathy similar to those of a paper/pen–based Stroop test.
Major finding: EncephalApp showed significant correlation with individual paper/pen test and with crashes and illegal turns in driving simulation tests, as well as high test/retest reliability.
Data source: Controlled study of 167 patients with cirrhosis and 114 healthy age-matched controls.
Disclosures: The National Institute of Diabetes and Digestive and Kidney Diseases, the National Center for Advancing Translational Research, and the McGuire Research Institute funded the study. There were no other conflicts of interest declared.
Integrated care overcomes HCV treatment barriers
Patients with hepatitis C and psychiatric disorders or substance abuse problems benefit significantly from an integrated care model of treatment, with a randomized controlled trial showing such an approach is linked to greater rates of antiviral therapy and treatment response.
The prospective trial of integrated care versus usual care involved 363 patients attending three hepatitis C (HCV) clinics, with the integrated care being delivered by a midlevel mental health provider within the clinic who served as the regular contact and case manager.
Patients randomized to integrated care, which included brief psychological interventions and case management, were more than twice as likely to start antiviral therapy earlier and achieve a sustained virologic response than those who received usual care, according to Dr. Samuel B. Ho of the VA San Diego Healthcare System and his coauthors.
While individuals with a history of prior psychiatric disorder or active drug use were significantly less likely to achieve sustained virologic response, the integrated-care approach had particularly positive effects on treatment initiative and response for individuals with a risk for active psychiatric disease at baseline, they said (Clin Gastroenterol Hepatol. 2015. doi: 10.1016/j.cgh.2015.02.022).
“To optimize the public health impact of antiviral treatments for HCV, the number of patients who are able to receive these treatments must be expanded,” wrote Dr. Ho and his associates, adding that “new interferon-free regimens have fewer side effects and are expected to expand treatment populations to include a broader range of patients, many with very significant psychiatric and substance abuse disorders.”
The study was supported by VA Health Services Research and Development. Three authors declared research support, grants, advisory board positions or speakers bureau roles with the pharmaceutical industry.
Patients with hepatitis C and psychiatric disorders or substance abuse problems benefit significantly from an integrated care model of treatment, with a randomized controlled trial showing such an approach is linked to greater rates of antiviral therapy and treatment response.
The prospective trial of integrated care versus usual care involved 363 patients attending three hepatitis C (HCV) clinics, with the integrated care being delivered by a midlevel mental health provider within the clinic who served as the regular contact and case manager.
Patients randomized to integrated care, which included brief psychological interventions and case management, were more than twice as likely to start antiviral therapy earlier and achieve a sustained virologic response than those who received usual care, according to Dr. Samuel B. Ho of the VA San Diego Healthcare System and his coauthors.
While individuals with a history of prior psychiatric disorder or active drug use were significantly less likely to achieve sustained virologic response, the integrated-care approach had particularly positive effects on treatment initiative and response for individuals with a risk for active psychiatric disease at baseline, they said (Clin Gastroenterol Hepatol. 2015. doi: 10.1016/j.cgh.2015.02.022).
“To optimize the public health impact of antiviral treatments for HCV, the number of patients who are able to receive these treatments must be expanded,” wrote Dr. Ho and his associates, adding that “new interferon-free regimens have fewer side effects and are expected to expand treatment populations to include a broader range of patients, many with very significant psychiatric and substance abuse disorders.”
The study was supported by VA Health Services Research and Development. Three authors declared research support, grants, advisory board positions or speakers bureau roles with the pharmaceutical industry.
Patients with hepatitis C and psychiatric disorders or substance abuse problems benefit significantly from an integrated care model of treatment, with a randomized controlled trial showing such an approach is linked to greater rates of antiviral therapy and treatment response.
The prospective trial of integrated care versus usual care involved 363 patients attending three hepatitis C (HCV) clinics, with the integrated care being delivered by a midlevel mental health provider within the clinic who served as the regular contact and case manager.
Patients randomized to integrated care, which included brief psychological interventions and case management, were more than twice as likely to start antiviral therapy earlier and achieve a sustained virologic response than those who received usual care, according to Dr. Samuel B. Ho of the VA San Diego Healthcare System and his coauthors.
While individuals with a history of prior psychiatric disorder or active drug use were significantly less likely to achieve sustained virologic response, the integrated-care approach had particularly positive effects on treatment initiative and response for individuals with a risk for active psychiatric disease at baseline, they said (Clin Gastroenterol Hepatol. 2015. doi: 10.1016/j.cgh.2015.02.022).
“To optimize the public health impact of antiviral treatments for HCV, the number of patients who are able to receive these treatments must be expanded,” wrote Dr. Ho and his associates, adding that “new interferon-free regimens have fewer side effects and are expected to expand treatment populations to include a broader range of patients, many with very significant psychiatric and substance abuse disorders.”
The study was supported by VA Health Services Research and Development. Three authors declared research support, grants, advisory board positions or speakers bureau roles with the pharmaceutical industry.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point:Patients with hepatitis C and psychiatric disorders or substance abuse problems benefit significantly from an integrated care model of treatment.
Major finding: Integrated care was associated with a more than twofold increase in early initiation of antiviral therapy and sustained virologic response.
Data source: A prospective, randomized controlled trial in 363 patients with hepatitis C and psychiatric disorders or substance abuse problems.
Disclosures: The study was supported by VA Health Services Research and Development. Three authors declared research support, grants, advisory board positions, or speakers bureau roles with the pharmaceutical industry.
Hepatitis E linked to 1 in 10 liver failure cases in Europe
A significant number of cases of acute liver failure may be caused by the hepatitis E virus, which a new study suggests may not necessarily be identified or excluded using serologic tests.
A retrospective analysis of 80 European patients with acute liver failure or acute hepatitis found that, while 12 patients (15%) tested positive for hepatitis E virus (HEV) IgG antibodies, seven of these patients were negative for IgM antibodies or HEV RNA, according to a study published in Clinical Gastroenterology and Hepatology.
Eight patients (10%) tested positive for HEV RNA, but only four of these were definitely positive for HEV IgG and five for HEV IgM.
Four were initially diagnosed as having idiosyncratic drug-induced liver injury, with other diagnoses being acetaminophen intoxication, amanita intoxication, and Wilson’s disease; one patient who had received a hematopoietic stem cell transplant was initially diagnosed with graft-versus-host disease.
One patient died, two received liver transplants, and the remaining patients survived (Clin Gastro Hepatol. 2015. doi: 10.1016/j.cgh.2015.04.014).
“Our data confirms recent descriptions of cases of severe liver injury in Europe, and underlines the necessity to consider hepatitis E as an underlying or additional cause for ALF [acute liver failure],” wrote Dr. Paul Manka of the University Duisburg-Essen in Essen, Germany, and coauthors.
The study was supported by the Deutsche Forschungsgemeinschaft (German Research Foundation) and by the Wilhelm-Laupitz Foundation. There were no other conflicts of interest declared.
A significant number of cases of acute liver failure may be caused by the hepatitis E virus, which a new study suggests may not necessarily be identified or excluded using serologic tests.
A retrospective analysis of 80 European patients with acute liver failure or acute hepatitis found that, while 12 patients (15%) tested positive for hepatitis E virus (HEV) IgG antibodies, seven of these patients were negative for IgM antibodies or HEV RNA, according to a study published in Clinical Gastroenterology and Hepatology.
Eight patients (10%) tested positive for HEV RNA, but only four of these were definitely positive for HEV IgG and five for HEV IgM.
Four were initially diagnosed as having idiosyncratic drug-induced liver injury, with other diagnoses being acetaminophen intoxication, amanita intoxication, and Wilson’s disease; one patient who had received a hematopoietic stem cell transplant was initially diagnosed with graft-versus-host disease.
One patient died, two received liver transplants, and the remaining patients survived (Clin Gastro Hepatol. 2015. doi: 10.1016/j.cgh.2015.04.014).
“Our data confirms recent descriptions of cases of severe liver injury in Europe, and underlines the necessity to consider hepatitis E as an underlying or additional cause for ALF [acute liver failure],” wrote Dr. Paul Manka of the University Duisburg-Essen in Essen, Germany, and coauthors.
The study was supported by the Deutsche Forschungsgemeinschaft (German Research Foundation) and by the Wilhelm-Laupitz Foundation. There were no other conflicts of interest declared.
A significant number of cases of acute liver failure may be caused by the hepatitis E virus, which a new study suggests may not necessarily be identified or excluded using serologic tests.
A retrospective analysis of 80 European patients with acute liver failure or acute hepatitis found that, while 12 patients (15%) tested positive for hepatitis E virus (HEV) IgG antibodies, seven of these patients were negative for IgM antibodies or HEV RNA, according to a study published in Clinical Gastroenterology and Hepatology.
Eight patients (10%) tested positive for HEV RNA, but only four of these were definitely positive for HEV IgG and five for HEV IgM.
Four were initially diagnosed as having idiosyncratic drug-induced liver injury, with other diagnoses being acetaminophen intoxication, amanita intoxication, and Wilson’s disease; one patient who had received a hematopoietic stem cell transplant was initially diagnosed with graft-versus-host disease.
One patient died, two received liver transplants, and the remaining patients survived (Clin Gastro Hepatol. 2015. doi: 10.1016/j.cgh.2015.04.014).
“Our data confirms recent descriptions of cases of severe liver injury in Europe, and underlines the necessity to consider hepatitis E as an underlying or additional cause for ALF [acute liver failure],” wrote Dr. Paul Manka of the University Duisburg-Essen in Essen, Germany, and coauthors.
The study was supported by the Deutsche Forschungsgemeinschaft (German Research Foundation) and by the Wilhelm-Laupitz Foundation. There were no other conflicts of interest declared.
Key clinical point: A significant number of cases of acute liver failure may be caused by the hepatitis E virus.
Major finding: 10% of patients with acute liver failure or acute hepatitis tested positive for hepatitis E virus RNA.
Data source: A retrospective analysis of 80 patients with acute liver failure or acute hepatitis.
Disclosures: The study was supported by the Deutsche Forschungsgemeinschaft (German Research Foundation) and by the Wilhelm-Laupitz Foundation. There were no other conflicts of interest declared.